Thoracic Spondylosis, Stenosis, and DISC Herniations
and, as with a disc herniation, may result in myelopathy,
radiculopathy, or both. Symptomatic thoracic disc disease is relatively
rare. Thoracic disc herniations represent less than 2% of all disc
operations, and less than 4% of symptomatic discs. Compared with
cervical and lumbar stenosis, thoracic stenosis represents a small
percentage of surgically treated cases.
spinous processes are long with considerable “overlap” between levels.
In the upper thoracic spine, the facets resemble cervical
articulations. Progressing toward the middle thoracic region, the joint
surfaces are nearly coronal, and in the lower thoracic region, they are
sagittal. The ribs articulate with the vertebrae in two areas:
-
At the anterior aspect of the transverse process
-
At the posterolateral aspect of the vertebral body
The spinal canal in the thoracic spine is smaller in relation to the
lumbar or cervical spine, resulting in a high rate of paraplegia with
traumatic injuries. Because of the stabilizing contribution of the rib
cage, more energy is needed to cause the initial injury. The borders of
the neural foramina are the pedicles superiorly and inferiorly, the
vertebral body and disc anteriorly, and the facet joint posteriorly.
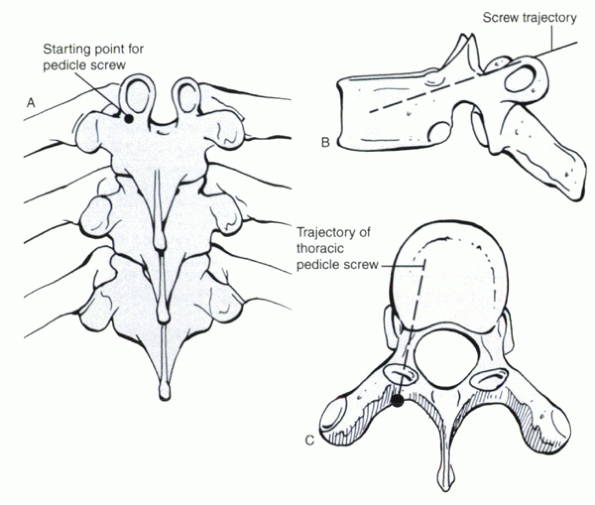
The inferolateral edge of the inferior articular process at its
junction with the transverse process is the approximate entry point for
a thoracic pedicle screw (Fig. 15-2).
degenerative. The degenerative process has been described more
extensively in the lumbar spine, which is discussed in subsequent
chapters. Briefly summarized, initial disruption of the integrity of
the intervertebral disc, including delamination, fibrillation, and
annular tears, leads to a change in the disc’s ability to withstand
force. At each motion segment (two vertebrae = one motion segment or
functional spinal unit), multiple joints interact. In the thoracic
spine, these are the intervertebral disc, the facet joints, and the
costovertebral junctions. In contrast to the cervical and lumbar
regions, the interaction of the ribs gives a substantial amount of
additional support. With a compromised disc, greater than normal
demands are placed on the other joints. These joints can undergo
subsequent articular surface breakdown with corresponding changes, such
as hypertrophy and osteophyte formation.
most common complaint is pain. Pain can be axial (central,
nonradiating) or radicular (follows dermatomal distribution). Axial
pain is thought to be generated from the degenerated disc or facets or
both. Both structures are innervated by nociceptive nerve endings. In
the lumbar and thoracic spine, the facet is innervated by medial
branches of the dorsal root ganglion. These branches arise from the two
nerve roots below the joint. The T3-4
facet joint is innervated by branches from the T4 and T5 nerve roots.
The posterior anulus of the disc is innervated by branches of the
sinuvertebral nerve, which itself is a branch from the rami
communicantes between the dorsal root ganglion and the autonomic
ganglion. Dysfunction, instability, or degeneration may transmit pain
through these nerves.
 |
|
Figure 15-1
The rib head articulates with the anterior aspect of the transverse process and the posterolateral aspect of suprajacent and infrajacent vertebral bodies. This “bridging” between vertebral bodies provides additional stability to the thoracic spine. |
changes, including osteophytes protruding from the anterior, posterior,
or lateral aspects of the vertebral bodies adjacent to the disc spaces.
These changes are age dependent and are most often clinically
asymptomatic. Facet joint hypertrophy also is characteristic.
disc disease is unclear. Most authors believe that mechanical
compression is a key factor. Stenosis, whether central or foraminal, is
a radiologic/pathoanatomic finding. Thoracic stenosis can be detected
by imaging studies, such as computed tomography (CT) or magnetic
resonance imaging (MRI), and represents narrowing of the spinal canal
or space for the exiting nerve roots. Not all patients with these
findings have neurologic signs or symptoms. Additional mechanisms are
likely, such as neural vascular insufficiency, but they cannot be
detected by presently available imaging techniques. Myelopathy and
radiculopathy are clinical diagnoses and should not be based solely on
imaging studies that may show evidence of neural compression. The
actual etiology is probably multifactorial and remains to be elucidated
clearly.
compression remains the focus of surgical treatment of thoracic disc
disease. Osteophytes, overgrown facets, or infolded ligamenta flava can
compress the spinal cord or nerve roots. Disc herniations may protrude
into the spinal canal or foramina as well, causing a similar clinical
picture. Recognizing the cause and nature of the offending elements is
crucial to effective treatment.
does not result in clinically apparent sensory or motor deficits. It
would be difficult to show isolated weakness of the right T9-10
intercostal muscles. Radicular pain is a more common complaint,
presenting as a bandlike sensation wrapping around the chest. Patients
can mistake this for the pain associated with a heart attack. In animal
studies, pure compression of a nerve root, although it produces
anesthesia, is not enough to cause pain (dysesthesia). Exposure to
chemical factors from an injured disc might potentiate nerve root
irritation. This “irascible” nerve root is more susceptible to
symptomatic compression. Often, removal of small discs with little
evidence of root compression relieves pain. Myelopathy itself is not
painful but frequently presents with concomitant radicular or axial
pain symptoms.
Hypertrophy of the facets or infolding of the ligamenta flava can
encroach on the posterior aspect of the spinal canal. Ossification of
the posterior longitudinal ligament, albeit rare, has been documented
as a cause of thoracic myelopathy. Synovial cysts, which may be related
to the degenerative process, also have been reported. Kyphotic
deformity can be a predisposing factor. Case reports of cord
compression in patients with Scheuermann’s disease have been
documented. Scheuermann’s kyphosis can be associated with disc
herniations that protrude into the vertebral bodies or the neural
elements.
thoracic disc herniation with or without neural dysfunction. About 30%
of affected patients relate a traumatic episode with the onset of pain
or neurologic dysfunction or both. In most cases, the disc likely had
been degenerated to some extent before the incident. Torsion and
bending may risk injury to the thoracic disc more than other movements.
abnormalities can be detected in 73% of asymptomatic patients. The
estimated incidence of symptomatic discs is about 1 in 1 million.
Symptomatic individuals usually are between 30 and 50 years old; men
and women are affected equally. In a two-part natural history study of
asymptomatic patients, about 58% of people had an annular tear, 37% had
a herniated
disc,
and 25% had imaging evidence of a deformed spinal cord. Patients with
Scheuermann’s kyphosis had a 38% incidence of disc or vertebral
irregularities, which may have represented disc herniations; only 29%
of patients were found to have an annular tear. All patients available
for long-term follow-up (26 months) remained asymptomatic. Discs
causing less than 10% canal compromise tended to get bigger, whereas
discs causing 20% or more compromise appeared to resorb. The
radiographic finding of thoracic spondylosis is common, but it would be
difficult to measure specifically. In most cases, thoracic spondylosis
is asymptomatic and never comes to clinical attention.
 |
|
Figure 15-2 (A)
The entry portal for a thoracic pedicle screw is at the inferolateral aspect of the facet joint, near the junction of the superomedial edge of the transverse process. This location can be appreciated further by viewing the lateral (B) and axial (C) views of the thoracic vertebra. The portal sits in the “valley” between the transverse process and the lamina (C). |
determining treatment. There is no gold standard classification system.
In general, three groups can be recognized:
-
Thoracic disc herniations
-
Thoracic stenosis
-
Thoracic spondylosis
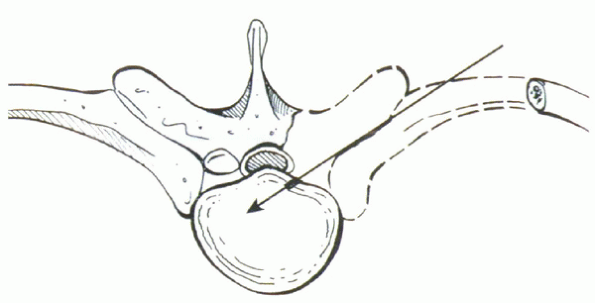
features. The location, which may be central, paracentral, or
foraminal, is important to note. Central herniations are most likely to
produce spinal cord compression and myelopathy. They are the least
likely to cause radicular pain, although this may occur. Paracentral
discs lie off the midline and can cause spinal cord and root
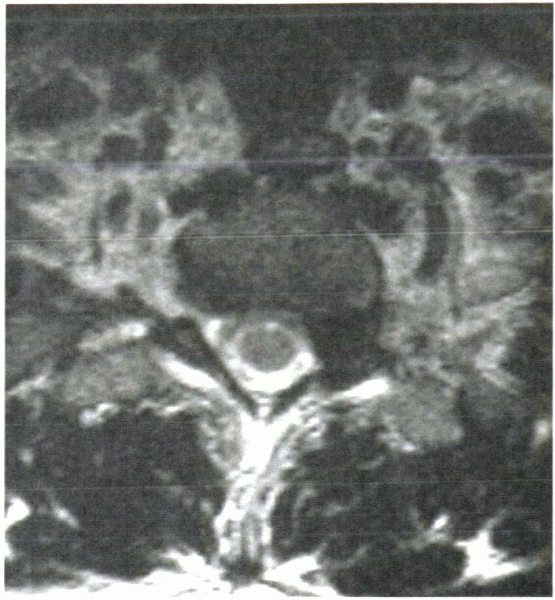
compression. Foraminal discs can cause isolated root compression (Fig. 15-3). The surgical approach for this type is distinct and is discussed subsequently.
calcifications. Calcified discs are more likely to be symptomatic than
noncalcified discs. They may be associated with adhesions between the
disc and the dura, making surgical excision more difficult.
herniations are the least common, whereas herniations at the
thoracolumbar junction (T11-12 and T12-L1) are the most common. It is
believed that the transition between the stiffer thoracic and more
mobile lumbar vertebrae is a contributing factor to accelerated
degeneration in this region. Most (about 60%) thoracic disc herniations
occur between T8 and L1.
not related to a soft disc herniation. Stenosis may be developmental or
acquired. Developmental stenosis is usually idiopathic and represents a
congenitally narrowed spinal canal.
It
is a predisposition to neurologic dysfunction but usually is not
sufficient alone to cause symptoms. Congenital stenosis is common in
patients with achondroplasia. Acquired stenosis usually is related to
the later stages of degenerative disc disease. This may be superimposed
on a congenitally narrowed canal.
 |
|
Figure 15-3 Axial MRI shows a foraminal thoracic disc herniation at T1-2.
|
ossification of the posterior longitudinal ligament. This rare disorder
is more frequent in Asians. Adhesion between the ossified ligament and
the dura make surgical excision demanding.
involvement is common and usually asymptomatic. There are no formal
classification systems to organize thoracic spondylosis. With the
stability of the ribs, degenerative instability or spondylolisthesis is
uncommon in the thoracic spine.
-
Pain (57% of patients)
-
Sensory complaints (24% of patients)
-
Motor complaints (17% of patients)
-
Bladder complaints (2% of patients)
complaints at presentation, which are more severe and include bladder
symptoms in 30% of patients and motor or sensory symptoms in 61% of
patients (Table 15-1).
|
TABLE 15-1 INITIAL VERSUS PRESENTING SYMPTOMS
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
down the arm and leg are uncommon. Radiculopathy usually presents as a
bandlike pain along the chest or abdomen. The level of complaint may
correlate to the anatomic region of disease, although most patients
exhibit T10 findings regardless of the level of disease.
indicate a traumatic etiology. Twisting or heavy lifting can be the
inciting event and suggests an acute soft disc herniation. Preinjury
back pain suggests underlying disc disease.
findings or long tract signs) must be noted. Weakness in the legs,
instability, gait disturbances, and imbalance can be clues. In some
situations, patients can present with complete or incomplete spinal
cord injury related to a minor injury. These cases have a poor
prognosis. Neurologic compression in the upper (T2-5) levels can lead
to Horner’s syndrome, characterized by a drooping eyelid, pupillary
constriction, and dry eye or infrequently pain radiating down the arm.
neurologic evaluation, is required. Specific attention is directed
toward the reflex examination. Hyperreflexia in the lower extremities
with normal findings in the upper extremities suggests thoracic level
spinal cord compression. Other findings indicating thoracic myelopathy
are gait imbalance (i.e., wide-based), clonus, and an up-going plantar
response (positive Babinski’s sign). Abdominal and cremasteric reflexes
also should be noted. The examiner specifically must examine for
pathologic cervical level reflexes, such as Hoffmann’s sign, to rule
out cervical myelopathy, which can be missed with a focal exam.
Objective weakness or sensory loss in the trunk or lower extremities
also can be present. Spinal cord injury may be complete or incomplete.
thoracic disc disease. Back or flank pain can be associated with renal
or gastrointestinal conditions. Zoster pain can present in a dermatomal
distribution, feigning the bandlike syndrome of thoracic radiculopathy.
Systemic neurologic disorders, such as multiple sclerosis, amyotrophic
lateral sclerosis, and Stickler’s syndrome, also can confuse the
diagnosis. Surgeries performed for radiologic evidence of thoracic disc
herniations with these underlying disorders often lead to a poor
neurologic outcome. Tumors, with and without neural involvement, also
can present similar to thoracic disc disease. Cardiac pain may radiate
to or from the thoracic spine and may be the first sign of ischemia.
disc disease is sparse. Clinically, approximately 77% of patients with
radiculopathy have some symptomatic resolution of symptoms with
conservative treatment. Symptoms are correlated poorly with imaging
evidence. The radiologic resolution of thoracic disc herniations seems
to correlate with initial size: Discs that cause less than 10% of canal
compromise tend to stay the same, whereas discs compromising more than
20% of the canal tend to get smaller with time. CT-myelography seems to
be no better than MRI in predicting symptoms. A possible advantage of
CT is superior detection of calcifications within the disc, which have
a higher rate of being symptomatic than noncalcified discs.
including high-quality anteroposterior and lateral views. Kyphotic
deformities, especially with Scheuermann’s disease, are associated with
a higher rate of thoracic disc herniations. The kyphosis may potentiate
spinal cord compression with small disc bulges or osteophytes (Fig. 15-4).
Radiographic hallmarks of spondylosis are vertebral body osteophytes,
disc space narrowing, and facet hypertrophy. Infrequently, listhesis of
the thoracic vertebrae can be noted. This finding is rare because of
the extra stability provided by the ribs. “Stippling” within the disc
space can suggest calcifications. As stated previously, 45% to 71% of
calcified discs are symptomatic, a much higher frequency than
noncalcified discs.
latter is not possible. With better bone detail, a clearer picture of
“hard” discs (i.e., bony osteophytes) is afforded. Facet involvement
also is well visualized. CT is the modality of choice to detect
ossification of the posterior longitudinal ligament or ossification of
the ligamentum flavum, a rare cause of myelopathy in the thoracic spine
(Fig. 15-5). CT is useful for detecting intradiscal calcifications.
 |
|
Figure 15-4
Kyphosis can exaggerate the compressive effects of small herniated discs. In this patient, posterior vertebral body osteophytes also contributed to canal compromise. |
“overdiagnose” thoracic disc herniations because the rate of abnormal
findings in asymptomatic individuals is high. Because of the smaller
spinal canal in the thoracic region, however, smaller herniations
(compared with lumbar disc herniations) can cause significant symptoms.
The integrity of the disc, including the presence of annular tears,
bulges, or frank herniations, and the ligaments, including the anterior
longitudinal ligament, posterior longitudinal ligament, flavum, and
facet capsule, can be noted on MRI. Edema within the spinal cord may be
appreciated, suggesting profound neurologic damage.
clearly shows the location of the disc. Most (70% to 90%) are central
or paracentral discs; foraminal discs are infrequent. A disc fragment
rarely is found within the dural sac. In contrast to cervical and
lumbar levels, sequestered fragments are extremely infrequent. The
level of disc herniation also is determined. The most common
symptomatic levels of herniation are T11-L1, representing the
biomechanical
transition
zone of the thoracolumbar junction. The most common overall
(symptomatic and asymptomatic) region is the T8-L1 area. Calcifications
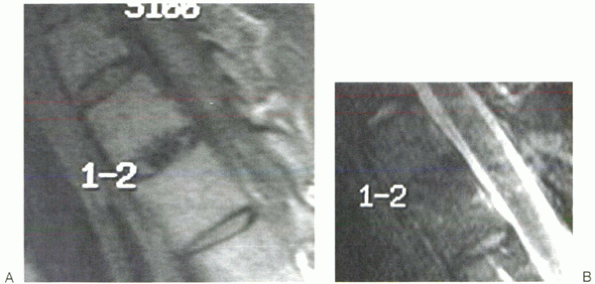
within the disc can appear as hypointensities on T1-weighted and
T2-weighted images within the nucleus (Fig. 15-6).
 |
|
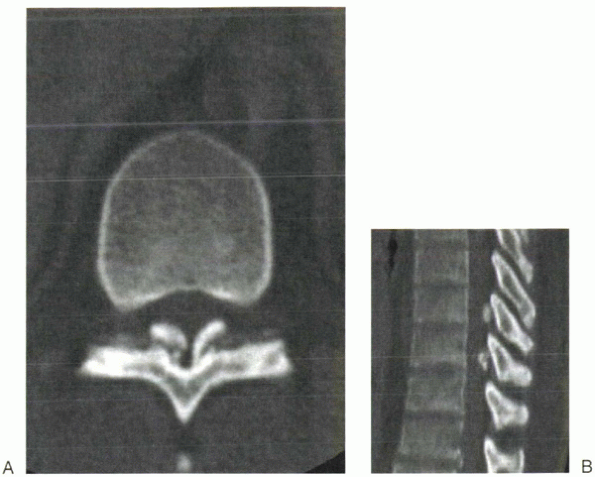
Figure 15-5 (A, B)
Ossification of the yellow ligament is an extremely rare cause of thoracic stenosis. On axial CT, the ossified ligament’s insertion onto the anterior aspect of the lamina can be seen. |
signs or symptoms of spinal cord compression. This includes patients
with signs of root compression or pure axial back pain. Patients with
evidence of spinal cord compression by physical examination and imaging
are treated better with surgical decompression. The best results for
surgical decompression for myelopathy are early in its presentation
while the patient is still highly functional and ambulatory.
 |
|
Figure 15-6 (A and B) Calcifications within the disc appear as hypointensities within the nucleus on T1-weighted and T2-weighted images.
|
medications, unless these are contraindicated because of
gastrointestinal or renal issues. Mild narcotics should be reserved for
severe pain and should not be continued for extended periods. A brief
course of rest may help acute pain episodes. Some physicians advocate a
short course of oral steroids. Bracing may be of most symptomatic
benefit in patients with spinal deformity. The efficacy of this
maneuver depends on the flexibility of the curve. Hyperextension
bracing may relieve compressive forces across the disc. Extended
periods of bracing should be avoided to minimize muscle deconditioning.
Rehabilitative efforts through formal physical therapy can be helpful.
Emphasis on strengthening, flexibility, and range of motion are
beneficial.
and lumbar spine for the temporary symptomatic treatment of
radiculopathy. Some practitioners have found injections to be useful in
the thoracic spine for similar indications. Epidural steroids in
patients with thoracic level myelopathy and stenosis can be dangerous
and are not indicated routinely. Intercostal nerve blocks, analagous to
selective nerve root blocks in the neck and low back, may offer some
relief for thoracic radiculopathy.
disc disease, whether herniation or spondylosis, is highly
controversial. Most of these patients should be treated with
observation and nonsurgical modalities. The goal for treating nerve
root or spinal cord compromise is decompression. This can be performed
through various approaches. Bone or disc or both that are believed to
be the offending elements are removed.
approach according to the location of the pathology. The disc should be
accessed with no manipulation of the spinal cord. For this reason,
standard posterior laminectomy is not advisable. Options include
anterior and posterior approaches.
anterior exposure. In the high thoracic spine (T1-2), this can be
performed with a modified low anterior cervical approach, including a
medial claviculectomy. Safe access to the T2-3 disc space is usually
possible; however, this should be determined by carefully examining a
preoperative sagittal MRI study. The inferior limit to access is the
manubriosternal body junction. If it lies proximal to the disc level in
question, an alternative approach should be sought. The disadvantages
of this approach are the risk for damage to the recurrent laryngeal
nerve and thoracic duct (left side). Patients should be advised
preoperatively of the cosmetic effects of removing the medial half of
the clavicle and manubrium.
It is best for exposure of T1-4 when other approaches are not
advisable; this should be determined preoperatively. A radiographic
marker can be placed within the axilla to determine the most proximal
extent of exposure through a thoracotomy. Only if the proposed level
cannot be reached in this manner should transsternal exposure be
planned. The approach should be performed by an experienced thoracic
surgeon.
intercostal dissection to gain lateral access to the thoracic disc
spaces from T4-12. A right-sided or left-sided technique can be used,
depending on the location of the disc hernation. A double-lumen
endotracheal tube should be used. Associated morbidity may be related
to lung deflation, lung injury, and intercostal neuralagia from
retractor compression.
-
Direct access to the disc space
-
Access to central and paracentral disc herniations
-
Direct visualization of spinal cord compression and subsequent decompression
-
Ability to perform interbody fusion
-
Safer approach for removal of most calcified discs
exposure, including the risk for pulmonary, vascular, and lymphatic
injury. Thoracotomies require a postoperative chest tube. Foraminal
disc pathology is not well addressed using anterior approaches.
approach is the possibility of spinal cord ischemia from ligation of
segmental arteries. The “watershed” region of the thoracic spine is
about T4-9, although this can vary. The artery of Adamkiewicz, or great
medullary artery, is usually a branch of an intercostal or lumbar
artery in the T10-12 region. It then anastomoses with the anterior
spinal artery in the spinal canal through a neural foramen. It is
present on the left 80% of the time. The artery travels cranially
within the spinal canal to supply the so-called watershed area.
Sacrifice of this artery can cause acute ischemia of the thoracic
spinal cord at this level. In performing an anterior discectomy, the
segmental vessels should be spared, which usually is possible unless
more extensive bone resection is required. If the segmental artery must
be sacrificed, it should be ligated within the midvertebral body. This
leaves the anastomosis of the radicular artery with the intercostal
artery patent, allowing the possibility of retrograde flow.
Intraoperatively the proposed segmental artery can be compressed
temporarily, while monitoring evoked potentials for signs of neurologic
compromise. A preoperative arteriogram of the spinal vasculature has
been used by some authors to determine the level of the great medullary
artery preoperatively.
technique has a learning curve and should be attempted only by properly
trained and experienced clinicians. Through multiple thoracic portals,
the disc space is accessed and dissected. In most cases reported, the
indications have been more for axial pain than for neurologic
decompression. The advantages seem to be related to avoidance of an
open thoracotomy. Intercostal neuralgia has been associated with large
rigid cannulae; neuralgia can be minimized with flexible devices.
disc excision, it usually is not for thoracic disc excision. The spinal
cord cannot be mobilized or retracted as the cauda equina. This
limitation has prompted numerous posterior alternatives for access to
thoracic disc herniations without the need for neural retraction.
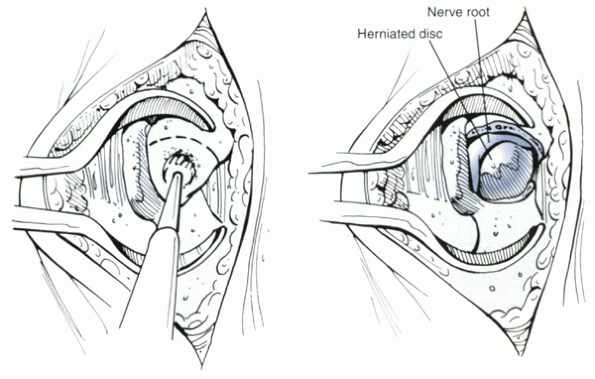
used to remove centrolateral (paracentral) and lateral disc
herniations. The side of the disc herniation is approached. The medial
rib, associated transverse process, and pedicle are removed (Fig. 15-7).
By maintaining an extrapleural dissection, placement of a postoperative
chest tube is avoided. This technique allows direct access to the
posterior and posterolateral disc space.
It
is difficult, and possibly dangerous, to remove central disc
herniations from this approach. Calcified discs may be approached
better by anterior excision. The aorta may be injured with right-sided
costotransversectomy. This technique is difficult in obese patients.
 |
|
Figure 15-7
Costotransversectomy necessitates resection of the pedicle, hemilamina, facet joint, and medial rib on the affected side. This allows decompression without manipulation of the cord. |
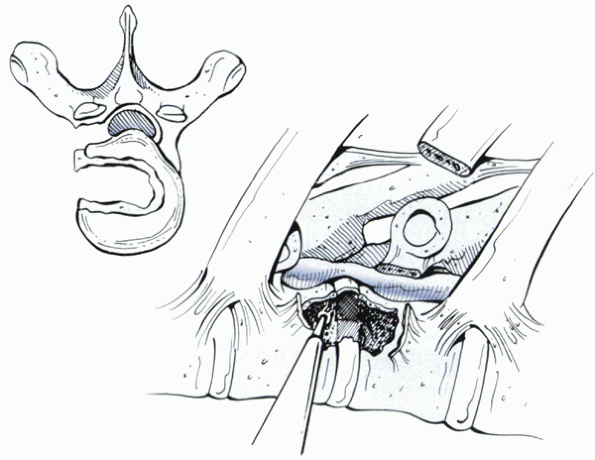
typically involves removal of the pedicle and facet to gain access to
the disc space. It is best reserved for lateral or paracentral discs.
Some surgeons have used this approach successfully for central disc
herniation, but this is technically demanding and requires specially
designed curets. By the nature of the procedure, the operation is
potentially destabilizing. Visualization is limited without a
significant amount of bone removal. Le Roux et al described a
modification of the approach that entails work through the pedicle
(transpedicular decompression). The authors reported excellent results
in lateral and central discs.
It is ideal for foraminal disc fragment excision, regardless of
calcifications. By keeping the periphery of the facet intact, the
procedure theoretically is less destabilizing. Other advantages include
decreased blood loss and shorter operative times. Disadvantages include
difficulty assessing the decompression through the small bone window,
difficult exposure in obese patients, and inability to decompress
centrally.
influenced by the number of discs removed and the amount of bone
resected. One-level or two-level anterior discectomies usually can be
left unfused, whereas multiple-level discectomies may benefit from
fusion. The presence of listhesis, instability, or kyphosis is an
indication for fusion (see Fig. 15-4). The
thoracolumbar junction (T12-L1) is an area of transition that might
benefit from fusion even after a one-level discectomy. This
determination is made by intraoperative assessment of stability and
imaging evidence of angulation or translation.
is not necessary for three consecutive levels of discectomy (which is
rarely performed). After corpectomy, the role of anterior
instrumentation must be weighed against the decision to use
supplemental posterior fixation. Extensive posterior facetectomy and
rib excision may result in instability that might benefit from fusion.
centrolateral thoracic disc herniations treated by anterior discectomy
through an open thoracotomy. All patients had neurologic evidence of
myelopathy. Primary disc excisions (16 of 19) yielded statistically
significant improvements in motor recovery. In these cases, outcomes
were rated as six excellent, six good, and three fair. Three patients
who had undergone a previous laminectomy responded poorly to surgery.
All patients were fused despite being one-level operations. The
authors’ justification included the more extensive bony resection
performed. Their technique avoided dissection within the neural
foramina with the intention of avoiding injury to the medullary artery
anastomosis. They also stated that motion at the degenerated segment
would produce pain and instability postoperatively. Bohlman and
Zdeblick reported their results in 19 cases; in half, they used a
transthoracic approach, and in the other half they used a
costotransversectomy. Five patients were treated for back pain alone
and had no signs of neurologic involvement. Two of these patients had
continued pain, with one remaining disabled with workers’ compensation.
Only one patient who had preoperative myelopathy (treated by
costotransversectomy) did not have neurologic improvement. Two patients
in the costotransversectomy group had a transient paraparesis. Fusion
was not performed routinely. The authors’ technique maintained the
anterior portion of the disc space and anterior longitudinal ligament (Fig. 15-9).
technique in six patients, three of whom had calcified discs.
Myelopathy and pain resolved in all patients. No patient underwent
fusion. Reviewing their results with the transpedicular approach in 20
patients, Roux et al found the only factor that influenced outcome was
the duration of symptoms preoperatively.
thoracoscopic excision of herniated thoracic discs. An initial report
in 1995 noted a long learning curve and various possible complications,
including intercostal neuralgia, atelectasis, excessive epidural
bleeding, and temporary paraparesis. A follow-up series of 29 cases
with 12- to 24-month follow-up showed that 76% of patients were
satisfied with the operation, 20% reported no change, and 4% were
worse. The most common indication was axial or radicular pain, with
only two patients reported to have mild or moderate myelopathy
preoperatively. The authors did not report the neurologic recovery in
these patients. Building on their series, the same group later
published results of 100 patients who underwent the procedure. Only
eight patients had thoracic myelopathy, and although improvements in
Oswestry scores were reported, the authors did not document
specifically neurologic recovery. Discography was used to aid diagnosis
of painful disc herniations. Overall the surgeons showed modest
improvements in pain in most patients. Future analysis must show that
thoracoscopic techniques are cost-effective. Their role in
decompression of the spinal canal for neurologic decompression has not
been well established.
 |
|
Figure 15-8
The pedicle-sparing transfacet approach is ideal for foraminal disc herniation causing radiculopathy. The nerve is displaced superiorly by the extruded disc material. A microscope can be helpful during excision. |
 |
|
Figure 15-9
Leaving the anterior aspect of the disc intact, parts of the posterior vertebral body can be removed to allow greater exposure. This technique can preserve anterior column stability. |
occur from spondylosis. Osteophytes along the posterior border of the
vertebral body at the disc space can encroach on the free space for the
spinal cord. Facet hypertrophy, also thought to arise from the
degenerative process, can decrease the posterior space for the cord.
Degenerative changes can be superimposed on a congenitally narrowed
canal. Other documented, but unusual, causes of thoracic stenosis are
ossification of the posterior longitudinal ligament and ossification of
the ligamentum flavum (see Figure 15-5 A, B).
decompress the spinal canal. There is little agreement about the gold
standard treatment. Conceptually, anterior compressive structures
should be removed by anterior techniques, such as discectomy and
corpectomy. An anterior technique allows direct access and
visualization of anterior spinal cord. Posterior pathology, such as
ossification of the ligamentum flavum or facet overgrowth, is addressed
better with posterior surgery, such as laminectomy and foraminotomy. An
important consideration in planning a laminectomy is the alignment of
the spine. In the cervical spine, lordotic alignment optimizes the
effectiveness of posterior decompression. Although laminectomy may be
an effective decompressive procedure in normokyphotic thoracic spines,
it may not be as effective in hyperkyphotic spines. The decision to
fuse should be based on the amount of destabilization created
iatrogenically during the operation, the degree of preoperative
kyphosis, and the presence of listhesis or instability.
thoracic stenosis, the results generally are worse than after surgery
for the cervical or lumbar stenosis. Palumbo et al
treated 12 patients with either an anterior or a posterior
decompression. The approach was based on the location of the
compressive pathology. Five of 12 patients endured neurologic
deterioration, one of whom was motor intact preoperatively. No attempt
at discectomy was made through the posterior approach. With greater
than 2-year follow-up in all patients, the authors noted that results
tended to deteriorate with time. In only six patients treated with
laminectomy, Barnett et al reported more encouraging results. All
showed some neurologic improvement. These findings are limited by low
patient numbers. Similarly, Smith and Godersky found that seven of
seven patients responded well—neurologically and in pain level—after a
laminectomy and facetectomy for degenerative thoracic stenosis
secondary to spondylosis. Follow-up was less than 1 year in this series.
SJ, Hoist RA, Hemmy DC, et al. Lateral extracavitary approach to
traumatic lesions of the thoracic and lumbar spine. J Neurosurg
1976;45:628-637.
PD, Haglund MM, Harris AB. Thoracic disc disease: experience with the
transpedicular approach in twenty consecutive patients. Neurosurg
1993;33:58-66.
MJ, Regan JJ, McAfee PC, et al. Video-assisted thoracic surgery for the
anterior approach to the thoracic spine. Ann Thorac Surg
1995;59:1100-1106.
JJ, Ben-Yishay A, Mack MJ. Video-assisted thoracoscopic excision of
herniated thoracic disc: description of technique and preliminary
experience in the first 29 cases. J Spinal Disord 1998;11: 183-191.
EG, Kypriades EM, Kellerman AJ, et al. Thoracic disc herniation:
analysis of 14 cases and review of the literature. Acta Neurochir
(Wien) 1992;116:49-52.
T, Battie MC, Gill K, et al. Magnetic resonance imaging findings and
their relationship in the throracic and lumbar spine. Spine
1995;20:928-935.
