FRACTURES OF THE HIP AND PROXIMAL FEMUR
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Pelvis and
Femur > CHAPTER 19 – FRACTURES OF THE HIP AND PROXIMAL FEMUR
following authors from the second edition, whose previous contributions
are included in part in this chapter: Timothy J. Bray, David C.
Templeman, Richard F. Kyle, Sara J. Campbell, Donald A. Wiss, and Hans
G. Ender.
Approximately 97% occur in patients over 50 years of age (the incidence
increases with age), and only 3% in patients under 50. In the latter
group, they occur most commonly between 20 and 40 years of age, usually
in men, and are due to high-energy trauma associated with sports and
industrial and motor-vehicle accidents (106,136).
In this young group, most hip fractures are subtrochanteric or
basicervical. In contrast, fractures of the hip in patients between 40
and 50 years of age usually occur in alcoholics or patients with
multiple medical diseases, whose fractures are related to osteoporosis.
occurring in the terminal years of life, and they have a major impact
on society, our health care system, and the cost of care (45).
Annually, 250,000 fractures of the hip occur in the United States. The
number of fractures is projected to double by the year 2050 as the
population ages (78). Health care costs for fractures exceed $6 billion per year. Martin et al. [quoted in Koval and Zuckerman (78)]
showed that in Canada from 1972 to 1984 the incidence of initial
fractures of the proximal femur in persons older than 50 years
increased 60% in women and 42% in men. The incidence increased
exponentially with age, doubling for every 6 years of age and reaching
a maximum incidence of 4% of women over 90. Martin et al. attributed
this increase to a gradual decline in physical activity, which
contributes to the bone loss (78). At 1 year after a hip fracture, mortality rates in elderly people range from 14% to 36% (78).
The highest risk of mortality occurs in the first 6 months after
fracture; after 1 year the mortality rate approaches that of persons
who have not sustained a hip fracture.
extensive study of functional recovery after fracture of the hip, state
that the factors influencing morbidity and mortality are best
understood if broken into three phases: the patient status before the
fracture, preoperative management, and postoperative care. Age at the
time of fracture does not necessarily correlate with a higher mortality
rate. Systemic illnesses, however, such as congestive heart failure,
coronary artery disease, diabetes mellitus, chronic obstructive
pulmonary disease, and rheumatoid arthritis have been shown to increase
the mortality rate. Koval and Zuckerman (78)
pointed out other preoperative factors that worsened the prognosis,
including cerebral dysfunction in the form of chronic organic brain
syndrome, cerebral vascular disease, or psychiatric illness; and
permanent habitation in an institution as opposed to a home.
associated with male sex, advanced age, untreated or poorly controlled
systemic disease, cerebral dysfunction, institutionalization, internal
fixation before control of medical comorbidities, and postoperative
complications.
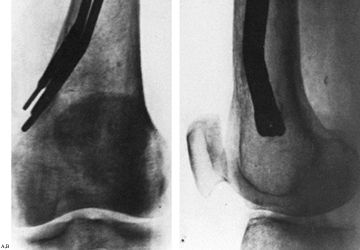
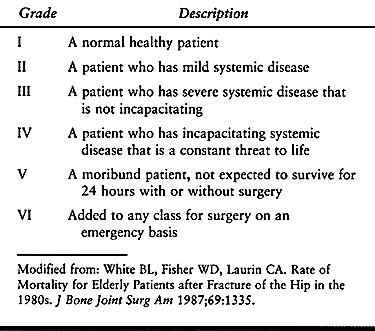
preoperative grading system of the American Society of
Anesthesiologists to predict mortality. They found that grade 1 or
grade 2 patients had a 1-year mortality rate of 8%, whereas grade 3 and
4 patients had a 1-year mortality rate of 49% (Table 19.1).
 |
|
Table 19.1. Classification of Physical Status According to the System of the American Society of Anesthetists
|
the effect of timing of internal fixation on mortality. They concluded
that patients with two or fewer comorbidities benefited by internal
fixation of the hip within 2 days after admission, whereas delay to
better treat comorbidities and better prepare the patient for surgery
was beneficial for patients with three or more comorbidities.
reducing mortality, are to return the patient to walking, and to give
her sufficient independence that she can live at home with or without
assistance. The factors that have been reported to be predictors of
return to ambulation are male sex, younger age, absence of mental
impairment, and use of a cane or walker before injury. The factors that
predict discharge to home are younger age, independent ambulation
before fracture, capability in activities of daily living, and the
presence of another person in the home. Similar factors apply to return
to activities of daily living. In addition, Zuckerman et al. (159)
showed that an interdisciplinary hospital program specifically designed
to manage elderly patients with hip fractures resulted in fewer
postoperative complications, fewer incidences of
treatment
in an intensive care unit, significantly improved ability to walk at
the time of hospital discharge, and fewer transfers to a nursing home.
head with its articular cartilage, and the femoral neck, which connects
the head to the shaft in the region of the lesser and greater
trochanters. The synovial membrane incorporates the entire femoral head
and the anterior neck, but only the proximal half of the neck
posteriorly. The shape and size of femoral necks vary widely. In our
practice, for example, there is a large discrepancy between those seen
in small Asians and those in large blacks. The neck–shaft angle does
not vary much, however, and is approximately 130° ± 7° (104). Anteversion of the femoral neck is 10° ± 7° in normal individuals, with no variation between the sexes (103). The diameter of the femoral head ranges from 40 to 60 mm, depending on the size of the individual (63). The thickness of the articular cartilage varies from 4 mm at the apex of the head to 3 mm at the periphery (63).
In contrast to the medial femoral neck as seen on an anteroposterior
(AP) radiograph of the hip, the calcar femorale is a dense plate of
bone that originates from the posterior medial portion of the femoral
shaft, where it blends into the neck of the femur and extends
superiorly toward the greater trochanter, fusing with the
posteriorcortex of the femoral neck. It is more of a posterior than a
medial structure (134).
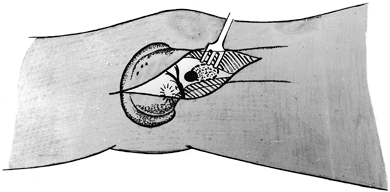
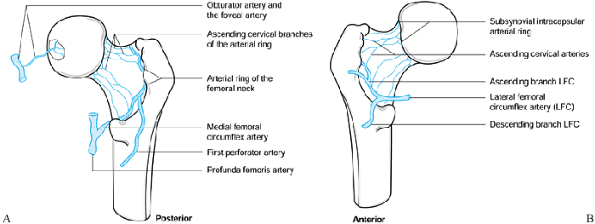
In the majority of persons, the major blood supply to the head comes
via the lateral epiphyseal vessels, which penetrate into the bone of
the femoral head at its junction with the neck. As seen in Figure 19.1,
these vessels are supplied by the subsynovial intracapsular arterial
ring, which derives from the ascending cervical arteries running
beneath the synovium of the femoral neck. These vessels originate from
the extracapsular arterial ring, which is primarily the termination of
the medial femoral circumflex artery on the posterior aspect of the hip
along the intertrochanteric basicervical line. The lateral femoral
circumflex artery on the anterior aspect of the neck also contributes
to this blood supply; however, the medial femoral circumflex artery
usually dominates. The artery of the ligamentum teres usually
originates from the anterior obturator artery but it contributes to the
blood supply of only a small area of the femoral head near the
attachment of the ligamentum teres. Intraosseous cervical vessels
derived from the femoral neck also penetrate into the femoral head but
are not the major blood supply (24,25,142).
 |
|
Figure 19.1. Posterior (A) and anterior (B) views of the hip, showing the extraosseous blood supply to the femoral head.
|
cervical vessels, making femoral head viability totally dependent on
the retinacular vessels and the artery of the ligamentum teres.
Displacement of the femoral neck fracture nearly always results in
severe compromise of the blood supply to the head (27,28,98,119).
is the accumulation of an intracapsular hematoma, which can interfere
with venous outflow from the head and perhaps vascular inflow. As a
result, some authors recommend routine aspiration of the hip or
incision of the hip joint capsule after fracture (30,134). Opinions on this are not uniform, however (38).
complete disruption of the epiphyseal vessels, mild to moderate
distortion of alignment at the fracture site may compromise intact
vessels. After 12 hours of disruption of the blood supply to the
femoral head, all cells within the head are most likely necrotic.
Therefore, in any patient in whom an effort will be made to preserve
the femoral head, the fracture should be gently reduced as soon as
possible. This can be achieved in the emergency room by aspiration of
the hip and injection of a small amount of local anesthetic to provide
pain relief. Simple longitudinal traction and mild gentle internal
rotation, placing the limb in 5–7 pounds (2.3–3.1 kg) of Buck’s
traction with the leg lying on a pillow, will nearly always result in
marked improvement in position, thus optimizing the opportunity for
early return of blood flow to the femoral head (131,133).
Anatomic reduction and excellent stability optimize the conditions for
rapid revascularization across the fracture into the femoral head. This
can occur by lumen-to-lumen reconnection of existing blood vessels. The
foveal blood supply may be important in this revascularization. Rotary
and valgus malposition have an adverse effect, not only on the
retinacular blood supply, but on that of the foveal blood vessel as
well (125).
the femoral head. Fixation devices placed in the superior lateral
aspects of the femoral head can inadvertently injure the lateral
epiphyseal vessels. Devices that are driven into the head rather than
being screwed into the head or inserted in an atraumatic manner can
lead to an increased incidence of aseptic necrosis (132).
Twisting of the femoral head while inserting hip screws and using large
implants that occupy a substantial cross-sectional area in the femoral
neck have also been identified as increasing the incidence of avascular
necrosis (84).
vascular supply to the femoral head at the time of internal fixation
has produced uniformly reliable results; therefore, the decision as to
whether to preserve the femoral head or to go on to hemiarthroplasty
remains a clinical surgical decision.
an elderly person falls from a standing position, resulting in a direct
blow over the greater trochanter. It has been hypothesized that fatigue
fractures of the femoral neck in the elderly with very osteoporotic
bone may be the precipitating cause of the fall rather than the fall
being the causal factor. It appears that this is highly unusual and
that the vast majority of fractures are indeed caused by a fall (70).
Femoral fractures in young and middle-aged adults are usually caused by
high-velocity vehicular trauma or a fall from a substantial height,
resulting in axial loading of the femur while the hip is abducted (70).
This same method of loading with the hip in adduction is more likely to
result in a dislocation with or without associated fractures of the
posterior acetabulum or femoral head (40).
Extreme external rotation tightening the anterior capsule and perhaps
leading to impingement of the posterior cortex of the femoral neck on
the acetabular rim can cause fracture as well and is compatible with
the marked posterior comminution of the neck frequently seen in
displaced fractures (5,116).
fracture; by 65 years of age, 50% of women show bone mineral content
below the threshold for fracture, and by 85 years of age this climbs to
100% (105). Osteomalacia plays a much smaller role—Wilton et al. (151)
found that only 2% of a large population of patients who had sustained
fractures of the femoral neck showed evidence of osteomalacia.
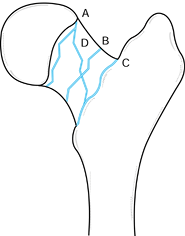
The first two are intracapsular and the third can be partially
intracapsular and extracapsular posteriorly. Subcapital fractures are
at greatest risk for disruption of the blood supply to the femoral
head, transcervical fractures have a somewhat lower risk, and the risk
is extremely low in basilar neck fractures. This is dependent mostly on
the degree of displacement, which is addressed better by the Garden
classification, discussed next. Fractures with a high shear angle, such
as high-velocity fractures in young persons, can begin in the basilar
neck area, traverse the femoral neck proximally, and exit in a
subcapital location. Usually these are not displaced because they are
commonly associated with fractures of the shaft of the femur, which
dissipates most
of
the energy. If displaced, these fractures have an incidence of
avascular necrosis of the femoral head similar to that seen in
displaced subcapital fractures.
 |
|
Figure 19.2. Types of intracapsular fractures of the femoral neck: subcapital (A), transcervical (B), basilar neck (C), and high-angle shear fracture typical of those seen in ipsilateral concomitant fractures of the hip and femoral shaft (D).
|
on the blood supply to the femoral head, the major importance of the
anatomic location of the fractures is its influence on the choice of
internal fixation device. Subcapital fractures and proximal
transcervical fractures are usually best internally fixed with multiple
screws, which threaten the blood supply to the femoral head least, and
leave the largest cross-sectional area in the femoral neck for bone
healing and revascularization. More distal fractures, in particular
those that are basilar neck and have a high shear angle, do not provide
enough bone stock for adequate purchase of the multiple screws in the
distal fragment; therefore, sliding compression hip screws with side
plates are indicated for basilar neck fractures, particularly in young
active individuals.
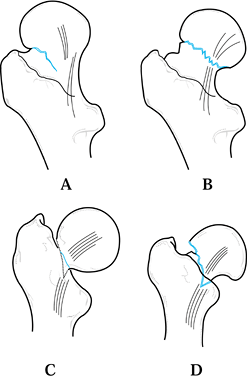
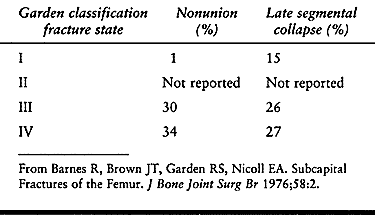
in a large multi-institutional study, found a reasonably good
correlation between the Garden classification and the incidence of
nonunion and avascular necrosis, as indicated in Table 19.2.
The interrater reliability of orthopaedic surgeons using the Garden
classification is not particularly good; therefore, from a practical
viewpoint, most surgeons lump Garden stage I and II fractures together
as “undisplaced” and Garden stage III and IV fractures together as
“displaced.” Undisplaced fractures, if internally fixed in good
position and stable, have a favorable prognosis, with union rates of
95% or better and an incidence of avascular necrosis of under 10%,
whereas displaced fractures have rates of
avascular
necrosis as high as 40% (in Garden stage IV fractures) and nonunion
rates of 10% or more. This difference in prognosis is the key factor in
deciding whether to perform prosthetic replacement of the femoral head
or internal fixation in elderly patients with these fractures. This is
discussed in more detail later.
 |
|
Figure 19.3. Garden classification of femoral neck fractures. A: Stage I: Incomplete fracture that is abducted and impacted. B: Stage II: Complete fracture without displacement. Note that the compression trabeculae are aligned. C:
Stage III: Complete fracture with partial displacement. The neck is still in apposition posteroinferiorly; therefore, the fragments have rotated in opposite directions like two cogwheels. Note that the compression trabeculae are angulated. D: Stage IV: Complete fracture with full displacement. Contact between the fracture surfaces is lost. The distal fragment is in full external rotation and lies anterior to the proximal fragment. The proximal fragment is free to resume its natural position in the acetabulum; therefore, the compression trabeculae lie in their normal alignment. |
 |
|
Table
19.2. Correlation between the Garden Classification of Subcapital Femoral Fractures and Rates of Nonunion and Late Segmental Collapse at 36 Months Follow-Up |
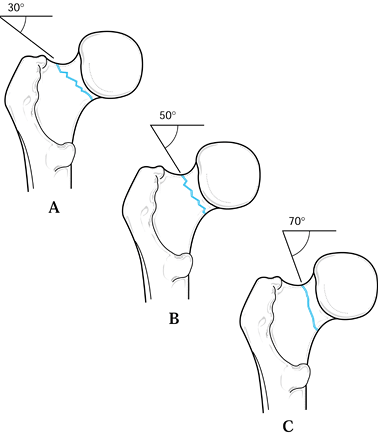
Pauwels’s type I fracture is the most horizontal, is often impacted,
and therefore with internal fixation tends to stabilize with weight
bearing, whereas the Pauwels’s type III fracture is nearly vertical,
experiences a large degree of shear with weight bearing, and is
therefore unstable.
 |
|
Figure 19.4. Pauwels’s classification of intracapsular hip fractures. A: Type I: Fracture is 30° to 49° from the horizontal. B: Type II: Fracture is 50° to 69° from the horizontal. C: Type III: Fracture is 70° or more from the horizontal.
|
interpretation of routine AP and lateral radiographs. For reproducible
interpretation, the AP view must show the femoral neck in full profile,
which requires internal rotation; in addition, the cross-table lateral
must also not have a rotational component. It is quite difficult to
obtain these radiographs in the emergency room setting. Once the
patient is taken to surgery, repeat the AP and lateral plain films, or
obtain good fluoroscopic views with the patient on the fracture table
and the hip positioned for ideal radiographic views.
none of them take into account the maximum displacement that occurred
at the time of injury, the degree of vascular or capsular damage, or
the amount of comminution of the posterior femoral neck, which makes
the fracture more difficult to reduce and much more unstable (6).
in the elderly; therefore, the history is usually one of a slip and
fall and landing on the side, resulting in a direct blow to the lateral
aspect of the greater trochanter. Pathologic fractures are suggested
when the patient’s hip suddenly “gives way” during normal activities of
daily living, associated with sudden severe pain, which then leads to a
fall. Fractures of the femoral neck in young active adults are rare and
nearly always due to high-energy trauma. In all fractures of the
femoral shaft, a concomitant ipsilateral fracture of the femoral neck
must be suspected (as discussed in Chapter 20).
The past medical history, the social and family history, and a review
of systems are very important, as indicated in the previous discussion
on epidemiology. Associated diseases and social circumstance have a
major influence on the outcome in fractures of the femoral neck and
must be considered early for discharge planning.
excessive external rotation. The hip is tender, and any motion usually
produces severe pain. A gentle blow to the bottom of the heel usually
results in hip pain. Because the fracture is intracapsular and the
capsule is usually intact, the amount of external rotation and
shortening seen is much less than that seen in intertrochanteric
fractures or fractures of the shaft. In the latter, shortening of an
inch or more may be present, and the lateral border of the foot lies
completely flat on the examining table. In neck fractures, shortening
is usually less than 1 inch and the degree of external rotation does
not usually allow the foot to lie completely flat on the tabletop
unless the hip is abducted. Usually there is not much swelling, and
large ecchymosis or hematomas such as seen in intertrochanteric or
subtrochanteric fractures is not usually found. The surrounding hip
joint capsule limits bleeding from the fracture; therefore, anemia is
rarely a problem.
with approximately 5 pounds (2.3 kg), with the foot in neutral
rotation, the knee and hip slightly flexed, and the calf supported on
one to two pillows. This immediately increases patient comfort and
places the fracture in a more anatomic position, which minimizes
distortion of the vessels providing the blood supply to the femoral
head. The flexed position helps accommodate the increased intracapsular
pressure that might be present from a hematoma. Immediate AP and
cross-table lateral radiographs will confirm the diagnosis. It is
important to plan the preoperative workup and radiography to minimize
moving the patient, because transfers are painful and risk further
comminution of the fracture.
a threat to the blood supply to the femoral head remains somewhat
controversial (70), I routinely place an
18-gauge or larger-diameter needle into the hip joint through either a
lateral or an anterior approach to detect and aspirate any hematoma,
but more important, to inject 5 ml of 0.5% Bupivacain without
epinephrin. This usually provides dramatic pain relief and permits
gentle further reduction of the fracture in the Buck’s traction, if
indicated.
fixation is indicated, so immediate consultation with the primary-care
physician or a medical consultation is indicated to clear them for
surgical treatment.
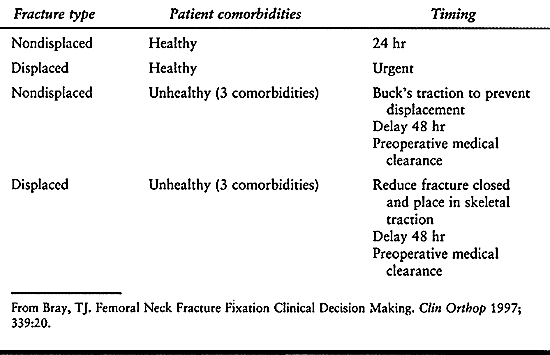
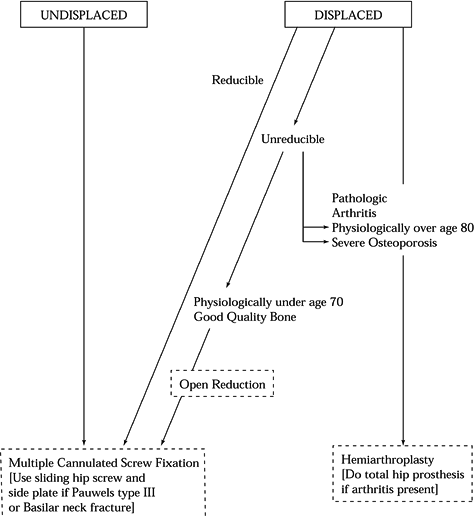
based on whether the fracture is displaced, and on the health of the
patient (16) (Table 19.3). Zuckerman et al. (160)
showed that healthy patients with two or fewer comorbidities did better
if the hip was treated within 48 hours of admission, whereas unhealthy
patients with three or more comorbidities benefited from delay in
surgery to treat comorbidities, which reduced the incidence of
postoperative medical complications. In healthy patients with
nondisplaced fractures, perform internal fixation ideally within 24
hours but no later than 48 hours to avoid the complications of
prolonged immobilization. In healthy patients with displaced fractures,
particularly where salvage of the femoral head with internal fixation
is to be performed, take the patients to surgery urgently because early
anatomic reduction and internal fixation optimizes the conditions for
preservation of the blood supply to the femoral head. In unhealthy
patients with three or more comorbidities, whether the fracture is
displaced or undisplaced, treatment in Buck’s traction as outlined
previously and thorough medical workup and treatment of comorbidities
are indicated prior to surgical treatment.
 |
|
Table 19.3. Timing of Fixation
|
can be treated in skeletal traction utilizing a proximal tibial or
distal femoral traction pin with an internal rotation component to the
traction to reduce the fracture. Because these fractures often require
6 months to heal, this is rarely practical. I have not used
nonoperative treatment in traction
for
a femoral neck fracture in the past 30 years. In the elderly, when
operative treatment is not possible, it is usually better to abandon
treatment of the fracture and mobilize the patient as symptoms permit.
Many of these patients are very sedentary or confined to nursing homes,
so they will often go on to a relatively pain-free nonunion, which is
compatible with their level of function. The other alternative is a
head and neck resection, but the decision to perform this procedure is
usually best delayed to see how the patient does with simple neglect of
the fracture.
stable fractures that were impacted into moderate valgus could be
successfully managed nonoperatively with initial traction for
symptomatic relief followed by limited protected weight bearing.
Bentley (9), however, showed in his series that
16% of stable fractures treated nonoperatively subsequently displace,
resulting in a much worse prognosis. For that reason, the nonoperative
treatment of stable impacted femoral neck fractures is of historical
interest only. The low morbidity of percutaneous cannulated screw
fixation of these fractures is such that the benefits of surgical
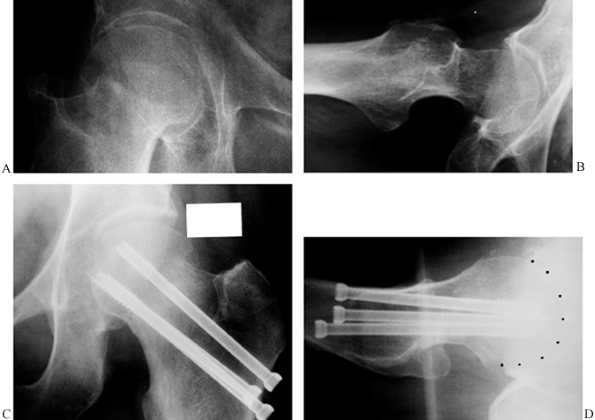
stabilization far outweigh the risks (Fig. 19.5).
 |
|
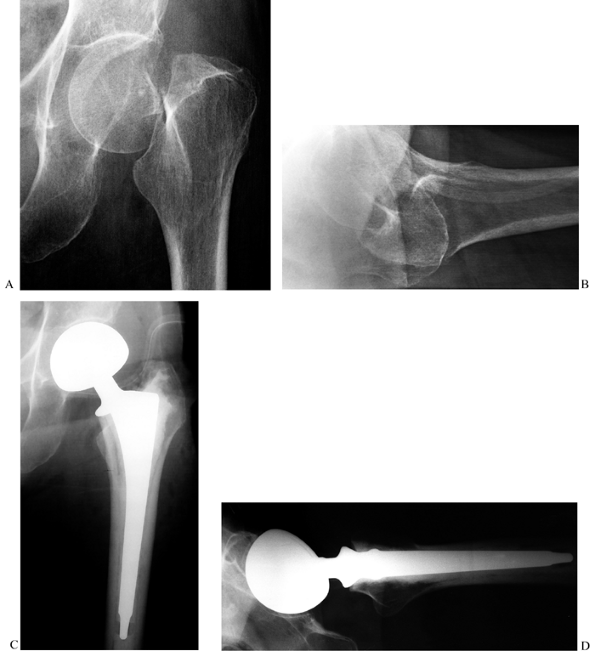
Figure 19.5. Percutaneous cannulated screw fixation of an impacted, Garden stage I, subcapital hip fracture. A: AP radiograph of the hip fracture prior to fixation. B: Lateral radiograph. C: AP radiograph after cannulated screw fixation. D: Lateral radiograph; ideally, the screws could be spread out somewhat more and be more parallel.
|
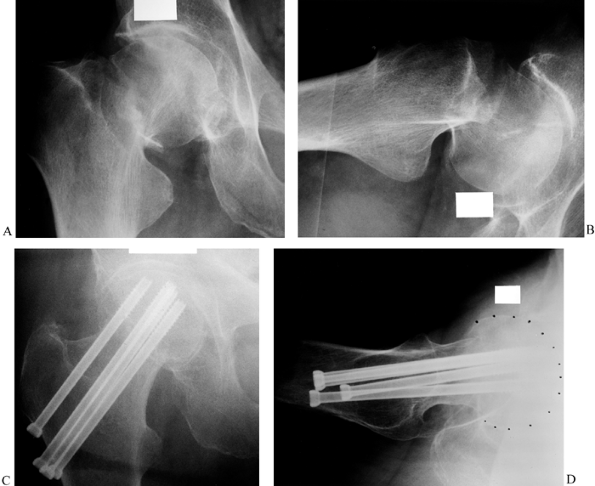
fractures, whether displaced or undisplaced, with internal fixation
rather than prosthetic replacement (Fig. 19.5, Fig. 19.6). Even in displaced fractures such as a Garden stage IV where treatment is delayed, good internal fixation in anatomic
position usually results in union of the fracture even though the
incidence of avascular necrosis may be 40% or more. This means that up
to half of these patients may have a satisfactory outcome, which is
always superior to an arthroplasty, in both the short and the long
term. In addition, if these patients are followed closely, subsequent
conversion to an arthroplasty, if required, is not compromised.
 |
|
Figure 19.6. Cannulated screw fixation of a displaced subcapital hip fracture: A: AP radiograph showing a fully displaced Garden stage IV subcapital fracture. B: Lateral radiograph of the displaced fracture. C: AP radiograph after closed reduction and cannulated screw fixation. D: Lateral radiograph after fixation.
|
run if their fracture heals; they experience no avascular necrosis, and
they retain their own femoral head. Because modern techniques of
percutaneous, multiple-cannulated-screw fixation has a low morbidity, I
feel that fixation is indicated in all nonpathologic, displaced
fractures regardless of the patient’s age, assuming that their bone
quality is sufficiently good that the screws can be expected to hold.
The controversy as to whether to perform internal fixation or
prosthetic replacement arises for patients 65 years of age or more (127).
People are living much longer today and, as a result of better living
conditions and health care, are physiologically quite young in their
middle 60s and are remaining athletically active into their middle 70s
and occasionally even into their early 80s. For that reason, the
decision of whether to internally fix or replace a displaced
femoral
neck fracture should be based on life expectancy, the presence of
chronic disease, bone quality, and level of function at the time of
fracture, as well as on expected function. In our practice, this means
that we commonly internally fix displaced fractures in active
70-year-olds who have no comorbidity, and we reserve prosthetic
replacement for patients who are physiologically in their 80s (64). In a meticulous review of the literature on fractures of the femoral neck, Swiontkowski (134)
stated that major deficiencies in the design of most studies did not
permit a meta-analysis of the literature to prove whether primary
internal fixation or a prosthetic replacement in older patients
provided the best results (5,19,31,57,62,65,67,68,69,70 and 85,86,101,107,123,127,153).
other institutions, and a review of the literature, I have drawn the
following conclusions regarding this controversy:
-
In community-based practices in North
America, the vast majority of displaced femoral neck fractures in
patients over 65 years of age are currently treated with
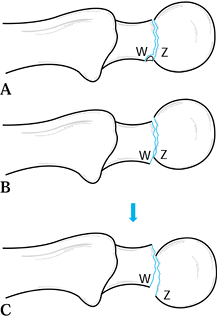
hemiarthroplasty (Fig. 19.7).![]() Figure 19.7. Hemiarthroplasty for a week-old Garden stage IV subcapital fracture of the femoral neck. A: AP radiograph showing a fully displaced fracture with some erosion of the head and femoral neck due to delay in fixation. B: Lateral radiograph. C: AP radiograph after cemented bipolar hemiarthroplasty. D: Lateral radiograph.
Figure 19.7. Hemiarthroplasty for a week-old Garden stage IV subcapital fracture of the femoral neck. A: AP radiograph showing a fully displaced fracture with some erosion of the head and femoral neck due to delay in fixation. B: Lateral radiograph. C: AP radiograph after cemented bipolar hemiarthroplasty. D: Lateral radiograph. -
Although more displaced fractures are
treated with internal fixation at academic trauma centers, the art of
successful closed reduction, in my opinion, is being lost because of
the default to arthroplasty. -
In most published series, the early
complication rate, including infection, other wound complications,
dis-location of the prosthesis, and medical complications, are higher
after hemiarthroplasty than after multiple-percutaneous-screw fixation (16,67,69,70,74,86,101,123,127). -
Because of average reported incidences of 16% for avascular necrosis and 32% for nonunion in the series of Söreide et al. (127),
the need for reoperation after internal fixation was 35% at 2 years,
compared to an average incidence of revision of arthroplasty of between
12% and 15%. This means that approximately 65% of patients after
internal fixation either have a successful outcome, or failure of their
fixation does not result in sufficient symptoms to require revision
surgery. In more active patients between 65 and 75 years of age, this
may well be acceptable because of the advantages of retaining the
patient’s own hip in this group. -
Rehabilitation after internal fixation,
in spite of perceptions to the contrary, is usually faster because,
with a good reduction and stable fixation, immediate weight bearing and
rehabilitation can be instituted. The same is true in hemiarthroplasty,
but the larger incision and risk of redislocation makes rehabilitation
slower.
have been used in the past; however, today most surgeons prefer three
to four 5–7 mm in diameter lag screws utilizing cannulated screw
techniques because of the advantages of placing guide pins prior to the
screws (135). Various types of compression hip
screws have also been used. I use three cannulated screws routinely and
reserve the standard compression hip screw for high shear angle
fractures in young vigorous patients for whom the stronger device is
needed to resist deforming forces across the fracture site. I will
often augment the latter with a 6–7 mm cannulated screw to improve
rotational control. In patients with severe osteoporosis, augmentation
with apatite cements has been used to increase the strength of the
fixation construct, but at this time this is an experimental technique (59).
or the newer bipolar prosthesis, including those that can be converted
to a total hip. These are available in both cemented and noncemented
versions (Fig. 19.7).
-
Inability to achieve a satisfactory reduction when open reduction with preservation of the femoral head is not indicated
-
Severe neck comminution that precludes a satisfactory outcome
-
Some pathologic fractures
-
Coexisting arthritis
contractures, or poor motor control have been mentioned as indications
for arthroplasty; however, the increased incidence of dislocation in
this group may in some cases make internal fixation a better choice.
Kenzora et al. (74), in a prospective outcomes
study, compared noncemented unipolar prostheses to cemented or
press-fit bipolar prostheses. Patients with the bipolar prostheses had
better pain relief and function compared to the unipolar prostheses at
2 years follow-up. The total cost of the bipolar was approximately 30%
more than the unipolar. Cornell et al. (26), in
a smaller study comparing cemented unipolar and bipolar prostheses, at
6 months follow-up found no differences in hip rating outcomes;
therefore, they suggested that the less expensive unipolar prostheses
might be justified. Neither study addressed the issue of whether
conversion to total hip arthroplasty was easier, or less expensive,
with the bipolar prosthesis designed for conversion to a total hip.
Based on personal experience and a review of the literature, I have
drawn the following conclusions regarding this controversial issue:
-
In patients with a limited lifespan or
who have low functional demands, a unipolar prosthesis is less
expensive and less likely to dislocate, and it provides satisfactory
function. -
A cemented bipolar prosthesis offers
optimal function and is more important in the younger group of
patients, for whom eventual conversion to total hip arthroplasty might
be necessary. A bipolar that offers conversion to total hip
arthroplasty without removal of the femoral stem should be used. -
Total hip arthroplasty is indicated only
in patients with coexisting arthritis or pathology of the acetabulum
that makes a hemiarthroplasty impractical (124).
view of the revision rate of hemiarthroplasty previously mentioned, but
I do not subscribe to that approach at the present time (23,26,33,55,66,72,108,123,137). An algorithm for the decision-making cascade is presented in Figure 19.8.
 |
|
Figure 19.8. Treatment of adult subcapital hip fractures.
|
-
Administer a general or regional
anesthetic. When this is contraindicated, the procedure can be done
under local anesthesia in a cooperative patient; use conscious sedation
supervised by an anesthesiologist. -
Gently transfer the patient to an orthopaedic fracture table that is compatible with the use of a fluoroscope.
-
In undisplaced fractures, and in those in satisfactory
P.629
position for fixation when a reduction is not required, place the
affected hip in neutral abduction, in neutral flexion–extension, and in
sufficient internal rotation to place the femoral neck parallel to the
floor, assuming that this will not displace the fracture. Apply only
enough traction to stabilize the limb on the table while avoiding
disimpaction of the fracture site. Fractures that have good apposition
but are simply angulated beyond the desirable range can often be
reduced in this manner without a formal reduction maneuver, as
described next. -
In fully displaced fractures, use the following protocol:
-
It is critical in the reduction of
displaced fractures to have the pelvis completely stable on the
fracture table. This is best achieved by putting both lower extremities
in longitudinal traction. -
Using a perineal post in the groin,
secure both feet firmly into traction stirrups, padding the feet well
to avoid bruising or injury to neurovascular structures. Abduct the
uninvolved hip to 45° or as needed to allow access for the C-arm
fluoroscope, and place the limb in sufficient traction to tip the
pelvis slightly toward the unaffected hip. If an adduction contracture
of the hip precludes placing this limb in abduction-traction, then
place it in a 90°-90° leg holder, but stabilize the pelvis by padding
and binding the thigh to the vertical post of the leg holder. A
separate post mounted on the fracture table above the iliac crest of
the uninvolved hip will work as well, if available (Fig. 19.9).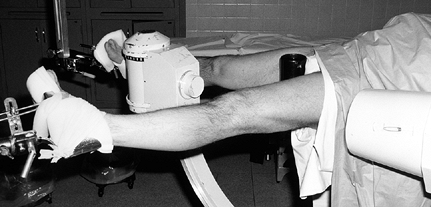 Figure 19.9.
Figure 19.9.
Patient on a fracture table for percutaneous screw fixation of a
subcapital hip fracture. Note that the uninvolved hip is in traction
and abducted 45°, permitting access for the C-arm. The fractured limb
is in the reduced position with the lower extremity in line with the
body and internally rotated to bring the femoral neck level with the
floor. The C-arm fluoroscope is best located between the legs. -
Bring the fluoroscope in between the
legs. Make certain that good-quality AP and lateral images of the
fractured hip are obtainable. Lock the base of the fluoroscope and
adjust it so that both views can be obtained without having to shift
the position of the base. -
Gently place sufficient traction on the fractured hip to pull it out to length and disengage the fracture fragments.
-
Place the hip in approximately 45° of abduction and 45° of external rotation.
-
Then gently and slowly adduct the hip to
neutral while simultaneously internally rotating the hip to bring the
femoral neck parallel to the floor. Having an assistant provide a
lifting and internal rotation pressure on the greater trochanter may
assist in the reduction.
-
-
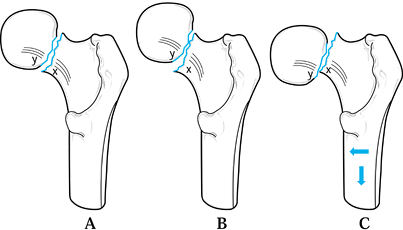
Now visualize the hip on an AP view (Fig. 19.10). One of three situations will usually be present. The fracture may be anatomic (Fig. 19.10A), or there may be a valgus reduction (Fig. 19.10B), where the femoral neck is supporting the femoral head. Note that point X on the neck lies somewhat medial and distal to the matching point Y on the head. As long as the valgus angle does not exceed 15°, either of these positions is acceptable.
P.630
Excessive valgus interferes with the ability to place the screws. This
can be eliminated by easing off on the traction. If the fracture is in
varus (Fig. 19.10C), where point X lies lateral and superior to point Y, then further reduction is necessary using the maneuver described next.![]() Figure 19.10. Reduction of a subcapital fracture on the AP view. A: Anatomic reduction. B: Valgus reduction. Notice that the femoral neck supports the head. This is acceptable. C:
Figure 19.10. Reduction of a subcapital fracture on the AP view. A: Anatomic reduction. B: Valgus reduction. Notice that the femoral neck supports the head. This is acceptable. C:
Varus reduction. There is no support of the femoral head by the neck.
Do not accept this reduction. Convert this to anatomic reduction (A) or
valgus reduction (B) by applying traction and pushing the femoral shaft
medially, as indicated by the arrows. -
Under fluoroscopic control, pull additional traction to bring point X even with or slightly distal to point Y, then displace the neck medially to bring point X slightly medial to point Y
to provide support for the femoral head. Achieve this by stabilizing
the femoral shaft with a hand on the medial side of the knee, while
pushing on the greater trochanter with the other hand to drive the
femoral neck beneath the head (Fig. 19.11). Do this using frequent spot images on the fluoroscope to control the reduction and to avoid comminution of the neck. Figure 19.11.
Figure 19.11.
Reduction maneuver for varus position on the AP view. Apply traction
and then shift the femoral neck medially beneath the femoral head by
supporting the medial aspect of the knee with one hand and pushing on
the trochanter with the other as illustrated. -
With this maneuver, sometimes the neck
will not remain in the reduced position because of excessive traction.
To stabilize the reduction in that situation, hold the fracture reduced
and release the traction enough to engage the fracture fragments. -
Now look at the fracture on the lateral view. Normally you will see one of the three situations illustrated in Figure 19.12. The fracture may be anatomic (Fig. 19.12A), or the fracture may be reduced in a stable configuration, with point W
representing the posterior proximal corner of the femoral neck,
displaced posterior to and supporting the posterior corner of the
femoral head as represented by Z (Fig. 19.12B).
As long as the neck is not posteriorly displaced more than 15% of the
width of the neck at the fracture, this position is acceptable.![]() Figure 19.12. Reduction of a subcapital fracture on the lateral view. A: Anatomic reduction. B:
Figure 19.12. Reduction of a subcapital fracture on the lateral view. A: Anatomic reduction. B:
Neck posterior reduction. This is acceptable because the neck supports
the femoral head and prevents it from collapsing posteriorly. C:
Neck anterior reduction. This is unacceptable. Convert it to anatomic
reduction (A) or neck posterior reduction (B) by pushing the shaft
posteriorly. -
If, however, point Z on the femoral head lies posterior to point W
on the femoral neck, particularly if there is any comminution of the
posterior neck, then this position is unstable and further reduction is
necessary (Fig. 19.12C). To solve this problem,
place your hand directly over the intertrochanteric region on the
anterior surface of the hip and gently push the proximal femoral shaft
posteriorly (Fig. 19.13) to obtain an anatomic or slightly overcorrected position (Fig. 19.12A, Fig. 19.12B). Figure 19.13.
Figure 19.13.
Reduction maneuver for displacement on the lateral view. To provide
support for the femoral head posteriorly, push the shaft posteriorly
with the palm of your hand located over the proximal femur as
illustrated. -
If the fracture will not remain in the
reduced position because of excessive traction, use the technique just
described to engage the fracture fragments in the reduced position. -
Once a final position is obtained on the
lateral view, return the C-arm to the AP view to verify that the
reduction has not been lost on this view. -
Acceptable ranges of angulation after
reduction are 130° to 150° of valgus on the AP view, and less than 15°
of either anterior or posterior angulation on the lateral view. -
Insertion of the initial guide pin for
the cannulated screws is greatly facilitated by having the femoral neck
parallel to the floor. This provides a reference for pin
P.631
insertion
on the lateral view. Place a Kirschner (K) wire as a radiopaque guide
on the anterior aspect of the hip for guidance in the AP view. When
using a percutaneous technique, this also helps to localize the site of
the incision used for inserting the guide pins and screws. -
Sterilely prep the hip and, under
fluoroscopy, lay a 0.062 mm K-wire on the anterior aspect of the skin
of the hip so that it subtends an angle of 130° with the femoral shaft
and is located directly over the middle of the femoral head and neck.
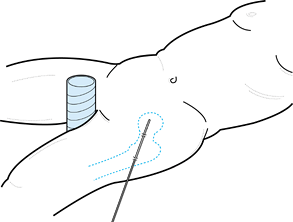
Once this location is established, mark it. Then pierce the K-wire into
and out of the skin on the anterolateral aspect of the hip, securing
the pin with a section of skin approximately 5 mm in length. Do the
same maneuver at the tip of the pin over the femoral head. This will
secure the K-wire and prevent it from shifting. The distal end of the
K-wire then marks the region for the skin incision, which can be
marked. Then cut off the excessive projection of the pin laterally,
leaving the K-wire on the anterior aspect of the hip (Fig. 19.14).![]() Figure 19.14.
Figure 19.14.
A K-wire pierced through the skin in two places on the anterior surface
of the thigh in line with the femoral neck, as seen on the fluoroscope
image, provides a guide to the incision and fixation. -
Now sterilely drape. I prefer the fully
transparent, lateral wall drape because the ability to fully visualize
the patient and the C-arm greatly facilitates orientation for placement
of the guide pins. It also facilitates communication with the x-ray
technician who will be standing behind this drape. -
Make a longitudinal skin incision on the
mid-lateral aspect of the thigh approximately 2–3 cm in length, and
incise the underlying subcutaneous fat and deep fascia in line with the
angle of the K-wire. -
Use a Cobb elevator to further establish
the hole in the fascia and to longitudinally split the muscles down to
the femur, where a small amount of periosteal elevation can be done to
expose the bone just below the greater trochanter on the lateral cortex
where the guide pins and screws will enter. -
Insert three or more guide pins or
cannulated screws. I prefer titanium lag screws, 6–7 mm in diameter and
self-tapping. The somewhat larger diameter provides additional
strength, but more important, it allows the use of a larger guide pin
that is stiff enough to prevent deflection during insertion. -
The details of insertion of guide pins and screws depends on the manufacturer, but the general principals are as follows:
-
The configuration of screw placement I strive for is illustrated in Figure 19.15. Swiontkowski (134)
has shown that three screws provide sufficient stability, and that four
or more screws are usually not necessary. This minimizes the number of
screws and maximizes the surface area available for healing and
revascularization. The keystone position is screw 1, which is placed in
the midline on the lateral view and 5–10 mm proximal to the inner
cortex of the medial femoral neck on the AP view. Insert this guide pin
first, staying parallel to the guide K-wire and maintaining an angle of
approximately 130°. This position is less likely to disrupt the
reduction, and it is a good position for securing the reduction.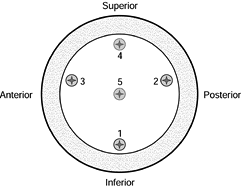 Figure 19.15.
Figure 19.15.
Screw positions for fixation of femoral neck fracture as seen on a
cross section of the femoral neck. Keep all screws in the inner
two-thirds of the head to avoid accidental penetration of the articular
surface of the femoral head. Try to use positions 1, 2, and 3, inserting the guide pins and screws in that order. If more than three screws are desired, use positions 4 and 5. Caution: Site 4 is the most risky for injuring the extraosseous blood supply to the head. -
Next, place guide pin 2, which is important to support the posterior neck.
-
Place guide pin 3. In Figure 19.15,
screw positions 2 and 3 are shown in the midsection of the femoral
head, but they can be placed more superiorly if more spread between the
screws is desired. -
Guide pin positions 4 and 5 are usually
not necessary, but if additional fixation is required, place 4 next and
then 5. Position 4 is good for neutralizing tension across the superior
aspect of the fracture, but usually it is not placed because of the
risk of injury to the blood supply to the femoral head if the superior
cortex were accidentally penetrated. -
To avoid accidental penetration of the articular surface, keep the guide pins within the central two thirds of the head (93), as shown in Figure 19.15.
-
I prefer to use guide pins that have a
threaded tip that can be secured into the subchondral bone of the
femoral head; then I drill for the screw 5–10 mm short of the tip of
the guide pin. This helps prevent dislodgement of the guide pin on
removal of the drill. -
Measure for the depth of the drill and screw length.
-
Now overdrill the guide pin with the
drillpoint specified by the manufacturer for the screw being used. Do
this under direct fluoroscopic control to avoid accidental penetration
of the hip and/or loss of the guide pin.Do not use the screws to apply
the initial compression. With the three guide pins in place and before
inserting the screws, loosen the traction somewhat and impact the
fracture by pounding directly on the greater trochanter. Visualize this
on the fluoroscope. At this point, measure for screw length and then
in-sert the screws and washers, compressing the fracture site (Fig. 19.6). -
Select a screw length that will permit
compression of the femoral neck while placing the tip of the screw no
closer than 7 mm to subchondral bone. Now insert the appropriate-length
lag screw with a washer, being certain that the screw threads do not
lie across the fracture site. -
Remove the guide pins, irrigate the wound, and close in layers.
-
Prior to breaking sterile technique, obtain AP and lateral radiographs.
P.632 -
closed reduction maneuvers as described, and if the patient is
sufficiently young and healthy that internal fixation rather than
hemiarthroplasty is indicated, perform an open reduction. The usual
cause of failure of reduction is severe comminution of the femoral
neck, which usually occurs posteriorly. The key to success of open
reduction is the avoidance of further damage to the blood supply to the
head, achievement of a stable anatomic reduction, and good stable
fixation in good-quality bone. Because of the threat to the blood
supply of the head caused by any type of bone grafting of the
comminution of the posterior neck, do not bone graft the femoral neck.
-
For this procedure, leave the patient on the fracture table with the fracture in the best-reduced position obtainable.
-
Prep the hip and then use traditional
draping rather than the translucent drape sheet. Sterilely drape the
head of the fluoroscope so that it is available throughout the
procedure. -
Expose the lateral aspect of the greater trochanter and the hip through a Watson-Jones approach (Chapter 3).
Expose the femoral neck through a longitudinal anterior midline
incision in the hip joint capsule parallel to the femoral neck. “T”
this at the base of the femoral neck only enough to visualize the
fracture for reduction. -
Irrigate the hip to remove any blood clots and to provide good visualization of the femoral neck fracture.
-
Now reduce the fracture by direct
manipulation of the femoral neck under direct visualization, using the
C-arm and the traction arm of the fracture table, which is manipulated
by an assistant surgeon. This direct manipulation must be gentle and it
must avoid disruption of the lateral epiphyseal vessels or any other
soft-tissue connections to the femoral head. The pointed pusher from
the pelvic fracture tray and small elevators are helpful. I almost
never use reduction forceps. If forceps are necessary to grasp the
femoral neck, use only a large pointed tenaculum forceps on a portion
of the neck where injury to the blood supply will not occur.
-
Place the femoral neck parallel to the
floor to facilitate insertion of the screws. In some fractures, more
internal rotation may be necessary to reduce posterior angulation at
the fracture on the lateral view because of posterior neck comminution. -
If the overall alignment of the fracture
is satisfactory, with the exception of residual posterior tilt of the
head caused by posterior neck comminution, this tilt can often be
reduced by placing the first guide pin along the posterior neck using
the guide pin to push the head into acceptable position. -
If, after the reduction sequence just
described, the fracture remains in unsatisfactory position on either
view, then repeat the entire sequence once more. If satisfactory
reduction is not present after that, proceed with either open reduction
or hemiarthroplasty. -
Insertion of guide pins can be difficult
because they tend to “walk” along the femoral shaft when power is
activated. Palpate the lateral cortex of the femur with the guide pin
anteriorly and posteriorly to be certain that the initial guide pin is
directly in the center of the shaft. Verify the location of the entry
point of the guide pin and begin initially with the guide pin at right
angles to the longitudinal axis of the femur. Once the guide pin has
entered the cortex just barely enough to obtain purchase, but before
penetrating so deep that its angle cannot be changed, align the guide
pin on the AP and lateral views. -
The surgeon can easily judge alignment on
the AP view, but the nurse or an assistant must visualize the guide pin
on the lateral projection to keep it parallel to the floor. -
Once all three guide pins are fully
inserted, it often saves time to next impact the fracture, because then
the initial measurement of screw length will be more accurate. -
In hard cortical bone, tapping of the
lateral cortex and/or the femoral head may be necessary prior to
insertion of the screw. Avoid inserting screws where excessive torque
is required, because this may displace the fracture. -
Always use washers on the screws to
permit compression of the fracture and to avoid penetration of the
lateral cortex by the screw head. -
Do not place screws at more than 135° of
valgus because this narrows the cross-sectional area of the femoral
neck available for screw insertion and may necessitate entry of the
screws at or below the lesser trochanter, which increases the risk of
subtrochanteric fracture (117). -
Take time to ensure that the entry of
each guide pin and screw is perfect, because mistakes requiring
additional unused drill holes in the lateral aspect of the femur
predispose the patient to subtrochanteric fracture. -
If a screw must be changed, insert the
guide pin back into the screw before the change because this greatly
facilitates location of the hole in the lateral cortex and ensures that
the screw passes down the same track. -
When there is any question about the
quality of reduction or location of the screws, examining the hip on
the AP view under direct live fluoroscopy by rotating the hip through a
full range of motion provides a three-dimensional visualization of the
hip that is very helpful.
-
Because these fractures are very
unstable, it is often necessary to manually reduce the fracture and
then hold it while an initial guide pin is placed by an assistant
surgeon, as previously described. Once one guide pin has been placed,
the fracture usually is stable and the insertion of fixation screws can
proceed as described for closed percutaneous fixation. -
In young patients with a high-shear-angle
(Pauwels’s type III) transcervical or basilar neck fracture, a
compression hip screw with side plates may be indicated. The screw and
plates are inserted with the technique described in Section C of this
chapter on intertrochanteric fractures. -
Keep the hip joint capsule open until
internal fixation is completed, because this will ensure maintenance of
reduction and will assist in the visualization of placement of the
fixation. -
Obtain final radiographs prior to wound closure, and then irrigate the wound, place a suction drain, and close in layers.
mobilized to a bedside chair the day after surgery and can begin
immediately to walk using a walker or crutches. Assuming that the
reduction is stable, fixation good, and bone stock acceptable, most
elderly patients can be allowed to bear weight as tolerated. Most
patients will voluntarily begin with the weight of the leg and by 6
weeks will be capable of full weight bearing with assistive devices,
although most elderly patients will continue to use assistive devices
for a number of additional months until they regain muscle strength and
endurance, and the fracture is healed. There is no point in keeping
these patients non-weight-bearing because the simple maneuvers of
getting on a bedpan, getting out of bed, and rising from a sitting
position in a chair subject the internal fixation to the same forces as
nonassisted full weight bearing (3).
when the patient slides the affected lower extremity along the floor
without activating hip musculature. This is best achieved by weight
bearing to the weight of the limb, combined with the use of a walker or
crutches. The latter regimen should be used in younger persons with
unstable fracture patterns until fracture healing occurs at about 6
months. We monitor patients with physical examination and radiographs
at 6 and 12 weeks, 6 months, and 12 months after injury and then follow
them yearly as needed. Avascular necrosis can occur even 2 years or
more after injury.
fixation of fractures of the femoral neck include avascular necrosis,
which, in large series including all grades, occurs in approximately
25% of fractures; nonunion, which in large series occurs in up to 25%;
and early failure of fixation. Because percutaneous techniques are
used, infection is uncommon, but it can occur. Most other complications
are related to perioperative medical problems.
generally require prosthetic replacement. For a discussion of the
treatment of nonunions of the femoral neck in younger patients, see Chapter 29.
Infection after internal fixation generally does not result in
osteomyelitis or pyarthrosis and can be treated with irrigation and
debridement of the wound, delayed primary closure after debridement,
and an appropriate course of intravenous bacteriocidal antibiotics
based on the results of culture. In most cases, the fixation implants
can be left in place. If pyarthrosis or osteomyelitis occurs, then
failure of fixation normally results, and head and neck resection as a
definitive procedure or followed by late total joint arthroplasty is
usually required. For complications following hemiarthroplasty, see Chapter 105.
mortality rates associated with these fractures varies from 10% to 30%
within the first year of injury (9). One year
after hip fracture, the life expectancy of the patient returns to the
normal value for the age group. In general, there is a slightly greater
mortality rate for intertrochanteric fractures than for intracapsular
fractures; this is because of the advanced age of patients who suffer
intertrochanteric fractures. Patients who are in nursing homes before
the fracture have the highest morbidity and mortality rate (30%) and
are least likely to resume ambulation (71). In
the socially independent population, most patients recover to their
previous levels of functioning if complications do not occur.
patients with intertrochanteric fractures are significantly older, more
likely to be limited to home ambulation, and more dependent in their
activities of daily living; therefore, they tend to have an overall
poorer prognosis (77,78).
peritrochanteric area about the insertion site of the abductor
musculature, a region with a very generous blood supply. Marked
bleeding may result after fracture, so watch carefully for excessive
blood loss. The nonunion and avascular necrosis rate in
intertrochanteric fractures is less than 1% because of the ample blood
supply in this region.
comminution, a large fragment of the posteromedial wall of the femur,
often including the lesser trochanter, splits free. This bony buttress
is important to the stability in the intertrochanteric region;
therefore, its comminution results in an unstable fracture.
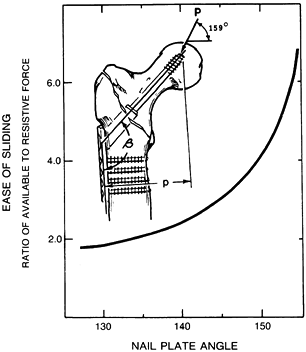
fractures, it is essential to understand the mechanics of the devices
and the forces that they must withstand. The magnitude and direction of
the force exerted across the hip joint are dictated by body weight and
the muscles acting on the hip. Pauwels (97) and others (46,69,96,110) showed that the forces acting on the hip in single-limb stance amount to about three times the body weight applied
at an angle of 159° to the vertical plane. This same force acts on any hip fixation device placed across the fracture site.
this force vector allows optimal sliding of the hip screw and impaction
of the fracture. The closer the nail-plate angle is to the resultant
force across the hip, the more force is available to assist impaction (82) (Fig. 19.16).
Devices of lower angles are subject to lower forces parallel to the
sliding axis of the device and greater forces perpendicular to the
axis; these perpendicular forces act to jam or bend the device, thereby
preventing impaction. Technically, however, the surgeon cannot place
the sliding device at an angle greater than 150°. It is desirable
mechanically to place the sliding fixation device at as high an angle
as clinically possible and still maintain placement of the fixation
device in the center of the femoral head to prevent cutout. Fixation of
the medial fragment, particularly if it is large, allows bony impaction
and creates a stable osteosynthesis with less shortening. For this
reason, in addition to bony impaction with a higher-angle device,
interfragmentary fixation of a large medial fragment is desirable when
possible.
 |
|
Figure 19.16.
The ratio of available to resistive forces for the initiation of sliding, plotted against nail-plate angle (β), assuming a constant applied load (P) and constant offset (p), for the fracture shown in the inset. |
not overshadow the need for a secure purchase in the center of the
femoral head (81) (Fig. 19.17).
If you cannot effectively place a high-angle device deep into the
center of the femoral head, use a lower-angle device to obtain optimal
placement in the head. The lower-angle devices must be used in patients
who are small and have varus hips. Most sliding devices are available
in 5° increments at the nail-plate junction; in unstable fractures,
select the highest angle that allows center head placement. This
optimizes both fixation of the fracture and ease of sliding the device,
allowing impaction of the fracture fragments.
 |
|
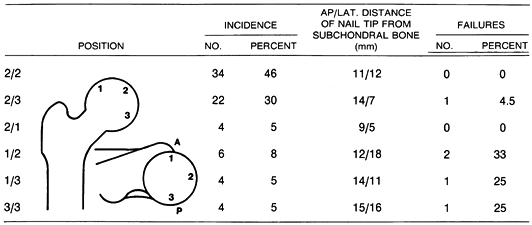
Figure 19.17. Failure rate versus nail position in Kyle type III fractures.
|
addition to emphasizing the importance of central placement of the
screw combined with a 150° angle plate, showed the importance of
reestablishing bony contact between the femoral shaft and the main head
and neck fragment medially. In their cadaveric study, they accomplished
this with a limited osteotomy of the greater trochanter.
more recent clinical experience with newer sliding hip screws has not
demonstrated an advantage of osteotomy over anatomic reduction or use
of a valgus reduction
and high-angle nail to restore the medial buttress (36,54).
Equally important, addition of an osteotomy has been found to increase
operating time, blood loss, and contribute to excessive shortening and
occasionally external rotation of the extremity. Introduction of the
Medoff sliding plate, which achieves compression not only along the
femoral neck but also along the longitudinal axis of the femoral shaft,
has not shown improved results over traditional compression hip screws,
and the added complexity of the device may add to longer operating
times and increased blood loss (147).
today is the head and neck fragment cutting off the hip screw, due to
severely osteoporotic bone in the very elderly or in those with
metabolic bone disease. Fatigue failure of sliding screws occurs but is
rare (128). This observation has been echoed by others (155).
Modi-fication of the traditional hip screw by replacement of the screw
with a dome plunger (Alta, Stryker-Osteonics-Howmedica, Rutherford, NJ)
uses the principle of an expandable molly bolt, which resists cutout by
compressing the cancellous bone of the femoral head around the
expandable dome, by providing a larger smooth surface area rather than
sharp threads, and by providing a mechanism for delivery of bone cement
that integrates the dome plunger with the cancellous bone of the
femoral head. The dome plunger alone fails at a load 50% higher than
that of stainless steel lag screws. Adding cement augmentation supports
higher loads, and it eliminates failure by cutout through the femoral
head (21) (Fig. 19.18). Intramedullary fixation devices, which combine a hip screw with either a short or long intramedullary nail such as the
Gamma nail (Stryker-Osteonics-Howmedica, Rutherford, NJ), have the
theoretical advantages of percutaneous insertion, a lower bending
moment on the fixation device, and an intramedullary buttress that
precludes excessive medial migration of the shaft. Biomechanical
comparison of intramedullary devices to sliding hip screw devices have
not demonstrated any distinct advantage of one system over the other;
however, the intramedullary devices transmit progressively decreasing
loads to the proximal femur with increased instability of the fracture,
and failure of the intramedullary devices occurred through the distal
cross-locking holes when short-stemmed devices were used (87,109).
 |
|
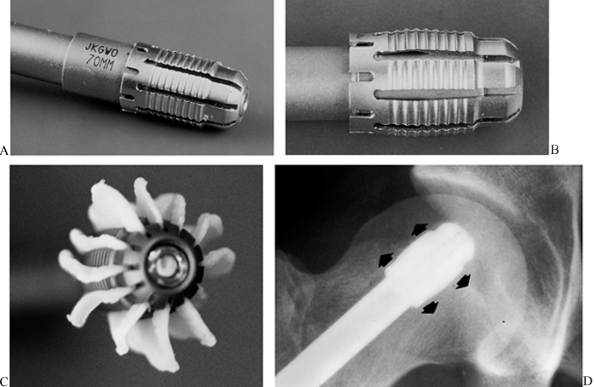
Figure 19.18. A:
The Alta dome plunger (Howmedica, Rutherford, NJ) when implanted in the femoral head provides superior resistance to cutout in osteoporotic bone, compared to compression hip screws. B: Insertion of the plunger into the dome expands it like a molly bolt. C: Polymethylmethacrylate cement can be placed in the dome and, when the plunger is driven home to expand the dome, the cement is extruded into the surrounding cancellous bone, as illustrated here, resulting in superior fixation in osteoporotic bone. D: AP radiograph of a dome-plunger in a femoral head. |
intertrochanteric hip fractures is to reestablish the continuity of
bone between the head and neck fragment and the shaft and to place the
fixation device central in the femoral head. This will allow the bone
to carry the majority of the load transmitted across the hip (46),
minimizing the risk for failure, and allowing frail patients to be
mobilized early with sufficient weight bearing so that they can gain a
reasonable degree of independence.
advanced greatly in the last three decades. In the early 1900s,
patients suffering intertrochanteric fractures were simply placed in
traction in bed for prolonged periods of time until healing, or more
commonly until death. In the 1930s, Smith-Peterson (126)
introduced his nail, which allowed immediate fixation and earlier
mobilization. Unstable fractures remained a problem, so in the mid
1960s, various osteotomies were advocated by Dimon and Hughston (37) and Sarmiento (113,114)
that used rigid fixation devices to create a stable fracture from an
unstable configuration. Unfortunately, both of these procedures have
been associated with increased morbidity and mortality due to the
increased surgery, and postoperative shortening was not well accepted
by patients. During this same period, Clawson (22) and Massie (89)
introduced sliding devices that allowed impaction of fracture
fragments. These devices have led to superior results in the treatment
of intertrochanteric fractures.
for fixation of intertrochanteric fractures. These devices are placed
retrograde from entry sites near the knee using percutaneous technique
under fluoroscopic control. Theoretical advantages include the
decreased bending moment on the device as previously described for the
Gamma nail; elastic fixation, which was proposed to aid fracture
healing; and percutaneous technique, which hastened fracture union by
preserving the blood supply to the fracture and decreased operating
time and blood loss. In spite of early reports of high rates of
success, later series showed a high incidence of varus deformity and
knee pain caused by the distal migration of pins (121,130).
This led to a high incidence of reoperation for pin extraction and
correction of deformity, which was a problem in elderly patients.
Shortening and external rotation were problems in many of those who
otherwise healed uneventfully. This has led most authorities to
recommend abandoning these devices for fixation of intertrochanteric
fractures. However, some surgeons believe that there is still a place
for Ender nails in the elderly debilitated patient who has a stable
fracture and who can tolerate only minimal operative intervention. The
details of the surgical technique described later in this chapter are
critical. The most recent development has been the antegrade
intramedullary devices such as the Gamma nail, which are very popular
in central Europe but seem to have outcomes similar to sliding hip
screws (8,58,83,144). These are discussed in more detail later in section D on second-generation interlocking nails.
leads to better care of the fracture or permits a more accurate
prognosis. In intertrochanteric fractures, the classification should
allow the surgeon to predict the stability of the fracture because
stability is the key to selection of treatment as well as prognosis.
stable or unstable. In the stable intertrochanteric fracture, the
posteromedial buttress remains intact or is minimally comminuted, and
therefore substantial collapse of the fracture fragments is unlikely.
In the unstable intertrochanteric fracture, however, a large segment of
the posteromedial wall is fractured free and comminuted, and therefore
the fracture tends to collapse into varus.
is useful because it further divides stable fractures into those
without comminution, those with minimal comminution, and those that are
subtrochanteric. A modification of Boyd’s classification is that of
Kyle, Gustilo, and Premer (81), which
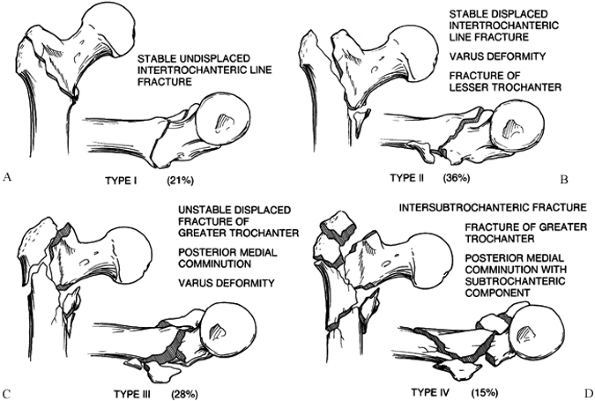
recognizes four basic intertrochanteric fracture types. Type I
fractures consist of nondisplaced stable intertrochanteric fractures
without comminution (21%) (Fig. 19.19A). Type
II fractures represent stable, minimally comminuted but displaced
fractures (36%); these are fractures that, once reduced, allow a stable
construct (Fig. 19.19B). Stable fractures are
not a problem and hold up well with any type of fixation device. The
unstable type III intertrochanteric fracture (28%) is a problem
fracture and has a large posteromedial comminuted area (Fig. 19.19C). The unstable
type IV fracture is uncommon (15%) and consists of an intertrochanteric fracture with a subtrochanteric component (Fig. 19.19D).
This is the most difficult type of fracture to fix because of the great
forces imposed by muscle forces and weight bearing on the
subtrochanteric region of the femur (81,150).
 |
|
Figure 19.19. A: Type I intertrochanteric fracture. B: Type II intertrochanteric fracture. C: Type III intertrochanteric fracture. D: Type IV intertrochanteric fracture.
|
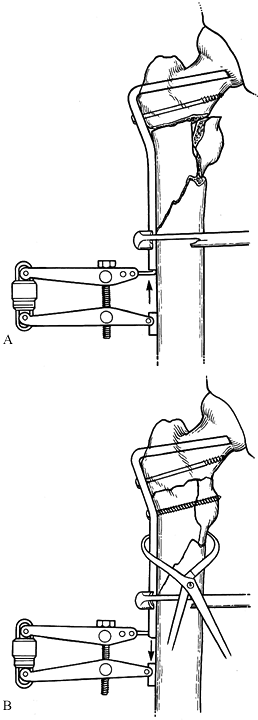
-
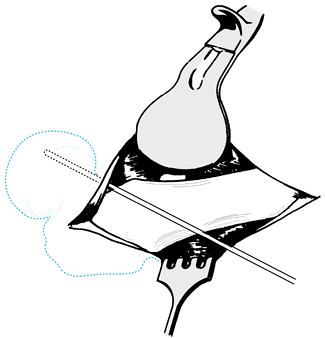
Place the patient supine on an orthopaedic fracture table (Fig. 19.20)
after administration of a general or regional anesthetic. Place the
unaffected leg into gentle traction to stabilize the pelvis on the
peroneal post, and abduct the hip 45° to provide access for the C-arm
fluoroscope.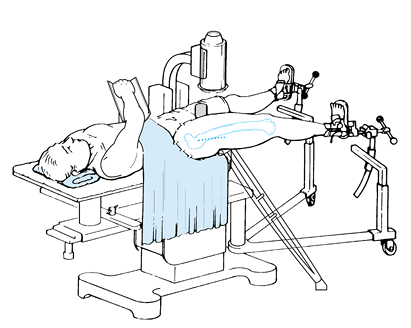 Figure 19.20.
Figure 19.20.
Supine position on a fracture table for fixation of an
intertrochanteric fracture with a compression hip screw or Ender nails.
Note that both legs are in traction with the C-arm located between the
legs. In comminuted unstable fractures where gravity causes the
fracture to sag posteriorly, support the fracture site with a crutch
placed under the proximal femur or greater trochanter, as illustrated. -
Apply gentle traction to the affected leg and use image intensification to discern the fracture elements.
-
Reduce the fracture with traction in line
with the body and enough internal rotation to place the femoral neck
parallel to the floor on the lateral view. Confirm reduction on the AP
and lateral views with image intensification. -
Type I fractures are undisplaced, so they
do not require a reduction maneuver and simply need to be placed in the
appropriate position for pinning, as previously described. -
Type II fractures require somewhat more
vigorous traction and internal rotation to close the fracture.
Internally rotating the hip to bring the femoral neck parallel to the
floor usually suffices. This helps to orient the surgeon to the
placement of the guide pin on the lateral view. Sometimes slight valgus
in these fractures produces a more stable position, particularly if
there is some medial comminution. -
Type III and type IV unstable fractures
require more vigorous traction and should be reduced in valgus of 140°
to 150° because this is more likely to result in good bone contact
medially. The valgus will compensate for the shortening that may be
necessary to gain good bone contact medially, and it will reduce the
bending moment on the fracture site. -
If traction alone does not reduce the
fracture, then abduction to obtain the appropriate position on the AP
view may be necessary. On the lateral view, gravity
P.639
often
causes the fracture to sag posteriorly, producing excessive anterior
angulation of the head and neck fragment. This may be difficult to
manage but can often be corrected by supporting the trochanteric region
with a crutch placed under the hip and angled to be out of the way of
the C-arm (Fig. 19.20). -
Prepare and drape the hip in the usual
manner. Make an incision over the lateral aspect of the thigh,
beginning at the flare of the greater trochanter and extending 12–15 cm
distally. Carry dissection down through the skin and subcutaneous
tissue to the fascia lata. Split the fascia lata along its posterior
extent, trying to avoid the muscle belly of the tensor fascia lata.
This exposes the vastus lateralis. Retract the vastus lateralis
superiorly with a rake and split it longitudinally if it is thin, or
reflect it anteriorly from the lateral intermuscular septum and
subperiosteally off the lateral aspect of the femoral shaft. Detach the
origin as necessary. Retract the vastus lateralis and fascia lata
anteriorly with a Bennett retractor. -
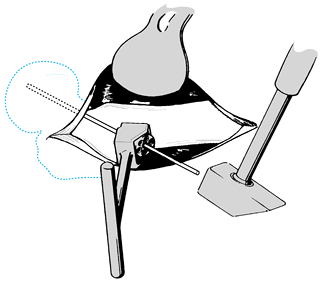
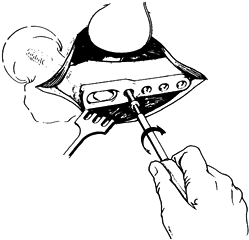
Under fluoroscopic control, place a guide
pin along the mid-anterior aspect of the femoral shaft and neck, in
line with the angle planned for the hip screw (141) (Fig. 19.21).
The guide pin should appear to lie within the center of the femoral
head on the AP radiograph, and parallel to the inferior femoral neck.
This helps to locate the site for the hole drilled in the lateral
aspect of the shaft.![]() Figure 19.21. Position of preliminary guide pin along the anterior aspect of the femoral neck.
Figure 19.21. Position of preliminary guide pin along the anterior aspect of the femoral neck. -
Using a drill slightly larger than the
size of the selected guide pin, perforate the lateral aspect of the
femoral shaft at the appropriate level as dictated by the guide pin (Fig. 19.22).
If the femoral head and neck lie posterior on the lateral view, start
the drill hole slightly anterior; if they are anterior, start the drill
hole slightly posterior.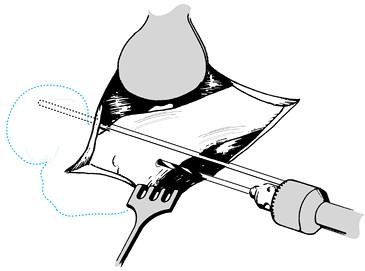 Figure 19.22.
Figure 19.22.
Drilling through the lateral cortex of the femoral shaft. Make the hole
large enough to accommodate variable positions of the guide pin. -
Prior to insertion of the guide pin, be
certain that the fracture is well reduced on both the AP and lateral
views. If the fracture is sagging posteriorly, adjust the crutch (if it
is being used), or place a bone hook on the
P.640
posterior
aspect of the fracture and lift the fracture to reduce the posterior
sag and to place the femoral neck in line with the shaft or in slight
anteversion. -
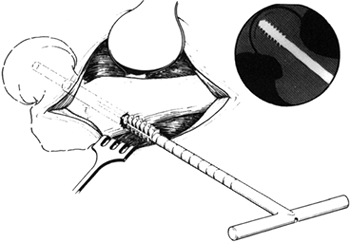
Now insert the guide pin specified by the
manufacturer for the type of sliding hip screw being used. In most
systems, side plates with angles from 130° to 150° at 5° increments are
available. If this is the case, some surgeons prefer to insert the
guide pin freehand, without using an angle guide, placing the guide pin
as close to the medial cortex of the neck of the femur as will
accommodate the hip screw, and ending up with the tip of the guide pin
in the dead center of the femoral head on both AP and lateral views.
Once satisfactory position of the guide pin has been obtained, they use
the angle-measuring device provided by the manufacturer to select the
side plate angle that is closest to the pin they have inserted. This
technique can lead to a maximum error on the AP view of 2.5°, which is
usually tolerable. I prefer to insert the guide pin through a guide set
at the desired angle, so that more precision can be gained in the
placement of the hip screw, which reduces the risk of displacing the
fracture (Fig. 19.23). In young, dense bone,
the guide pin may need to be drilled, but in the average elderly
patient it can be driven with a mallet. The tip of the hip screws
should not lie closer than 7 mm to the subchondral bone of the femoral
head. This needs to be taken into account, depending on the particular
instrumentation being used.![]() Figure 19.23.
Figure 19.23.
Use a guide to establish the angle of the guide pin in the femoral
neck. Insert the guide pin through the guide using a drill or mallet,
placing it dead center in the femoral head. On the AP views, some
surgeons prefer to have the guide pin somewhat inferior to the midline
of the head. -
Determine the length of screw to be used
by measuring the amount of the guide pin that is inside the proximal
femur and the head and neck fragments (Fig. 19.24).
Once the length has been measured, it is advisable in most systems to
drive the guide pin up to subchondral bone so that the guide pin is not
accidentally removed when the channel for the hip screw is reamed.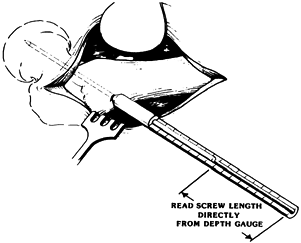 Figure 19.24.
Figure 19.24.
Use a depth gauge to determine the length of the hip screw. Plan to
place the screw no closer than 7 mm from the subchondral bone of the
head. -
Then place a step drill over the guide
pin and ream a hole in the lateral aspect of the femoral shaft to the
appropriate depth. Depending on the device used, place a tap over the
guide pin and advance it across the fracture site into the neck and
head fragment to the level of the desired position of the screw (Fig. 19.25).![]() Figure 19.25.
Figure 19.25.
Place a tap over the guide pin and tap the dense cancellous bone of the
femoral head. In osteoporotic bone, tapping is usually not necessary or
advisable. -
Place the screw or nail over the guide pin and insert it to the proper level under image intensification (Fig. 19.26).
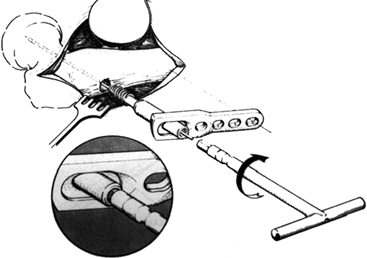 Figure 19.26.
Figure 19.26.
In most systems, the sliding hip screw and side plate can be
preassembled and the hip screw then screwed into place over the guide
pin. -
After seating the screw, insert the
plate, ensuring that it is parallel to the femoral shaft and lies
snugly against it. A fixed nail-plate angle device that does not lie
parallel to the shaft after the screw has been inserted may cause a
subtrochanteric fracture if forced down on the shaft. If an
inappropriate angle has been selected, so that the plate diverges by
more than 5° from the shaft, select a plate with the proper nail-plate
angle. -
Fix the plate to the lateral aspect of the shaft with three or four bicortical bone screws (Fig. 19.27).
Secure medial fragments with screw technique or a circlage cable, if
possible. This is possible in most current designs by the oval-shaped
hole in the side plate. Use image intensification during the final
seating of the screw to ensure that it is well located in the femoral
head and within 7 mm of subchondral bone.![]() Figure 19.27. Fit the plate snugly against the femoral shaft and secure it with at least three bicortical screws.
Figure 19.27. Fit the plate snugly against the femoral shaft and secure it with at least three bicortical screws. -
The sliding between the hip screw and the
side plate now allows impaction of the fragments to a stable position.
Release traction from the affected hip and grasp the patient at the
knee through the sterile drapes to ensure that traction is released and
that impaction can occur. Accomplish impaction by a direct blow on the
plate with an impactor. Then insert a compression screw, if available,
to secure the position. Obtaining impaction with the compression screw
alone is usually not advisable because in weak bone the screw can be
pulled out of the femoral head (Fig. 19.28).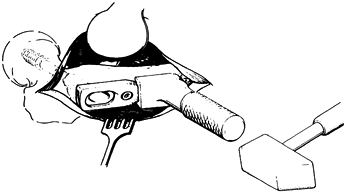 Figure 19.28. Release the traction on the foot and impact the fracture using the impaction device.
Figure 19.28. Release the traction on the foot and impact the fracture using the impaction device. -
Last, rotate the hip through its full
range of motion under fluoroscopic visualization to ensure that the
nail is within the confines of the femoral head and the fracture is
stable. -
Thoroughly irrigate the wound, ensure
hemostasis, place a suction drain, close the wound in layers, and apply
a sterile compressive dressing.
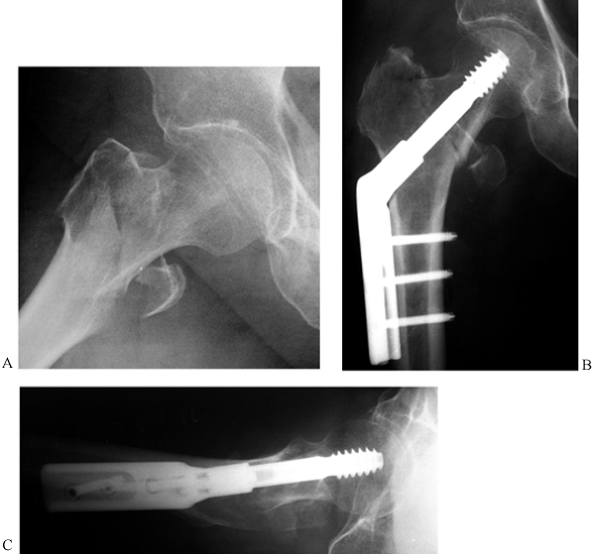 |
|
Figure 19.29. Sliding compression hip screw and side plate fixation of an intertrochanteric fracture. A: AP radiograph of a comminuted intertrochanteric fracture. B: AP radiograph of fixation with a compression hip screw. C: Lateral radiograph.
|
day after surgery, as dictated by comfort. As soon as practical, begin
ambulation with aids, allowing weight bearing on the injured extremity
as tolerated if solid fixation of a stable reduction has been obtained.
Progress weight bearing as tolerated. Take radiographs at weekly
intervals for the first 2 weeks to ensure proper impaction of the
fragments and function of the sliding device. If there is a
subtrochanteric component to the fracture, or the bone quality or
reduction is marginal, delay weight bearing until callus is seen on
radiographs.
I prefer to place these patients in a lateral decubitus position on a
regular operating table and expose the base of the neck as well as the
shaft with a limited Watson-Jones exposure.
-
Visualize the femoral head and fracture
with a C-arm fluoroscope placed in the AP position over the top of the
patient. The C-arm of the fluoroscope must be sterilely draped. It can
be rotated up over the torso out of the way when it is not needed and
then swiveled into the AP position on the hip when used. -
Expose the fracture with a limited
Watson-Jones exposure. In this type of fracture, the greater trochanter
is fractured and free of the shaft fragment; therefore, the
trochanteric fragment and the shaft can be pushed posteriorly out of
the way to expose the base of the head and neck fragment. This needs to
be exposed only enough to have good visualization of the base of the
neck, and a good feeling for the axis of the neck anteriorly. -
Insert a guide pin into the inferior half
of the base of the neck parallel to the medial neck under fluoroscopic
control to place the guide pin dead center in the middle of the femoral
head on both the AP and lateral views. Obtain fluoroscopic
visualization of the head and neck
P.643
fragment by manipulating this fragment alone, rather than by moving the extremity or the C-arm. With a T-handle
on the guide pin and a sharp pointed tenaculum grasping the base of the
femoral neck, rotate it to obtain perfect AP and lateral views. Then
ream the channel for the hip screw and insert the hip screw under
direct fluoroscopic control. Judge the proper length screw by measuring
the guide pin in the head and neck fragment and adding to it the width
of the femoral shaft at the level of the hip screw.
-
If patients are thin and lightly muscled,
a direct split of the vastus lateralis is easiest and quickest. In
younger, heavily muscled patients, or in comminuted fractures where
extension of the approach into a Watson-Jones exposure may be
necessary, release the vastus lateralis from the anterior and lateral
aspects of its origin, elevate it off the lateral intermuscular septum,
and reflect it anteriorly as a single unit. This provides a clean
exposure for management of comminuted fragments in the subtrochanteric
area, facilitates a Watson-Jones exposure, and allows identification of
the proximal arterial perforators for control of bleeding. -
Many different types of hip screws and
instrumentation systems are available. Most of these offer various
guides and mechanisms for setting the depths of reamers, for example.
Do not rely solely on these mechanical devices, but visualize the
insertion of tools and implants on fluoroscopy at all times. Use of the
step image minimizes radiation exposure of the patient and surgeon. -
If the patient is being treated supine on
a fracture table, and reduction of the fracture is difficult or
maintenance of the reduction is challenging, do not hesitate to extend
the exposure somewhat proximallytin the manner of Watson-Jones to gain
exposure of the base of the femoral head and neck fragment, because
this greatly facilitates reduction. -
Most stable fracture patterns can be done
through a relatively small incision. Three bicortical screws in the
plate are nearly always sufficient. The plate can be slid
subperiosteally beneath the vastus lateralis and the screws inserted
through a stab wound in the muscle, which minimizes soft-tissue
dissection. Where longer plates are needed, the modular Alta system
(Howmedica, Rutherford, NJ) facilitates this minimally invasive
technique. -
Controlled impaction of the fracture on
the table under fluoroscopic control produces immediate stability of
the fracture in most hips. Careful examination under fluoroscopy will,
in most cases, demonstrate sufficient stability in the fracture site to
confidently allow early weight bearing. -
During rehabilitation, even though you
are allowing early weight bearing, always have the patient use an
assistive device. In the elderly, walkers are usually the best—not so
much for protection of the fracture, but to prevent the patient from
having another fall and sustaining additional injuries.
-
Once the hip screw is securely in place,
select either a 145° or 150° side plate and slip it onto the hip screw
to the appropriate depth. Then bring the femoral shaft into proper
alignment with the head and neck fragment, align the side plate on the
lateral aspect of the shaft, and secure it loosely with a Lowman
bone-holding for-ceps. -
Then, under fluoroscopic control, impact
the head and neck fragment and the shaft together to restore cortical
continuity, particularly along the medial side. Be certain that
rotation is correct. Then secure the plate to the shaft of the femur
with an appropriate number of bicortical screws, and secure the hip
screw to the side plate with the compression screw. -
In some cases, the fragments of the
greater trochanter will lie in appropriate position; however, in many
cases a circlage cable placed around the medial neck of the femur, at
the level of the lesser trochanter, or around the base of the hip screw
and subsequently through a drill hole in or over the top of the greater
trochanter, will reestablish the continuity of the abductor mechanism. -
Close the wound over a suction drain in a routine manner.
limited weight bearing to the weight of the leg until bridging callus
is seen on radiographs.
time is much quicker because a fracture table is not involved; the
effect of gravity, which causes the fracture to sag, is eliminated,
making reduction much easier; and the relative positions of the patient
and surgeons plus the limited open exposure make the procedure quicker
and easier
than
when the patient is in the supine position on a fracture table. The
disadvantages are the increased soft-tissue exposure and, perhaps, some
increased blood loss.
be fixed with Ender nails or a second-generation interlocking nail such
as a Gamma-type interlocking nail. Use full-length second-generation
interlocking nails when there is distal extension of the femoral shaft
fracture, or if a distal femoral shaft fracture is combined with an
intertrochanteric/subtrochanteric fracture. Ideally, the piriform fossa
should be intact for the entry point of a standard intramedullary nail.
But Gamma nails enter at the tip of the trochanter, which is nearly
always intact, and Ender nails enter distally. The techniques for
insertion of Gamma and Ender nails are described next. See Chapter 20 for the interlocking nail technique.
-
Position the patient supine on a fracture
table and reduce the fracture anatomically as previously described for
insertion of a compression hip screw. Access to the tip of the
trochanter must be unimpeded; therefore, if the patient is heavily
muscled or obese, tilt the torso toward the opposite side. Be certain
that high-quality AP and lateral views on the C-arm fluoroscope can be
obtained, and then prepare and drape the hip and thigh in the usual
fashion. -
Make a longitudinal incision 3–4 cm long,
directly over the tip of the greater trochanter. Carry this directly
down to bone and expose the tip of the greater trochanter by splitting
the muscle fibers of the gluteus maximus and medius. -
Insert a guide pin into the tip of the trochanter and open it with a reamer.
-
Then insert a ball-tip guide pin across
the fracture into the shaft of the femur, and use flexible reamers to
ream the intramedullary canal 2–3 mm larger in diameter than the Gamma
nail to be inserted. The proximal femur down to the lesser trochanter
must be reamed to at least 17 mm in diameter to accommodate the nail.
Remove the guide pin. -
Assemble the appropriate-size Gamma nail
on the driver, selecting the valgus angle most suitable for the
fracture. More comminuted fractures can be nailed in more valgus.
Available angles are 125°, 130°, and 135°. The nail is 17 mm in
diameter proximally and 11 mm in the shaft portion. Ten degrees of
anteversion is built into the nail. When the reduction is done, if the
femoral neck is placed parallel to the floor, then the nail can be
inserted in a neutral position, which facilitates proper placement. -
Under fluoroscopic control, locate the
entry site for the hip screw and make a 2.5 cm longitudinal incision in
the skin, over the lateral aspect of the hip, at the appropriate point.
Carry dissection sharply down through the deep fascia and vastus
lateralis, and expose sufficient lateral femur just below the greater
trochanter in a subperiosteal manner. Assemble the targeting jig on the
nail. Insert the appropriate guide sleeve (tissue protector) down to
bone, make a starting point with the awl, and insert a guide pin under
fluoroscopic control. Make certain that the guide pin on the AP view is
at or inferior to the midline of the neck, and that it is dead center
on the lateral view, with the guide pin ending up dead center in the
femoral head. Be certain that the angle of the targeting jig matches
that of the nail. -
Measure the length of the hip screw off the guide pin.
-
Now ream over the guide pin to the appropriate depth for the hip screw, and tap the hole if hard cancellous bone is present.
-
Then insert the appropriate-length hip
screw to the appropriate depth, under fluoroscopic control; confirm
that it is in appropriate position, and then release the traction and
impact the fracture to ensure good bone contact and a stable position.
Particularly in osteoporotic bone, it is essential that good medial
bone contact occur. -
Finally, place the set screw through the
top of the nail to secure the position of the hip screw. Tighten it,
and then loosen it one-quarter turn to permit sliding between the hip
screw and the nail. -
If the fracture is unstable and
comminuted, and further resistance to shortening and additional
rotational control is desired, distally cross-lock the nail, using the
cross-locking guide for the short Gamma nail and the free-hand
technique for the long Gamma nail. -
After closure of the wounds and
application of a sterile dressing, take AP and lateral radiographs on
the fracture table to be certain that the fracture is well reduced and
in stable position, and that the Gamma nail is in appropriate position (Fig. 19.30).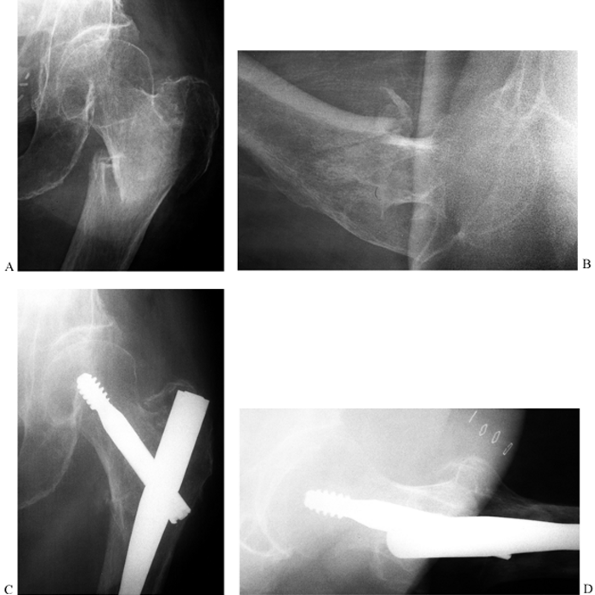 Figure 19.30. Gamma nail fixation of an intertrochanteric fracture. A: AP radiograph of a comminuted intertrochanteric fracture with severe osteoporosis. B: Lateral radiograph. C: AP radiograph of fixation of the fracture with a long Gamma nail. D: Lateral radiograph.
Figure 19.30. Gamma nail fixation of an intertrochanteric fracture. A: AP radiograph of a comminuted intertrochanteric fracture with severe osteoporosis. B: Lateral radiograph. C: AP radiograph of fixation of the fracture with a long Gamma nail. D: Lateral radiograph.
fractures, which was extended to include shaft fractures using multiple
solid elastic stainless steel nails, using a retrograde percutaneous
approach, became popular in the 1970s (11,39).
Although some surgeons still use Ender nailing as their primary means
for fixing hip fractures, the technique is not used much in North
America today. The nails offer little resistance to shortening in
unstable fracture patterns, and fractures tend to externally rotate.
Prominence of the nails at the knee may require a second operation to
remove them. In addition, because the fixation is much
less
rigid than with a compression hip screw, patients experience more pain
postoperatively and do not rehabilitate as quickly. Ender nailing of
the femur, tibia, and humerus, however, is a very useful technique that
should be in the armamentarium of every surgeon treating these
fractures, because in the femur there are certain situations for which
the nail is ideal:
-
Anatomic reduction of the fracture prior to insertion of the nail.
-
Proper entry point with overreaming of
the nail so that the intramedullary nail can be pushed into place by
hand without using a mallet. -
Proper seating of the nail so that the
screw is in line with the femoral neck and located dead center in the
femoral head, or perhaps somewhat inferior on the AP view. -
Improper technique can lead to
microcracks in the proximal portion of the femur, near the end of the
nail, which can cause femoral shaft fractures (100).
This risk can be minimized by proper surgical technique with the short
Gamma nail, or by using the long Gamma nail if bone quality is poor.
-
Use it for internal fixation of fractures
in the proximal femur when the condition of the skin about the hip
precludes a surgical approach at the hip. -
Use it for severely ill patients with
stable fracture patterns, in whom percutaneous technique with minimal
soft-tissue dissection offers the advantages of rapidity and minimal
blood loss. -
Use it for patients with hip fractures in
severely osteoporotic bone, in whom a medullary device is preferred
because of the risk of a pathologic fracture at the site of the plate
and a hip screw. Exercise caution with Ender nails, because
supracondylar fractures can occur through the distal entry holes. -
Use it for fractures in children and
adolescents with open physes, where internal fixation is required but
larger intramedullary devices would threaten the growth plates or blood
supply to the femoral neck. Ender nails are currently the device of
choice for older children with femoral shaft fractures accompanied by
multiple injuries, who require intramedullary fixation of the femur
(see Chapter 164).
-
Place the patient supine on a fracture
table in the same position as described for the sliding hip screw. In
type I and II fractures, reduce the fracture anatomically. In type III
and IV fractures, use a valgus reduction of up to 150° because this
greatly facilitates insertion of the Ender nails. Because of the
tendency of the nails to run straight rather than curve into the
femoral head fragment as much as you might like, comminuted fractures
are often easier to fix than more simple fracture patterns reduced
anatomically. Ender advises placing the hip in more internal rotation
than you would for a traditional hip screw to compensate for the
tendency of the fractures to externally rotate as they compress into
stable position. In unstable fracture patterns, the crutch beneath the
greater trochanter is very useful in Ender nailing, because having a
straight shot proximally into the femoral head and neck fragment from
the medullary canal on both views greatly facilitates the nailing. -
Prepare and drape the knee circumferentially from the mid thigh to below the tibial tubercle.
-
Because the primary entry site for the
Ender pins is in the distal medial femur, stand between the legs with
your assistant on the lateral side of the knee, and the operating nurse
behind you. Locate the C-arm just above the affected hip on the lateral
side, making certain that good-quality AP and lateral views can be
obtained without moving the base of the C-arm. -
Make a longitudinal skin incision 7 cm
long, beginning just distal to the medial epicondyle and extending
proximalward. Split the deep fascia just anterior to the medial
intermuscular septum, and reflect the vastus medialis anteriorly to
expose the femur subperiosteally just above the superior medial
geniculate artery. Identify and protect the superior medial geniculate
artery because this is the landmark to the entry site for the pins.
Laceration of this artery can lead to profuse bleeding. Ligate it if it
is in the way or if significant bleeding occurs. -
Next, make the entry hole for the nails (Fig. 19.31).
The distal end of this hole should be 1 cm proximal to the medial
geniculate artery. The hole needs to be at least 15 mm wide to
accommodate two 4.5 mm Ender nails side by side, and it must have a
length of 20–25 mm to accommodate at least three nails without causing
enough pressure on the proximal end of the hole to lead to unexpected
fracture of the entry hole or distal femur. Make an initial entry hole
with a Steinmann pin or drill point, and follow this with a Küntscher
awl. Use this to enter the cancellous bone of the metaphysis of the
femur. Take care to not use it to open the harder cortical bone near
the diaphysis, because this can lead to fracture of the cortex. Follow
the awl with a small-angled rongeur and use this to develop an oval
hole with a smooth contour. Use a nail as a reference to be certain
that the hole is of adequate size. The longitudinal axis of this hole
must be directly in line with the shaft of
P.647
the
femur, and it is better placed slightly more posterior than anterior,
because the nails in a more anterior position are more likely to result
in knee pain.![]() Figure 19.31.
Figure 19.31.
Entry site for retrograde Ender nailing of a hip fracture just proximal
to the medial epicondyle. See text for full description. -
Use a Küntscher skin protector distally.
Standard femoral nails are 4.5 mm in diameter, with lengths of 34 to 49
cm. Shorter nails of 4 mm diameter from 28 to 44 cm long are available
for smaller people. Be certain that reduction of the hip fracture has
been maintained. Determine the nail length by inserting a forceps into
the distal end of the entrance hole as a landmark, and then placing the
nail on the anterior aspect of the thigh with the tip directly over the
femoral head. The nail length will be correct when the tip touches or
is just slightly distal to the subchondral bone of the weight-bearing
portion of the femoral head (use visualization on a fluoroscopic image)
and the flange of the nail rests on the cortex immediately distal to
the entry hole. The nail will bend as it is being inserted, shortening
its effective working length and resulting in the tip of the nail lying
approximately 5–7 mm below the subchondral bone of the femoral head. If
the nail length is not quite correct after insertion, leave the nail in
place and insert a second nail of appropriate length prior to
withdrawing the first nail. Sometimes the first nail can be left in as
a stacking nail (see later) if multiple nails are to be used to gain
stability in a wide medullary canal. -
Nails are available with a C or an S
curvature. For intertrochanteric fracture, use the C nails. In anatomic
reductions, particularly when placing the first nail along the medial
femoral neck, bending the tip of the nail to increase its curvature is
helpful as long as the bend in the nail is not so much that it impedes
the passage of the nail down the medullary canal. The tip of the nail
has a smooth bevel that facilitates passage of the nail when it
encounters a cortex. When passing the nails, think about driving the
tip of the nail along the curvature of the femur, as you would drive a
car down a winding highway. Insert the first nail by hand with the T-handled
driver into the hole, matching the curvature of the nail to the
curvature of the femur. Begin at an angle of approximately 45° to the
longitudinal axis of the femur, and then reduce the angle to come in
line with the femur as the nail progresses proximally. The nail passes
smoothly across the fracture and into the head and neck fragment if it
is twisted to stay in the middle of the medullary canal until it
reaches the level of the lesser trochanter. At the lesser trochanter
twist the nail internally to place the maximum curvature along the
medial aspect of the femoral neck. Insert this first nail just past the
fracture site, being certain that it is firmly located in the proximal
fragment, but do not insert it to its full depth until all of the nails
are in place. Next, insert a second and third nail, making an effort to
fan the nails in the femoral head on both the AP and lateral views (Fig. 19.32).
Once all three nails are into the head and neck fragment, they can be
sequentially driven as a group to within 5–7 mm of the subchondral bone
of the head. Distally, the nails should lie flush with the medial
cortex of the femur, above the epicondyle (Fig. 19.33).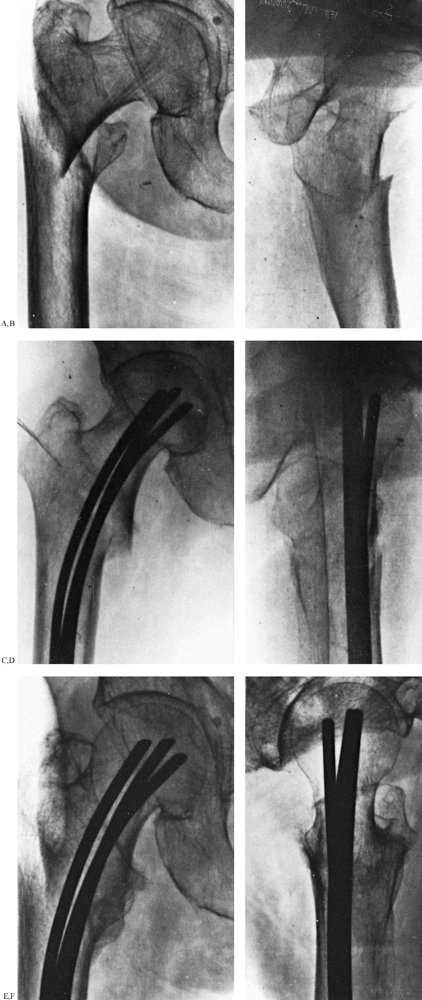 Figure 19.32. Ender nail fixation of a four-part intertrochanteric hip fracture. A,B:
Figure 19.32. Ender nail fixation of a four-part intertrochanteric hip fracture. A,B:
In this impacted pertrochanteric fracture, the impaction of the
proximal fragment into the trochanteric region and the posterior
angulation are easily discernible on the lateral view. C,D:
Fixation after overreduction in a slight valgus position was performed
with three nails. Full weight bearing three days after surgery led to
the anatomic position and collapsing of the diastasis seen in the
intraoperative lateral view. E,F: Follow-up after 1 year shows solid healing in good position.![]() Figure 19.33.
Figure 19.33.
Note the entrance site for the nails, which is proximal enough to the
medial epicondyle that the nails lie flat along the bone surface (A) and are angulated somewhat posteriorly on the lateral view (B). -
The technique for combined
intersubtrochanteric fractures or for subtrochanteric fractures is the
same, except one or more nails are inserted through a lateral portal
into the greater trochanter using a technique identical to that
described for the medial side (Fig. 19.34).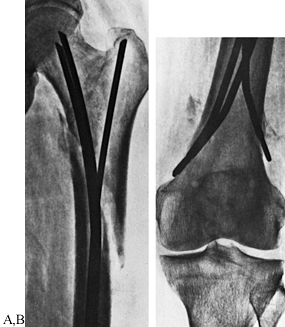 Figure 19.34. A: In subtrochanteric fractures, arrange the nails in a V
Figure 19.34. A: In subtrochanteric fractures, arrange the nails in a V
formation in the proximal fragment so that two or more nails are
inserted from the medial condyle into the femoral neck or head, and one
or more into the greater trochanter. B: Note the separate entrance hole in the lateral condyle, just opposite the medial entrance hole. -
When the nails are in place, loosen the
traction and maximally impact the fracture site, visualizing the head
and neck fragment on the AP view to be certain that the nails do not
penetrate the femoral head into the joint. -
Ensure hemostasis in the soft tissues,
and then close the wound in layers. Suction drains are usually not
advisable because if there is continued bleeding from the medullary
canal, excessive blood loss into the suction drain may occur. Usually
it is better to simply let a small
P.648P.649
hematoma form, which tamponades the medullary canal. This is rarely a problem.
-
Frequent fluoroscopic visualization
during nailing, using the step mode on the fluoroscope to limit
radiation exposure, is advisable to be certain that the nails are
following the desired track, and that nails already inserted are not
accidentally pushed proximally too far as the other nails are inserted. -
Stable fracture patterns in patients with
narrow medullary canals can often be managed with two nails, but most
fractures do best if fixed with three. It is rarely necessary to use
more than three, but if the nails are loose in the medullary canal, add
short nails that extend only into the isthmus portion of the femur to
jam the nails to prevent back-out. -
Be certain that the flats of the nails
distally lie flush and parallel to the cortex, lying on solid cortical
bone. Prominent nails can cause knee pain. Nails that are too short can
accidentally spring into the medullary canal of the femur and then, if
they back out, can penetrate the knee joint or at a minimum be very
difficult to remove. -
To produce a more stable fixation
construct, some surgeons wire the distal ends of the nails together
through the extraction hole. Ender nails can be interlocked distally by
placing a screw through the eye of the nail, but this risks penetration
of the articular surface of the femoral head if excessive shortening
occurs and therefore is not recommended as a routine procedure. -
When driving a nail, be careful not to
hold it too far from the long axis of the femur, particularly as it
progresses proximalward, because this may produce excessive pressure on
the proximal medial surface of the entry hole, resulting in a fracture
of the cortex above the hole. This can cause a major stress riser,
which can lead to supracondylar fracture of the femur. -
Nail removal is usually not necessary,
but up to a third of patients experience knee pain that requires
removal of the nails. This can be accomplished through a small
incision, using the Ender nail extraction tool. This is most easily
inserted by placing the extraction tip beneath the nail toward the bone
and twisting it into the extraction hole of the nail. -
Be certain that postoperative radiographs
cover the entire length of the femur, so that the position on both AP
and lateral views can be fully assessed at the hip and the position at
the entry hole can be fully visualized as well. -
In unstable subtrochanteric and
comminuted fractures for which unacceptable shortening is predictable,
Ender advises keeping the patients in postoperative traction until
early callus is seen on radiographs. With this technique, this averages
between 3 and 4 weeks. It is the need for postoperative traction in
these unstable fractures that has limited the use of Ender nails in
favor of interlocking nails, which offer far superior stability.
tolerate. Use assistive devices for ambulation and limit weight bearing
to the weight of the leg until bridging callus is seen on radiographs,
which is usually at about 6 weeks. At this time, progress weight
bearing as tolerated until full weight bearing is achieved. In stable
fracture patterns, this usually occurs within 1–2 or more weeks, but in
unstable patterns, particularly those with a subtrochanteric component,
full weight bearing is often delayed until 12 or more weeks after
surgery.
fractures can be treated with primary internal fixation. Indications
for primary prosthetic replacement using a proximal femoral replacement
prosthesis would include the following:
-
Peritrochanteric fractures in the presence of severe arthritis of the hip, especially if the hip is stiff
-
Pathologic fractures in which the bone stock precludes internal fixation
-
Unstable, severely comminuted fractures
in the very elderly, whose bone is so osteoporotic that internal
fixation, even with cement augmentation, is expected to fail
that compared compression hip screws to a Vandeputte endoprosthesis in
these fractures suggested that primary prosthetic replacement might
have fewer early complications and satisfactory functional results.
are minimal compared with other hip fractures if the surgeon uses the
appropriate device and pays close attention to the mechanical
principles involved. The overall failure rate using a sliding hip screw
or nail of newer alloys should not exceed 10%. Nail breakage is
extremely rare with use of current high-technology metals. The
infection rate in intertrochanteric fractures should not exceed 1% to
2% with the use of prophylactic antibiotics. Acute infection usually
responds well to irrigation and debridement, possibly implantation of
antibiotic-impregnated beads, and intravenous antibiotics if the
fracture construct is stable. Avascular necrosis is extremely rare in
intertrochanteric fractures and has not been reported to occur in more
than 1% of patients in any series (122). If
nonunion does occur, the success rate after removal of the device and
renailing in a more valgus position is 90%; for this reason, repeated
fixation is recommended.
reduction with a too-superior placement of the nail, which results in
the head and neck fragment cutting off the hip screw. This can usually
be salvaged by rereduction and nailing in a valgus position, either
with a new Gamma nail or with conversion to a compression hip screw.
The other complication in Gamma nails is fracture of the femur at the
tip of a short Gamma nail. This is best treated by conversion to a long
Gamma nail. Failure in Ender nails is usually caused by a varus
reduction, persistent instability, and failure to fill the canal with
nails, which results in back-out of the nails and collapse at the
fracture site. This can often be corrected by rereducing the fracture,
reinserting the same nails using proper technique, and adding nails to
produce stability. Supracondylar fracture at the entry hole can be
managed by circlage wiring in many cases. Instability and displacement,
however, may require conversion to a condylocephalic interlocking nail
or plate fixation distally.
as the region between the lesser trochanter and the junction of the
proximal and middle third of the femur. Although fractures in this area
affect all age groups, there are two peak ages of incidence. The first
occurs during late adolescence and early adulthood, when high-energy
trauma from motor-vehicle and motorcycle accidents causes displaced or
comminuted fractures (1). With these mechanisms
of injury, severe injuries to other organ systems are frequent. The
other age group of increased incidence is the geriatric population, for
whom minor slips and falls are common, often resulting in
subtrochanteric fractures. Metastasis from tumors (e.g., lung and
breast cancer) often cause pathologic subtrochanteric fractures through
compromised bone stock.
desirable features of intertrochanteric and femoral shaft fractures. If
they are comminuted, stable internal fixation may be difficult to
achieve with plates and screws. Moreover, the predominantly cortical
nature of the subtrochanteric region prolongs healing times (120). For even the experienced traumatologist, subtrochanteric fractures may present formidable problems in management (120).
The proximal end of the femur has been likened to a cantilevered arch
that transfers the force of weight bearing from the lower extremity to
the hip and pelvis. Vertical loading forces on the femoral head
generate a large moment arm in the proximal femur, concentrating
compressive forces medially and tension forces laterally. When
comminution, bone loss, or tumors create deficiencies in the medial
cortex, the delicate balance of forces is altered, leading to deformity.
surgery, a plate placed laterally acts as a tension band, allowing
impaction with protected weight bearing. If the medial cortical contact
is not restored, bending stresses are concentrated in one small area of
the plate, which often results in mechanical failure of the internal
fixation device with delayed union, nonunion, or malunion of the
fracture (143). Until recently, restoration of
the continuity of the medial cortex of the proximal femur has been the
key to success. However, the superior strength and mechanics of locked
intramedullary nails combined with closed nailing techniques have
eliminated the mandate to reconstitute the medial cortex at the time of
surgery (13,17,152).
The major advantage of intramedullary fixation is that it allows the
bone to carry a substantial portion of the load, which significantly
reduces the risk of implant failure while preserving the blood supply
to bone when a percutaneous technique is used, which hastens healing.
nails in the 1980s, the indications for closed nailing of
subtrochanteric fractures have dramatically expanded. Locking the nail
into good-quality bone above and below the fracture site produces
immediate fracture stability. Patients can be mobilized shortly after
surgery without fear of loss of length or malrotation. The load-sharing
intramedullary nail lies within the weight-bearing axis of the leg and
is better suited to resist torsional and bending forces than a plate
and screws.
classified trochanteric fractures of the hip into four types. In their
classification, type III injuries were pure subtrochanteric fractures,
and the type IV fractures were combined
intertrochanteric–subtrochanteric fractures. Fielding and Magliato (44) in 1966, and Zickel et al. (156,157)
a decade later, classified subtrochanteric fractures according to
radiographic appearance. Since that time, several investigators have
modified existing classifications or proposed new ones (115,118,145).
developed a classification for subtrochanteric fractures that allowed
the surgeon to analyze results based on a specific fracture group or
subtype (Fig. 19.35). The IIIA subtrochanteric
fracture was associated with a poor outcome in eight of nine patients
treated with internal fixation in his series. In what is probably the
most widely used classification of subtrochanteric fractures, the
Association for the Study of Internal Fixation (AO-ASIF) group (91) divides these injuries into three basic types and ten subtypes, based on their radiographic appearance (Fig. 19.36).
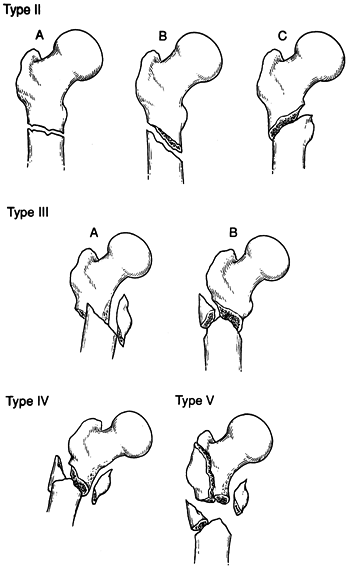 |
|
Figure 19.35. The Seinsheimer classification of subtrochanteric femur fractures.
|
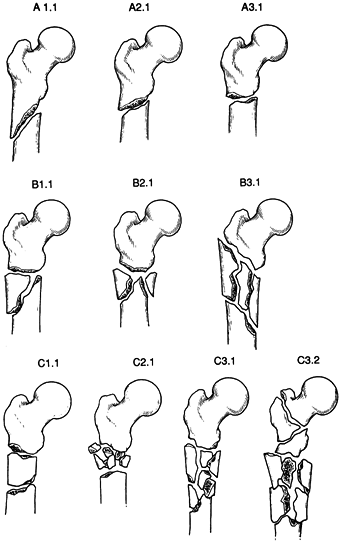 |
|
Figure 19.36. The AO-ASIF classification of subtrochanteric femur fractures.
|
are the most useful. Unfortunately, anatomic fracture classifications
fail to address associated conditions commonly seen with
subtrochanteric femur fractures, although they often influence
treatment or outcome. The factors that
play a dynamic role in fracture management have been termed the personality
of the fracture. Among these are the amount of fracture displacement,
the extent of soft-tissue injury, the presence or absence of open
wounds, associated neurovascular injuries, the degree of osteoporosis,
multiple trauma, and complex ipsilateral injuries (e.g., ipsilateral
femoral neck or segmental fractures). A large number of fracture
patterns are seen in clinical practice, and some do not fit neatly into
any classification scheme. This emphasizes the fact that every case
must be individually evaluated and that the “personality” of the
fracture must be considered in selecting the method of treatment.
complete elimination of nonoperative treatment in adults and a
corresponding increase in operative treatment of subtrochanteric
fractures. A thorough understanding of the anatomy and biomechanics of
the subtrochanteric region is essential if nonoperative treatment is to
be used. Powerful hip and thigh muscles lead to significant deformities
after fracture. The iliopsoas and hip abductors cause flexion,
abduction, and external rotation of the proximal fragment, and the
strong pull of the adductors produces shortening and varus of the
distal fragment. Skeletal traction followed by a spica cast or a cast
brace 4–6 weeks later is still the method of choice for most fractures
in childhood and early adolescence.
with subtrochanteric fractures with extreme fracture comminution. Lack
of appropriate implants and surgical inexperience make operative
intervention hazardous (34). Although this
method of treatment eliminates many operative complications, such as
anesthetic complications, blood loss, and infection, it is not without
its own complications. In adults, prolonged costly hospitalization is
necessary, and acceptable alignment may be difficult to achieve despite
frequent adjustments of the traction. Knee stiffness and varus malunion
remain common problems after skeletal traction. Furthermore, traction
treatment is usually contraindicated in the multiply injured or elderly
patient.
a hip spica cast is invariably required. Traction modalities depend on
the patient’s body habitus and the radiographic fracture pattern. For
some patients, a Thomas splint and Pearson knee attachment can be
effective. In other patients, alignment is better maintained with a
modified form of Russell’s traction using a proximal tibial pin. If the
hip must be flexed more than 45°, or if significant external rotation
is required to achieve alignment, a distal femoral pin with 90°-90°
traction may be more practical (Fig. 19.37).
Approximately 30–40 lbs (14–18 kg) of traction is required to reduce
the fracture in adults. After length and alignment are restored, the
weight can usually be decreased (see Chapter 10).
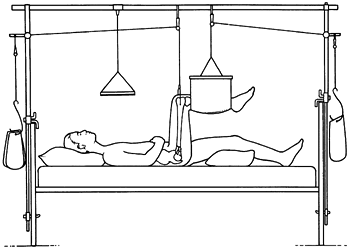 |
|
Figure 19.37. Treatment of a subtrochanteric fracture in skeletal traction using a distal femoral traction pin and the 90°-90° position.
|
practical with treatment in traction, but restoration of overall length
and alignment is important. Do not accept more than 5° to 7° of varus,
or 10° of anterior or posterior angulation if possible. Limb shortening
of 1.0–1.5 cm does not usually compromise functional results. While the
patient is in traction, institute a full rehabilitation program with
upper extremity weight lifting, as well as range-of-motion and
strengthening exercises of the uninvolved lower extremity. As the
fracture begins to consolidate, range-of-motion exercises of the hip
and knee in traction are usually possible.
of subtrochanteric fractures is premature termination of traction and
application of a spica cast (20). Because
of the tremendous forces concentrated in the subtrochanteric region,
discontinuing traction earlier than 8–12 weeks usually leads to a varus
deformity. This can occur even if the patient is immobilized in a hip
spica. The cast should not be applied until the fracture site is no
longer tender and radiographs show abundant callus formation. To
minimize the risk of varus deformity, cast braces must include a pelvic
band, which holds the hip in an abducted position. Application of a
fracture brace should not lull the surgeon into a false sense of
security. Careful attention to the details of fracture reduction and
the application of the cast or brace are crucial to success. Examine
the patient and take radiographs at 1 and 3 weeks after cast
application to guard against unrecognized loss of reduction. Protect
the fracture until it is healed, which may take as long as 6 months
(see Chapter 10).
fractures has gained widespread acceptance as surgical techniques and
implants have improved over the past 40 years. The combination of
properly engineered implants, a better understanding of soft-tissue
handling, perioperative antibiotics, and improved anesthetic methods
have made internal fixation safe and effective (111).
The goals of surgical treatment of subtrochanteric femur fractures are
anatomic alignment, stable internal fixation, rapid mobilization of the
patient, and early functional rehabilitation of the limb. However, it
is important to remember that internal fixation of subtrochanteric
fractures is difficult.
essential to have complete sets of instruments and implants, and
experienced surgical, nursing, and physiotherapy staff. If these
criteria are met, the following may be considered indications for
surgery:
-
Displaced subtrochanteric fractures in adults
-
Fractures in multiply injured patients
-
Most open fractures
-
Associated vascular injuries requiring repair
-
Severe ipsilateral limb injuries
-
Unacceptable alignment after attempted closed treatment
-
Pathologic fractures
-
Certain fractures around a hip prosthesis
stabilization, but there are several relative contraindications to
internal fixation:
-
Active infection
-
Severely contaminated high-energy open fractures (grade IIIB)
-
Massive comminution or bone loss
-
Severe osteopenia
-
Fractures in hemodynamically unstable, multiply injured patients
-
Unavailability of adequate implants
-
Unavailability of experienced surgeons
require surgery, perform internal fixation as soon as practical, and
within the first 48 hours if possible. If surgery is delayed at all,
place the patient in skeletal traction. Stabilize closed fractures in
patients with multiple injuries during or at the conclusion of the
thoracic, abdominal, vascular, or neurosurgical procedures, if possible.
widely used in the management of subtrochanteric femur fractures:
locking intramedullary nails and plates. Because the spectrum of
injuries to the subtrochanteric region is so great, no single implant
can be suitable for every case. Careful assessment of the patient and a
critical review of the radiographs and the personality of the fracture
are essential.
subtrochanteric fractures with Küntscher-type nails does not provide
reliable fixation of the proximal part of the femur because of its wide
medullary canal. Their use is restricted to transverse or short oblique
fractures without comminution.
Even
with these simple fracture patterns, shortening, malrotation, or nail
back-out often leads to unacceptable results. In comminuted fractures,
supplemental fixation with cerclage wires or unicortical plates has
frequently been necessary. The major advantage of intramedullary
fixation is that it allows the bone to carry a substantial portion of
the load. This significantly reduces the risk of implant failure.
Additionally, fixation can be done using closed nailing techniques,
minimizing soft-tissue disruption at the fracture site with better
preservation of periosteal blood supply.
early 1980s, the indications for closed nailing of proximal femoral
fractures has expanded (17,152).
All closed adult subtrochanteric fractures below the level of the
lesser trochanter can be safely nailed with a first-generation nail,
regardless of the fracture pattern or degree of comminution (Fig. 19.38).
Nails with transverse proximal locking, such as the Alta nail
(Howmedica, Rutherford, NJ), can be used for fractures at or above the
lesser trochanter (Fig. 19.39). Closed locked
intramedullary nailing is the current treatment of choice in adults for
all acute nonpathologic subtrochanteric femur fractures that require
operative stabilization.
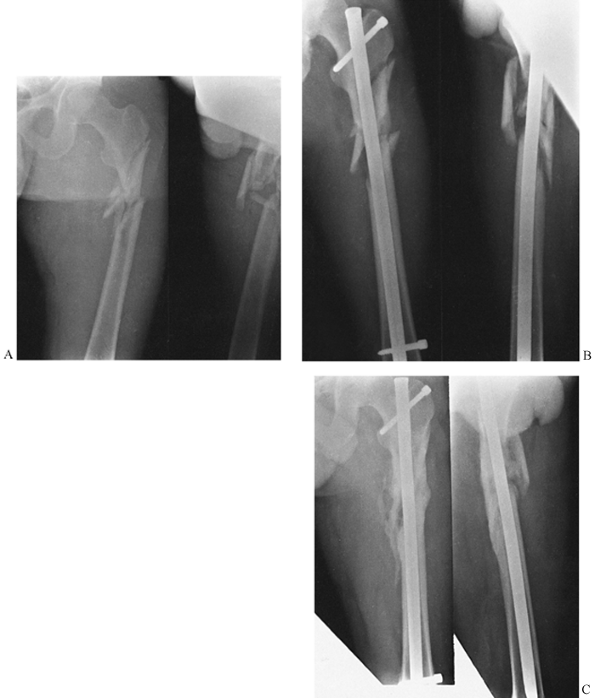 |
|
Figure 19.38. A: A comminuted subtrochanteric femur fracture in a 23-year-old man was the result of a motorcycle accident. B: Length and alignment were restored after static locked intramedullary nailing. C: At 6 months, the fracture is healed.
|
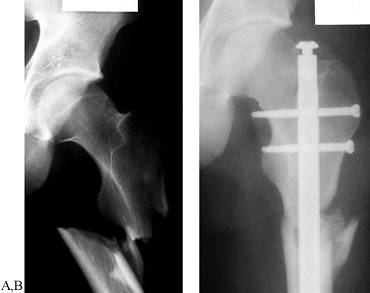 |
|
Figure 19.39. A: AP radiograph of a subtrochanteric fracture. B:
Radiograph after fixation with a standard Alta intramedullary nail with static proximal and distal cross-locking. Note the location of the proximal transverse cross-locking screws in the femoral neck. |
be performed, depending on the fracture location and configuration. In
static locking, screws are inserted in the proximal and distal
fragments. Rotational stresses are minimized, and shortening at the
fracture site is prevented. With dynamic nailing of subtrochanteric
fractures, a proximal screw is inserted. Rotational movement is
neutralized, but shortening of the fracture site is not always
prevented. Because of the small proximal fragment in subtrochanteric
fractures, always lock subtrochanteric fractures proximally.
comminution types II, III, and IV and in long spiral fractures. If any
doubt exists about the stability of fixation after nailing, the nail
should be statically locked. Locking the nail into the bone above and
below the fracture site produces immediate fracture stability. Distal
locking adds little to the procedure, so I now statically lock all
nails. Patients can then be mobilized shortly after surgery without
fear of malrotation or loss of length. Closed locked femoral nailing
can now be performed routinely in the vast majority of patients who
previously would have required open reduction and internal fixation or
prolonged traction. Early mobilization should reduce postoperative
medical complications, maintain joint motion, and decrease hospital
stay (Fig. 19.40).
 |
|
Figure 19.40. A: Displaced subtrochanteric femur fracture of a 31-year-old woman who sustained multiple injuries in a motor-vehicle accident. B:
Closed intramedullary interlocking nailing restored the length and alignment. No attempt was made to reduce the medial butterfly fragment. C: Follow-up at 14 months showed union of the fracture with incorporation of the butterfly fragment. |
fracture table in the lateral decubitus or supine position, or open
exposure of the fracture site can be done with the patient in the
lateral decubitus position on a regular table.
I
prefer the lateral decubitus position on a regular table for most
comminuted subtrochanteric fractures. Positioning on a fracture table
in the lateral position is somewhat more difficult than in the supine
position, but the fixation of the fracture is greatly facilitated
because there is far superior access for the instrumentation, and
reduction of the fracture is much simpler. The supine position is much
more familiar to most surgeons and therefore is preferred by many. The
flexed adducted position of the proximal fragment, however, makes
reduction of the fracture difficult, and the patient’s buttocks and
thigh are frequently in the way of the instrumentation, particularly in
heavily muscled or obese patients. I use the lateral position with open
technique when speed is essential, or when the patient is already on a
regular operating table because of general surgical procedures that
have just been completed for multiple injuries. In addition, in
intertrochanteric–subtrochanteric combinations, open technique makes
obtaining a satisfactory reduction and solid fixation easier at the
expense of a larger wound, more blood loss, and more threat to the
blood supply of bone.
-
The proximal fragment is frequently quite
flexed and externally rotated. This alignment is often difficult for
the surgeon to ascertain. It is critical that the very best images on
the C-arm be obtained, and this can be difficult in large patients.
Because of the position of the proximal fragment, it is quite easy to
place the starting point much too anterior and too medial on the
femoral neck. When using first-generation nails, be certain that the
starting point is directly over the intramedullary canal. -
Again, because of the flexed–adducted
position of the proximal fragment, reaming of the proximal fragment may
be eccentric and produce malposition when the nail is inserted. Avoid
this by paying attention to the alignment of the proximal fragment. If
satisfactory position cannot be maintained, make a small incision and
insert a bone hook or bone-holding forceps to hold the proximal
fragment in proper position. Sometimes the fracture must be opened. -
My custom is to distally cross-lock
first, and then to use the driver on the nail to back-slap the nail to
ensure optimal contact between the proximal fragment and the shaft, so
that the femur can load-share when there is greater than 50% contact
between the fragments. -
Nails such as the Grosse-Kempf
(Howmedica, Rutherford, NJ), with an oblique proximal cross-locking
screw, require an intact lesser trochanter to obtain adequate fixation
in the proximal fragment. Nails that offer transverse cross-locking
screws proximally, such as the Alta nail, can be positioned more
proximally (the Alta nail is specifically designed to do this), and the
cross-locking screws can be inserted into the medial femoral neck,
which gives excellent fixation and does not threaten the mechanical
integrity of the femoral neck or the blood supply to the femoral head (158) (Fig. 19.39).
nails for complex subtrochanteric fractures expanded the indications
for closed nailing of these difficult injuries. However, as the
indications for nailing were extended to more proximal fractures, an
increased incidence of implant and proximal screw failures were noticed
in comminuted fracture patterns. Furthermore, most first-generation
nails provided inadequate fixation if the fracture extended above the
level of the lesser trochanter. These problems led to the development
of a new generation of interlocked nails that provided better fixation
by directing screws into the head of the femur, and that allowed distal
interlocking (Fig. 19.41). These implants are
called reconstruction or second-generation nails. They have an
increased wall thickness proximally, stronger and larger proximal
screws, and reliable proximal targeting devices.
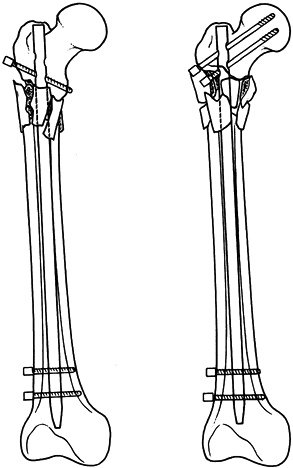 |
|
Figure 19.41. A: A first-generation interlocking nail. B: A second-generation (reconstruction) interlocking nail.
|
second-generation nail is a “high” subtrochanteric fracture, in which
the lesser trochanter is fractured but the greater trochanteric mass
remains intact (Fig. 19.42).
With this fracture pattern, most conventional first-generation
interlocked nails may not provide stable fixation. The use of a
second-generation nail for a combined intertrochanteric–subtrochanteric
fracture requires considerable surgical experience because these
fractures are very difficult to fix (Fig. 19.43).
If fracture comminution involves the greater trochanter or the region
of piriformis fossa, reconstruction nailing is associated with an
increased incidence of complications, particularly varus deformities
and implant cutout. A Gamma nail might be a better alternative because
it enters through the top of the trochanter (see previous section). In
these complex fractures, treatment with a compression hip screw or an
angled blade plate may be a better alternative. Although reconstruction
or second-generation nailing remains an exciting new surgical
technique, there are few published reports of treatment results.
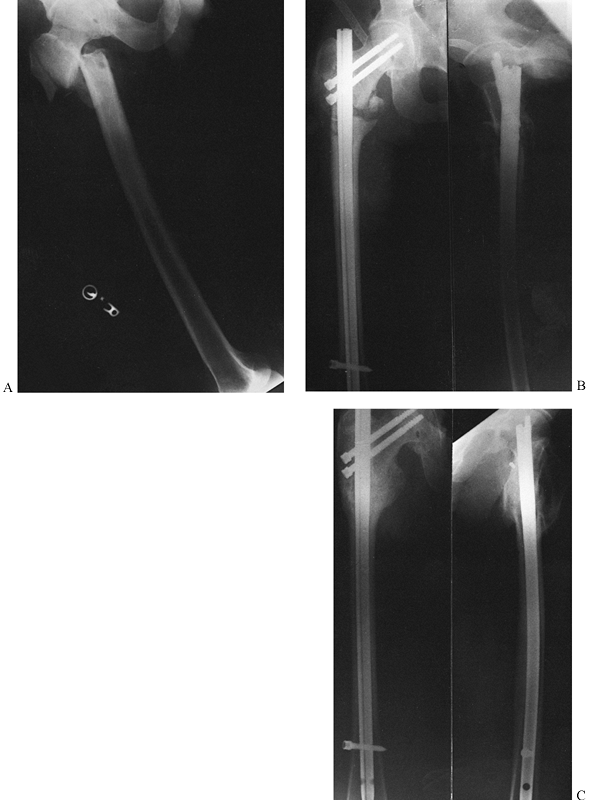 |
|
Figure 19.42. A:
Displaced subtrochanteric femur fracture sustained by a 27-year-old man who fell from a roof. Notice the linear fracture extension into the greater trochanter. B: Fixation was achieved with a second-generation reconstruction nail. C: Follow-up at 60 months shows union of the fracture. |
 |
|
Figure 19.43. A:
Comminuted intertrochanteric–subtrochanteric femur fracture sustained by a 23-year-old woman involved in a motor-vehicle accident. B: Treatment with a reconstruction nail provided stable fixation and early mobilization and weight bearing. C: Follow-up at 15 months confirmed that the fracture was soundly united. |
analyzed the results in 45 Russell-Taylor type IB subtrochanteric
fractures stabilized with a reconstruction nail. Their intraoperative
complication rate was 13.5%, with the most frequent problem being varus
malposition. The final outcomes, however, were excellent: 100% of the
fractures healed at an average of 13.5 weeks. There were no implant
failures and 96% of patients gained greater than 120° of knee motion.
their experience with the use of the Russell-Taylor reconstruction nail
(Smith Nephew Richards, Memphis, TN) for five ipsilateral femoral neck
and shaft fractures and six comminuted subtrochanteric fractures. All
of the fractures united. Technical errors occurred in three patients,
and three patients ended up with malalignment or shortening,
demonstrating that this method of fixation is challenging.
reported their experience with 42 patients treated with the Gamma nail,
of which 31 were subtrochanteric fractures. All 31 subtrochanteric
fractures healed, but 16 patients had shortening that averaged 1.7 cm
with a range of 1 to 4 cm. Six healed with varus deformity, and three
of those also had external rotation deformity. Apparently, these
authors did not cross-lock the nails distally. An acceptable reduction
of the hip must be achieved and maintained during the insertion of the
hip screw. In the vast majority of fractures, distally cross-locking is
advisable to avoid the shortening and external rotation deformity
encountered by Rodriguez-Alvarez et al. See Chapter 11 and in particular Chapter 20 for details on the surgical technique for these devices.
provided the first major advance in the treatment of subtrochanteric
fractures when he introduced his reinforced nail, which provided
proximal cross-locking into the femoral head and neck in the early
1970s. His nail enjoyed its greatest success in the treatment of
impending and acute pathologic fractures in the subtrochanteric area (10,32,112).
The Zickel nail is no longer used, for the most part, because it does
not provide distal cross-locking. Complete stabilization of the
fracture requires additional fixation at the fracture site, and
refracture of the femur upon removal of the nail has been reported (10,94,139,154).
the Ender nail has particular advantages in unusual situations where
the soft tissues around the hip preclude the use of any device that
enters from around the hip and where a retrograde device inserted
through the knee, such as the Ender nail, is particularly advantageous.
As pointed out in the discussion on Ender nails in the
intertrochanteric fracture section, the Ender nail does not offer
enough stability in unstable subtrochanteric fractures to permit
immediate mobilization of the patient. Either the fracture must be
opened and supplementary fixation applied, or the patient must be
protected in traction postoperatively. For that reason, Ender nails are
rarely used now for the treatment of subtrochanteric fractures.
patients can be mobilized from bed to chair as soon as they can
tolerate it, and can begin crutch ambulation. If the patient’s bone
quality is good, the fracture is a stable pattern, and if there is at
least 50% cortical contact between the proximal and distal fragments,
then 50% weight bearing with crutches is usually possible immediately.
Weight bearing can be progressed to full weight bearing once bridging
callus is seen on both AP and lateral views. In unstable fractures,
patients can bear weight to the weight of the leg, but they must not
progress weight bearing until bridging callus is seen on two views. In
nearly all patients, there is sufficient stability that knee and hip
range-of-motion exercises can begin immediately. An aquatic therapy
program and use of a stationary bicycle are useful for building range
of motion and enhancing muscle strengthening while the fixation must be
protected. Healing usually requires 12–24 weeks.
the technique aimed at anatomic reduction and stable fixation of all
fragments. Primary bone healing was found to be possible if fracture
gaps were closed and if rigid stabilization was achieved. However, in
comminuted fractures for which extensive soft-tissue dissection was
necessary to achieve anatomic reduction, the incidence of delayed
union, nonunion, infection, and implant failure was significant (4) (Fig. 19.44).
The favorable experience with interlocked nailing for comminuted
subtrochanteric fractures gave the surgeon the opportunity to treat
difficult fractures with much less soft-tissue dissection. It showed
conclusively that anatomic alignment rather than anatomic reduction
combined with stable fixation results in a high percentage of favorable
fracture outcomes. However, interlocked nailing did not solve the
dilemma of difficult intraarticular or epiphyseal-metaphyseal
fractures. For these injuries, plate and screw osteosynthesis remains
the treatment of choice (56,75,90).
 |
|
Figure 19.44. A: Highly comminuted subtrochanteric femur fracture sustained by a 29-year-old man in a motor-vehicle accident. B: Open reduction internal fixation with a 95° angled blade plate. C: At 10 months, there was plate failure and nonunion. D: After repeat plating with a supplemental iliac crest bone graft, the fracture united at 14 months.
|
of the soft tissues and fracture repair, the methods and techniques of
internal fixation have gradually evolved during the past decade into a
method termed biological fixation. The aim of current fracture
treatment is to achieve stable rather than rigid fixation with a
minimum of soft-tissue dissection and implants. The goal is to preserve
the blood supply to bone to enhance early callus formation.
planning. Perform the surgery on paper or on the computer before going
to the operating room. Executed properly, this surgical tactic shortens
operative time, minimizes intraoperative decision making, and improves
surgical results. In preoperative planning for a subtrochanteric femur
fracture, take high-quality radiographs of the intact femur and the
injured side. Using plastic templates, trace the fracture and its
subsequent reduction, the type and size of implants, and the exact
position of screws on tracing paper. Multiple drawings are frequently
necessary to arrive at the optimal fixation construct with the least
soft-tissue dissection. Careful preoperative planning ensures that the
proper implants are available at the time of surgery (56,75,90). When subtrochanteric fractures are reduced open and fixed with plates, always consider autologous bone grafting.
-
Perform surgery on a standard operating table or a fracture table with biplanar image intensification (75). Make a standard lateral approach to the proximal femur (see Chapter 3).
Take down the vastus lateralis from its origin at the base of the
greater trochanter, and carefully detach it to expose only the lateral
aspect of the proximal femur. Do not dissect the anterior and medial
soft-tissue envelope. To protect the anterior and medial tissues, avoid
using Bennett-, Cobra-, and Hohmann-type retractors. -
To achieve the desired position for the
blade on the AO 95° blade plate on the AP view, enter in the region of
the prominence of the greater trochanter. Be sure that the contour of
the lateral plate matches that of the femur, with the blade traversing
transversely into the center of the femoral neck, inferior to the
midline of the neck. On the lateral view, the chisel should be
absolutely dead midline. Because the corners of the chisel can
accidentally penetrate the articular surface if the tip of the blade
plate is placed too close to subchondral bone, always leave it a
minimum of 1 cm from subchondral bone on any view. Prior to inserting
the seating chisel, drive a 2 mm K-wire into the bone, visualizing it
on the AP and lateral views, just superior to where the seating chisel
will be placed and exactly parallel to the anticipated path. -
Either using the triple drill guide or
free hand, use a 4.5 mm drill point to open up three drill holes in the
lateral cortex, transverse to the long axis of the femur in the plane
that the blade will sit. In hard young bone, removing about 5 mm of the
inferior edge of this hole with a small osteotome at a 45° angle allows
room for the bend of the blade plate to seat into the greater
trochanter. -
Take the seating chisel (a tuning fork
mallet can be slipped over it to provide additional rotational control)
and drive it with the U-shape of the blade
facing superiorly to match that of the blade on the blade plate.
Confirm proper position on AP and lateral views with the fluoroscope. -
The length for the blade is measured
directly from the seating chisel at the lateral cortex. Now insert the
seating chisel into the proximal femur, matching the level determined
in the preoperative drawings. -
In patients positioned on a regular operating table, a modified Watson-Jones approach (Chapter 3)
and an anterior arthrotomy of the hip with visualization of the femoral
head and neck help to guide the placement of the seating chisel. In
patients positioned on a fracture table, exposure of the femoral head
and neck is not necessary because the position of the seating chisel
and blade can be determined solely with the aid of the image
intensifier. -
Next, secure the side plate to the
lateral side of the femur with bone-holding forceps. Reduce the
subtrochanteric fracture to the plate by one of three techniques. One
method uses the fracture table to restore length by longitudinal
skeletal traction. A second technique to overcome significant
shortening uses the femoral distractor (Fig. 19.45).
Initial overdistraction often permits gentle teasing of comminuted
fracture fragments into near-anatomic positions. A third method of
reduction uses the articulating tension device as a distractor
P.662P.663
(Fig. 19.46).
With the fracture temporarily overdistracted, the medial fragments
often reduce spontaneously because of their soft-tissue attachments, or
they may be reduced by gentle manipulation. Try not to manipulate
fragments from the cortical surfaces to avoid soft-tissue stripping.
Anatomic reduction is carried out whenever possible, but neither
anatomic reduction nor restoration of the medial buttress is absolutely
necessary when a biologic approach is employed.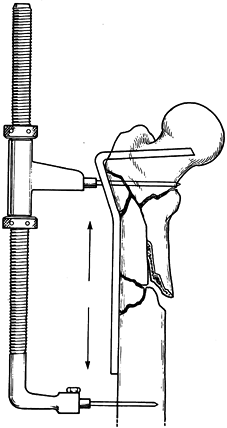 Figure 19.45. Indirect reduction technique using a 95° angled blade plate and the femoral distractor.
Figure 19.45. Indirect reduction technique using a 95° angled blade plate and the femoral distractor.![]() Figure 19.46. Indirect reduction technique uses the articulating tension device. A: In distraction. B: In compression.
Figure 19.46. Indirect reduction technique uses the articulating tension device. A: In distraction. B: In compression. -
Regardless of the reduction maneuver,
after the comminuted fracture fragments are realigned axially, compress
the fracture using the articulating tension device. The blade plate
then acts as a lateral tension band, with compressive forces
transmitted through the fracture and the restored medial cortex. If the
medial comminuted fracture fragments are not keyed into place because
of extensive comminution, they are considered a vascularized bone graft
and left in situ. Supplemental bone graft
is not required if the medial soft-tissue envelope has been respected.
However, the plate should still be loaded to partially offset varus
tendencies. Occasionally, supplemental interfragmentary screws outside
the plate increase the stability of the fixation. -
Always apply an autologous cancellous
bone graft when the soft tissue has been stripped medially. Or, a bone
graft can be inserted medially through the fracture before reduction
and fixation of the fracture.
of subtrochanteric fractures (4,73,115,140,145).
In the past, orthopaedic implant manufacturers warned against its use
in subtrochanteric fractures, but newer devices with improved design
and materials with higher fatigue strengths have overcome many of the
obstacles to its use in the treatment of subtrochanteric fractures. The
compression hip screw is more forgiving of imperfect insertion than the
blade plate, allowing for sliding impaction of the fracture surfaces
with slight medialization of the shaft. Secure fixation in the proximal
and distal fragments allows controlled collapse with a decrease in the
bending moment and resultant forces. This method of treatment is
attractive in high subtrochanteric fractures and in those with proximal
extension into the intertrochanteric region. These devices usually must
be used in a keyed or locked mode to prevent rotation between the
compression hip screw and the barrel of the side plate. A keyless
system may lead to instability between the proximal and distal fragment
with institution of hip flexion. In cases with medial comminution,
place bone graft medially to hasten fracture union (14).
This is usually necessary because, unlike the 95° blade plate
technique, indirect reduction techniques are not as easily accomplished
with a compression hip screw.
developed for the treatment of supracondylar and intercondylar
fractures of the femur, and it has been adapted for use in the proximal
femur. The dynamic condylar screw appears to be a reasonable
alternative to the fixed angled plate for the surgeon who only
occasionally uses this device (111). However,
as with all laterally based plates, reconstruction of the medial calcar
is important. Many orthopaedic surgeons suggest cancellous bone
grafting if the medial cortex cannot be restored at the time of surgery
(73,88).
cannot be rendered stable, then consider double plate fixation to
reduce the risk of fatigue fracture of the side plate. Use a smaller
plate such as a 4.5 mm, four- to six-hole narrow plate placed
anteriorly through a modified Watson-Jones exposure.
dynamic condylar screw, or a compression hip screw, mobilize patients
as soon as their overall condition permits. If stable fixation has been
achieved at the time of surgery, protected crutch ambulation can begin
on the second or third postoperative day. Depending on the fracture
pattern and the completeness of restoration of the medial cortex,
protected weight bearing can usually begin at 4 to 6 weeks. This is
gradually increased as clinical symptoms subside and radiographs show
progressive fracture union. Do not allow full unrestricted weight
bearing until at least 12 weeks, at which time callus should be seen
bridging the fracture on two views. Failure to show progressive signs
of radiographic union 4–6 months after internal fixation is cause for
concern. Bone grafting, with or without revision of the internal
fixation, should be considered to prevent delayed union, nonunion, or
mechanical failure of the implant.
of subtrochanteric femur fractures. The most common indication for its
use is severe open fractures, particularly grade IIIB injuries in
multiply injured patients. Depending on the location of the wounds and
the degree of fracture comminution, fixation into the iliac crest may
be necessary. For most patients, the external fixator is a temporary
device used for initial management of the fracture and soft tissues.
After control of the soft tissues is achieved, delayed internal
fixation can be done. Place fixator pins to avoid areas of planned
surgical incisions and implant placement, if possible. The major
advantages of external fixation are rapid application, minimal
soft-tissue dissection, and the ability to maintain length, provide
wound access, and mobilize the patient. Problems associated with its
use include pin loosening and infection, loss of knee motion secondary
to binding of the quadriceps mechanism, increased risk of delayed union
and nonunion, and loss of reduction after its removal.
subtrochanteric femur fractures, excluding gunshot wounds. The
traumatic wound is usually anterior or lateral but may be located
anywhere. As with all open fractures, thorough irrigation and
debridement of the fracture and traumatic wounds remain the single most
important step in the prevention of infection. Serial debridement may
be necessary in many grade III open fractures. With few exceptions, the
traumatic wound should be left open. If immediate internal fixation of
the open fracture is performed, the surgical extensions can be closed,
but the open fracture wounds should not be closed primarily. Although
immediate internal fixation is done in most cases, it is not indicated
for all fracture patterns. The risk-to-benefit ratio for the patient
must be carefully assessed when contemplating primary internal
fixation. Advantages of immediate internal fixation in open
subtrochanteric fractures include ease of wound care, pain relief, and
mobilization of the patient and the injured limb. The major
disadvantage of immediate internal fixation is the increased risk of
infection
as a consequence of further soft-tissue dissection and interference with local blood supply.
subtrochanteric femur fractures, I favor definitive internal fixation
after debridement of the traumatic wounds. Treatment of most grade IIIB
and IIIC open subtrochanteric fractures depends on the circumstances.
Some of these fractures may be more safely managed with external
fixation or skeletal traction and delayed internal fixation.
fixation of all grades of open subtrochanteric fractures may be
advisable. After irrigation and debridement of the wounds, the injured
limb can be splinted or placed in skeletal traction. Subsequent surgery
can be carefully planned with optimal operating room personnel.
Unfortunately, many open subtrochanteric fractures occur in patients
with multiple injuries, and failure to stabilize the fracture early
often leads to missed opportunities. Associated injuries and pulmonary
problems may delay definitive fixation for days or weeks. This
increases the technical difficulty of the procedure, contributes to
patient morbidity, and compromises the full benefits of internal
fixation.
of subtrochanteric fractures, compared to blade plates and the Zickel
nail, was shown by Brien et al. (17) in a
nonrandomized, nonconsecutive series. They had 21 patients in the
Zickel nail group, 25 treated with blade plates, and 33 treated with
the interlocking nail. Operating times were longest and blood loss
greatest with the blade plates. Operating times were shortest and blood
loss lowest with the interlocking nail. Combining the incidence of
malunion, nonunion, and infection, the overall complication rate in the
Zickel group was 57%; in blade plate patients, 36%; and in the nail
patients, only 9%, with two malunions, one nonunion, and no infections.
trochanter is intact—and even for some where it is fractured but the
head and neck and trochanters are one solid unit—I prefer to use a
standard Alta titanium intramedullary nail that has two transverse
cross-locking screws both proximally and distally. When this nail is
seated with its top flush with the top of the femoral neck, the
transverse locking screws are located just superior to and inferior to
the lesser trochanter. Seating the nail more proximally to place it
level with the tip of the trochanter places these two screws in the
femoral neck, and seating it 1 cm proximal to the tip of the greater
trochanter allows the most proximal screw to be placed into the femoral
head. Placement of the screws in the femoral neck eliminates any need
to worry about the position of the screws relative to the axis of the
femoral neck fragment, which is one of the more difficult technical
aspects of placing reconstruction nails, whose screws must traverse up
the femoral neck and into the femoral head. Whether these screws are in
the posterior, medial, or anterior cortex is irrelevant because a solid
hold is obtained in all of these positions, and none of these creates a
significant stress riser in the femoral neck, or has ever been shown to
interfere with the blood supply to the head (158).
trochanteric region, I prefer to do these fractures in the
lateral-decubitus position on a regular operating table, under
fluoroscopic control, utilizing an Alta CFX nail (Howmedica,
Rutherford, NJ). When the trochanters are so comminuted that the head
and neck fragment is totally free and the entry site for an
intramedullary device is essentially destroyed, my implant of choice is
usually a compression hip screw and occasionally a blade plate. When
using this open technique, it is very difficult to preserve the
anterior and medial soft-tissue attachments to the femur; therefore, I
routinely do autologous bone grafting.
discussed in the text under the individual techniques. The most common
complication of subtrochanteric fractures of the hip is early failure
of fixation, with failure of the side plate when hip screws or 95°
blade plates are utilized, and cutting of the femoral head and neck
fragment off the hip screws when the bone is osteoporotic and there is
inadequate medial stability. Because of the large muscle forces around
the hip, which are encountered even with the simplest of day-to-day
activities such as getting in and out of a chair, fatigue failure of
appliances inadequately supported by a good reduction can occur fairly
early. Although fracture reduction is under the control of the surgeon,
comminution and poor bone quality can preclude adequate stability, so
subtrochanteric fractures continue to be a problem. Whenever early
failure occurs in a subtrochanteric fracture, infection should be
looked for as well. Most early device failures can be treated by early
reoperation, replacement with a similar or stronger device, addition of
additional fixation such as an anterior plate, and copious autologous
bone grafting. Postoperatively, these patients must be very carefully
protected until bone union
occurs.
They must be taught how to get on and off toilets and in and out of
chairs, and how to walk to minimize the stress on their implants.
implant failure, but with intramedullary devices this is less common.
Lack of any visible callus at the fracture site at 3 months after
fracture is characteristic of delayed unions. The chances of these
progressing to a nonunion are high; therefore, some surgeons feel that
bone grafting at 12 weeks, if bridging callus is not seen, is indicated
to prevent a nonunion. Nonunions in compression hip screws and blade
plate devices at 6 months are usually best treated by conversion to an
intramedullary implant combined with bone graft. Nonunion in
intramedullary devices is uncommon and can often be treated with
exchanged reamed intramedullary nailing to a larger device, usually
done by closed technique, but sometimes combined with bone graft with
the addition of a unicortical plate. See Chapter 29 for more details.
and external rotation. Treatment of these complications is complex,
usually requiring an osteotomy and repeat internal fixation. Leg-length
discrepancy often requires management with Ilizarov techniques or
closed intramedullary shortening of the opposite femur (see Chapter 29, Chapter 30, and Chapter 32).
postoperative weeks. Management depends on the severity of the
infection and the organism involved. Acute staphylococcal and
streptococcal infections without intramedullary involvement, regardless
of the device used, usually respond to thorough irrigation and
debridement of the wound, closure over antibiotic-impregnated beads,
and treatment with appropriate bacteriocidal intravenous antibiotics.
Most patients respond quickly, showing resolution of systemic and local
signs of infection within a few days. The wound can be reopened again
in 5–7 days for removal of the beads; closure over suction drainage or
reinstallation of beads can be repeated as many times as is necessary
to control the acute infection. Some type of antibiotic treatment for
up to 6 weeks is usually required. In more benign infections,
intravenous antibiotics followed by oral antibiotics suffice. See Chapter 132 and Chapter 135 for more details.
accompanied by nonunion with unstable implants. Chronic infection in
the presence of bone union usually responds nicely to removal of the
implant, debridement, and antibiotic therapy as already described. This
complex topic is addressed in detail in Chapter 133 and Chapter 135.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
MR, Curtin SL, Lindskog DM. Intramedullary Versus Extramedullary
Fixation for the Treatment of Intertrochanteric Hip Fractures. Clin Orthop 1998;348:87.
WJ, Corces DA, Anderson LD. A Preliminary Experience with the
Russell-Taylor Reconstruction Nail for Complex Femoral Fractures. J Trauma 1992;33:71.
WW, Wiss DA, Becker V. Subtrochanteric Femur Fractures: A Comparison
Between the Zickel Nail, 95 Degree Blade Plate and Interlocking Nail. J Orthop Trauma 1991;5:458.
PL, Rommens PM, Deleyn PR, et al. Pertrochanteric Fractures in the
Elderly: Are There Indication of Primary Prosthetic Replacement? J Orthop Trauma 1991;5:446.
CC, Levine D, O’Doherty JO, Lyden J. Unipolar Versus Bipolar
Hemiarthroplasty for the Treatment of Femoral Neck Fractures in the
Elderly. Clin Orthop 1998;348:67.
PA, Kruse T. Hip Fractures in the County of Funen, Denmark.
Implications of Demographic Aging and Changes in Incidence Rates. Acta Orthop Scand 1983;54:681.
JS, Amstutz HC, Zinar DM, Dorey FJ. A Comparison of Total Hip
Arthroplasty and Hemiarthroplasty for Treatment of Acute Fracture of
the Femoral Neck. Clin Orthop 1992;282:123.
PR, O’Connor DR, Schwarze D, Schwartz E. A Prospective Comparative
Study of the Compression Hip Screw and the Gamma Nail. J Orthop Trauma 1994;8:367.
JT, Kenzora JE, Hebel JR, et al. Eight-year Outcome Associated with
Clinical Options in the Management of Femoral Neck Fractures. Clin Orthop 1998;348:59.
S, Kalen R, Thorngren KG. Treatment and Outcome of Femoral Neck
Fractures. An Analysis of 2418 Patients Admitted from Their Own Homes. Clin Orthop 1987;218:42.
GA. A Comparison of the Use of Internal Fixation and Prosthetic
Replacement for Fresh Fractures on the Neck of the Femur. Br J Surg 1974;56:229.
JTH, Crothers O. Nailing Versus Prosthesis for Femoral Neck Fractures.
A Critical Review of Long-term Results in Two Hundred and Thirty-nine
Consecutive Private Patients. J Bone Joint Surg Am 1975;57:686.
C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric Fractures of the
Femur: Results of Treatment with the 95° Condylar Blade Plate. Clin Orthop 1989;238:122.
RW, Teal P, Probe RA, et al. Early Experience with the Gamma
Interlocking Nail for Peritrochanteric Fractures of the Proximal Femur.
J Trauma 1991;31:1649.
GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after Displaced
Fractures of the Femoral Neck. A Meta-analysis of One Hundred and Six
Published Reports. J Bone Joint Surg Am 1994;76:15.
DN, Chess JL. Intraoperative and Postoperative Subtrochanteric Fracture
of the Femur Associated with Removal of the Zickel Nail. J Bone Joint Surg Am 1988;70:239.
DB. Fractures of the Neck of the Femur, Dislocation of the Hip and
Obscured Vascular Disturbances Producing Aseptic Necrosis of the Head
of the Femur. Surg Gynecol Obstet 1934;59:415.
GET. A Comparison of Internal Fixation and Prosthetic Replacement for
Recent Displaced Subcapital Fractures of the Neck of the Femur. Injury 1972;5:25.
O, Bjerkreim I, Kolbenstvedt A. Anteversion of the Acetabulum and
Femoral Neck in Normals and in Patients with Osteoarthritis of the Hip.
Acta Orthop Scand 1983;54:18.
O, Hoiseth A, Reigstad A, Fonstelien E. Femoral Neck Angles: A Specimen
Study with Special Regard to Bilateral Differences. Acta Orthop Scand 1982;53:775.
BL, Wakner HW, Dunn WL, et al. Differential Changes in Bone Mineral
Density of the Apendiculum and Axial Skeleton with Aging: Relationship
to Spinal Osteoporosis. J Clin Invest 1981;67:328.
J, Herrara A, Canales V, Serrano S. Epidemiologic Factors, Morbidity
and Mortality after Femoral Neck Fractures in the Elderly. A
Comparative Study: Internal Fixation vs. Hemiarthroplasty. Acta Orthop Belg 1987;53:472.
A. Intertrochanteric Fractures of the Femur. 150° Angle Nail-Plate
Fixation and Early Rehabilitation: A Preliminary Report of 100 Cases. J Bone Joint Surg Am 1963;45:706.
A, Williams EM. The Unstable Intertrochanteric Fracture: Treatment with
a Valgus Osteotomy and I-beam Nail-Plate—A Preliminary Report of 100
Cases. J Bone Joint Surg Am 1970;52:1309.
RG, Gregg JR. Subtrochanteric Fracture Complicating Multiple Pin
Fixation of the Hip: An Orthopaedic Dilemma. Paper presented at the
American Academy of Orthopaedic Surgeons Scientific Program, January
24, 1985, p. 38.
JM, Barrington R. Internal Fixation Versus Hemiarthroplasty for the
Displaced Subcapital Fracture of the Femur. A Prospective Randomized
Study. J Bone Joint Surg Br 1981;63:357.
O, Mölster A, Raugstad TS. Internal Fixation vs. Primary Prosthetic
Replacement in Acute Femoral Neck Fractures: A Prospective Randomized
Clinical Study. Br J Surg 1979;66:56.
JM, Zuckerman JD, Kummer FJ, Frankel VH. Fatigue Failure of the Sliding
Screw in Hip Fracture Fixation: A Report of Three Cases. J Orthop Trauma 1991;5:325.
KH, Deldycke J, Broos PLO, et al. Treatment of Unstable
Peritrochanteric Fractures in Elderly Patients with a Compression Hip
Screw or with the Vandeputte (VDP) Endoprosthesis: A Prospective
Randomized Study. J Orthop Trauma 1995;9:292.
B, Hansson LI, Palmer J, et al. Scintillometric Evaluation of Nailed
Femoral Fracture with Special Reference to Type of Osteosynthesis. Acta Orthop Scand 1993;54:340.
MF, Harrington RM, Keller TS, Van Patten PK. Torsion and Bending
Analysis of Internal Fixation Techniques for Femoral Neck Fractures.
The Role of Implant Design and Bone Density. J Orthop Res 1987;5:433.
MF, Winquist RS, Hansen S. Fractures of the Femoral Neck in Patients
between the Ages of Twelve and Forty-Nine Years. J Bone Joint Surg Am 1984;66:837.
AF, Johnson KD, Johnston DWC, Gill K. A Biomechanical Comparison of
Various Methods of Stabilization of Subtrochanteric Fractures of the
Femur. J Orthop Res 1984;2:297.
RA, Wright PH, Gilbert JA, Taylor DF. Biomechanics of Ender Rods,
Compression Screw, and Zickel Nail in the Fixation of Stable
Subtrochanteric Femur Osteotomies. J Orthop Trauma 1990;4:58.
JT, Moed BR, Cramer KE, Karges DE. Comparison of the Compression Hip
Screw with the Medoff Sliding Plate for Intertrochanteric Fractures. Clin Orthop 1998;348:79.
F, Latta LL, Milne EL. Sliding Characteristics of Compression Hip
Screws in the Intertrochanteric Fracture: A Clinical Study. J Orthop Trauma 1993;7:348.
JD, Sakales SR, Fabian DR, Frankel VH. Hip Fractures in Geriatric
Patients. Results of an Interdisciplinary Hospital Care Program. Clin Orthop 1992;274:213.
JD, Skovron ML, Koval KJ, et al. Postoperative Complications and
Mortality Associated with Operative Delay in Older Patients Who Have a
Fracture of the Hip. J Bone Joint Surg Am 1995;77:1551.