Principles of Nonoperative Fracture Treatment
One – General Principles: Basics > Principles of Treatment > 6 –
Principles of Nonoperative Fracture Treatment
fracture management until about 1750. Since then there have been
advances in operative fracture treatment, which accelerated
considerably after World War II because of improved surgical
techniques, better anesthesia and postoperative treatment, and the
introduction of antibiotics. Even today, nonoperative management
remains a very important tool in the armamentarium of the orthopaedic
trauma surgeon. The concentration of severe injuries into specialized
trauma centers in many countries has unquestionably improved their
treatment but has also caused surgeons to overestimate the role of
operative treatment in the full spectrum of fractures. In fact,
nonoperative fracture treatment remains the most common method of
fracture management, although its role has changed significantly during
the last 20 to 30 years. This chapter presents an epidemiological
analysis of nonoperative fracture management from a major trauma
center, illustrates common nonoperative techniques, and discusses
indications for their use.
fractures should be managed and to record the basic results of their
management.69 The Edwin Smith Papyrus dates from 2800 to 3000 BC and was translated in 1930 in the United States.12
It is composed of a series of case reports of specific injuries and
their associated prognoses, good and bad. Case 37 describes a
coexisting humeral fracture and wound over the upper arm. It suggests
that if the two are not connected the arm should be splinted and the
wound dressed. If the wound and fracture connect the prognosis is poor
and the ailment should not be treated! In those days, splintage relied
on bandaging over splints of wood and linen and using glue to stiffen
the bandages.
advance in fracture management until the Ancient Greek Empire, with
Hippocrates being credited with many advances that were probably the
results of clinical work of many doctors. Hippocrates
describes
six different methods of applying roller bandages depending on the
fracture location. The bandages were stiffened with cerate, which was
an ointment consisting of lard or oil mixed with wax, resin, or pitch
to essentially create a cast. It was customary to defer definitive
management, usually fracture manipulation, until the swelling had
diminished, which often took about 7 days. It is interesting to note
that delayed management still remains popular in the treatment of some
fractures. The Ancient Greeks also used mechanical aids to facilitate
the reduction of fractures and dislocations, and Hippocrates is
credited with the first audit of fracture healing time. However, he was
either an optimist or the ancient Greeks had a superior genetic makeup
because he said that femoral fractures and tibial fractures united in
50 and 40 days, respectively!45
but it is Albucasis, an Arabic physician, who is credited with
advancing nonoperative fracture treatment and for acting as a conduit
through which the philosophies of Ancient Rome and Greece could be
transferred to Western Europe. Albucasis clearly upset his colleagues
by suggesting that in femoral diaphyseal fractures the knee should be
placed in full flexion.69 His cast
was a mixture of mill dust and egg whites or mixtures of grain, herbs,
clay, and egg whites that were supported by bandages. He also
introduced the somewhat radical practice of maintaining his casts for a
longer period rather than changing them every few days, as had been
done up to that time.
shot in 1346, and half-pound gunshot in 1364, it was obvious that
surgeons were going to be faced with many more open fractures than they
had encountered before. As one would expect this stimulated innovation
and surgeons began to challenge the views that open wounds should be
encouraged to suppurate and that “laudable pus” was essential for wound
healing. Paré and others demonstrated that wounds could be cleaned and
sometimes closed primarily. Paré made the discovery that primary wound
cleaning using a paste of oil of roses, turpentine, and egg yolk gave
better results than the use of boiling oil. Paré’s views were very
influential, and the management of open wounds improved considerably.2
He and others realized that devitalized bone fragments should be
removed from open wounds but it was Desault and Larrey who introduced
debridement at the l’Hotel Dieu in Paris at the end of the 18th century.69
management of open wounds, surgeons were essentially still left with
the fracture treatment principles outlined by Albucasis around 1000 AD.
Seutin,87 a Belgian surgeon, had
introduced a method of applying rigid dressings which could be left in
position for a longer period, but it was the introduction of plaster of
Paris bandages that revolutionized fracture treatment. These were
introduced by Pirogov from Russia and Mathijsen from Holland in the
early 1800s.69 A better method of
fracture management had become essential because of the carnage caused
by the Napoleonic wars in Europe and the increased urbanization
associated with the Industrial Revolution. While plaster of Paris
bandages were not used during the American Civil War, Sayre85 and Stimson93 in New York together with Scudder86 in Boston promoted the use of plaster of Paris bandages in the United States. Volkmann103 was a particular enthusiast of the use of plaster of Paris in the management of fractures in Europe.
surgeons to accept plaster of Paris bandaging, and the use of
supportive splints such as the Thomas splint remained popular in the
United Kingdom. They were strongly supported by Hugh Owen Thomas94 and Robert Jones.50
Eventually plaster casts became the routine method of managing most
fractures and the arguments between surgeons centered around the amount
of padding that should be used, the use of early weight bearing, and
whether early joint motion could be allowed. Lorenz Böhler of Vienna7
was a particular proponent of plaster of Paris cast treatment,
believing in accurate reduction, the use of skintight casts, and
intensive physical therapy. He was also very influential in developing
a system of fracture treatment that was adopted throughout the world.
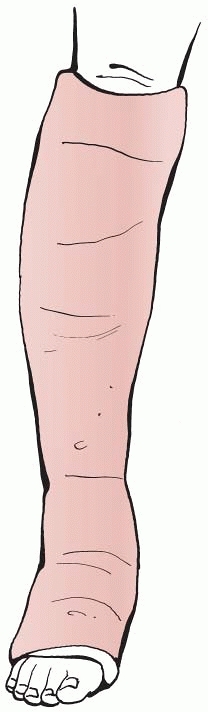
was a particular advocate of nonoperative management, particularly of
tibial fractures. He introduced a lower-leg functional brace to permit
early joint mobilization. Credit must be given to Sarmiento for
continuing to popularize nonoperative management of diaphyseal
fractures and for providing a counterargument to those surgeons who
felt that operative management was always indicated. Sarmiento’s tibial
functional brace became popular but its introduction coincided with the
explosion of interest in operative lower-limb fracture treatment, which
started in the 1960s.
around 1775 in France, and the first operative textbook detailing
techniques of fracture fixation was published by Bérenger-Féraud in
1870.6 He described six methods of
fracture management, of which three are still in use today—cerclage
wiring, interosseous sutures, and external fixation. In the 20th
century operative management rapidly increased in popularity in both
the United States and Europe. Pioneers such as Lambotte, Hey-Groves,
Lane, Hoffman, Kuntscher, Ilizarov, and Müller and his colleagues in
Europe and Parkhill, the Rush brothers, and Sherman in the United
States promoted internal and external fixation.69
However, it was the introduction of antibiotics and the development of
modern anesthesia and improved surgical techniques that altered the way
orthopaedic surgeons considered fracture management. The prevalence of
operative fracture management has now increased significantly but is
not used in all fractures. It is instructive to review the current use
of nonoperative fracture management and to compare it with 50 or 60
years ago, when many surgeons were beginning to think seriously about
operative management for the first time.
nonoperative management in a defined population of adults, although
there have been studies of the use of nonoperative treatment in more
specialized hospitals, which were not responsible for treating all
fractures in an entire community.31,39,59,95 These studies have mainly dealt with pediatric fractures39,59,95 but in 1958 Emmett and Breck31
published a paper detailing the treatment of almost 11,000 fresh
fractures in El Paso, Texas. To analyze the current role of
nonoperative management, a study of the primary treatment of 7863
consecutive fractures in Edinburgh, Scotland, in 2000 was undertaken.
To allow the examination of the role of nonoperative management in the
complete population, the fractures in adults and children have been
combined.
the Royal Infirmary of Edinburgh and The Royal Hospital for Sick
Children in Edinburgh. These two hospitals provide the only trauma care
for a defined population in the East of Scotland. In 2000 the catchment
population of the area was 643,702 patients. In the study all patients
treated in the catchment area but residing outside were excluded, and
all patients who had primary treatment outside the catchment area but
were subsequently treated within the area were included. All inpatient
and outpatient fractures were included except spinal fractures. As in
other centers these are treated by both orthopaedic surgeons and
neurosurgeons in Edinburgh, with spinal cord injury patients being
transferred to a specialized national center outside Edinburgh.
as nonoperative management but the soft tissue surgery inherent in the
management of open fractures was defined as operative treatment
regardless of whether fixation was used. Secondary procedures were not
analyzed and the management of pure dislocations and soft tissue damage
was not considered. In the study children were defined as being less
than 16 years of age, with all patients 16 years and older being
defined as adults. The basic demographic details of all patients were
included in the database. Fracture location was defined using regional
descriptors familiar to all orthopaedic surgeons. The OTA classification34 was used to classify all long bone fractures and the Carstairs and Morris index15
was used to define social deprivation. This index has been used
extensively to investigate correlation between disease and social
deprivation.27,32
In this study, it was used to test whether social deprivation
determined the choice of treatment method in different fractures.
Several measures were used to analyze fracture severity and the
subsequent decision to use operative treatment. Fracture severity was
assessed using the OTA classification34
in metaphyseal and intraarticular fractures of the long bones. OTA type
A fractures are extra-articular, type B fractures are
partial-articular, and type C fractures are complete articular
fractures. This system does not apply to proximal humeral, proximal
forearm, or proximal femoral fractures, and fracture severity was
therefore assessed in fractures of the distal humerus, distal radius,
distal femur, proximal tibia, and distal tibia. Nowadays the degree of
severity of diaphyseal fractures is often not a major factor in
determining management. This is particularly true of lower limb
diaphyseal fractures for which intramedullary nailing is now commonly
used regardless of the degree of displacement, comminution, or soft
tissue damage.
reference to the mode of injury and the presence of multiple fractures.
The seven most common modes of injury were examined to see if
particular modes of injury were associated with a higher prevalence of
operative treatment. These were motor vehicle accidents, twisting
injuries, falls, falls down stairs or slopes, falls from a height,
assaults or direct blows, and sporting injuries. The association
between operative treatment and the presence of multiple fractures was
also examined.
67.6% of fractures were nonoperatively managed in 2000 with 63% of
fractures in females and 72.8% of fractures in males being treated
nonoperatively. There is a significant difference between upper and
lower limb fractures, with 81.7% of upper limb fractures and 46.8% of
lower limb fractures being treated nonoperatively. In addition, 84.3%
of pelvic fractures were treated nonoperatively but most of these were
pubic rami fractures occurring in elderly patients.
|
TABLE 6-1 Number and Prevalence of Surgically Treated Adult Fractures Showing Gender and Regional Differences
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
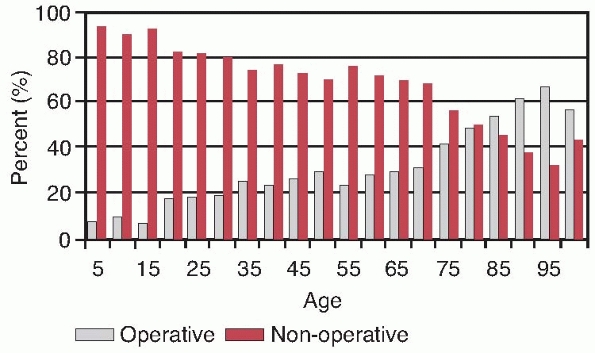
To allow for a complete analysis of the relationship between age and
the requirement for operative fracture treatment, the children’s data
from 2000 has been combined with the adult data. Figure 6-1
shows a gradual increase in operative treatment with age. Only 7.3% of
patients younger than 5 years were treated operatively compared with
56.9% of patients aged 95 years or more. At about 80 years the
prevalence of operative management overtakes nonoperative management
and the highest prevalence of operative management is seen between 90
and 94 years of age when 67.4% of patients were treated operatively.
Analysis of the equivalent results for males and females shows that
both sexes have a similar distribution to the overall distribution
shown in Figure 6-1.
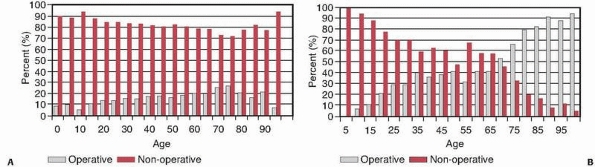
there is a progressive increase in surgery from 9.1% in patients aged
less than 5 years to 27.9% in patients aged 70 to 75 years. Older
patients show a gradual reduction in surgical treatment. In the lower
limb (Fig. 6-2B) there was no surgery
undertaken in patients less than 5 years old but in older patients
there was a gradual increase in operative treatment up to 95.1% in
patients aged 95 years or more. The prevalence of lower limb operative
surgery overtakes nonoperative treatment between 65 and 70 years of
age. Analysis of the gender-specific curves for upper and lower limb
fractures shows no difference to the overall distribution curves shown
in Figure 6-2.
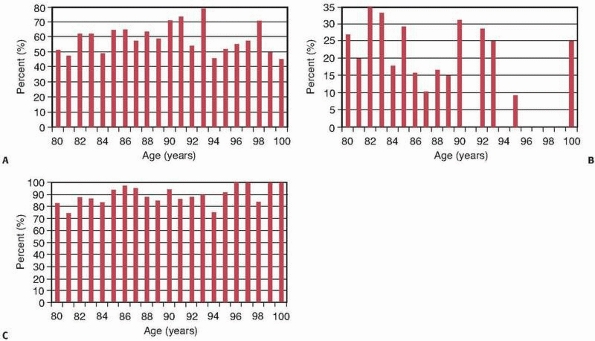
important to look carefully at the elderly. There has been an increase
in the incidence of osteoporotic fractures23,48 as well as an appreciation that many fractures that formerly occurred in younger patients now commonly occur in the elderly.21 Figure 6-3A
shows the prevalence of operative treatment in adults aged 80 years or
more, and it can be seen that there is a gradual increase in the use of
surgery to treat fractures in this group up to about 93 years of age,
when the use of surgical management begins to decline. Figures 6-3B and 6-3C show the relationship between old age and surgery in upper and lower limb fractures.
In the upper limb, Figure 6-3B
shows that 25% to 35% of adults in their early eighties who present
with upper limb fractures are treated surgically, but the prevalence
declines to the extent that only 7.4% of upper limb fractures in
patients aged 95 years or more were treated surgically. The situation
is very different in lower limb fractures, and Figure 6-3C shows that the operative treatment of lower limb fractures gradually increases in the ninth and tenth decades of life.
 |
|
FIGURE 6-1
The prevalence of operatively and nonoperatively treated fractures according to patient age. The children’s fracture data has been included and all patients have been divided into 5-year age bands. |
 |
|
FIGURE 6-2 The prevalence of operatively and nonoperatively treated upper limb (A) and lower limb (B)
fractures according to patient age. Patients are divided into 5-year age bands. The children’s data has been added to the adult data. |
 |
|
FIGURE 6-3 A. Prevalence of operative surgery in adults aged 80 years or more. B,C. Equivalent graphs for upper limb (B) and lower limb (C) fractures.
|
of nonoperative management in different fractures. It indicates that
virtually all proximal femoral, femoral diaphyseal, and tibial
diaphyseal fractures are now treated operatively, with a very high
prevalence of surgery in forearm diaphyseal fractures. There is a very
low prevalence of surgery in proximal humeral, proximal radial,
clavicular, metatarsal, and toe phalangeal fractures, and in this study
no scapular surgery was undertaken—although obviously it is sometimes
required. In the remaining fractures shown in Table 6-2,
the prevalence of operative treatment varies between 11% and 71%,
suggesting that both operative and nonoperative treatments are commonly
used. In all fractures the surgeon clearly has to decide whether to
treat the fracture operatively or nonoperatively based on many
objective and subjective criteria, in
cluding
the location and severity of the fracture and any associated soft
tissue damage; the age and medical condition of the patient; the
ability to cooperate with a postoperative treatment regime; and any
social habits such as smoking, drinking, and drug taking. Tables 6-1 and 6-2 both show that more surgical intervention is undertaken in lower limb fractures than in upper limb fractures. Table 6-2
also shows the five fractures for which multivariate analysis showed
that age was an independent predictor of fracture management. In three
fractures—those of the tibial diaphysis, humeral diaphysis, and the
pelvis—increasing age was associated with the use of nonoperative
treatment but for fractures of the proximal ulna and the distal radius
increasing age predicted surgical management.
|
TABLE 6-2 The Prevalence of Operatively Treated Fractures in Adults in Decreasing Order
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
relationship between the prevalence of operative surgery and the
severity of the fracture that has been treated. It is quite difficult
to define such a relationship in diaphyseal fractures, as Table 6-2
shows that most diaphyseal fractures tend to be treated operatively now
regardless of how serious they are. This does not apply to isolated
fractures of the ulnar diaphysis or to humeral diaphyseal fractures but
femoral, tibial, and other forearm diaphyseal fractures are now usually
treated by internal fixation. On the other hand, an analysis of the
severity of the five metaphyseal or intra-articular fractures
classified by the OTA34 shows that fracture severity is an independent predictor of surgery (Table 6-3).
The only fracture that does not appear to show such a relationship is
the distal femoral fracture and many of the patients that present with
this fracture are very elderly and frail. It is also interesting to
note that ankle fractures show a relationship between fracture severity
and the requirement for operative treatment, although the
classification basis is different from the fractures listed in Table 6-3. In the 517 ankle fractures shown in Table 6-2,
12.3% of the OTA type A ankle fractures were operatively treated
compared with 49.1% of type B fractures and 70% of type C fractures.
patients who present with multiple fractures shows that 42.1% of
fractures that occur in adults who present with multiple fractures were
treated surgically. Statistical analysis showed that the presence of
more than one fracture was an independent predictor of surgery in
fractures of the midfoot, distal radius, and metatarsus. Table 6-4
shows the prevalence of surgical treatment for the seven most common
modes of injury for those fractures in which multivariate analysis
showed that the mode of injury was an independent predictor of surgical
treatment. The seven modes of injury shown in Table 6-4
accounted for 93.4% of adult fractures. As one might expect, the
highest prevalence of surgical fracture treatment is often, but not
exclusively, related to motor vehicle accidents. Ankle fractures
following falls were more commonly treated operatively than ankle
fractures that occurred as a result of motor vehicle accidents, but
further analysis showed a higher prevalence of OTA Type C fractures in
the older population who sustained an ankle fracture as a result of a
fall. The only fracture in which social deprivation independently
determined treatment was the metacarpal. These fractures often occur in
socially deprived male adolescents and in the Edinburgh study 46.3%
followed a fight or an assault. As in many centers, these fractures
were most frequently treated nonoperatively.
|
TABLE 6-3 Prevalence of Surgical Treatment in Different Severities of Metaphyseal and Intra-articular Fractures
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
67.6% of fractures were treated nonoperatively in a major trauma unit.
One assumes that the prevalence of nonoperative management is
declining, and almost certainly this is the case, but this study
indicates that in fact nonoperative management is still the most common
overall treatment method for fractures in general. However, the overall
figure of 67.6% disguises the overall trends. Figures 6-2 and 6-3
show a difference between upper and lower limb fractures, particularly
in the elderly. It would be interesting to know if the prevalence of
surgery in different fractures is changing in response to a changing
population and to improved treatment methods.
prevalence can be assessed. There has been no previous complete
epidemiological study in adults but in a remarkable paper Emmet and
Breck31 working in El Paso, Texas,
before, during, and after World War II analyzed about 11,000 fresh
fractures. They combined their pediatric and adult fractures and
detailed the management of different fractures. The epidemiology of
their population was different from the Edinburgh population, but they
analyzed a very large number of fractures and it is interesting to
compare their results between 1937 and 1955 with the Edinburgh results
in 2000. To permit this the data from the pediatric fractures that were
treated in Edinburgh in 2000 have been combined with the adult data.
|
TABLE 6-4 Prevalence of Surgical Treatment in Different Modes of Injury and the Probability of a Statistical Association
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
They combined all of their tibial fractures, except for ankle
fractures, and they also combined talar, calcaneal, and midfoot
fractures as tarsal fractures. They separated forearm fractures into
radius and ulna fractures as well as isolated radius and ulna fractures
but they combined proximal and diaphyseal forearm fractures together.
Using Emmet and Breck’s fracture criteria the comparative data between
1937 and 1955 and 2000 are shown in Tables 6-5 and 6-6.
indicates that we operate on many more diaphyseal fractures than in the
early 1950s. The only exception appears to be the isolated radial
fracture (Table 6-6). It must be remembered that proximal radial fractures have been combined with radial diaphyseal fractures and if one looks at Table 6-2 it is obvious that we now operate on many more diaphyseal fractures than were operated on in the 1950s. Table 6-5
also shows that we operate on four or five times the amount of distal
radial fractures and this difference is undoubtedly greater if adults
alone are examined.
and see which fractures we do not operate on any more frequently than
in the 1950s. It would seem that we in fact treat fewer hand fractures
nonoperatively, and this is presumably because of the beneficial
effects of industrial legislation, which has significantly decreased
the incidence of crushed hand injuries in many countries. However, in
some parts of the world serious hand injuries are still relatively
common and operative treatment will be more common.
toe and patella fractures, surgeons now have access to superior
implants and techniques than surgeons in the 1950s. It is therefore
interesting that the treatment of fractures of the clavicle and
proximal humerus in particular seem to be much the same as 50 or 60
years ago. There are now studies suggesting that more of these
fractures may be treated surgically in the future, but only time will
tell if this occurs.14,62
Many clavicle fractures have a relatively simple morphology and the
early results of locked plating of proximal humeral fractures have not
been as encouraging as was hoped.67 Therefore, it seems likely that nonoperative management of the fractures listed in Table 6-6 will continue to be a popular treatment method. The fractures in Table 6-6
comprise 46.2% of all the fractures treated in Edinburgh in 2000 and
this explains the relatively low overall operation rate for this year.
The demographic characteristics of nonoperative fracture treatment are
summarized in Table 6-7.
treat stable fractures rather than to facilitate the reduction and
stabilization of unstable fractures. It tends to be used to treat
undisplaced or minimally displaced fractures or in patients who are
elderly, frail, or who have significant medical or social
comorbidities. However, in parts of the world with less access to
operative fixation techniques, it remains an important treatment method
for all fractures, and it is therefore important that surgeons
understand the rationale behind the use of all nonoperative techniques.
|
TABLE 6-5 Comparison of Edinburgh Data with Emmet and Breck, Fractures with an Increased Prevalence of Surgery in 2000
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
fracture management in the last 20 to 30 years, although the basic
tenets of management remain unchanged. The use of plaster of Paris
casts remains widespread as they are inexpensive and easy to apply.
However fiberglass casts are now more frequently used as they are
lighter and more radiolucent. In addition, plastic orthoses, braces,
and splints are now more frequently used. Their design has improved but
their overall function remains unchanged.
|
TABLE
6-6 Comparison of Edinburgh Data with Emmet and Breck Detailing the Fractures without an Increased Prevalence of Surgery in 2000 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
fixation of fractures after World War II centered on femoral diaphyseal
fractures. Intramedullary nailing gradually grew more popular
and
essentially superceded traction as the treatment of choice for femoral
fractures in the 1970s and 1980s, but traction is still used in parts
of the world and surgeons should understand the rationale behind its
use and its complications. In addition to the treatment of femoral
diaphyseal fractures, traction was used to treat acetabular fractures
and fracture dislocations of the hip as well as comminuted fractures of
the tibial diaphysis and distal tibia, although its role in the
management of these fractures is now extremely limited and essentially
confined to situations when internal and external fixation techniques
are unavailable. It is still used for the acute management of cervical
spine fractures.
|
TABLE 6-7 Essential Demographics of Nonoperative Management
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
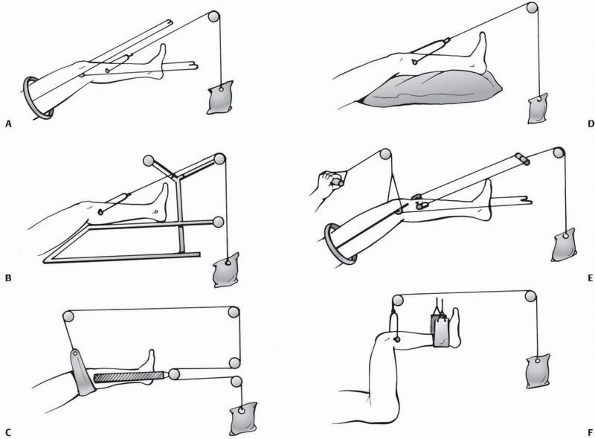
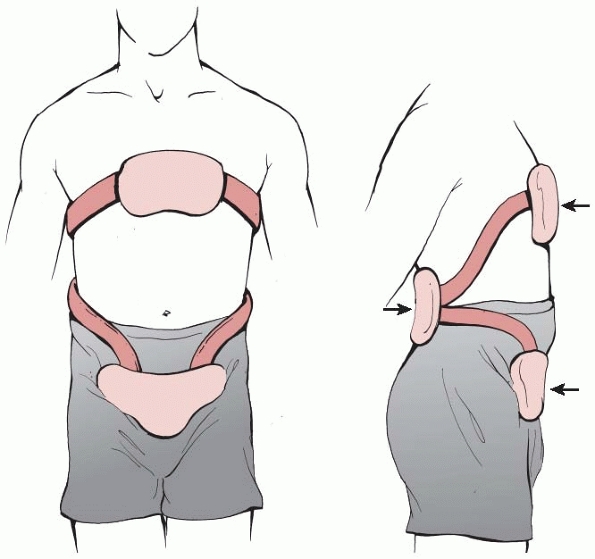
Most traction methods rely on a splint on which the leg is placed. The
proximal end or ring of the splint is placed in the patient’s groin and
traction is applied by placing a transosseous pin through the distal
femur or proximal tibia. Fixed traction is undertaken when the pin is
secured to the distal end of the splint by traction cords. In balanced
traction the splint is suspended by a pulley system and a second pulley
system is applied to the transosseous pin. Traction, using a variable
weight, then alters the fracture position with countertraction being
achieved by placing the patient head down and raising the end of the
bed. Once traction is established the fracture alignment is checked
radiologically and pads inserted appropriately to push the femur into
correct alignment. A posterior pad under the distal femur is almost
always required because of the posterior sag produced by the effect of
gravity.
The Thomas splint supports the leg and balanced traction is applied.
After 4 to 6 weeks the knee piece is applied and knee mobilization
commenced. This was a commonly used traction apparatus.
This is a very simple traction system that permits traction in the
longitudinal axis of the femur. Control of the femoral fragments was
difficult. The system, using skin rather than skeletal traction, is
still used for temporary traction prior to femoral diaphyseal surgery.
which uses a one-pulley system to provide support for the femur and to
apply traction (Fig. 6-4C). The mechanical
advantage offered by two pulleys at the foot of the bed theoretically
meant that the longitudinal pull was twice as great as the upward pull
and the resulting traction was at an axis of 30 degrees to the
horizontal, approximately in line with the femur. This method of
traction does not adequately control the femoral fragments and it was
sometimes used after a period of skeletal traction.
This is essentially a straight pull along the axis of the femur through
a proximal pin but without a splint. The control of femoral alignment
was poor and malunion was common. Perkins believed in early knee
mobilization and advocated the use of a split bed later in the
treatment of femoral diaphyseal fractures. In this system the patients
sat on a bed with the knee flexed over the mattress and knee movement
was encouraged while longitudinal traction was maintained.
This consists of a short Thomas splint and a hinged knee piece.
Traction in the axis of the femur was maintained using a proximal
tibial transosseous pin but the patient could flex the hip and knee by
pulling on a separate cord attached to the end of the thigh splint.
In this method, the thigh is pulled upward and both hip and knee are at
90 degrees. The advantage of this method is that gravity does not cause
posterior sag of the femoral fragments. It was used for proximal
femoral diaphyseal fractures when the proximal femoral fracture was
flexed by the unopposed action of iliopsoas. The method is still used
for pediatric femoral fractures.
should be reserved for cases for which no other method is available.
There is considerable morbidity associated with its use. The main
complications are failure to maintain normal femoral alignment and
significant knee stiffness. Charnley16
documented 34 cases in patients between 20 and 45 years of age with
middle and distal third diaphyseal fractures. On average, knee
mobilization was commenced at 10 to 25 weeks and the final range of
motion was 120 degrees. He also quoted very similar results from
Massachusetts General Hospital stating that 44.4% of patients, with an
average age of 37 years, had actually regained full knee function. Keep
in mind that these were selected series of patients and Charnley’s
results were not matched by other surgeons. Connolly et al.17 reported that the use of traction was associated with malunion and nonunion requiring
operative treatment in 11% to 29% of cases. Shortening of more than 2
cm occurred in 14% to 30% of cases and refracture in 4% to 17% of
cases. They pointed out that the most significant complication was knee
stiffness, which occurred in 30% to 50% of cases and affected both
elderly and younger patients. In addition to these complications,
prolonged traction is associated with significant medical problems and
decubitus ulcers. Younger patients also suffered significantly with
loss of employment and financial hardship. Psychological problems
associated with prolonged bed rest were not uncommon.
 |
|
FIGURE 6-4 Six methods of skeletal traction. See text for explanation.
|
use of a cast brace, which is essentially a long leg cast with knee
hinges to facilitate knee mobilization. This was applied after a few
weeks of bed rest but its use was far from problem free. If the surgeon
used prolonged bed rest prior to the application of the cast, patients
tended to have the problems associated with traction, and if they
shortened the period of bed rest it was difficult to apply the cast and
mobilize the patient without losing fracture alignment. Using a regime
of early application of a cast brace and mobilization, Connolly et al.17
documented a 0.7% prevalence of nonunion and malunion with 13%
shortening of more than 2 cm and 5.4% symptomatic loss of knee motion,
2% refracture, and 3% pulmonary emboli. They found the method
particularly useful for distal fractures, comminuted middiaphyseal
fractures, and open fractures. Hardy42
used a similar regime and quoted femoral malalignment in 72.2% of
patients, significant knee disfunction in 7.4%, and knee instability in
35.2% of patients. As with femoral traction, the cast brace has now
essentially disappeared and should only be used if surgical treatment
is unavailable.
of middiaphyseal comminution or if it was considered that a tibial
plafond fracture was too complex to be treated surgically. Traction was
applied through a transosseous calcaneal pin. Unfortunately, the use of
excessive traction has been shown to increase the risk of compartment
syndrome88 and even if this
complication does not occur, traction is associated with the same
complications as femoral fractures, these being malalignment, joint
stiffness, and nonunion. There is now no indication for tibial traction
unless appropriate internal or external fixation techniques are
unavailable.
and is in widespread use for the management of cervical fractures and
dislocations. It has been shown to be effective in various cervical
fractures.
Traction is commonly used to reduce a fracture or dislocation, thereby
decompressing the neural elements and providing a degree of spinal
stability. Spinal traction is rarely used for definitive management and
it is usually changed to a halo-body cast or vest, or the surgeon may
opt for later surgical stabilization. There are two principal types of
cervical traction. These are cranial tongs, of which the best known are
the Gardner-Wells tongs, and halo traction.
 |
|
FIGURE 6-5 The use of cranial tongs to apply traction.
|
that are placed into the outer table of the skull at points about 1 cm
posterior to the external auditory meatus and 1 cm superior to the
pinna of each ear. Because this is below the widest diameter of the
skull the upward pin angulation means that traction can be applied.
Each spring loaded pin is applied with an insertion torque of 6 to 8
inch pounds, and once the tongs are in position a simple pulley system
can be set up with a weight hanging over the end of the frame or bed.
Care must be exercised in applying weights in case overdistraction and
neural damage occurs.
position of the fracture, the degree of ligamentous damage, and the
size of the patient. As a rule the surgeon should start with an initial
weight of 10 pounds. Approximately 5 pounds per spinal segment are
required to reduce the fracture in most patients, although this is only
a guide. Thus a load of about 40 pounds will be required for a C5-C6
injury although the exact weight varies and serial imaging is required
to check the position as the load is increased. It is important to
obtain a lateral radiograph or fluoroscopic image to visualize fracture
reduction.
because they can tolerate higher loading than cranial tongs and can be
incorporated into a cast or brace to allow definitive treatment. The
halo is attached with four pins: two anterior and two posterior. The
pins should be inserted below the widest diameter of the skull with two
anterior pins being placed through stab incisions under local
anesthetic about 1 cm above the lateral third of the orbital rim. In
this location they are lateral to the supraorbital and supratrochlear
nerves. The posterior pins are placed about 1 cm above the helix of the
ear and to prevent skin necrosis they should not make contact with the
ear. Opposing pins should be tightened at the same time to avoid pin
displacement, with the pins then being retightened 24 to 48 hours after
the initial application. If a pin loosens it can be retightened once to
8 inch pounds.
 |
|
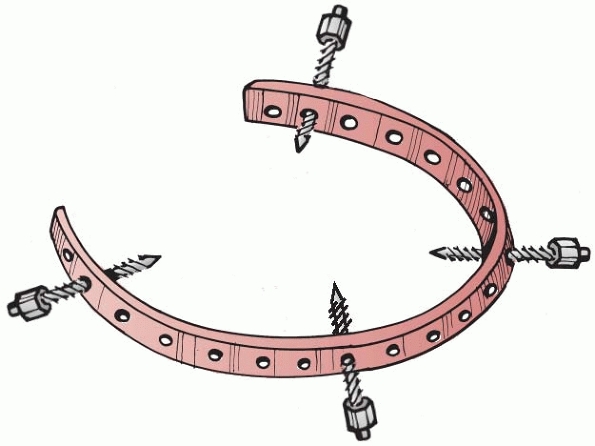
FIGURE 6-6 A halo ring.
|
Halo casts may still be useful if the appropriate bracing materials are
not available or if the patient is uncooperative, but nowadays the halo
is usually attached to a vest or orthosis (Fig. 6-7),
which is made of plastic and tightened with buckles or straps. It is
attached to the halo by two anterior and two posterior rods and it is
worn until union occurs or a cervical brace is used.
traction is associated with several complications. It has been
estimated that up to 31% of normal cervical spinal motion is permitted
by halo-body orthoses and about 10% of patients lose fracture reduction.53
Thus serial radiographs are essential during treatment. As with
external skeletal fixation, pin track sepsis is a problem with it
occurring in up to 20% of patients. As the fixation is unicortical, pin
loosening is also a problem and rates of 36% to 60% have been recorded.35,60
Nerve damage, dural puncture, skull perforation, and brain abscesses
have all been reported, and when halo-body fixation is used in
quadriplegic patients there is a high incidence of pressure sores,
decubitus ulcers, and respiratory complications.35,60 Dysphagia has also been reported.
 |
|
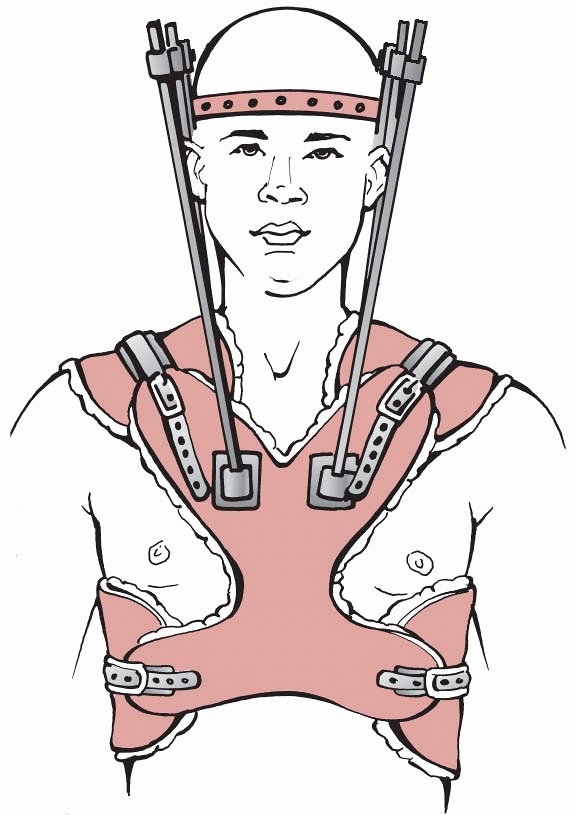
FIGURE 6-7 A halo vest.
|
thoracolumbar fractures although prolonged bed rest is still used
despite an increasing prevalence of surgical stabilization. Prolonged
immobilization necessitates the use of a rotating bed, such as a
Stryker bed, which is designed to facilitate skin care, physiotherapy,
and personal hygiene. Complications include respiratory problems and
decubitus ulcers, and intensive nursing is required. In less severe
thoracolumbar fractures the surgeon may opt for a short period of bed
rest followed by surgical stabilization or the use of a thoracolumbar
brace or orthosis.
sometimes used as a method of reducing thoracolumbar and lumbar burst
fractures prior to the application of a thoracolumbar cast.97
This technique involves the use of a Cotrel frame for a few days to
facilitate fracture reduction. At this time, this technique is not in
widespread use.
fracture treatment and probably remain the most common method of
fracture treatment throughout the world. Figures 6-2 and 6-3 and Table 6-2 show that casts are more commonly used to treat upper limb fractures but Table 6-2
also indicates that many lesssevere lower limb fractures continue to be
treated with casts. Nowadays casts are less commonly used to control
the position of a diaphyseal fracture after closed reduction but in
some metaphyseal and intra-articular fractures, such as distal radial
fractures and ankle fractures, this method of treatment is still widely
used. Casts are often used for pain management and to facilitate
mobilization in less severe fractures. The decision between cast
management and surgery is frequently subjective and influenced by the
patient’s age, physical condition, mental status, and degree of
prefracture mobility. In decades to come, it is likely that this
decision will become more difficult as the age of the patients
increases and they get progressively less fit.
-
Utilization of intact soft tissues
-
Three-point fixation
-
Hydrostatic pressure
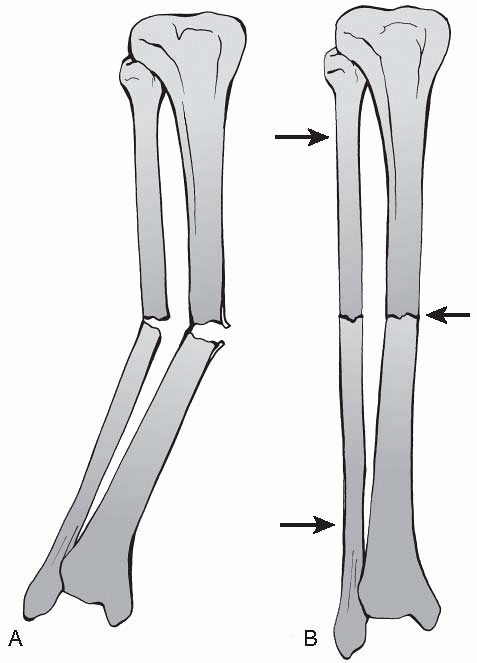
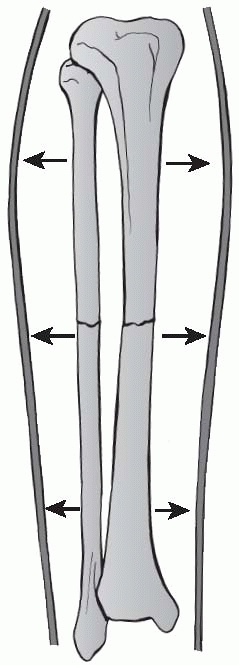
with reference to a fracture of the tibia and fibula. In theory there
will often be a hinge of intact soft tissue on one side of the
fracture, which can be used to assist with fracture reduction. If
three-point fixation is applied through the cast the fracture will be
maintained in a reduced position. This theory is somewhat naïve,
although it may well work in the OTA A3.3 tibial fracture illustrated
in Figure 6-8. However, many tibial fractures
are not transverse, and obviously the theoretical concept of a soft
tissue hinge will be less applicable in spiral, butterfly, segmental,
or comminuted fractures. In addition, there may well be soft tissue
stripping from the diaphysis adjacent to the fracture and the fracture
ends may overlap, which makes reduction more difficult. The last point
to bear in mind is that while the soft tissue hinge may be intact in
low velocity fractures in younger patients, it is unlikely to be intact
after high energy injury or in older patients. The periosteum becomes
thinner with increasing age and is more easily damaged. As many
fractures occur in older patients, the fracture reduction concepts
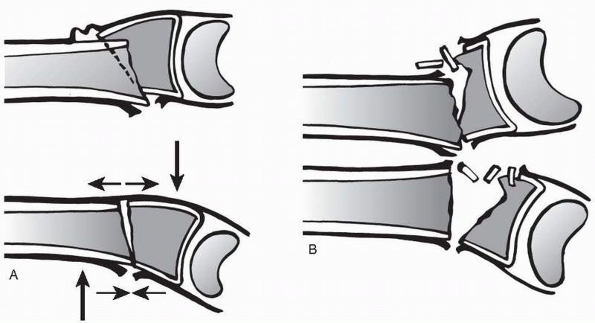
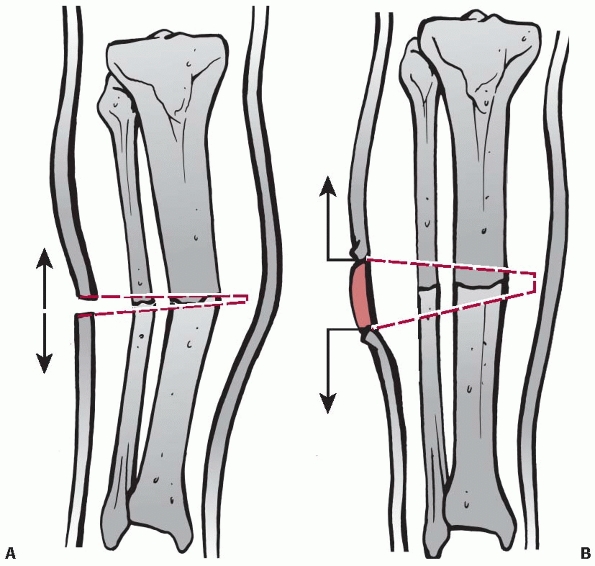
promoted by Charnley16 and others are less applicable. This is illustrated in Figure 6-9.
It shows the theoretical use of the soft tissue hinge in a metaphyseal
distal radial fracture compared with the more common distal radial
fracture in an older person, which is associated with metaphyseal
comminution and a poor or absent soft tissue hinge.
 |
|
FIGURE 6-8 A. An OTA A3.3 fracture with valgus angulation. B. Three-point fixation or pressure, will reduce fracture if a soft tissue hinge is present.
|
Hydrostatic pressure relies on the fact that the soft tissues and the
diaphysis of the bone are not compressible. Thus, when they are encased
in a complete cast or brace they essentially become rigid and maintain
the position of the fracture. As with the soft tissue hinge, the
explanation is somewhat simplistic and does not take into account
active muscle contraction around the fracture.
whether the traditional plaster of Paris or more modern fiberglass
materials are used. Both types of cast material are frequently used as
“slabs,” which are often applied to a limb soon after injury to give
temporary support. A full cast is rarely applied immediately after
injury because of the potential of swelling associated with the injury
to lead to compartment syndrome if the limb is encased in a rigid cast.
Slabs are applied by using a layer of protective stockinette and layers
of synthetic wool padding (Fig. 6-11). A slab of the appropriate length is then cut and, after
soaking, applied to the limb. The location of the slab depends on the
fracture. In the lower limb, backslabs or dorsal slabs are usually
used, these being applied to the posterior leg and calf to support the
fracture until a full cast can be applied or surgery is undertaken. In
the upper limb, humeral diaphyseal fractures are often supported with a
laterally located slab, fractures around the elbow and forearm being
supported with a posteriorly located backslab, and distal radial and
carpal fractures with a dorsal slab.
 |
|
FIGURE 6-9 A. The use of an intact soft tissue hinge and three-point fixation in a distal radial fracture in a young patient. B. The same situation in an older patient with poor soft tissues and bone comminution.
|
fiberglass bandages around the limb after stockinette and synthetic
wool have been applied (Fig. 6-12). Up to 30
years ago there was considerable debate regarding how much padding
should be used, as surgeons recognized that too much padding permitted
secondary fracture displacement but too little padding caused skin
problems and increased the risk of compartment syndrome. On the other
hand, if the cast is being used to control the position of a reduced
fracture, excessive padding should be avoided because redisplacement of
the fracture may occur. Cast bandages should be applied carefully,
keeping the bandages flat to avoid soft tissue damage. As the cast
hardens the surgeon should manipulate the fracture, taking care not to
indent the cast material, thereby compressing the underlying soft
tissue. Care must be taken not to obstruct joint motion or, if a joint
is encased by the cast, it should be placed in the correct position.
Once the cast has been applied, radiographs should be obtained to
confirm the fracture is in an acceptable position. Cast management of
unstable fractures is very labor intensive. Follow-up must be assiduous
until callus starts to stabilize the fracture, as it is easy to miss
secondary fracture displacement. If this occurs, the position of the
fracture must be corrected without undue delay as soft tissue
contracture occurs fairly quickly and secondary reduction becomes
progressively more difficult. If this occurs, it is important that the
surgeon knows how to deal with it.
 |
|
FIGURE 6-10 The principle of hydrostatic pressure in cast use. See text for explanation.
|
radiographs, or preferably fluoroscopy, are used to identify the
fracture site and the cast is cut leaving a hinge of 2 to 3 cm of the
cast intact, the location of the hinge depending on the direction of
the necessary correction. Thus if the fracture is in valgus a medial
hinge is left and a varus force applied to the distal cast to open the
window. Once opened, the position is maintained until more cast
material can be applied to maintain the reduced position. In years gone
by, plaster rooms would keep a jar of wooden dowling to insert into the
cast window to maintain the reduced fracture position while the
supplementary plaster of Paris dried. Theoretically, rotational
deformity is also correctible by cutting the cast. Again a cut is made
in the cast at the level of the fracture and the rotation is corrected,
but it is easy to lose position and sometimes it is better to remove
the cast and reapply it. Surgeons should be aware that it is difficult
to maintain the position of an unstable fracture in a cast, and that is
why earlier surgeons defined levels of “acceptable” malunion. If
the fracture position is not maintained by the cast, consideration should be given to operative treatment.
 |
|
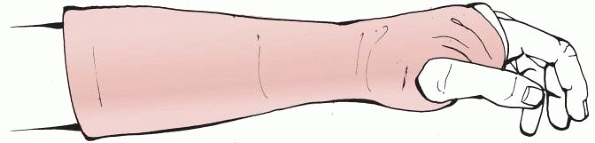
FIGURE 6-11 A forearm back slab used to treat an undisplaced distal radial fracture.
|
is less commonly used now because forearm and elbow fractures are often
internally fixed, but it is still used for less severe fractures. The
cast is applied from just below the axilla to just proximal to the
metacarpophalangeal joints of the digits but leaving the thumb free.
The wrist is placed in 30 degrees of dorsiflexion and the elbow in 90
degrees of flexion. In more minor fractures the wrist may not be
included and a full arm cylinder is then applied.
These casts are routinely used to treat humeral diaphyseal fractures in
the acute phase. The arm is placed over the lower chest with the elbow
at 90 degrees. A collar and cuff support can be used to maintain the
position. A cast is then applied as shown in Figure 6-15,
so that the top of the humeral component of the cast is above the
humeral fracture. Gravity is used to regain humeral length and the
alignment of the fracture can be theoretically adjusted by altering the
length of the cast between the neck and forearm. The shorter the cuff
the more varus is applied to the fracture. An alternative to the
hanging cast is the U-slab or sugar-tong splint, in which a plaster is
placed from just below the axilla on the medial side of the arm down
and around the elbow and then upwards to just below the shoulder. The
slab is then bandaged into position. In proximal humeral fractures the
slab can be extended above the shoulder but surgeons should be aware
that this will negate any beneficial reduction effects of gravity.
These casts are often replaced at 2 to 4 weeks by a functional brace
(see Fig. 6-23).
 |
|
FIGURE 6-12 A fiberglass scaphoid cast.
|
The Colles, or forearm cast, is the most widely used upper limb cast
and is used for most distal radial and ulnar fractures as well as for
some carpal injuries. The cast extends from below the elbow to just
proximal to the metacarpal necks of the digits with the thumb left free
(Fig. 6-16). The application of the Colles cast
is frequently preceded by the use of a dorsal plaster slab, which is
replaced by the cast once the swelling has reduced.
cast is commonly used to treat scaphoid fractures and pain in the
anatomical snuff box on the radial border of the wrist when radiographs
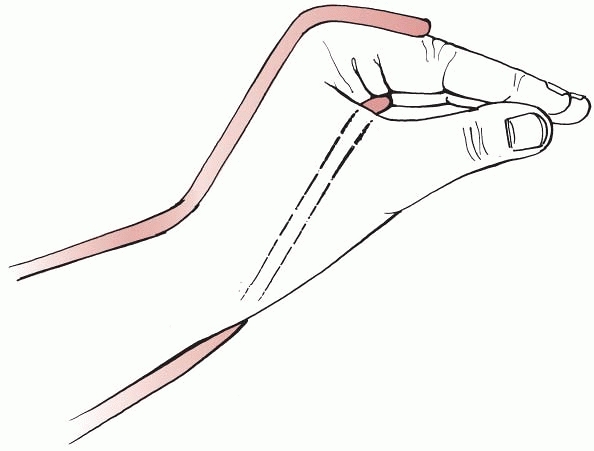
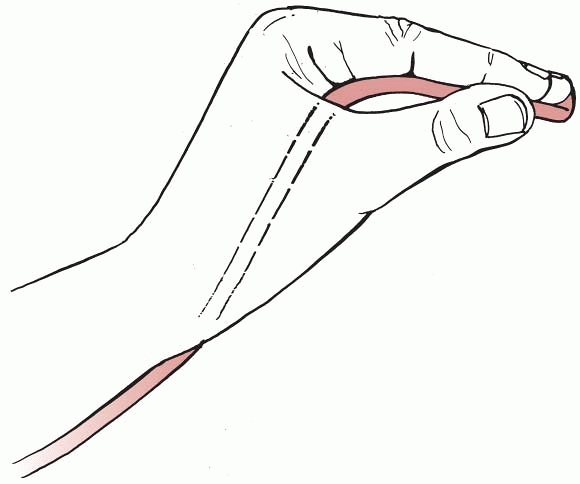
do not confirm the presence of a fracture. The wrist is held in slight
dorsiflexion and the thumb is in abduction and slight flexion as if a
glass is being held between the index finger and thumb (Fig. 6-17).
The cast extends from just below the elbow to just proximal to the
metacarpal necks of the digits. On the thumb the cast extends to just
proximal to the interphalangeal joint. A modification of the scaphoid
cast is the extended scaphoid cast, which may be used for fractures
distal to the metacarpophalangeal joint of the thumb. In the extended
scaphoid cast the whole thumb is included.
is a variant of the extended scaphoid cast that is cut short to release
the wrist joint. It is particularly useful for the treatment of
ligamentous injuries of
the thumb metacarpophalangeal joint but may be used to treat associated minor avulsion fractures.
 |
|
FIGURE 6-13 Wedging a cast to straighten a diaphyseal fracture of the tibia and fibula. A. The fracture is in valgus. The cast is cut at the level of the fracture to leave a medial hinge. B. The fracture is straightened and the gap in the cast kept open while the cast is completed.
|
is used to treat metacarpal or phalangeal fractures. The wrist is
placed in 40 degrees of extension and the metacarpophalangeal joints
are placed in 70 to 90 degrees of flexion (Fig. 6-18).
The cast relies on the intact dorsal hood of the fingers acting as a
tension band or a soft tissue hinge. It is usually applied by placing a
slab over the dorsum of the forearm and the hand, with the wrist and
fingers in the correct position and then applying a forearm cast to
secure the slab. Finger extension is not permitted by the dorsal slab
but some flexion is allowed.
 |
|
FIGURE 6-14 A long-arm cast.
|
fingers are kept in the “position of function” of the hand. The wrist
is maintained at 40 degrees of extension with the metacarpophalangeal
joints at 90 degrees and the interphalangeal joints of the fingers at
70 to 90 degrees. In this position the collateral ligaments of the
metacarpophalangeal joints and the interphalangeal joints are stretched
maximally and thus contractures will not occur (Fig. 6-19).
As with the Burkhalter cast, the James cast is in fact a combination of
a slab and a cast. Initially a volar slab is applied to the forearm
and hand with the joints in the correct position. A forearm cast is then applied.
 |
|
FIGURE 6-15 A hanging cast.
|
 |
|
FIGURE 6-16 A Colles, or forearm, cast.
|
 |
|
FIGURE 6-17 A scaphoid cast.
|
 |
|
FIGURE 6-18 A Burkhalter cast. This is a combination of a forearm cast and a dorsal slab.
|
 |
|
FIGURE 6-19 A James slab. This is volar slab that may be supplemented by a forearm cast.
|
Surgeons used to use shoulder spicas to treat factures around the
shoulder girdle. These were mainly used for clavicle or proximal
humeral fractures. Sometimes a shoulder was placed at 90 degrees of
abduction with the elbow at 90 degrees of flexion and the forearm
pronated in the “policeman’s halt position.” These casts are now very
rarely used with surgeons favoring operative management for the
fractures that they were employed to treat.
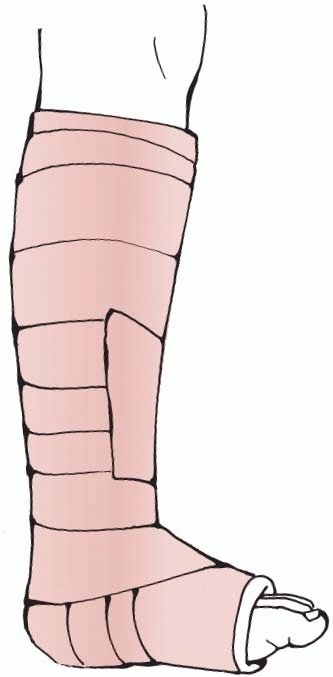
most common cast used for lower limb injury including ankle fractures,
foot fractures, and soft tissue injuries. It is occasionally used to
treat undisplaced lower tibial diaphyseal fractures or minor pilon
fractures. The cast is applied from below the level of the fibular neck
proximally to the level of the metatarsal heads distally with the ankle
at 90 degrees and the foot in the plantigrade position (Fig. 6-20). The below knee cast may be applied as a first stage in a long leg cast used to treat an unstable tibial diaphyseal fracture.
usually use a long leg cast to treat unstable tibial diaphyseal
fracture in the acute phase changing to a patellar tendon-bearing cast
after a few weeks. They may also be used to treat fractures around the
knee. A long leg cast is best constituted by applying a below knee cast
and then flexing the knee to about 10 degrees, following which the
thigh extension is applied (Fig. 6-21).
The other variant of the below knee cast is the patellar tendon-bearing
cast, which is usually used to treat tibial diaphyseal fractures after
a few weeks in a long leg cast. In this cast the proximal end of a
below knee cast
is
extended upward as far as the lower pole in the patella and moulded
around the patellar tendon to provide a degree of rotational stability (Fig. 6-22). Care must be taken not to apply pressure over the common peroneal nerve running around the neck of the fibula.
 |
|
FIGURE 6-20 A below knee cast.
|
 |
|
FIGURE 6-21 A long leg cast.
|
 |
|
FIGURE 6-22 A patella tendon-bearing cast.
|
basic cast is a plaster jacket that extends from the sternal notch to
the symphysis pubis and is carefully moulded. If fractures lower than
L3 are to be treated, the cast should be extended downwards to include
one thigh. If cervical fractures are treated in a cast, the cast is
extended upward into a collar but the use of cervical casts is now
extremely unusual and they would only be used if no other treatment
method was available. Thoracolumbar casts are still used by some
surgeons,97 but the results are no better than those associated with spinal braces.
fall into four main types used to treat fractures of the humeral
diaphysis, distal radius, metacarpus, and lower leg. Most braces are
made of polyethylene or plastic and secured by Velcro, plastic straps,
and buckles. Braces tend to be lighter than casts and are often used
after a short period of cast immobilization once the fracture is more
stable. Other advantages are that braces can be tightened as the soft
tissue swelling decreases and they can be removed for personal hygiene
and radiological evaluation of the fracture.
polyethylene or plastic brace is often used to treat humeral diaphyseal
fractures after the initial cast management. The brace fits around the
arm and is usually wider laterally than medially to support the humerus
proximally (Fig. 6-23).
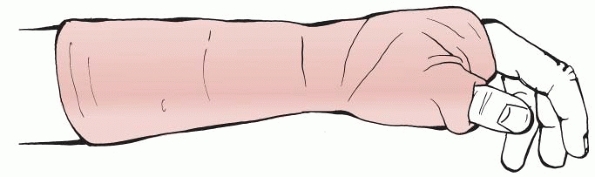
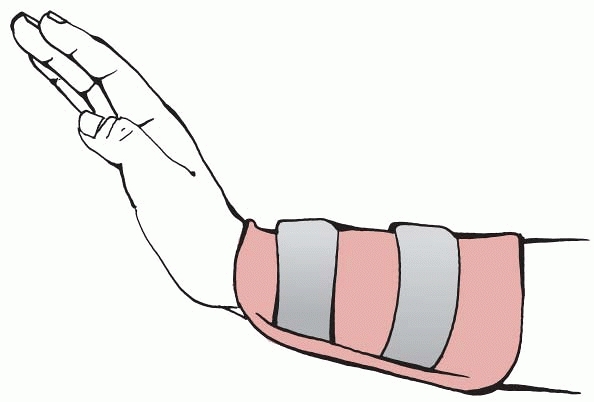
are used to treat distal radial fractures and may be used after a
period of cast immobilization or they may be applied primarily to the
forearm. There are two basic types. Figure 6-24
shows a conventional distal forearm brace, which extends to the
radiocarpal joint. Alternatively, the brace may have a dorsal extension
to just proximal to the metacarpophalangeal joints of all digits except
the thumb.
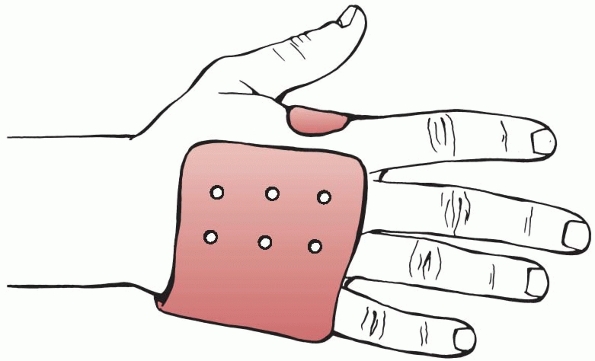
placed to maintain fracture reduction or they take the form of a
heat-molded plastic brace which is placed around the hand and then
molded into an appropriate shape to maintain fracture reduction (Fig. 6-25). They can be used for the primary treatment of metacarpal fractures40 or to protect the metacarpus after operative fracture treatment.55 Skin necrosis has been reported.36
 |
|
FIGURE 6-23 A humeral brace. The sling length can be altered to change the fracture position.
|
 |
|
FIGURE 6-24 A distal forearm brace. A modification of this brace includes an extension to just proximal to the MCPJs, except the thumb.
|
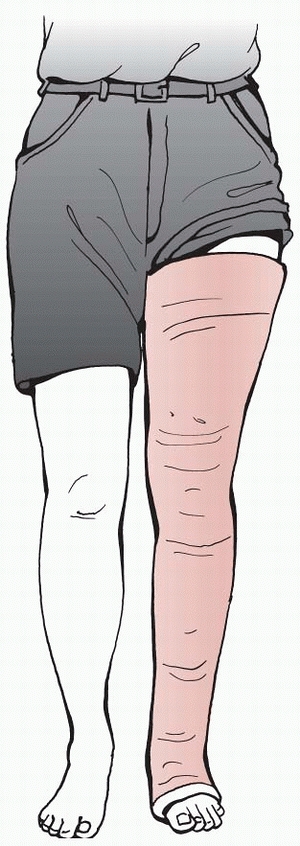
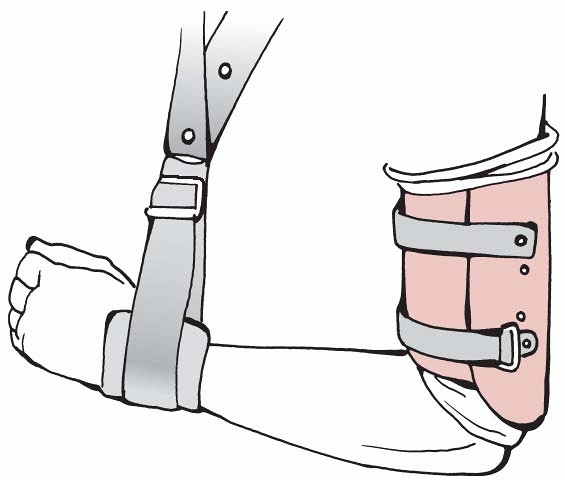
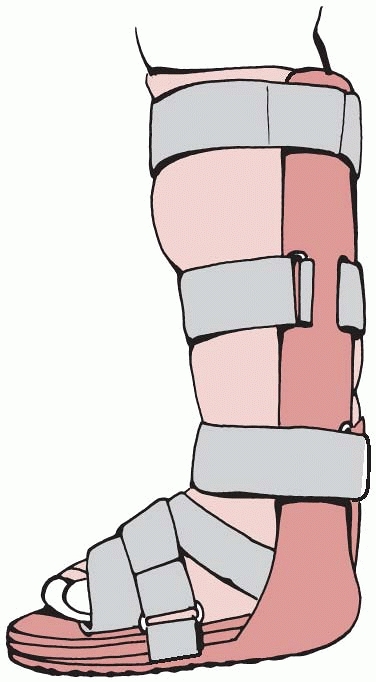
popular lower limb brace is the equivalent of the below knee cast.
There are many available but all tend to be made of plastic and fasten
with Velcro or straps (Fig. 6-26). They are
used for the same indications as below knee casts and may be used after
an initial period of cast management. They are most commonly used after
internal fixation of ankle and foot fractures or to allow mobilization
after a soft tissue injury to the ankle, hindfoot, or midfoot.
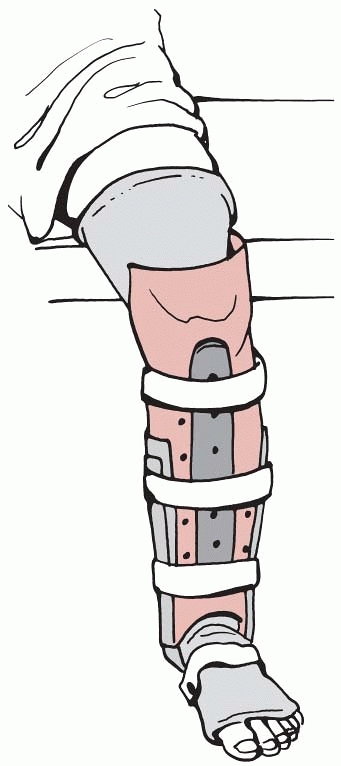
modern equivalent of the old cast brace but it is no longer used to
treat femoral diaphyseal fractures. Now it is made from synthetic
material and fitted with adjustable integral knee hinges (Fig. 6-28).
These are often used to treat soft tissue injuries around the knee but
may be used to facilitate mobilization after internal fixation of
distal femoral or proximal tibial fractures. In some minor fractures
around the knee they may be used for definitive treatment.
 |
|
FIGURE 6-25 A metacarpal brace.
|
 |
|
FIGURE 6-26 A below knee brace.
|
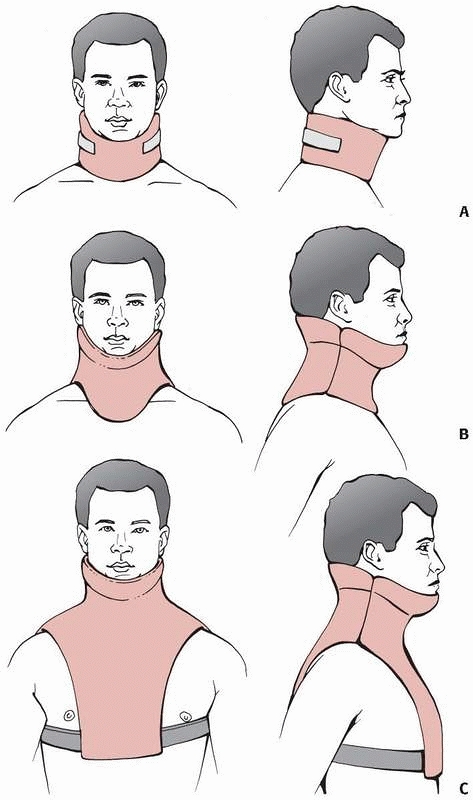
braces: soft and hard collars, high cervicothoracic orthoses, and low
cervicothoracic orthoses (Fig. 6-29A). Within
these three types there are many different designs but they all have
the same basic function. Standard soft and hard collars are not
generally used for the treatment of acute cervical fractures or
dislocations but they are useful for the treatment of minor soft tissue
sprains and whiplash injuries. They allow up to 80% of normal cervical
movement and therefore confer little stability to the cervical spine.49,60 Their main function is to act as a proprioceptive stimulus to remind patients to take care. Rigid cervical collars
may be used for emergency stabilization of the injured cervical spine
but the most effective way of stabilizing the cervical spine is by
strapping the chin and forehead to a rigid spinal board.
 |
|
FIGURE 6-27 A patella tendon-bearing brace.
|
have molded occipito-mandibular supports that extend to the upper part
of the thorax. The best-known example of this orthosis is the
Philadelphia collar. Studies indicate that the Philadelphia collar
resists 71% or normal cervical flexion and extension, 34% of lateral
bending, and 54% of rotation.60
Other similar orthoses show similar results. These types of braces are
useful for the management of cervical sprains or to provide temporary
immobilization during transport or after surgical stabilization of the
cervical spine.
 |
|
FIGURE 6-28 A knee brace.
|
 |
|
FIGURE 6-29 Different types of cervical braces. A. A cervical collar. B. A high cervicothoracic orthosis. C. A low cervicothoracic orthosis.
|
Examples of these braces are the Minerva and SOMI
(sternaloccipital-mandibular immobilizer) braces. Low cervicothoracic
orthoses are better than high cervicothoracic orthoses in resisting
cervical rotation and sagittal movement in the mid and lower cervical
spine but they do not prevent all cervical movement. If any type of
neck brace is used to treat an unstable or potentially unstable
cervical fracture serial radiographs must be taken to check that
fracture reduction is maintained until union.
as those associated with limb braces. As cervical movement is not
prevented, loss of fracture reduction may occur in unstable fractures.
In addition, a poorly fitting brace may be uncomfortable and cause skin
and soft tissue irritation and damage.60
 |
|
FIGURE 6-30 A thoracolumbarsacral orthosis.
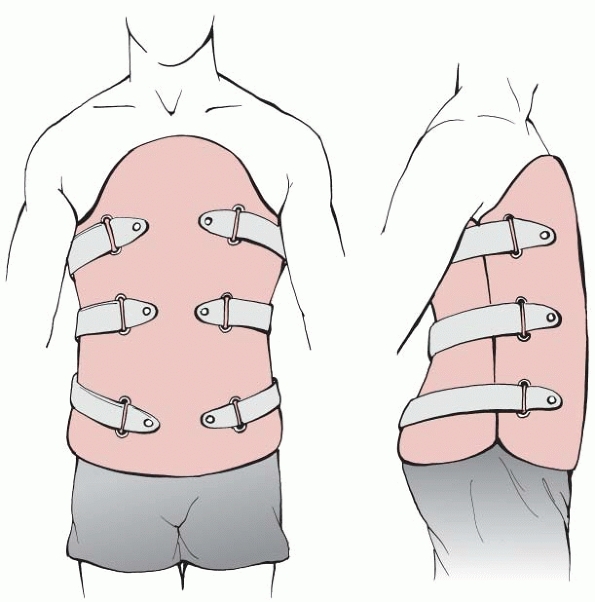
|
braces is to support the spine by limiting overall trunk motion,
decreasing muscular activity, increasing the intra-abdominal pressure,
resisting spinal loading, and limiting spinal motion. Several braces
are available; the simplest is a lumbosacral corset and the most
complex is an individually moulded thoracolumbarsacral orthosis made
from plastic and tightened by buckles and straps (Fig. 6-30). A useful intermediate brace is the Jewett brace (Fig. 6-31), which provides three-point fixation and permits spinal extension but not flexion.
 |
|
FIGURE 6-31 A Jewett brace.
|
proprioceptive and serve to remind the patient to take care. They are
used in the management of low back pain but their only use in spinal
injury is in the management of minor stable fractures or soft tissue
injury. The Jewett brace is useful in the treatment of injuries between
T6 and L3, which are unstable in flexion. Studies have shown that it
reduces intersegmental motion and flexion at the thoracolumbar joint
while lateral bending and axial rotation remain unaffected.9
They are more effective in the treatment of one- and two-column spinal
fractures than in the treatment of three-column fractures.
Thoracolumbar-sacral orthoses provide more stability but maintenance of
reduction of unstable thoracolumbar fractures cannot be guaranteed and
serial radiographs are required to confirm the maintenance of fracture
reduction.
are more useful and which gives better results. The debate is mainly
centered on tibial diaphyseal fractures, distal radial fractures, and
ankle fractures. In ankle fractures the debate has mainly concerned the
management of internally fixed fractures in the postoperative phase,
whereas in the other fractures surgeons have compared the use of casts
and braces in nonoperatively managed patients.
treatment of tibial diaphyseal fractures was a subject of considerable
debate until about 15 years ago, when intramedullary nailing became the
treatment of choice for these fractures. The implication in the
literature is that functional bracing produced better results, with
Sarmiento and colleagues being particular proponents of functional
bracing.80,81,82 Table 6-8
shows a comparison of the results of tibial fractures treated with long
leg casts, patellar tendon-bearing casts, and functional bracing. It
shows the results of the major papers published between 1965 and 1992,
when patellar tendon-bearing casts and functional braces were popular.
It must be remembered that the importance of functional outcome
following tibial diaphyseal fracture became more widely recognized
during this period, and several earlier papers extolled the virtues of
their chosen method without analyzing functional outcome to any
significant degree.
that discuss the use of long leg casts confirm that the method is
associated with significant knee stiffness, particularly if used for
complex fractures, open fractures, or in fractures that were associated
with nonunion. Few modern surgeons would treat open tibial diaphyseal
fractures with a long leg cast but it is interesting to note that Nicoll63
reported 60% delayed or nonunion in open tibial fractures managed in a
long leg cast in 1965. He also reported 25% joint stiffness rising to
70% in tibial nonunions associated with an open fracture. The results
of the use of long leg casts were reported as late as 1991, when Kyrö
et al56 analyzed the use of long leg
casts in 165 consecutive tibial fractures. Traction was used in severe
open fractures and a calcaneal pin was incorporated into the cast of
23% of the patients. They found that 26% of patients had impaired knee
flexion and 9% had impaired knee extension. In addition, 42% had
impaired ankle flexion and 37% had impaired toe movement. Only 21% of
the patients
thought that they had an excellent result. The other papers listed in Table 6-8 show the significant problems of malunion and joint stiffness associated with the use of long leg casts.
|
TABLE 6-8 Comparison of Use of Long Leg Casts, Patellar Tendon-Bearing Casts and Functional Braces
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
tendon-bearing casts and functional braces facilitated knee
mobilization but it should be remembered that during the period when
these methods of management were introduced surgeons had turned to
operative treatment for open and more severe closed fractures, and thus
the results presented in Table 6-8 for
patellar tendon-bearing casts and functional braces may well have been
achieved in more straightforward fractures than those treated by long
leg casts in earlier years. However, comparison of the results of
tendon-bearing casts with long leg casts shows a similar prevalence of
malunion and probably joint stiffness. Functional braces were
introduced to facilitate hindfoot mobility but again one must remember
that the patients analyzed in these studies almost certainly had more
benign fractures than those treated previously in long leg casts.
Sarmiento et al.82 analyzed 780
patients treated with a functional brace but selected ambulatory
patients and excluded fractures with excessive initial shortening and
those that showed an increasing angular deformity in the initial cast.
Their results were good but they did not assess malunion or joint
stiffness. Table 6-8 shows that other studies have found significant levels of malunion and joint stiffness. Digby et al.25
reviewed 103 adult tibial fractures and reported that 11% had
restricted ankle motion and 45% had reduced subtalar function. These
results match those of the other papers listed in Table 6-8,
and it is salutary to observe that a comparison of the three methods of
casting and bracing does not show that functional bracing gives
superior results, although long leg casts are associated with greater
knee stiffness.
undertook a prospective study comparing a conventional Colles cast with
an above elbow cast brace and a below elbow cast brace in the treatment
of displaced distal radial fractures. In both the above elbow and below
elbow cast brace they used a dorsal extension of the brace beyond the
wrist joint, which extended as far as the metacarpophalangeal joints of
the fingers. The brace only extended to the carpometacarpal joint of
the thumb. The authors undertook a radiographic and functional analysis
of the patients and found no statistical difference in either the
radiographic or functional results between the three different methods
of management. They also noted no difference
in
the prevalence of complications between the three groups of patients.
They did comment that there was better patient tolerance of casts than
braces with the main problem of bracing being pressure over the distal
radial border and the head of the ulna. They felt that in most patients
there was no reason to change from the traditional Colles cast.
compared the traditional Colles cast with a forearm functional brace
that did not have an extension beyond the wrist joint (see Fig. 6-24).
They treated both minimally displaced fractures, which did not require
manipulation, and displaced fractures which did require manipulation.
The results were assessed using a functional and anatomical scoring
system. They found that the brace-treated patients had lower functional
scores than the cast-treated group at 12 weeks, but the difference was
not statistically significant. By 24 weeks the results were similar.
Grip strength was initially higher in both manipulated and
nonmanipulated brace-treated groups, but by 12 weeks there was no
difference with cast-managed fractures. There was also more pain
associated with the brace during the first five weeks, but this settled
later. Their conclusion was that a brace could be used effectively in
treating Colles fractures. In a similar study O’Connor et al.65
compared a plastic cast with a lightweight removable splint in 66
patients with minimally displaced radial fractures. They also used both
anatomical and functional evaluation systems and found no significant
differences between the two groups, but patients tended to prefer the
brace.
casts and braces after operative management of ankle fractures. Tropp
and Norlon98 compared the use of a
plaster cast for 6 weeks with an ankle brace applied 1 to 2 weeks after
surgery. They permitted early weight bearing in both groups and showed
that by 10 weeks there was improved function in the brace-managed
group. This had disappeared by 12 months but they did report impaired
dorsiflexion in the cast group, compared with the functional brace
group.
examined a group of U.S. military personnel with operatively treated
ankle fractures. They compared the use of a non-weight-bearing cast for
6 weeks with the use of a non-weight-bearing removable orthosis, and
showed that the orthosis group had better subjective scores for pain,
function, cosmesis, and motion 3 and 6 months after injury, but there
was no difference in objective assessment of function on return to
duty. Simanski et al.89 compared the
use of a functional brace with early weight bearing with a standard
cast without weight bearing after ankle fixation. Both groups did well
and most of the patients achieved their preinjury level of activity.
The authors of both these studies stated that braces were useful but
emphasized the requirement of reliable, cooperative patients! In a
prospective randomized study Lehtonen et al.57
compared the use of a below knee cast and a functional brace in Weber
type A and B fractures treated operatively. There were no significant
differences between the study groups in the final subjective and
objective evaluations, but there were more wound complications in the
brace-managed group. In all studies dealing with casts or braces in
operatively managed ankle fractures, differences in outcome have been
shown to be relatively minor.
tibial diaphyseal fractures, distal radial fractures, and ankle
fractures indicate that there is no advantage of either method. The
studies suggest return of joint movement is slightly faster if a brace
is used but there is no evidence that overall function is better with a
brace. There is also some evidence that early complications are higher
if a brace is used. The choice between a brace and a cast is determined
by the surgeon and patient. Braces are obviously useful. Personal
hygiene is easier, and physical therapy, if indicated, can be more
easily undertaken, but braces are also more expensive and are not
freely available in all countries. The decision should be based on
these factors but also on the reliability of the patient. Casts have a
great advantage in that they are difficult, although not impossible, to
remove and are therefore advantageous in the treatment of many young
males in particular!
and minor fractures are treated by support and analgesia with
mobilization of the affected area encouraged after a relatively short
period. Tubular elastic support bandages are frequently used to treat
minor soft tissue injuries such as ankle and foot sprains, wrist
sprains, or minor ligament damage in other joints. Several upper limb
fractures are treated by the use of slings, which may be supplemented
by bandaging.
head and neck are often treated by sling support until the discomfort
settles enough to allow joint movement. Several different methods of
bandaging have been used to treat clavicle fractures in an effort to
reduce pain and maintain fracture reduction. The figure-of-eight
bandage remains popular in the treatment of clavicle fractures. This is
placed anteriorly around both shoulders and crossed over at the level
of the upper thoracic spine. Theoretically, tightening the bandage
reduces and stabilizes the fracture, but unfortunately it loosens
quickly and clinical evidence suggests that it is no better than a
sling.3 Fractures of the clavicle,
proximal humerus, and proximal radius that are treated nonoperatively
are best treated by the use of a sling for 2 weeks followed by
mobilization of the affected joint.
management of stable undisplaced fractures of the phalanges of the hand
and foot. These fractures can be treated by buddy strapping the
affected digit to an adjacent digit (Fig. 6-32).
Usually two strips of half-inch tape are placed around the proximal and
middle phalanges with protective gauze between the fingers. The joints
should be left free to permit mobilization. It should be remembered
that this type of strapping loosens quickly and the patient, or
companion, should be taught how to replace it.
may be helpful in treating sprains or minor tears of the collateral
ligaments of the thumb. It can also be used for treating minor
associated avulsion fractures. These are constructed of elastoplast
tape, which is placed around the thumb and extends down to the
carpometacarpal area. As with buddy strapping, they tend to loosen
quickly and need to be replaced. Neither buddy strapping nor
elastoplast spicas should be used to treat unstable fractures.
popular splints are the aluminium-backed foam splint (Fig. 6-34) and the mallet finger splint (Fig. 6-35).
Aluminium-backed foam splints are used for phalangeal fractures. They
are commonly applied to the volar or dorsal aspects of the digits to
immobilize fractures or joints after reduction of a dislocation. They
are also useful for immobilizing the finger after soft tissue injuries,
and a volar splint may be particularly helpful for maintaining
extension after a volar plate injury. In more unstable fractures the
surgeon may elect to use an aluminium-backed splint in the same way as
a Burkhalter (Fig. 6-18) or James (Fig. 6-19)
cast might be used. This is appropriate for a single digit fracture and
the splint is extended across the wrist joint maintaining the position
of the wrist as described for the Burkhalter or James splint.
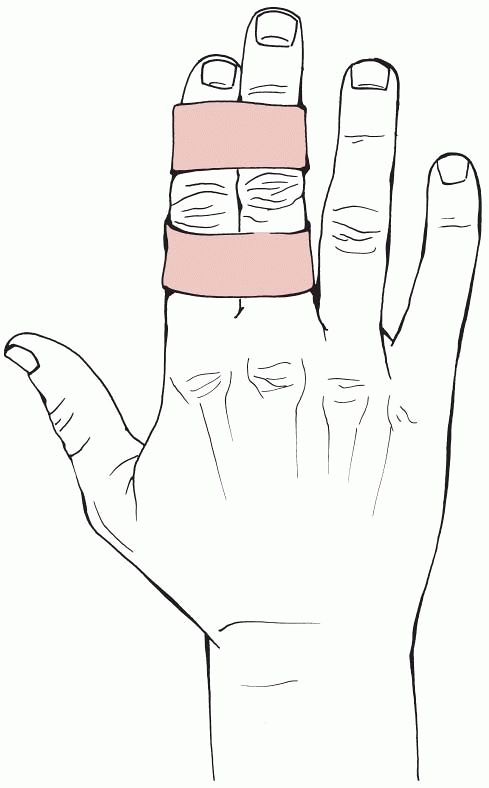 |
|
FIGURE 6-32 Buddy strapping.
|
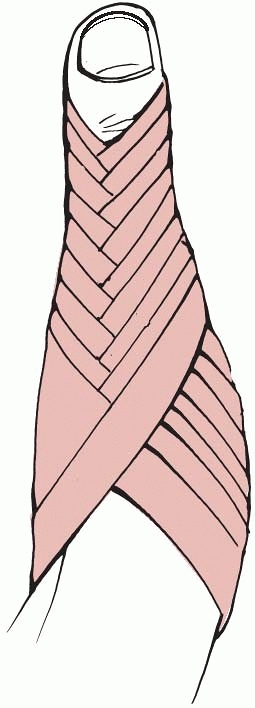 |
|
FIGURE 6-33 A thumb spica.
|
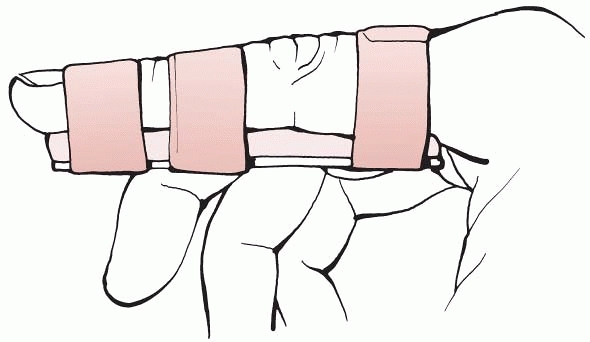 |
|
FIGURE 6-34 An aluminium-backed foam splint.
|
tendons from the distal phalanx or by a fracture of the distal phalanx
are well treated by the use of a Mallet finger splint (Fig. 6-35).
An appropriately sized splint is applied to the digit with the distal
interphalangeal joint in full extension. If this method of management
is used the patient is taught that the distal interphalangeal joint
must be kept extended for a period of 6 weeks. The main problem with
the technique is failure of the patient to follow the treatment
protocol, with the splint being removed too early.
shows that this continues to be the case. In recent years there has
been considerable interest in primary internal fixation of clavicle
fractures, with both plating and intramedullary pinning being
used.14,37,64 Not surprisingly, opinion continues to be divided regarding the best method of treatment. Nordquist et al.64
analyzed 225 consecutive clavicle fractures treated nonoperatively and
showed that 185 were symptomatic, 39 had moderate pain, and 1 patient
had a poor result. There were seven nonunions in displaced fractures.
They advocated nonoperative management as did Grassi et al., who
compared nonoperative treatment and intramedullary pinning in 80
clavicle fractures.37 They found no difference in the outcome scores between the two groups.
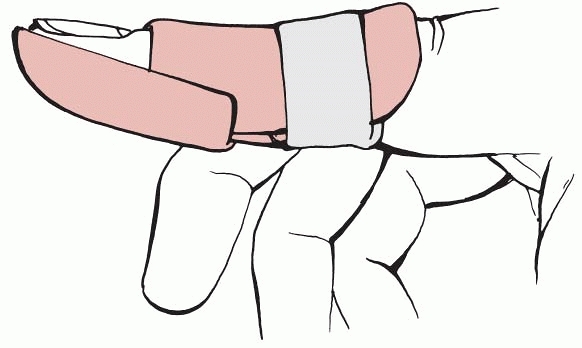 |
|
FIGURE 6-35 A mallet finger splint.
|
|
TABLE
6-9 Guidelines for Nonoperative Management for Different Upper Limb Fractures if Nonoperative Management Is Chosen as the Treatment Method* |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
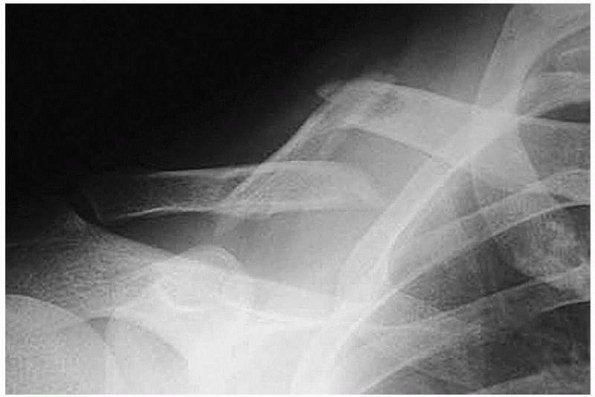 |
|
FIGURE 6-36
A clavicular fracture with a large intermediate fragment. There is debate about operative or nonoperative treatment for these fractures, but in this case union and good function was successfully achieved with nonoperative management. |
pointed out that several studies indicated there was a high prevalence
of symptomatic malunion and nonunion after nonoperative management of
midshaft clavicle fractures, and they undertook a prospective study
comparing plate fixation with nonoperative management in displaced
clavicle fractures. They found that the outcome scores were
significantly improved in the operatively managed group at all time
points and that there was a reduced union time and prevalence of
nonunion in the operatively managed fractures. They advocated plate
fixation of completely displaced midshaft clavicle fractures in active
adult patients.
will be primarily plated in the future but clearly more work is
required to establish the precise indications for operative treatment.
As many clavicle fractures are undisplaced or minimally displaced
nonoperative management will continue to be an important treatment
method and it is important to review the alternative methods of
nonoperative management.
fractures nonoperatively. The sling is usually maintained for 2 weeks
and then physical therapy is started. The historical alternative to the
sling
was the figure-of-eight bandage. The rationale behind the use of a
figure-of-eight bandage was that the shoulders were extended and
fracture reduction thereby facilitated, but comparative studies have
shown no advantage of the figure-of-eight bandage over a simple sling.
Andersen et al.3
actually found that the sling caused less discomfort and fewer
complications. If nonoperative management is used to treat a clavicle
fracture, it is suggested that a sling should be worn for about 2 weeks
and then a physical therapy regime instituted.
As with midshaft clavicle fractures, there has been debate about how
lateral clavicular fractures should be treated, with interest centring
on the Neer type 2 distal clavicle fractures associated with
transection of the coronoid and trapezoid ligaments. The treatment of
the condition will be discussed in detail in Chapter 36,
but the literature suggests that nonoperative management is a good
alternative for lateral third clavicle fractures, particularly in
middle-aged and elderly patients.76,77
As with middiaphyseal clavicle fractures, if nonoperative management is
chosen to treat a distal clavicle fracture a sling should be used for 2
weeks and a physical therapy regime then commenced.
are predominantly treated nonoperatively. The implication is that they
occur in high energy injuries and they have been documented to occur in
7% of multiple-injured patients.102 However, Chapter 3
shows that they actually have a type A distribution with a proportion
of scapula fractures occurring in the elderly and, in general,
nonoperative treatment will be used.
intra-articular and extra articular glenoid fractures, acromion
fractures, coracoid fractures, and fractures of the scapula body. Most
scapular fractures do not require operative management, the obvious
exception being the displaced glenoid rim fracture associated with
instability of the glenohumeral joint. Most coracoid and acromion
fractures are undisplaced and few require surgical treatment. In
addition, there is little evidence that scapular body fractures need
operative treatment, with a metaanalysis of scapula fractures showing
that 99% of body fractures were treated nonoperatively.106 The same study also showed that the literature indicates that 83% of scapula neck fractures are treated nonoperatively.106 Van Noort and van Kampen101 examined 13 patients with scapula neck fractures and found an average Constant score18 of 90 after nonoperative management with no correlation between functional outcome and malunion. Pace et al.68
confirmed the good outcome associated with nonoperative management but
pointed out that most patients had some activity-related pain and minor
cuff tendinopathy which, they thought, related to glenoid neck malunion.
to be treated nonoperatively and if this method of treatment is chosen,
it is suggested a sling is used for about 2 weeks to provide pain
relief, following which a physical therapy program should be
instituted. Scapular fractures are discussed in detail in Chapter 37.
to a combination of clavicle and scapular neck fractures. It was
initially felt that clavicle stabilization would minimize scapular neck
malunion44 but later papers suggest that nonoperative treatment of the floating shoulder gives equivalent or better results. Egol et al.29
compared operative and nonoperative management and showed no
significant difference between the two methods. They did note that
internal and external rotation was weaker in the operatively treated
group although there was improved forward flexion in this group.
Edwards et al.28 reported similar
results but stressed that more severely displaced fractures were
associated with poorer results. Thus the literature suggests that most
floating shoulders should be treated nonoperatively using a sling for 2
weeks followed by a course of physical therapy.
suggests that there has been little change for a considerable period.
The recent introduction of locking plates may increase the rate of
surgical treatment but this must be balanced against the increasing age
and infirmity of the elderly population who tend to present with this
fracture. It seems logical to assume that most proximal humeral
fractures will continue to be treated nonoperatively for the
foreseeable future. The overall management of this fracture is
discussed in Chapter 35.
fractures is centered around three- and four-part fractures and
fracture dislocations, which comprise about 12.5% of proximal humeral
fractures.20 Neer61
stated that 85% of proximal humeral fractures were minimally displaced
fractures, although a more recent study showed that 49% of proximal
humeral fractures were minimally displaced.19 The difference probably relates to
the increased incidence of osteopenic and osteoporotic fractures in the
population since Neer’s study. These fractures should be managed
nonoperatively. There is debate about the management of two-part
fractures, particularly with the introduction of the locking proximal
humeral plate, but these plates have only been partially successful67
and it seems likely that many two-part fractures will continue to be
managed nonoperatively. If further information about the results of
nonoperative treatment of two-part proximal humeral fractures and
fracture dislocations is required, the 1-year Neer61 and Constant18 scores of all two-part fractures classified according to the OTA classification has been published.22
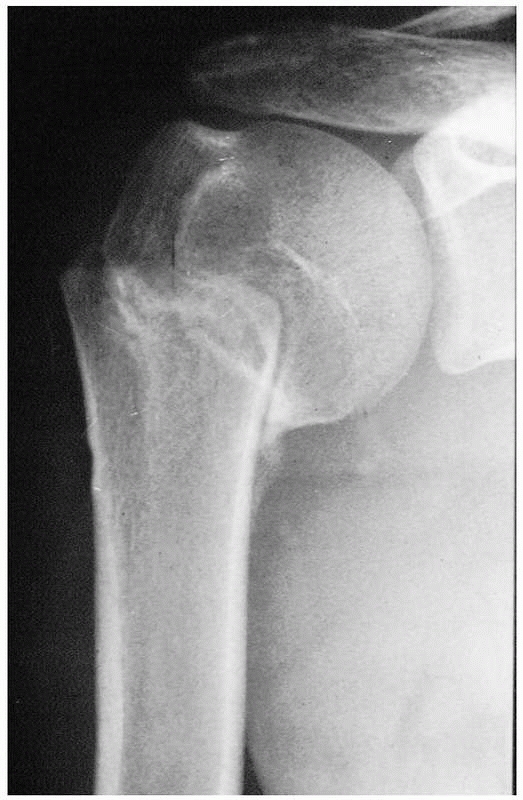 |
|
FIGURE 6-37 A varus impacted (OTA A2.2) proximal humeral fracture. This united well with a good clinical result.
|
patient in a sling for 2 weeks and then gradually introducing a program
of physical therapy. The patient should be warned that progress is slow
and that it is often more than 1 year before maximum shoulder motion is
regained.
with isolated ulnar diaphyseal fractures, humeral diaphyseal fractures
are the only diaphyseal fractures that are now commonly treated
nonoperatively. Table 6-2 also shows that
there is a significant age difference between the patients treated
operatively and those treated nonoperatively, with younger patients
tending to be treated operatively. About two thirds of patients with
humeral diaphyseal fractures are treated nonoperatively (Fig. 6-38) and this figure is supported by an analysis of the literature. In 1988, Zagorski et al.105
reported on the use of a functional brace in humeral diaphyseal
fracture. They analyzed 170 patients and showed that 167 had excellent
or good functional results. Since then, further studies30,33,47,74,78,96
have accepted that nonoperative management gives good results but they
have tried to analyze which fractures, if any, are better treated
surgically. Clearly open fractures, irreducible fractures, pathological
fractures, fractures in the multiply injured, and floating elbows may
well be treated surgically, but Ekholm et al.30
also noted that OTA type A fractures seemed to have a high prevalence
of nonunion and often required revision surgery. Ring et al.74
took a similar view stating that spiral or oblique fractures that
involved the middle or proximal third had a high rate of nonunion after
treatment with a functional brace. Toivanen et al.96
treated 93 consecutive fractures with a brace but found that 23%
required surgery. Again they found a higher rate of nonunion in
proximal third diaphyseal fractures.
 |
|
FIGURE 6-38 A. An OTA B1.2 humeral diaphyseal fracture. B. After the application of a U-slab the fracture has reduced and union occurred.
|
has been highlighted recently is impairment of shoulder function.
Fjalestad et al.93 reported that 38%
of patients treated with a humeral brace lost external rotation of the
shoulder, which they attributed to malrotation at the fracture site.
Rosenberg and Soudry78 analyzed 15
patients treated by bracing and showed that the Constant shoulder
scores were significantly lower in the injured shoulder. The average
age was only 43 years and only 40% of the patients returned to their
previous professional activities.
fractures of the distal third of the humeral diaphysis. Fracture
alignment can be difficult to maintain and there is concern about elbow
stiffness.47 Sarmiento et al.83
analyzed 85 distal third fractures, of which 15% were open. They
recorded 96% union with no infections. In a recent study Jawa et al.47
compared operative and nonoperative management and found very similar
results between them, although they stated that operative treatment
gives more predictable alignment and potentially a quicker return of
function, although there was as risk of nerve damage and infection.
treatment of humeral diaphyseal fractures will increase. As studies
have become more refined it is becoming apparent that there are
advantages to surgery in some fractures. Nonoperative management will
probably continue to be an important method of management for reducible
middle-third closed fractures but other fracture types will probably be
treated operatively more frequently than they are now. If nonoperative
management is selected, it is suggested that a U-slab or sugar-tong
cast is used for about 2 weeks and a functional brace then applied. The
brace is usually used for 8 to 12 weeks with serial radiographs used to
determine union. Active elbow motion is usually allowed by about 4
weeks. The treatment of humeral diaphyseal fractures is discussed in Chapter 34.
shows there is a considerable difference in surgery based on the OTA
classification. A review of the OTA Type 1 extra-articular distal
humeral fractures shows that nonoperative management was mainly
reserved for undisplaced or minimally displaced epicondylar fractures
or supracondylar fractures in the elderly. Most OTA Type B and C
fractures were treated operatively. The average age of the patients
with Type C fractures who were treated nonoperatively was 92 years!
Thus most displaced distal humeral fractures are treated operatively.
extra-articular distal humeral fractures. A1 fractures affecting the
epicondyle tend to occur in younger patients and A2 and A3
supracondylar fractures tend to occur in the elderly. There is debate
about whether these should be managed nonoperatively as there is a
relatively high rate of nonunion. It is likely that some Type A distal
humeral fractures will continue to be treated nonoperatively. If
nonoperative management is used for A1 fractures, a long arm cast
should be used for 4 to 6 weeks. If an A2 or A3 fracture is treated in
the elderly the cast may need to be worn for up to 8 weeks. Distal
humeral fractures are discussed in Chapter 33.
related mainly to complex fracture dislocations of the elbow and the
relatively uncommon OTA C2 and C3 fractures. Most surgeons accept that
most proximal radial fractures should be treated nonoperatively. If
nonoperative management is used, all that is required is a sling with
joint mobilization being started as soon as pain permits.
shows that most olecranon fractures are treated by internal fixation.
It also shows that those fractures treated nonoperatively tended to
occur in younger patients. Nonoperative treatment is usually used for
undisplaced fractures or if there is only a minor avulsion fracture
from the tip of the olecranon. If nonoperative management is used for a
potentially unstable olecranon fracture, a long arm cast should be
applied for 6 weeks following which a physical therapy regime is
instituted. If there is a minor avulsion fracture from the tip of the
olecranon treatment should be symptomatic and mobilization commenced
about 2 weeks after fracture. The treatment of proximal forearm
fractures is discussed in Chapter 32.
shows that over 80% of isolated radial diaphyseal and 90% of radial and
ulna diaphyseal fractures will be treated operatively. The only
exceptions are stable undisplaced fractures, which can be treated in a
cast or brace. Isolated ulna diaphyseal fractures are frequently
treated nonoperatively, with Table 6-2
indicating that about 30% are treated operatively. Many isolated ulna
diaphyseal fractures are undisplaced or minimally displaced and the use
of a cast or brace will give good results (Fig. 6-39). Sarmiento et al.84
reported on 287 ulnar shaft fractures and recorded 99% union. They
found that proximal third ulna fractures were associated with an
average loss of pronation of 12 degrees but overall there were good or
excellent
results in 96% of patients. If nonoperative management is used for
undisplaced fractures of the radius and ulna, a long arm cast should be
applied, which can be converted to a forearm cast or brace at about 6
weeks if further immobilization is required. For undisplaced isolated
fractures of the radius, a forearm cast or brace can be used, usually
for 6 weeks, and if isolated ulna fractures are to be treated
nonoperatively a forearm cast or brace can be applied for 6 weeks.
 |
|
FIGURE 6-39 A segmental ulna fracture in a 54-year-old male. The alignment is well maintained and operative treatment is not required.
|
shows that there has been an increase in operative management over the
years. There is an increased appreciation of the importance of fracture
reduction and carpal alignment and progressively more distal radial
fractures are being treated operatively. The introduction of locked
plates and different types of external fixation has altered the
management of these fractures but a substantial proportion of distal
radial fractures are stable and will continue to be managed
nonoperatively. As with other osteopenic and osteoporotic fractures the
epidemiology of distal radial fractures will be change significantly in
a rapidly aging population, who will present with more medical
comorbidities. As a result of changing patient demographics it may well
be that more distal radial fractures will be treated nonoperatively in
the future. Distal radial fracture treatment is discussed in Chapter 30.
nonoperatively, a forearm cast or brace should be applied for 6 weeks,
and following removal a physical education program instituted. If an
unstable fracture is to be treated nonoperatively, reduction needs to
be undertaken using a haematoma block, regional block, or general
anesthetic. The classic reduction technique is to apply traction,
flexion, and ulnar deviation and to check the fracture position on
radiographs or fluoroscopy. If the fracture does not reduce, the Agee
maneuver can be used (Fig. 6-41). Once the
fracture has been reduced a dorsal slab or short forearm cast is
applied. The fracture must be x-rayed 7 to 10 days after the initial
reduction to check that the reduction has been maintained. If it has
not been maintained, the surgeon must decide on further fracture
management based on the age of the patient, his or her functional
state, and the presence of medical comorbidities. Remanipulation is
generally unsuccessful in older patients, and in most cases of
redisplacement the surgeon will have to consider operative treatment,
although in very elderly demented patients the fracture will often be
left in the malreduced position. If the fracture position is maintained
the cast or slab is completed and worn for 6 weeks. Alternatively, a
functional brace can be used. Following removal of the cast or brace, a
physical therapy regime should be instituted.
indicates that the prevalence of operative treatment has recently
increased. There has been increasing interest in primary scaphoid
fixation after fracture and it seems likely that the number of scaphoid
fractures treated surgically will increase. Still, many scaphoid
fractures are minor stable fractures and it is likely that nonoperative
management will continue to be popular. A recent analysis20
showed that scaphoid fractures comprise about 82% of carpal fractures
suggesting that nonoperative management for carpal fractures will
continue to be used. A further 9% of carpal fractures were triquetral
fractures, which are also treated nonoperatively. Complex carpal
fractures and dislocations do require surgical treatment but are
relatively uncommon.
It usually needs to be worn for 6 to 8 weeks but union can be slow and
the cast may need to be worn for up to 12 weeks. If other carpal
fractures are treated a cast or brace is usually worn for 3 to 6 weeks,
depending on the type of fracture. Flake fractures of the triquetrum
usually require only 3 weeks in a forearm cast. The treatment of carpal
fractures is discussed in Chapter 29.
seem that they are more frequently treated nonoperatively than they
were 60 years ago, despite the availability of mini-plates and
minifixators. Table 6-2 shows than only about
11% of metacarpal fractures had primary operative treatment in 2000 in
a major trauma unit. It is likely that the reduction in operative
treatment relates to improved industrial and workplace safety
legislation in many countries. Crushed hands are much less common than
in the post-World War II period and an analysis of metacarpal fractures
in 2000 shows that they are mainly low energy fractures with about 50%
being caused by a direct blow. About 60% of fractures affect the little
finger metacarpal (Fig. 6-42) and 54% of these affect the metacarpal neck.20
minimally displaced metacarpal fractures usually involves the use of
buddy strapping and mobilization, although not infrequently no
supportive strapping is actually required at all. If closed reduction
is required, it can be achieved by flexing the metacarpophalangeal
joint to 90 degrees and using the proximal phalanx to push the
metacarpal head dorsally and to control rotation. This is known as the
Jahss technique. The indications for fracture reduction mainly relate
to angulation, rotation, and shortening and are discussed in Chapter 28.
Surgeons may elect to treat malreduced or unstable fractures
operatively but if nonoperative management is undertaken a Burkhalter
or James type of cast or splint should be used. These are usually
maintained for about 3 weeks, following which a physical therapy regime
is organized. Fractures of the neck, diaphyses, and bases of
metacarpals are similarly treated but basal fractures or fracture
dislocations of the thumb metacarpal may well be treated by the
application of a Brunner cast, which may be maintained for 4 to 6 weeks.
shows that we seem to operate less now. Presumably, as with metacarpal
fractures, this is because the incidence of crushed hands and severe
hand injuries has declined mainly as a result of improved workplace
legislation. As with metacarpal fractures, many phalangeal fractures
are stable and require no more than buddy strapping or the application
of an aluminium foam backed splint to minimize pain and the possibility
of secondary displacement. If phalangeal fractures are stable after
reduction they can be treated by the application of a Burkhalter or
James type splint, or by the use of a longer aluminium
backed
foam splint bent to maintain the finger in the same position as
achieved by the splint. Again the splint will be maintained for 2 to 3
weeks.
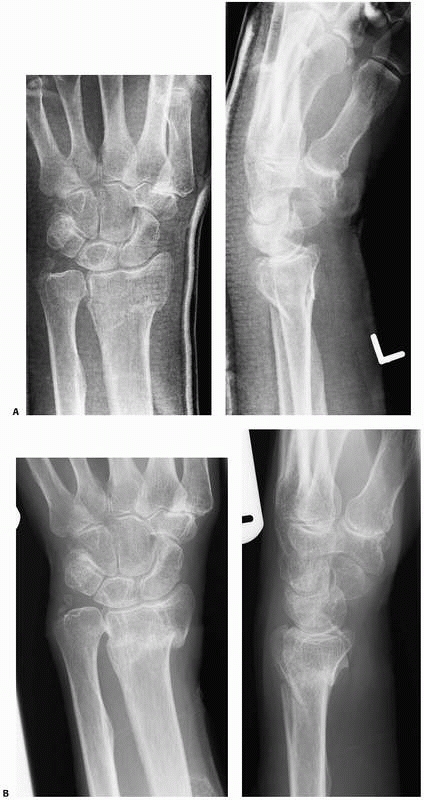 |
|
FIGURE 6-40 A. A-P and lateral radiographs of a distal radial fracture in a 68-year-old male. Note the relative lack of dorsal comminution. B. Closed manipulation was undertaken and A-P and lateral radiographs at 6 weeks show that good alignment has been maintained.
|
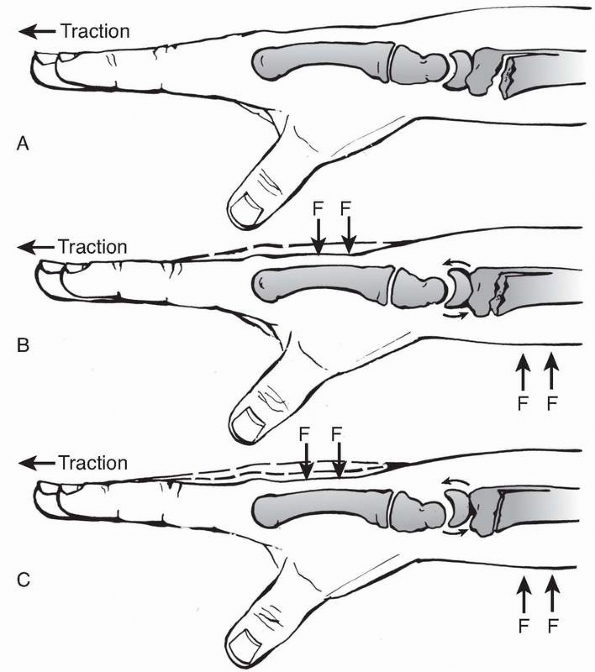 |
|
FIGURE 6-41
The Agee maneuver. This places a volar translation force on the distal radial fragment, which allows the lunate to tilt the distal fragment in a volar direction. |
nonoperatively. Tuft fractures and closed diaphyseal fractures tend to
be stable and are often treated by local splintage for pain relief.
Basal fractures of the distal phalanx are often unstable but can
frequently be treated in full extension on a splint for 4 weeks. Bony
mallet injuries are treated similarly in a mallet splint. For further
information about the treatment of phalangeal fractures see Chapter 28.
 |
|
FIGURE 6-42 A fracture of the neck of the little finger metacarpal. Most of these fractures are treated nonoperatively.
|
proximal femoral fractures are treated operatively unless the patient’s
medical condition means that surgery is contraindicated. In undisplaced
intracapsular femoral neck fractures, there is a higher prevalence of
nonunion, avascular necrosis, and fracture displacement in
nonoperatively treated fractures.20
In addition, nonoperative management means that an elderly patient,
often with significant medical comorbidities, is confined to bed for 4
to 6 weeks, which is clearly undesirable. The only proximal femoral
fracture for which nonoperative management may be the treatment of
choice is the greater trochanter fracture, when there may be little or
no displacement. Even in these fractures, surgeons should be aware that
there may be an intertrochanteric extension. Lesser trochanter
fractures are very rare but may be treated nonoperatively. In older
patients these fractures should be assumed to be metastatic fractures
until proven otherwise. The treatment of proximal femoral fractures is
discussed in Chapters 47, 48 and 49.
nonoperatively unless the patient is not fit for surgery or the
facilities to allow operative treatment are unavailable. The results
from nonoperative treatment are significantly inferior to operative
management. If nonoperative management is used then one of the methods
of traction illustrated in Figure 6-4 should
be used. There is probably no other fracture in which there is such a
strong consensus in favor of one treatment method, and intramedullary
nailing is generally used for all femoral diaphyseal fractures (see Chapter 50).
femoral fractures are treated operatively, which is what one would
expect, although in recent years there has been a significant change in
the epidemiology of distal femoral fractures. These fractures now
commonly occur in the elderly, with the epidemiological review in Chapter 3
giving an average age of 61 years for patients with this fracture. A
review of the 39.1% of distal femoral fractures that were treated
nonoperatively as detailed in Table 6-2 shows
that virtually all were undisplaced fractures in older or clinically
unwell patients. Thus, nonoperative management is now mainly used for
low-energy undisplaced fractures that commonly occur in elderly
patients. Nonoperative management will usually involve the application
of a long leg cast for about 4 weeks following which a hinged knee
brace can be applied. As fractures treated nonoperatively are usually
undisplaced, union may be fairly rapid. This is particularly true for
OTA type B partial articular fractures, which are not infrequently
undisplaced or minimally
displaced.
Under these circumstances a cast or brace may well only need to be used
for 6 to 8 weeks. The treatment of distal femoral fractures is detailed
in Chapter 51.
|
TABLE
6-10 Guidelines for Nonoperative Management for Different Lower Limb Fractures if Nonoperative Management Is Chosen as the Treatment Method* |
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||
Therefore, undisplaced or minimally displaced patella fractures are
relatively common and these are usually treated nonoperatively. Table 6-2
shows that about 35% to 40% of patella fractures are treated
operatively, these being the more serious fractures. Nonoperative
management usually involves the use of a long leg cylinder cast or
brace, which is worn for about 6 weeks. A physical therapy program is
then instituted.
were high energy injuries that occurred in younger patients, which
explains the higher incidence of operative treatment, compared with
distal femoral fractures, with almost 70% of patients being treated
operatively. As with distal femoral fractures, the patients treated
nonoperatively tend to present with undisplaced or minimally displaced
fractures (Fig. 6-43). If nonoperative
management is used for proximal tibial fractures, a hinged knee brace
should be applied for 6 to 8 weeks. If this is unavailable a long leg
cylinder cast can be used. The treatment of proximal tibial fractures
is discussed in Chapter 53.
considerably in the last 20 years. The treatment of these fractures was
the subject of much debate until relatively recently. Long leg casts,
patellar tendon-bearing casts and functional braces have all been used
to treat both closed and open tibial diaphyseal fractures (Table 6-8)
but the results were relatively poor and intramedullary nailing has
become the treatment of choice for these fractures. This is discussed
in Chapter 55. Table 6-2
shows that about 94% of tibial diaphyseal fractures were treated
operatively in Edinburgh, with nonoperative management being mainly
reserved for stable OTA A3.1 transverse tibial fractures with an intact
fibula that occur mainly in younger patients. These unite quickly and
are treated in a below knee cast.
tibial diaphyseal fracture it is recommended that a long leg cast is
applied initially and that a patellar tendon-bearing cast or brace be
applied after 4 to 6 weeks. Serial radiographs will be required to
determine when union has occurred and, therefore, when to remove the
cast. Traction should not be used to stabilize tibial diaphyseal
fractures as it is associated with increased intracompartmental
pressure and the effects of prolonged bed rest. There is now no
indication for traction. If internal fixation cannot
be used to treat a tibial diaphyseal fracture, external fixation is usually possible.
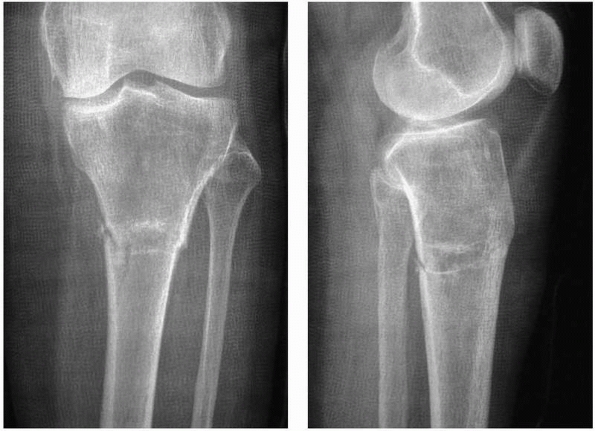 |
|
FIGURE 6-43
AP and lateral radiographs of an OTA A2.3 extra-articular proximal tibial fracture in a 78-year-old female with significant medical cormorbidities. A long leg cast was used. |
pilon fractures concerns displaced high energy fractures occurring in
younger patients. These fractures are treated operatively as detailed
in Chapter 56. Further analysis of the distal tibial fractures shown in Table 6-2 shows that about 40% of them were OTA type A extra-articular fractures and 31% were OTA type B partial articular fractures. Table 6-3
shows the prevalence of surgery in the different OTA fracture types,
and it can be seen that while most type B and all type C fractures are
treated operatively only 30% of type A fractures were treated
surgically. Of these patients, 47% were 14 to 16 years of age and had
physeal fractures, and the remaining 53% had an average age of 59 years
and presented mainly with low energy undisplaced or minimally displaced
fractures. Thus, as with other lower limb fractures, there is a
distinct difference in fracture treatment based on age, mode of injury,
and fracture displacement. If nonoperative management is to be used for
an undisplaced or a minimally displaced type A or type B pilon
fracture, a non-weight-bearing below-knee cast or brace is adequate and
it may need to be worn for 8 to 10 weeks depending on the speed of
union. In younger patients with physeal fractures the use of a cast or
brace for 4 to 6 weeks is adequate.
about 40% of ankle fractures are treated operatively. As has already
been pointed out, the prevalence of operative treatment of metaphyseal
and intra-articular fractures varies with the degree of severity of the
fracture as defined by the OTA classification (Table 6-3).
This principle also applies to ankle fractures, although their OTA
classification is somewhat different from the classifications of the
fractures shown in Table 6-3. Further analysis of the ankle fractures shown in Table 6-2
shows that about 12% of type A infrasyndesmotic fractures were treated
operatively, these mainly being isolated medial malleolar fractures.
This compares with 49% of transsyndesmotic type B fractures and 70% of
suprasyndesmotic type C fractures. Thus most type A and about half of
type B fractures will be treated nonoperatively. A review of the
patients who present with type C fractures but were treated
nonoperatively shows that most had external rotation rather than
abduction injuries and it was felt that the posterior tibio-fibula
ligaments were intact. They were considered to be stable after the
application of a cast. If this method of management is chosen, serial
radiographs must be undertaken to make sure there is no evidence of
late syndesmotic widening.
bimalleolar fractures and 94.3% of the trimalleolar fractures were
treated operatively. A review of the lateral malleolar fracture
associated with talar shift, the OTA B2.1 fracture, showed that 91.4%
of fractures were treated operatively but an analysis of the prevalence
of operative management in the common OTA B1.1 spiral lateral malleolar
fracture caused by external rotation shows that only 16.8% of these
fractures were treated operatively. It is important to realize that
B1.1 fractures associated with 2 to 3 mm of displacement do not require
operative treatment and that an excellent result can be obtained with
cast or brace management (Figure 6-44).5,54
Care must be taken to be certain that the patient does not actually
have an OTA B2.1 fracture with talar shift, and radiographs should be
obtained after the application of the cast and at 2 weeks to check for
this. If nonoperative ankle fracture treatment is undertaken a below
knee cast or brace is applied for 6 weeks. Many surgeons do not permit
weight bearing for 6 weeks after cast application but there is no good
evidence to support this regime41 and
weight bearing can be allowed in most ankle fractures. Ankle fractures are discussed in Chapter 57.
 |
|
FIGURE 6-44 A. An OTA B1.1 ankle fracture in a 50-year-old female. Note the slight lateral translation of the distal fibula. B. Surgery is not required. Union occurred with good ankle function.
|
shows that about 50% are treated operatively. A review of the
epidemiology of talar fractures has shown that about 70% are body
fractures and 30% are neck fractures.20
Further analysis of the body fractures shows that about 42% are shear
or crush injuries but 50% are fractures of the lateral or posterior
processes, which are often treated nonoperatively (Fig. 6-45).
fractures, which are also commonly treated nonoperatively. Thus while
displaced neck and body fractures will usually be treated operatively,
there are several talar fractures that will be managed nonoperatively.
If nonoperative management is to be undertaken, the use of a
non-weight-bearing below knee cast or brace for 6 to 8 weeks is
recommended. Following its removal a physical therapy regime should be
instituted. Talar fractures are discussed in Chapter 58.
These are often displaced intra-articular fractures and as such should
benefit from operative treatment. There is continued debate about the
indications for surgery and many calcaneal fractures continue to be
managed nonoperatively.13 Table 6-2
shows that in a trauma unit where fracture fixation of intra-articular
calcaneal fractures remains routine about 35% of fractures are treated
by primary operative fixation. As with talar fractures, it is important
to understand the epidemiology of calcaneal fractures in order to
understand why only 35% of fractures are treated operatively. Analysis
of the calcaneal fractures included in Table 6-2 shows that about 60% are intra-articular; the remaining 40% are extra-articular calcaneal body fractures (Fig. 6-46) or fractures of the anterior, medial, or lateral processes or of the posterior tuberosity.20
Many of these fractures will be treated nonoperatively. Also, an
analysis of types of intra-articular calcaneal fracture using the
Sanders classification79
shows that about 16% of intraarticular calcaneal fractures are
undisplaced Sanders type 1 that do not require surgery. In addition,
there are other factors that affect the choice of management in
calcaneal fractures. It is assumed that intra-articular calcaneal
fractures occur in young patients and many do, but there has been an
increasing prevalence of these fractures in older patients, with 12.7%
of the calcaneal fractures included in Table 6-2 occurring in patients of at least 65 years of age. Surgeons often treat these patients nonoperatively.
 |
|
FIGURE 6-45 A talar lateral process fracture. Most of these fractures are treated nonoperatively as are fractures of the posterior process.
|
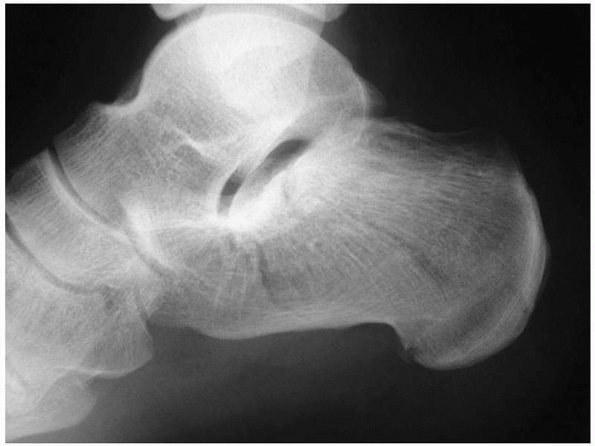 |
|
FIGURE 6-46 A calcaneal body fracture with an undisplaced fracture entering the posterior facet. Surgery is not required.
|
fractures it is suggested that a non-weight-bearing below knee cast or
brace be used for 6 weeks, and then weight bearing and a physical
therapy regime instituted. Calcaneal fractures are discussed in Chapter 59.
30% of midfoot fractures are treated operatively. A review of the
epidemiology of midfoot fractures shows that there are four basic
fracture types, these being avulsion fractures, shear fractures,
uni-articular impaction fractures, and biarticular impaction fractures.20 About 45% of midfoot fractures are avulsion fractures, which are generally treated nonoperatively (Fig. 6-47)
as operative treatment tends to be used mainly for shear fractures or
for maintaining length in the medial and lateral columns of the midfoot
in more severe fractures or fracture dislocations. The other indication
for operative treatment is if the fracture is associated with a
Lisfranc dislocation of the tarso-metatarsal joint. Thus, more severe
midfoot injuries tend to be treated operatively. If nonoperative
treatment is used it is usually for less severe injuries and the use of
a non-weight-bearing cast or brace for 6 weeks is adequate. Midfoot
fractures are discussed in Chapter 60.
shows that very few are treated operatively. About 90% of metatarsal
fractures are isolated injuries, with about 75% affecting the fifth
metatarsal.20 Most are low-energy injuries and are treated nonoperatively (Chapter 60).
Some multiple metatarsal fractures or fractures associated with
significant displacement or with a Lisfranc dislocation of the
tarso-metatarsal joint require operative treatment but these are
frequently associated with high energy injuries to the foot. Stress
fractures of the metatarsal are not uncommon and are also treated
nonoperatively. Treatment of metatarsal fractures is essentially
symptomatic. No treatment is required if the patient can manage to
mobilize without significant discomfort. If the fracture is painful, it
is suggested that a below knee cast or brace be applied for 3 weeks and
then reapplied if the pain continues. Mobilization can be allowed when
the patient can manage this.
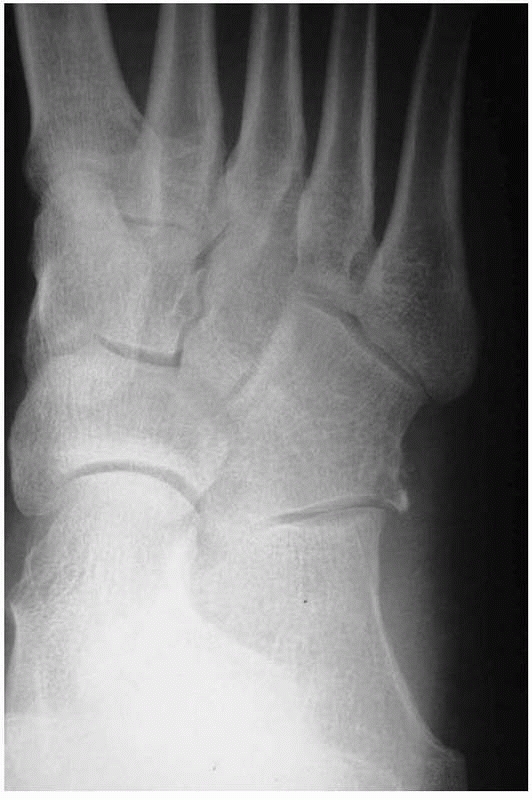 |
|
FIGURE 6-47 A minor avulsion fracture of the cuboid. This type of midfoot fracture is very common and does not require surgery.
|
metatarsal fractures, nonoperative treatment of toe fractures is very
common. Analysis of the toe phalangeal fractures in Table 6-2
shows that about 20% involved the hallux, and that five of the eight
fractures that were treated operatively were in the hallux. Surgical
treatment of the other toes is rarely required. If nonoperative
management is used, buddy strapping to the adjacent toe is usually all
that is needed, although the treatment is usually symptomatic and
frequently no treatment is actually required.
prevalence of operative management of pelvic and acetabular fractures
is relatively low. This may be surprising to surgeons working in Level
I trauma centers but it must be remembered that most fractures
involving the pelvis are insufficiency fractures of the pubic rami and
occur in the
elderly.
In the last 30 years there has been an explosion of interest in the
surgical treatment of pelvic and acetabular fractures. The pelvic
fractures that occur in younger patients that are still frequently
treated nonoperatively are the anterior posterior compression type I
injuries and the lateral compression104
type I injuries. Treatment is restricted weight bearing depending on
the degree of discomfort. Most acetabular fractures are treated
operatively with nonoperative management reserved for undisplaced
fractures with the exception of transtectal transverse fractures, which
may displace later.20 Treatment is
restricted weight bearing for 10 to 12 weeks and a physical therapy
program. Pelvic and acetabular fractures are discussed in Chapters 44 and 45.
nonoperative management of all cervical and thoracolumbar fractures,
but it is a very common method of treatment with many of the perceived
advantages of spinal fixation not having been proven in clinical
trials. The management of spinal fractures is discussed in detail in Chapters 42 and 43.
osteoporosis, together with an increased use of arthroplasty and
fracture fixation have lead to a rapid increase in the incidence of
periprosthetic fractures. These usually occur in older patients and can
be very difficult to treat. Many periprosthetic fractures will be
treated operatively but there is a role for nonoperative management in
certain circumstances. Most periprosthetic fractures associated with
arthroplasty will occur in the femur following hip or knee replacement.
The classification and management of these is detailed in Chapter 21 but if the Vancouver classification11
of proximal femoral periprosthetic fractures is employed, most Type B
and C fractures will be treated operatively with nonoperative treatment
being reserved for stable Type A fractures (Fig. 6-48).
The basic principle governing the use of nonoperative management is
that the fractures should be undisplaced or minimally displaced and the
implant should not be loose. If these conditions apply, type A proximal
femoral periprosthetic fractures can be treated by a period of
restricted weight bearing.
fractures affecting the acetabulum or distal femur. Minor undisplaced
perioperative acetabular fractures are sometimes caused by the
insertion of hemiarthroplasty prosthesis in the treatment of proximal
femoral fractures. These can be treated nonoperatively with a period of
restricted weight bearing. More severe displaced acetabular fractures
are usually treated operatively. In the distal femur Lewis and Rorabeck58
type I fractures can be treated nonoperatively as they are undisplaced
and stable, but type II and III fractures are best treated operatively.
Again a period of restricted weight bearing is used. The same
principles are applied to periprosthetic patellar and proximal tibial
fractures.
to treat. They occur in elderly patients and analysis of implant
failure has shown that loosening is relatively rare.75 Thus the surgeon may be faced with a type B104 periprosthetic fracture in osteopenic bone and a stable implant. An example of this is shown in Figure 6-49
in which there had been an earlier humeral diaphyseal fracture as well.
Nonoperative management may be the only realistic option under these
circumstances. Periprosthetic fractures associated with elbow or ankle
arthroplasties are treated using the basic principles of fracture
displacement and implant stability that have already been outlined.
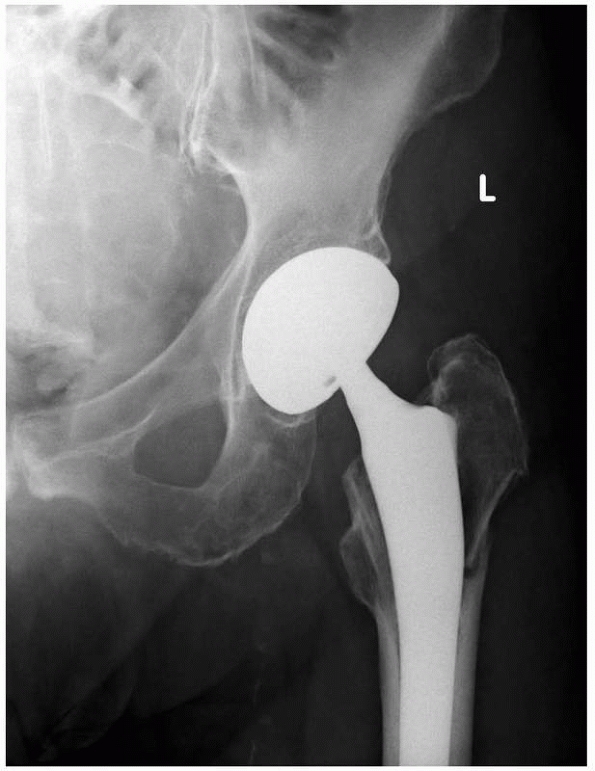 |
|
FIGURE 6-48
A Vancouver Type A fracture around the proximal stem of a stable bipolar prosthesis. This type of periprosthetic fracture generally does not need surgical treatment. |
of femoral fractures associated with proximal femoral fracture
fixation. These are most commonly associated with proximal femoral
nails but may occur after the use of compression and dynamic hip
screws. These fractures are usually displaced and there is little role
for nonoperative management.
Fatigue fractures usually occur in younger patients and, with the
exception of some fractures of the proximal femur, femoral diaphysis,
distal femur, and tibial diaphysis they are usually undisplaced and are
managed nonoperatively (Fig. 6-50). The general
principles of management are the same as described for other fractures
and the same treatment regimes outlined in Tables 6-9 and 6-10
should be followed. Insufficiency fractures occur in abnormal bone and
obviously the most common causes for these fractures are osteopenia and
osteoporosis. Many of these fractures are undisplaced and nonoperative
management will be
used. The treatments outlined in Tables 6-9 and 6-10 should be followed.
 |
|
FIGURE 6-49
A periprosthetic fracture that is virtually impossible to treat surgically. A Vancouver Type B fracture in a humerus with a old nonoperatively managed diaphyseal fracture in an 89-year-old female. The shoulder was already very stiff. |
 |
|
FIGURE 6-50 A stress fracture of the second metatarsal. The treatment is nonoperative.
|
It is difficult to be prescriptive about the role of nonoperative
treatment as it largely depends on the location of the fracture, the
type of tumor, and the medical condition of the patient. Generally
speaking, most metastatic fractures are treated operatively unless the
patient has a very short life expectancy as surgical stabilization will
diminish pain and improve the quality of the patient’s remaining life.
determine the role of nonoperative management of fractures in the
future. It is likely that fracture fixation techniques will become more
sophisticated and fractures that we now treat nonoperatively may be
shown in the future to have better results if treated operatively. It
is certain that in many parts of the world the population that is going
to present with fractures is the elderly population and it is highly
likely that the patients who present with fractures in the future will
be older and less fit than current patients. Future fracture research
will need to determine the role of operative management in elderly
patients who already have functional impairment and significant medical
comorbidities. It seems likely that as we develop into a
“super-elderly” population we will re-evaluate the role of nonoperative
management in many fractures.
bone in the belief that better fixation methods will improve the
outcome of fractures in the elderly, but it is also necessary to
consider the effect of aging on soft tissues and their recovery after
injury and surgery. It may well be that the effect of increasing age on
muscles, tendons, ligaments, and other soft tissues will negate any
advantages gained by improved operative fixation but only time will
tell.
treatment will rise, but probably not as quickly as has been the case
in the last 30 to 40 years. Improved vehicle design together with
enhanced industrial legislation, speed restrictions, and drinking and
driving laws will probably reduce the incidence of severe injuries but
there is no doubt that orthopaedic surgeons will be faced with an
epidemic of less severe fractures in the elderly.
A, Benterud JG, Hogevold HE, et al. Comparison of functional bracing
and locked intramedullary nailing in the treatment of displaced tibial
shaft fractures. Clin Orthop 1992;277:243-250.
K, Jensen PO, Lauritzen J. Treatment of clavicular fractures.
Figure-of-eight bandage versus a simple sling. Acta Orthop Scand
1987;58:71-74.
LB, Sucato D, Stegemann PM, et al. Displaced isolated fractures of the
tibial shaft treated with either a cast or intramedullary nailing. J
Bone Joint Surg (Am) 1997;79A: 1336-1341.
CM, Rinaldi M. Thoracolumbar fractures and dislocations. In:
Court-Brown CM, McQueen MM, Tornetta P, eds. Trauma. Philadelphia:
Lippincott Williams and Wilkins, 2006:226-237.
OH, Kerry R, Masri BA, et al. The Vancouver classification of
periprosthetic fractures of the hip: a rational approach to treatment.
Tech Orthop 1999;14:107-114.
R, Tough S, McCormack R, et al. Operative compared with nonoperative
treatment of displaced intra-articular calcaneal fractures: a
prospective, randomized, controlled multicenter trial. J Bone Joint
Surg (Am) 2002;84A:1733-1744.
Orthopaedic Trauma Society. Nonoperative treatment compared with plate
fixation of displaced midshaft clavicular fractures. A multicenter,
randomized clinical trial. J Bone Joint Surg (Am) 2007;89:1-10.
JF, Dehne E, Lafollette B. Closed reduction and early cast-brace
ambulation in the treatment of femoral fractures. Part II: results in
one hundred and forty-three fractures. J Bone Joint Surg (Am)
1973;55A:1581-1599.
Outer AG, Meeuwis JD, Hermans J, et al. Conservative versus operative
treatment of displaced noncomminute tibial shaft fractures. Clin Orthop
1990;252:231-237.
AJ, Jaggears FR, DePasquale LV, et al. Protected early motion versus
cast immobilization in postoperative management of ankle fractures.
Contemp Orthop 1994;29:273-277.
L, Henry J, Beard D. Socal deprivation and adult head injury: a
national study. J Neurol Neurosurg Psychiatry 2003;74:1060-1064.
SG, Whittle AP, Wood GW. Nonoperative treatment of ipsilateral
fractures of the scapula and clavicle. J Bone Joint Surg (Am)
2000;82A:774-780.
KA, Connor PM, Karunakar MA, et al. The floating shoulder: clinical and
functional results. J Bone Joint Surg (Am) 2001;83A:1188-1194.
R, Tidermark J, Törnkvist H, etc. Outcome after closed functional
bracing of humeral shaft fractures. J Orthop Trauma 2006;20:591-596.
JE, Breck LW. A review and analysis of 11,000 fractures seen in a
private practice of orthopaedic surgery 1937-1956. J Bone Joint Surg
(Am) 1958;40: 1169-1175.
JMM, Newton RW, Ruta DA, et al. Socioeconomic status, obesity, and
prevalence of Type 1 and Type 2 diabetes mellitus. Diabetic Med
2000;17:478-480.
T, Strømsøe K, Salvesen P, et al. Functional results of braced humeral
diaphyseal fractures; why do 38% lose external rotation of the
shoulder? Arch Orthop Trauma Surg 2000;120:281-285.
KR, Karpman RR. Necrosis of the skin over the metacarpal as a result of
functional fracture-bracing. J Bone Joint Surg (Am) 1989;71:1199-1202.
FA, Tajana MS, D’Angelo F. Management of midclavicular fractures:
comparison between nonoperative reatment and open intramedullary
fixation in 80 patients. J Trauma 2001;50:1096-1100.
JF, Williams EA, Hargadon ES, et al. Is conservative treatment of
displaced tibial shaft fractures justified? J Bone Joint Surg (Br)
1984;66B:84-88.
PB, Hansen TB. The treatment of fractures of the ring and little
metacarpal necks. A prospective randomized study of three different
types of treatment. J Hand Surg (Br) 1998;23B:245-247.
K, Hviid K, Jensen CM, et al. Successful immediate weight-bearing of
internally fixated ankle fractures in a general population. J Orthop
Sci 2000;5:52-54.
AE. The treatment of femoral fractures by cast-brace application and
early ambulation. A prospective review of 106 patients. J Bone Joint
Surg (Am) 1983;65A:56-65.
D, Fiennes AG, Allgöwer M, et al. The floating shoulder: ipsilateral
clavicle and scapular neck fractures. J Bone Joint Surg (Br)
1992;74B:362-364.
GJ, Keddell RG, Penny ID. Conservative management or closed nailing for
tibial shaft fractures. A randomized prospective trial. J Bone Joint
Surg (Br) 1991;73B: 83-85.
A, McCarty P, Doornberg J, et al. Extra-articular distal-third
diaphyseal fractures of the humerus. A comparison of functional bracing
and plate fixation. J Bone Joint Surg (Am) 2006;88A:2343-2347.
O, Kanis JA. An estimate of the worldwide prevalence and disability
associated with osteoporotic fractures. Osteoporos Int
2006;17:1726-1733.
RM, Hart DL, Simmons BF, et al. Cervical orthoses: a study comparing
their effectiveness in restricting cervical movement in normal
subjects. J Bone Joint Surg (Am) 1977;59A:332-339.
KD, Hansen T. Closed treatment of ankle fractures. Stage II
supinationeversion fractures followed for 20 years. Acta Orthop Scand
1985;56:107-109.
M, Blazek J, Brüner S, et al. Functional bracing after operative
treatment of metacarpal fractures. Unfallchirurg 2002;105:1109-1114.
A, Tunturi T, Soukka A. Conservative treatment of tibial fractures.
Results in a series of 163 patients. Ann Chir Gynaecol 1991;80:294-300.
H, Järvinen TLN, Honkonen S, et al. Use of a cast compared with a
functional ankle brace after operative treatment of an ankle fracture:
a prospective, randomized study. J Bone Joint Surg (Am)
2003;85A:205-211.
PL, Rorabeck CH. Periprosthetic fractures. In: Engh GA, Rorabeck CH,
eds. Revision Total Knee Arthroplasty. Baltimore: Wiliams and Wilkins,
1997.
RW, Pneumaticos SG, Gugala Z. Management techniques for spinal
injuries. In: Browner BD, Jupiter JB, Levine AM, et al., eds. Skeletal
Trauma. 3rd Ed. Philadelphia: WB Saunders, 2003:746-776.
SJ, Brophy RH, Barker JU, et al. Management of proximal humeral
fractures based on current literature. J Bone Joint Surg 2007;89(Suppl
3):44-58.
A, Pettersson CJ, Redlund-Johnell I. Midclavicle fractures in adults:
end result study after conservative treatment. J Orthop Trauma
1998;12:572-576.
D, Mullett H, Doyle M, et al. Minimally displaced Colles fractures: a
prospective randomized trial of treatment with a wrist splint or a
plaster cast. J Hand Surg (Br) 2003;28:50-53.
KC, Gorczyca JT. Fracture displacement and screw cutout after open
reduction and locked plate fixation of proximal humeral fractures. J
Bone Joint Surg (Am) 2008; 90:233-240.
M, Verbruggen JP, Brink PR. The relationship between the outcome of
operatively treated calcaneal fractures and institutional fracture
load. A systematic review of the literature. J Bone Joint Surg (Am)
2008;90A:1013-1021.
WK, Chow SP, Fang D, et al. A study of function and residual joint
stiffness after functional bracing of tibial shaft fractures. Clin
Orthop 1991;267:157-163.
RM, Teynor JT, Nagano J, et al. Critical analysis of results of
treatment of 201 tibial shaft fractures. Clin Orthop 1986;212:113-121.
D, Chin K, Taghinia AH, et al. Nonunion after functional brace
treatment of diaphyseal humerus fractures. J Trauma 2007;62:1157-1158.
CM, Page RS, Hill RM. Primary hemiarthroplasty for treatment of
proximal humerus fractures. J Bone Joint Surg (Am) 2003;85A:1215-1223.
CM. Cairns DA. Primary nonoperative treatment of displaced lateral
fractures of the clavicle. J Bone Joint Surg 2004;86A:778-782.
AS, Zuckerman JD, Shaari JM, et al. A comparison of nonoperative and
operative treatment of type II distal clavicle fractures. Bull Hosp Jt
Dis 2002;61:32-39.
N, Soudry M. Shoulder impairment following treatment of diaphyseal
fractures of humerus by functional brace. Arch Orthop Trauma Surg
2006;126:437-440.
R, Fortin P, DiPasquale T, et al. Operative treatment in 120 displaced
intraarticular calcaneal fractures: results using a prognostic computed
tomography scan classification. Clin Orthop 1993;290:87-95.
A. Gersten LM, Sobol PA. Tibial shaft fractures treated with functional
braces. Experience with 780 fractures. J Bone Joint Surg (Br)
1989;71B:602-609.
A, Horowitch A, Aboulafia A, et al. Functional bracing for comminuted
extra-articular fractures of the distal third of the humerus. J Bone
Joint Surg (Br) 1990; 72B:283-287.
A, Latta LL, Zych GA, et al. Isolated ulnar shaft fractures treated
with functional braces. J Orthop Trauma 1998;12:420-423.
DT, Henderson NJ. Compartment pressure changes during calcaneal
traction in tibial fractures. J Bone Joint Surg (Br) 1982:64:498-499.
CJ, Maegele MG, Lefering R, et al. Functional treatment and early
weightbearing after an ankle fracture: a prospective study. J Orthop
Trauma 2006;20:108-114.
Jensen J, Wang Hansen S, Johansen J. Tibial shaft fractures: a
comparison of conservative treatment and internal fixation with
conventional plates or AO compression plates. Acta Orthop Scand
1977;48:204-212.
HD, Innes AR, Burke FD. Functional cast-bracing for Colles fractures. A
comparison between cast-bracing and conventional plaster casts. J Bone
Joint Surg (Br) 1984;66B:749-753.
P, Huang RC, Louis CA, et al. Functional and radiographic outcome of
thoracolumbar and lumbar burst fractures managed by closed orthopaedic
reduction and casting. Spine 2003;28:2459-2465.
H, Norlin R. Ankle performance after ankle fracture: a randomized study
of early mobilization. Foot Ankle Int 1995;16:79-83.
N, Wardlaw D, Hallett J, et al. Aberdeen Colles brace as a treatment
for Colles fracture. A multicenter, prospective, randomized, controlled
trial. J Bone Joint Surg (Br) 2003;85:78-82.
der Linden W, Larsson K. Plate fixation versus conservative treatment
of tibial shaft fractures. A randomized trial. J Bone Joint Surg (Am)
1979;61A:873-878.
Noort A, van Kampen A. Fractures of the scapula surgical neck: outcome
after conservative treatment in 13 cases. Arch Orthop Trauma Surg
2005;125:696-700.
R. Verletzungen der knochen (knochenbruchen und knochenwunden). In:
Pithia and Billroth, eds. Handbuch der Allemeinen und Speziellen
Chirurgie. vol 2. Erlangen: Ferdinand Enke, 1865.
JWR, Burgess AR, Brumback RJ, et al. Pelvic fractures: value of plain
radiography in early assessment and management. Radiology
1986;160:445-451.
JB, Latta LL, Zych GA, et al. Diaphyseal fracture of the humerus.
Treatment with prefabricated braces. J Bone Joint Surg (Am)
1988;70A:607-610.
M, Bhandari M, Zelle BA, et al. Treatment of scapula fractures:
systematic review of 520 fractures in 22 case series. J Orthop Trauma
2006;20:230-233.
