Ankle Block
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section II – Single-Injection Peripheral Blocks > B – Lower Extremity > 15 – Ankle Block
15
Ankle Block
Thomas O. Clanton
David P. Loncarich
Anesthesia and immediate postoperative analgesia for any surgery below
the ankle including bunion correction, amputation, tendon repair,
fracture open reduction and internal fixation, arthrodesis, and lesser
toe correction. The entire foot or only a part of it can be blocked
depending on the surgical requirement.
-
The posterior tibial nerve,
a branch of the tibial nerve, travels behind the medial malleolus with
the posterior tibial artery and vein before passing through the tarsal
tunnel with the tendons of the flexor digitorum longus, flexor hallucis
longus, and posterior tibialis. It provides motor innervation to the
muscles on the plantar aspect of the foot and sensory innervation to
the plantar aspect of the foot. The posterior tibial nerve divides into
four terminates branches: (a) the medial plantar nerve, (b) the lateral
plantar nerve, (c) the calcaneal sensory branches, and (d) the nerve to
the abductor digiti quinti. -
The superficial peroneal nerve
is a branch of the common peroneal nerve. It travels down the leg deep
to the fascia and exits to the subcutaneous tissue approximately 10 to
14 cm above the lateral malleolus. At varying levels it then branches
into the medial dorsal cutaneous nerve and the lateral or intermediate
dorsal cutaneous nerve. The superficial peroneal nerve is purely
sensory and provides sensation to the dorsal aspect of the foot, the
lateral aspect of the hallux, and the second through fourth toes. -
The deep peroneal nerve
is a branch of the common peroneal nerve. It travels with the anterior
tibial artery between the tendons of the extensor hallucis longus and
the extensor digitorum longus. It divides into the medial and lateral
branches, and provides sensory innervation to the first web space.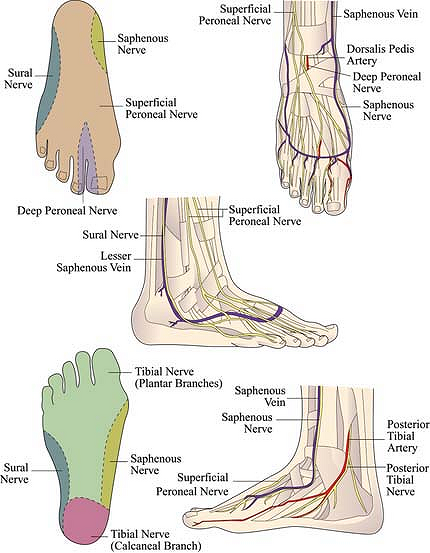 Figure 15-1. Anatomic landmarks.
Figure 15-1. Anatomic landmarks. -
The sural nerve
is a purely sensory nerve formed from the branches of the common
peroneal nerve (anastomotic branch) and the tibial nerve (median sural
nerve). It travels along the lateral border of the Achilles tendon and
passes 1.0 to 1.5 cm distal to the tip of the lateral malleolus. At
this point, it gives off the calcaneal and cutaneous branches and
subsequently terminates as medial and lateral branches. The sural nerve
provides sensory innervation to the dorsolateral aspect of the foot
including the fourth and fifth toes. -
The saphenous nerve
is a terminal branch of the femoral nerve. It travels posterior to the
saphenous vein on the anteromedial aspect of the tibia. At the ankle,
it is approximately one fingerbreadth anterior to the medial malleolus.
It terminates as two branches: the anterior and posterior branches. It
provides sensory innervation to the medial aspect of the ankle, foot,
and hallux.
P.158
P.159
 |
|
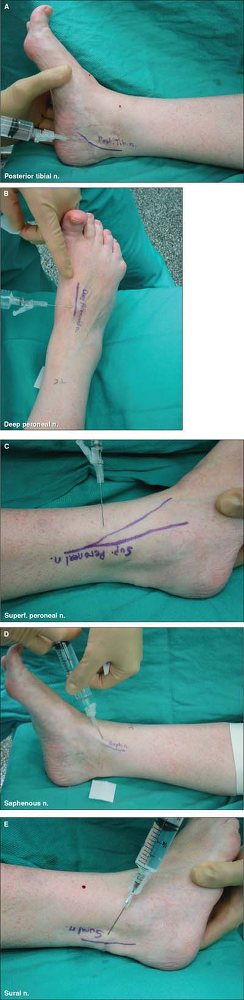
Figure 15-2. Approach and technique.
Block of the posterior tibial nerve.
The leg is rotated laterally to allow access to the posteromedial aspect of ankle. It lies in the tarsal tunnel, one fingerbreadth posterior to the tip of the medial malleolus. Palpation of the posterior tibial artery provides guidance. The needle is inserted posterior to the palpated pulse. After negative aspiration for blood, 5 to 7 mL of the local anesthetic mixture is slowly injected with concomitant palpation of the tendon sheath filling to ensure accurate placement. Block of the deep peroneal nerve.
The dorsalis pedis pulse is palpated in the interval between the extensor hallucis longus and the extensor digitorum longus. The deep peroneal nerve lies lateral to the pulse. The needle is inserted perpendicular to the skin and down to the level of the tarsal bones. The needle is slightly withdrawn, and, after negative aspiration for blood, 5 to 7 mL of the local anesthetic mixture is slowly injected. Block of the superficial peroneal nerve.
The branches of the superficial peroneal nerve are blocked with a ring of anesthetic in the subcutaneous tissue of the anterior ankle. As a guide, the lateral branch can be palpated after plantar flexing the foot and the fourth toe. The subcutaneous tissue on the anterior aspect of the ankle at the level of the malleoli is infiltrated with 5 to 10 mL of the local anesthetic mixture. Block of the saphenous nerve.
The saphenous nerve is located two fingerbreadths proximal and one fingerbreadth anterior to the tip of the medial malleolus. Approximately 5 to 7 mL of the local anesthetic mixture is injected in the subcutaneous tissues after negative aspiration for blood. Block of the sural nerve.
The leg is rotated medially to allow access to the lateral aspect of the ankle. The sural nerve is one fingerbreadth distal to the tip of the lateral malleolus within the subcutaneous tissues. The needle is inserted, and the region is infiltrated with approximately 5 to 7 mL of the local anesthetic mixture. |
-
Local infection and prolonged tourniquet time represent relative contraindications for this block.
-
Although the block can be performed
without sedation, intravenous sedation usually increases patient
tolerance during the procedure. -
A combination of a short-acting
anesthetic (lidocaine) and a long-acting anesthetic (bupivacaine or
ropivacaine) provides an optimal effect for most procedures.
Epinephrine is generally not required and has the potential for local
and systemic complications. -
Because the posterior tibial nerve is the biggest of these nerves to be blocked, it is important to block it first.
-
Alternatively, the posterior tibial nerve
can also be blocked by inserting the needle perpendicular to the tibial
shaft at two fingerbreadths proximal to the tip of the medial malleolus
and just medial to the Achilles tendon where the posterior tibial nerve
lies posterior to the tibial metaphysis. -
Alternatively, the superficial peroneal
nerve can be blocked at its exit from the fascia in the distal leg.
Approximately 10 to 14 cm above the ankle joint the nerve has exited
the fascia and lies in the subcutaneous tissues, one to two
fingerbreadths lateral to the tibial crest. The needle is inserted
perpendicular to the leg, and 5 to 10 mL of the local anesthetic
mixture is injected in the subcutaneous tissue anterior to the fascia
of the anterior and lateral compartments.
P.160
P.161
Suggested Readings
Coughlin MJ. Peripheral anesthesia. In: Mann RA, Coughlin MJ, eds. Surgery of the foot and ankle, 7th ed. St. Louis: Mosby-Year Book, 1999:131–148.
Myerson MS, ed. Foot and ankle disorders. Philadelphia: WB Saunders, 2000.
Netter F. Atlas of human anatomy. Summit, NJ: Ciba-Geigy, 1989.
