Pediatric Tibia and Fibula
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > V – Pediatric Fractures and Dislocations > 50 – Pediatric Tibia and Fibula
50
Pediatric Tibia and Fibula
EPIDEMIOLOGY
-
Tibia fractures represent the third most common pediatric long bone fracture, after femur and forearm fractures.
-
They represent 15% of pediatric fractures.
-
The average age of occurrence is 8 years of age.
-
Of these fractures, 30% are associated with ipsilateral fibular fractures.
-
Ratio of incidence in boys and girls is 2:1.
-
The tibia is the second most commonly
fractured bone in abused children; 26% of abused children with
fractures have a tibia fracture.
ANATOMY
-
The anteromedial aspect of the tibia is subcutaneous, with no overlying musculature for protection.
-
Three consistent ossification centers form the tibia:
-
Diaphyseal: Ossifies at 7 weeks of gestation.
-
Proximal epiphysis: The ossification center appears just after birth, with closure at age 16 years.
-
Distal epiphysis: The ossification center appears in second year, with closure at age 15 years.
-
-
The medial malleolus and tibial tubercle may present as separate ossification centers and should not be confused with fracture.
-
Fibular ossification centers:
-
Diaphyseal: Ossifies at 8 weeks of gestation.
-
Distal epiphysis: The ossification center appears at age 2 years, with closure at age 16 years.
-
Proximal epiphysis: The ossification center appears at age 4 years, with closure at age 16 to 18 years.
-
MECHANISM OF INJURY
-
Of pediatric ipsilateral tibia and fibula fractures, 50% result from motor vehicle trauma.
-
Of tibia fractures with an intact fibula, 81% are caused by indirect rotational forces.
-
Children ages 1 to 4 years old are
susceptible to bicycle spoke trauma, whereas children 4 to 14 years old
most often sustain tibia fractures during athletic or motor vehicle
accidents. -
Isolated fibula fractures are usually the result of a direct blow.
CLINICAL EVALUATION
-
Full pediatric trauma protocol must be
observed because >60% of tibial fractures are associated with motor
vehicle or pedestrian-motor vehicle trauma. -
Patients typically present with the
inability to bear weight on the injured lower extremity, as well as
pain, variable gross deformity, and painful range of motion of the knee
or ankle. -
Neurovascular evaluation is essential, with assessment of both the dorsalis pedis and posterior tibial artery pulses.
-
Palpation of the anterior, lateral, and
posterior (deep and superficial) muscle compartments should be
performed to evaluate possible compartment syndrome. When suspected,
compartment pressure measurement should be undertaken, with emergent
fasciotomies performed in the case of compartment syndrome. -
Field dressings/splints should be removed
with exposure of the entire leg to assess soft tissue compromise and to
rule out open fracture.
P.610
RADIOGRAPHIC EVALUATION
-
Anteroposterior (AP) and lateral views of
the tibia and knee should be obtained. AP, lateral, and mortise views
of the ankle should be obtained to rule out concomitant ankle injury -
Comparison radiographs of the uninjured contralateral extremity are rarely necessary.
-
Technetium bone scan or MRI may be obtained to rule out occult fracture in the appropriate clinical setting.
PROXIMAL TIBIAL METAPHYSEAL FRACTURES
Epidemiology
-
Uncommon, representing <5% of pediatric fractures and 11% of pediatric tibia fractures.
-
Peak incidence is at 3 to 6 years.
Anatomy
-
The proximal tibial physis is generally
structurally weaker than the metaphyseal region; this accounts for the
lower incidence of fractures in the tibial metaphysis.
Mechanism of Injury
-
Most common is force applied to lateral
aspect of the extended knee that causes the cortex of the medial
metaphysis to fail in tension, usually as nondisplaced greenstick
fractures of the medial cortex. -
The fibula usually does not fracture, although plastic deformation may occur.
Clinical Evaluation
-
The patient typically presents with pain, swelling, and tenderness in the region of the fracture.
-
Motion of the knee is painful, and the child usually refuses to ambulate.
-
Valgus deformity is typically present.
Radiographic Evaluation
-
AP and lateral views of the tibia should
be obtained, as well as appropriate views of the knee and ankle to rule
out associated injuries.
P.611
Classification
Descriptive
-
Angulation
-
Displacement
-
Open versus closed
-
Pattern: transverse, oblique, spiral, greenstick, plastic deformation, torus
-
Comminution
Treatment
Nonoperative
-
Nondisplaced fractures may be treated in a long leg cast with the knee in near full extension and with a varus mold.
-
Displaced fractures should undergo closed
reduction with the patient under general anesthesia, with application
of a long leg cast with the knee in full extension and varus moment
placed on the cast to prevent valgus collapse. -
The cast should be maintained for 6 to 8 weeks with frequent radiographic evaluation to rule out displacement.
-
Normal activities may be resumed when normal knee and ankle motions are restored and the fracture site is nontender.
Operative
-
Fractures that cannot be reduced by closed means should undergo open reduction with removal of interposed soft tissue.
-
The pes anserinus insertion should be repaired if torn, with restoration of tension.
-
A long leg cast with the knee in full
extension should be placed and maintained for 6 to 8 weeks
postoperatively with serial radiographs to monitor healing. -
Open fractures or grossly contaminated
fractures with associated vascular compromise may be treated with
debridement of compromised tissues and external fixation, particularly
in older children. Regional or free flap or skin grafting may be
required for skin closure.
Complications
-
Progressive valgus angulation: May result
from a combination of factors, including disruption of the lateral
physis at the time of injury, exuberant medial callus formation that
results in fracture overgrowth, entrapment of periosteum at the medial
fracture site with consequent stimulation of the physis, or concomitant
pes anserinus injury that results in a loss of inhibitory tethering
effect on the physis, allowing overgrowth. The deformity is most
prominent within 1 year of fracture; younger patients may experience
spontaneous correction with remodeling, although older patients may
require hemiepiphysiodesis or corrective osteotomy. -
Premature proximal tibial physeal
closure: May occur with unrecognized crush injury (Salter V) to the
proximal tibial physis, resulting in growth arrest. This most commonly
affects the anterior physis and leads to a recurvatum deformity of the
affected knee.
P.612
DIAPHYSEAL FRACTURES OF THE TIBIA AND FIBULA
Epidemiology
-
Of pediatric tibial fractures, 39% occur in the middle third.
-
Approximately 30% of pediatric diaphyseal
fractures are associated with a fracture of the fibula. Occasionally,
this is in the form of plastic deformation, producing valgus alignment
of the tibia. -
Isolated fractures of the fibular shaft are rare and result from direct trauma to the lateral aspect of the leg.
Anatomy
-
The nutrient artery arises from the
posterior tibial artery, entering the posterolateral cortex distal to
the origination of the soleus muscle, at the oblique line of the tibia.
Once the vessel enters the intramedullary canal, it gives off three
ascending branches and one descending branch. These give rise to the
endosteal vascular tree, which anastomoses with periosteal vessels
arising from the anterior tibial artery. -
The anterior tibial artery is particularly vulnerable to injury as it passes through a hiatus in the interosseus membrane.
-
The peroneal artery has an anterior communicating branch to the dorsalis pedis artery.
-
The fibula is responsible for 6% to 17%
of weight-bearing load. The common peroneal nerve courses around the
neck of the fibula, which is nearly subcutaneous in this region; it is
therefore especially vulnerable to direct blows or traction injuries at
this level.
Mechanism of Injury
-
Direct: Trauma to the leg occurs, mostly in the form of vehicular trauma or pedestrian-motor vehicle accident.
-
Indirect: In younger children, most
tibial fractures result from torsional forces. These spiral and oblique
fractures occur as the body mass rotates on a planted foot. The fibula
prevents significant shortening when intact, but the fracture
frequently falls into varus.
Clinical Evaluation
-
The patient typically presents with pain, swelling, and tenderness in the region of the fracture.
-
Motion of the knee is painful, and the child usually refuses to ambulate.
-
Children with stress fractures of the tibia may complain of pain on weight bearing that is partially relieved by rest.
Radiographic Evaluation
-
Standard AP and lateral views of the leg should be obtained.
-
Radiographs of the ipsilateral ankle and knee should be obtained to rule out associated injuries.
-
Comparison views of the uninjured, contralateral leg may be obtained in cases in which the diagnosis is unclear.
-
Technetium bone scan or MRI may be obtained to rule out occult fracture.
P.613
Classification
Descriptive
-
Angulation
-
Displacement
-
Open versus closed
-
Pattern: transverse, oblique, spiral, greenstick, plastic deformation, torus
-
Comminution
Treatment
Nonoperative
-
Most pediatric fractures of the tibia and
fibula are uncomplicated and may be treated by simple manipulation and
casting, especially when they are nondisplaced or minimally displaced.
However, isolated tibial diaphyseal fractures tend to fall into varus,
whereas fractures of the tibia and fibula tend to fall into valgus with
shortening and recurvatum (Fig. 50.1).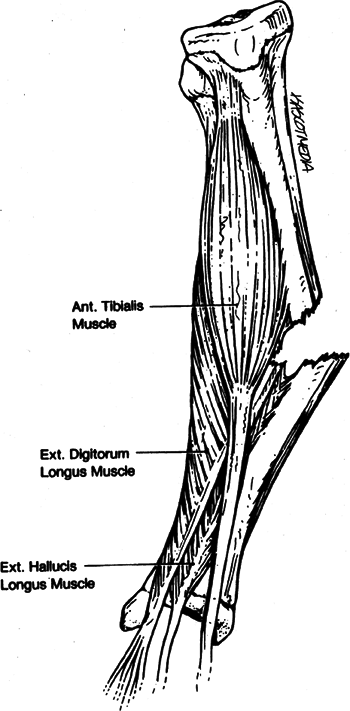 Figure
Figure
50.1. The muscles in the anterior and the lateral compartments of the
lower leg produce a valgus deformity in complete ipsilateral tibia and
fibula fractures.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
Displaced fractures may be initially treated with closed reduction and casting with the patient under general anesthesia.
-
In children, acceptable reduction
includes 50% apposition of the fracture ends, <1 cm of shortening,
and <5- to 10-degree angulation in the sagittal and coronal planes. -
A long leg cast is applied with the ankle
slightly plantar flexed (20 degrees for distal and middle third
fractures, 10 degrees for proximal third fractures) to prevent
posterior angulation of the fracture in the initial 2 to 3 weeks. The
knee is flexed to 45 degrees to provide rotational control and to
prevent weight bearing. -
Fracture alignment must be carefully
monitored, particularly during the initial 3 weeks when atrophy and
diminished swelling may result in loss of reduction. Some patients
require repeat manipulation and cast application under general
anesthesia 2 to 3 weeks after initial casting. -
The cast may require wedging (opening or closing wedge) to provide correction of angulatory deformity.
-
Time to healing varies according to patient age:
-
Neonates: 2 to 3 weeks
-
Children: 4 to 6 weeks
-
Adolescents: 8 to 12 weeks
-
-
P.614
Operative
-
Operative management of tibial fractures in children are typically required in <5% of cases.
-
Indications for operative management include:
-
Open fracture.
-
Fractures in which a stable reduction is unable to be achieved or maintained.
-
Associated vascular injury.
-
Fractures associated with compartment syndrome.
-
Severely comminuted fractures.
-
Associated femoral fracture (floating knee).
-
Fractures in patients with spasticity syndromes (cerebral palsy, head injury).
-
Patients with bleeding diatheses (hemophilia).
-
Patients with multisystem injuries.
-
-
Open fractures or grossly contaminated
fractures with associated vascular compromise may be treated with
debridement of compromised tissues and external fixation, particularly
in older children. Severe degloving injuries may require the use of
flexible, intramedullary nails for fracture stabilization. Regional or
free flaps or skin grafting may be required for skin closure. -
Other methods of operative fixation
include percutaneous pins, plates and screws, flexible intramedullary
nails or rigid intramedullary nails (in adolescents after closure of
the proximal tibia physis). -
Postoperatively, a long leg cast is
usually placed (depending on the method of fixation), with the knee in
45 degrees of flexion to allow for rotational control. The cast is
maintained for 4 to 16 weeks depending on the status of healing, as
evidenced by serial radiographs, as well as the healing of associated
injuries.
P.615
Complications
-
Compartment syndrome: In pediatric tibia
fractures, compartment syndrome is most common after severe injury in
which the interosseous membrane surrounding the anterior compartment is
disrupted. Patients with elevated compartment pressures >30 mm Hg or
within 30 mm Hg of diastolic blood pressure should receive emergency
fasciotomies of all four compartments of the leg to avoid neurologic
and ischemic sequelae. -
Angular deformity: Correction of deformity varies by age and gender.
-
Girls <8 years old and boys <10 years old often experience significant remodeling.
-
Girls 9 to 12 years old and boys 11 to 12 years old can correct up to 50% of angulation.
-
In children >13 years, <25% angular correction is expected.
-
Posterior and valgus angulation tends to correct the least with remodeling.
-
-
Malrotation: Rotational deformity of the
tibia does not correct with remodeling and is poorly tolerated, often
resulting in malpositioning of the foot with the development of
associated ankle and foot problems. Supramalleolar osteotomy may be
required for rotational correction. -
Premature proximal tibial physeal
closure: This may occur with unrecognized crush injury (Salter Type V)
to the proximal tibial physis, resulting in growth arrest. This most
commonly affects the anterior physis and leads to a recurvatum
deformity of the affected knee. -
Delayed union and nonunion: Uncommon in
children, but it may occur as a result of infection, the use of
external fixation, or inadequate immobilization. Fibulectomy, bone
grafting, reamed intramedullary nailing (adolescents), and plate
fixation with bone grafting have all been described as methods to treat
tibial nonunions in the pediatric population.
FRACTURES OF THE DISTAL TIBIAL METAPHYSIS
Epidemiology
-
Fractures of the distal third of the tibia comprise approximately 50% of pediatric tibia fractures.
-
Most occur in patients younger than 14 years, with the peak range of incidence in children between ages 2 and 8 years.
Anatomy
-
Distally, the tibia flares out as the
cortical diaphyseal bone changes to cancellous metaphyseal bone
overlying the articular surface. This is similar to the tibial plateau
in that there is primarily cancellous bone within a thin cortical shell.
Mechanism of Injury
-
Indirect: An axial load results from a jump or fall from a height.
-
Direct: Trauma to the lower leg occurs,
such as in bicycle spoke injuries in which a child’s foot is thrust
forcibly between the spokes of a turning bicycle wheel, resulting in
severe crush to the distal leg, ankle, and foot with variable soft
tissue injury.
P.616
Clinical Evaluation
-
Patients typically are unable to ambulate or are ambulatory only with severe pain.
-
Although swelling may be present with
variable abrasions or lacerations, the foot, ankle, and leg typically
appear relatively normal without gross deformity. -
The entire foot, ankle, and leg should be
exposed to evaluate the extent of soft tissue injury and to assess for
possible open fracture. -
A careful neurovascular examination is important, and the presence of compartment syndrome must be excluded.
-
In cases of bicycle spoke injuries,
palpation of all bony structures of the foot and ankle should be
performed as well as assessment of ligamentous integrity and stability.
Radiographic Evaluation
-
AP and lateral views of the leg should be
obtained. Appropriate views of the ankle and knee should be taken to
rule out associated injuries, as well as views of the foot as indicated. -
Fractures of the distal metaphysis
typically represent greenstick injuries, with anterior cortical
impaction, posterior cortical disruption, and tearing of the overlying
periosteum, often resulting in a recurvatum pattern of injury. -
In severe torsional injuries with impaction or distraction forces, a spiral fracture may result.
-
Computed tomography is usually unnecessary, but it may aid in fracture definition in comminuted or complex fractures.
Classification
Descriptive
-
Angulation
-
Displacement
-
Open versus closed
-
Pattern: transverse, oblique, spiral, greenstick, plastic deformation, torus
-
Comminution
-
Associated injuries: knee, ankle, foot
Treatment
Nonoperative
-
Nondisplaced, minimally displaced, torus,
or greenstick fractures should be treated with manipulation and
placement of a long leg cast. -
In cases of recurvatum deformity of the
tibial fracture, the foot should be placed in plantar flexion to
prevent angulation into recurvatum. -
After 3 to 4 weeks of plaster
immobilization, if the fracture demonstrates radiographic evidence of
healing, the long leg cast is discontinued and is changed to a short
leg walking cast with the ankle in the neutral position. -
A child with a bicycle spoke injury
should be admitted as an inpatient for observation, because the extent
of soft tissue compromise may not be initially evident.P.617-
A long leg splint should be applied with
the lower extremity elevated for 24 hours, with serial examination of
the soft tissue envelope over the ensuing 48 hours. -
If no open fracture exists and soft
tissue compromise is minimal, a long leg cast may be placed before
discharge, with immobilization as described previously.
-
Operative
-
Surgical intervention is warranted for cases of open fracture or when stable reduction is not possible by closed means.
-
Unstable distal tibial fractures can
typically be managed with closed reduction and percutaneous pinning
using Steinmann pins or Kirschner wire fixation. Rarely, a comminuted
fracture may require open reduction and internal fixation using pins or
plates and screws.-
Postoperatively, the patient is
immobilized in a long leg cast. The fracture should be monitored with
serial radiographs to assess healing. At 3 to 4 weeks, the pins may be
removed with replacement of the cast either with a long leg cast or a
short leg walking cast, based on the extent of healing.
-
-
Open fractures may require external
fixation to allow for wound management. Devitalized tissue should be
débrided as necrosis becomes apparent. Aspiration of large hematomas
should be undertaken to avoid compromise of overlying skin. Skin grafts
or flaps (regional or free) may be necessary for wound closure.
Complications
-
Recurvatum: Inadequate reduction or
fracture subsidence may result in a recurvatum deformity at the
fracture. Younger patients tend to tolerate this better, because
remodeling typically renders the deformity clinically insignificant.
Older patients may require supramalleolar osteotomy for severe
recurvatum deformity that compromises ankle function and gait. -
Premature distal tibial physeal closure:
May occur with unrecognized crush injury (Salter Type V) to the distal
tibial physis, resulting in growth arrest.
TODDLER’S FRACTURE
Epidemiology
-
A toddler’s fracture is by definition a spiral fracture of the tibia in the appropriate age group.
-
Most of these fractures occur in children younger than 2.5 years.
-
The average age of incidence is 27 months.
-
This tends to occur in boys more often than in girls and in the right leg more frequently than the left.
Anatomy
-
The distal epiphysis appears at
approximately 2 years of age; thus, physeal injuries of the distal
tibia may not be readily apparent and must be suspected.
P.618
Mechanism of Injury
-
The classic description of the mechanism
of a toddler’s fracture is external rotation of the foot with the knee
in fixed position, producing a spiral fracture of the tibia with or
without concomitant fibular fracture. -
This injury has also been reported as a result of a fall.
Clinical Evaluation
-
Patients typically present irritable and nonambulatory or with an acute limp.
-
The examination of a child refusing to
ambulate without readily identifiable causes should include a careful
history, with attention to temporal progression of symptoms and signs
(e.g., fever), as well as a systematic evaluation of the hip, thigh,
knee, leg, ankle, and foot, with attention to points of tenderness,
swelling, or ecchymosis. This should be followed by radiographic
evaluation as well as appropriate laboratory analysis if the diagnosis
remains in doubt. -
In the case of a toddler’s fracture, pain
and swelling are variable on palpation of the tibia. These features are
usually appreciated over the anteromedial aspect of the tibia, where
its subcutaneous nature allows for minimal soft tissue protection.
Radiographic Evaluation
-
AP and lateral views of the leg should be obtained.
-
An internal oblique radiograph of the leg may be helpful for demonstration of a nondisplaced spiral fracture.
-
Occasionally, an incomplete fracture may
not be appreciated on presentation radiographs but may become
radiographically evident 7 to 10 days after the injury as periosteal
new bone formation occurs. -
Technetium bone scans may aid in the
diagnosis of toddler’s fracture by visualization of diffusely increased
uptake throughout the tibia. This may be differentiated from infection,
which tends to produce a localized area of increased uptake.
Treatment
-
A long leg cast for 2 to 3 weeks followed
by conversion to a short leg walking cast for an additional 2 to 3
weeks is usually sufficient. -
Manipulation is generally not necessary because angulation and displacement are usually minimal and within acceptable limits.
Complications
-
Complications of toddler’s fractures are
rare owing to the low-energy nature of the injury, the age of the
patient, and the rapid and complete healing that typically accompanies
this fracture pattern. -
Rotational deformity: Toddler’s fractures
may result in clinically insignificant rotational deformity of the
tibia as the fracture slides minimally along the spiral configuration.
This is usually unnoticed by the patient but may be appreciated on
comparison examination of the lower limbs.
P.619
STRESS FRACTURES
Epidemiology
-
Most tibia stress fractures occur in the proximal third.
-
The peak incidence of tibia stress fractures in children is between the ages of 10 and 15 years.
-
Most fibula stress fractures occur in the distal third.
-
The peak incidence of fibula stress fractures in children is between the ages of 2 and 8 years.
-
The tibia is more often affected than the fibula in children; the opposite is true in adults.
Mechanism of Injury
-
An acute fracture occurs when the force
applied to a bone exceeds the bone’s capacity to withstand it. A stress
fracture occurs when a bone is subjected to repeated trauma with a
strain that is less than what would have produced an acute fracture. -
With microtrauma, osteoclastic tunnel
formation increases to remodel microcracks. New bone formation results
in the production of immature, woven bone that lacks the strength of
the mature bone it replaced, predisposing the area to fracture with
continued trauma. -
Stress fractures in older children and adolescents tend to be as a result of athletic participation.
-
Distal fibula stress fractures have been
referred to as the “ice skater’s fracture,” because of the repeated
skating motion that results in a characteristic fibular fracture
approximately 4 cm proximal to the lateral malleolus.
Clinical Evaluation
-
Patients typically presents with an antalgic gait that is relieved by rest, although younger patients may refuse to ambulate.
-
The pain is usually described as insidious in onset, worse with activity, and improved at night.
-
Swelling is generally not present,
although the patient may complain of a vague ache over the site of
fracture with tenderness to palpation. -
Knee and ankle range of motion are usually full and painless.
-
Occasionally, the patient’s symptoms and signs may be bilateral.
-
Muscle sprains, infection, and
osteosarcoma must be excluded. Exercise-induced compartment syndrome
overlying the tibia may have a similar clinical presentation.
Radiographic Evaluation
-
AP and lateral views of the leg should be
obtained to rule out acute fracture or other injuries, although stress
fractures are typically not evident on standard radiographs for 10 to
14 days after initial onset of symptoms. -
Radiographic evidence of fracture repair
may be visualized as periosteal new bone formation, endosteal
radiodensity, or the presence of “eggshell” callus at the site of
fracture. -
Technetium bone scan reveals a localized
area of increased tracer uptake at the site of fracture and may be
performed within 1 to 2 days of injury. -
Computed tomography rarely demonstrates
the fracture line, although it may delineate increased marrow density
and endosteal/periosteal new bone formation and soft tissue edema. -
Magnetic resonance imaging may demonstrate a localized band of very low signal intensity continuous with the cortex.
P.620
Classification
-
Stress fractures may be classified as
complete versus incomplete or acute versus chronic or recurrent. They
rarely are displaced or angulated.
Treatment
-
The treatment of a child presenting with a tibia or fibula stress fracture begins with activity modification.
-
The child may be placed in a long leg
(tibia) or short leg (fibula) cast, initially non–weight bearing with a
gradual increase in activity level. The cast should be maintained for 4
to 6 weeks until the fracture site is nontender and radiographic
evidence of healing occurs. -
Nonunion may be addressed with open excision of the nonunion site with iliac crest bone grafting or electrical stimulation.
Complications
-
Recurrent stress fractures: These may be
the result of overzealous training regimens, such as for gymnastics or
ice skating. Activity modification must be emphasized to prevent
recurrence. -
Nonunion: Rare, occurring most commonly in the middle third of the tibia.
