Pediatric Foot
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > V – Pediatric Fractures and Dislocations > 52 – Pediatric Foot
52
Pediatric Foot
TALUS
Epidemiology
-
Extremely rare in children (0.01% to 0.08% of all pediatric fractures).
-
Most represent fractures through the talar neck.
Anatomy
-
The ossification center of the talus appears at 8 months in utero (Fig. 52.1).
-
Two thirds of the talus is covered with articular cartilage.
-
The body of the talus is covered
superiorly by the trochlear articular surface through which the body
weight is transmitted. The anterior aspect is wider than the posterior
aspect, which confers intrinsic stability to the ankle. -
Arterial supply to the talus is from two main sources:
-
Artery to the tarsal canal: This arises
from the posterior tibial artery 1 cm proximal to the origin of the
medial and lateral plantar arteries. It gives off a deltoid branch
immediately after its origin that anastomoses with branches from the
dorsalis pedis over the talar neck. -
Artery of the tarsal sinus: This
originates from the anastomotic loop of the perforating peroneal and
lateral tarsal branches of the dorsalis pedis artery.
-
-
An os trigonum is present in up to 50% of
normal feet. It arises from a separate ossification center just
posterior to the lateral tubercle of the posterior talar process.
Mechanism of Injury
-
Forced dorsiflexion of the ankle from
motor vehicle accident or fall represents the most common mechanism of
injury in children. This typically results in a fracture of the talar
neck. -
Isolated fractures of the talar dome and body have been described but are extremely rare.
Clinical Evaluation
-
Patients typically present with pain on weight bearing on the affected extremity.
-
Ankle range of motion is typically painful, especially with dorsiflexion, and may elicit crepitus.
-
Diffuse swelling of the hindfoot may be present, with tenderness to palpation of the talus and subtalar joint.
-
A neurovascular examination should be performed.
Radiographic Evaluation
-
Standard anteroposterior (AP), mortise,
and lateral radiographs of the ankle should be obtained, as well as AP,
lateral, and oblique views of the foot. -
The Canale view provides an optimum view
of the talar neck. With the ankle in maximum equinus, the foot is
placed on a cassette, pronated 15 degrees, and the x-ray tube is
directed cephalad 75 degrees from the horizontal.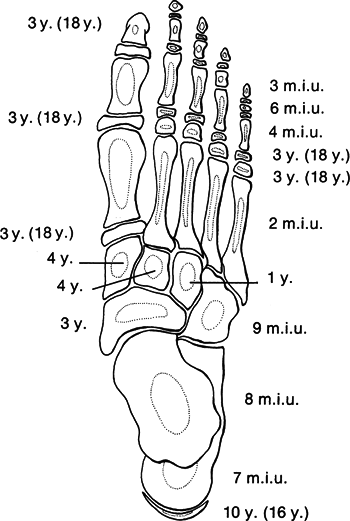 Figure
Figure
52.1. Time of appearance and fusion of ossification centers of the
foot. Figures in parentheses indicate the time of fusion of primary and
secondary ossification centers (y., years; m.i.u, months in utero).(Redrawn from Aitken JT, Joseph J, Causey G, et al. A Manual of Human Anatomy, 2nd ed, vol. IV. London: E & S Livingstone, 1966:80.) -
Computed tomographic scanning may be useful for preoperative planning.
-
Magnetic resonance imaging may be used to
identify occult injuries in children <10 years old owing to limited
ossification at this age.
P.630
Classification
Descriptive
Hawkins Talar Neck Fractures
This classification is for adults, but it is often used for children.
| Type I: | Nondisplaced |
| Type II: | Displaced with associated subtalar subluxation or dislocation |
| Type III: | Displaced with associated subtalar and ankle dislocation |
| Type IV: | Type III with associated talonavicular subluxation or dislocation |
See Chapter 40 for figures.
Treatment
Nonoperative
-
Nondisplaced fractures may be managed in
a long leg cast with the knee flexed 30 degrees to prevent weight
bearing. This is maintained for 6 to 8 weeks with serial radiographs to
assess healing status. The patient may then be advanced to weight
bearing in a short leg walking cast for an additional 2 to 3 weeks.
Operative
-
Indicated for displaced fractures (defined as >5 mm displacement or >5-degree malalignment on the AP radiograph).
-
Minimally displaced fractures can often
be treated successfully with closed reduction with plantar flexion of
the forefoot as well as hindfoot eversion or inversion, depending on
the displacement.-
A long leg cast is placed for 6 to 8
weeks; this may require plantar flexion of the foot to maintain
reduction. If the reduction cannot be maintained by simple positioning,
operative fixation is indicated.
-
-
Displaced fractures are usually amenable
to internal fixation using a posterolateral approach and 4.0 mm
cannulated screws or Kirschner wires placed from a posterior to
anterior direction. In this manner, dissection around the talar neck is
avoided. -
Postoperatively, the patient is maintained in a short leg cast for 6 to 8 weeks, with removal of pins at 3 to 4 weeks.
Complications
-
Osteonecrosis: may occur with disruption
or thrombosis of the tenuous vascular supply to the talus. This is
related to the initial degree of displacement and angulation and,
theoretically, the time until fracture reduction. It tends to occur
within 6 months of injury. -
Hawkins sign represents subchondral
osteopenia in the vascularized, non–weight-bearing talus at 6 to 8
weeks; although this tends to indicate talar viability, the presence of
this sign does not rule out osteonecrosis.
P.632
| Type I fractures: | 0% to 27% incidence of osteonecrosis reported |
| Type II fractures: | 42% incidence |
| Type III, IV fractures: | >90% incidence |
CALCANEUS
Epidemiology
-
A rare injury, typically involving older children (>9 years) and adolescents.
-
Most are extraarticular, involving the apophysis or tuberosity.
-
Of these, 33% are associated with other injuries, including lumbar vertebral and ipsilateral lower extremity injuries.
Anatomy
-
The primary ossification center appears
at 7 months in utero; a secondary ossification center appears at age 10
years and fuses by age 16 years. -
The calcaneal fracture patterns in children differ from that of adults, primarily for three reasons:
-
The lateral process, which is responsible
for calcaneal impaction resulting in joint depression injury in adults,
is diminutive in the immature calcaneus. -
The posterior facet is parallel to the ground, rather than inclined as it is in adults.
-
In children, the calcaneus is composed of a ossific nucleus surrounded by cartilage.
-
These are responsible for the dissipation of the injurious forces that produce classic fracture patterns in adults.
Mechanism of Injury
-
Most calcaneal fractures occur as a
result of a fall or a jump from a height, although typically a
lower-energy injury occurs than seen with adult fractures. -
Open fractures may result from lawnmower injuries.
Clinical Evaluation
-
Patients typically are unable to walk secondary to hindfoot pain.
-
On physical examination, pain, swelling, and tenderness can usually be appreciated at the site of injury.
-
Examination of the ipsilateral lower extremity and lumbar spine is essential, because associated injuries are common.
-
A careful neurovascular examination should be performed.
-
Injury is initially missed in 44% to 55% of cases.
Radiographic Evaluation
-
Dorsoplantar, lateral, axial, and lateral oblique views should be obtained for evaluation of pediatric calcaneal fractures.
-
The Böhler tuber joint angle: This is
represented by the supplement (180 degree measured angle) of two lines:
a line from the highest point of the anterior process of the calcaneus
to the highest point of the posterior articular surface and a line
drawn between the same point on the posterior articular surface and the
most superior point of the tuberosity. Normally, this angle is between
25 and 40 degrees; flattening of this angle indicates collapse of the
posterior facet (Fig. 52.2). -
Comparison views of the contralateral foot may help detect subtle changes in the Böhler angle.
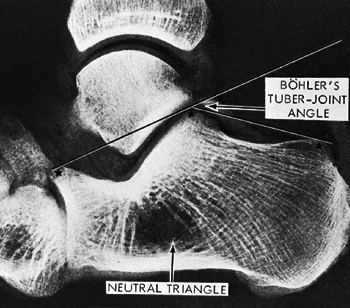
![]() Figure
Figure
52.2. The landmarks for measuring the Böhler angle are the anterior and
posterior facets of the calcaneus and the superior border of the
tuberosity. The neutral triangle, largely occupied by blood vessels,
offers few supporting trabeculae directly beneath the lateral process
of the talus.(From Harty MJ. Anatomic considerations in injuries of the calcaneus. Orthop Clin North Am 1973;4:180.) -
Technetium bone scanning may be utilized when calcaneal fracture is suspected but is not appreciated on standard radiographs.
-
Computed tomography may aid in fracture
definition, particularly in intraarticular fractures in which
preoperative planning may be facilitated by three-dimensional
characterization of fragments.
P.633
Classification
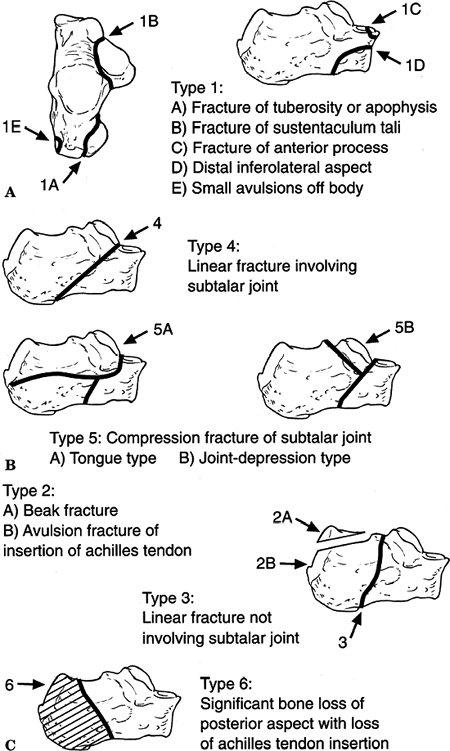
Schmidt and Weiner (Fig. 52.3)
| Type I: | A. Fracture of the tuberosity or apophysis |
| B. Fracture of the sustentaculum | |
| C. Fracture of the anterior process | |
| D. Fracture of the anterior inferolateral process | |
| E. Avulsion fracture of the body | |
| Type II: | Fracture of the posterior and/or superior parts of the tuberosity |
| Type III: | Fracture of the body not involving the subtalar joint |
| Type IV: | Nondisplaced or minimally displaced fracture through the subtalar joint |
| Type V: | Displaced fracture through the subtalar joint |
| A. Tongue type | |
| B. Joint depression type | |
| Type VI: | Either unclassified (Rasmussen and Schantz) or serious soft tissue injury, bone loss, and loss of the insertions of the Achilles tendon |
 |
|
Figure
52.3. Classification used to evaluate calcaneal fracture pattern in children. (A) Extraarticular fractures. (B) Intraarticular fractures. (C) Type VI injury with significant bone loss, soft tissue injury, and loss of insertion of Achilles tendon. (From Schmidt TL, Weiner DS. Calcaneus fractures in children: an evaluation of the nature of injury in 56 children. Clin Orthop 1982;171:150.)
|
P.634
P.635
Treatment
Nonoperative
-
Cast immobilization is recommended for
pediatric patients with extraarticular fractures as well as
nondisplaced (<4 mm) intraarticular fractures of the calcaneus.
Weight bearing is restricted for 6 weeks, although some authors have
suggested that in the case of truly nondisplaced fractures in a very
young child, weight bearing may be permitted with cast immobilization. -
Mild degrees of joint incongruity tend to
remodel well, although severe joint depression is an indication for
operative management.
Operative
-
Operative treatment is indicated for displaced articular fractures, particularly in older children and adolescents.
-
Displaced fractures of the anterior
process of the calcaneus represent relative indications for open
reduction and internal fixation, because up to 30% may result in
nonunion. -
Anatomic reconstitution of the articular surface is imperative, with lag screw technique for operative fixation.
Complications
-
Posttraumatic osteoarthritis: This may be
secondary to residual or unrecognized articular incongruity. Although
younger children remodel very well, this emphasizes the need for
anatomic reduction and reconstruction of the articular surface in older
children and adolescents. -
Heel widening: This is not as significant
a problem in children as it is in adults because the mechanisms of
injury tend not to be as high energy (i.e., falls from lower heights
with less explosive impact to the calcaneus) and remodeling can
partially restore architectural integrity. -
Nonunion: This rare complication most
commonly involves displaced anterior process fractures treated
nonoperatively with cast immobilization. This is likely caused by the
attachment of the bifurcate ligament that tends to produce a displacing
force on the anterior fragment with motions of plantar flexion and
inversion of the foot. -
Compartment syndrome: Up to 10% of
patients with calcaneal fractures have elevated hydrostatic pressure in
the foot; half of these patients (5%) will develop claw toes if
surgical compartment release is not performed.
TARSOMETATARSAL (LISFRANC) INJURIES
Epidemiology
-
Extremely uncommon in children.
-
They tend to occur in older children and adolescents (>10 years of age).
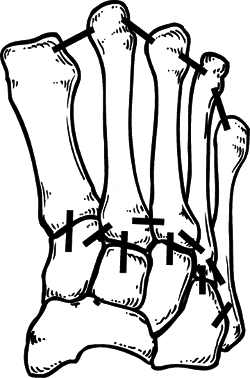
Anatomy (Fig. 52.4)
-
The base of the second metatarsal is the “keystone” of an arch that is interconnected by tough, plantar ligaments.
-
The plantar ligaments tend to be much stronger than the dorsal ligamentous complex.
![]() Figure
Figure
52.4. The ligamentous attachments at the tarsometatarsal joints. There
is only a flimsy connection between the bases of the first and second
metatarsals (not illustrated). The second metatarsal is recessed and
firmly anchored.(From Wiley JJ. The mechanism of tarsometatarsal joint injuries. J Bone Joint Surg Br 1971;53:474.) -
The ligamentous connection between the
first and second metatarsal bases is weak relative to those between the
second through fifth metatarsal bases. -
Lisfranc ligament attaches the base of the second metatarsal to the medial cuneiform.
P.636
Mechanism of Injury
-
Direct: Secondary to a heavy object
impacting the dorsum of the foot, causing plantar displacement of the
metatarsals with compromise of the intermetatarsal ligaments. -
Indirect: More common and results from violent abduction, forced plantar flexion, or twisting of the forefoot.
-
Abduction tends to fracture the recessed
base of the second metatarsal, with lateral displacement of the
forefoot variably causing a “nutcracker” fracture of the cuboid. -
Plantar flexion is often accompanied by fractures of the metatarsal shafts, as axial load is transmitted proximally.
-
Twisting may result in purely ligamentous injuries.
-
Clinical Evaluation
-
Patients typically present with swelling over the dorsum of the foot with either an inability to ambulate or painful ambulation.
-
Deformity is variable, because spontaneous reduction of the ligamentous injury is common.
-
Tenderness over the tarsometatarsal joint
can usually be elicited; this may be exacerbated by maneuvers that
stress the tarsometatarsal articulation. -
Of these injuries, 20% are missed initially
Radiographic Evaluation
-
AP, lateral, and oblique views of the foot should be obtained.
-
AP radiographP.637
-
The medial border of the second metatarsal should be colinear with the medial border of the middle cuneiform.
-
A fracture of the base of the second
metatarsal should alert the examiner to the likelihood of a
tarsometatarsal dislocation, because often the dislocation will have
spontaneously reduced. One may only see a “fleck sign,” indicating an
avulsion of the Lisfranc ligament. -
The combination of a fracture at the base
of the second metatarsal with a cuboid fracture indicates severe
ligamentous injury, with dislocation of the tarsometatarsal joint. -
More than 2 to 3 mm of diastasis between the first and second metatarsal bases indicates ligamentous compromise.
-
-
Lateral radiograph
-
Dorsal displacement of the metatarsals indicates ligamentous compromise.
-
Plantar displacement of the medial
cuneiform relative to the fifth metatarsal on a weight-bearing lateral
view may indicate subtle ligamentous injury.
-
-
Oblique radiograph
-
The medial border of the fourth metatarsal should be colinear with the medial border of the cuboid.
-
Classification
Treatment
Nonoperative
-
Minimally displaced tarsometatarsal
dislocations (<2 to 3 mm) may be managed with elevation and a
compressive dressing until swelling subsides. This is followed by short
leg casting for 5 to 6 weeks until symptomatic improvement. The patient
may then be placed in a hard-soled shoe or cast boot until ambulation
is tolerated well. -
Displaced dislocations often respond well to closed reduction using general anesthesia.
-
This is typically accomplished with patient supine, finger traps on the toes, and 10 lb of traction.
-
If the reduction is determined to be
stable, a short leg cast is placed for 4 to 6 weeks, followed by a
hard-soled shoe or cast boot until ambulation is well tolerated.
-
Operative
-
Surgical management is indicated with displaced dislocations when reduction cannot be achieved or maintained.
-
Closed reduction may be attempted as
described earlier, with placement of percutaneous Kirschner wires to
maintain the reduction. -
In the rare case when closed reduction
cannot be obtained, open reduction using a dorsal incision may be
performed. Kirschner wires are utilized to maintain reduction; these
are typically left protruding through the skin to facilitate removal.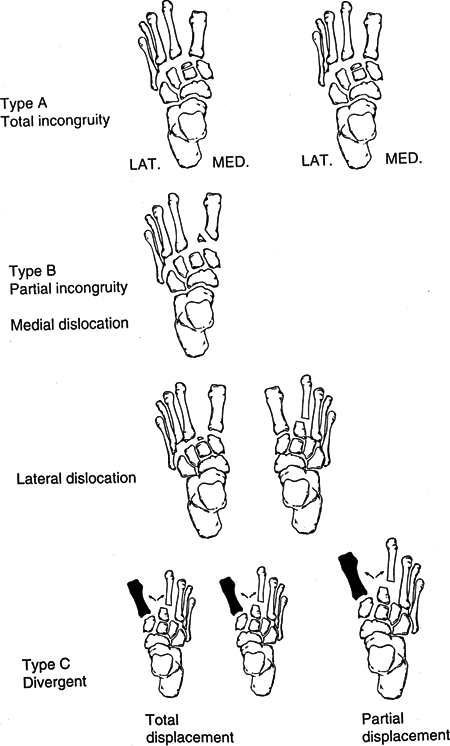 Figure 52.5. Quenu and Kuss classification of tarsometatarsal injuries.(From Hardcastle
Figure 52.5. Quenu and Kuss classification of tarsometatarsal injuries.(From Hardcastle
PH, Reschauer R, Kitscha-Lissberg E, et al. Injuries to the
tarsometatarsal joint: incidence, classification and treatment. J Bone Joint Surg Br 1982;64B:349.) -
A short leg cast is placed
postoperatively; this is maintained for 4 weeks, at which time the
wires and cast may be discontinued and the patient placed in a
hard-soled shoe or cast boot until ambulation is well tolerated.
P.638
P.639
Complications
-
Persistent pain: May result from
unrecognized or untreated injuries to the tarsometatarsal joint caused
by ligamentous compromise and residual instability. -
Angular deformity: May result despite
treatment and emphasizes the need for reduction and immobilization by
surgical intervention if indicated.
METATARSALS
Epidemiology
-
Very common injury in children and accounts for up to 60% of pediatric foot fractures.
-
The metatarsals are involved in only 2%
of stress fractures in children; in adults, the metatarsals are
involved in 14% of stress fractures.
Anatomy
-
Ossification of the metatarsals is apparent by 2 months in utero.
-
The metatarsals are interconnected by tough intermetatarsal ligaments at their bases.
-
The configuration of the metatarsals in
coronal section forms an arch, with the second metatarsal representing
the “keystone” of the arch. -
Fractures through the metatarsal neck most frequently result from their relatively small diameter.
-
Fractures at the base of the fifth
metatarsal must be differentiated from an apophyseal growth center or
an os vesalianum, a sesamoid proximal to the insertion of the peroneus
brevis. The apophysis is not present before age 8 years and usually
unites to the shaft by 12 years in girls and 15 years in boys.
Mechanism of Injury
-
Direct: Trauma to the dorsum of the foot, mainly from heavy falling objects.
-
Indirect: More common and results from
axial loading with force transmission through the plantar flexed ankle
or by torsional forces as the forefoot is twisted. -
Avulsion at the base of the fifth
metatarsal may result from tension at the insertion of the peroneus
brevis muscle, the tendinous portion of the abductor digiti minimi, or
the insertion of the strong lateral cord of the plantar aponeurosis. -
“Bunk-bed fracture”: This fracture of the
proximal first metatarsal is caused by jumping from a bunk bed landing
on the plantar flexed foot. -
Stress fractures may occur with repetitive loading, such as long-distance running.
P.640
Clinical Evaluation
-
Patients typically present with swelling, pain, and ecchymosis, and they may be unable to ambulate on the affected foot.
-
Minimally displaced fractures may present with minimal swelling and tenderness to palpation.
-
A careful neurovascular examination should be performed.
-
The presence of compartment syndrome of
the foot should be ruled out in cases of dramatic swelling, pain,
venous congestion in the toes, or history of a crush mechanism of
injury. The interossei and short plantar muscles are contained in
closed fascial compartments.
Radiographic Evaluation
-
AP, lateral, and oblique views of the foot should be obtained.
-
Bone scans may be useful in identifying
occult fractures in the appropriate clinical setting or stress
fractures with apparently negative plain radiographs. -
With conventional radiographs of the
foot, exposure sufficient for penetration of the tarsal bones typically
results in overpenetration of the metatarsal bones and phalanges;
therefore, when injuries to the forefoot are suspected, optimal
exposure of this region may require underpenetration of the hindfoot.
Classification
Descriptive
-
Location: metatarsal number, proximal, midshaft, distal
-
Pattern: spiral, transverse, oblique
-
Angulation
-
Displacement
-
Comminution
-
Articular involvement
Treatment
Nonoperative
-
Most fractures of the metatarsals may be
treated initially with splinting, followed by a short-leg walking cast
once swelling subsides. If severe swelling is present, the ankle should
be splinted in slight equinus to minimize neurovascular compromise at
the ankle. Care must be taken to ensure that circumferential dressings
are not constrictive at the ankle, causing further congestion and
possible neurovascular compromise. -
Alternatively, in cases of truly
nondisplaced fractures with no or minimal swelling, a cast may be
placed initially. This is typically maintained for 3 to 6 weeks until
radiographic evidence of union. -
Fractures at the base of the fifth
metatarsal may be treated with a short-leg walking cast for 3 to 6
weeks until radiographic evidence of union. Fractures occurring at the
metaphyseal-diaphyseal junction have lower rates of healing and should
be treated with a non–weight-bearing short leg cast for 6 weeks; open
reduction and intramedullary screw fixation may be considered,
especially if a history of pain was present for
P.641
3 months or more before injury, which indicates a chronic stress injury. -
Stress fractures of the metatarsal shaft
may be treated with a short leg walking cast for 2 weeks, at which time
it may be discontinued if tenderness has subsided and walking is
painless. Pain from excessive metatarsophalangeal motion may be
minimized by the use of a metatarsal bar placed on the sole of the shoe.
Operative
-
If a compartment syndrome is identified, release of all nine fascial compartments of the foot should be performed.
-
Unstable fractures may require
percutaneous pinning with Kirschner wires for fixation, particularly
with fractures of the first and fifth metatarsals. Considerable lateral
displacement and dorsal angulation may be accepted in younger patients,
because remodeling will occur. -
Open reduction and pinning are indicated
when reduction cannot be achieved or maintained. The standard technique
includes dorsal exposure, Kirschner wire placement in the distal
fragment, fracture reduction, and intramedullary introduction of the
wire in a retrograde fashion to achieve fracture fixation. -
Postoperatively, the patient should be
placed in a short leg, non–weight-bearing cast for 3 weeks, at which
time the pins are removed and the patient is changed to a walking cast
for an additional 2 to 4 weeks.
Complications
-
Malunion: This typically does not result
in functional disability because remodeling may achieve partial
correction. Severe malunion resulting in disability may be treated with
osteotomy and pinning. -
Compartment syndrome: This uncommon but
devastating complication may result in fibrosis of the interossei and
an intrinsic minus foot with claw toes. Clinical suspicion must be high
in the appropriate clinical setting; workup should be aggressive and
treatment expedient, because the compartments of the foot are small in
volume and are bounded by tight fascial structures.
PHALANGES
Epidemiology
-
Uncommon; the true incidence is unknown because of underreporting.
Anatomy
-
Ossification of the phalanges ranges from
3 months in utero for the distal phalanges of the lesser toes, 4 months
in utero for the proximal phalanges, 6 months in utero for the middle
phalanges, and up to age 3 years for the secondary ossification centers.
P.642
Mechanism of Injury
-
Direct trauma accounts for nearly all
these injuries, with force transmission typically on the dorsal aspect
from heavy falling objects or axially when an unyielding structure is
kicked. -
Indirect mechanisms are uncommon, with rotational forces from twisting responsible for most.
Clinical Evaluation
-
Patients typically present ambulatory but guarding the affected forefoot.
-
Ecchymosis, swelling, and tenderness to palpation may be appreciated.
-
A neurovascular examination is important,
with documentation of digital sensation on the medial and lateral
aspects of the toe as well as an assessment of capillary refill. -
The entire toe should be exposed and examined for open fracture or puncture wounds.
Radiographic Evaluation
-
AP, lateral, and oblique films of the foot should be obtained.
-
The diagnosis is usually made on the AP
or oblique films; lateral radiographs of lesser toe phalanges are
usually of limited value. -
Contralateral views may be obtained for comparison.
Classification
Descriptive
-
Location: toe number, proximal, middle, distal
-
Pattern: spiral, transverse, oblique
-
Angulation
-
Displacement
-
Comminution
-
Articular involvement
Treatment
Nonoperative
-
Nonoperative treatment is indicated for
almost all pediatric phalangeal fractures unless there is severe
articular incongruity or an unstable, displaced fracture of the first
proximal phalanx. -
Reduction maneuvers are rarely necessary; severe angulation or displacement may be addressed by simple longitudinal traction.
-
External immobilization typically
consists of simple buddy taping with gauze between the toes to prevent
maceration; a rigid-soled orthosis may provide additional comfort in
limiting forefoot motion. This is maintained until the patient is pain
free, typically between 2 and 4 weeks (Fig. 52.6). -
Kicking and running sports should be limited for an additional 2 to 3 weeks.
P.643
Operative
 |
|
Figure
52.6. Method of taping to adjacent toe(s) for fractures or dislocations of the phalanges. Gauze is placed between the toes to prevent maceration. The nailbeds are exposed to ascertain that the injured toe is not malrotated. (From Weber BG, Brunner C, Freuler F. Treatments of Fractures in Children and Adolescents. New York: Springer-Verlag, 1980:392.)
|
-
Surgical management is indicated when
fracture reduction cannot be achieved or maintained, particularly for
displaced or angulated fractures of the first proximal phalanx. -
Relative indications include rotational
displacement that cannot be corrected by closed means and severe
angular deformities that, if uncorrected, would lead to cock-up toe
deformities or an abducted fifth toe. -
Fracture reduction is maintained via retrograde, intramedullary Kirschner wire fixation.
-
Nailbed injuries should be repaired. Open
reduction may be necessary to remove interposed soft tissue or to
achieve adequate articular congruity. -
Postoperative immobilization consists of a rigid-soled orthosis or splint. Kirschner wires are typically removed at 3 weeks.
Complications
-
Malunion uncommonly results in functional
significance, usually a consequence of fractures of the first proximal
phalanx that may lead to varus or valgus deformity. Cock-up toe
deformities and fifth toe abduction may cause cosmetically undesirable
results as well as poor shoe fitting or irritation.