Pediatric Ankle
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > V – Pediatric Fractures and Dislocations > 51 – Pediatric Ankle
51
Pediatric Ankle
EPIDEMIOLOGY
-
Ankle injuries account for 25% to 38% of
all physeal injuries, third in frequency following phalangeal and
distal radius physeal injuries.-
Fifty-eight percent of ankle physeal injuries occur during athletic participation.
-
They represent 10% to 40% of all injuries in skeletally immature athletes.
-
Tibial physeal fractures are most common from 8 to 15 years of age.
-
Fibular physeal injuries are most common from 8 to 14 years of age.
-
-
Ligamentous injuries are rare in children because their ligaments are stronger relative to the physis.
-
After age 15 to 16 years, see adult fracture pattern.
ANATOMY
-
The ankle is a modified hinge joint
stabilized by medial and lateral ligamentous complexes. All ligaments
attach distal to the physes of the tibia and fibula—important in the
pathoanatomy of pediatric ankle fracture patterns. -
The distal tibial ossific nucleus appears
between the ages of 6 and 24 months; it fuses with the tibial shaft at
about age 15 years in girls and 17 years in boys. Over an 18-month
period, the lateral portion of the distal tibial physis remains open
while the medial part has closed. -
The distal fibular ossific nucleus
appears at the age of 9 to 24 months and unites with the fibula shaft
12 to 24 months after tibial physis closure. -
Secondary ossification centers occur and
can be confused with a fracture of either the medial or lateral
malleolus; they are often bilateral.
MECHANISM OF INJURY
-
Direct: Trauma to the ankle from a fall, motor vehicle accident, or pedestrian-motor vehicle accident.
-
Indirect: Axial force transmission
through the forefoot and hindfoot or rotational force of the body on a
planted foot; it may be secondary to a fall or, more commonly, athletic
participation.
CLINICAL EVALUATION
-
Patients with displaced ankle fractures typically present with pain and gross deformity, as well as an inability to ambulate.
-
Physical examination may demonstrate tenderness, swelling, and ecchymosis.
-
Ligamentous instability may be present,
but it is usually difficult to elicit on presentation owing to pain and
swelling from the acute injury. -
Ankle sprains are a diagnosis of
exclusion and should be differentiated from a nondisplaced fracture
based on the location of tenderness. -
Neurovascular examination is essential,
with documentation of dorsalis pedis and posterior tibial pulses,
capillary refill, sensation to light touch and pinprick, and motor
testing. -
Dressings and splints placed in the field
should be removed and soft tissue conditions assessed, with attention
to skin lacerations that may indicate open fracture or fracture
blisters that may compromise wound healing. -
The ipsilateral foot, leg, and knee should be examined for concomitant injury.
P.622
RADIOGRAPHIC EVALUATION
-
Anteroposterior (AP), lateral, and
mortise views of the ankle should be obtained. Tenderness of the
proximal fibula warrants appropriate views of the leg. -
Clinical examination will dictate the possible indication for obtaining views of the knee and foot.
-
Stress views of the ankle may be obtained to determine possible ligamentous instability.
-
The presence of secondary ossification
centers (a medial os subtibiale in 20% of patients or a lateral os
subfibulare in 1% of patients) should not be confused with fracture,
although tenderness may indicate injury. -
A Tillaux fragment represents an osseous fragment from the lateral distal tibia that has been avulsed during injury.
-
Computed tomography (CT) is often helpful
for evaluation of complex intra-articular fractures, such as the
juvenile Tillaux or triplane fracture. -
Magnetic resonance imaging has been used to delineate osteochondral injuries in association with ankle fractures.
CLASSIFICATION
Dias and Tachdjian
-
Lauge-Hansen principles are followed, incorporating the Salter-Harris classification.
-
The typology is simplified by noting the
direction of physeal displacement, Salter-Harris type, and location of
the metaphyseal fragment. -
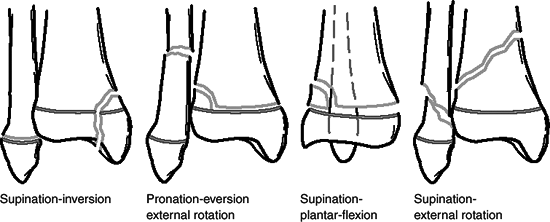
The classification aids in determining the proper maneuver for closed reduction (Fig. 51.1)
Supination–External Rotation (SER)
| Stage I: | Salter-Harris Type II fracture of the distal tibia with the metaphyseal fragment located posterolaterally; the distal fragment is displaced posteriorly, but the Thurston-Holland fragment is seen on the AP x-ray, which differentiates it from a supination–plantar flexion (SPF) injury. |
| Stage II: | As external rotation force continues, a spiral fracture of the fibula occurs beginning medially and extending posterosuperiorly; it differs from an adult SER injury. |
P.623
Pronation–Eversion–External Rotation (PEER)
 |
|
Figure 51.1. Dias-Tachdjian classification of physeal injuries of the distal tibia and fibula.
(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
-
This type comprises 15% to 20% of pediatric ankle fractures.
-
Marked valgus deformity occurs.
-
Tibial and fibular fractures occur simultaneously.
-
Salter-Harris Type II fracture of the
distal tibial physis is most commonly seen, but Type I also occurs; the
metaphyseal fragment is located laterally. -
The short oblique distal fibular fracture occurs 4 to 7 cm proximal to the fibula tip.
Supination–Plantar Flexion (SPF)
-
Most commonly, this is a Salter-Harris
Type II fracture of the distal tibial physis with the metaphyseal
fragment located posteriorly; Type I Salter-Harris fractures are rare. -
Fibula fracture is rare.
Supination–Inversion (SI)
-
This is the most common mechanism of fracture and has the highest incidence of complications.
| Stage I: | Salter-Harris Type I or II fracture of the distal fibular physis is most common because the adduction or supination force avulses the epiphysis; pain is noted along the physis when x-rays are negative. This is the most common pediatric ankle fracture. |
| Stage II: | Salter-Harris Type III or IV fracture of the medial tibial physis occurs as the talus wedges into the medial tibial articular surface; rarely, this is a Type I or II fracture. These are intraarticular fractures that exhibit the highest rate of growth disturbance (i.e., physeal bar formation). |
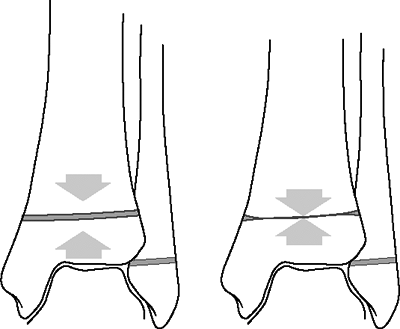
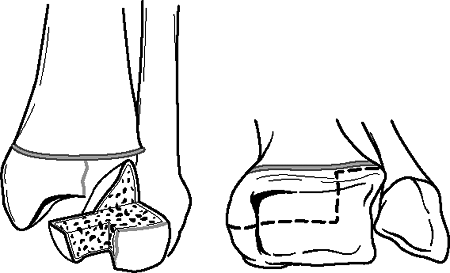
Axial Compression (Fig. 51.2)
-
A Salter-Harris Type V injury to the distal tibia.
-
A rare injury with poor prognosis secondary to physeal growth arrest.
-
Diagnosis is often delayed until premature physeal closure is found with a leg length discrepancy.
P.624
 |
|
Figure 51.2. Compression-type injury of the tibial physis. Early physeal arrest can cause leg length discrepancy.
(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
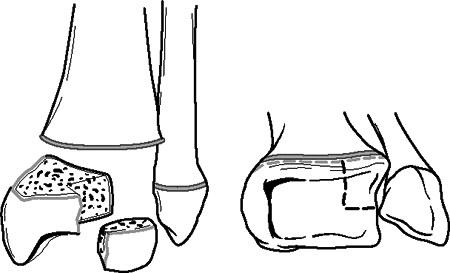
Juvenile Tillaux Fractures (Fig. 51.3)
-
These are Salter-Harris Type III fractures of the anterolateral tibial epiphysis; they occurs in 2.9% of ankle fractures.
-
External rotation force causes the anterior tibiofibular ligament to avulse the fragment.
-
These fractures occur in the 13- to
16-year age group when the central and medial portions of the distal
tibial physis have already fused, and the lateral physis remains open (Fig. 51.4). -
Patients with Tillaux fractures are generally older than those with triplane fractures.
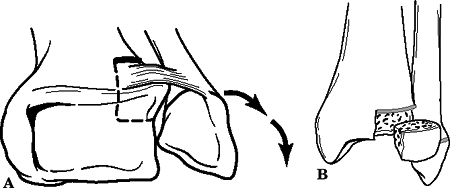 Figure
Figure
51.3. Juvenille Tillaux fracture. Mechanism of injury, the
anteroinferior tibiofibular ligament avulses a fragment of the lateral
epiphysis (A) corresponding to the portion of the physis that is still
open (B).(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
CT scans or tomograms are helpful in distinguishing these injuries from triplane fractures.
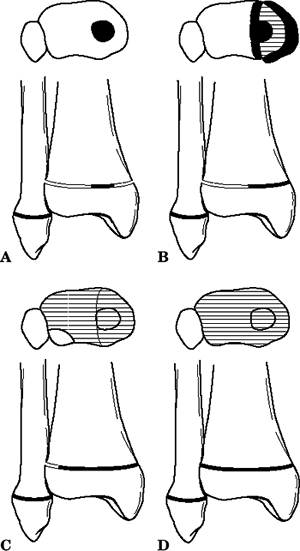
P.625
 |
|
Figure
51.4. Closure of the distal tibial physis begins centrally (A) and extends medially (B) and then laterally (C) before final closure (D). (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
Triplane Fractures
-
Occur in three planes: transverse, coronal, and sagittal.
-
Fractures are explained by fusion of tibial physis from central to anteromedial to posteromedial and finally to lateral.
-
Peak age incidence is 13 to 15 years in boys and 12 to 14 years in girls.
-
Mechanism is thought to be external rotation of the foot and ankle.
-
Fibula fracture is possible; it is usually oblique from anteroinferior to posterosuperior 4 to 6 cm proximal to the fibula tip.
-
CT is valuable in the preoperative assessment.
-
Two- and three-part types have been described (Figs. 51.5 and 51.6):
-
Two-part fractures are either medial, in
which the coronal fragment is posteromedial, or lateral, in which the
coronal fragment is posterolateral.
-
 |
|
Figure
51.5. Anatomy of a two-part lateral triplane fracture (left ankle). Note the large posterolateral epiphyseal fragment with its posterior metaphyseal fragment. The anterior portion of the medial malleolus remains intact. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
TREATMENT
Lateral Malleolar (Distal Fibula) Fracture
Salter-Harris Type I or II
-
Closed reduction and casting with a short leg walking cast for 4 to 6 weeks is recommended.
Salter-Harris Type III or IV
-
Closed reduction and percutaneous pinning with Kirschner wire fixation is followed by placement of a short leg cast.
-
Open reduction may be required for
interposed periosteum, with fixation using an intramedullary Kirschner
wire perpendicular to the physis.
P.627
 |
|
Figure
51.6. Anatomy of a three-part lateral triplane fracture (left ankle). Note the large epiphyseal fragment with its metaphyseal component and the smaller anterolateral epiphyseal fragment. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
Medial Malleolar (Distal Tibia) Fracture
Salter-Harris Type I or II
-
Closed reduction is the treatment of choice; it is usually attainable unless soft tissue interposition prevents reduction.
-
In children <10 years old, some residual angulation is acceptable, because remodeling occurs.
-
Open reduction may be necessary for
interposed periosteum, with placement of a transmetaphyseal compression
screw or Kirschner wire parallel and proximal to the physis. -
A long leg cast for 3 weeks is followed by a short leg walking cast for 3 weeks.
Salter-Harris Type III or IV
-
Anatomic reduction is essential.
-
Intraarticular displacement >2 mm is unacceptable; open reduction and internal fixation is indicated.
-
Open reduction and internal fixation may
be performed through an anteromedial approach with cancellous screw(s)
placed parallel below and/or above the physis. -
Postoperative immobilization consists of short leg casting for 6 weeks.
-
Weekly x-rays should be obtained for the first several weeks to ensure that the intraarticular fragment does not displace.
Juvenile Tillaux Fracture
-
Closed reduction can be attempted by
gentle distraction accompanied by internal rotation of the foot and
direct pressure over the anterolateral tibia; reduction may be
maintained in a short or long leg cast, depending on the rotational
stability. The patient is non–weight bearing for the initial 3 weeks,
followed by a short leg walking cast for an additional 3 weeks. -
Unstable injuries may require percutaneous pinning with Kirschner-wire fixation.
-
Displacement >2 mm is unacceptable and warrants open reduction and internal fixation.
-
Open reduction and internal fixation may be achieved via an anterolateral approach with cancellous screw fixation.
-
CT may be used to assess reduction.
Triplane Fracture
-
Nondisplaced fractures may be treated in
a long leg cast with the knee flexed to 30 degrees for 3 to 4 weeks,
followed by an additional 3 weeks in a short leg walking cast. -
Articular displacement >2 mm warrants
operative fixation, either by closed reduction and percutaneous pinning
or by open reduction and internal fixation using a combination of
cancellous screws or Kirschner wires for fixation. -
CT may be used to assess the adequacy of reduction.
-
Postoperative immobilization consists of
a short or long leg cast (depending on stability of fixation) for 3 to
4 weeks followed by a short leg walking cast for an additional 3 weeks.
P.628
COMPLICATIONS
-
Angular deformity: May occur secondary to
premature physeal arrest, especially after Salter-Harris Type III and
IV injuries. Harris growth lines may be seen at 6 to 12 weeks after
injury as an indication of growth arrest. -
Varus deformity is most common in SI injuries with premature arrest of the medial tibial physis.
-
Valgus deformity is seen with distal fibula physeal arrest; it may result from poor reduction or interposed soft tissue.
-
Rotational deformities may occur with
inadequately reduced triplane fractures; extraarticular rotational
deformities may be addressed with derotational osteotomies, but
intraarticular fractures cannot. -
Leg length discrepancy: Complicates up to
10% to 30% of cases and is dependent on the age of the patient.
Discrepancy of 2 to 5 cm may be treated by epiphysiodesis of the
opposite extremity, although skeletally mature individuals may require
osteotomy. -
Posttraumatic arthritis: may occur as a
result of inadequate reduction of the articular surface in
Salter-Harris Type III and IV fractures.
