Pediatric Knee
-
The knee is a ginglymoid (hinge) joint consisting of three articulations: patellofemoral, tibiofemoral, and tibiofibular.
-
Under normal cyclic loading, the knee may experience up to five times body weight per step.
-
The normal range of motion is from 10
degrees of extension to 140 degrees of flexion, with 8 to 12 degrees of
rotation through the flexion/extension arc. -
The dynamic and static stability of the
knee is conferred mainly by soft tissues (ligaments, muscles, tendons,
menisci) in addition to the bony articulations. -
Because ligaments in the immature
skeleton are more resistant to tensile stresses than are physeal
plates, trauma leads to physeal separation and avulsions not seen in
the skeletally mature patient. -
There are three physeal plates with secondary ossification centers.
-
Appearance of ossification centers is as follows:
-
Distal femur: thirty-ninth fetal week
-
Proximal tibia: by 2 months
-
Tibial tubercle: 9 years
-
-
Physeal closure is as follows:
-
Distal femur: 16 to 19 years
-
Proximal tibia: 16 to 19 years
-
Tibial tubercle: 15 to 17 years
-
-
The patella is a sesamoid bone, with its own ossification center, which appears at age 3 to 5 years.
-
Tibial spine: This is the site of insertion of the anterior cruciate ligament (ACL).
-
Two-thirds of longitudinal growth of the
lower extremity is provided by the distal femoral (9 mm/year) and
proximal tibial (6 mm/year) physes.
-
The most commonly injured physis around the knee.
-
These comprise 1% to 6% of all physeal injuries and less than 1% of all fractures in children.
-
Most (two-thirds) are Salter-Harris Type II fractures and occur in adolescents.
-
The distal femoral epiphysis is the largest and fastest growing physis in the body.
-
There is no inherent protection of the physis; ligamentous and tendinous structures insert on the epiphysis.
-
The sciatic nerve divides at the level of the distal femur.
-
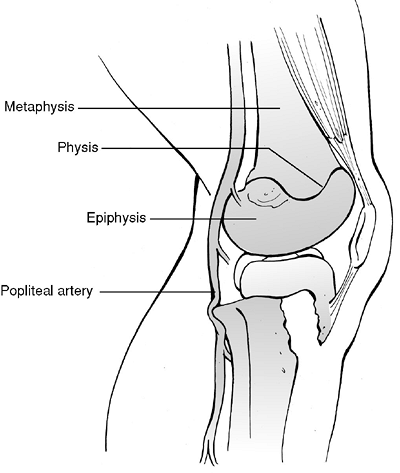
The popliteal artery gives off the superior geniculate branches to the knee just posterior to the femoral metaphysis.
-
Direct trauma to the distal femur:
Uncommon, but it may occur from vehicular trauma, falling onto a flexed
knee, or during athletic activity, such as a lateral blow to the knee
with a planted, cleated foot in football. In infants, this injury must
be suspected to be the result of child abuse. -
Indirect injury: Varus/valgus or
hyperextension/hyperflexion; it usually results in simultaneous
compression to one aspect of the physis with distraction to the other,
with the epiphysis separating from the metaphysis owing to tension.
Most typically, the physeal separation begins on the tension side and
exits the metaphysis on the compression side (Salter-Harris Type II). -
Birth injury secondary to breech presentation or arthrogryposis may cause this injury.
-
Minimal trauma in conditions that cause
generalized weakening of the growth plate (osteomyelitis, leukemia,
myelodysplasia) may also be causative.
-
Patients are typically unable to bear
weight on the injured lower extremity, although patients with a
nondisplaced physeal injury from a low-energy mechanism (e.g., athletic
injury) may ambulate with an antalgic gait. -
Older children and adolescents may relate
a history of hearing or feeling a “pop;” along with associated knee
effusion and soft tissue swelling, this may be confused with a
ligamentous injury. -
The knee is typically in flexion owing to hamstring spasm.
-
Gross shortening or angular deformity is
variable, with potential compromise of neurovascular status resulting
from traction injury or laceration. A complete neurovascular assessment
is thus critical. -
Point tenderness may be elicited over the
physis; this is usually performed by palpating the distal femur at the
level of the superior pole of the patella and adductor tubercle. -
Most commonly, epiphyseal displacement is in the coronal plane producing varus/valgus deformity.
-
Anteroposterior (AP), lateral, and
oblique views should be obtained. Radiographs of the contralateral
lower extremity may be obtained for comparison. -
Stress views may be obtained to diagnose
nondisplaced separations in which the clinical examination is highly
suggestive of physeal injury (knees with effusion and point tenderness
over physis in setting of negative AP and lateral x-rays). Adequate
analgesia is necessary to relax muscular spasm and to prevent both
false-negative stress radiographs and physeal injury. -
The physeal line should be 3 to 5 mm thick until adolescence.
-
Salter-Harris Type III injuries usually
have vertically oriented epiphyseal fracture components that are best
appreciated on an AP view. -
Computed tomography may be useful to assess articular involvement or to aid in fracture definition.
-
In infants, separation of the distal
femoral physis may be difficult to assess unless there is gross
displacement because only the center of the epiphysis is ossified at
birth; this should be in line with the anatomic axis of the femur on
both AP and lateral views. Magnetic resonance imaging, ultrasound, or
arthrography may aid in the diagnosis of distal femoral injury in these
patients. -
Arteriography of the lower extremity should be pursued if vascular injury is suspected.
|
Table 49.1. Imaging studies in the evaluation of distal femoral physeal fractures
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
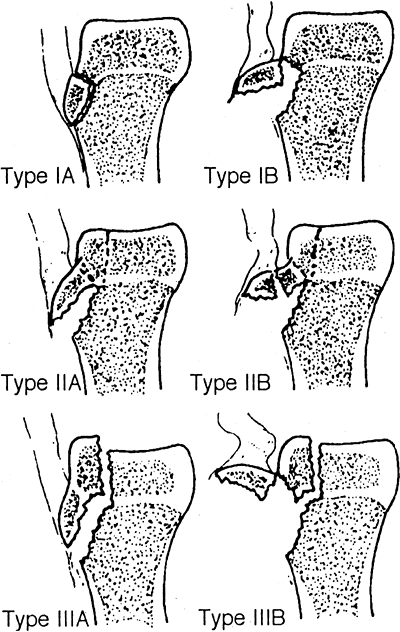
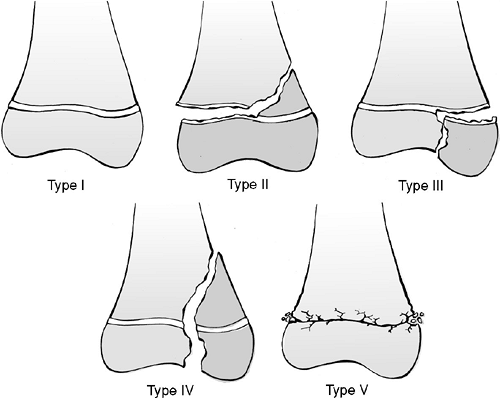
| Type I: | Seen in newborns and adolescents; diagnosis easily missed; physeal widening may be demonstrated on stress radiographs |
| Type II: | Most common injury of the distal femoral physis; displacement usually medial or lateral, with metaphyseal fragment on compression side |
| Type III: | Intraarticular fracture exiting the epiphysis (typically medial condyle from valgus stress |
| Type IV: | Intraarticular fracture exiting the metaphysis; high incidence of growth inhibition with bar formation; rare injury |
| Type V: | Physeal crush injury; difficult diagnosis, made retrospectively after growth arrest; narrowing of physis possible |
 |
|
Figure 49.1. The Salter-Harris classification of fractures involving the distal femoral physis.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
| Anterior: | Results from hyperextension injury; high incidence of neurovascular injury from proximal metaphyseal spike driven posteriorly |
| Posterior: | Rare injury caused by knee hyperflexion |
| Medial: | Valgus force most common, usually Salter-Harris Type II |
| Lateral: | Varus force |
-
Indicated for nondisplaced fractures.
-
A tense effusion may be addressed with sterile aspiration for symptomatic relief.
-
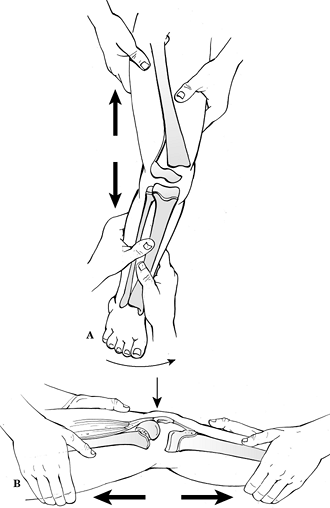
Closed reduction using general anesthesia may be performed for displaced fractures in which a stable result can be obtained (Fig. 49.2).
![]() Figure
Figure
49.2. Closed reduction and stabilization of a Salter-Harris Type I or
II distal femur fracture. (A) With medial or lateral displacement,
traction is applied longitudinally along the axis of the deformity to
bring the fragments back to length. (B) For anterior displacement, the
reduction can be done with the patient prone or supine. Length is
gained first, then a flexion moment is added.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Sufficient traction should be applied
during manipulation to minimize grinding of physeal cartilage (90%
traction, 10% leverage). The position of immobilization varies with
direction of displacement:-
Medial/lateral: Immobilize in 15 to 20
degrees of knee flexion. Cast in valgus mold for medial metaphyseal
fragment and varus mold for lateral metaphyseal fragment to tension
intact periosteum. -
Anterior: Immobilize initially at 90 degrees of knee flexion, then decrease flexion with time.
-
Posterior: Immobilize in extension.
-
-
A residual varus/valgus deformity after reduction tends not to remodel.
-
Crutch ambulation with toe-touch weight bearing may be instituted at 3 to 6 weeks after injury.
-
The cast may be discontinued at 4 to 8
weeks depending on the patient age and healing status. A removable
posterior splint and active range-of-motion exercises are instituted at
this time. -
Athletic involvement should be restricted
until knee range of motion has returned, symptoms have resolved, and
sufficient quadriceps strength has been regained.
-
Indications for open reduction and internal fixation include:
-
Irreducible Salter-Harris Type II
fracture with interposed soft tissue: Cannulated 4.0- or 6.5-mm screw
fixation may be used to secure the metaphyseal spike (Fig. 49.3). -
Unstable reduction.
-
Salter-Harris Type III, IV: Joint congruity must be restored.
-
-
To minimize residual deformity and growth disturbance, certain guidelines should be observed for internal fixation
-
Avoid crossing the physis if possible.
-
If the physis must be crossed, use smooth pins as perpendicular as possible to the physis.
-
Remove fixation that crosses the physis as soon as possible.
-
-
Postoperatively, the patient is
maintained in a long leg cast in 10 degrees of knee flexion. The
patient may be ambulatory with crutches in 1 to 2 days with non–weight
bearing on the injured extremity. At 1 week, the patient may begin
straight leg raises. -
If at 4 weeks evidence of osseous healing
is demonstrated radiographically, the cast may be discontinued with a
posterior splint in place for protection. The patient may be advanced
to partial weight bearing with active range-of-motion exercises. -
The patient typically resumes a normal, active lifestyle at 4 to 6 months after injury.
-
Popliteal artery injury (<2%):
Associated with hyperextension or anterior epiphyseal displacement
injuries in which a traction injury may be sustained or by direct
laceration from the sharp metaphyseal spike.P.589-
A cool, pulseless foot that persists despite reduction should be worked up with angiography to rule out laceration.
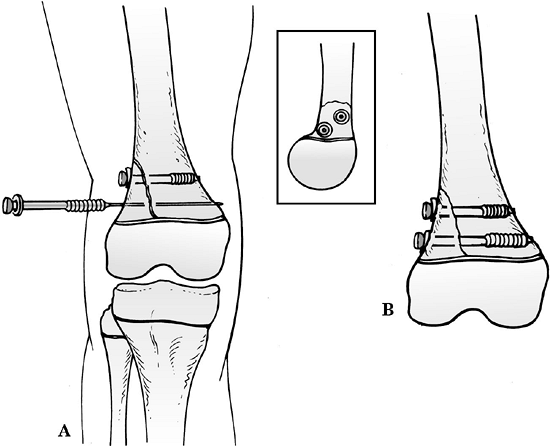 Figure
Figure
49.3. Screw fixation following closed or open reduction of a
Salter-Harris Type II fracture with a large metaphyseal fragment. (A)
When using cannulated screws, place both guide wires before screw
placement to avoid rotation of the fragment while drilling or inserting
screw. Screw threads should be past the fracture site to enable
compression. Washers help increase compression. Screws may be placed
anterior and posterior to each other, which is particularly helpful
when trying to fit multiple screws in a small metaphyseal fragment. (B)
This form of fixation is locally “rigid,” but it must be protected with
long leg immobilization or long lever arm.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Vascular impingement that resolves
following reduction should be observed for 48 to 72 hours to rule out
an intimal tear and thrombosis.
-
-
Peroneal nerve palsy (3%): Caused by
traction injury during fracture or reduction or secondary to initially
anterior/medial displaced epiphysis. Persistent peroneal palsy over 3
to 6 months should be evaluated by electromyography, with possible
exploration as indicated. -
Recurrent displacement: Fractures of
questionable stability following closed reduction should receive
operative fixation (either percutaneous pins or internal fixation) to
prevent late or recurrent displacement. Anterior and posterior
displacements are particularly unstable.
-
Knee instability (up to 37% of patients): Knee instability may be present, indicating concomitant ligamentous compromise that
P.590
was not appreciated at the time of index presentation. The patient may
be treated with rehabilitation for lower extremity strengthening or may
require operative treatment. Collateral ligaments may be acutely
repaired if instability exists after fixation. -
Angular deformity (19%): Results from the
initial physeal injury (Salter-Harris Types I, II), asymmetric physeal
closure (bar formation, Salter-Harris Type III, IV), or unrecognized
physeal injury (Salter-Harris Type V).-
Observation, physeal bar excision
(<30% of physis, >2 years of remaining growth),
hemiepiphysiodesis, epiphyseolysis, or wedge osteotomy may be indicated.
-
-
Leg length discrepancy (24%): Usually
clinically insignificant if <2 years of growth remain; otherwise,
the discrepancy tends to progress at the rate of 1 cm per year.-
Discrepancy <2.5 cm at skeletal maturity usually is of no functional or cosmetic significance.
-
Discrepancy of 2.5 to 5 cm may be treated with contralateral epiphysiodesis (femoral or tibial) or femoral shortening.
-
Discrepancy >5 cm may be an indication
for femoral lengthening combined with epiphysiodesis of the
contralateral distal femur or proximal tibia.
-
-
Knee stiffness (16%): Results from
adhesions or capsular or muscular contracture. It is usually related to
the duration of immobilization; therefore, early discontinuation of the
cast with active range of motion is desirable.
-
Comprise 0.6% to 0.8% of all physeal injuries.
-
Average age is 14 years.
-
Most occur in adolescent boys.
-
The popliteal artery traverses the
posterior aspect of the knee and is tethered to the knee capsule by
connective tissue septa posterior to the proximal tibia. The vascular
supply is derived from the anastomosis of the inferior geniculate
arteries. -
The physis is well protected by osseous
and soft tissue structures, which may account for the low incidence of
injuries to this structure.-
Lateral: fibula
-
Anterior: patellar tendon/ligament
-
Medial: medial collateral ligament (MCL; inserts into metaphysis)
-
Posteromedial: semimembranosus insertion
-
-
Direct: Trauma to the proximal tibia (motor vehicle bumper, lawnmower accident).
-
Indirect: More common and involves
hyperextension, abduction, or hyperflexion from athletic injury, motor
vehicle accident, fall, or landing from a jump with a concurrent MCL
tear. -
Birth injury: Results from hyperextension during breech delivery or arthrogryposis.
-
Pathologic condition: Osteomyelitis of the proximal tibia and myelomeningocele are causes.
-
Patients typically present with an
inability to bear weight on the injured extremity. The knee may be
tense with hemarthrosis, and extension is limited by hamstring spasm. -
Tenderness is present 1 to 1.5 cm distal to the joint line, and variable gross deformity may be present.
-
Neurovascular status should be carefully
assessed for popliteal artery or peroneal nerve compromise. The
anterior, lateral, superficial posterior, and deep posterior
compartments should be palpated for pain or turgor. Patients suspected
of having elevated compartment pressures should receive serial
neurovascular examinations with measurement of compartment pressures as
indicated. -
Associated ligamentous injuries should be
suspected, although it may be difficult to appreciate these injuries
secondary to the dramatic presentation of the fracture.
-
AP, lateral, and oblique views of the
affected knee should be obtained. Radiographs of the contralateral knee
may be obtained for comparison. -
Stress radiographs in coronal and
sagittal planes may be obtained, but hyperextension of the knee should
be avoided because of potential injury to popliteal structures. -
Most patients with proximal tibial
physeal injuries are adolescents in whom the secondary ossicle of the
tibial tubercle has appeared. A smooth, horizontal radiolucency at the
base of the tibial tubercle should not be confused with an epiphyseal
fracture. -
Magnetic resonance imaging may aid in identification of soft tissue interposition when reduction is difficult or impossible.
-
Computed tomography may aid in fracture definition, especially with Salter-Harris Type III or IV fractures.
-
Arteriography may be indicated in patients in whom vascular compromise (popliteal) is suspected.
|
Table 49.2. Classifications and implications of proximal tibial physeal fractures
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
| Type I: | Transphyseal injury; diagnosis often missed; may require stress or comparison views; 50% initially nondisplaced. |
| Type II: | Most common; transphyseal injury exiting the metaphysis; one-third nondisplaced; those that displace usually do so medially into valgus |
| Type III: | Intraarticular fracture of the lateral plateau; MCL often torn |
| Type IV: | Intraarticular fracture of the medial or lateral plateau; fracture line exiting the metaphysis |
| Type V: | Crush injury; retrospective diagnosis common after growth arrest |
-
Nondisplaced fractures may be treated
with a long leg cast with the knee flexed to 30 degrees. The patient
should be followed closely with serial radiographs to detect
displacement. -
Displaced fractures may be addressed with
gentle closed reduction, with limited varus and hyperextension stress
to minimize traction to the peroneal nerve and popliteal vasculature,
respectively. The patient is placed in a long leg cast in flexion
(typically 30 to 60 degrees, depending on the position of stability). -
The cast may be discontinued at 4 to 6
weeks after injury. If the patient is symptomatically improved and
radiographic evidence of healing is documented, active range-of-motion
and quadriceps strengthening exercises are initiated.
-
Commonly, displaced Salter Type I or II
fractures in which stable reduction cannot be maintained may be treated
with percutaneous smooth pins across the physis (Type I) or parallel to
the physis (metaphysis) in Type II. -
Open reduction and internal fixation are indicated for displaced Salter-Harris Types III and IV to restore articular congruity.
P.593
This may be achieved with pin or screw fixation parallel to the physis; articular congruity is the goal.![]() Figure
Figure
49.4. Posterior displacement of the epiphysis following
fracture-separation at the time of injury can cause arterial injury. In
addition, a posteriorly displaced fragment can cause persistent
arterial occlusion by direct pressure.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Postoperatively, the patient is
immobilized in a long leg cast with the knee flexed to 30 degrees. This
is continued for 6 to 8 weeks, at which time the cast may be removed
with initiation of active range-of-motion exercises.
-
Recurrent displacement: This may occur if
closed reduction and casting without operative fixation are performed
on an unstable injury. It is likely secondary to a lack of collateral
ligamentous attachment to the epiphysis. -
Popliteal artery injury (10%): This
occurs especially in hyperextension injuries; it is related to
tethering of the popliteal artery to the knee capsule posterior to the
proximal tibia (Fig. 49.4). Arteriography may be indicated when distal pulses do not return following prompt reduction of the injury. -
Peroneal nerve palsy: This traction
injury results from displacement, either at the time of injury or
during attempted closed reduction, especially with a varus moment
applied to the injury site.
 |
|
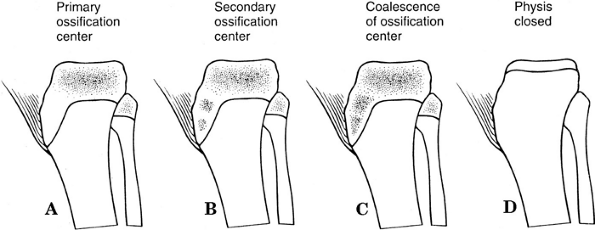
Figure 49.5. Development of the tibial tubercle. (A) In the cartilaginous stage, no ossification center is present in the cartilaginous anlage of the tibial tubercle. (B) In the apophyseal stage, the secondary ossification center forms in the cartilaginous anlage of the tibial tubercle. (C) In the epiphyseal stage, the primary and secondary ossification centers of the proximal tibial epiphysis have coalesced. (D) In the bony stage, the proximal tibial physis has closed.
(From Rockwood CA Jr, Wilkins KE, Beaty JH, eds. Rockwood and Green’s Fractures in Children, 4th ed, vol. 3. Philadelphia: Lippincott-Raven, 1996:1274.)
|
-
Angular deformity: Results from the
initial physeal injury (Salter-Harris Types I, II), asymmetric physeal
closure (bar formation, Salter-Harris Type III, IV), or unrecognized
physeal injury (Salter-Harris Type V). However, Salter-Harris
classification has shown to be not useful in predicting growth
disturbance in proximal tibial fracture types.-
Observation, physeal bar excision
(<30% of physis, >2 years of remaining growth),
hemiepiphysiodesis, epiphyseolysis, or wedge osteotomy may be indicated.
-
-
Leg length discrepancy: This is usually
clinically insignificant if <2 years of growth remain; otherwise,
discrepancy tends to progress at the rate of 1 cm per year. Treatment
for leg length discrepancy remains similar to that for distal femur
physeal injuries.
-
Represent 0.4% to 2.7% of all physeal injuries.
-
They are seen most commonly in athletic boys 14 to 16 years old.
-
It is important to differentiate these fractures from Osgood-Schlatter disease.
-
The tibial tubercle physis, which is
continuous with the tibial plateau, is most vulnerable between the ages
of 13 and 16 years, when it closes from posterior to anterior. -
The tubercle is located one to two
fingerbreadths below the joint line. It is in line with the medial
patella in flexion and the lateral patella in extension.
-
The mechanism of injury is typically
indirect, usually resulting from a sudden accelerating or decelerating
force involving the quadriceps mechanism. -
Predisposing factors include:
-
Patella baja.
-
Tight hamstrings (increase flexion torque).
-
Preexisting Osgood-Schlatter disease (uncertain whether mechanical vulnerability or overdevelopment of quadriceps mechanism).
-
Disorders with physeal anomalies.
-
-
Patients typically present with a limited
ability to extend the knee as well as an extensor lag. The leg is held
in 20 to 40 degrees of flexion by spastic hamstrings. -
Swelling and tenderness over the tibial tubercle are typically present, often with a palpable defect.
-
Hemarthrosis is variable.
-
Patella alta may be observed if displacement is severe.
-
AP and lateral views of the knee are
sufficient for the diagnosis, although a slight internal rotation view
best delineates the injury because the tibial tubercle lies just
lateral to the tibial axis. -
Patella alta may be noted.
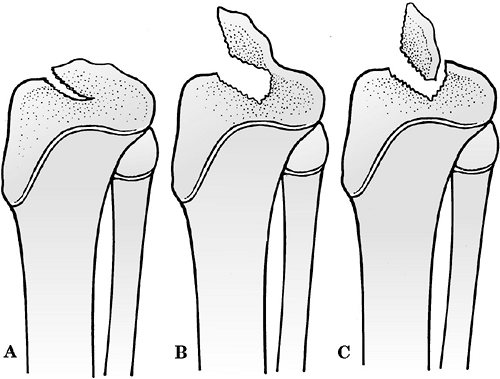
| Type I: | Small fragment avulsed and displaced proximally; fracture through secondary ossification center |
| Type II: | Secondary ossification center already coalesced with proximal tibial epiphysis; fracture at level of horizontal portion of tibial physis |
| Type III: | Fracture line passing proximally through tibial epiphysis and into joint; possibly confused with Salter-Harris Type III tibial physeal injury |
(see earlier) subdivides each type into A and B categories to account
for the degree of displacement and comminution (Fig. 49.6).
-
Indicated for Type IA fractures with intact extensor mechanism.
-
It consists of manual reduction and immobilization in a long leg cast with the knee extended, with patellar molding.
![]() Figure 49.6. Ogden classification of tibial tuberosity fractures in children.(From Ogden JA. Skeletal Injury in the Child, 2nd ed. Philadelphia: WB Saunders, 1990:808.)
Figure 49.6. Ogden classification of tibial tuberosity fractures in children.(From Ogden JA. Skeletal Injury in the Child, 2nd ed. Philadelphia: WB Saunders, 1990:808.) -
The cast is worn for 4 to 6 weeks, at
which time the patient may be placed in a posterior splint for an
additional 2 weeks. Gentle active range-of-motion exercises and
quadriceps strengthening exercises are instituted and advanced as
symptoms abate.
-
Indicated for Types IB, II, III fractures or irreducible Type IA fractures (periosteum may be interposed).
-
A vertical midline approach is used; the
fracture can be stabilized using smooth pins (>3 years from skeletal
maturity), screws, threaded Steinmann pins, or a tension band. -
Postoperatively, the extremity is placed
in a long leg cast in extension with patella molding for 4 to 6 weeks,
at which time the patient may be placed in a posterior splint for an
additional 2 weeks. Gentle active range-of-motion exercises and
quadriceps strengthening exercises are instituted and advanced as
symptoms abate.
-
Genu recurvatum: This occurs secondary to
premature closure of anterior physis; it is rare because injury occurs
typically in adolescent patients near skeletal maturity. -
Loss of knee motion: Loss of flexion may
be related to scarring or postoperative immobilization. Loss of
extension may be related to nonanatomic reduction and emphasizes the
need for operative fixation of Type IB, II, and III fractures. -
Patella alta: May occur if reduction is insufficient.
-
Osteonecrosis of fracture fragment: Rare because of soft tissue attachments.
-
Compartment syndrome: Rare, but it may
occur with concomitant tearing of the anterior tibial recurrent vessels
that retract to the anterior compartment when torn.
-
Relatively rare injury, occurring in 3 per 100,000 children per year.
-
Most commonly caused by a fall from a bicycle (50%).
-
There are two tibial spines: anterior and
posterior. The ACL spans the medial aspect of the lateral femoral
condyle to the anterior tibial spine. -
In the immature skeleton, ligaments are
more resistant to tensile stresses than are physeal cartilage or
cancellous bone; therefore, forces that would lead to an ACL tear in an
adult cause avulsion of the incompletely ossified tibial spine in a
child.
-
Indirect trauma: The mechanism includes rotatory, hyperextension, and valgus forces.
-
Direct trauma: Extremely rare, secondary to multiple trauma with significant knee injury.
-
Patients are typically reluctant to bear weight on the affected extremity.
-
Hemarthrosis is usually present, with painful range of motion and a variable bony block to full extension.
-
The MCL and lateral collateral ligament (LCL) should be stressed with varus/valgus pressure to rule out associated injury.
-
AP and lateral views should be obtained.
The AP view should be scrutinized for osseous fragments within the
tibiofemoral articulation; these may be difficult to appreciate because
only a thin, ossified sleeve may be avulsed. -
Obtaining an AP radiograph to account for
the 5 degrees of posterior slope of the proximal tibia may aid in
visualization of an avulsed fragment. -
Stress views may be useful in identification of associated ligamentous or physeal disruptions.
 |
|
Figure
49.7. Classification of tibial spine fractures. (A) Type I, minimal displacement. (B) Type II, hinged posteriorly. (C) Type III, complete separation. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Indicated for Type I and II fractures of the tibial spine.
-
The knee should be immobilized in extension; the fat pad may contact the spine in extension and thus help with reduction.
-
Indicated for Type III and IV fractures of the tibial spine owing to uniformly poor results with nonoperative management.
-
Debridement of fracture site is recommended with fixation using sutures, pins, or screws.
-
The fracture may be repaired arthroscopically with an ACL guide.
-
Postoperatively, the patient is placed in
a long leg cast with the knee in slight (10 to 20 degree) flexion. In 4
to 6 weeks, the cast is removed with initiation of active
range-of-motion and quadriceps and hamstrings strengthening.
-
Loss of extension: Present in up to 60%
of cases. Extension loss is typically clinically insignificant and may
represent a bony block to extension caused by malunion of a type III
fracture. -
Knee instability: May persist with Type
III or IV fractures accompanied by collateral ligament injuries and/or
physeal fractures.
-
Very rare in children; only 1% of all patella fractures are seen in patients less than 16 years of age.
-
The patella is the largest sesamoid in the body.
-
The function of the patella is to
increase the mechanical advantage and leverage of the quadriceps
tendon, aid in nourishment of the femoral articular surface, and
protect the femoral condyles from direct trauma. -
Forces generated by the quadriceps in
children are not as high as in adults owing to a smaller muscle mass
and shorter moment arm. -
The blood supply to the patella derives
from the anastomotic ring from the superior and inferior geniculate
arteries. An additional supply through the distal pole is from the fat
pad. -
The ossification center appears between 3
and 5 years. Ossification then proceeds peripherally and is complete by
10 to 13 years. -
Patella fracture must be differentiated
from a bipartite patella (present in up to 8% of patients), which is
located superolaterally. One should obtain contralateral films because
bilateral bipartite patella is present in up to 50% of cases.
-
Direct: Most common and involves trauma
to the patella secondary to a fall or motor vehicle accident. Cartilage
anlage acts as a cushion to a direct blow. -
Indirect: A sudden accelerating or decelerating force on the quadriceps.
-
Marginal fracture: Usually medial owing to patellar subluxation or dislocation laterally.
-
Predisposing factors include:
-
Previous trauma to the knee extensor mechanism.
-
Spasticity or contracture of the extensor mechanism.
-
-
Patients typically present with refusal to bear weight on the affected extremity.
-
Swelling, tenderness, and hemarthrosis are usually present, often with limited or absent active extension of the knee.
-
Patella alta may be present with avulsion or sleeve fractures, and a palpable osseous defect may be appreciated.
-
An apprehension test may be positive and
may indicate the presence of a spontaneously reduced patellar
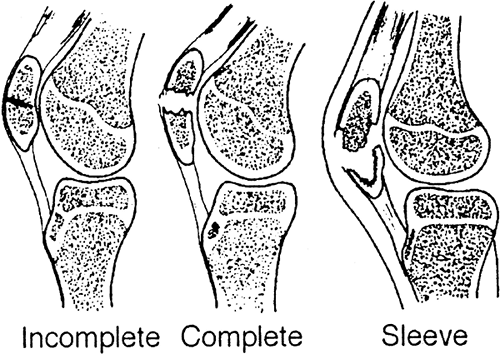
dislocation that resulted in a marginal fracture.![]() Figure 49.8. Patellar fractures in children.(From Ogden JA. Skeletal Injury in the Child, 2nd ed. Philadelphia: WB Saunders, 1990:761.)
Figure 49.8. Patellar fractures in children.(From Ogden JA. Skeletal Injury in the Child, 2nd ed. Philadelphia: WB Saunders, 1990:761.)
-
AP, lateral, and patellar (sunrise) views of the knee should be obtained.
-
Transverse fracture patterns are most
often appreciated on lateral view of the knee. The extent of
displacement may be better appreciated on a stress view with the knee
flexed to 30 degrees (greater flexion may not be tolerated by the
patient). -
Longitudinally oriented and marginal
fractures may be best appreciated on AP or sunrise views. It is
important to distinguish this from osteochondral fracture, which may
involve a large amount of articular surface. -
Stellate fractures and bipartite patella
are best appreciated on AP radiographs. Comparison views of the
opposite patella may aid in delineating a bipartite patella.
| Transverse: | Complete versus incomplete |
| Marginal fractures: | Generally resulting from lateral subluxation or dislocation of the patella; may be either medial (avulsion) or lateral (direct trauma from condyle) |
| Sleeve fracture: | Unique to immature skeleton; consisting of an extensive sleeve of cartilage pulled from the osseous patella with or without an osseous fragment from the pole |
| Stellate: | Generally from direct trauma in the older child |
| Longitudinal avulsion |
-
Displaced fractures (>3 mm diastasis
or >3 mm articular step-off): Stabilization involves use of cerclage
wire, tension band technique, sutures, or screws; the retinaculum must
also be repaired. -
Sleeve fracture: Careful reduction of the
involved pole and cartilaginous sleeve is performed with fixation and
retinacular repair; if this is missed, the result is an elongated
patella with extensor lag and quadriceps weakness. -
Postoperatively, the leg is maintained in
a well-molded cylinder cast for 4 to 6 weeks. Quadriceps strengthening
and active range-of-motion exercises are instituted as soon as possible. -
Partial patellectomy should be reserved for severe comminution.
-
Quadriceps weakness: Compromised
quadriceps function occurs secondary to missed diagnosis or inadequate
treatment with functional elongation of the extensor mechanism and loss
of mechanical advantage. -
Patella alta: Results from functional
elongation of the extensor mechanism and is associated with quadriceps
atrophy and weakness. -
Posttraumatic osteoarthritis: Degenerative changes occur secondary to chondral damage at the time of injury.
-
Typically involve the medial or lateral femoral condyles or the patella.
-
Often occur in association with patellar dislocation.
-
As the knee flexes, the patella engages the condylar groove. At 90 to 135 degrees, the patella rides within the notch.
-
Exogenous: A direct blow or a shearing force (patellar dislocation). This is the most common pathologic process.
-
Endogenous: A flexion/rotation injury of
the knee. Contact between the tibia and the femoral condyle results in
osteochondral fracture of the condyle.
-
The patient presents with knee effusion and tenderness over the site of fracture.
-
The knee is held in a position of comfort, usually in 15 to 20 degrees of flexion.
-
Standard knee AP and lateral x-rays often establish the diagnosis.
-
Schuss and Tunnel views may be helpful to localize the fragment near the notch.
-
Operative excision versus fixation of
fragment depends on the size and location of the defect as well as on
the timing of surgery. -
Small fragments or injuries to non–weight-bearing regions may be excised either open or arthroscopically.
-
Large fragments may be fixed with subchondral or headless lag screws.
-
If surgery is delayed more than 10 days
after the injury, the piece should be excised because the cartilage is
not typically viable. -
Postoperatively, in patients with
internal fixation, a long leg cast with 30 degrees of flexion is
applied. The patient is typically non–weight bearing for 6 weeks. -
If excision is performed, the patient may bear weight as tolerated and range the knee after soft tissues heal.
-
Patella dislocation is more common in
women, owing to physiologic laxity, as well as in patients with
hypermobility and connective tissue disorders (e.g., Ehlers-Danlos or
Marfan syndrome).
-
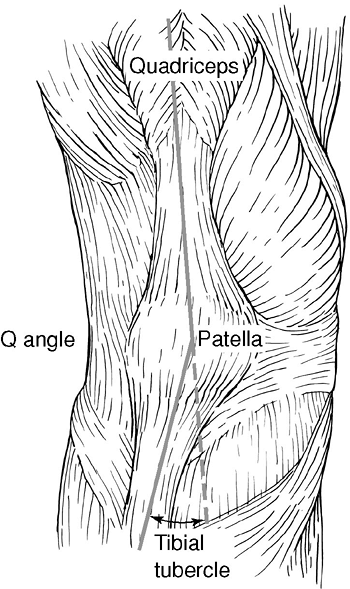
The “Q angle” is defined as the angle
subtended by a line drawn from the anterior superior iliac spine
through the center of the patella and a second line from the center of
the patella to the tibial tubercle (Fig. 49.9).
The Q angle ensures that the resultant vector of pull with quadriceps
action is laterally directed; this lateral moment is normally
counterbalanced by patellofemoral, patellotibial, and retinacular
structures as well as patellar engagement within the trochlear groove.
An increased Q angle predisposes to patella dislocation. -
Dislocations are associated with patella
alta, congenital abnormalities of the patella and trochlea, hypoplasia
of the vastus medialis, and hypertrophic lateral retinaculum.
-
Lateral dislocation: The mechanism is
forced internal rotation of the femur on an externally rotated and
planted tibia with the knee in flexion. It is associated with a 5% risk
of osteochondral fractures. -
Medial instability is rare and usually
iatrogenic, congenital, traumatic, or associated with atrophy of the
quadriceps musculature. -
Intraarticular dislocation: Uncommon, but
it may occur following knee trauma in adolescent boys. The patella is
avulsed from the quadriceps tendon and is rotated around the horizontal
axis, with the proximal pole lodged in the intercondylar notch.
 |
|
Figure
49.9. The Q (quadriceps) angle is measured from the anterior superior iliac spine through the patella and to the tibial tubercle. (From Insall JN. Surgery of the Knee. New York: Churchill Livingstone, 1984.)
|
-
Patients with an unreduced patella
dislocation will present with hemarthrosis, an inability to flex the
knee, and a displaced patella on palpation. -
Patients with a lateral dislocation may also present with medial retinacular pain.
-
Patients with reduced or chronic patella
dislocation may demonstrate a positive “apprehension test,” in which a
laterally directed force applied to the patella with the knee in
extension reproduces the sensation of impending dislocation, causing
pain and quadriceps contraction to limit patellar mobility.
-
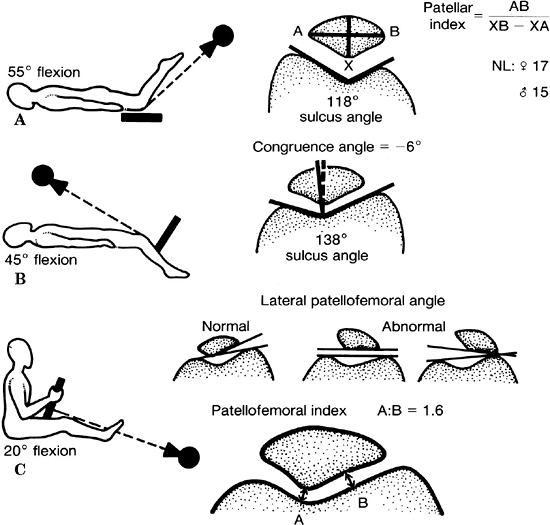
AP and lateral views of the knee should
be obtained. In addition, an axial (sunrise) view of both patellae
should be obtained. Various axial views have been described by several
authors (Fig. 49.10)-
Hughston 55 degrees of knee flexion: sulcus angle, patellar index
-
Merchant 45 degrees of knee flexion: sulcus angle, congruence angle
-
Laurin 20 degrees of knee flexion: patellofemoral index, lateral patellofemoral angle
-
-
Assessment of patella alta or baja is based on the lateral radiograph of the knee.
-
Blumensaat line: The lower pole of the
patella should lie on a line projected anteriorly from the
intercondylar notch on the lateral radiograph with the patient’s knee
flexed to 30 degrees. -
Insall-Salvati ratio: The ratio of the
length of the patellar ligament (LL; from the inferior pole of the
patella to the tibial tubercle) to the patellar length (LP; the
greatest diagonal length of the patella) should be 1.0. A ratio of 1.2
indicates patella alta, whereas 0.8 indicates patella baja (Fig. 49.11).
P.604 -
 |
|
Figure
49.10. Representation of the (A) Hughston (knee flexed to 55 degrees) (B) merchant (knee flexed to 45 degrees) and (C) Laurin (knee flexed to 20 degrees) patellofemoral views. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
-
Reduced versus unreduced
-
Congenital versus acquired
-
Acute (traumatic) versus chronic (recurrent)
-
Lateral, medial, intraarticular, superior
-
Reduction and casting or bracing in knee extension may be undertaken with or without arthrocentesis for comfort.
-
The patient may ambulate in locked extension for 3 weeks, at which time progressive flexion can be instituted with physical
P.605
therapy for quadriceps strengthening. After a total of 6 to 8 weeks, the patient may be weaned from the brace.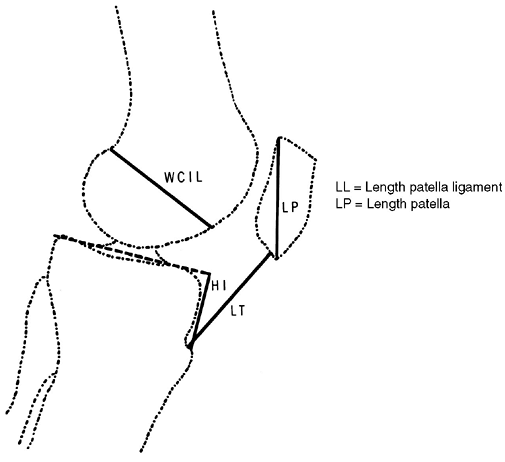 Figure 49.11. Insall-Salvati technique for measuring patellar height.(From Insall NJ. Surgery. New York: Churchill Livingstone, 1984.)
Figure 49.11. Insall-Salvati technique for measuring patellar height.(From Insall NJ. Surgery. New York: Churchill Livingstone, 1984.) -
Surgical intervention for acute dislocations is rarely indicated except for displaced intraarticular fractures.
-
Intraarticular dislocations may require reduction with patient under anesthesia.
-
Functional taping with moderate success has been described in the physical therapy literature.
-
Primarily used in cases of recurrent dislocations.
-
No single procedure corrects all patella
malalignment problems—the patient’s age, diagnosis, level of activity,
and condition of the patellofemoral articulation must be taken into
consideration. -
Patellofemoral instability should be addressed by correction of all malalignment factors.
-
Degenerative articular changes influence the selection of realignment procedure.
-
Surgical interventions include:
-
Lateral release: Indicated for
patellofemoral pain with lateral tilt, lateral retinacular pain with
lateral patellar position, and lateral patellar compression syndrome.
It may be performed arthroscopically or as an open procedure. -
Medial plication: May be performed at the time of lateral release to centralize the patella.
-
Proximal patellar realignment: Medialization of the proximal pull of the patella is indicated when a lateral release/medial
P.606
plication fails to centralize the patella. The release of tight
proximal lateral structures and reinforcement of the pull of medial
supporting structures, especially the vastus medialis obliquus, are
performed in an effort to decrease lateral patellar tracking and
improve congruence of the patellofemoral articulation. Indications
include recurrent patella dislocations after failed nonoperative
therapy and acute dislocations in young, athletic patients, especially
with medial patella avulsion fractures or radiographic lateral
subluxation/tilt after closed reduction. -
Distal patella realignment: Reorientation
of the patella ligament and the tibial tubercle is indicated when an
adult patient experiences recurrent dislocations and patellofemoral
pain with malalignment of the extensor mechanism. This is
contraindicated in patients with open physes and normal Q angles. It is
designed to advance and medialize tibial tubercle, thus correcting
patella alta and normalizing the Q angle.
-
-
Redislocation: A younger age at initial
dislocation increases the risk of recurrent dislocation. Recurrent
dislocation is an indication for surgical intervention. -
Loss of knee motion: May result from prolonged immobilization.
-
Patellofemoral pain: May result from retinacular disruption at the time of dislocation or from chondral injury.
-
Infrequent in skeletally immature
individuals, because physeal injuries to the distal femur or proximal
tibia are more likely to result.
-
Typically occurs with major ligamentous
disruptions (both cruciates or equivalent spine injuries with
disruption of either MCL or/and LCL) about the knee. -
Associated with major disruption of soft
tissue and damage to neurovascular structures; vascular repair must
take place within the first 6 to 8 hours to avoid permanent damage. -
Associated with other knee injuries, including tibial spine fractures, osteochondral injuries, and meniscal tears.
-
Most dislocations occur as a result of multiple trauma from motor vehicle accidents or falls from a height.
-
Patients almost always present with gross
knee distortion. Immediate reduction should be undertaken without
waiting for radiographs in the displaced position. Of paramount
importance is the arterial supply, with secondary consideration given
to neurologic status. -
A careful neurovascular examination is
critical both before and after reduction. The popliteal artery is at
risk during traumatic dislocation of the knee owing to the bowstring
effect across the popliteal fossa secondary to proximal and distal
tethering. Peroneal nerve injuries are also common, mostly in the form
of traction neurapraxias.
-
Gross dislocation should be reduced first and not delayed for films.
-
AP and lateral views are sufficient to establish the diagnosis; the most common direction is anterior.
-
Radiographs should be scrutinized for
associated injuries to the tibial spine, distal femoral physis, or
proximal tibial physis. Stress views may be obtained to detect
collateral ligament injury. -
It remains controversial whether all
patients should have an arteriogram. Some authors state that if pulses
are present both before and after reduction, arteriography is not
indicated. The patient must be monitored for 48 to 72 hours after
reduction because late thrombus may develop as a result of intimal
damage.
to the distal femur. It also should include open versus closed and
reducible versus irreducible. The injury may be classified as occult,
indicating a knee dislocation with spontaneous reduction.
| Anterior: | Forceful knee hyperextension beyond 30 degrees; most common; associated with PCL with or without ACL tear, with increasing incidence of popliteal artery disruption with increasing degree of hyperextension |
| Posterior: | Posteriorly directed force against proximal tibia of flexed knee; “dashboard” injury; accompanied by ACL/PCL disruption as well as popliteal artery compromise with increasing proximal tibial displacement |
| Lateral: | Valgus force; medial supporting structures disrupted, often with tears of both cruciate ligaments |
| Medial: | Varus force; lateral and posterolateral structures disrupted |
| Rotational: | Varus/valgus with rotatory component; usually result in buttonholing of femoral condyle through capsule |
-
Vascular compromise: Unrecognized and
untreated vascular compromise to the leg, usually in the form of an
unrecognized intimal injury with late thrombosis and ischemia,
represents the most serious and potentially devastating complication
from a knee dislocation. Careful, serial evaluation of neurovascular
status is essential, up to 48 to 72 hours after injury, with aggressive
use of arteriography as indicated. -
Peroneal nerve injury: Usually represents
a traction neurapraxia that will resolve. Electromyography may be
indicated if resolution does not occur within 3 to 6 months.