Scapular Fractures
between the upper extremity and the axial skeleton. This highly mobile,
thin sheet of bone articulates in three different joints: with the
humerus in the glenohumeral joint, with the clavicle in the
acromioclavicular joint, and with the thorax in the scapulothoracic
joint. To accomplish a full range of shoulder motion, a smooth
coordination is required of motion in all three articulations.
Therefore, a complex interaction of several muscles that envelope the
scapula is necessary.146 Besides its
assistance in the movements of the arm in the shoulder joint, the
scapula has two other functions. It is a mobile platform for the
humeral head and upper extremity to work against, and it serves as a
point of attachment for muscles, tendons, and ligaments.62
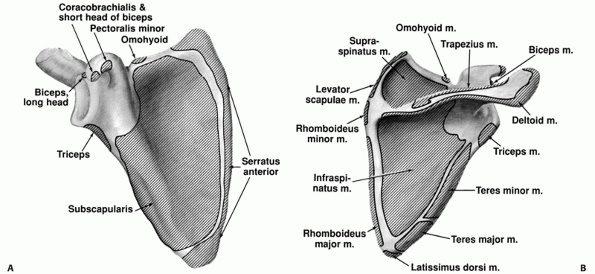
No less than 18 different muscles insert on or originate from the
scapula allowing six basic movements of the shoulder blade over the
posterior chest wall: elevation, depression, upward rotation, downward
rotation, protraction, and retraction.63
high-energy trauma with a high incidence of significant associated
(local and remote) injuries.3,67,79,115,116,169,184,191
These associated injuries are often major, multiple, and sometimes
life-threatening, therefore needing priority in treatment. The relative
infrequency (prevalence 1 %) and “benign characteristics” of a scapular
fracture probably explain the limited attention in the literature.78
closed means. One of the earliest descriptions of treating scapular
fractures was published in 1805 in Desault’s treatise on fractures.
Since then, it has been suggested in the literature that over 90% of
scapular fractures are non- or minimally displaced and do well with
conservative treatment.79,115,184
This observation, however, has been based on the treatment of scapular
fractures in general and its relevance is therefore very limited. A
more differentiated approach is necessary as good results are not
guaranteed with exclusively conservative treatment.8 Recent literature is more focussed on the results of conservative79,115 or operative treatment41,42,61,66,74,84,98,99,112,132,133,156
with regard to specific fracture types. This contrasts with
publications before the 1990s which were particularly focussed on the
trauma mechanism and associated injuries.115,116,169,184
Specific types of scapular fractures are severe injuries that may
result in significant shoulder dysfunction. There are a few reports on
poor
prognosis after conservative treatment of displaced glenoid, scapular neck, coracoid, and acromion fractures.1,77,127
Along with technical refinement of diagnostic tools, more attention is
currently paid to these fracture types as demonstrated by the rising
number of publications on this subject.
This direct force may cause fractures in all anatomic areas of the
scapula. Other mechanisms are indirect injuries: (i) traction by
muscles or ligaments may induce avulsion fractures of the acromion or
coracoid, which in rare cases are caused by a seizure or an electrical
shock110,166; and (ii) impaction of the humeral head into the glenoid fossa which may induce glenoid and some scapular neck fractures.
are the main cause of scapular fractures (occupants of motor vehicles
in about 50% of cases1,8,115 and pedestrians in 20%3,115).
Other causes are motorcycle accidents, fall from heights, crush
injuries, or sporting activities (horseback riding, skiing, and contact
sports).
hence scapular fractures are commonly associated with concomitant
injuries. Research shows that 61% to 98% of scapula fractures have
associated injuries.1,3,17,21,79,97,115,116,165,169
These associated injuries may be multiple and may need priority in
treatment. As a result, diagnosis and treatment of scapular injuries
may be delayed or suboptimal.
reported that may be life-threatening, such as pneumothorax (9% to 38%),3,45,118,169 pulmonary contusion (8% to 54%),45,116,169 arterial injury (11%),45,169 closed head injuries (20% to 42%),79,115 and splenic or liver lacerations 3% to 5%.116 Brachial plexus injury is present in 5% to 13%3,45,79,115,169
and is often the most important prognostic factor with regard to the
final clinical outcome, whether fracture treatment be conservative or
otherwise. The reported mortality rate of patients with scapular
fractures from the concomitant injuries varies between 2% and 15%.115,169,191
analyzed the associated injuries of 160 cases in 11 different studies.
Rib fractures were the most common associated injury, followed by head
and chest injuries. Fractures in remote anatomic areas were found in
nearly 20% of patients. To determine the significance of scapular
fractures in blunt trauma, Stephens161
compared two matched groups of patients with and without scapular
fractures. Except for a significantly higher incidence of thoracic
injuries in the group with scapular fractures, he found no difference
in mortality or incidence of neurovascular injuries. Veysi179
reported in 2003 that patients with scapula fractures have more severe
underlying chest injuries and overall injury severity scores (ISS).
However, these findings, which were confirmed by other authors,161,183
did not correlate with a higher rate of intensive therapy unit
admission, length of hospital stay, or mortality. There is no clear
correlation between the number and severity of associated injuries and
the type of scapular fracture. Nevertheless, Tadros165
found in a prospective study that the ISS and abbreviated injury score
for chest injuries are higher and posterior structure injuries are more
frequent in patients with fractures involving multiple scapular regions.
to the presence of other, sometimes very severe injuries. Severe chest
injury should also raise suspicion of a possible scapular fracture.108
with the arm adducted along the body and will protect the injured
shoulder from all movements.
crepitus, and local tenderness. The ecchymosis is in general less than
expected probably because the scapula is protected by a thick layer of
soft tissue. Active range of motion is restricted in all directions.
Abduction in particular is very painful.
in 1956 that the rotator cuff function is weak and very painful
secondary to inhibition from intramuscular hemorrhage. This has been
described as a “pseudorupture” of the rotator cuff and usually resolves
within a few weeks. When a scapular fracture is diagnosed, it is
important to perform a careful neurovascular examination to rule out
arterial injury and/or brachial plexopathy.
Life Support (ATLS) principles, specific radiographic evaluation of the
injured shoulder is indicated as soon as the patient is in a stable
condition. Associated injuries requiring urgent treatment may force the
treating surgeon, particularly in polytrauma patients, to evaluate the
chest only by a routine supine chest radiograph. This is the earliest
opportunity to identify a scapular fracture. Harris68
pointed out in a retrospective analysis of 100 patients with major
blunt chest trauma that the scapular fracture was diagnosed on the
initial chest radiograph in only 57 of 100 patients and, although
present, was not recognized in 43%. Particularly extensive associated
chest injuries may overshadow the scapula with a delay in diagnosis as
a result.164
visualize radiographically. Except for the chest radiograph, a true
anteroposterior (AP) view, perpendicular to the plane of the scapula, a
lateral, and an axillary view are recommended. A true axillary
projection of the glenohumeral joint and scapula is ideally performed
with the arm in 70 to 90 degrees of abduction, which might be very
painful for the patient in the acute situation. Alternatives for this
view are the Velpeau axillary lateral view12 (see Fig. 39-6) or the trauma axillary lateral view,170
which can be taken while the patient is supine. In case of a complex
shoulder injury with a double disruption of the superior shoulder
suspensory complex (SSSC) (Fig. 37-1), a weight-bearing AP projection of the shoulder is recommended by Goss.60
three-view scapula trauma series, but special views may be necessary
for selected fracture types. The Stryker notch view is useful for
coracoid fractures (see Fig. 39-8) while the apical oblique view48 and the West Point lateral view147 are useful for glenoid rim fractures. In cases of scapular fractures with multiple fracture
lines and particularly significant displacement, a computed tomography
(CT) scan is recommended, although the additional value is not clear in
every fracture type.113
It is, however, useful to assess the size, location, and degree of
displacement of fragments in coracoid, acromion, and glenoid fractures.
In glenoid fractures, it is also helpful to evaluate the position of
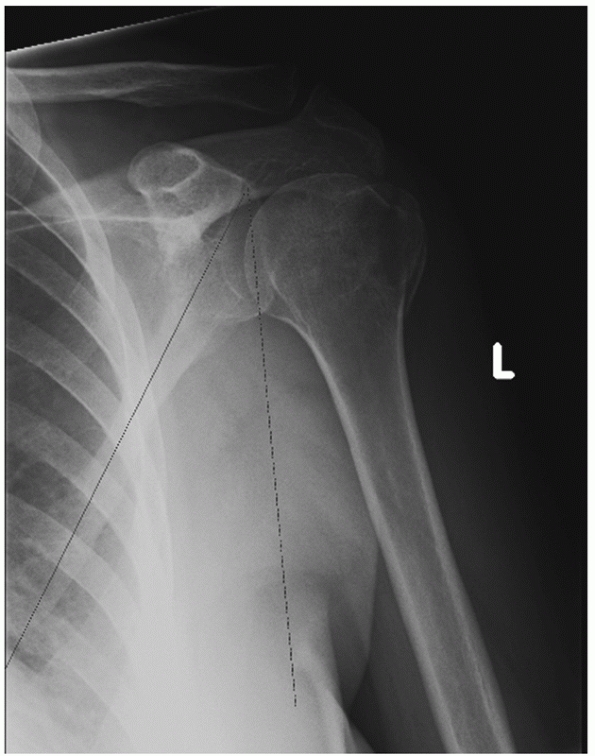
the humeral head in relation to the glenoid fossa or fracture fragment (Fig. 37-2).
Finally, a three-dimensional CT scan can be very helpful in
understanding complex fracture patterns and in preoperative planning.
 |
|
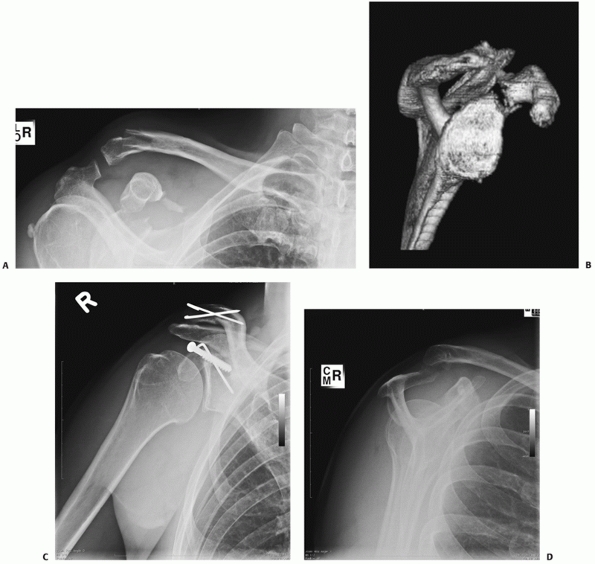
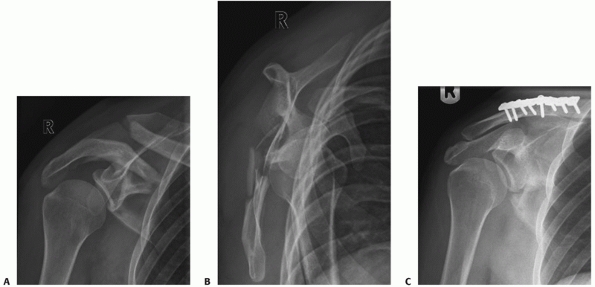
FIGURE 37-1 A,B. A double disruption of the SSSC (fracture of the coracoid process and ipsilateral lateral clavicle fracture). C,D.
After open reposition and internal fixation of both clavicle and coracoid process, both fractures healed. Despite the acromioclavicular joint subluxation, the patient had a maximum constant score of 100. |
area (body and spine, glenoid cavity, glenoid [scapular] neck,
acromion, and coracoid).
(approximately 50%), followed by the scapular neck (approximately 25%),
glenoid cavity (approximately 10%), acromion (approximately 8%), and
coracoid process (approximately 7%).1,79,115,127,184
divided scapular fractures into three types: type 1, fractures of the
body; type 2, fractures of the apophysis (including acromion and
coracoid); and type 3, fractures of the superior lateral angle,
including the glenoid neck and glenoid. Zdravkovic and Damholt191 considered type 3 fractures, which represented only 6% of their series to be the most difficult to treat.
 |
|
FIGURE 37-2 The humeral head is subluxed along with a posterior fracture fragment.
|
 |
|
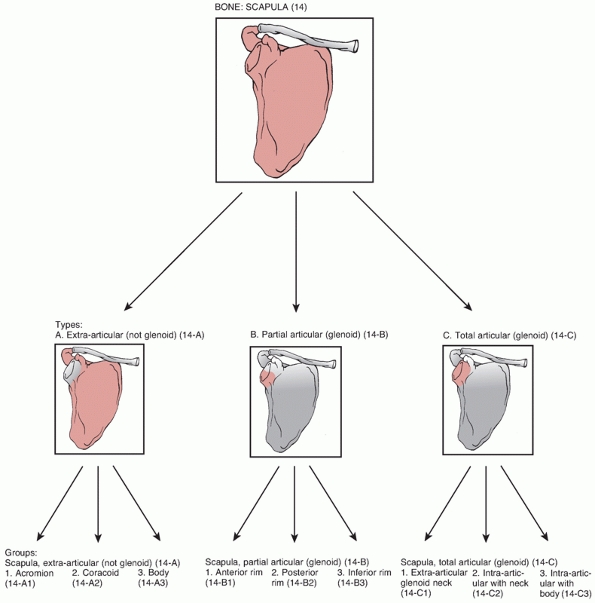
FIGURE 37-3 The OTA classification of scapular fractures.
|
divided scapular fractures into two groups. Group 1 included patients
with fractures of the scapular body, scapular neck, and spine; group 2
included patients with fractures of the acromion, coracoid process, and
glenoid. They reported poor functional outcome caused by loss of
glenohumeral motion and residual pain in patients of group 2.
classification, which was originally published in 1996, has been
revised for scapular fractures.107
In this new format, the differences between the OTA and AO
classification have now been eliminated by a unified alpha-numeric code
(Fig. 37-3).
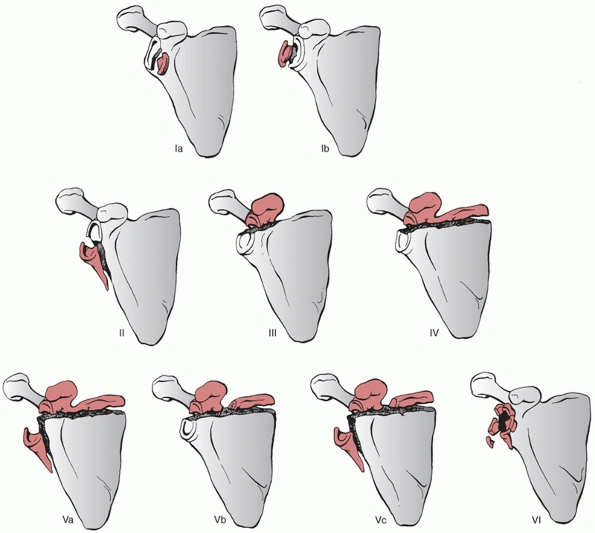
modified this system by subdividing type 5 and introducing type 6, a
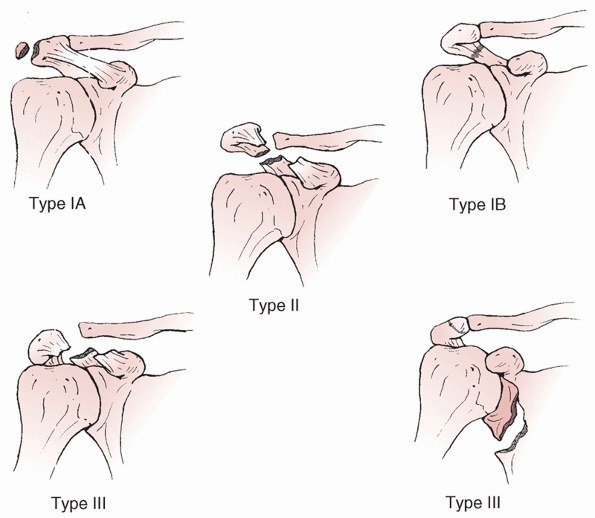
stellate glenoid fracture with extensive intra-articular comminution (Fig. 37-4).
the standard three-view trauma series. The axillary radiograph combined
with CT scanning is used to demonstrate any subluxation or displacement.
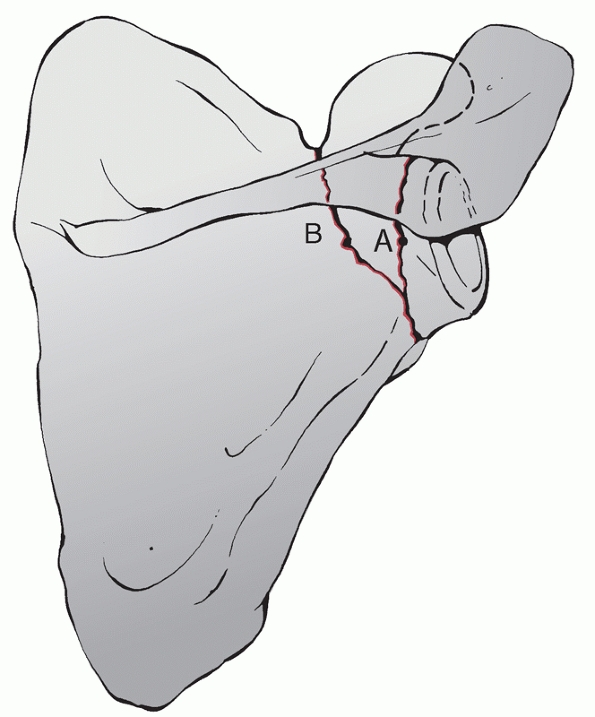
definition. Although three fracture patterns have been described as
scapular neck fractures,62 only two run through the scapular neck (Fig. 37-5).
One fracture pattern runs lateral from the origin of the coracoid to
the lateral border of the scapula (anatomic neck), and the other runs
medial from the coracoid to the lateral border of the scapula.
According to the OTA, both are classified as type 14-C1 (see Fig. 37-3).
 |
|
FIGURE 37-4
Classification of fractures of the glenoid cavity: type Ia, anterior rim fracture; type Ib, posterior rim fracture; type II, fracture line through the glenoid fossa exiting at the lateral scapular border; type III, fracture line through the glenoid fossa exiting at the superior scapular border; type IV, fracture line through the glenoid fossa exiting at the medial scapular border; type Va, combination of types II and IV; type Vb, combination of types III and IV; type Vc, combination of types II, III, and IV; type VI, comminuted fracture. (Goss TP. Scapular fractures and dislocations: diagnosis and treatment. J Am Acad Orthop Surg 1995;3(1):22-33, with permission.) |
by plain films, in contrast with assessment of the amount of fracture
displacement and angulation.26,113 A common method to determine angulation deformity and shortening, as described by Bestard,10 is on an AP radiograph of the scapula (Fig. 37-6).
Three-dimensional CT reconstruction images may be of more benefit in
assessment of displacement and angulation, in contrast with the images
of a conventional CT scan.113
 |
|
FIGURE 37-5 Line A is a fracture through the anatomic scapular neck. Line B is a fracture through the surgical scapular neck.
|
 |
|
FIGURE 37-6
The GPA is the angle between the line connecting the most cranial with the most caudal point of the glenoid cavity and the line connecting the most cranial point of the glenoid cavity with the most caudal point of the scapular body. It provides a value for the obliquity of the glenoid articular surface in relation to the scapular body. A GPA ranging from 30 to 45 degrees is considered normal.10 |
subclassification of acromion fractures, which are classified by the
OTA as type 14-A1 fractures, to help determine the need for operative
intervention. According to the classification of Kuhn, type 1 are
nondisplaced fractures, type 2 displaced fractures without reduction of
the subacromial space, and type 3 displaced fractures with reduction of
the subacromial space (Fig. 37-7).90
series, including an AP view, a lateral view, and an axillary view of
the scapula, will detect most acromial fractures. Caution should be
used to differentiate an acromial fracture from an os acromiale. An
axillary radiograph of the contralateral shoulder may be helpful,
because an os acromiale is bilateral in approximately 45% to 62% of the
cases.38,101 Occasionally, a CT scan is necessary to define the configuration of the fracture precisely (Fig. 37-8B,C).
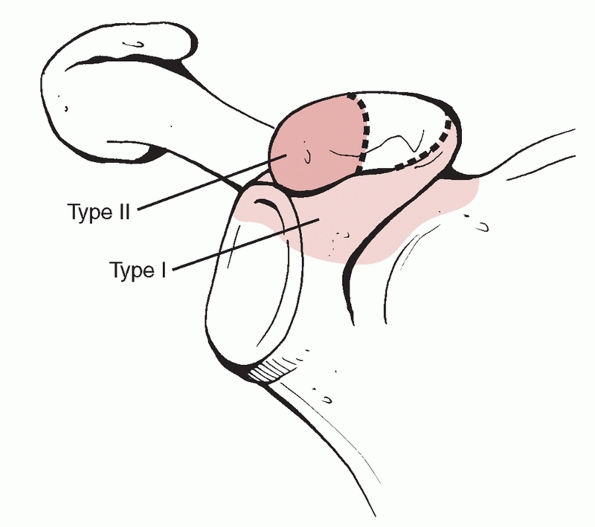
classified coracoid fractures into two different types. Type 1 is
situated proximal to the coracoclavicular ligament attachment and type
2 distal to these ligaments (Fig. 37-9). Ogawa133 suggested that a type 1 fracture may disturb the scapulothoracic connection (see Fig. 37-1).
fracture type difficult. The coracoid process is not easily visualised
on a radiograph. Apart from the usual three-view trauma series, an AP
tilt view (35 to 60 degrees),60 a Stryker notch view,145 and a Goldberg posterior oblique 20-degree cephalic tilt view53 may be helpful. A CT scan with three-dimensional reconstruction images will give more insight into the fracture pattern.
proposed a classification system for scapulothoracic dissociation in
1997 based on musculoskeletal, vascular, and neurologic impairment.
Zelle et al.192 modified the group
of neurologic impairment of this classification scheme and added the
group with a complete brachial plexus avulsion as the most severe type (Table 37-1).
on history, clinical findings, and radiography. The difficulty for the
treating physician is that the severe associated injuries may divert
attention away from the sometimes subtle clinical signs of the
scapulothoracic dissociation.94 The clinical signs may vary between swelling from a dissecting hematoma and a flail and pulseless extremity.
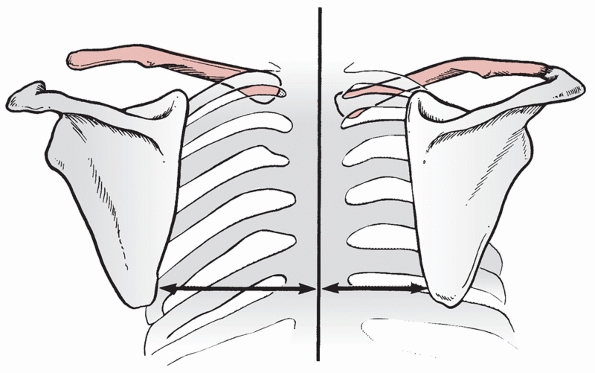
lateral displacement of the scapula on the injured side, which is
pathognomic of a scapulothoracic dissociation. The degree of
lateralization can be quantified using the scapula index (Fig. 37-10).86,134
required for adequate treatment of patients with scapular fractures,
particularly if operative treatment is considered. The scapula is a
large, flat, triangular bone that connects the clavicle to the humerus.
At least 18 different muscles originate from and insert into this
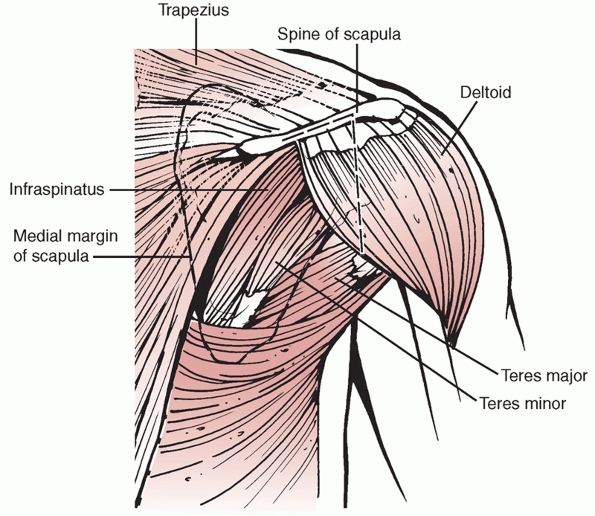
highly mobile bone (Fig. 37-11).
 |
|
FIGURE 37-7
Kuhn classification of fractures of the acromion process. Type I undisplaced: Ia avulsion fractures and Ib true fractures. Type II displaced without reduction of the subacromial space. Type III displaced with reduction of the subacromial space. This reduction may be by inferior displacement of the acromion or by an association with a superiorly displaced glenoid neck fracture. |
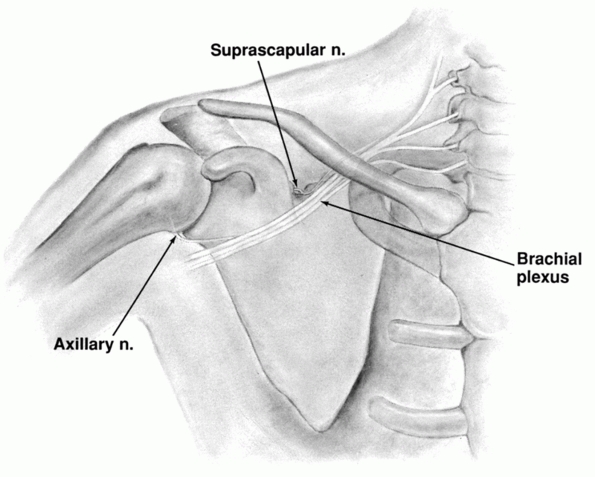
structures at risk when surgery (both anteriorly and posteriorly) is
undertaken.
medial two thirds of the clavicle, accompanies the axillary artery, and
lies beneath the pectoralis minor muscle. The musculocutaneous nerve
originates from the lateral cord and penetrates the conjoined tendon of
biceps and coracobrachialis at a variable distance (average 5 cm) from
the coracoid tip (Fig. 37-12).
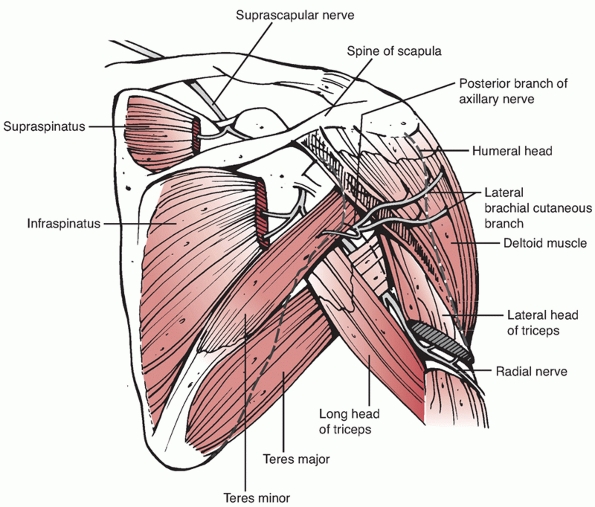
suprascapular nerve enters the supraspinous fossa under the transverse
ligament (or suprascapular ligament). The nerve runs beneath the
supraspinatus muscle and curves round the external corner of the spine
of the scapula to the infraspinous fossa (Fig. 37-13).
In the supraspinous fossa, it gives off two branches to the
supraspinatus muscle, and in the infraspinous fossa, it gives off two
branches to the infraspinatus muscle, besides some filaments to the
shoulder joint and scapula.
during open surgical procedures require dissection of the posterior
shoulder joint within 2.3 cm of the superior glenoid rim and within 1.4
cm of the posterior rim of the glenoid at the level of the base of the
scapular spine (see Fig. 37-13).157
nerve runs together with the circumflex humeral artery overlying the
subscapular muscle. The axillary nerve divides in this space and sends
a posterior branch to the teres minor muscle, together with a lateral
brachial cutaneous nerve (see Fig. 37-13).6
An anterior branch runs from this space approximately 5 cm below the
edge of the acromion as the nerve passes anteriorly to innervate the
anterior two thirds of the muscle.
variable. In 70%, it is innervated by the posterior branch, in 27% by
posterior and anterior branches, and 3% only by the anterior branch.172 One should therefore be careful when performing a deltoid splitting approach in a posterior surgical approach.
branch of the axillary nerve immediately adjacent to the inferior
aspect of the capsule at the level of the glenoid rim (see Fig. 37-13).6
It is an extensive approach which involves dissection of the
infraspinatus muscle from the infraspinatus fossa with the risk of
neurovascular damage (suprascapular nerve) and structural muscle
damage. Nowadays, the advocated posterior approaches are less invasive,
since no or minimal infraspinatus detachment is necessary when using
the interval between the teres minor and infraspinatus muscle.16,36,82,128,129
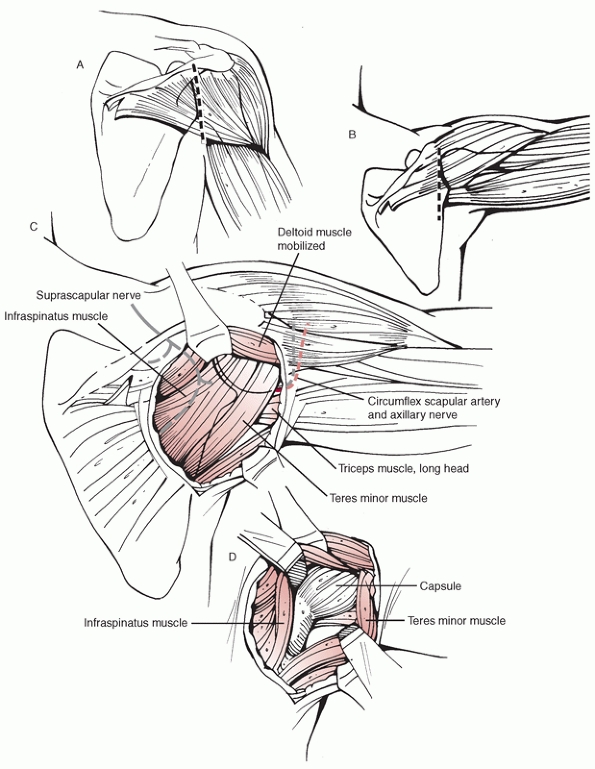
a skin incision is utilized along the scapular spine and then a
vertical extension is made at the lateral border of the scapula (a
“reverse Judet” skin incision) (Fig. 37-14).
This allows the surgeon to reflect the complete posterior deltoid, if
necessary, off the scapular spine. A medially based fascia flap is
raised to expose the scapular musculature. The interval between the
infraspinatus and teres minor muscles is entered with the infraspinatus
muscle retracted cranially and the teres minor muscle laterally. This
avoids any injury to the suprascapular nerve supplying
the
infraspinatus muscle as well as to the axillary nerve supplying the
teres minor muscle. The lateral border of the scapula and the glenoid
joint are then displayed, with the possibility of open reduction and
internal fixation of scapular neck fractures and posterior glenoid
fractures (types Ib, II, IV, and possibly V) (see Fig. 37-14).
 |
|
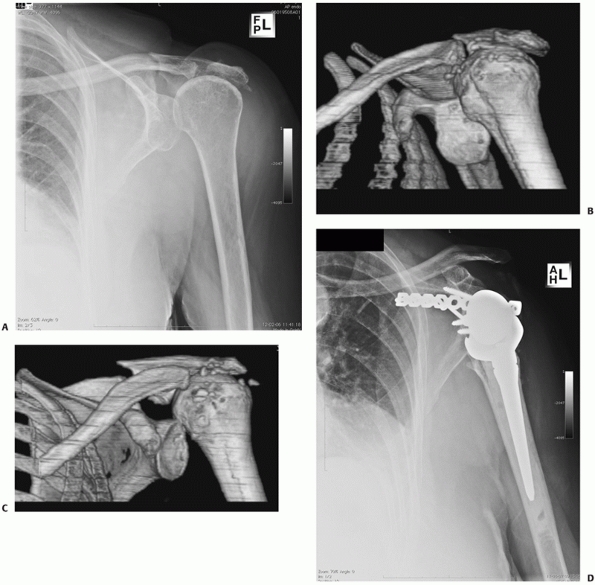
FIGURE 37-8 The radiograph (A) and CT (B,C)
scan of an 80-year-old woman with a posterocranial glenohumeral luxation with a symptomatic pseudarthrosis of an acromion fracture. D. The patient underwent a plate osteosynthesis with bone graft and a reversed shoulder prosthesis. |
 |
|
FIGURE 37-9 Ogawa classification of coracoid fractures. Type I is proximal to and type II is distal to the coracoclavicular ligaments.
|
|
TABLE 37-1 The Classification System for Scapulothoracic Dissociation as Proposed by Damschen et al.29 and Modified by Zelle et al.192
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 37-10
The diagnosis of scapulothoracic dissociation can be made on a nonrotated AP radiograph by comparing the distance from the medial border of the scapula with the spinous processes between the affected (long arrow) and unaffected (short arrow) sides. Kelbel et al.86 created the scapula index and reported a normal value to be a ratio of 1.07 ± 0.04.134 |
 |
|
FIGURE 37-11 Muscle insertions onto the scapula. Anterior (A) and posterior (B) views.
|
 |
|
FIGURE 37-12
The position of the brachial plexus in relation to the anterior surface of the scapula. The supraclavicular and axillary nerves are also shown. |
 |
|
FIGURE 37-13
A posterior view of the course of the suprascapular nerve and posterior branch of the axillary nerve in relation to the scapula and overlying muscles. |
of the posterior deltoid muscle off the scapular spine. Alternatives
are described by Wirth186 who
described a posterior approach with splitting of the posterior deltoid
in line with its fibers distally to the upper border of the teres
minor. Splitting the deltoid muscle, however, endangers the integrity
of the axillary nerve
at
the level of the dense connective tissue of the subdeltoid fascia.
Furthermore, the intramuscular nerve branches can occasionally be
damaged within the lateral deltoid compartment.
 |
|
FIGURE 37-14 Posterior approach to the glenohumeral joint/ scapular neck showing the skin incision.
|
claim excellent exposure with their posterior subdeltoid approach to
the posterior aspect of the glenohumeral joint and scapular neck (Fig. 37-15).
After a vertical skin incision, the inferior border of the spinal part
of the deltoid is identified and mobilized by blunt dissection. By
abducting the free draped arm 60 to 90 degrees, it is easier to retract
the mobilized deltoid muscle and enter the interval between the
infraspinatus and teres minor muscle as described above, allowing
access to the posterior aspect of the glenoid and lateral border of the
scapular body. Care should be taken to avoid injury to the circumflex
scapular artery, which lies directly medial to the insertion of the
long head of triceps, and the axillary and suprascapular nerves.
 |
|
FIGURE 37-15 The posterior approach to the glenohumeral joint and scapula. A. Arm in adduction. B. Arm in 90 degrees of abduction. C. The underlying rotator cuff muscles. D. The capsular incision.
|
incision made in Langer lines over the coracoid process to the axillary
fold. The deltopectoral groove is opened with the cephalic vein
attached to the deltoid muscle. In the presence of an anterior glenoid
rim (type Ia) fracture, the subscapularis tendon is dissected off the
anterior glenohumeral capsule and turned back medially. The capsule is
opened and a humeral retractor is inserted behind the posterior aspect
of the glenoid to visualize the entire glenoid cavity. After reduction
and internal fixation of the glenoid fracture, the capsule, which is
usually not stretched by the injury, is closed without performing a
capsular shift.
fragment (type III, type V glenoid fracture) or an anatomic neck
fracture of the scapula is difficult to control or stabilize. This
approach can be added to an anterior or posterior approach. It is
performed in a beach chair position with the skin incision made midway
between the scapular spine and clavicle, laterally over the edge of the
acromion. The trapezius can then be split in the line of its fibers,
taking care to protect the accessory nerve which runs from anterior to
posterior. After identifying the suprascapular notch, the supraspinatus
muscle can either be split or shifted to the anterior or posterior part
of the supraspinatus fossa depending on whether access is required to
the anterosuperior or posterosuperior aspect of the glenoid. Care
should be taken to protect and avoid injury to the suprascapular nerve
and vessels that lie medial to the coracoid process.
meriting surgical consideration. The majority (90%) are minimally
displaced or undisplaced and should be treated nonoperatively.
Fractures of the glenoid are commonly found in the middle aged, between
40 and 60 years, with a male prevalence,78 and result most often from high-energy direct trauma.1,57,79,112,115,150
They occur when the humeral head is driven with a substantial force
against the glenoid fossa. This may be caused by a direct force on the
shoulder or an axial force through the humerus. The direction of this
axial force will predict the fracture pattern. The most common fracture
type is the anterior chip fragment fracture (type Ia), which is often
associated with an anterior shoulder dislocation.78
in patients treated nonoperatively with intra-articular fractures
without associated instability.20,77,144,151 Since the late 1980s, operative treatment of glenoid fractures has gained more attention.4,8,74,84,89,98,156
There is a current trend towards arthroscopic techniques of glenoid
fracture treatment, particularly in Ideberg type I fractures.9,22,24,51,138,163,167
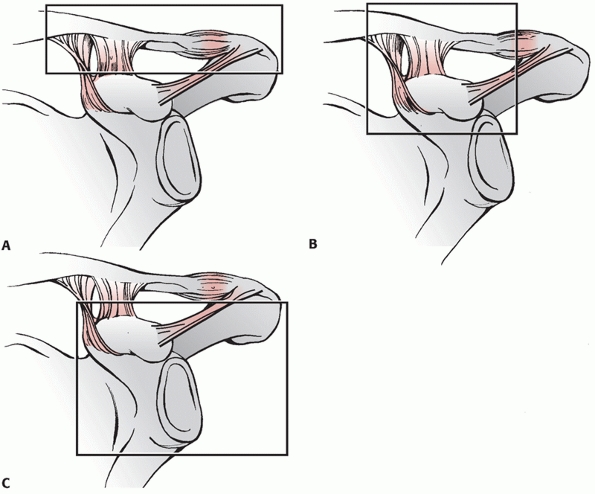
glenoid (types Ia and Ib, respectively) may cause instability of the
glenohumeral articulation. These fracture types are usually sustained
during traumatic glenohumeral subluxation or dislocation.76,77
After injury, the continuity between capsule, labrum, and fracture
fragment is usually maintained. Instability of the glenohumeral joint
can be expected when the fragment is displaced more than 1 cm and if at
least 25% of the glenoid cavity anteriorly or at least 33% of the
glenoid cavity posteriorly is involved.32
Although debate exists among surgeons about the amount of displacement
and the size of the fragment that is acceptable, it is accepted that
rim fractures associated with persistent or recurrent instability
should undergo open reduction and internal fixation.32,66,77,159
An axillary radiograph and CT scan will demonstrate whether the humeral
head is centered exactly in the glenoid fossa or is displaced along
with the fracture fragment. The latter is an indication for surgical
treatment. The goal of surgery is to prevent morbidity secondary to
glenohumeral instability or degenerative joint disease by accurate
reduction of the articular surface. According to the literature of the
last decade, open procedures can be replaced by arthroscopic fixation
of fragments with promising results particularly in type I fractures9,22,24,138,163,167; most authors reported restoration of glenohumeral stability and good functional results.
humeral head is directed somewhat inferiorly, with a fracture line
running from the glenoid fossa to the lateral border of the scapula
body as a result. The amount of articular displacement and the degree
of comminution determines the need for open reduction and internal
fixation. Goss60 advocates open
reduction and internal fixation with displacement of more than 5 mm.
This is based on the findings of Soslowsky et al.,162 who demonstrated that the maximum thickness of glenoid articular cartilage is 5 mm. Schandelmaier156
reviewed 22 patients with displaced glenoid fractures after a mean
review period of 10 years: 9 had a type 2 fracture and were treated by
open reduction and internal fixation through a posterior approach. He
found a mean constant score of 94.
is directed superiorly, causing a fracture that involves the upper
third of the glenoid fossa including the coracoid. The fracture runs
from the glenoid fossa through the superior scapular body in the
proximity of the scapular notch. According to Goss,60,61
type III,V, and VI injuries in particular are prone to neurovascular
injuries and damage to the SSSC. As with all other glenoid fractures, a
type III injury is usually undisplaced and can be treated
conservatively with good functional outcome in absence of associated
neurologic injury. The indication for operative treatment is also
displacement of more than 5 mm.
centrally into the glenoid fossa. A fracture line runs from the fossa
directly across the scapula body to exit along its medial border and
splits the glenoid fossa into two parts. Surgery is indicated when
there is more than a 5-mm separation between the two parts. Surgery may
prevent symptomatic degenerative joint disease, instability of the
glenohumeral joint and, although extremely rare, nonunion of the
fracture.
of injury in most cases.20 Goss57 subdivided type 5 into three different subtypes (see Fig. 37-4).
Type Va is a combination of type II and IV, Type Vb a combination of
type III and IV, and type Vc a combination of type II, III, and IV.
These subtypes are caused by more complex and probably greater forces
than those causing the simpler fracture patterns.57 The same indications used for type II, III, and IV should be applied when determining the need for open reduction.19
Operative treatment of type V injuries does not uniformly lead to a
good functional outcome, which is probably mostly related to associated
neurovascular injuries and postoperative complications.77,84,98,112,156
are caused by the most violent force and include all fractures with at
least two articular fragments. Even if displacement of the fragments is
substantial, with or without subluxation of the humeral head, open
reduction and internal fixation is not indicated due to the extensive
comminution.60
-
Closed reduction under anesthesia is unsuccessful in improving position of the fracture fragment(s);
-
Secondary improvement of position of
fracture fragments is possible after conservative treatment due to
moulding of the fracture by muscle forces across the glenohumeral joint; -
A good result occurred in 75% of the cases after early mobilization;
-
Open reduction and internal fixation may
also lead to a good result in the absence of other significant
ipsilateral shoulder fractures, nerve, or muscle injuries.76,77,78
The suggested mechanisms of trauma are a direct blow to the shoulder, a
fall on the point of the shoulder, or a fall on the outstretched arm.
The fracture line most often extends from the suprascapular notch area
across the neck of the scapula to its lateral border inferior to the
glenoid (surgical neck fracture) or, rarely, lateral from the origin of
the coracoid to its lateral border inferior to the glenoid (anatomic
neck) (see Fig. 37-5).
fractures, are sometimes accompanied by a fracture line through the
coracoid process or may remain as an intact unit. If the scapular neck
fracture is not associated with an ipsilateral shoulder lesion (of the
SSSC), displacement is possible but rare.31,58,176 According to the concept of the SSSC, isolated fractures of the scapular neck are considered stable fractures.61
Some authors doubt the usefulness of closed reduction in these
fractures, advocating the use of a sling and suggest mobilizing the
affected arm as soon as possible.117 Lindholm and Leven103
studied a series of scapular neck and body fractures and concluded that
if untreated, all fractures healed in the position displayed at the
time of the original injury.
these recommendations. A more differentiated approach is necessary as
conservative treatment does not uniformly lead to a good result.
Several authors noted fair to poor results after conservative treatment
of severely displaced scapular neck fractures.1,3,49,127,135,148
Displacement is defined as at least 1 cm of translation or 40 degrees
of angulation (or a glenopolar angle [GPA]<20 degrees) in the AP
plane of the scapula and separates minor from major injuries according
to Zdravkovic,191 Nordqvist and Petersson,127 and Geel.50
scapular neck fractures. Of the 16 patients treated conservatively, 50%
complained of pain at night, 40% had weakness of abduction, and 20% had
decreased range of motion. Whether translational displacement of at
least 1 cm remains a good criterion for surgical treatment of scapular
neck fractures is controversial.148,176
The criterion of angulation greater than or equal to 40 degrees (or a
GPA <20 degrees) is probably less questionable. Several authors
reported less favorable long-term outcome after conservative treatment
of angulated scapular neck fractures, compared with scapular neck
fractures without angular displacement.15,88,148,173
Good to excellent results have been reported on open reduction and
internal fixation of patients with displaced scapular neck fractures.9,67,88,100
In these series, however, displaced scapular neck fractures are in most
cases associated with ipsilateral clavicle fractures. According to
Zlowodzki,194 who performed a
systematic review of 520 scapular fractures in 22 case series,
excellent or good results can be achieved with nonoperative treatment
of isolated neck fractures in 77% of the cases and in 88% of the cases
with operative treatment. Universal guidelines for conservative or
operative treatment are difficult to establish empirically because the
available literature does not include randomized or nonrandomized
comparative studies. Treatment should, therefore, be individualized.
SSSC, consisting of the glenoid, coracoid, acromion, distal clavicle,
coracoclavicular ligaments, and acromioclavicular ligaments (Fig. 37-16).
This bone-soft tissue ring maintains the normal, stable relationship
between the upper extremity and the axial skeleton. Single disruptions
of the SSSC, such as an isolated scapular neck fracture, are usually
anatomically stable because the integrity of the complex is preserved,
and nonoperative management yields good functional results. When the
complex is disrupted in two places (double disruption), such as a
scapular neck fracture with an acromioclavicular joint disruption, a
potentially unstable anatomic situation is created. Because the SSSC
includes the glenoid, acromion, and coracoid, many double disruption
injuries involve the scapula. In the presence of a displaced fracture
of the acromion, coracoid process, glenoid, or scapular neck, the
possibility of another lesion of the SSSC (i.e., a double disruption)
should be considered. According to Goss,61
open reduction is indicated for double disruptions that are accompanied
by significant displacement, which may lead to delayed union, malunion,
or nonunion as well as long-term functional deficits.
 |
|
FIGURE 37-16 The SSSC A. Clavicle-acromioclavicular joint-acromion strut. B. Clavicle-coracoclavicular ligament-coracoid linkage. C.
Three process-scapular body junction. (From Goss TP. Fractures of the scapula. In: Rockwood CA, Matsen FA, Wirth MA, et al., eds. The Shoulder. 3rd ed. Philadelphia: Saunders, 2004:413, with permission.) |
is the ipsilateral glenoid surgical neck and midshaft clavicle
fracture. This injury, although the terminology is criticized,91 is also defined as a floating shoulder.
were the first authors who described this injury in 1975. They
suggested a loss of the stabilizing effect of the clavicle in the case
of a combination of these two fractures. In contrast to isolated
scapular fractures, they found more severe displacement of the scapular
fracture when combined with an ipsilateral clavicle fracture. The
weight of the arm and the combined contraction of the biceps, triceps,
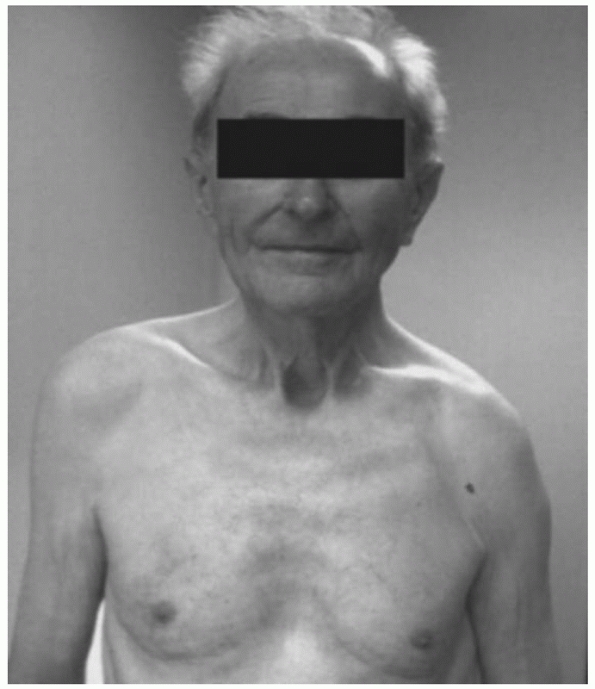
and coracobrachialis muscles may cause inferior and rotational
displacement of the distal fragment resulting in a change in the
contour of the affected shoulder, the so-called drooping shoulder (Fig. 37-17). Apart from this possible caudal and rotational displacement, it is also suggested, although criticized by some,129,175 that the glenoid fragment is displaced anteromedially by contraction of the rotator cuff muscles (Fig. 37-18).46,66,71
Translational displacement of the scapular neck will result in
shortening of the lever arm of the rotator cuff musculature and
threaten the functional balance of the glenohumeral joint.66,158 This may result in loss of abduction strength,1,20,66 although this is not necessarily synonymous with limitation of range of motion, as demonstrated in a biomechanical analysis.25 Williams and colleagues185
conducted the only cadaver study on this subject to determine the
stability afforded by specific structures. They concluded that
ipsilateral fractures of the scapular neck and the shaft of the
clavicle do not produce a floating shoulder without additional
disruption of the coracoacromial and acromioclavicular capsular
ligaments. These findings have not yet been confirmed in clinical
studies.
by the complete lack of well-performed, prospective studies with
comparison of different treatment options. The literature on this
subject is limited to data provided only by case reports and
retrospective studies of small patient series.
Traditionally, floating shoulders were treated nonoperatively. However,
over the last 2 decades, there has been increased interest in open
reduction and internal fixation of these fractures.40,66,69,71,93,99,141 Herscovici71
reported on nine patients: seven had been treated operatively (with
osteosynthesis only of the clavicle) and the remaining two had been
treated nonoperatively. Their good results led them to recommend open
reduction and internal fixation of the clavicle only, in order to
prevent malunion of the scapular neck. The authors presumed that the
glenoid neck fracture would usually reduce and be stabilized
indirectly. Rikli141
retrospectively analyzed 12 cases, 11 with osteosynthesis of the
clavicle alone, whereas one had both the clavicle and the glenoid neck
fractures fixed. The findings of Leung and Lam99
are based on the treatment results in 15 cases in whom simultaneous
fixation of the displaced scapular and clavicle fractures had been
performed. All but one patient had a good, or excellent, functional
result, according to the scoring system of Rowe.151
All fractures healed at an average of 8 weeks postoperatively. Good
results in seven operatively treated patients, by fixation of both the
scapular neck and clavicle fractures, or disrupted acromioclavicular
joint, have also been described in a retrospective study by Egol et al.40 Finally, in a study of Labler et al.,93
six patients were treated with internal fixation of only the clavicle
and three with fixation of both clavicle and scapular fractures.
 |
|
FIGURE 37-17 Drooping aspect of the left shoulder.
|
 |
|
FIGURE 37-18 A,B. Radiographs of an ipsilateral scapular neck and midshaft clavicle fracture. C. The glenoid fossa is still not reduced despite open reduction and internal fixation of the clavicle.
|
|
TABLE 37-2 Reported Results of Conservative and Operative Management of the Floating Shoulder
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
reported excellent results in 17 and good results in 3 patients in whom
all ipsilateral fractures of the scapula and clavicle had been treated
nonoperatively by a shoulder immobilizer, until the associated injuries
allowed mobilization of the shoulder. They recommend conservative
treatment, especially in patients with less than 5-mm displacement. In
a retrospective study, van Noort et al.173
reported fair to good results in 28 patients treated conservatively
(mean constant score: 76), with a well-aligned glenoid. The authors
concluded that these rare shoulder lesions are not unstable by
definition and that conservative treatment leads to a good functional
outcome in the absence of caudal displacement of the glenoid. Caudal
displacement was defined as an inferior angulation of the glenoid of at
least 20 degrees.174 Ramos et al.139
in 1997 reviewed 13 patients with ipsilateral fracture of the clavicle
and scapular neck treated conservatively. The average follow-up was 7.5
years. Using Herscovici’s scoring method,71 they reported 84.6% excellent, 7.7% good, and 7.7% fair results.
remains unclear under which criteria a floating shoulder should be
treated operatively. Current experience indicates that an undisplaced,
or minimally displaced, ipsilateral clavicle and scapular neck fracture
can be treated conservatively, with a good functional outcome. The
amount of displacement that is acceptable at the fracture sites of the
glenoid neck and clavicle is controversial.
reported a scapular body fracture in a professional boxer who sustained
the injury during an attempted punch. More rare causes are seizures,
electrical shock treatments,11,70,110,166 or stress fractures.136 Scapular body fractures heal readily and do not merit operative intervention,115,116,184
regardless of the number of fracture fragments. The fact that these
fractures heal well without significant clinical symptoms is probably
directly related to the protection of a thick layer of muscles
surrounding the scapula. Several series of conservatively treated
patients with scapular body fractures have been reported with union of
the fracture and a good functional outcome.3,79,103,115 Zlowodzki194
reported in a systematic review of 520 scapular fractures in 22 case
series, that 99% of all scapular body fractures had been treated
nonoperatively. Excellent or good results were achieved with
nonoperative treatment in 88% of the cases.
malunion of the scapular body may have adverse mechanical and
functional effects on shoulder movement. Excision of the bony
prominence in these cases is usually curative.44,45 Other clinical symptoms are pain, limited range of motion, and winging of the scapula by loss of the serratus anterior muscle.64 Nordqvist and Petersson127
found poor long-term results in some patients with more than 10 mm of
displacement. Nonunions are extremely rare. Two cases have been
reported which were both treated successfully by open reduction, rigid
internal fixation, and bone grafting.43,64
joint and serves as the point of attachment for the deltoid muscle and
a number of ligaments. By forming the roof of the glenohumeral joint,
it lends posterosuperior stability. Approximately 8% to 9% of all
scapular fractures involve the acromion.3,115,184
-
A direct blow from the outside, in general a significant force.
-
A force transmitted via the humeral head
from the inside. Traumatic superior displacement of the humeral head,
which may also result in an associated rotator cuff tear, can cause an
(superiorly displaced) acromial fracture. Another mechanism is rotator
cuff arthropathy, in which an acromial fracture may occur by superior
migration of the humeral head.20 -
An avulsion fracture is usually caused by an indirect force. Heyse-Moore and Stoker,72 Rask and Steinbergh,140 and Russo et al.153 reported forceful contraction of the deltoid muscle resulting in an avulsion fracture of the acromion.
-
Stress fractures of the acromion have been reported, particularly in sports.65,178,181 Subacromial decompression with significant thinning of the acromion may also lead to a stress fracture.106,111,152,182
with an acromion fracture is described. The brachial plexus is at risk
particularly with an inferiorly displaced acromion fracture.114,123 Other associated lesions, as reported earlier, are rotator cuff lesions.104,145
Finally, ipsilateral acromioclavicular joint lesions, coracoid,
clavicle, glenoid, and proximal humeral fractures and shoulder
dislocations have been reported.58,92,95,102,114,122,193
does occur, it is usually non- or minimally displaced. Nonoperative
treatment in these cases will lead to union of the fracture with a good
to excellent functional outcome.61
Most acromion fractures are successfully treated simply by
immobilization with a sling or Velpeau dressing until the pain has
subsided, which is usually within 3 weeks.1,81,90,92,102,114,120 Some authors have advocated the use of a spica cast with the shoulder in abduction.122,184 Omission of a sling or another form of immobilization may cause secondary displacement of the fracture.59
the group of nonor minimally displaced fractures are type I fractures
and caused by indirect force (avulsion fracture-type Ia) or a direct
trauma (type Ib). Nonoperative treatment is also advocated by Kuhn90
in dislocated acromial fractures in which the subacromial space is not
compromised (type II fracture). However, a poor clinical outcome or a
symptomatic pseudarthrosis of patients with a type II fracture has been
reported.34,90
In type III displaced fractures in which the subacromial space is
diminished by the inferior pull of the deltoid on the acromial
fragment, open reduction with internal fixation is advocated by Kuhn90 and Ogawa132 to prevent secondary impingement. Most authors recommend open reduction and internal fixation for markedly displaced
acromion fractures to reduce the acromioclavicular joint and prevent nonunion, malunion, and secondary impingement.124,151
When surgery is performed, a variety of surgical techniques may be
employed, including the use of tension band wiring, sutures, Kirschner
wires, staples, lag screws, and plates.8,30,61,66,81,182
Excision of the acromial fragment has been reported but is generally
not recommended for fragments larger than half an inch because it can
result in substantial weakness of the deltoid muscle.90,120,123,130
-
A direct blow to the superior point of the shoulder;
-
A direct contact between the humeral head and coracoid process in case of an anterior shoulder dislocation;47,168
-
An avulsion fracture by a forceful contraction of the short head of the biceps, pectoralis minor, or coracobrachialis muscle;5,149
-
As part of an acromioclavicular dislocation;180 and
-
Stress fractures have been reported:
medial migration of the humeral head from rotator cuff arthropathy may
result in a coracoid fracture.14
reported acromioclavicular dislocations as the most common associated
lesion, seen in 60 of the 67 described patients. Other common
associated lesions are lacerations or abrasions over the posterolateral
or lateral deltoid muscle, (lateral) clavicle fractures, shoulder
dislocations, and rotator cuff tears.
coracoid, whether or not with extension in the upper border of the
scapula and/or the glenoid.42,80,131,188 Other reported sites are the middle portion33,137 and the tip.75,121,193
been described. There is, however, no consensus in the literature about
the preferred treatment of coracoid fractures. Many authors suggest
that non- or minimally displaced fractures can be successfully treated
by conservative treatment.42,52,109,193
On occasion, however, these injuries may be significantly displaced and
of functional importance, thus making surgical management a
consideration. Fractures of the coracoid tip are avulsion injuries
(Ogawa type 2) that may displace considerably. Despite the chance of
nonunion,117 this type of fracture can be treated conservatively with good functional outcome.23,42,52,109,132
On occasion, operative treatment is indicated when the fractured
coracoid tip impedes the reduction of an anterior dislocated humeral
head.42,189 Other indications for surgery include a painful nonunion after anterior shoulder dislocation.47,85
follow the same reasoning described for fractures of the coracoid tip.
However, displacement of the fracture is more common which may be due
to accompanying ipsilateral shoulder injuries (double disruptions of
the SSSC). In these circumstances, or in cases with extension of the
fracture into the glenoid fossa (with displacement), open reduction and
internal fixation with screw fixation of the coracoid fracture is
advocated.42,61,133 Martin-Herrero,109
however, described satisfactory outcome in conservative treatment in
seven patients despite displacement of the fracture and associated
ipsilateral shoulder injuries in six.
complete loss of scapulothoracic articulation and lateral displacement
of the scapula, while the skin is usually intact. It is classically
caused by a violent lateral distraction or rotational displacement of
the shoulder girdle when the upper extremity is caught on a fixed
object while the body is moving at high speed.2 It is a rare, severe injury of the shoulder girdle with a high mortality rate (10%).29
Some authors describe this injury, which is almost always associated
with severe vascular injuries (prevalence 88% to 100%), as an internal
forequarter amputation.96,154,187,192
As well as lesions of the subclavian and axillary artery, associated
complete or partial disruptions of the brachial plexus (prevalence up
to 94%)29 are frequent and well
described in the literature. Other described associated lesions are
osseous injuries to the shoulder girdle (particularly clavicle
fractures, but also acromioclavicular or sternoclavicular dislocation),
injury to muscles (deltoid, pectoralis minor, rhomboids, levator
scapulae, trapezius, and latissimus dorsi), and massive soft tissue
swelling in the shoulder region. Approximately 50% of the reported
cases are the result of a motorcycle accident.18
dissociation should follow the ATLS principles with cardiopulmonary
stabilization and resuscitation being of paramount importance.
Treatment recommendations have focused on the care of the accompanying
neurovascular injury. In a hemodynamically stable patient,
arteriography is used to determine the vascular integrity, followed by
surgical repair if necessary. However, it should be appreciated that an
extensive collateral network around the shoulder can protect against
limb-threatening ischemia.54,100,171 Sampson et al.154
presented a series of 11 cases). They questioned the need for vascular
repair in these patients, all of whom had a complete brachial plexus
palsy, no radial pulse, and subclavian or axillary artery occlusion on
arteriography. Of these 11 cases, 6 were revascularized and 5 were not.
All 11 limbs remained viable, although none of the 11 patients regained
any function. Zelle et al.192
demonstrated that the extent of the neurologic injury is of paramount
importance in predicting the functional outcome. All of their patients
with a complete brachial plexus avulsion either had an amputation or
had poor shoulder function at the time of follow-up. Partial plexus
injuries, however, have a good prognosis, and most patients achieve
complete recovery or regain functional use of the extremity.60
If upper extremity function is not restorable, an immediate above-elbow
amputation seems to result in better functional outcomes, lower
complication rates, better relief of causalgia, and more successful
return to work than a late amputation.13,18,192 Many patients refuse a secondary amputation despite a flail, anesthetic upper extremity.27,35,54,171
in patients with scapulothoracic dissociation is unclear and should
therefore be individualized. Nevertheless, Goss61
advised open reduction and internal fixation of clavicle fractures and
stabilisation of disrupted acromioclavicular or sternoclavicular joints
for three reasons: to avoid delayed or nonunion, to restore as much
stability as possible to the shoulder complex thus reducing long-term
functional problems, and to protect the brachial
plexus, subclavian, and axillary vessels from further injury caused by tensile forces.
isolated scapular neck fracture is not necessary to obtain a good
functional outcome with conservative treatment. One should be aware of
the possibility of ipsilateral shoulder lesions (e.g., fractures,
rotator cuff lesions, and intra-articular glenohumeral damage), which
may influence the final functional outcome.155,176
Symptomatic local care in a shoulder immobilizer followed by passive
exercises as soon as the pain allows will not interfere with fracture
healing and will result in a good to excellent functional outcome.
(floating shoulder), there is a chance of further displacement of
either or both of the fractures. Current experience indicates that
undisplaced, or minimally displaced, ipsilateral clavicle and scapular
neck fractures can be treated conservatively with a good functional
outcome. In relatively young patients without comorbidities, open
reduction and internal fixation by plate osteosynthesis should be
considered in displaced, shortened, midshaft clavicle fractures because
of the chance of nonunion (prevalence 15%)73,142
or malunion. Fixation of the clavicle fracture may allow reduction of
the glenoid neck fracture and restoration of the shoulder contour.
However, despite anatomic reduction of the clavicle fracture,
displacement of the scapular neck fracture may persist. In particular,
rotational displacement of the scapular neck will compromise the
functional outcome. In case of caudal angulation of the glenoid fossa
of more than 20 degrees (or a GPA angle <30 degrees) (see Fig. 37-6),
operative treatment should be considered through a posterior approach
with plate osteosynthesis along the lateral border of the scapula (Fig. 37-19). However, caution should be employed to avoid surgical overtreatment in the absence of data to support an aggressive approach.
where there is subluxation of the humeral head or in fractures likely
to cause glenohumeral instability, which can be predicted if the
fracture is displaced more than 5 mm or if a quarter or more of the
glenoid cavity is involved. Exposure is performed through a standard
deltopectoral approach with mobilization of the subscapularis muscle. A
large fragment can be fixed with two screws, but smaller or comminuted
fragments may require a buttress plate with smaller screws.
fracture should be applied for a type Ib fracture except that the size
of the posterior fragment which will predict instability is a third or
more of the glenoid cavity. For posterior fractures, a posterior
glenohumeral exposure is advocated with access to the glenohumeral
joint through the interval between the infraspinatus and teres minor
muscles. In both types Ia and Ib, there are possible advantages of
arthroscopically controlled operative treatment using percutaneous
screw fixation. This is typically dependable on the skill of the
surgeon but also on the size and comminution of the fracture fragment.
 |
|
FIGURE 37-19 A scapular neck fracture which has been reduced and stabilized with a plate.
|
operative treatment. However, on the basis of available reports, it
seems reasonable to conclude that surgery has a definite role in the
treatment of glenoid fossa fractures. When the humeral head is not
centered in the major portion of the glenoid fossa and is subluxed
along with the fracture fragment, open reduction and internal fixation
of the fracture is indicated. Type II fractures are approached
posteriorly, and type III by either a superior or combined posterior
and superior approach. A cannulated interfragmentary compression screw
(3.5-mm) is placed after a Kirschner wire positioned in the superior
fragment is used to manipulate and reduce the fracture. A
posterosuperior approach is usually required for the treatment of types
III, IV, Vb, and Vc, so that the superior glenoid fragment can be
reduced and fixed relative to the inferior aspect of the glenoid
cavity. Care should be taken when using the posterosuperior approach
which places the suprascapular nerve in some jeopardy as the nerve
passes through the scapular notch, the supraspinatus muscle, the
spinoglenoid notch, and the infraspinatus muscle.
exercises should be started as soon as possible in order to prevent the
development of a stiff painful shoulder. These injuries have the
highest chance of posttraumatic arthritis.
make a distinction between the complications of treatment and
concomitant injuries associated with scapular fractures. The latter are
sometimes life-threatening and may have more consequences with respect
to the priorities of treatment and the overall functional outcome. On
the other hand, regional complications such as nerve injuries may
influence the functional outcome of the affected shoulder dramatically.
An example is a brachial plexus injury, which is described by Rockwood,143
after coracoid fracture. Suprascapular nerve injuries are reported
following scapular neck fracture with extension into the suprascapular
notch37,160 and from coracoid base fractures.143 Axillary nerve and brachial plexus injuries have been described in association with an acromion fracture.114,115
in general uncommon and variable. Malunion and particularly nonunion of
scapula fractures are very rare. In a recent search of the medical
literature, Marek105 discovered only
15 cases of scapula nonunion after nonoperative management. Malunion of
particularly scapular body fractures is well tolerated, although
painful scapulothoracic crepitus is described.1,3,127 Displaced glenoid fractures may lead to glenohumeral arthritis and instability,1,66 pain (in rest and with exertion), limitation in range of motion, and weakness.1,3,127,191
Some authors suggest that displaced fractures of the glenoid neck can
lead to altered mechanics of the surrounding soft tissues, giving rise
to glenohumeral pain and dysfunction.1,3,49,127,135,148
analyzed the postoperative complications of 212 cases described in 15
retrospective case series. The overall reported complication rate in
these studies was fairly low. The most common complications were
removal of implants in 7 % due to metal failure or local discomfort and
infection in 4 %. Other mentioned complications were nerve injuries
(2%), mostly involving the suprascapular nerve (4 out of 5),
reoperation other than hardware removal for posttraumatic arthritis
(2%), rotator cuff dysfunction (1%), and heterotopic ossification (1%).
Nonunion after operatively treated scapular fractures is not cited as a
complication except for one reported case by Marek.105
Finally, an improper physical therapy rehabilitation program or a poor
patient compliance may contribute to unnecessary postoperative shoulder
stiffness.
or minimally displaced and do well clinically after conservative
treatment.79,115,184
This observation has been based on treatment of scapular fractures in
general, and its relevance is therefore very limited. A more
differentiated approach turned out to be necessary as conservative
treatment does not uniformly lead to good results.1,9,135
Literature regarding outcome of treatment of specific fracture types,
however, is mostly comprised of case reports and small series and is
therefore scarce. There is particularly concern about poor functional
outcome after conservative treatment of displaced acromion, coracoid
process (base), scapular neck, and glenoid fossa fractures.1,3,49,127,135,148 With respect to functional outcome after operative treatment, most series concern glenoid fossa fractures57,66,84,98,112,156 and scapular neck fractures with or without an ipsilateral clavicle fracture.1,8,40,66,69,71,93,99,141,173 In a systematic review of 243 cases, Lantry97
pointed out that good to excellent functional results were obtained in
approximately 85% of cases which mainly consisted of displaced glenoid
fossa and scapular neck fractures. Limitations of interpreting these
study results are the retrospective character of the case series (level
IV) and the various outcome scales and scoring systems. In the above
mentioned studies, the following shoulder scoring systems were used:
American Shoulder and Elbow Surgeons,40 constant score,8,39,93,141,156,173,176 Herscovici score,39,71,139 Neer score,131,133 Rowe score,98,99 University of California, Los Angeles, score,69 or subjective scores based on the surgeon’s assessment mainly based on pain and range of motion.1,3,66,112,116,127
general is the lack of evidence-based treatment. The scientific
knowledge is based on case series and expert opinion (level IV and V).
The available literature includes neither randomized nor nonrandomized
comparative studies. Apart from the different nonvalidated and
nonspecific outcome measures and methodological limitations of many
studies, the influence is of associated injuries on the final outcome
is unclear.
well-documented, methodologically correct, comparative studies on the
fracture types that may benefit from surgical treatment, such as
displaced glenoid and scapular neck fractures.
PL, Lee MA, Finkemeier CG. Scapulothoracic dissociation: diagnosis and
treatment. Clin Orthop Relat Res 2003;416:237-244.
CP, Vanderspuy J. The fractured scapula: importance in management based
on series of 62 patients. Injury 1984;15:324-329.
PL, Reinert C, Kornberg M, et al. Displaced intra-articulair glenoid
fractures treated by open reduction and internal fixation. J Trauma
1986;26:1137-1141.
CM, Steger T, Galatz LM, et al. The posterior branch of the axillary
nerve: an anatomic study. J Bone Joint Surg 2003;85-A:1497-501.
G, Fleischmann W, Dussler E. Displaced scapular fractures: indication
and longterm results of open reduction and internal fixation. Arch
Orthop Trauma Surg 1995; 114:215-219.
DR, Morse SD, Barnes AU. Bilateral scapular fractures from low-voltage
electrical injury: a case report. Ann Emerg Med 1982;11:11-12.
MH, Obata WG. Diagnosis of posterior dislocation of the shoulder with
use of the Velpeau axillary and angled up radiographic views. J Bone
Joint Surg 1967;49-A: 943-949.
FJ, Cotler HB, Buckle R, et al. The medical and economic impact of
severely injured lower extremities. J Trauma 1988;28:1270-1273.
M, Can F, Kirdemir V, et al. Conservative treatment of scapular neck
fracture: the effect of stability and glenopolar angle on clinical
outcome. Injury 2005;36: 1176-1181.
CV, Velmahos G, Wang D, et al. Association of scapular fractures and
blunt thoracic aortic injury: fact or fiction? Am Surg 2005;71:54-57.
KP. Fractures of the scapula. In: Buchholz RW, Heckman JD, eds.
Fractures in Adults. 5th ed. Philadelphia: Lippincott Williams and
Williams, 2002:1095.
LP, Nunez MP, Llata JI. Arthroscopic-assisted reduction and
percutaneous external fixation of a displaced intraarticular glenoid
fracture. Arthroscopy 1999;15: 211-214.
EKJ, van Noort A, van der Helm FCT. Biomechanical analysis of scapular
neck malunion-a simulation study. Clin Biomech 2004;19:906-912.
RS, Brems JJ, Katschi H. Glenoid size, inclination, and version: an
anatomic study. J Shoulder Elbow Surg 2001;10:327-332.
Beer J, Berghs BM, van Rooyen KS, et al. Displaced scapular neck
fracture: a case report. J Shoulder Elbow Surg 2004;13:123-125.
AF. Fractures and fracture-dislocations of the shoulder girdle. In:
Jacob RP, Kristiansen T, Mayo K, et al., eds. Surgery of the Shoulder.
3rd ed. Philadelphia: JB Lippincott, 1983:366-367.
JS, Pedowitz RA, Garfin SR. Symptomatic pseudarthrosis of the scromion:
report of a case and review of the literature. J Orthop Trauma
1999;13:63-66.
NA, Mekhail AO, Padanilum TG, et al. Anatomic considerations for a
modified posterior approach to the scapula. Clin Orthop
1997;334:136-143.
HG, Zachrisson BE. Fracture of the scapular notch associated with
lesion of the suprascapular nerve. Acta Orthop Scand 1975;46:758.
SG, Whittle AP, Wood GW 2nd, et al. Nonoperative treatment of
ipsilateral fractures of the scapula and clavicle. J Bone Joint Surg
2000;82-A:774-780.
KA, Connor PM, Karunakar MA, et al. The floating shoulder: clinical and
functional results. J Bone Joint Surg 2001;83-A:1188-1194.
H, Kay SP. Arthroscopic subacromial decompression for chronic
impingement. Two- to 5-year results. J Bone Joint Surg
1991;73-B:395-398.
RP, Flynn TC, Miller PW, et al. Scapular fractures and associated major
ipsilateral upper-torso injuries. Current Concepts in Trauma Care
1985;1:14-16.
M, Salo JM. Nonunion of a fractured coracoid process after dislocation
of the shoulder. J Bone Joint Surg 1985;67-B:722-723.
WP, Slappey CE, Ochs CW. Roentgenographic demonstration of instability
of the shoulder: the apical oblique projection. J Bone Joint Surg
1984;66-A:1450-1453.
O, Curey JP, Mazas F. Recent fractures of the scapula. Apropos of 43
cases. Rev Chir Orthop Reparatrice Appar Mot 1984;70:443-447.
A, Marinelli M, Verdenelli A, et al. Arthroscopy-assisted reduction and
percutaneous fixation of a multiple glenoid fracture. Knee Surg Sports
Traumatol Arthroscopy 2003;11:112-115.
A, Crosland E, Pye J. Acromion fractures associated with posterior
shoulder dislocation. J Orthop Trauma 1998;12:521-522.
JT, Davis RT, Hartford JM, et al. Open reduction internal fixation
after displacement of a previously nondisplaced acromial fracture in a
multiply injured patient: case report and review of literature. J
Orthop Trauma 2001;15:369-373.
TP. Fractures of the scapula: diagnosis and treatment. In: Rockwood CA,
Matsen FA, Wirth MA, et al., eds. The Shoulder. Philadelphia:
Saunders-Elsevier, 2004: 413-454.
RJ, Calvert PT. Stress fracture of the acromion: an unusual mechanism
and review of the literature. J Bone Joint Surg 1995;77-B:153-154.
RD, Harris JH Jr. The prevalence and significance of missed scapular
fractures in blunt chest trauma. Am J Roentgenol 1988;151:747-750.
H, Ito H. Clinical outcome of the treatment of floating shoulder by
osteosynthesis for clavicular fracture alone. J Shoulder Elbow Surg
2003;12:589-591.
D Jr, Fiennes AG, Allgower M, et al. The floating shoulder: ipsilateral
clavicle and scapular neck fractures. J Bone Joint Surg
1992;74-B:362-364.
JM, McGuire MH, Crosby LA. Closed treatment of isplaced middle-third
fractures of the clavicle gives poor results. J Bone Joint Surg
1997;79-B:537-541.
K. Beobachtung eines U berlastungsschadens der Schulterblattgrate und
des Proc coracoideus. Wschr Unfallheilk 1942;49:53-59.
R. Fractures of the scapula involving the glenoid fossa. In Welsh R,
ed. Surgery of the Shoulder. Philadelphia, PA: BC Decker, 1984:63.
R, Grevsten S, Carsson S. Epidemiology of scapular fractures. Incidence
and classification of 338 fractures. Acta Orthop Scan 1995;66:395-397.
M, Yamaura I, Isobe Y, et al. Avulsion fracture of the superior border
of the scapula. J Bone Joint Surg 1981;63-A:820-822.
J, Greig M, Peuker ET. The posterior subdeltoid approach: a modified
access to the posterior glenohumeral joint. J Shoulder Elbow Surg
2001;10:265-268.
BF, Bradway JK, Cofield RH. Open reduction and internal fixation of
displaced intraarticular fractures of the glenoid fossa. J Bone Joint
Surg 1993;74-A: 479-484.
T, Andereya S, Gekle J, et al. Coracoid pseudarthrosis caused by
anterior shoulder dislocation with concomitant coracoid fracture.
Unfallchirurg 2002;105:843-844.
KC, Rhee KJ, Shin HD, et al. Can the glenopolar angle be used to
predict outcome and treatment of the floating shoulder? J Trauma
2008;64:174-178.
JE, Blasier RB, Carpenter JE. Fractures of the acromion process: a
proposed classification system. J Orthop Trauma 1994;8:6-13.
L, Platz A, Weishaupt D, et al. Clinical and functional results after
floating shoulder injuries. J Trauma 2004;57:595-602.
RH, Noel SH. Traumatic lateral scapular displacement: an expanded
spectrum of associated neurovascular injury. J Orthop Trauma
1993;7:361-366.
KS, Lam TP. Open reduction and internal fixation of ipsilateral
fractures of the scapular neck and clavicle. J Bone Joint Surg
1993;75-B:1015-1018.
KE, Wang CR, Chin KC, et al. Concomitant fracture of the coracoid and
acromion after direct shoulder trauma. J Orthop Trauma 1996;10:437-439.
A, Leven H. Prognosis in fractures of the body and neck of the scapula.
A follow-up study. Acta Chir Scand 1974;140:33-36.
P, Buckingham R, Stableforth PG. Avulsion injury of the subscapularis
tendon associated with fracture of the acromion. Injury 1994;25:271-272.
DJ, Sechriest VF 2nd, Swiontkowski MF, et al. Case report:
reconstruction of a recalcitrant scapular neck nonunion and literature
review. Clin Orthop Relat Res 2009;467(5):1370-1376.
JL, Slongo TF, Agel JNA, et al. Fracture and dislocation classification
compendium —2007: Orthopaedic Trauma Association classification,
database, and outcomes committee. J Orthop Trauma 2007;21:S1-S6.
SD, Weiland AJ. Missed scapular fracture after trauma. A case report
and a 23-year follow-up report. Clin Orthop 1994;299:259-262.
T, Rodriguez-Merchan C, Munuera-Martinez L. Fractures of the coracoid
process: presentation of seven cases and review of the literature. J
Trauma 1990; 30:1597-1599.
LS, Burkhead WZ, Gordon S, et al. Acromial fracture: a complication of
arthroscopic subacromial decompression. J Shoulder Elbow Surg
1994;3:256-261.
RE, Cocke TB, D’Ambrosia RD. Scapular fractures secondary to seizures
in patients without osteodystrophy. J Bone Joint Surg 1983;65-A:850-853.
TR, Blevins FT, Martin TP, et al. The role of plain films and
computered tomography in the evaluation of scapular neck fractures. J
Orthop Trauma 2002;16: 7.
JP, Rab GT. Fracture of the acromion associated with an axillary nerve
deficit: a case report and review of the literature. Clin Orthop Relat
Res 1980;147:216-218.
LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons
Standardized Shoulder Assessment Form, patient self-report section:
reliability, validity, and responsiveness. J Shoulder Elbow Surg
2002;11:587-594.
SP, Loyd RD. Avulsion fracture of the coracoid epiphysis with
acromioclavicular separation: report of two cases in adolescents and
review of the literature. J Bone Joint Surg 1977;59-A:963-965.
H, Endo S. Traumatic posterior dislocation of the shoulder with
fracture of the acromion in a child. Arch Orthop Trauma Surg
1996;115:238-239.
CS II. Fractures about the shoulder. In: Rockwood Jr CA, Green DP, ed.
Fractures. Philadelphia: JB Lippincott, 1984:713-721.
SL, Burgess A, Levine AM. Traumatic lateral displacement of the
scapula: a radiographic sign of neurovascular disruption. J Bone Joint
Surg 1984;66-A:758-763.
L, Mencia R, Alonso A, et al. Conservative treatment of ipsilateral
fractures of the scapula and clavicle. J Trauma 1997;42:239-242.
D, Regazzoni P, Renner N. The unstable shoulder girdle: early
functional treatment utilizing open reduction and internal fixation. J
Orthop Trauma 1995;9:93-97.
CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion
following nonoperative treatment of a clavicle fracture. J Bone Joint
Surg 2004;86-A: 1359-1365.
CA Jr. Dislocations about the shoulder. In: Rockwood CA Jr, Green DP,
eds. Fractures in Adults. 2nd ed. Philadelphia: JB Lippincott,
1984:719-721.
MW. Traumatic injuries of the shoulder and shoulder girdle. In: Dee R,
Hurst LC, Gruber MA, et al., eds. Principles of Orthopaedic Practice.
2nd ed. Columbus, OH: McGraw-Hill, 1997:398.
JR, Feagin JA, Abbott HG. Modified axillary roentgenogram. A useful
adjunct in the diagnosis of recurrent instability of the shoulder. Clin
Orthop Relat Res 1972; 82:84.
J, Schai P, Imhoff AB. Scapular neck fracture—the influence of
permanent malalignment of the glenoid neck on clinical outcome. Arch
Orthop Trauma Surg 2001;121:313-316.
S, Seil R, Kohn DM. Surgical reconstruction of a stress fracture of the
Acromion after arthroscopic subacromial decompression in an elite
tennis player. Arthroscopy 1998;14:106-108.
R, Vernaglia, Lombardi L, et al. Arthroscopic treatment of isolated
fracture of the posterolateral angle of the acromion. Arthroscopy
2007;23:798.
LN, Britton JC, Eldrup-Jorgensen J, et al. The neurovascular outcome of
scapulothoracic dissociation. J Vasc Surg 1993;17:1083-1089.
PA, Hintermann B, Koris MJ. Preoperative arthroscopic assessment of
fractures about the shoulder. Arthroscopy 1999;15:827-835.
P, Blauth M, Schneider C, et al. Fractures of the glenoid treated by
operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg
2002;84-B:173-177.
H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an
anatomic study. J Shoulder Elbow Surg 2001;10:372-376.
NG, Morgan AS, Corvo P, et al. Significance of scapular fracture in the
blunttrauma patient. Ann Emerg Med 1995;26:439-442.
AM, Lunsjo K, Czechowski J, et al. Multiple-region scapular fractures
had more severe chest injury than single-region fractures: a
prospective study of 107 blunt trauma patients. J Trauma
2007;63:889-893.
M, Moursy M, Eppel M, et al. Arthroscopic screw fixation of large
anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc
2008;6:326-332.
Slaa RL, Verburg H, Marti RK. Fracture of the coracoid process, the
greater tuberosity, and the glenoid rim after acute first-time anterior
shoulder dislocation: a case report. J Shoulder Elbow Surg
2001;10:489-492.
Noort A, te Slaa RL, Marti RK, et al. The floating shoulder, a Dutch
multicenter study (correspondence). J Bone Joint Surg 2002;84-B:776.
Noort A, van Kampen A. Fractures of the scapula surgical neck—outcome
after conservative treatment in 13 cases. Arch Orthop Trauma Surg
2005;125:696-700.
KC, Hsu KY, Shih CH. Coracoid process fracture combined with
acromioclavicular dislocation and coracoclavicular ligament rupture. A
case report and review of the literature. Clin Orthop Relat Res
1994;300:120-122.
MC, Evans EB. Fractures of the scapula. An analysis of 40 cases and a
review of the literature. J Bone Joint Surg 1977;59-A:358-362.
GR Jr, Naranja J, Klimkiewicz J, et al. The floating shoulder: a
biomechanical basis for classification and management. J Bone Joint
Surg 2001;83-A:1182-1187.
MA, Butters KP, Rockwood CA Jr. The posterior deltoid-splitting
approach to the shoulder. Clin Orthop Relat Res 1993;296:92-98.
AW, Shoji H, Chuinard RG. Unusual fracture of the coracoid process. A
case report and review of the literature. J Bone and Joint Surg
1976;58-A:423-424.
J, Quinlan W. Fractured coracoid process preventing closed reduction of
anterior dislocation of the shoulder. Injury 1989;20:296-297.
M, Bhandari M, Zelle BA, et al. Treatment of scapula fractures:
systematic review of 520 fractures in 22 case series. J Orthop Trauma
2006;20:230.
