Lateral Tibial Plateau Fracture: Open Reduction and Internal Fixation
VI – Knee > Chapter 30 – Lateral Tibial Plateau Fracture: Open
Reduction and Internal Fixation
and from direct axial compressive forces. These forces drive the
femoral condyle into the tibial plateau, producing a spectrum of
fracture patterns. Fracture fragment size, location, and displacement
are determined by the direction, magnitude, and location of the
generated force, as well as by the bone quality and the degree of knee
flexion at the moment of impact. The combination of compression and
valgus produces a lateral plateau fracture, and compression coupled
with varus results in a medial fracture pattern. The prevalence of
lateral plateau fractures is related to the valgus inclination of the
anatomic axis and the usual lateral direction of the applied force.
This chapter discusses open reduction and internal fixation of the
lateral tibial plateau.
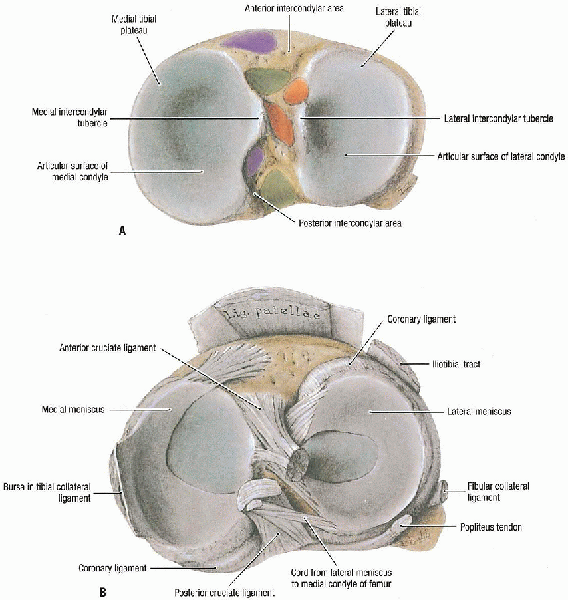
The medial plateau is larger and is concave in the sagittal and coronal
axes. The lateral plateau extends higher and is convex in the sagittal
and coronal planes. The normal tibial plateau has a 10-degree
posteroinferior slope. The two plateaus are separated from one another
by the intercondylar eminence, which is nonarticular and serves as the
tibial attachment of the cruciate ligaments.
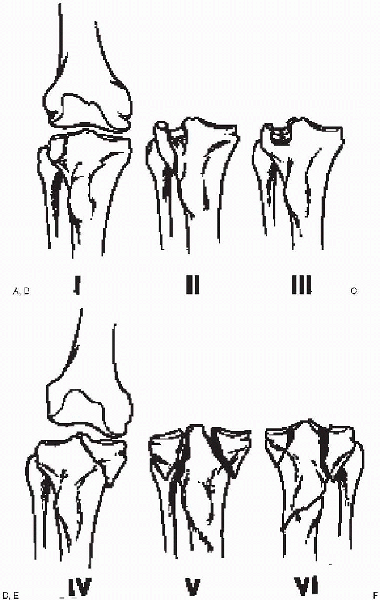
Type I is a wedge (split) fracture of the lateral tibial plateau. Type
II is a split depression fracture of the lateral plateau; the femoral
condyle first splits the condyle and then depresses the medial edge of
the remaining plateau. Type III is a pure central depression fracture
of the lateral plateau without an associated split. Type IV is a
fracture of the medial tibial plateau that usually involves the entire
condyle. Type V is a bicondylar fracture that typically consists of
split fractures of the medial and lateral plateaus without articular
depression. Type VI is a tibial plateau fracture with an associated
proximal shaft fracture.
for open versus closed management of tibial plateau fractures. Some
surgeons advocate nonoperative treatment for fractures with up to 1 cm
of depression. Others accept only minimal displacement of the articular
surface. However, there is general agreement that instability of more
than 10 degrees (compared with the uninvolved knee) of the nearly
extended knee is an indication for operative intervention. Open tibial
plateau fractures or those associated with a compartment syndrome or
vascular insult require emergent care.
displacement resulting in instability is unknown; it depends on the
fracture type, location, and associated ligamentous disruption. Split
fractures, in addition to disrupting the articular surface, involve the
rim of the tibial plateau and are likely to be unstable in response to
axial loading. Split depression fractures are at a higher risk for
instability because of the depressed surface adjacent to the split
component. Pure central depression fractures are usually stable unless
the depression involves the entire plateau; the intact cortical rim
provides varus-valgus stability. Plateau fractures that are associated
with a tibial shaft fracture are usually not amenable to closed
treatment, because traction often results in separation of the shaft
components rather than reduction of the articular surface.
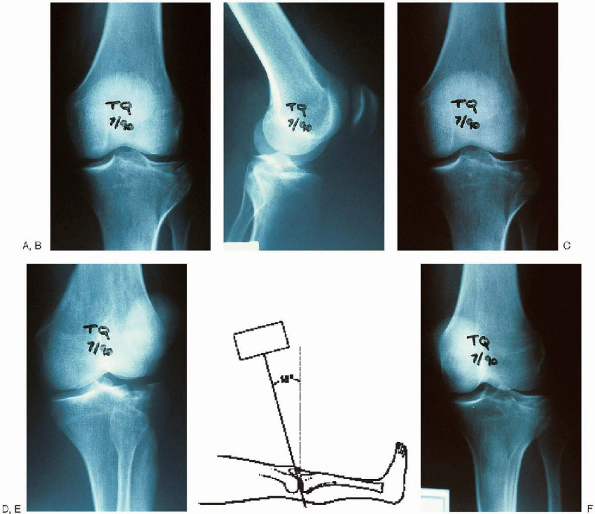
These films are analyzed for rim widening, articular depression, shaft
extension, and bony avulsions. The amount of condylar depression can be
measured from the remaining intact articular surface on the 10-degree
caudal plateau or lateral radiographs.
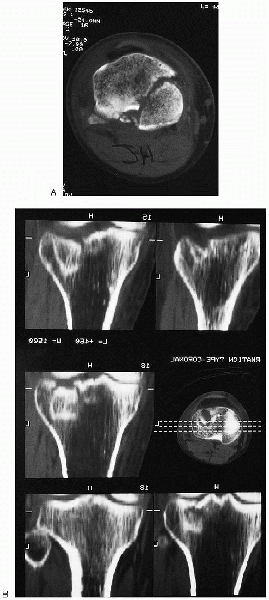
are useful for the preoperative plan. Tri-spiral and computed
tomography coupled with sagittal reconstructions are helpful in
evaluating the degree of articular displacement
(Fig. 30-4).
These studies are an excellent adjunct to plain x-ray films in the
preoperative planning for lag screw placement, particularly when
contemplating percutaneous fixation. Magnetic resonance imaging may
play a role in the future in the evaluation of meniscal and ligamentous
injuries associated with these fractures.
 |
|
FIGURE 30-1. A and B: Right tibial plateau. (From Agur AMR, Lee MJ. Grant’s atlas of anatomy, 10th ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
|
 |
|
FIGURE 30-2. The Schatzker classification of tibial plateau fractures. A: Type I, split fracture of the lateral tibial plateau. B: Type II, split depression fracture of the lateral plateau. C: Type III, central depression fracture of the lateral plateau. D: Type IV, fracture of the medial tibial plateau. E: Type V, bicondylar tibial plateau fracture. F: Type VI, tibial plateau fracture with an associated proximal shaft fracture.
|
 |
|
FIGURE 30-3. Radiographic evaluation of tibial plateau fractures should include an anteroposterior view (A), a lateral view (B), two oblique views (C and D), and the 10-degree caudal plateau view (E and F).
|
 |
|
FIGURE 30-4. Computed tomographic scan (A) and sagittal reconstruction (B) of a tibial plateau fracture.
|
Although useful for simpler fractures, preoperative planning is
critical for more complex injuries. This forces the surgeon to
understand the “personality of the fracture” and mentally prepare an
operative plan. All aspects of the reduction and fixation should be
drawn out to help avoid technical pitfalls and ensure that all the
needed equipment is available.
-
Small fragment plate and screws
-
Large fragment plate and screws
-
Large- and small-diameter cannulated screws
-
Large and small pointed reduction clamps
-
Femoral distractor with or without an external fixator set
-
Tamp and gouge set
 |
|
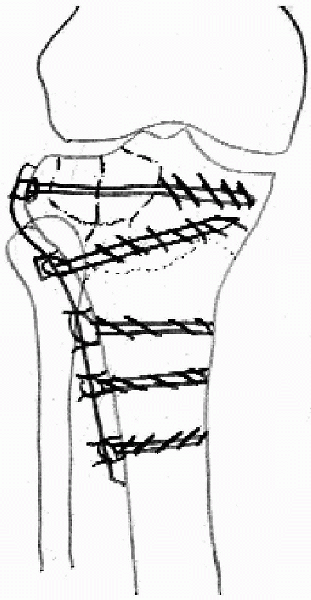
FIGURE 30-5. Preoperative plan for operative treatment of a lateral tibial plateau fracture.
|
 |
|
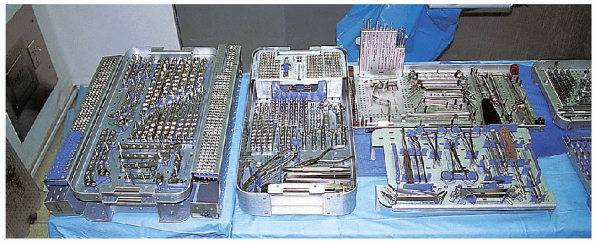
FIGURE 30-6.
The instruments needed for open reduction and internal fixation of a lateral tibial plateau fracture: large fragment set and small fragment set (left to right), cannulated screw set (far right, top), second small fragment set (far right, bottom). |
 |
|
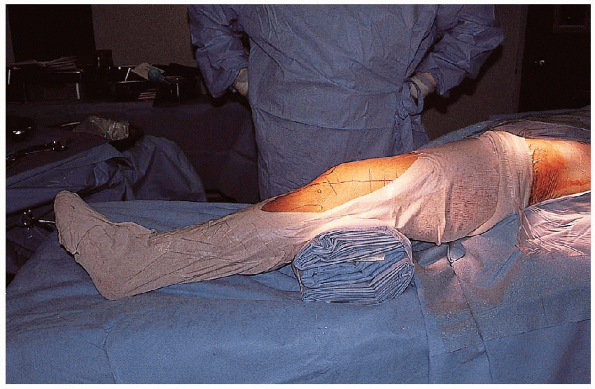
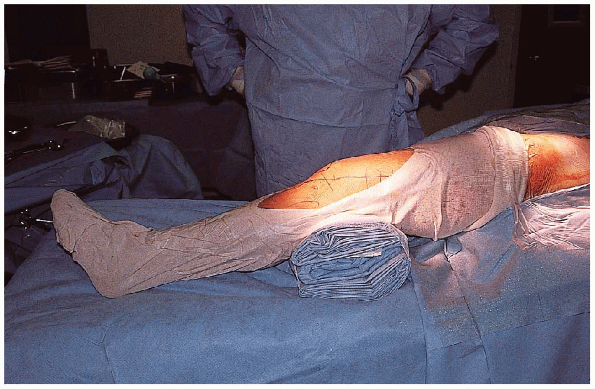
FIGURE 30-7. The patient is positioned supine with a bolster under the knee.
|
 |
|
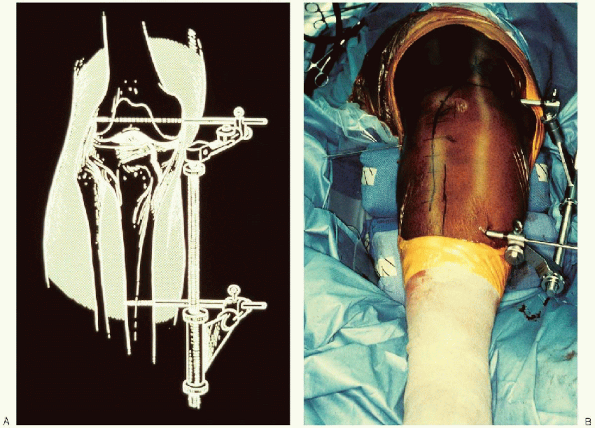
FIGURE 30-8. A and B: Use of a femoral distractor to reduce the lateral tibial plateau.
|
under the knee or on a table that has the ability to flex the foot of
the table (Fig. 30-7). The ipsilateral iliac
crest should be prepared and draped if a need for autogenous bone graft
is contemplated. The patient’s position should take into account the
need for intraoperative image intensification, with the ability to
obtain anteroposterior, lateral, plateau, and oblique views. If
arthroscopy is to be used, a well-padded leg holder or post should be
available.
ligamentotaxis using a femoral distractor. This instrument be placed on
the ipsilateral side of the tibial plateau fracture, extending across
the knee joint, with one pin in the femoral condyle and the other pin
in the mid to distal tibia, well away from the anticipated distal end
of the implant (Fig. 30-8). In the event of bicondylar or type VI fractures, bilateral femoral distractors may be required.
inflation of the tourniquet, the knee should be flexed to allow the
quadriceps muscle to stretch distally. Exposure of the tibial plateau
can be gained through a variety of approaches. The surgical approach
should provide maximum visualization, combined with preservation of all
vital structures and minimal soft tissue and osseous devitalization.
Skin incisions for tibial plateau fractures should be longitudinal (Fig. 30-9).
Midline skin incisions are favored in bicondylar fractures to allow
access to both knee compartments and facilitate any future
reconstructive procedures. Because most plateau fractures involve the
lateral compartment, a lateral parapatellar incision and arthrotomy are
often used. Medial fractures use a medial parapatellar approach. Flaps
that are raised should be full thickness down to the crural fascia and
retinaculum and include the subcutaneous fat (Fig. 30-10).
 Excessive
Excessivesoft tissue dissection can result in osseous devascularization and
increase the risk for soft tissue complications, including skin slough.
 |
|
FIGURE 30-9. Use of a longitudinal skin incision to approach the lateral tibial plateau.
|
 |
|
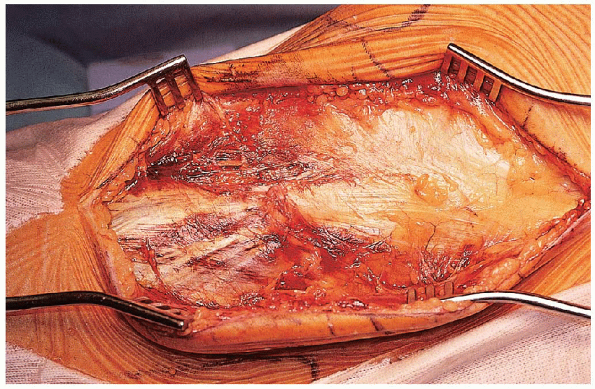
FIGURE 30-10. Exposure of the fascia and retinaculum through a full-thickness skin flap.
|
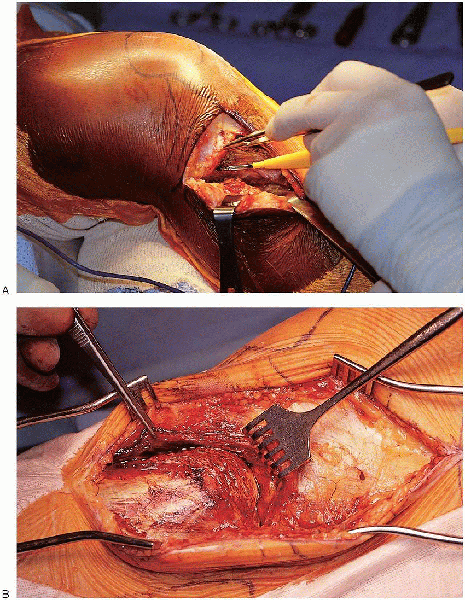
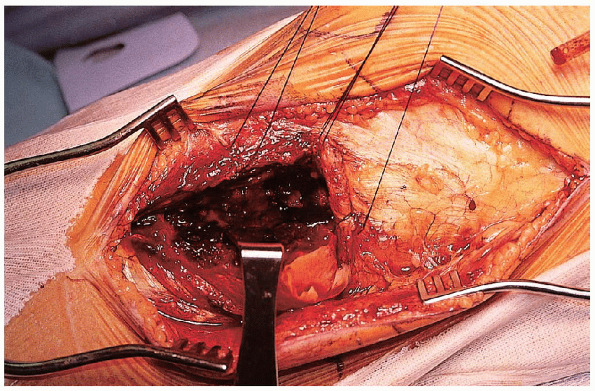
 or vertical with division of the anterior horn of the lateral meniscus. When
or vertical with division of the anterior horn of the lateral meniscus. Whenusing a submeniscal arthrotomy, the surgeon should leave a soft tissue
cuff on the proximal tibia for capsular reattachment or prepare to use
Mitek anchors. With either approach, the split fracture component can
be displaced open and depressed fracture fragments elevated. The joint
must be examined for evidence of meniscal pathology, because meniscal
tears have been reported in up to 50% of tibial plateau fractures.
 Lesions
Lesionsthat are not appropriate for repair should be excised at this time.
Peripheral tears should have a suture repair at closure. Posteromedial
fractures of the plateau can be approached through a separate incision
between the medial gastrocnemius and semitendinosus and then between
the medial collateral ligament and the posterior oblique ligament.
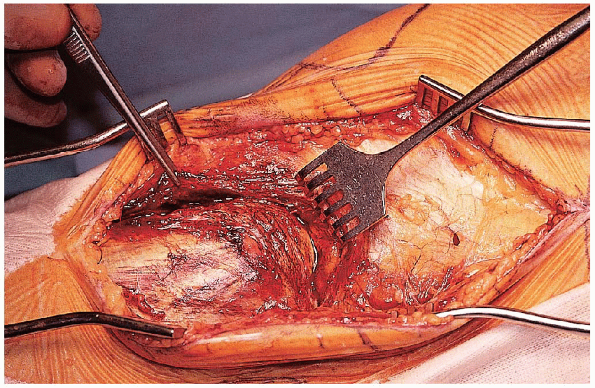
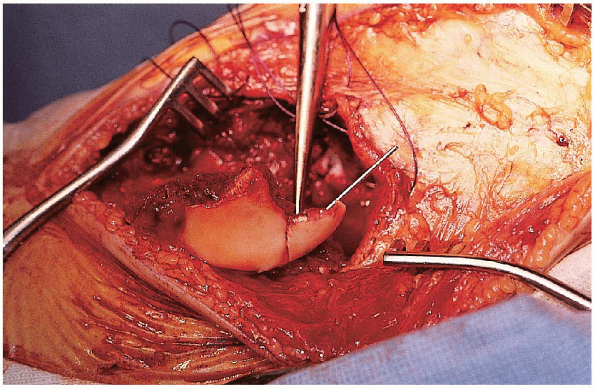
Exposure of the depressed articular fragment is accomplished by opening
the metaphysis like a book at the split fracture line and hinging the
peripheral fragments outward, preserving their soft tissue attachments (Fig. 30-13).

Reduction of the depressed articular surface fragment should start by
recognizing the area of uninvolved articular surface. Depressed
articular fragments should be elevated en mass from below as large cancellous blocks to prevent articular surface fragmentation (Fig. 30-14).
 This can be achieved with the use of a bone tamp or elevator working through the split component.
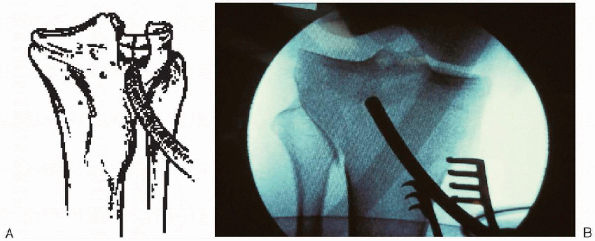
This can be achieved with the use of a bone tamp or elevator working through the split component.wires (K-wires) is performed (Fig. 30-15). 
These K-wires should be placed to avoid interfering with reduction of
the split fragment. At this point, the metaphyseal defect should be
bone grafted  and the split fragment reduced
and the split fragment reduced  and provisionally stabilized (Fig. 30-16).
and provisionally stabilized (Fig. 30-16).
 |
|
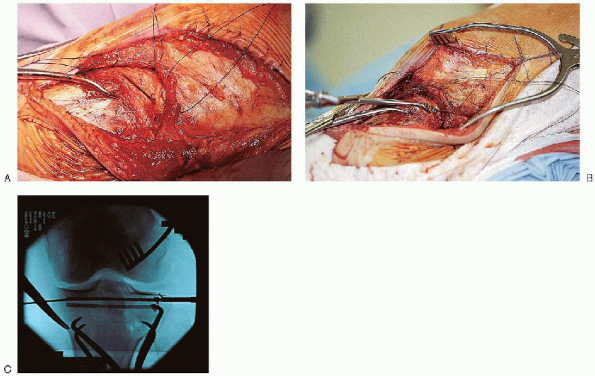
FIGURE 30-11. A and B: Use of submeniscal arthrotomy to approach the articular surface.
|
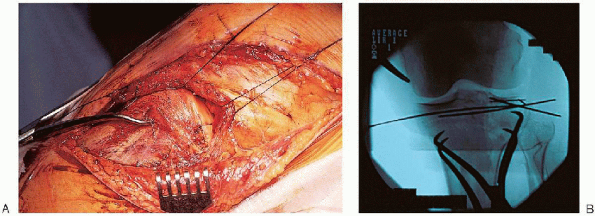
stabilization is performed. Definitive stabilization requires the
insertion of two 6.5- or 7.0-mm cancellous lag screws parallel to the
joint (Fig. 30-17), followed by metaphyseal buttress plating (Fig. 30-18).
This buttress must be located at the distal extent of the fracture line
and serves to prevent shear forces from causing late collapse. The
choice of plates depends on the degree of cortical comminution and may
be as simple as a washer (i.e., one-hole plate), two-hole plate, T- or
L- buttress plate, or Burri plate. The surgeon should select that plate that offers stable fixation but minimizes bulk to prevent complications with wound closure.
irrigated and the wound closed. The coronary ligament of the knee
capsule is reattached using sutures or Mitek anchors, or both (Fig. 30-19). Wound closure is performed over suction drains. If the wound cannot be closed without tension, it is
preferable to leave the incision partially open and covered with a
sterile dressing. Wound closure may then be performed at a later date.
 |
|
FIGURE 30-12. Identification of the split fracture component.
|
 |
|
FIGURE 30-13. Working through the split fracture component to expose the area of articular depression.
|
 |
|
FIGURE 30-14. A and B: Use of a tamp to elevate depressed articular fragments en mass to pre-
|
 |
|
FIGURE 30-15. Reduction and provisional stabilization of the articular fragments using Kirschner wires.
|
 |
|
FIGURE 30-16. Reduction (A) and provisional stabilization (B) of the split fracture component.
|
hinged knee brace and started on continuous passive motion with a range
of motion of 0 to 30 degrees and advanced as tolerated. The machine is
kept on as much as possible during waking hours; early motion has been
clearly demonstrated to promote cartilage healing. Physical therapy for
active assisted range-of-motion exercises and touch-down weight bearing
is initiated and continued until the patient is independent with
ambulatory aids. Full weight bearing is permitted
by 12 weeks based on radiographic evidence of consolidation.
 |
|
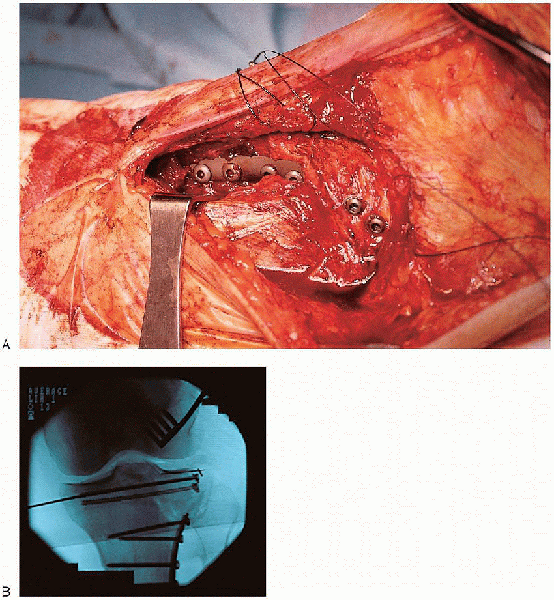
FIGURE 30-17. A to C: Placement of lag screws across the split fracture component.
|
 |
|
FIGURE 30-18. A and B: Placement of the lateral buttress plate.
|
 |
|
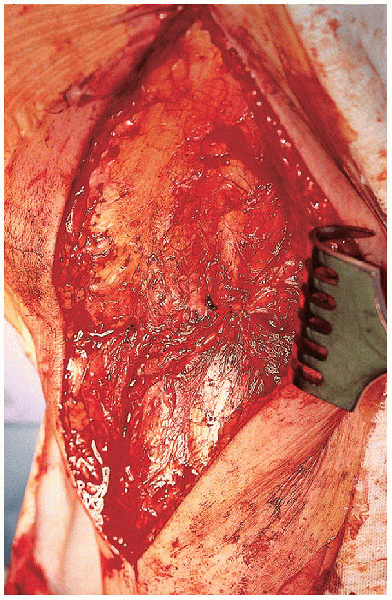
FIGURE 30-19. Reattachment of the coronary ligament of the knee capsule
|
The use of an anterior incision of the meniscus for exposure of tibial
plateau fractures requiring open reduction and internal fixation. J Orthop Trauma 1996;10: 243-247.
