Extensor Tendon Laceration
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Extensor Tendon Laceration
Extensor Tendon Laceration
John J. Carbone MD
Dawn M. LaPorte MD
Description
-
Extensor tendon lacerations are common because of the superficial location of the extensor tendons on the back of the hand (1).
-
Tendon disruption often is indicated by a change in the posture of the hand or fingers.
-
The most distal injury, at the DIP joint, shows a mallet-type of deformity.
-
An injury over the PIP joint may result in a boutonniere deformity.
-
Extensor injuries usually are repaired
surgically, either in the emergency department or in the operating room
within 2 weeks of injury. -
These injuries, most common in young adults, affect active finger extension and wrist extension.
-
Males are affected more commonly than are females.
-
Classification: Partial or complete laceration, as noted during wound exploration
Epidemiology
Incidence
This laceration is less common than flexor tendon injuries.
Etiology
-
Laceration on dorsum of hand or wrist, coupled with the superficial location of the extensor mechanism
-
Possible association with bite injuries
Associated Conditions
Open fractures and joints
Signs and Symptoms
-
Laceration on the dorsum of the hand:
-
Tendon ends frequently visible in wound with minimal exploration
-
Change in posture of finger or hand
-
Inability to extend actively the joints distal to the injury
-
-
Mallet deformity:
-
Inability to extend the distal joint of the finger (The finger droops downward.)
-
-
Boutonniere deformity:
-
The PIP joint goes into flexion, whereas the DIP joint extends or hyperextends.
-
-
Decrease in extension strength or ROM of
the index or the small finger, both of which have small secondary
independent extensor muscle and tendon units
Physical Exam
-
Examine all fingers for active extension and the wrist for strength and ROM.
-
Carefully explore the wound for evidence of tendon lacerations (partial or complete).
Tests
Lab
If operative treatment is necessary, standard preoperative tests are performed, depending on the health of the patient.
Imaging
AP and lateral radiographs are obtained to rule out foreign body or fracture.
Differential Diagnosis
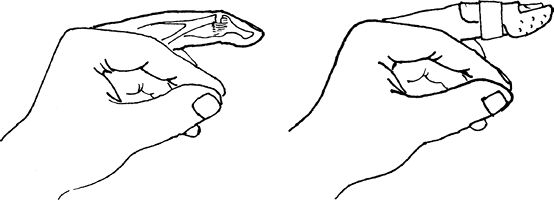
Fracture or avulsion injury of extensor mechanism (Fig. 1)
 |
|
Fig. 1. An extensor tendon laceration or avulsion over the DIP joint will heal with a finger splint.
|
General Measures
-
Tetanus booster or toxoid as needed
-
Intravenous antibiotics, typically a 3rd-generation cephalosporin, if the wound is contaminated
-
Skin closure until definitive surgery is performed
-
Hand splinted in wrist or finger extension (Fig. 1)
-
Wound irrigation and débridement as needed
-
Orthopaedic surgery or hand surgery consult
Special Therapy
Physical Therapy
-
Physical therapy regimens are based on injury type and location and on the type of repair.
-
The goal is to achieve a repair that allows early passive and active ROM.
Surgery
-
The tendon ends are isolated,
approximated, and repaired with 4-0 Prolene or 4-0 Ticron
(Sherwood-Davis & Geck, St. Louis, MO).-
Mattress sutures are used.
-
If the injury is at the level of the wrist, then the repair usually is performed in the operating room.
-
The repair is less surgically demanding
than a repair of a flexor tendon lacerated at the same level because no
tendon pulley is present around extensor tendons. -
This anatomy also allows delayed surgical repair for up to 2 weeks without any adverse effects on outcome.
-
Postoperative splinting is necessary while the tendon heals.
-
P.123
Prognosis
Good with complete surgical repair
Complications
-
Infection
-
Open joint injuries
-
Failure of tendon repair/tendon rupture
-
Scarring
-
Adhesions
-
Loss of function
References
1. Newport ML. Extensor tendon Injuries in the hand. J Am Acad Orthop Surg 1997;5:59–66.
Additional Reading
American Society for Surgery of the Hand. The Hand: Primary Care of Common Problems, 2nd ed. New York: Churchill Livingstone, 1990.
Ariyan S. The Hand Book. New York: McGraw-Hill, 1989.
Baratz ME, Schmidt CC, Hughes TB. Extensor tendon injuries. In: Green DP, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005:187–217.
Codes
ICD9-CM
884.2 Tendon laceration with open wound, upper extremity
Patient Teaching
-
Patient compliance with splinting, wound care, and physical therapy is critical to good functional outcome.
-
It is important to stress the fact that,
with a complete laceration, the tendon will not heal or repair itself
for normal function.
FAQ
Q: What should be done for a patient with an extensor tendon laceration if the surgeon is not available?
A:
The wound should be washed out and, if clean, the skin should be
reapproximated and the joint splinted in full extension. The patient
should be seen promptly in follow-up with a surgeon for operative
exploration and repair within 7–10 days.
The wound should be washed out and, if clean, the skin should be
reapproximated and the joint splinted in full extension. The patient
should be seen promptly in follow-up with a surgeon for operative
exploration and repair within 7–10 days.
Q: What is the most common complication after extensor tendon repair?
A:
The most common complication is formation of adhesions between the
repair site and adjacent tissue, which can restrict joint motion.
Therapy helps to minimize adhesion formation and to improve tendon
gliding, but occasionally surgical tenolysis is necessary.
The most common complication is formation of adhesions between the
repair site and adjacent tissue, which can restrict joint motion.
Therapy helps to minimize adhesion formation and to improve tendon
gliding, but occasionally surgical tenolysis is necessary.
