Physical Evaluation of the Knee
formulation of the correct diagnosis and initiation of an appropriate
course of treatment. Despite many advances in laboratory and imaging
technology, a thorough history and physical examination remains the
most effective instruments in achieving these goals. The clinician may
establish a provisional diagnosis early in the patient encounter after
hearing only the patient’s presenting complaint and history of present
illness. A detailed history will direct the focus and extent of the
physical examination and aid in refining the diagnosis. Close
interaction with the patient during the history and physical
examination promotes accurate assessment of the patient’s level of
disability and formulation of an individualized treatment plan
appropriate for their expectations and goals for recovery.
explored in a clear, systematic fashion and include discussion of
location, timing, quality, severity, and aggravating/relieving factors.
Pain is the most common complaint that drives orthopaedic patients to
seek medical evaluation. Asking the patient to point to the most
painful area of the knee is a simple way to determine the anatomic
location of the symptoms. The timing of onset should be explored,
because symptoms may start insidiously and slowly progress with a
waxing and waning course, or may start suddenly after a major or minor
traumatic event. The pattern of symptoms may provide immediate insight
regarding a presumptive diagnosis. For example, initially
osteoarthritis may cause aching pain that localizes to one area of the
knee, occurs only after prolonged weight-bearing activities, and is
relieved by short periods of rest. This may be differentiated from
early pain owing to inflammatory arthritis, which may be more diffuse,
constant, and unrelieved by rest. Besides pain, the presence of
mechanical symptoms and subjective instability should be reviewed.
Locking, catching, and popping are suggestive of a meniscal tear, loose
body, or focal lesion of the articular surface. Instability can be
caused by true ligamentous insufficiency or may be owing to reflex
inhibition of the quadriceps from knee pain or effusion. It is
important to inquire about past events specific to the joint, as
patients may not readily recall childhood illnesses or conditions that
affected the knee, and they may not mention previous minor surgical
interventions such as arthroscopy.
paramount. Informed discussions regarding risk-benefit ratios of
potential conservative and surgical treatment options cannot take place
until this is established. Functional deficits should be evaluated in
the context of the patient’s baseline level of physical activity
including activities of daily living, occupational and work-related
activities, and leisure activities (Table 16-1).
As symptoms worsen patients typically exhibit progressive activity
modification and adaptive mechanisms, such as using assistive devices
for ambulation (cane, walker), using the hands to assist in rising from
a chair, and altering stair climbing technique or avoiding stairs
altogether. Standardized physician-administered (e.g., Knee Society
Clinical Rating System) and patient-administered (e.g., Western Ontario
and McMaster University Osteoarthritis Index) rating scales can be
useful in evaluating patients’ functional deficits. Perceptions
regarding level of disability may vary greatly between patients with
different occupations or cultural backgrounds. Because of the physical
demands of his work, a laborer may perceive himself to be disabled
earlier in the disease process than a sedentary office worker. Some
patients tolerate lifestyle changes more effectively than others and
may be willing to change careers or give up favorite leisure activities
to avoid surgical treatment.
prescribed and unprescribed, should be discussed. Patients will often
fail to mention treatments such as over-the-counter nonsteroidal
anti-inflammatory medications and self-directed therapeutic exercise.
Discovering the
frequency,
duration, and efficacy of all prescribed interventions, including
activity modification, orthotics, physical therapy, pain and
anti-inflammatory medications, and injections, is important for
determining the next step in treatment.
|
TABLE 16-1 History: Assessing Functional Deficits and Disability
|
|
|---|---|
|
and may be included in the history of present illness. Specific inquiry
regarding constitutional symptoms may uncover fever, anorexia, weight
loss, fatigue, and generalized morning stiffness, which are indicative
of an inflammatory condition such as rheumatoid arthritis or infection.
The review of systems should also cover other possible sources of knee
symptoms, including the neurovascular system, spine, and adjacent
joints. The hip and spine are common sources of referred pain to the
knee (Fig. 16-1). The review of systems should
also be used to identify medical issues that require attention prior to
any surgery, such as undiagnosed cardiac or respiratory disease and
recent or ongoing infections, particularly of the genitourinary tract
and oropharynx.
 |
|
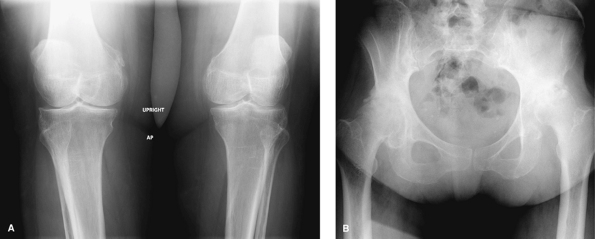
Figure 16-1 Radiographs of a 54-year-old patient referred for treatment of severe bilateral knee pain. A:
Standing anteroposterior radiograph of both knees demonstrates mild to moderate osteoarthritis. Note the oblique view of both knees, as the patient could not internally rotate her hips to neutral for the study. B: Anteroposterior radiograph of the pelvis demonstrates severe arthrosis of both hip joints. Staged bilateral total hip arthroplasty resulted in complete resolution of her symptoms. |
social histories will offer diagnostic clues as well as information
that dictates available treatment options and the manner in which they
are executed. The medical history may reveal an underlying systemic
inflammatory condition as the cause for the knee condition and preclude
nonarthroplasty surgical options. An extensive medical history,
especially cardiac, may eliminate surgical options altogether. A review
of the patient’s medications may identify active medical conditions the
patient failed to discuss previously. In addition, make note of any
medications that should be discontinued perioperatively, such as
nonsteroidal anti-inflammatory agents, anticoagulants, and
disease-modifying antirheumatic drugs. The social history should
include details of the patient’s current living conditions and whether
the patient will have adequate assistance at home after hospital
discharge. The patient’s use of alcohol, tobacco, or illicit substances
must be documented accurately, as these agents may necessitate
alterations in perioperative medical management or possibly disqualify
the patient from surgical intervention.
evaluation of the patient presenting with knee symptoms must be
completed in a systematic fashion. The order and organization of the
exam is a matter of personal preference, but in general must include
inspection, palpation, range of
motion,
ligamentous exam, and neurologic and vascular evaluation. The
examination should include evaluation of both knees. Normal findings
are most frequently symmetrical, so asymmetry may indicate the presence
of pathology. To minimize guarding during examination of the affected
knee, examine the uninvolved knee first. Avoid areas of known
tenderness and exacerbating maneuvers until as late in the exam as
possible.
clinician lays eyes on the patient. Briefly observing how the patient
moves on the way to the examination room may provide a more candid
glimpse of the patient’s gait and reliance on assistive devices than
when he or she is asked to ambulate during the formal exam. Much can be
learned regarding a patient’s level of physical dysfunction and
disability by general observation during the interview as well as
during the formal examination. General appearance and body habitus must
be noted. Observe the patient’s posture of the spine, hips, and knees
while seated. While removing shoes and socks and getting on and off the
exam table, the patient may exhibit abnormal movement to compensate for
pain or stiffness. Watch carefully for facial expressions and wincing
that indicate pain.
standing. Inspection of the spine may reveal a scoliosis or alteration
of normal lumbar lordosis with associated paravertebral spasm. Check
the range of motion of the lumbar spine with flexion, extension, side
bending, and rotation. Patients with osteoarthritis of the lumbar spine
often experience lumbar pain with extension. The bony landmarks of the
pelvis can be palpated to assess for pelvic obliquity. A fixed pelvic
obliquity owing to lumbosacral disease will not correct when a block is
placed under the apparently short limb. Abductor weakness, often
associated with hip pathology, can be recognized with the Trendelenburg
test. During a single leg stance, the abductor muscles on the
supporting extremity contract to maintain a level pelvis. A positive
test occurs when the abductors are not strong enough to support the
body’s weight and the hemipelvis opposite the supported limb drops
toward the floor.
some indication of the location of the knee pathology. Genu varum
suggests involvement of the medial compartment, whereas genu valgum
suggests involvement of the lateral compartment. During gait these
deformities may prove to be dynamic, with worsening of the varus and
valgus deformities during stance phase observed as lateral and medial
thrusts at the knee, respectively. The presence of a thrust in the
setting of osteoarthritis has prognostic implications, as these knees
demonstrate a propensity for disease progression. A dynamic recurvatum
deformity during stance phase should alert the clinician to the
possibility of an underlying neurologic condition, extensor mechanism
dysfunction, or significant ligamentous laxity. Posture of the ankles
and feet should not be overlooked. Hindfoot bracing for a flexible
planovalgus deformity of the foot and ankle may provide symptomatic
relief for an ipsilateral valgus knee.
component of the examination. The patient’s effort to reduce joint load
at the knee can result in many compensatory gait changes. Pain during
weight bearing causes the patient to limit the amount of time spent in
stance phase of gait, producing an antalgic gait (classic limp), which
is the most common adaptive gait pattern. Decreased cadence may be
observed, which effectively reduces all external moments on the
affected knee. Reduced stride length results from a decrease in forward
reach of the involved extremity in late swing phase, which diminishes
the external sagittal plane moment at the knee during heel strike. An
out-toeing gait may be observed in patients with painful varus
osteoarthritis of the knee, which reduces the adduction moment at the
knee by shortening the moment arm. Likewise, patients may lean the
trunk toward the affected weight-bearing extremity to reduce the moment
arm between their center of gravity and the limb’s mechanical axis.
This should not be confused with the Trendelenburg lurch observed with
hip pathology and concurrent abductor weakness and dysfunction.
exam can be completed with the patient lying supine before focusing on
the knee. Patients with a lumbar radiculopathy may exhibit tenderness
in the region of the sciatic notch. The clinician should perform
maneuvers that place the sciatic nerve under tension, including the
straight leg raise and contralateral straight leg raise tests. Examine
the hips, starting with palpation of the greater trochanter. Localized
tenderness suggests greater trochanteric bursitis, which can present
with referred pain to the lateral thigh and occasionally the lateral
aspect of the knee. The ability to perform an active straight leg raise
against gravity and added resistance should be tested. Groin and
anterior hip or thigh pain with this maneuver may suggest
intra-articular hip pathology. Active side-lying hip abduction may
produce similar symptoms, and patients with advanced hip disease may
not be able to overcome gravity. Passive hip motion may also produce
groin and thigh pain. Loss of hip motion, especially flexion and
internal rotation, is a strong indicator for the presence of advanced
hip pathology.
inspection of the lower extremities should be performed. Muscle tone,
atrophy, and defects in the thigh and calf should be noted. Recording
thigh and calf circumference at fixed distances above and below the
patella allows objective measurement of muscle atrophy. The presence
and severity of peripheral edema should be noted, along with any
pretibial skin changes or varices associated with chronic venous stasis.
reassessed. In thin patients, varus and valgus alignment can be
quantified with a goniometer centered on the anterior aspect of the
patella. Deformities of the thigh and lower leg should not be
overlooked. Many patients will fail to mention remote trauma and
surgery in their history. Healed scars should be discussed with the
patient, because they may indicate the presence of posttraumatic or
surgical deformities that are not outwardly visible, especially in
overweight and obese patients. Scars about the knee may provide insight
regarding the underlying diagnosis and should be accurately documented
for preoperative planning. Skin rashes
may
suggest a systemic cause for the patient’s knee pathology. When present
over the knee, rashes are associated with increased risk of surgical
site infection and should be treated prior to operative intervention.
assessed with the patient supine and the knee in extension and in
flexion. Knee effusions can be assessed by compressing the
suprapatellar pouch and assessing ballottement of the patella.
Effusions must be differentiated from synovial thickening or bogginess,
which suggests inflammatory arthritis. Although nonspecific, slight
skin warmth over the knee relative to the adjacent calf and thigh can
indicate the presence of a generalized synovitis. Localized swelling
may represent the site of isolated pathology or may be an indicator of
a more remote or generalized process. For example, localized medial
joint line swelling may be identified in the presence of a meniscal
cyst with an underlying meniscal tear. In contrast, swelling and
fullness in the popliteal fossa at or medial to the midline commonly
represents a popliteal (Baker) cyst. A popliteal cyst can be associated
with any process that produces a chronic effusion, such as a remote,
isolated process that results in synovitis, or a generalized condition
such as inflammatory arthritis.
gross anatomy of the knee joint is imperative for diagnosing underlying
knee pathology. The normal anatomic landmarks of the anterior knee may
be obscured by a large knee effusion or diffuse soft tissue swelling.
Bony landmarks should be identified and palpated, including the femoral
epicondyles, fibular head, tibial tubercle, patellar margins, and
medial and lateral joint lines. Bony thickening at the joint line
suggests the presence of osteophytes. Note areas of localized
tenderness. Soft tissue structures adjacent to or crossing the knee
joint, such as the pes anserine bursa and hamstring tendons, are often
significant pain generators and should not be ignored. The integrity of
the extensor mechanism can be checked with an isometric quadriceps
contraction and straight leg raise.
position. By convention, full extension is 0 degrees, with up to 10
degrees of hyperextension considered normal. Flexion in the normal
adult knee is to approximately 135 or 140 degrees, with 105 degrees
required for normal performance of activities of daily living in
Western societies. Comparison of active and passive range of motion is
necessary to distinguish between joint contracture and extensor lag. A
flexion contracture is identified by the inability to passively
position the knee in full extension. Causes include soft tissue
contracture such as hamstring and gastrocnemius tightness, and
mechanical block from a meniscus tear, loose body, or osteophyte
formation. A discrepancy in active and passive extension represents an
extensor lag and may be attributable to pain or extensor mechanism
dysfunction from weakness or disruption. A knee with a large joint
effusion assumes a 15- to 25-degree resting position and can cause loss
of both active and passive flexion and extension. During range of
motion assessment, crepitus is a common finding and may be localized to
a particular compartment by palpation of the knee.
the patient standing. The Q-angle (quadriceps angle), which is the
acute angle formed by intersecting lines drawn from the center of the
tibial tubercle to the center of the patella and from the center of the
patella to the anterior-superior iliac spine, is a measure of the
lateral pull of the quadriceps on the patella. A Q-angle >15 to 17
degrees is associated with altered patellofemoral mechanics and
anterior knee pain. Complex torsional deformities of the lower
extremity, most commonly increased femoral anteversion, can be
associated with an increased Q-angle and should be evaluated during
assessment of hip motion. Tracking of the patella in the femoral sulcus
should be observed during gait and with both active and passive knee
extension. Excessive lateral movement of the patella as it exits the
femoral sulcus during terminal knee extension is known as the J-sign.
Typically the patella does not articulate with the femoral sulcus until
the knee is flexed 25 to 30 degrees, so patellar tilt and
medial-lateral patellar glide should be assessed with the knee in a
slightly flexed position. Lack of patellar mobility, as well as lateral
tracking with crepitus as the knee flexes past 30 degrees, may indicate
the presence of patellofemoral arthritis. Patella alta and baja can be
assessed clinically with the knee flexed 90 degrees over the end of the
exam table. Tenderness of the medial and lateral facets of the patella
can be evaluated, but may be falsely positive in the presence of
interposed synovitis.
the medial and lateral joint lines. Tenderness at the apex of a
meniscal tear is a common finding owing to its peripheral nerve fibers
and localized synovitis. Numerous provocative tests exist for
evaluation of the menisci, most of which attempt to reproduce pain or
palpable clicks by trapping the abnormally mobile or torn meniscus
between two joint surfaces. Of these, the McMurray test is probably the
most widely used. With the patient supine, the knee is brought into
deep flexion and maximal external rotation with one hand on the foot.
The opposite hand is placed on the knee with the fingers over the
posteromedial joint line, and the knee is brought into extension while
a varus force is applied to the knee. Posteromedial pain and a palpable
or audible click indicate a positive test. The maneuver can be repeated
for the posterolateral meniscus by internally rotating the tibia and
applying a valgus force as the knee is passively extended.
establishing a diagnosis and formulating potential conservative and
operative treatment plans. The clinician must be able to distinguish
isolated ligament deficiency from complex and rotational instability
patterns. However, exhaustive review of the many specific tests for
ligament integrity and complex instability patterns of the knee are
beyond the scope of this chapter. Simple evaluation of the cruciate and
collateral ligaments is presented here. The reader should refer to a
comprehensive source for a complete review of the ligamentous
examination of the knee.
to anterior movement of the tibia on the femur. Its integrity is best
evaluated with the Lachman and anterior drawer tests.
The
Lachman test is performed with the knee in 30 degrees of flexion. With
one hand stabilizing the femur, anteriorly directed pull is applied to
the tibia. A positive test results in excessive anterior translation of
the tibia with a soft end point. In knees that are difficult to
examine, such as those of obese patients, or in the setting of acute
pain or swelling, the anterior drawer test may be useful. With the hip
flexed 45 degrees and the knee flexed 90 degrees, the foot is
stabilized on the exam table and again anteriorly directed pull is
applied to the tibia. The posterior cruciate ligament is the primary
restraint to posterior movement of the tibia on the femur. It is best
evaluated with the posterior drawer test, performed with the extremity
in the same position used for the anterior drawer test. A positive test
is marked by posterior subluxation of the tibia on the femur when a
posteriorly directed force is applied to the anterior tibia.
applying simple varus and valgus stresses to the knee in both full
extension and again with the knee flexed 30 degrees. In full extension,
the collateral ligaments, posterolateral capsule, and posteromedial
capsule are all in a taut position. Therefore, varus and valgus
stresses applied with the knee in full extension tests the integrity of
the collateral ligaments as well as the posterolateral and
posteromedial capsular structures. The posterior capsular structures
relax when the knee is flexed 30 degrees, better isolating the
collateral ligaments in resisting varus and valgus stresses. The
cruciate ligaments are also taut in extension, so the presence of
significant laxity to varus or valgus stress in full extension suggests
cruciate ligament disruption in addition to collateral ligament
disruption.
varus-valgus instability, the clinician must distinguish true
ligamentous insufficiency from pseudolaxity. For example, varus knees
with osteoarthritis typically exhibit articular cartilage and bone loss
in the medial compartment. Laxity to varus stress could represent
lateral collateral ligament insufficiency or rotation of the tibia into
varus as the medial femoral condyle settles into the defect in the
medial tibial plateau. Conversely, laxity to valgus stress may
represent correction of varus alignment as the tibia rotates back to
neutral position. Inability to passively correct a coronal plane
deformity may indicate the presence of long-standing disease with
secondary medial or lateral soft tissue contracture that requires
release at the time of reconstruction.
not be neglected. Neurologic evaluation should include muscle testing,
sensory examination, and assessment of deep tendon reflexes. Prior
inspection should have identified atrophy or loss of muscle tone in the
thigh and leg. Strength testing is performed by resisted isometric
contraction of all major muscle groups, including hip flexion,
extension, and abduction; knee flexion and extension; and ankle
dorsiflexion and plantarflexion. Sensation can be evaluated by testing
light touch, paying special attention to deficits in a dermatomal
distribution. Deep tendon reflexes can be tested at the knee and ankle.
The patellar reflex is predominantly an L4 reflex, and the Achilles
reflex is an S1 reflex. Vascular assessment must include examination of
the skin for signs of peripheral vascular disease, such as smooth shiny
skin with hair loss, skin and subcutaneous soft tissue atrophy, and
ulcerations. Palpation of peripheral pulses should include femoral,
popliteal, posterior tibial, and dorsalis pedis pulses.
N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a
health status instrument for measuring clinically important patient
relevant outcomes to antirheumatic drug therapy in patients with
osteoarthritis of the hip or knee. J Rheumatol. 1988; 15:1833-1840.
JP, Hudak PL, Hawker GA, et al. The moving target: a qualitative study
of elderly patients’ decision-making regarding total joint replacement
surgery. J Bone Joint Surg Am. 2004; 86:1366-1374.
