FRACTURES OF THE TIBIAL PLATEAU
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Patella and
Tibia > CHAPTER 23 – FRACTURES OF THE TIBIAL PLATEAU
The majority of tibial plateau fractures reported in the recent
literature have resulted from high-speed motor vehicle accidents and
falls from a height (7,21,48,50).
Fractures of the tibial plateau are caused by direct axial compression,
usually with a valgus (more common) or varus (less common) moment and
indirect shear forces. The anterior aspect of the femoral condyles is
wedge shaped; with the knee in full extension, the force generated by
the injury drives the condyle into the tibial plateau (47).
The direction, magnitude, and location of the force, as well as the
position of the knee at impact, determines the fracture pattern,
location, and degree of displacement.
 |
|
Figure 23.1. The classic mechanism of injury in tibial fractures is shown.
|
This is because the anatomic axis at the knee joint (which is normally
in 7° of valgus) as well as the mechanism of injury usually causes a
direct force from lateral to medial (30).
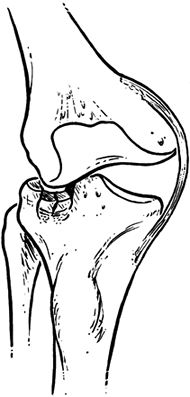
Patient factors such as age and bone quality can also influence the
fracture pattern. Elderly individuals with osteopenic bone are more
likely to sustain depression-type fractures (4) because their subchondral bone is less likely to resist axially directed loads (Fig. 23.2).
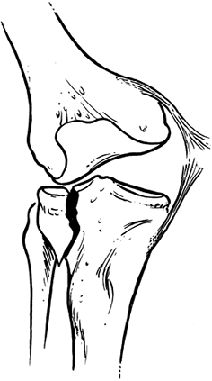
In contrast, younger individuals with denser subchondral bone are more
likely to sustain cleavage-type fractures and have an associated
ligamentous disruption (Fig. 23.3) (26,51,52).
 |
|
Figure 23.2. In pure depression fractures, the cancellous bone absorbs the energy, thus sparing the medial collateral ligament of injury.
|
 |
|
Figure 23.3. In split fractures, the cancellous bone does not compress, thus imparting the energy to the medial collateral ligament
|
differential diagnosis any time a patient complains of pain and
swelling about the knee following major or minor trauma. Decision
making regarding the treatment of periarticular fractures about the
knee depends on knowledge of the mechanism of injury, clinical
stability, radiographic findings, and associated injuries. Initial
evaluation of the knee following trauma includes palpation to elicit
tenderness over a potential fracture or site of ligamentous disruption.
Generally, hemarthrosis is present; however, significant capsular
disruption may lead to dispersion into surrounding soft tissues.
should follow documentation of the skin condition and presence of
swelling. Because many of these injuries are produced by high-energy
forces, the presence of compartment syndrome must be ruled out. If
pulses are not palpable, perform Doppler studies. If the clinical signs
of an impending compartment syndrome (pain out of proportion to the
injury, pallor, pain on passive stretch of the toes, or impaired
neurologic status) are present, compartment pressures must be measured.
Pressures should also be measured in the unconscious patient with a
tense, swollen leg.
with tibial plateau fractures. Injury to the collateral ligaments have been reported to occur in 7% to 43% of cases (2,7,12,20,21,51,52), and ruptures of the anterior cruciate have been reported in up to 23% of high-energy injuries (2).
Furthermore, meniscal injuries have been reported in up to 50% of
tibial plateau fractures; the meniscus may be incarcerated within the
fracture site (21,40,41,48).
Ligamentous injuries may be difficult to diagnose on initial
examination during the acute phase. Varus and valgus stress testing of
the knee in near full extension can be performed under general
anesthesia if one is unable to assess the knee properly in the
emergency room (19). Split fractures of the
lateral plateau have a high incidence of associated ligamentous injury,
because the dense cancellous bone associated with split fractures does
not compress. Energy is therefore not dissipated, and the force is
imparted to the medial collateral ligament.
problematic; thus, any open wound should be evaluated for the
possibility of an open joint injury. Because an open joint injury is an
absolute indication for surgical intervention (2,9,30),
it is incumbent on the treating physician to make the diagnosis. If you
are unsure as to whether the open wound communicates with the joint,
instill at least 50 ml of sterile normal saline into the knee away from
the wound. If fluid extravasation is noted, the diagnosis is confirmed (30).
It should be stated that a negative injection test does not exclude the
possibility of an open joint injury. Exploration of the knee in the
operating room is indicated any time the suspicion for an open joint
wound is significant.
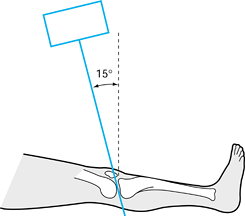
evaluation. The standard knee trauma series includes an anteroposterior
(AP) view, a lateral view, and two oblique views. Owing to the 10° to
15° posterior slope of the articular surface of the tibia, a 10° to 15°
caudally tilted plateau view provides more accuracy in assessing
articular stepoff (Fig. 23.4) (19,37).
In addition to providing an assessment of the fracture patterns,
radiographs often provide evidence of associated ligamentous injury.
Avulsion of the fibular head, the Segund sign (lateral capsular
avulsion), and Pellegrini-Stieda lesion (calcification along the
insertion of the medial collateral ligament) are indicative of
associated ligamentous injury (12,17,19). Stress views may be helpful as well but take care not to displace the fracture further.
 |
|
Figure 23.4.
To obtain a tibial plateau view, the x-ray beam is angle caudally 15°. (From Koval KJ, Helfet DL. Tibial Plateau Fractures: Evaluation and Treatment. Journal of the American Academy of Orthopaedic Surgeons 1995;3:86, with permission.) |
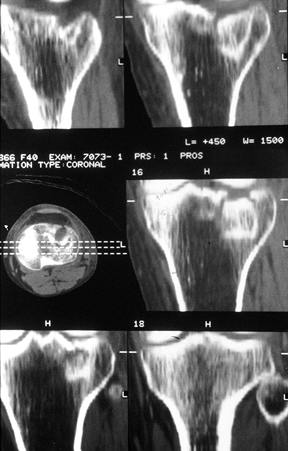
tomography for the evaluation of displaced tibial plateau fractures. CT
scanning with sagittal reconstruction has increased the diagnostic
accuracy in tibial plateau fractures and is indicated in cases of
articular depression (Fig. 23.5) (19,43).
CT scans have been shown to increase the interobserver and
intraobserver agreement of the classification of tibial plateau
fractures (8). Furthermore, these studies are excellent adjuncts in the preoperative
planning of lag screw placement when percutaneous fixation is to be
undertaken. Magnetic resonance imaging (MRI) has recently been
suggested as a method for evaluation of these injuries as an
alternative to CT scan and arthroscopy. MRI theoretically evaluates
both the osseous as well as the soft-tissue components of the injury (6). Currently, however, no clear indication exists for the use of MRI in tibial plateau fractures.
 |
|
Figure 23.5. A CT scan is shown with two-dimensional reconstructions demonstrating a pure depression fracture.
|
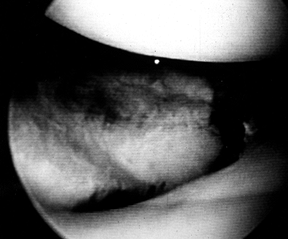
In addition, one can irrigate the joint of any loose debris and
hematoma. However, development of compartment syndrome (related to the
extravasation of arthroscopy fluid) has been reported in the literature
(16,23,40).
 |
|
Figure 23.6.
Arthroscopic view of a split fracture of the lateral tibial plateau. One can obtain good visualization of the articular surface, femoral condyles, and meniscus. |
The majority are very similar, with each system recognizing wedge,
compression, and bicondylar types. The Hohl classification was the
first widely accepted description of tibial plateau fractures (17),
classifying these fractures into displaced and undisplaced. Under the
displaced category, he recognized local compression, split compression,
total condyle depression, and comminuted fractures.
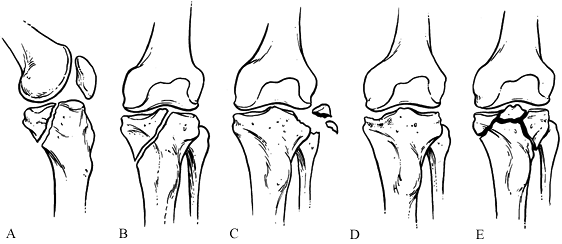
His classification of fracture subluxations of the knee is divided into
five types: Type 1 is a split fracture of the medial tibial plateau in
the coronal plane; Type 2 an entire condyle fracture with the fracture
line beginning in the opposite compartment and extending across the
tibial eminence; Type 3 is a rim avulsion fracture (these fractures are
associated with a high rate of associated neurovascular injury); Type 4
is another type of rim fracture, a rim compression injury, usually
associated with some type of contralateral ligamentous injury; and Type
5 is a four-part fracture with the tibial eminence separated from the
tibial condyles and the tibial shaft (Fig. 23.7) (36).
 |
|
Figure 23.7. The Moore classification of tibial plateau fractures. A: Split fracture of the medial plateau in the coronal plane. B: An entire condyle fracture. C: Rim avulsion fracture. D: A pure compression fracture. E: A four-part fracture.
|
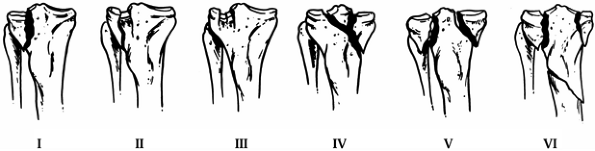
plateau fractures (51,52).
Type I is a pure cleavage fracture of the lateral tibial plateau that
results in a wedge-shaped fracture fragment. Type II is a cleavage
fracture of the lateral tibial plateau in which the remaining articular
surface is depressed into the metaphysis. Type III is a pure central
depression fracture of the lateral tibial with an intact osseous rim.
Type IV involves the medial tibial plateau and is divided into two
subtypes: type A is a split fracture and type B is a depression
fracture. Either type may be combined with a tibial spine fracture.
Type V is a bicondylar fracture with the fracture line often forming an
inverted Y; the metaphysis and diaphysis
remain intact. Type VI is a tibial plateau fracture in which there is
dissociation between the metaphysis and the diaphysis; these fractures
may have varying degrees of comminution of one or both tibial condyles
and the articular surface (51,52).
Honkonen and Jarvinen have recently modified Shatzker’s classification
to take into account residual limb alignment. They divide type VI
fractures into medially and laterally tilted fractures to take into
account functional results in treated fractures with residual
angulation (21).
 |
|
Figure 23.8. Schatzker’s classification of tibial plateau fractures is shown. Types I to IV are defined as follows: I: A split fracture of the lateral tibial plateau. II: A pure depression fracture of the lateral tibial plateau. III: A split-depression fracture of the lateral tibial plateau. IV: A fracture of the medial tibial plateau. V: A bicondylar fracture of the tibial plateau. VI: A fracture of the tibial plateau with metaphyseal-diaphyseal dissociation.
|
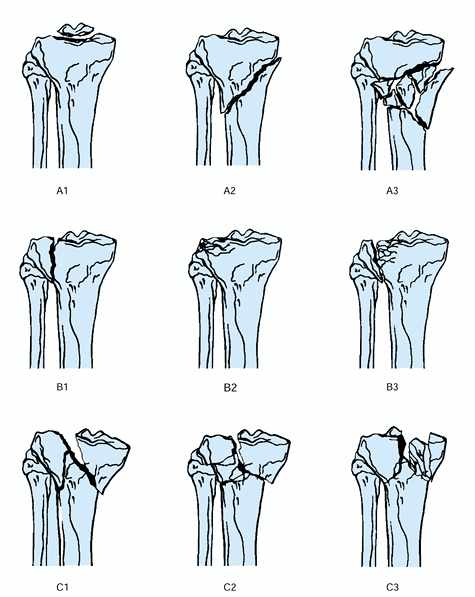
and is most useful as a research tool. Type A fractures are
extraarticular. Type B fractures are partially articular and are
subdivided into three main categories: B1 fractures are pure splits, B2
fracture are pure depression, and B3 fractures are split depression.
Type C fractures are complete articular fractures and are also
subdivided into three subtypes: (a) being articular and metaphyseal
simple, (b) articular simple and metaphyseal multifragmentary, and (c)
articular multifragmentary (39).
 |
|
Figure 23.9. The AO classification of tibial plateau fractures is shown.
|
The indications for nonoperative versus operative treatment of
displaced tibial plateau fractures, however, vary widely in the
literature. Numerous authors have reported excellent results with
nonoperative treatment of displaced tibial plateau fractures (1,11,14,18,24,48,49), whereas others advocate anatomic restoration of the articular surface (7,51,52,54). The degree of articular depression that can be accepted has varied and ranges from less than 2 mm to 1 cm (11,18,45,51).
Most authorities today believe that more than 2 mm of offset in the
weight-bearing portion of the articular surface is not acceptable in
active patients. The need for surgery on tibial plateau fractures can
also be based on instability of more than 10° of varus or valgus in the
nearly extended knee compared with the contralateral side (32,44,45).
This potential instability depends on the status of the rim of the
tibial plateau. Split fractures are more likely to be unstable than
pure depression fractures in which the rim is intact. Open fractures
and fractures associated with vascular injury or compartment syndrome
require urgent surgical intervention.
nonoperatively. Protected weight bearing and early range of knee motion
in a hinged cast-brace are the authors’ preferred method of treatment.
Initiate isometric quadriceps exercises and progressive passive,
active-assisted, and active range of knee motion exercises as the
stability of the fracture permits. Allow partial weight bearing for 8
to 12 weeks, with progression to full weight bearing as tolerated
thereafter.
historical interest. Significant quadriceps atrophy and restricted
range of knee motion are likely to result from prolonged
joint immobilization (18,19).
Reserve treatment in a long leg cast for unreliable patients who cannot
be trusted to bear partial weight; in this instance, the cast should be
applied with the knee flexed to 45°. Cast immobilization may also be
necessary in unstable fractures in which a cast brace is insufficient
and, for some reason, surgery is contraindicated. Apley described the
use of skeletal traction to provide alignment of displaced tibial
plateau fractures yet allow for range of motion of the knee joint (1).
This method involves the use of a Steinmann pin inserted transversely
through the tibia, usually in the distal third below the fracture.
Patients are restricted to bed rest for 6 weeks but allowed active
range of motion exercises of the knee. The major limitations of this
form of treatment include inadequate reduction of the articular surface
and ineffective control of limb alignment (19).
Furthermore, the extended period of hospitalization and recumbency are
not cost-effective in today’s health care environment. If the criteria
for operative treatment are not met, cast bracing has provided
excellent results (11,12,14,50).
before attempting any type of surgical intervention. Preoperative
planning is essential for any complex injury because it forces the
surgeon to understand the “personality” of the fracture and to prepare
an operative strategy mentally. Radiographs of the contralateral
extremity can serve as templates. Traction radiographs often allow
better visualization of individual fracture fragments. Plan all aspects
of fracture reduction and fixation to avoid technical
pitfalls (Fig. 23.10). Furthermore, be certain that all needed equipment and implants are available.
 |
|
Figure 23.10. An example of preoperative templating is illustrated.
|
tibial plateau fractures follow those of other articular fractures.
First should be reconstruction of the articular surface, followed by
reestablishment of tibial alignment. Buttress securely with bone graft
or a bone graft substitute to support depressed articular fragments.
Fracture fixation can involve the use of plates and screws, screws
alone, external fixation, or combinations of these methods. Finally,
adequate soft-tissue reconstruction that includes preservation or
repair, or both, of the meniscus and ligaments may be required (54).
variety of approaches. The surgical approach should provide maximum
visualization, combined with preservation of all vital structures as
well as minimal soft-tissue dissection and osseous devitalization (52).
-
Make the skin incisions for tibial
plateau fractures longitudinal and as close to the midline as possible.
Because the majority of plateau fractures involve the lateral
compartment, a lateral parapatellar incision and arthrotomy is often
used. Medial fractures use a medial parapatellar approach. In either
case, plan the incisions so that implants do not lie directly below the
skin incision. Any flaps that are raised should be full thickness down
to the crural fascia and retinaculum and include the subcutanous fat.
We favor midline skin incisions in bicondylar fractures to allow access
to both knee compartments and facilitate any future reconstructive
procedures. -
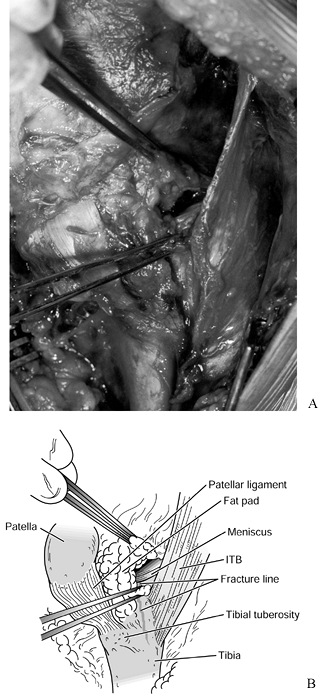
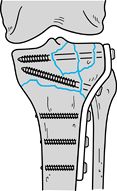
Once the level of the capsule has been reached, make an arthrotomy. The arthrotomy can be submeniscal (52,54) (Fig. 23.11) or vertical, with division of the anterior horn of the lateral meniscus (19,25,41,42); division
P.744
of the anterior horn of the meniscus near its origin has been shown to heal reliably at follow-up arthroscopy (25,41,42).
With either approach, the split fracture component can be displaced
open, and depressed fracture fragments can be elevated. In any case,
all efforts should be made to preserve the meniscus.![]() Figure 23.11. The technique of submeniscal arthrotomy is shown. ITB, iliotibial band.
Figure 23.11. The technique of submeniscal arthrotomy is shown. ITB, iliotibial band. -
Posteromedial fractures of the plateau
can be approached through a separate incision, between the medial
gastrocnemious and semitendinosus and then between the medial
collateral ligament and the posterior oblique ligament (22,33). -
Occasionally, it is necessary to obtain
better exposure of severely comminuted bicondylar fractures. If the
tibial tubercle is a separate fragment and free, it can be reflected
along with the patellar tendon to afford excellent exposure of both
compartments. Because of the difficulties of repair, avoid actual
osteotomy of the tibial tubercle. If the tubercle is intact, incise the
patellar tendon in a Z-plasty fashion with the same resultant exposure (19,52). Following the completion of surgery and repair of the extensor mechanism, protect the patellar tendon using a tension band.
-
Position the patient supine, with a bolster under the knee or on a table where the foot of the table can be dropped.
-
Prep and drape the ipsilateral iliac crest if a need for autogenous bone graft is contemplated.
-
Furthermore, the patient’s position
should take into account the need for intraoperative image
intensification, with the ability to obtain AP, lateral, plateau, and
oblique views. A fully radiolucent table is preferred. -
If arthroscopy is to be used, either a well-padded leg holder or post should be available.
-
Reduction of tibial plateau fractures can
be attained either by direct or indirect means. Direct reduction of the
articular surface and tibial metaphysis can be performed either open (5,7,51,53) or by semiopen means (16,23,40). -
Indirect reduction techniques have been described in the literature (14,15,27,29,35).
These methods use ligamentous and capsular attachments to the fracture
fragments to indirectly reduce the joint surface and align the tibial
shaft (Fig. 23.12). Indirect reduction
techniques have the advantage of minimal soft-tissue stripping, thus
protecting the blood supply to the bone fragment (35).
However, ligamentotaxis does not work on centrally depressed articular
fragments. For badly comminuted fractures, use of a femoral distractor
with threaded pins placed into the femoral condyles and the tibial
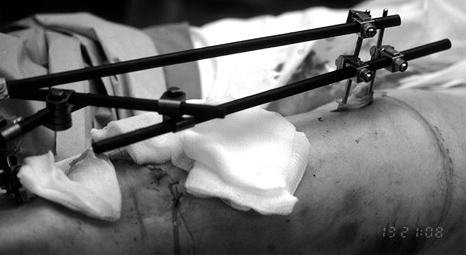
shaft can aid in fracture reduction (29,35,53).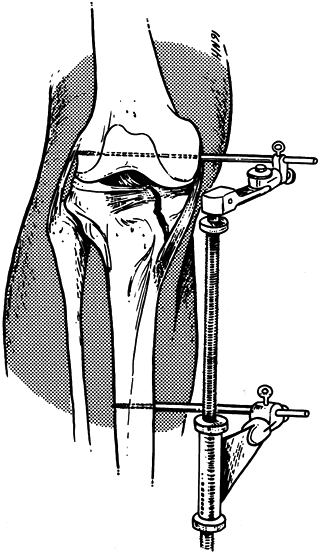 Figure 23.12. The use of the femoral distractor to provide indirect reduction of a split fracture component.
Figure 23.12. The use of the femoral distractor to provide indirect reduction of a split fracture component. -
For unicondylar fractures, place the
femoral distractor on the side of the fracture. For bicondylar
fractures, use two femoral distractors or one distractor and an
external fixator. Keep the threaded pins parallel to the joint surface. -
An alternative method for severe
bicondylar fractures is to place the pins anteriorly, superior to the
patella on the femoral side and distal to the fracture in the tibia.
With this technique, however, the knee cannot be flexed (35). Spanning external fixators can be used in much the same way as the femoral distractor (57). The key is to place the pins far enough away from the fracture site so as not to compromise future reconstructive options (35). -
If segments of articular surface remain depressed following attempted indirect reduction or in a pure depression
P.745
fracture, make a cortical window in the metaphysis, the site of which depends on the location of the depression (Fig. 23.13). Elevate the entire osteochondral segment en masse using bone tamps and punches (15,29,51,52).![]() Figure 23.13.
Figure 23.13.
Depressed segments of articular surface can be elevated using a curved
tamp inserted through the anterior fracture line as shown here or
through a cortical window. -
Following articular surface elevation,
fill the void left by impacted cancellous bone with either autogenous
bone graft, allograft, or bone graft substitute (27,29,51,57).
early 1980s. Arthroscopic management of tibial plateau fractures is
generally indicated for Shatzker Type I, II, and III fractures (16,29,40).
The role of arthroscopy in these fractures is twofold: (a) as a
diagnostic tool to assess the articular surface, menisci, and the
cruciate ligaments accurately and (b) as an adjunct to treatment. For
Type I fractures, pure splits that may be treated with closed reduction
and percutaneous screw placement, arthroscopy permits debridement of
loose joint fragments and repair of meniscal damage in addition to
direct assessment of the articular reduction. For Type II and III
fractures, depressed segments can be elevated through a cortical window
under image intensification and confirmed visually with the arthroscope
(16,29).
treatment of tibial plateau fractures. They can act as a buttress
against shear forces or function in a capacity to neutralize rotational
forces. Owing to the tenuous soft-tissue envelope around the proximal
tibia, thinner plates have been advocated. Recently, percutaneous
plating, which is a more biologic approach, has been described (30a,47a) (Fig. 23.14).
In this technique, the plate is slid subcutaneously without soft-tissue
stripping. Some authors advise against double plating of the tibial
plateau due to an increase in soft-tissue complications (58).
These complications are more likely caused by the higher energy injury,
resulting in greater soft-tissue injury than from double plating (55).
One may need to use double plates for a bicondylar fracture if the far
cortex has an unstable fracture pattern; the use of low-profile plates
with minimal soft-tissue devitalization through a separate incision is
recommended. In such cases, plan to use the major plate on the most
unstable or displaced side, using a much smaller plate and very limited
dissection on the opposite side. An alternative is to use adjunctive
external fixation on the opposite side rather than a plate; however,
pin tract infection is a risk.
 |
|
Figure 23.14. A 45-year-old woman who sustained a Schatzker type VI fracture in addition to a closed femur fracture. A: Initial radiograph. B: CT scan. C: The swollen limb with evidence of healing blisters. D: Reduction of the articular surface and placement of 7.3 cannulated screws. E: A femoral distractor is used to align the tibial shaft followed by subcutaneous insertion of a tibial buttress plate. F: Screws are placed percutaneously under image intensification. G: Final appearance of the limb after placement of a second plate subcutaneously on the medial side. H: Postoperative radiographs.
|
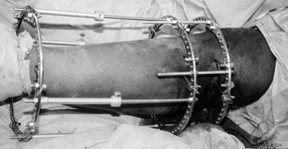
wire, or a combination of the two (hybrids). External fixators may be
placed across the fracture such that thin wires, with or without olive
beads, capture fracture fragments or across the knee joint in a
bridging fashion to make use of ligamentotaxis (38).
The key is placement of the pin or wire 10 to 14 mm below the articular
surface to avoid penetration of the synovial recess posteriorly. This
approach will help minimize the development of a septic joint from a
pin tract infection (46). Anatomic studies have
shown cadavers to have some communication between the tibial-fibular
joint and the knee joint. Thus a transfibular wire could potentially
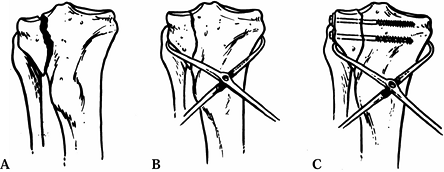
seed the knee joint if a pin tract infection were to develop (46). Place smooth wires parallel to the articular surface and below any percutaneously placed screws (Fig. 23.15). If an Ilizarov construct is used, place half pins and wires into the intact tibial diaphysis below the fracture (13,16,38,57) (Fig. 23.16).
 |
|
Figure 23.15. Example of thin wires placed below percutaneously inserted lag screws.
|
 |
|
Figure 23.16. The use of an Ilizarov external fixator to stabilize a Schatzker VI fracture.
|
half-pin or smooth wire. These constructs can be used temporarily to
allow the soft tissue envelope time to heal (Fig. 23.17).
In certain situations, however, spanning external fixators used in
conjunction with limited internal fixation may be considered definitive
fixation and left on for a longer period of time.
 |
|
Figure 23.17.
A patient with an open tibial plateau fracture with extensive comminution is shown. A bridging external fixator was applied for 10 days until the soft tissues allowed for definitive fixation. |
-
Position the patient supine on a radiolucent table, as described earlier.
-
Make a longitudinal skin incision just
lateral to the midline from 2 cm proximal to the joint line and long
enough to expose the distal extent of the fracture. -
Make a inframeniscal incision through the
meniscotibial ligament and continue this longitudinally distalward
along the anterior border of the anterior compartment to identify the
vertical fracture in the lateral condyle. -
Expose the lateral condyle just enough to apply the smallest buttress plate that will be strong enough to support the plateau.
-
Open the fracture site through this
exposure and hinge the lateral condylar fragment laterally enough to
visualize the depressed central fragment. -
Elevate the central fragment to slightly
higher than an anatomic position and pack an appropriate graft beneath
it to maintain its position. Preliminary fixation with Kirschner wires
may be necessary. -
Now reduce the main condylar fragment
into anatomic position and secure it with a bone holding forceps. The
central fragments should now be aligned anatomically because they tend
to subside slightly during these maneuvers. If not, make adjustments as
necessary. -
Now apply a buttress plate of your choice
with cancellous lag screws through the superior most holes and cortical
screws more distally. Confirm the result with radiographs (Fig. 23.18).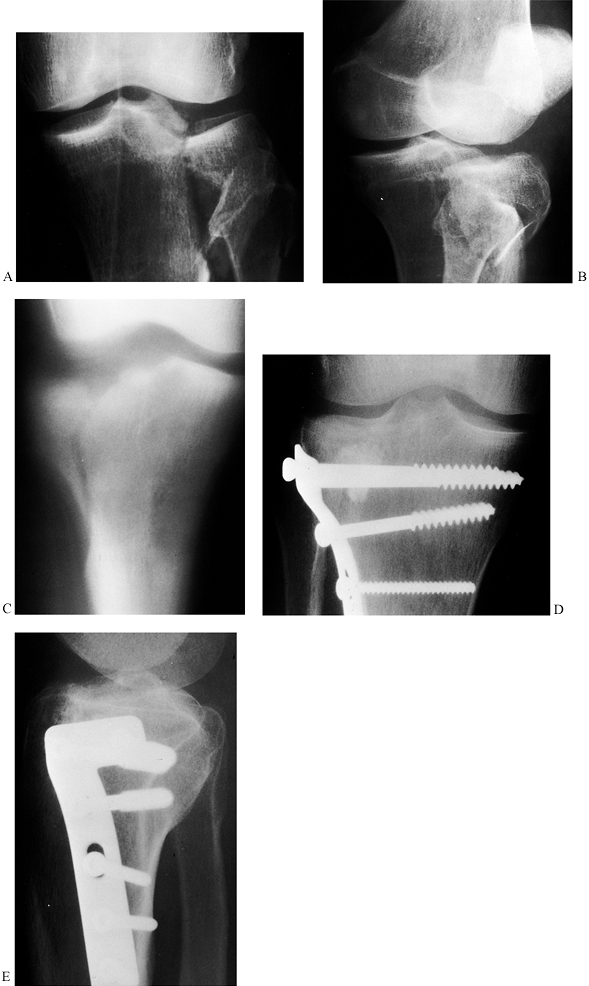 Figure 23.18. A: Type 2 fracture (Schatzker) of the lateral tibial plateau, AP view is shown. B: Oblique view. C: AP tomogram showing the split in the plateau and the depressed central fragment. D:
Figure 23.18. A: Type 2 fracture (Schatzker) of the lateral tibial plateau, AP view is shown. B: Oblique view. C: AP tomogram showing the split in the plateau and the depressed central fragment. D:
Postoperative AP radiograph after elevation of the central fragment,
grafting with corraline hydroxyapatite, and fixation with a buttress
plate. E: Postoperative lateral view. -
Create a tension-free layered closure over a suction drain.
hinged brace. Many authors have reported the benefits of early range of
motion to the knee following tibial plateau fracture (1,18,47).
Continuous passive motion from 0° to 30° may be started on
postoperative Day 1 and increased as tolerated. Physiotherapy should
consist of active and active-assisted range of motion to the knee,
isometric quadriceps strengthening, and protected weight bearing.
Progressive weight bearing depends on fracture healing. Some authors
allow full weight bearing in cases in which there is an isolated
lateral plateau fracture and in which a well-molded cast-brace is used
to unload the affected compartment (11,49).
For patients treated with external fixation, dynamization may be
delayed 4 to 6 weeks following surgery and the fixator may be removed
on radiographic evidence of fracture healing.
fractures can occur whether operative or nonoperative management is
chosen. Complication rates of 10% to 12% (14,51,52) have been reported for patients treated nonoperatively and 1% to 54% (5,24,47,57)
for those treated with surgery. Most complications that occur with
nonoperative treatment are related to prolonged recumbency and include
thromboembolic disease and pneumonia (14,27,47). In addition, peroneal nerve palsy has been reported to occur with cast-brace treatment (14). Finally, pin tract infection can occur in patients if tibial pin skeletal traction is chosen.
treatment of tibial plateau fractures is infection. Infection rates
range from 1% to 38% (5,24,31,57) depending on which technique is employed. Superficial infections occur in 3% to 38% of cases (5,24,47,57) and deep wound infections from 2% to 9.5% (5,24,57).
Skin slough is a risk factor for late infection and is of particular
concern in the proximal leg because of exposure of ligaments, bone, and
implants. Factors relating to skin slough include the severity of the
initial injury, poor surgical timing and improper soft-tissue
techniques with extensive osseous devitalization and use of bicondylar
implants (58).
Deep vein thrombosis prophylaxis includes the use of compression
stockings, low-molecular weight heparin or coumadin; aggressive
treatment of suspected pulmonary embolus is critical.
fixation, posttraumatic arthritis, and malunion. The most common late
complication following operative treatment of tibial plateau fractures
is so-called symptomatic hardware.
The reported incidence is between 10% to 54% (4,27,57).
Hardware may be removed usually 1 year following initial treatment.
Loss of fixation is a complication that can be avoided by proper
preoperative planning. Improper use of implants and the failure to use
bone graft or bone graft substitutes adequately to buttress the
articular surface may lead to loss of reduction or backout of hardware
(loosening of screws or failure of fixation) (30,51). Posttraumatic arthrosis may result from the initial chondral damage or be related to residual joint incongruity (56).
Good functional results can be obtained in the face of poor
radiographic results, however, and they may be due to the preservation
of the meniscus and its ability to bear a substantial portion of the
load of the lateral compartment (12,20,27,32,56).
Malunion can occur either intraarticularly because of inadequate
reduction or loss of reduction or with respect to the articular surface
to the tibial shaft. Patients with malunions with residual varus or
valgus of greater than 10° have been shown to have a higher incidence
of poor long-term functional results (21). Rare complications include popliteal artery lacerations, osteonecrosis, and nonunion (19,53).
determine the choice of treatment. Our indications for surgery in
addition to the absolute indications of open fracture, compartment
syndrome, and vascular injury include instability of the nearly
extended knee of greater than 10° compared with the uninvolved knee and
unacceptable articular incongruence. The timing of surgery depends on
the condition of the soft tissue. Early postinjury swelling represents
hematoma. Within 8 to 12 hours following injury, the soft tissues
become edematous. Fracture blisters may develop and are an indication
of soft-tissue compromise. Earlier surgery in high-energy injuries
through compromised soft tissues is inadvisable and may lead to a
higher incidence of wound problems. Whenever possible, we prefer to use
indirect reduction techniques with pointed bone forceps, a femoral
distractor, and cortical bone windows, as described above.
Recent biomechanical studies have shown no advantage to the addition of
a buttress plate or an antiglide screw in the treatment of this
fracture pattern in nonosteopenic bone (28). A thin plate may be helpful in patients with osteopenia.
 |
|
Figure 23.19. A: Schatzker type I fracture is shown. B: Reduction of the split component with a tenaculum clamp. C: Placement of partially threaded lag screws across the fracture site.
|
addition to the split fragment. We have generally been dissatisfied
with the quality of reduction achieved with indirect reduction and
percutaneous fixation and usually perform a formal open reduction, as
described above. We place 6.5 to 7.3 mm lag screws across the reduced
split fracture fragments. Biomechanical testing has shown that
subchondral Kirschner wires positioned as a horizontal array or cluster
significantly enhance the load-bearing capacity of the articular
surface (3). Therefore, we place three to four
3.5 mm cortical screws in the subchondral region, spread from anterior
to posterior like leaves of a raft to support the articular surface.
Because type II fractures tend to occur in older patients, these
fractures may also require a thin buttress plate (30,52,54).
 |
|
Figure 23.20.
A Schatzker type III fracture treated by elevation of the depressed segment through a cortical window. In this case, the fenestration was made medially to facilitate placement of the curved tamp. |
using a femoral distractor. We usually reduce type IVb fractures open.
Displaced type V fractures (bicondylar) may require two femoral
distractors. If a closed reduction is not possible, these fractures are
reduced open. Internal fixation of fracture types IV to VI generally
requires the use of plate and screws. Type IV fractures require a
medial buttress plate to counteract the shear forces acting on the
medial plateau. We stabilize low-energy type V fractures with medial
and lateral plates (51,55). We treat higher energy injuries with comminution with a combination of limited internal fixation and external fixation (13,34,57).
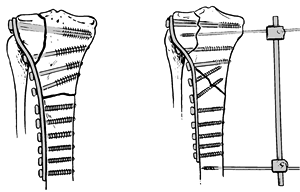
Type VI fractures have metaphyseal-diaphyseal dissociation. Following
articular reconstruction, we stabilize the tibial shaft using either a
single plate, double plates, a single plate and a contralateral two-pin
external fixator or a thin wire fixator. If the fracture is transverse,
a single plate will suffice. Oblique fracture lines exiting the
opposite cortex require a second plate or external fixator to resist
shear forces. When we use a second plate we use minimal dissection (Fig. 23.21) and a thin plate (one half or one third tubular).
 |
|
Figure 23.21.
Treatment of a Schatzker type VI fracture with either a plate (for a transverse shaft fracture) or a plate and a 2-pin ex-fix (for an oblique shaft fracture). |
soft-tissue envelope, we prefer to use a temporary spanning external
fixator. The spanning external fixator is used to allow the soft
tissues to heal in the critically ill patient and in those with severe
soft-tissue injuries. This can be converted to internal fixation or a
hybrid frame as soft tissues allow or maintained as definitive
treatment.
to reduce bacterial contamination, and then perform open reduction and
limited internal fixation of the articular surface. We perform repeat
irrigation and debridement at 48 hours and as often as necessary
thereafter. Injuries with extensive soft-tissue devitalization are
temporarily spanned with an external fixator and converted later to a
hybrid fixator or definitive internal fixation once the soft tissues
have healed. There is no consensus on how long antibiotics should be
continued following open joint injury, but we continue antibiotics for
48 hours following final debridement and wound closure over suction
drainage tubes.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
SK, Agnew SG, Mayo KA, et al. Immediate Internal Fixation of Open
Complex Tibial Plateau Fractures: Treatment by a Standard Protocol. J Orthop Trauma 1992;6:78.
A, Reddy NS, Chaudhury J, et al. The Results of Surgical Management of
Displaced Tibial Plateau Fractures in the Elderly. Injury 1995;26:291.
PS, Klimkiewicz JJ, Luchetti WT, et al. Impact of CT Scan on the
Treatment Plan and Fracture Classification of Tibial Plateau Fractures.
J Orthop Trauma 1997;11:484.
GK, Kontos S, Katsenis D, Dalas A. Treatment of High Energy Tibial
Plateau Fractures by the Ilizarov Circular Fixator. J Bone Joint Surg 1996;78B:710.
PJ, Connolly JF. Closed Reduction of Tibial Plateau Fractures: A
Comparison of Functional and Roentenographic End Results. Clin Orthop 1988;230:116.
EH, Weiner LS, Yang EC. The Use of an Anterior Incision of the Meniscus
for Exposure of tibial Plateau Fractures Requiring Open Reduction and
Internal Fixation. J Orthop Trauma 1996;10:243.
KJ, Sanders R, Borrelli J, et al. Indirect Reduction and Percutaneous
Screw Fixation of Displaced Tibial Plateau Fractures. J Orthop Trauma 1992;6:340.
C, Niclaw T, Schandelmaier P, et al. Minimally Invasive Osteosynthesis
for a Distal Femur Fracture Using a Parapatellar or Percutaneous
Approach and Retrograde Plate Placement. Presented at AAOS Meeting,
1999, Anaheim, CA.
P, Gerich T, Bertram T, et al. Particular Posteromedial and
Posterolateral Approaches for the Treatment of Tibial Head Fractures. Unfallchirurgie 1997;100:957.
MM, Landi S, Kilaghbian V, Randelli P. Shatzker Type VI Tibial Plateau
Fractures Treated with the Ilizarov External Fixator. Bull Hosp Jt Dis 1997;56:46.
JS, Vanslyke M, Moulton MJR. Safe Placement of Proximal Tibial
Transfixtion Wires with Respect to Intracapsular Penetration. Presented
at the Annual Meeting of the OTA. September 29, 1995. Tampa, FL.
LS, Kelley M, Yang E, et al. The Use of Combination Internal Fixation
and Hybrid External Fixation in Severe Proximal Tibial Fractures. J Orthop Trauma 1995;9:244.