Imaging
detection, preoperative management, surgical planning, and follow-up of
orthopaedic spinal disorders. The use of routine radiography to
identify fractures constituted the earliest application of imaging
techniques for spinal pathology. Although fracture detection and
follow-up remain common indications for spinal imaging, new imaging
modalities, such as computed tomography (CT) and magnetic resonance
imaging (MRI), allow accurate diagnosis of a broad range of osseous,
articular, and soft tissue abnormalities in the spine. Currently,
spinal imaging is used frequently for the evaluation of degenerative
disorders of the spine. The appropriate use of these modalities is
presented in relation to an accurate work-up of spinal trauma,
neoplastic disease, infection, and degenerative conditions.
radiography, MRI, CT, and myelography in the preoperative assessment of
spinal disorders. Although imaging depicts the anatomy of the various
disorders involving the spine, the importance of the physical
examination for accurate diagnosis and surgical planning cannot be
overstated. Although newer imaging modalities have high sensitivity for
the detection of apparent pathology, their specificity is low in the
absence of clinical symptoms at that particular level. Approximately
30% of asymptomatic individuals may display abnormal MRI changes
consistent with disc degeneration in the absence of clinical symptoms.
The findings from imaging studies must be used in conjunction with
clinical and laboratory findings for accurate diagnosis and optimal
patient management.
important to review the basic issues of quality assurance that apply to
all imaging modalities. Imaging studies should be labeled appropriately
with patient identification information and the date of the study. The
examination should include the entire area of interest to the surgeon.
For example, the lateral cervical spine radiograph should include C7-T1
for adequate assessment of a traumatized spine. The technical factors
unique to the imaging exam should be optimized so that there is
acceptable spatial resolution for fine anatomic detail and adequate
contrast resolution to differentiate anatomic structures. Correct
patient positioning also is crucial for diagnostic imaging studies.
These technical factors should be optimized for the best possible
imaging quality without unnecessary patient discomfort or exposure of
the patient to unwarranted high radiation doses.
groups—modalities that employ ionizing radiation and modalities that do
not. The modalities that employ ionizing radiation include radiography,
tomography, and scintigraphy. MRI does not use ionizing radiation to
form an image.
suited to assess the osseous skeleton. Assessment of the soft tissues
is limited, however, to identifying swelling, blurring, or displacement
of fat stripes; visualizing focal masses; and identifying soft tissue
gas or radiopaque foreign bodies. Despite their limited contrast
resolution, radiographs typically are the initial imaging modality
employed to assess spinal pathology. Bone lesions producing disruption
or proliferation of the vertebral cortex are visualized relatively
easily. Bone loss limited to trabecular bone from tumor, osteoporosis,
or infection is seen less easily. It has been estimated that trabecular
bone loss must be greater than 30% to 40% to be detected on
conventional radiographs. Stress radiographs are x-rays obtained at the
extremes of range of motion or during manual application of distraction
or angular stress. These views may show instability or imply
ligamentous injuries when no abnormalities are seen in the neutral
position.
technique that has been virtually replaced by CT. Synchronous motion of
the radiographic film and x-ray tube produces blurring of objects
outside the selected focal plane. This technique was used widely in the
past for assessment of
spinal
injury and spinal fusion. Conventional tomography significantly
increases radiation exposure to the patient and no longer is widely
used or available.
are obtained. CT is an important adjunct to x-rays, particularly in
complex anatomic areas, such as the spine and pelvis. The contrast
resolution for soft tissues is much better than with radiographs,
although soft tissue contrast is still less than that achieved with
MRI. CT is well suited to assess spinal trauma, particularly to
identify retropulsed bone fragments narrowing the spinal canal and to
identify posterior element fractures. Although conventional CT images
are in the axial plane, manipulating the data can reconstruct serial
axial images to create sagittal or coronal reconstructions. Reformatted
three-dimensional images also can be generated, allowing the viewer to
study the object from a variety of perspectives as the image is
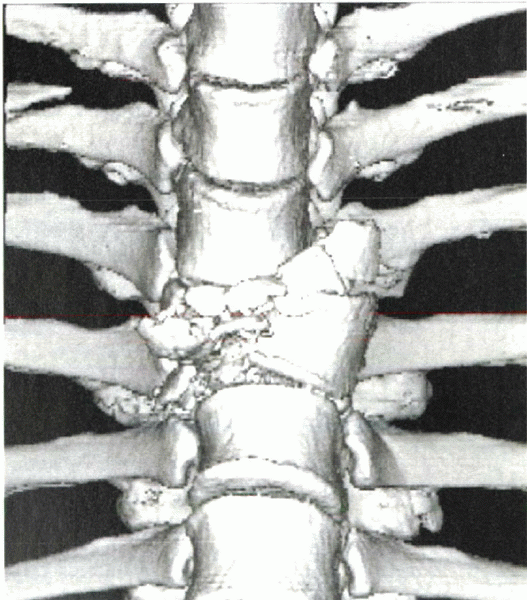
digitally rotated through space (Fig. 2-1). Metallic objects produce extensive artifact and limit the use of this technique.
diphosphonate compounds plays an important role in orthopaedic imaging.
For spinal imaging, scintigraphy is used most often to survey the
skeleton for metastatic disease and to identify stress fractures and
osteomyelitis. In contrast to CT and plain radiographs, which are
purely anatomic, scintigraphy reflects bone metabolic activity. The
spatial resolution of the exam is limited, and any lesion causing
increased turnover of bone can produce abnormal uptake, resulting in
low specificity. Single-photon emission computed tomography images
provide improved image contrast and spatial resolution.
 |
|
Figure 2-1 Three-dimensional reconstruction of a traumatic fracture-dislocation at the thoracic level.
|
imaging, myelography now has been replaced largely by planar imaging
techniques such as CT and MRI. Limitations of myelography include
complications related to the procedure, reactions to contrast material,
high radiation dose, indirect assessment of discal pathology, and
relative insensitivity to pathology in the lateral spaces and epidural
space in the lower lumbar spine. The two disorders for which
myelography still is considered necessary for accurate diagnosis are
arachnoiditis and traumatic nerve root avulsion. Currently, myelography
rarely is used for presurgical planning, unless MRI is unavailable or
contraindicated. When myelography is performed, it typically is
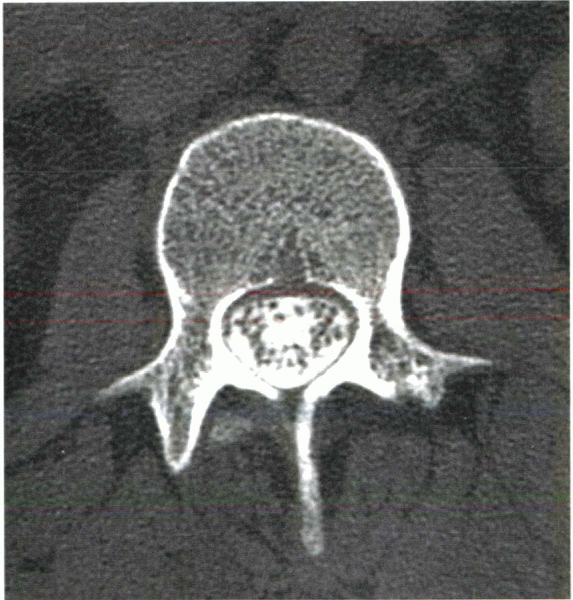
combined with postmyelography CT to assess the spinal structures
adequately (Fig. 2-2).
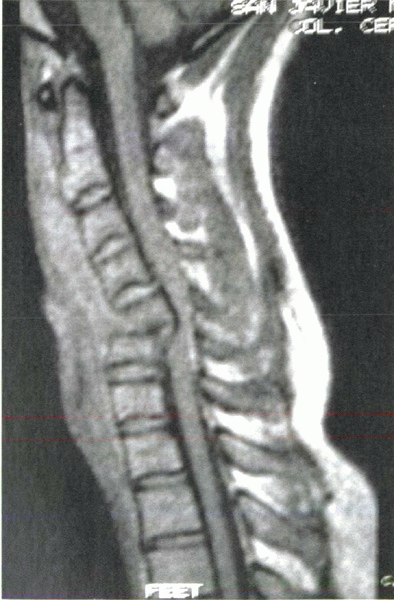
assessment of spinal disorders and is now the diagnostic imaging
technique of choice for preoperative assessment. The major advantages
of MRI are that the technique is noninvasive, is nonionizing, has
multiplanar capability, and provides excellent contrast and spatial
resolution. In contrast to CT, MRI can evaluate long segments of the
spine, allowing visualization of a broad anatomic region in one image.
The major disadvantages of MRI include relatively high cost (although
cost has decreased considerably since the 1990s), long examination
times requiring the patient to hold still, and limited availability. An
important disadvantage of MRI for the surgeon is the extreme
sensitivity of this technique to implanted metal, resulting in
artifacts that often render
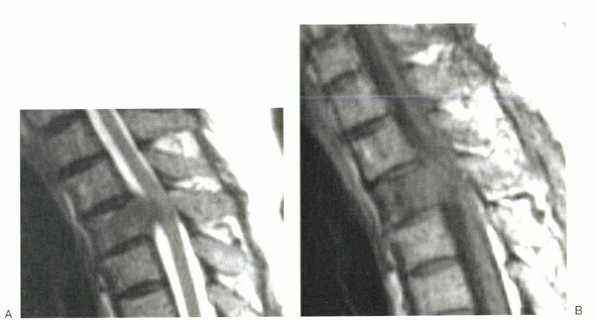
the exam uninterpretable. Stainless steel instrumentation is ferromagnetic and leads to significant artifact (Fig. 2-3),
whereas newer titanium devices do not cause any noticeable image
degradation. Absolute contraindications for MRI include implanted
pacemakers, cardiac valve replacement, implanted electrical devices,
intraocular metallic bodies. and intracranial clips.
 |
|
Figure 2-2 Normal CT myelogram shows excellent spatial resolution and detail.
|
to other modalities. Normal bone marrow in adults is of high signal
intensity on T1-weighted and T2-weighted images owing to the
predominance of fat. The intervertebral disc, which has a low signal on
T1 images and increases to intermediate high signal on T2 images, is
seen well and separated easily from adjacent tissues. Although
mineralized bone is not as well seen as with CT, the adjacent medullary
changes render MRI more sensitive than CT for bone trauma,
osteomyelitis, and marrow replacement processes. MRI is an excellent
technique to assess spinal tumors. Marrow replacement by tumor and soft
tissue abnormalities are detected more accurately than with CT, and the
multiplanar capabilities of MRI allow accurate anatomic staging of the
lesion.
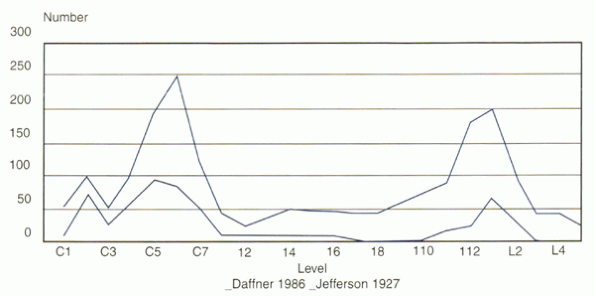
United States sustain a spinal cord injury. The early identification,
immobilization, and treatment of spinal cord injury and spinal trauma
are paramount in preventing further morbidity or mortality. Spinal
trauma is categorized by the location of the injury, its presumed
mechanism, and the presence or absence of instability. The most common
locations of injury include the lower cervical and thoracolumbar
regions (Fig. 2-4). The most common mechanisms are flexion and axial loading.
 |
|
Figure 2-3 Postsurgical MRI shows significant hardware artifact from ferromagnetic metallic implants.
|
radiographs. Advanced imaging often is required, however, for a
complete assessment of injury to the intervertebral discs, interspinous
ligaments, and direct cord injury (Fig. 2-5).
Initial radiographic evaluation of the traumatized spine begins with
conventional radiography, with the spine still protected by a cervical
collar. A cervical spine series comprises a lateral view that includes
the cervicothoracic junction, an anteroposterior view, and an odontoid
view. If the lateral radiograph is inadequate secondary to body habitus
or technique, a swimmer’s view is obtained. Certain soft tissue “red
flags” must be kept in mind. Greater than 5 mm of soft tissue swelling
at the anteroinferior margin of C2 is considered abnormal. Greater than
14 mm of soft tissue swelling below the arytenoid cartilage level (C3-4
vertebral bodies) also is considered abnormal. The radiographs also are
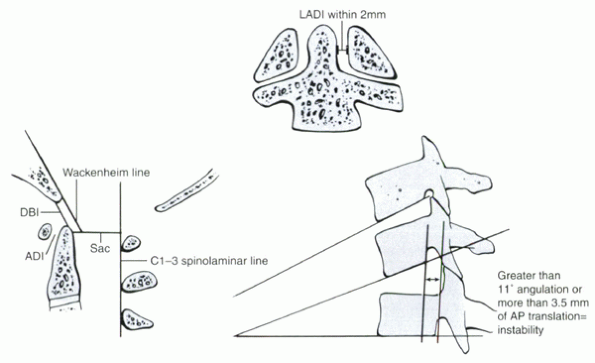
evaluated for spinal alignment, by assessing the normal “spinal lines” (Fig. 2-6)
and adjacent segment angulation. The posterior vertebral margins and
the spinolaminar lines are most useful in the overall assessment of
spinal alignment. Findings indicating traumatic cervical spine
instability include greater than 3 mm of anterior or posterior
translation (Fig. 2-7), angulation greater than
11 degrees compared with other contiguous spinal segments, rotation or
widening of facet joints, and focal widening of an interspinous process
distance.
compromise and to assess the posterior arch of the spine. CT has been
shown to be far more sensitive than conventional radiography for
detection of spinal fractures. Several institutions now rely on CT for
initial screening of the injured spine and use CT routinely in all
cases of trauma. Other institutions use CT for evaluation of regions
not seen adequately on the initial radiographs and to assess areas of
suspected injury.
trauma, particularly patients with neurologic injury unexplained by CT.
MRI is superior to CT in evaluating intervertebral discs, ligaments,
and the spinal cord. The early detection of ligamentous and cord
injuries is paramount in the polytrauma patient. Newer MRI techniques,
such as short tau inversion recovery or fat saturation techniques,
allow highly T2weighted images to be obtained rapidly, increasing the
sensitivity of MRI in detecting injuries about the spine.
almost always fatal at the time of impact. In the typical case, there
is anterior and superior displacement of the occipital condyles with
respect to the superior articular facets of C1. Radiographs show
displacement of the anterior rim of the foramen magnum (basion)
anterior to the dens and widening of the occipitoatlantal
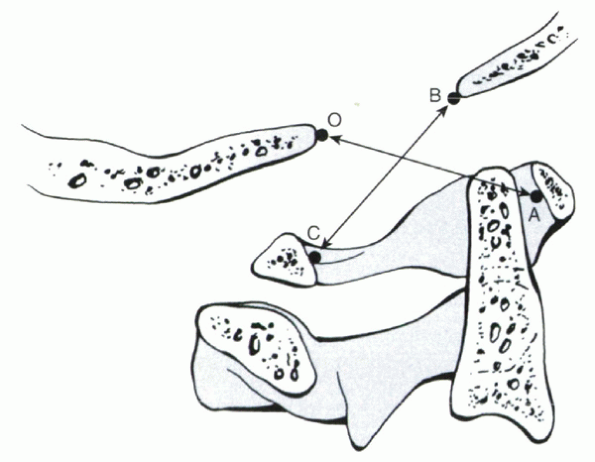
articulations, and Power’s ratio (Fig. 2-8) is abnormal. Atlantoaxial rotary fixation may be due to
trauma or follow an upper respiratory tract infection. In this
condition, the patient presents with a torticollis as C1 is fixed in
rotation relative to C2. The anteroposterior odontoid view shows
asymmetry in the sizes of the C1 lateral masses and in the distance
between the dens and the lateral masses of C2. CT shows if the C1-2
axis is abnormally fixed in rotation.
 |
|
Figure 2-4
Bimodal distribution of frequency of spine fractures. The most common locations are the cervicothoracic and thoracolumbar junctions. |
 |
|
Figure 2-5
Cervical spine MRI shows gross disruption of the anterior longitudinal ligament after a displaced teardrop fracture. The posterior longitudinal ligament appears to be “peeled away” from the vertebral body, but it appears to be in continuity. Compression of the spinal cord is clearly visible. |
resulting in simultaneous anterior and posterior arch fractures. It may
be unilateral or bilateral. The anteroposterior odontoid view shows
lateral displacement of the lateral masses of C1 with respect to the
articular pillars of C2. The fracture lines may not be seen directly on
routine radiographs, although
CT
shows the fracture lines well. Odontoid fractures are overlooked
easily, particularly if the fracture is undisplaced. The fracture line
occurs obliquely in the upper dens in type 1 fractures, occurs at the
base of the dens in type 2 fractures, and extends into the body of C2
in type 3 injuries. Anterior or posterior displacement results in
malalignment of the spinolaminar line at C1 and C2. Because the injury
typically is transverse, routine axial CT may not show the fracture.
The fracture is identified easily, however, on coronal and sagittal
reconstructed images. Hangman’s fracture, also known as traumatic
spondylolisthesis of C2, is caused by hyperextension. The bilateral
pars fractures of C2 occur just anterior to the inferior articular
facets; 20% extend into the C2 vertebral body. Typically the fracture
results in anterior displacement of C2 relative to C3, resulting in
disruption of the C1-2 spinolaminar line and the C2-3 posterior
vertebral body line.
 |
|
Figure 2-6 Diagram depicting cervical spine radiographic parameters of instability.
|
 |
|
Figure 2-7
The spinolaminar junction and posterior vertebral body alignment lines. Note they are disrupted at the level of the injury (C5 dislocation). ADI, atlantodens interval; AP, anteroposterior; DBI, dens-basion interval; LADI, lateral atlantodens interval. |
 |
|
Figure 2-8
Power’s ratio. A line is drawn from the basion (B) to the posterior arch of the atlas (C). Another line is drawn from the opisthion (O) to the anterior aspect of the atlas. Normally the ratio of BC is greater than AO. With atlantooccipital dissociation, BC increases while AO decreases. A ratio greater than 1 is diagnostic of atlantooccipital dissociation. |
posterior ligaments. No fracture is seen, so the injury may be missed
unless delayed flexion views are obtained. In severe injuries, the
initial lateral film may suggest posterior ligament disruption by
interspinous widening. CT is typically normal. The diagnosis of
isolated ligament injury is made most effectively with MRI. The torn
ligaments appear irregular and show high signal within their substance
on T2-weighted images. The “clay shoveler’s” fracture is an avulsion
fracture limited to the spinous process of the vertebra. This injury is
most common at T1 and C7, and the fractured spinous process typically
is displaced inferiorly. Associated ligamentous tears may accompany
this fracture, resulting in malalignment of the facet joint.
arising from the anteroinferior vertebral body is avulsed, with
malalignment of the spine. This unstable fracture is associated with
posterior ligamentous tears and a high incidence of spinal cord injury.
Serious injury to the spinal cord may occur if there is encroachment of
the canal by displaced bone, disc fragments, or significant epidural
hemorrhage.
Disruption
of the facet capsule can result in the presence of a facet lock, which
can occur unilaterally or bilaterally. Unilateral and bilateral facet
lock are assessed best on the lateral view, which shows anterior
displacement of the affected upper vertebra. Bilateral facet lock is
due to flexion and is easy to recognize because the degree of
displacement is large, averaging more than 50% of the vertebral body
width. Unilateral facet lock is more difficult to appreciate, and
careful analysis of the appearance of the facet joints is necessary to
avoid missing this injury. CT shows a “naked” facet or shows the
abnormal reversed position of the dislocated facet joint.
neurologic deficit, particularly in the spondylitic or stenotic spine.
Conventional radiographs may be normal after a hyperextension injury,
even in the presence of profound neurologic deficit. MRI is the optimal
method of assessing the spinal cord after a hyperextension injury and
allows differentiation between a frank cord hematoma, which has a
universally poor prognosis, and a cord contusion, which may resolve
clinically.
support provided by the rib cage and is injured infrequently. Injuries
in this area, when they do occur, have a significant incidence of
neurologic injury due to the small size of the spinal canal in this
area. In young patients, upper thoracic injuries tend to be severe
fracture-dislocations resulting in severe neurologic deficit. Although
traumatic fractures are uncommon, osteoporotic compression fractures in
this area occur with high frequency in the elderly.
according to the Denis classification system, which divides the spine
into three columns:
most important for stability, includes the posterior half of the
vertebral body, posterior half of the disc, and posterior longitudinal
ligament.
fractures consisting of a single break limited to the posterior bony
arch. Major injuries include compression fractures, burst fractures,
seat belt-type injuries, and fracture-dislocations. On radiographs,
burst fractures can be distinguished from simple compression fractures
by loss of height of the posterior vertebral body, retropulsed bone
fragments in the spinal canal, interpedicular widening, and posterior
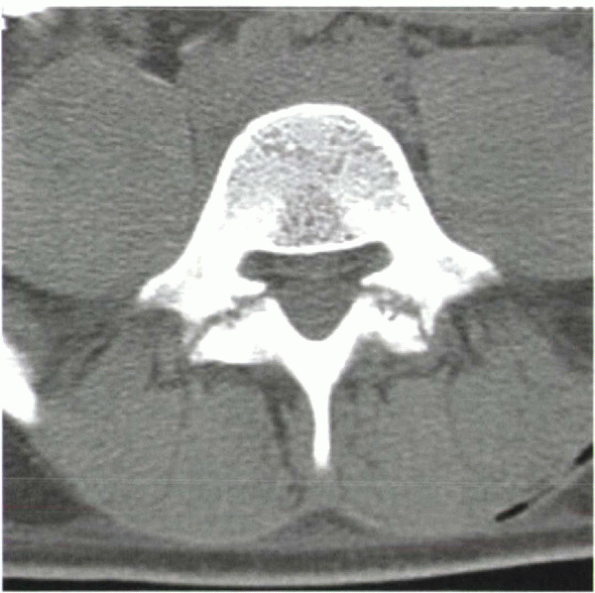
element fractures. CT is the best method for visualizing involvement of
the posterior vertebral body column and assessing the extent of osseous
retropulsion. Seat-belt injuries are due to flexion combined with
distraction. They produce posterior element widening and horizontal
vertebral fractures. Fracture-dislocations disrupt the entire spine,
allowing large amounts of translation and displacement.
overlying muscles and is injured rarely. The same types of injuries
that occur at the thoracolumbar region also occur in the lumbar spine,
although with decreased frequency. Transverse process fractures are
stable injuries that are rarely significant clinically. In rare cases,
they may be associated with injury to the genitourinary tract.
Spondylolysis defects are a developmental abnormality that result in
disruption of the pars interarticularis during early childhood. Most
pars defects involve L5, with the upper levels involved in less than 5%
of cases. The defects are seen best on oblique or lateral lumbar
radiographs; on oblique views, they are shown as disruption of the
collar of the “Scotty dog.” On CT and MRI, the defects are seen as
disruption of the posterior arch at the level of the basivertebral vein
(Figs. 2-9 and 2-10).
Spondylolysis may result in anterolisthesis of the vertebral body
relative to the body below; this displacement also is termed spondylolisthesis.
Spondylolisthesis accelerates degeneration of the intervening disc and
can result in foraminal stenosis; this is depicted best on MRI.
In infectious spondylitis, the initial site of infection is the
anterior vertebral body, with subsequent erosion of the adjacent end
plate and involvement of the adjacent disc. When the disc is infected,
the organism can extend into the adjacent vertebral body.
The
radiographic findings of infectious spondylitis consist of disc space
narrowing, adjacent end plate erosion, bone destruction, and soft
tissue swelling. These radiographic findings are delayed, and
definitive evidence of infection may not appear for several weeks after
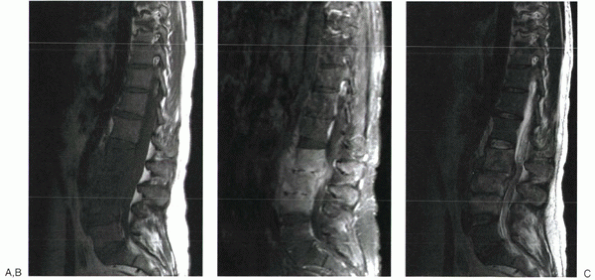
the onset of symptoms. MRI has replaced scintigraphy and CT as the
definitive modality for the detection and evaluation of suspected
spinal infection (Fig. 2-11).
MRI is more sensitive than conventional radiography and CT for early
infection and has been shown to provide equivalent sensitivity (96%),
specificity (93%), and accuracy (94%) compared with gallium and with
bone scans. MRI provides detailed anatomic information about the
paraspinal and spinal tissues and the adjacent thecal sac. On
T1-weighted MRI, there is decreased marrow signal in the affected
vertebral bodies, with high signal intensity of the disc on T2 images.
Enhancement is present after intravenous gadolinium administration, and
the enhanced regions are more consistent with an abscess versus a
phlegmon.
 |
|
Figure 2-9 Sagittal CT reconstructions can be useful in detecting and visualizing spondylolytic defects.
|
 |
|
Figure 2-10
On axial CT scans, bilateral spondylolytic defects might be mistaken for arthritic facet joints. This CT slice is at the level of the pedicles, however, which is above (or below) the level of the facet joints. |
 |
|
Figure 2-11 T1-weighted (A), T2-weighted (B), and gadolinium-enhanced (C) images of a patient with lumbar osteomyelitis.
|
relatively uncommon destructive process affecting the intervertebral
disc space, adjacent vertebral bodies, and facet joints. The radiologic
appearance may be similar to that of infection or other inflammatory
processes. MRI shows great variability in the signal characteristics of
these lesions. Findings suggesting spinal neuroarthropathy on CT and
MRI include the presence of vacuum disc phenomenon, debris and
disorganization of the involved areas, facet malalignment,
spondylolisthesis, and rim enhancement of discs on gadolinium-enhanced
MRI. Biopsy is frequently necessary for accurate differentiation from
infection.
predominate in the cervical spine, specifically the craniocervical
junction. Synovial proliferation can cause pannus formation, erosions
of the odontoid, vertebral bodies or facets, autofusion of facet
joints, cranial settling, and atlantoaxial and subaxial subluxations.
The most common radiographic pattern of spinal instability in these
patients is widening of the atlantodens interval. Flexion-extension
radiographs are essential to assess the atlantoaxial joint accurately
because the instability frequently is manifested only
on
the flexion examination. MRI can be helpful in identifying and
characterizing the soft tissue pannus and assessing the degree of cord
compression and canal compromise, which can be underestimated by plain
radiographs. Some authors advocate the use of functional MRI of the
cervical spine performed in varying degrees of flexion and extension to
evaluate atlantoaxial instability and its effect on the spinal cord.
ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome,
arthritis related to inflammatory bowel disease, and other much less
common arthritides associated with the HLA-B27 antigen. The most common
condition involving the spine is ankylosing spondylitis, which
typically presents in young men. Symptoms usually are related to
involvement of the spine and sacroiliac joints.
include bilateral symmetric narrowing and erosion of the sacroiliac
joints and later bone proliferation (syndesmophytes) and erosions
(“shiny corners”) at the thoracolumbar junction. CT and MRI are helpful
in the detection and characterization of erosive changes at the
sacroiliac joints. A major complication of ankylosing spondylitis is
the development of a fracture and subsequent formation of a
pseudarthrosis in the spine. On MRI, the pseudarthrosis can mimic
infection, with signal changes surrounding the abnormal fractured disc.
The detection of a horizontal fracture line through the posterior
elements allows differentiation of a pseudarthrosis after traumatic
fracture from discal infection (Fig. 2-12).
frequently misdiagnosed. Deposition of urate crystals in the spine with
advanced gout can cause erosions of the odontoid process and the end
plates, disc space narrowing, and vertebral subluxation. Calcium
pyrophosphate deposition disease is characterized by the presence of
crystal deposition in the articular cartilage, menisci, synovium, and
periarticular tissues. In the spine, calcium pyrophosphate deposition
disease can cause destructive lesions of the vertebral bodies and disc
spaces and calcification of the discs. Masslike deposits of calcium
pyrophosphate deposition disease crystals have been described in the
atlantoaxial region, and the cystic changes seen in the adjacent bone
increase the risk of fracture of the dens significantly. Calcium
hydroxyapatite crystal deposition disease more characteristically is
associated with extraarticular tendinous calcific deposits. In the
spine, hydroxyapatite crystal deposition disease is seen most
frequently in the tendon of the longus colli muscle. A painful,
inflammatory tendinitis is present with soft tissue swelling anterior
to C2. The calcific deposit is seen best on CT. On MRI, prevertebral
edema is seen in the upper cervical spine as thickening and signal
alterations in the tendon.
radiographically. The etiology is thought to be amyloid deposition
within the disc space. Slowly progressive end plate erosions, disc
space narrowing, and vertebral destruction are seen typically in the
cervical and lumbar regions. Multiple levels may be involved. In
contrast to infection, the soft tissues remain normal in dialysis
spondyloarthropathy. On MRI, the vertebral bodies also show normal
marrow signal except for minimal alterations adjacent to the erosions.
The T2-weighted image is particularly helpful because it shows no
abnormal high signal in the affected region.
because of local pain, pathologic fracture, or neurologic deficit.
Occasionally a spinal tumor is detected as an incidental finding in an
asymptomatic patient; in this situation, the lesions are typically
benign. MRI plays a complementary role with plain film radiography, CT,
myelography, and scintigraphy for the assessment of spinal neoplasms.
and the most common site of metastasis to the skeleton. The vertebral
body is involved with greater frequency than the posterior elements.
Scintigraphy traditionally is used as the initial imaging test for the
detection of metastatic disease in a patient with a known primary
malignancy. Scintigraphy allows whole-body screening, which currently
is not feasible by MRI. Scintigraphy is considerably less sensitive
than MRI, however. The advantage of MRI is particularly evident for
infiltrative neoplasms, such as multiple myeloma and lymphoma, which
may have normal scintigrams in the presence of widespread disease.
Another disadvantage of scintigraphy is that a positive exam provides
no morphologic information about the spinal lesion. MRI can detect the
presence of a fracture or soft tissue encroachment on the neural
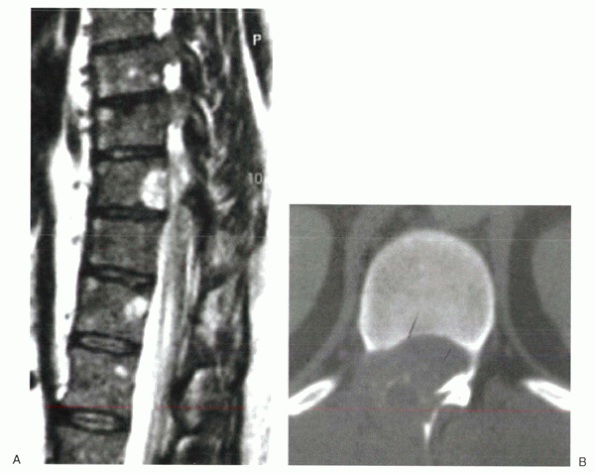
structures, which have an impact on therapy (Fig. 2-13).
with multiple noncontiguous sites of involvement. Metastases appear as
areas of diminished signal loss within the bone marrow on T1-weighted
images. The signal of metastatic disease on T2-weighted images is more
variable, depending on the nature of the adjacent bony response. Lytic
tumors are typically bright on T2-weighted images. Sclerotic lesions
are highly variable and may appear hypointense, hyperintense, or
isointense to normal bone marrow. Most metastases, with the exception
of a few densely osteoblastic lesions, show enhancement after
intravenous gadolinium. The use of fat suppression after gadolinium
injection increases the ability to identify areas of enhancement.
vertebra requires consideration of the patient’s age, the location of
the lesion, and the lesion’s appearance. MRI is not particularly
helpful for predicting the histologic type of neoplasm in many cases.
Multiple myeloma is the most common primary osseous tumor, typically
presenting with bone pain and osteopenia in an elderly individual. It
may be in its solitary (plasmacytoma), disseminated (multiple
plasmacytoma), or diffuse (multiple myeloma) form at the time of
diagnosis. The MRI appearance of myeloma is variable and depends on the
pattern and degree of infiltration. Mild disease, producing only subtle
marrow inhomogeneity, is common and may be interpreted as within the
normal range. Approximately 20% to 25% of cases of myeloma cannot be
detected by MRI. Other common primary neoplasms of the skeleton include
hemangioma, lymphoma, chordoma, and chondrosarcoma. Primary neoplasms
typically do not involve the disc space and remain confined to the
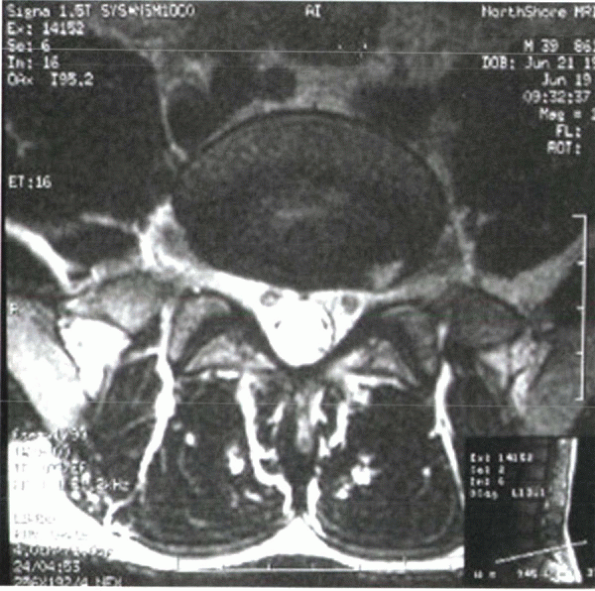
vertebral body or posterior arch (Fig. 2-14).
Exceptions to this rule include chordoma, which frequently extends via
the epidural space to involve the disc and adjacent vertebral body, and
plasmacytoma, which frequently involves multiple contiguous vertebrae
and the intervening disc spaces.
 |
|
Figure 2-12
Cervical fractures in patients with ankylosing spondylitis can be missed easily. This patient was complaining of neck pain for 1 week after a minor fall before initial x-rays were taken. (A) The hallmark “bamboo” spine, produced by marginal ossification of the spinal ligaments with preservation of disc spaces, can be noted. (B) Sagittal CT reconstruction shows a fracture line extending from the posterior elements to the anterior elements. Fractures occur most commonly through the brittle disc spaces. (C) MRI shows acute bone edema within the region of the fracture. This can be difficult to differentiate from infection. |
 |
|
Figure 2-13 T2-weighted (A) and T1-weighted (B)
images of the upper thoracic spine of a patient who presented with bandlike chest pain at rest from activity. He had a history of lung cancer. Open biopsy confirmed the lesion to be metastatic adenocarcinoma. This is an example of direct tumoral expansion into the spinal canal without pathologic fracture. |
problem in society. Approximately 60% to 80% of all adults develop
severe incapacitating low back pain sometime in their life.
Approximately 2% of all adults visit a physician because of back pain
each year. It is particularly common among middle-aged adults and
accounts for 25% of missed workdays. Low back pain is also one of the
leading causes of chronic work-related disability. The cause of back
pain, the need for surgery, and the role of imaging in low back pain
syndrome all are subjects of controversy (Fig. 2-15).
and adjacent end plates, mimicking infection, is seen in approximately
5% of patients. Modic et al classified the bone marrow changes
according to the signal intensity on MRI. The described patterns
include the following:
changes are seen. Modic et al suggested this appearance is due to an
inflammatory response to disc degeneration. Type 1 changes are
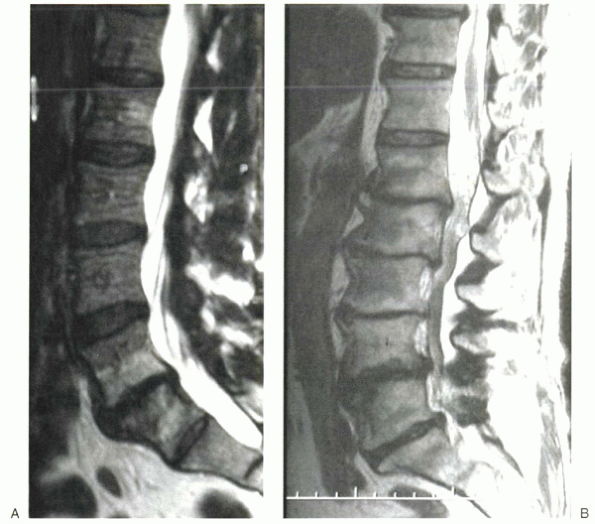
hypointense on T1-weighted images and hyperintense on T2-weighted
images (Fig. 2-16). Type 1 change routinely enhances with gadolinium and can simulate an osteomyelitis.
converted to predominantly fat. This pattern has been shown to be
stable over a 2- to 3-year period. Type 2 changes show a hyperintense
signal on T1-weighted images and isointense-to-hypointense signal on
T2-weighted images. Chronic disc disease leads to vertebral body end
plate sclerosis, which is known as a type 3 change.
the marrow abnormalities are less extensive, the intranuclear cleft of
the disc is preserved, and the end plates are not eroded and are
preserved. Type 1 changes tend to resolve spontaneously over a few
months. They can be difficult to differentiate from infection, and
laboratory studies, such as C-reactive protein and sedimentation rate,
are required.
is a condition seen predominantly in adolescents and young adults. It
is poorly understood, although many investigators think it is a
postrepetitive stress osteochondrosis of the vertebral end plate,
leading to secondary degenerative disc disease. The radiographic
findings include end plate irregularity, multiple Schmorl’s nodes,
wedging of the bodies, and kyphosis. In most reported cases, MRI shows
loss of disc
height,
disc dehydration, and variable herniation of nuclear material into the
annulus fibrosus or vertebral end plates known as Schmorl’s nodes.
These herniations may incite an inflammatory response in the vertebra,
which can be difficult to distinguish from focal osteomyelitis. On MRI,
10% of Schmorl’s nodes may show vascularization and adjacent bone
marrow edema. There is speculation that the degree of vascularity may
reflect the age of the abnormality and the likelihood that it will be
symptomatic. An inflammatory response to intrabody discal herniation
also can be seen in adults, although it is much less common than in
children. Hemispherical sclerosis results in a rounded area of
sclerosis and mild bone marrow edema surrounding a Schmorl’s node. This
condition typically is seen in middle-aged women at L4.
 |
|
Figure 2-14 Benign primary bone tumors most often occur within the posterior vertebral body and posterior arch. (A) Sagittal MRI shows a benign hemangioma of the posterior vertebral body that extended into the pedicle (image not shown). (B) Axial CT scan of an aneurysmal bone cyst. The patient presented with pain and myelopathy.
|
 |
|
Figure 2-15 Small annular tears can be detected with MRI. They are thought to contribute to back pain.
|
patients with acute back pain is related to the high incidence of
morphologic abnormalities in asymptomatic patients. Studies have shown
that there is little difference between symptomatic and asymptomatic
individuals in the frequency of spinal anatomic lesions, such as disc
space narrowing, osteophyte formation, spondylolysis, and disc
herniations. In 1994, Jensen et al published a landmark article
regarding MRI findings in asymptomatic individuals. They performed
a
prospective study of 98 people with no history of back pain or
radiculopathy. In their study group, which was evaluated using the
North American Spine Society (NASS) criteria, only 36% of persons had a
totally normal examination. Of patients, 52% had at least one bulging
disc, and 27% had at least one disc protrusion. Schmorl’s nodes (19%),
annular defects (14%), facet joint arthrosis (8%), and spondylolysis
(7%) also were common. The only finding that was infrequent in
asymptomatic individuals was the presence of disc extrusion. In their
series, only one asymptomatic person showed a disc extrusion.
 |
|
Figure 2-16 Degenerative disc disease can manifest in many ways. (A)
Sagittal MRI shows type 1 Modic changes within the adjacent end plates of the L5-S1 disc. Note the marked collapse of the disc space, with only minor bulging of the annulus. This has been referred to as the “flattire” syndrome. (B) Sagittal MRI of an elderly man who presented with neurogenic claudication. Type 2 and 3 Modic changes can be noted in multiple vertebral bodies. Of most interest, profound spinal stenosis is noted from L2-4. Nerve root clumping is evident above the level of stenosis (behind L1 vertebral body). |
suggested. Although they differ in their details, all guidelines
recommend conservative management of back pain for 4 to 7 weeks before
any diagnostic imaging, unless the patient meets criteria for earlier
radiographic evaluation. Suggested criteria for early imaging include
the following:
-
Neurologic deficit (myelopathy or radiculopathy or both) unexplained by plain films
-
Suspected fracture (significant trauma, steroid use, severe osteoporosis)
-
Suspected vertebral infection (immunocompromised, fever, or elevated laboratory values)
-
Suspected metastatic disease (history of malignancy)
-
Before radiation therapy
-
Before spinal surgery
-
New-onset or increasing postoperative back pain
degenerative disease of the spine. Perhaps the difficulties with the
terminology are partly responsible for the poor correlation between
imaging findings and symptoms. Terminology used by radiologists to
describe degenerative diseases of the spine is highly variable. Terms
such as spondylosis deformans (annular
degeneration), intervertebral osteochondrosis (nuclear degeneration),
osteoarthrosis, osteoarthritis, diffuse skeletal hyperostosis,
degenerative spondylosis, disc
desiccation, disc degeneration, annular fissure, annular tear, and disc herniation
commonly are used interchangeably when describing degenerative disease,
often without precision or consistency. There is also considerable
variability in the terminology used by spine surgeons in describing
degenerative diseases of the spine. A study by the NASS found wide
variation in description of common spinal degenerative conditions by
eight highly experienced surgeons. The eight surgeons used almost 50
terms collectively to describe eight different imaging findings.
-
Disk dehydration
-
Generalized bulge
-
Annular fissure
-
Disc protrusion
-
Disc extrusion
-
Sequestration
which is confusing and medicolegally significant. The dehydrated disc
shows loss of signal on T2-weighted sequences. A generalized bulge is
due to weakening of annular fibers, allowing the disc to protrude
greater than 2 mm circumferentially beyond the bone margin. A disc
protrusion is broad based and is wider in the coronal plane than in the
sagittal plane. All of these findings are common in the asymptomatic
population. A disc extrusion has a narrow pedunculated segment and is
elongated in the sagittal plane. A sequestered disc has lost its
attachment to the parent disc. Both of these findings are uncommon in
the asymptomatic population. Although they can be missed with CT
myelography, foraminal discs are detected readily on MRI (Fig. 2-17).
 |
|
Figure 2-17
Foraminal disc herniations are detected readily on MRI, whereas they may be missed by myelographic techniques. This is because the nerve root compression occurs beyond the point that the dura becomes confluent with the spinal nerve epineurium. |
69 patients with disc herniation were followed longitudinally while
undergoing nonsurgical, conservative therapy. Of patients, 63% showed
spontaneous decrease in volume of the disc greater than 30%, and 48%
showed decrease in volume of the disc greater than 70%. The most
dramatic decrease in size was seen in the largest disc herniations.
Perhaps some, or even most, of the decrease in size of the disc
herniation apparent by MRI is due to resolution of the inflammation
that surrounds the symptomatic herniated disc.
findings on postoperative imaging studies. In many patients, follow-up
imaging studies show no improvement in the anatomic lesion thought to
be responsible for symptoms, despite excellent response to the
intervention.
and Boden et al reviewed MRI studies postoperatively in patients who
were greatly improved or rendered completely asymptomatic after
surgery. Both of these series showed no correlation between
postoperative mass effect and patient outcome. In both studies,
significant residual mass effect persisted in most patients after
successful surgery. Persistent disc protrusion/extrusion was present in
69% of surgical responders. Imaging showed a slow, incomplete
resolution of mass effect over 36 months, despite immediate clinical
response.
D, Fishman EK. Imaging of musculoskeletal trauma in three dimensions:
an integrated two-dimensional/three-dimensional approach with computed
tomography. Radiol Clin North Am 1989;27:945-956.
CG, DP. Rockwood and Green’s fractures in adults. In: Bucholz RH, JD,
eds. Vol. 1-2, 5th ed. Philadelphia: Lippincott Williams & Wilkins,
2001.
C, Modic MT, Kearney F, et al. Rheumatoid arthritis of the cervical
spine: surface-coil MR imaging. AJR Am J Roentgenol 1988;151:181-187.
Roos A, et al. MR imaging of marrow changes adjacent to end plates in
degenerative lumbar disk disease. AJR Am J Roentgenol 1987;149:531-534.
SC, et al. Can imaging findings help differentiate spinal neuropathic
arthropathy from disk space infection? Initial experience. Radiology
2000;214:693-699.
A, Gallucci M, Masciocchi C, et al. Lumbar disk herniation: MR imaging
assessment of natural history in patients treated without surgery.
Radiology 1992;185:135-141.
A, Bellan M, Weiss M, et al. MR imaging of enhancing intraosseous disk
herniation (Schmorl’s nodes). AJR Am J Roentgenol 1997;168:933-938.
WR, Dotter WE. Comparative roentgenographic study of the asymptomatic
and symptomatic lumbar spine. J Bone Joint Surg Am 1976;58:850-853.
