The Hypoglossal Nerve
XII) is a purely motor nerve, supplying the tongue. Its cells of origin
are in the hypoglossal nuclei. The paired nuclei extend almost the
entire length of the medulla just beneath the floor of the fourth
ventricle, close to the midline, under the medial aspect of the
hypoglossal trigone. The nerve emerges from the medulla in the sulcus
between the pyramid and inferior olive as a series of 10 to 15 rootlets
on each side, anterior to the rootlets of CNs IX, X, and XI.
the neck to the level of the angle of the mandible, then passes forward
under the tongue to supply its extrinsic and intrinsic muscles. In the
upper portion of its course, the nerve lies beneath the internal
carotid artery and internal jugular vein, and near the vagus nerve. It
passes between the artery and vein, runs forward above the hyoid bone,
and breaks up into a number of fibers to supply the various tongue
muscles. At the base of the tongue it lies near the lingual branch of
the mandibular nerve.
the lower portion of the precentral gyrus near and within the sylvian
fissure. The supranuclear fibers run in the corticobulbar tract through
the genu of the internal capsule and through the cerebral peduncle.
Supranuclear control to the genioglossus muscle is primarily crossed;
supply to the other muscles is bilateral but predominantly crossed.
consists of evaluating the strength, bulk, and dexterity of the
tongue—looking especially for weakness, atrophy, abnormal movements
(particularly fasciculations), and impairment of rapid movements. After
noting the position and appearance of the tongue at rest in the mouth,
the patient is asked to protrude it, move it in and out, from side to
side, and upward and downward, both slowly and rapidly. Motor power can
be tested by having the patient press the tip against each cheek as the
examiner tries to dislodge it with finger pressure. The normal tongue
is powerful and cannot be moved. For more precise testing, press firmly
with a tongue blade against the side of the protruded tongue, comparing
the strength on the two sides.
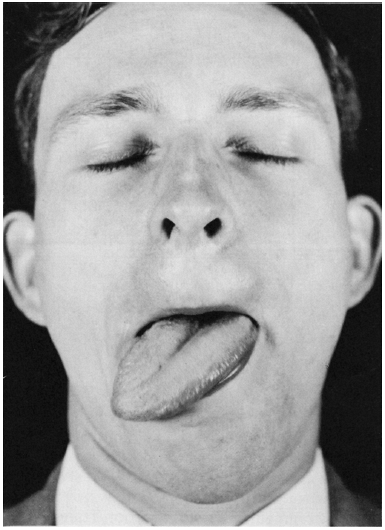
toward the weak side on protrusion because of the action of the normal
genioglossus, which protrudes the tip of the tongue by drawing the root
forward (Figure 16.1). Because the tip of the
tongue is pushed out of the mouth it deviates toward the weak side.
There is impairment of the ability to deviate the protruded tongue
toward the nonparetic side and of the ability to push the tongue
against the cheek on the normal side, but the patient is able to push
it against the cheek on the weak side. Lateral movements of the tip of
the nonprotruded tongue, controlled by the intrinsic tongue muscles,
may be preserved.
Because
of the extensive interlacing of muscle fibers from side to side, the
functional deficit with unilateral tongue weakness may be minimal.
There may be difficulty manipulating food in the mouth, and an
inability to remove food from between the teeth and the cheeks on
either side. With either weakness or incoordination, rapid tongue
movements may be impaired. In bilateral paralysis, the patient may be
able to protrude the tongue only slightly, or not at all.
 |
|
FIGURE 16.1
• Infranuclear paralysis of muscles supplied by the hypoglossal nerve: Unilateral atrophy and deviation of the tongue following a lesion of the right hypoglossal nerve. |
difficult to evaluate deviation of the tongue. Patients with
significant lower facial weakness often have distortion of the normal
facial appearance that can produce the appearance of tongue deviation
when none is present (Figure 11.1). Protruding
the tongue may cause an appearance of deviation toward the side of the
facial weakness. Because of the lack of facial mobility the corner of
the mouth does not move out of the way and the protruded tongue lies
tight against it, making it look as though the tongue has deviated.
Manually pulling up the weak side of the face eliminates the
“deviation.” It may also be helpful to gauge tongue position in
relation to the tip of the nose or the notch between the upper incisors.
With advanced atrophy, the tongue is wrinkled, furrowed, and obviously
smaller. The epithelium and mucous membrane on the affected side are
thrown into folds. As the paralyzed side becomes wasted, the protruded
tongue may curve strikingly toward the atrophic side, assuming a sickle
shape.
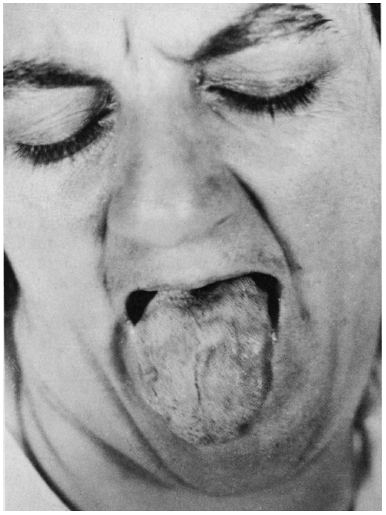
lateral sclerosis, the atrophy may be so severe that the tongue cannot
be protruded; it lies inert on the floor of the mouth (glossoplegia).
Atrophy may be accompanied by fasciculations, especially in motor
neuron disease. In some patients, the tongue is tremulous and it may be
difficult to distinguish these fine, rapid tremors from fasciculations,
especially when the tongue is protruded. Tremors will usually disappear
when the tongue is lying at rest in the mouth, whereas fasciculations
persist.
of the tongue sometimes occur. Tremors are usually accentuated by
protrusion of the tongue or by talking. Coarse tremors of the
tongue
can occur in parkinsonism; a fine tremor can occur in thyrotoxicosis.
Chorea may cause irregular, jerky movements of the tongue, and often
the patient is unable to keep the tongue protruded (snake tongue,
trombone tongue). Abnormal involuntary movements may involve the
tongue. It is often prominently involved in orofacial or buccolingual
dyskinesias, which usually occur as a type of tardive dyskinesia
following the use of psychotropic drugs. Similar dyskinesias may also
occur in patients with Parkinson disease related to the use of levodopa
and dopamine agonists, and in Meige syndrome. Seizures may involve the
tongue, either as part of a Jacksonian seizure or rarely in isolation.
 |
|
FIGURE 16.2
• Nuclear paralysis of muscles supplied by the hypoglossal nerve. Atrophy and fasciculations of the tongue in a patient with amyotrophic lateral sclerosis. |
significance in many medical conditions. Macroglossia occurs in
hypothyroidism, Down syndrome, amyloidosis, acromegaly, and rarely in
some myopathies. The term atrophic glossitis refers to atrophy of the
epithelium and papillae, causing a smooth, glistening, often reddened
tongue. There may be punctate, erythematous lesions from atrophic,
hyperemic papillae. Atrophic glossitis occurs in certain deficiency
states, especially vitamin B12, folate, other B vitamins, and iron. In
pernicious anemia, the tongue is smooth, slick, and translucent. In
some stages the tongue is pale; in others, it is red. In pellagra and
niacin deficiency, the tongue is smooth and atrophic; acutely it is
scarlet red and swollen and may have ulcerations. In riboflavin
deficiency, the tongue may be a purplish or magenta hue, with
prominent, edematous fungiform and filiform papillae that resemble
cobblestones. Fusion and atrophy of the papillae and fissuring may
cause a geographic, or scrotal, tongue. Burning tongue (glossodynia,
glossalgia) with no visible lesions may occur from early glossitis,
tobacco abuse, heavy metal intoxication, as a menopausal symptom, and
in pellagra. Xerostomia and local irradiation may cause the tongue to
be dry and sore. Melkersson-Rosenthal syndrome causes facial nerve
palsy and scrotal tongue. Longitudinal lingual fissuring occurs in
syphilitic glossitis. Ulcerations of the tongue may be seen in primary
syphilis (lingual chancre) and in Behçet disease. Three parallel
longitudinal fissures of the tongue is characteristic of myasthenia
gravis (trident or triple furrowed tongue). The tongue is often bitten
during generalized tonic clonic seizures.
weakness of the tongue. There are no sensory changes. Unilateral
weakness may cause few symptoms; speech and swallowing are little
affected. With severe bilateral weakness the tongue cannot be protruded
or moved laterally; the first stage of swallowing is impaired, and
there is difficulty with articulation, especially in pronouncing
linguals. Rarely, the tongue tending to slip back into the throat may
cause respiratory difficulty.
or infranuclear lesion. Supranuclear lesions cause weakness but no
atrophy, and the weakness is rarely severe. Since the genioglossus—the
principal protractor of the tongue—has mainly crossed supranuclear
innervation, the tongue protrudes toward the weak side, but to the side
opposite the supranuclear lesion. Supranuclear tongue weakness may
occur with a destructive lesion of the cerebral cortex or the
corticobulbar tract in the internal capsule, cerebral peduncle, or
pons. Pontine lesions may cause supranuclear tongue weakness depending
on the relationship to the decussating corticolingual fibers.
Supranuclear lesions may cause dysarthria due to tongue weakness and
incoordination. Pseudobulbar palsy due to bilateral upper motor neuron
disease may cause bilateral tongue weakness. Patients with hemispheric
lesions may have apraxia of tongue movements, and are often unable to
protrude it on command. Extrapyramidal disorders may cause slowing of
tongue movements, with thickness of speech and difficulty in protrusion.
lesions cause atrophy of the involved side. The tongue protrudes toward
the weak side, which is also the side of the lesion. Progressive
nuclear lesions, such as motor neuron disease, often cause
fasciculations in addition to weakness. Common disorders that may
involve the hypoglossal nucleus include neoplasms, vascular lesions,
and motor neuron disease. Nuclear lesions may be accompanied by
involvement of contiguous structures, such as the ascending sensory or
descending motor pathways.
fibers between the nucleus and the point of exit. Except for motor
neuron disease and similar conditions, causes are generally the same as
for nuclear lesions. Processes involving the extramedullary,
intracranial course of the nerve include disorders involving the
meninges, such as infectious and neoplastic meningitis, subarachnoid
hemorrhage, neoplasms and other mass lesions (e.g., schwannoma),
inflammation, and trauma. Processes involving the skull base—such as
basal skull fractures, basilar impression, and platybasia—may affect
the nerve before it leaves the skull. Lesions along the clivus may
cause bilateral hypoglossal palsies. Processes involving the
extracranial course of the nerve include trauma of various types,
especially penetrating wounds (including surgery on the neck, mouth, or
tongue), carotid aneurysms (especially dissections), tumors or
infections in the retroparotid or retropharyngeal spaces, deep cervical
adenopathy, cranial irradiation, and tumors involving the neck, tongue
base, or salivary glands. Hypoglossal nerve palsy can also occur as an
idiopathic, benign syndrome that resolves spontaneously. Mechanical
lesions may result in aberrant regeneration, which causes progressive
difficulty with coordinated tongue movements. Rarely, primary neural
tumors involve CN XII extracranially. CN XII may be involved with other
lower cranial nerves and the cervical sympathetics in lesions in the
retroparotid space. Cranial nerve XII may be involved unilaterally or
bilaterally in Guillain-Barré syndrome and related polyneuropathies.
disorders and myopathies rarely involve the tongue to any clinically
significant degree. Tongue weakness and fatigability may occur in
myasthenia gravis but generally only with severe involvement.
although it rarely causes any symptoms. One way to test for myotonia is
to place the edge of a tongue blade across the tongue, then percuss it
sharply. Myotonia may cause a temporary focal contraction along the
line of percussion, causing the tongue to narrow sharply at that point.
The appearance of the resulting constriction has been referred to as
the napkin ring sign.
