Femoral Shaft Fractures: Retrograde Nailing
accepted method of treatment for femoral shaft fractures, especially
those associated with other injuries. Early attempts at retrograde
nailing with entry portals through the medial femoral condyle led to
comminution and malunion. Moving the starting point to a
centromedullary position produced better results with fewer
complications. Prior to the introduction of locked plates, internal
fixation of comminuted, supracondylar femur fractures was associated
with a relatively high incidence of malunion, nonunion, hardware
failure, and loss of knee motion. For this reason, a retrograde locking
nail was developed. Originally designed as a short nail for distal
femur fractures, full-length nails were ultimately developed to manage
diaphyseal injuries.
fractures at least 5 cm below the bottom of the lesser trochanter down
to the supracondylar femur including fractures with an intercondylar
split. Associated musculoskeletal injuries often favor retrograde over
antegrade femoral nailing. The ability to do a retrograde nailing in a
patient with an ipsilateral acetabulum fracture, which might require a
posterior approach, allows for the femoral shaft to be treated and for
a pristine area around the posterior trochanter for fixation of the
acetabulum fracture.
managed through a single, small incision with placement of a retrograde
femoral nail and an antegrade tibial nail. In multiply injured patients
with other ipsilateral or contralateral lower-extremity fractures,
supine retrograde nailing on a radiolucent table allows either
simultaneous or sequential fixation of other fractures, saving valuable
operating time.
candidates for retrograde nailing. One of the best indications for a
retrograde nail is an ipsilateral hip and shaft fracture. Most authors
recommend independent fixation of both injuries with cannulated screws
or a sliding hip screw proximally followed by a retrograde nail for the
shaft fracture. This approach allows for the best possible treatment of
each fracture without compromising fixation of either one.
femoral shaft fracture in the obese or very muscular patient or in
patients with trochanter lipodystrophy where antegrade nailing may be
difficult. Polytraumatized patients often benefit from rapid
positioning on a
radiolucent
table and freeing the area around the pelvis and abdomen for
simultaneous treatment by other surgical disciplines. Although
antegrade nailing techniques can be done on a radiolucent table rather
than a fracture table, it is still more cumbersome than a retrograde
approach. The supine position allows for more physiologic treatment of
the lungs and brain in a seriously injured patient being resuscitated.
with open growth plates; previous anterior cruciate ligament
reconstruction; or preexisting hardware or prosthesis that would block
a retrograde insertion technique. The use of a retrograde nail in
complex, grades IIIA and IIIB, open femur fractures is controversial
due to the risk of contamination and subsequent infection in the knee
joint. Other treatment modalities, such as bridging external fixation,
may be more appropriate.
patient should be performed. Many patients with femur fractures have
serious associated limb or life-threatening injuries. The condition of
the soft tissues and limb compartments, as well as the neurovascular
status should be clearly documented.
necessary. Dedicated radiographs of the knee and hip are needed to rule
out intercondylar extension or ipsilateral femoral-neck fractures.
Displaced intra-articular fractures are often obvious; however,
traction views or fluoroscopic radiographs in the operating room may be
helpful in identifying subtle injuries to the knee joint. Full-length
films also allow determination of the length and diameter of the
intramedullary canal. Small women, persons of Asian descent, and those
with developmental problems often have very narrow canals. Most
manufacturers do not make retrograde nails smaller than 9 or 10 mm in
diameter. This must be recognized prior to surgery so that either a
nail of appropriate diameter is available or other surgical options are
considered. Many studies have shown that the best results following
retrograde femoral nailing are achieved with full-length nails inserted
to the lesser trochanter. The surgeon should be certain that a full
complement of nails is available at the time of surgery.
approach for nail insertion may be dependent on several factors. The
presence of an intra-articular split in the femoral condyles should be
a priority concern when planning the approach. Visualization and
fixation may be compromised by an ill-placed incision. Cannulated
screws of similar metallurgy to the retrograde nail should be
available, as well as a sliding hip screw for associated hip fractures.
When planning for treatment of an ipsilateral femoral-neck fracture,
important decisions must be made prior to surgery about the table and
patient position during this combined surgical technique. For patients
with multiple fractures, as well as a femoral shaft fracture, proper
positioning of all involved extremities and adequate prepping and
draping can all be done prior to the initiation of surgery if
preoperative planning is performed.
but in isolated injuries in the elderly, a spinal may be utilized.
Retrograde intramedullary femoral nailing is performed with the patient
supine on a radiolucent table. Some authors prefer a bolster under the
torso, but we believe that this can interfere with the determination of
appropriate femoral rotation. With few exceptions, we favor a straight
supine position and anterior positioning of the patella. The limb is
sterilely prepped and draped from the toes to the iliac crest. It is
important to have the entire leg exposed to allow for evaluation of
length and rotation, as well as placement of proximal
anterior-posterior locking screws.
the case. Too little knee flexion does not allow for correct position
of the guide pin or passage of the reamers and nail, which can impinge
on the tibial plateau. Too much flexion can cause the patella to
obscure
the
distal-femoral entry site and leads to excessive shortening in
comminuted fractures. Appropriate flexion can be maintained with a
radiolucent triangle or sheets used as bolsters with the leg maintained
in neutral rotation. For the percutaneous approach, a 2- to 3-cm
incision is made just medial to the patellar tendon. Alternatively, a
patellar tendon splitting approach can be used. Our preference is
medial to the tendon because the incidence of anterior knee pain
appears to be less with this approach. The fat pad and synovium are
bluntly dissected from the intercondylar region by spreading with a
scissors. The intercondylar notch is either visualized through a larger
incision or palpated through the percutaneous incision.
Anterior-posterior fluoroscopy is used, and a trochar-tipped guide pin
is positioned in the center of the notch. Rotation of the fluoroscopy
unit to a lateral view needs to confirm that the guide pin is centered
just at the tip of the inverted V formed by Blumensaat’s line. The
guide pin is then inserted 4 to 5 cm into the distal femoral
metaphysis, with the surgeon making sure that it is centered in both
projections (Fig. 22.1).
The entry portal is created with the use of a cannulated 12- or 13-mm
straight reamer while the patellar tendon is protected with retractors
or a sleeve. The guide pin is then removed (Fig. 22.2).
 |
|
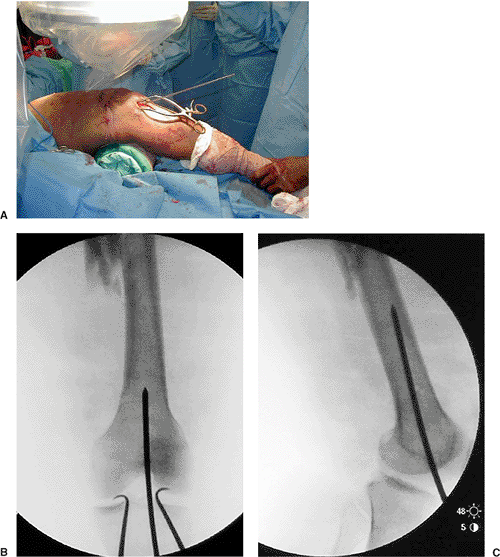
Figure 22.1. A.
Retrograde nailing through a percutaneous incision and the knee flexed over a bolster at 40 degrees of flexion. Guide pin in place. B. Anteroposterior (AP) and (C) lateral fluoroscopic views of guide pin placement. Centered on AP view of femoral condyles and at the top of the intercondylar notch; Blumensaat’s line is viewed on the lateral view. |
 |
|
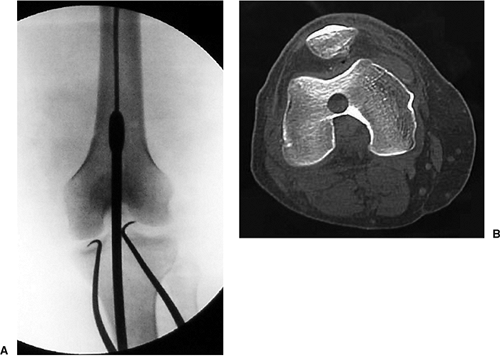
Figure 22.2. A. Rigid reamer inserted over guide pin. B. Retrograde nail starting point on computed tomography (CT) scan. Note that it is just above the intercondylar notch.
|
the tip is inserted into the distal femur where it was previously
reamed. The most difficult part of the surgery may be the reduction of
the fracture. Chemical paralysis from anesthesia is helpful to allow
for traction on the limb to gain length. Reduction of the fracture can
be done by positioning sterile bolsters under the thigh or using
external devices to apply forces in the direction appropriate for
achieving fracture reduction.
device can be placed over the guide rod to manipulate the distal
fragment so that it aligns with the proximal fragment, and the guide
rod is then inserted up to the intertrochanteric region of the femur.
In addition, a terminally threaded guide pin or Schanz pin can be
inserted through the cortex and used as a joystick to help with
reduction (Figs. 22.3 and 22.4). In some cases, a femoral distractor can be very useful.
radiopaque ruler placed on the anterior surface of the leg while slight
traction is pulled (Fig. 22.5). The nail should
span from 5 mm deep to the articular surface of the knee joint to the
level of the lesser trochanter. This span gives the nail a longer
working length and better fit in the isthmus to prevent the nail from
toggling within the intramedullary canal. Recently, a report on the
biomechanics of supracondylar femur fractures suggests that a
full-length nail provides better fixation, less of a stress riser at
the tip, and minimal windshield-wiper effect in the distal femoral
metaphysis.
fractures that may be short at the time of nail length determination.
Some systems have a reverse depth gauge that can be placed over the
guide wire to assess length. For comminuted fractures, the radiopaque
ruler can also be placed on the anterior surface of the uninjured limb,
and a measurement from the epiphyseal scar distally to the top of the
lesser trochanter can give a reasonable estimate and allow for final
assessment of nail and femoral length.
nail diameter will then be individualized. We usually ream 1 mm greater
than cortical chatter and insert a nail 1 mm less than the final reamer
size. The plastic intramedullary tube is then used to exchange the
ball-tipped guide wire for the stiffer guide wire used for nail
insertion. The insertion and
targeting
guide is inserted onto the nail with the outrigger for distal
screw-locking placed laterally. The nail is then inserted with light
blows from a mallet or slap hammer. The patella is placed in a straight
anterior orientation, pointing toward the ceiling.
 |
|
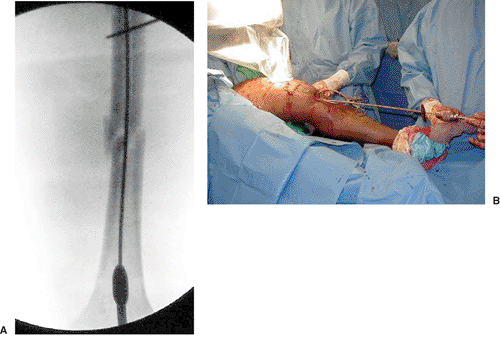
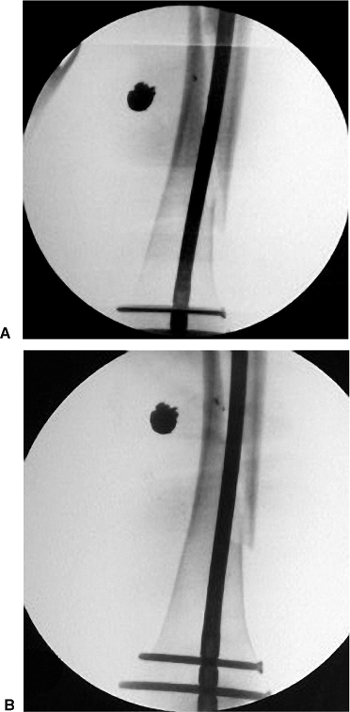
Figure 22.3. A.
Radiograph showing insertion of a reduction tool in the distal femur to facilitate fracture reduction with ball-tip guide rod inside of tool. Note Schanz pin proximally placed in segmental piece to aid in reduction. B. Reduction tool in distal femur with ball-tip guide rod inside. Lateral traction on the segmental piece through the Schanz pin. |
 |
|
Figure 22.4. A. Ball-tip guide rod in distal metaphysis and (B) threaded guide pin in the anterior portion of the segmental fragment to control this segment and help with reduction.
|
 |
|
Figure 22.5. A. Placing guide rod up to lesser trochanter and barrel of sliding hip screw. B. Measurement of nail length using radiopaque ruler.
|
rotation are critical steps prior to final nail seating and locking.
There are rings on the insertion jig that may be visible with the
fluoroscope. The most reliable way to assure that the nail is at least
3 to 5 mm deep to the articular surface is to place the most distal
locking screw at or just above the epiphyseal scar. With most
retrograde nails, the most distal screw hole is 15 mm from the tip of
the nail. One distal locking screw inserted percutaneously through the
distal locking jig is sufficient for diaphyseal fractures with greater
than 50% cortical contact. Two screws should be used for comminuted and
spiral fractures that do not have axial stability (Fig. 22.6).
Distal third femur fractures should also have two distal locking screws
applied to prevent the nail from toggling with flexion and extension of
the knee. Prior to proximal locking, final determination of length must
be ascertained.
slight mallet blows on the insertion handle after distal interlocking
will close the cortical gap. More commonly, comminuted fractures will
shorten during the insertion of the retrograde nail. To help restore
femoral length, a slap hammer device is used after the insertion of the
distal interlocking screws to back slap the nail in the direction of
nail removal. Sometimes length can be sufficiently judged by cortical
alignment. When comminution is extensive, preoperative measurement of
the contralateral limb from epiphyseal scar to the top of the lesser
trochanter with placement of the same length nail to those landmarks
should give proper measurement for restoration of femoral length.
will usually not result in over distraction due to the intact
iliotibial band. Once length has been determined to be appropriate, the
insertion device can be removed. A fingertip placed in the insertion
site should show that the tip of the nail is 3 to 5 mm deep to the
articular surface. The nail should not be prominent by even 1 mm at the
notch because this may adversely affect the patellofemoral joint. With
the limb in neutral rotation and the knee bolster removed, fluoroscopy
of the proximal nail holes in an anterior-posterior direction is
performed. The perfect circle technique of rotating of the limb or
c-arm until round holes are obtained is essential to proximal
interlocking.
A
1- to 2-cm anterior incision is made over the screw hole as determined
by fluoroscopy. The quadriceps fascia is opened sharply with a knife,
and a hemostat is used to spread down to the bone. A trochar, tipped,
short, drill bit is inserted at a 45-degree angle onto the anterior
femoral cortex such that the tip of the drill is centered in the hole.
For those nails with a dynamic slot proximally placed, insertion in
this hole can be done proximally or distally, depending on the fracture
morphology. For axially stable fractures, the dynamic screw can be
placed in the top of the hole to allow for compression with weight
bearing. For unstable fractures, the screw can be placed in the bottom
of the hole to work as a buttress screw to prevent further shortening.
The drill is inserted through the proximal cortex perpendicular to the
head of the fluoroscope, and the drill is removed from the drill bit.
Fluoroscopy can then be used to evaluate the position of the drill bit
in the hole. Minor adjustments to the drill bit can then be made, and
once the bit is centered in the hole, a mallet can be used to gently
push the bit through the hole in the nail. The drill bit is then
attached back onto the drill, and the far, posterior, cortex is
drilled. Careful attention should be made to not plunge too deep with
this drill bit because the sciatic nerve lies posterior to the femur at
this level. A depth gauge is used to determine screw length, and a
locking screw driver is used to insert the proximal screw. If a locking
screwdriver is not available, then an absorbable suture can be tied to
the neck of the screw during insertion to that the screw is not dropped
or lost in the soft tissues of the thigh during insertion. Final screw
seating should be checked by finger palpation and a cross-table lateral
of the limb to assure that the screw is fully seated. Often the screw
will tighten when just entering the far cortex and give the illusion of
final seating of the screw head. One screw is sufficient for most
fractures, with the exception of subtrochanteric fractures where there
is limited isthmal fixation of the proximal fragment (see Fig. 22.6).
 |
|
Figure 22.6. A. Placement of distal locking screws using insertion handle outrigger and jig. B. Using the free hand perfect circle technique for insertion of the proximal locking screw in the dynamic slot in the nail. C. Placement of the proximal locking screw with a locking screwdriver or suture tied around the screw head. D. Frog lateral view obtained in operating room to check the length and bicortical location of the proximal screw. E.
Lateral radiograph demonstrating proper insertion of the retrograde nail deep to the articular cartilage after insertion handle removal. |
patellar-tendon insertion site is closed in layers with absorbable
suture and a routine skin closure. The lateral screw insertion site is
closed in layers starting with the iliotibial band and then the
subcutaneous tissue and the skin. The proximal locking site is closed
only with subcutaneous absorbable suture and skin closure. The wounds
are dressed with sterile pads, and a compression bandage is used from
toes to groin with tape over the anterior proximal locking site. With
the drapes removed, the length, angulation, and rotation of the two
limbs are compared. The ipsilateral knee is also examined for
ligamentous instability.
postoperative period, and continuous passive motion machines are
reserved for multiply injured or head injury patients who are at higher
risk for knee stiffness or heterotopic ossification. Full extension and
flexion greater than 90 degrees should be obtained between 6 and 8
weeks. Weight bearing can be initiated early in axially stable
fractures and is usually delayed 6 to 10 weeks until callus is apparent
on postoperative radiographs in unstable fractures. Most fractures heal
between 3 and 5 months.
filling nails are employed. Reamed canal-sized implants have been shown
to achieve union rates greater than 90%, which equals antegrade
nailing. In patients with delays in union, dynamization can be
performed on axially stable fractures. This is most commonly performed
in fractures that are showing callus but have a gap at the fracture
site with a well-fitting nail. Usually, the proximal screw is removed
to allow the nail to move in a proximal direction with compression of
the fracture site and not toward the knee joint. Pain caused by the
distal screw is common and is often caused by screws that are too long,
but is found in patients in which screws of the proper length were
used. The most distal locking screw is inserted into the trapezoidal
distal femur, and screws that appear with their tips just outside the
medial femoral cortex are usually too long. Sometimes screw heads are
palpable or cause an auditory click on the
iliotibial
band in thin patients. Distal screws can be removed with an outpatient
procedure once union has occurred, or a painful screw may be removed
once abundant callus is visible on radiographs. Knee pain is uncommon
with proper operative technique. In patients with limited knee motion,
we recommend an aggressive physical therapy program for limb
rehabilitation. Full extension and flexion to 120 degrees should be
expected with a well-placed, retrograde, femoral nail. Residual
anterior knee pain is occasionally seen and is most common secondary to
trauma and residual weakness in the quadriceps muscle with patellar
maltracking rather than impingement from the retrograde nail.
fractures can be a problem with either antegrade or retrograde nailing
techniques. For unstable fractures, back slapping of the nail after
screw insertion can help overcome shortening (Fig. 22.7).
For bilateral fractures, by treating the stable fracture first and then
using the same length nail in the same position on the unstable
fracture, surgeons will ensure appropriate length of the limb.
Fractures at the tip of the implant have been reported in osteoporotic
bone with the use of a short nail. Full-length nails are suggested for
all fractures, including those in the supracondylar region (Fig. 22.8).
 |
|
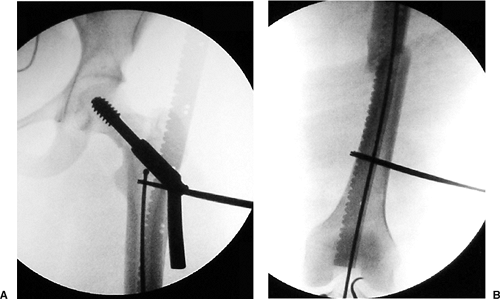
Figure 22.7. A.
Retrograde nailing of gunshot fracture of femur with axially unstable, long, spiral fracture of the femur. Note shortening of femur after insertion of retrograde nail. B. Following distal locking of the insertion jig, back slapping the nail until soft tissues tighten restores femoral length prior to proximal freehand locking. |
 |
|
Figure 22.8. A. Intercondylar-supracondylar femur fracture treated with a lag screw and full-length retrograde nail up to lesser trochanter. B. Diaphyseal fracture after the patient fell. Note tip of a short retrograde nail.
|
P, DiCicco J, Karpik K, et al. Ipsilateral fractures of the femur and
tibia: treatment with retrograde femoral nailing and unreamed tibial
nailing. J Orthop Trauma 1996;10(5):309–316.
BR, Watson JT. Retrograde intramedullary nailing, without reaming, of
fractures of the femoral shaft in multiply injured patients. J Bone Joint Surg Am 1995;77A:1520–1527.
