Medial Epicondylitis
Georgetown University Medical School, Washington, D.C.; and Arlington
Hospital/Nirschl Orthopedic Sports Medicine Clinic, Arlington, Virginia.
chronic loads applied to the flexor pronator mass of the forearm
resulting in activity-related medial and elbow proximal forearm pain (6).
It is approximately one-fourth as common as lateral epicondylitis and
has a similar demographic profile. The concomitant presence of ulnar
neuropathy at the elbow is seen in 30% to 50% of patients and may be
the primary management concern (3,5,9).
Physical examination reveals direct epicondylar tenderness and indirect
tenderness with resisted pronation. Ulnar nerve examination may
demonstrate a positive Tinel’s sign, elbow flexion test, or nerve
compression test. Valgus stress examination is essential to assess
medial instability either as an associated concern or as the primary
process. Subluxation of the medial head of the triceps and medial
antebrachial cutaneous neuropathy should be ruled out as well (1,7).
diagnoses, most commonly degenerative arthritis (which may require
diagnostic xylocaine injection of the elbow to differentiate an
intraarticular or extraarticular source of symptoms). Valgus stress
radiographs should be obtained if indicated. Magnetic resonance imaging
is usually not required, as this is primarily a clinical diagnosis.
To simplify the original classification, type I is an isolated medial
epicondylitis and type II is medial epicondylitis with an associated
ulnar neuropathy. This may be further classified as of minimal or
moderate severity.
similar to that of lateral epicondylitis, including corticosteroid
injection, counterforce bracing, wrist splinting, and a conditioning
program. Injections should be placed at the anterior aspect of the
epicondyle with the elbow in extension to avoid the ulnar nerve (8)
as well as the anterior oblique fragment. Instances of type I medial
epicondylitis that fail to respond to nonoperative management and all
type II medial epicondylitis are indications for surgical intervention.
surgery are pain that limits daily activity and/or interrupts sleep.
The duration of nonoperative management is a minimum of 6 to 9 months
and ideally at least 12 months. All conservative measures should have
been tried. At least one cortisone injection is helpful to isolate the
lesion, and failure of this therapy strengthens the indications for
surgery.
physical that does not accurately coincide with expectations of medial
epicondylitis. Poor motivation, worker’s compensation, and unrealistic
expectations are also issues of concern and to be considered before
surgical intervention is carried out. Individuals who are improving or
who have had symptoms less than 6 months are generally not considered
candidates for surgery.
classification of medial epicondylitis. Operative management of type I
medial epicondylitis involves medial epicondylar debridement alone. The
type II medial epicondylitis may require ulnar nerve decompression,
including cubital tunnel release if symptoms are mild (A) or medial
epicondylar debridement and ulnar nerve transposition if nerve symptoms
predominate (B). Medial epicondylitis should be avoided, as anterior
epicondylar removal (for the medial epicondylitis) and posterior
epicondylar removal (for the ulnar nerve) may result in compromise of
the anterior oblique ligament origin. When medial epicondylar
debridement is carried out, the flexor pronator mass is already
violated, so submuscular translocation is logical.
in association with submuscular ulnar nerve transposition and medial
epicondylar debridement. The obvious concern of elevation of the active
medial elbow stabilizer (the flexor pronator mass) at the same time as
the passive ligamentous restraint (the anterior oblique ligament) can
be obviated by formal repair of the flexor pronator origin in addition
to the anterior oblique ligament (AOL) reconstruction.
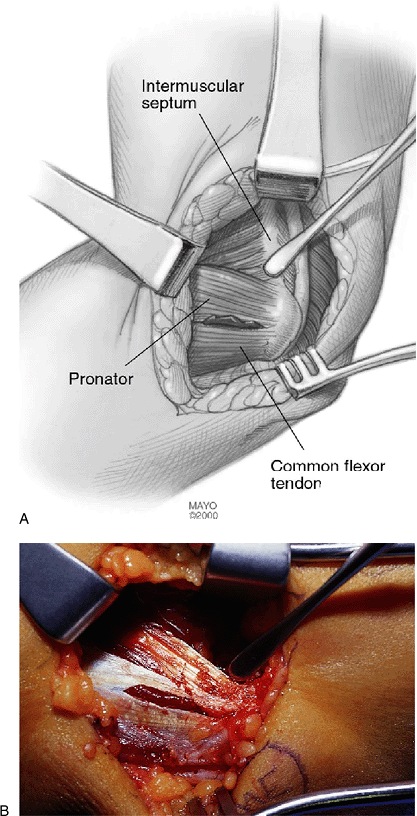
focus in medial epicondylitis. The MCT is the perpendicularly oriented
septum originating on the anterior aspect of the medial epicondyle and
separates the common flexor and pronator teres origins (Fig. 13-1).
It lies immediately anterior to the anterior oblique ligament with, in
most cases, no identifiable interval between these two structures. The
MCT serves as the intramuscular tendon origin for the flexor pronator
mass musculature, including the flexor carpi radialis, the pronator
teres, the palmaris longus, and the flexor digitorum sublimis. At the
level of the medial epicondyle the tendon is fully conjoint and remains
so for the first 2 cm, at which point the MCT splits into two septae
separated by the muscle belly of the flexor carpi radialis. The
anterior oblique ligament remains along the posterior border of the MCT
throughout the course of the anterior oblique ligament. The medial
conjoint tendon extends distally 10 to 12 cm into the forearm. Gross
pathologic involvement of the tendon is seen within the proximal 2 to 3
cm of the tendon, the level where it is conjoint. It is at this level
that the surgical debridement in medial epicondylitis is conducted.
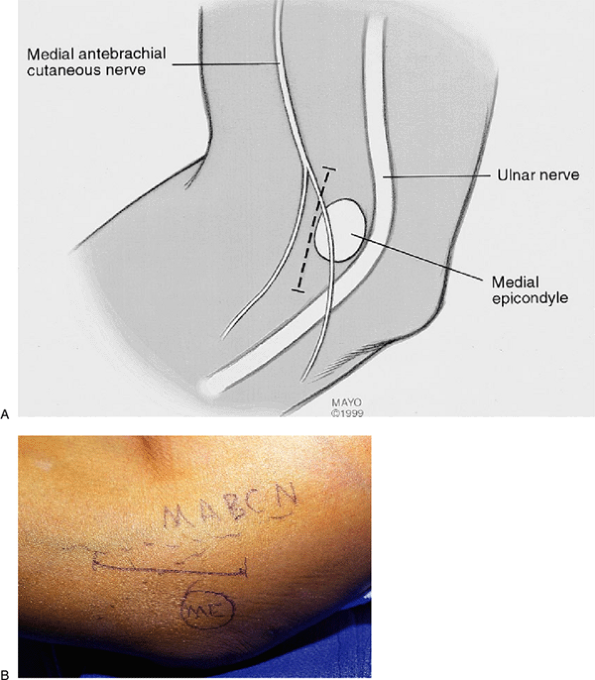
prepped and draped in usual fashion. A longitudinal incision is created
starting 1 cm anterior to the proximal margin of the medial epicondyle
and extending distally for 3 to 4 cm (Fig. 13-2). Blunt subcutaneous dissection is performed to allow for identification and protection of the posterior branch of the medial
antebrachial cutaneous nerve (Fig. 13-3).
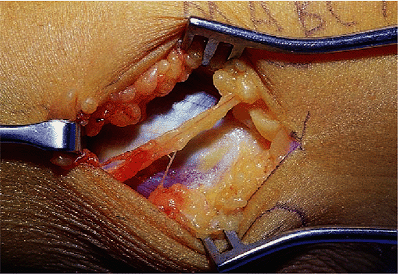
The flexor pronator fascia is discretely exposed from the proximal
margin of the pronator teres origin at the superior aspect of the
medial epicondyle extending distally to a level approximately 3 cm
distal to the inferior aspect of the medial epicondyle. The superficial
fascia of the flexor pronator mass is incised starting at its proximal
(pronator teres) edge leaving a 3- to 4-mm rim attached to the
epicondyle. This initially involves elevation of the pronator teres
muscle off the anterior aspect of the medial epicondyle, but as
dissection extends distally to the anterior inferior margin of the
epicondyle, the proximal border of the medial conjoint tendon is
encountered. The superficial fascia of
the
flexor pronator mass is incised longitudinally along the anterior edge
of the medial conjoint tendon. Pronator teres elevation continues in a
proximal-to-distal manner off the anterior margin of the medial
conjoint tendon with tenotomy scissors to discretely expose the
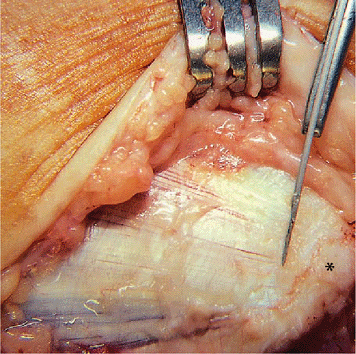
proximal 2 to 3 cm of the medial conjoint tendon. The medial conjoint
tendon is usually 2 to 3 mm thick from anterior to posterior, and the
posterior margin can be readily identified using a freer elevator or
tenotomy scissors to expose this posterior margin (Fig. 13-4).
 |
|
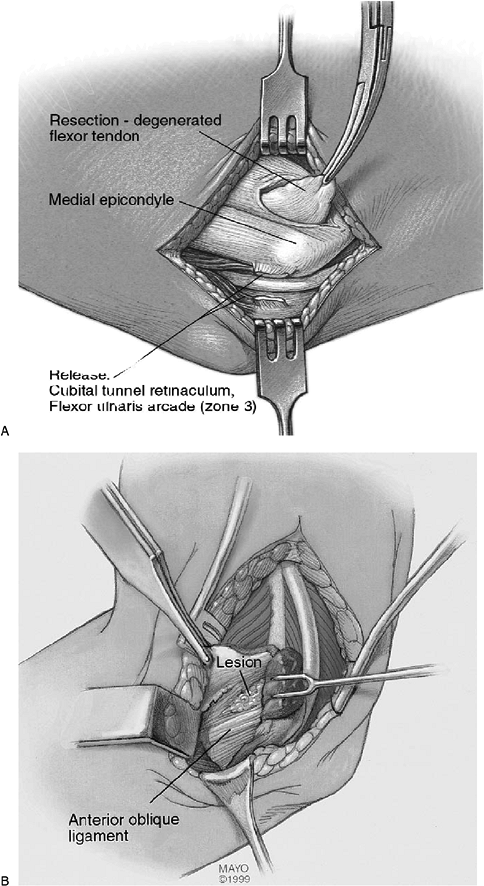
Figure 13-1. A,B:
The medial conjoint tendon within the flexor pronator mass. This is the tendinous origin of the flexor carpi radialis, pronator teres, palmaris longus, and flexor digitorum sublimis. It lies immediately anterior to the anterior oblique ligament. |
 |
|
Figure 13-2. A,B:
Incision for medial epicondylar debridement with or without cubital tunnel release. This incision can be extended proximally and distally for conversion to a transposition procedure if necessary. |
 |
|
Figure 13-3.
Exposure of flexor pronator mass. Note the posterior branch of the medial antebrachial cutaneous nerve, which can be easily identified and protected. |
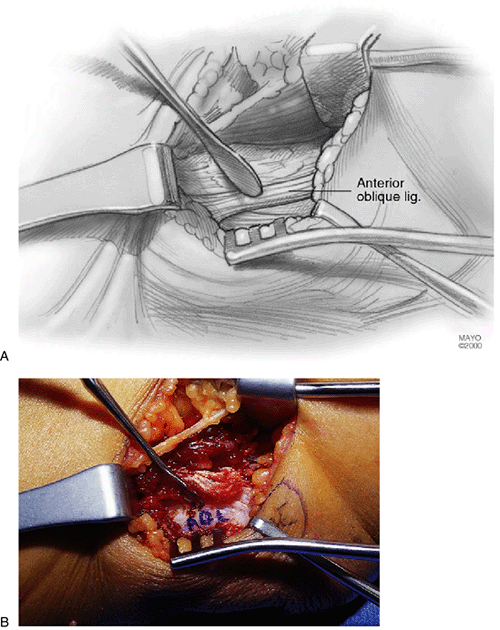
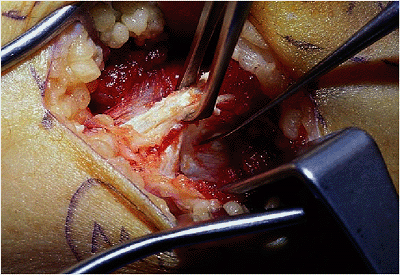
If a degenerative nidus is present it is usually seen at the proximal
aspect of the medial conjoint tendon along its anterior margin
extending at times to the posterior aspect of the tendon. The anterior
oblique ligament can be seen and palpated with a freer elevator
immediately posterior to the medial conjoint tendon (Fig. 13-6).
The interval between these two structures can be developed by passing
the freer elevator down along the posterior margin of the medial
conjoint tendon, creating an interval at the corner formed by the
anterior oblique ligament and the medial conjoint tendon. Once the
anterior oblique ligament is identified, debridement of the medial
conjoint tendon can be safely and fully performed. Tenotomy scissors or
a scapula are used to elevate the origin of the medial conjoint tendon
of the anterior aspect of the epicondyle, leaving the anterior oblique
ligament. The tendon is elevated off the epicondyle flush with the
anterior oblique ligament and elevation continues distally, again flush
with the ligament for 2 to 3 cm. At this point, the proximal 2 to 3 cm
of the medial conjoint tendon have been isolated and are excised with
tenotomy scissors (Fig. 13-7). The anterior
oblique ligament can be inspected but is usually grossly normal except
in chronic valgus loading situations. (This is usually anticipated
preoperatively on physical examination.)
 |
|
Figure 13-4. A,B:
Elevation of pronator teres muscle from the anterior aspect of the medial epicondyle and from the anterior aspect of the medial conjoint tendon. The probe marks the proximal anterior margin of the medial conjoint tendon. |
 |
|
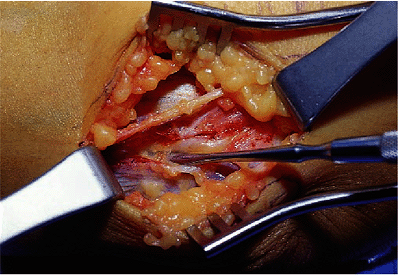
Figure 13-5. A,B: Extensive degenerative lesion and disruption of the common flexor pronator origin at the medial conjoined tendon.
|
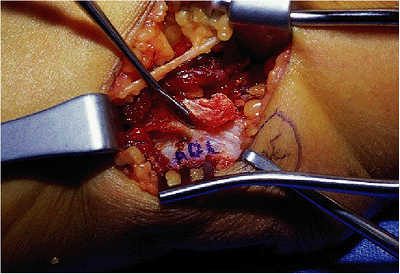 |
|
Figure 13-6.
Posterior dissection along the medial conjoint tendon exposes the anterior oblique ligament contiguously along the posterior border of the medial conjoint tendon. There is typically no anatomic interval, but a surgical interval can be identified (at the level of the probe) to allow excision. |
 |
|
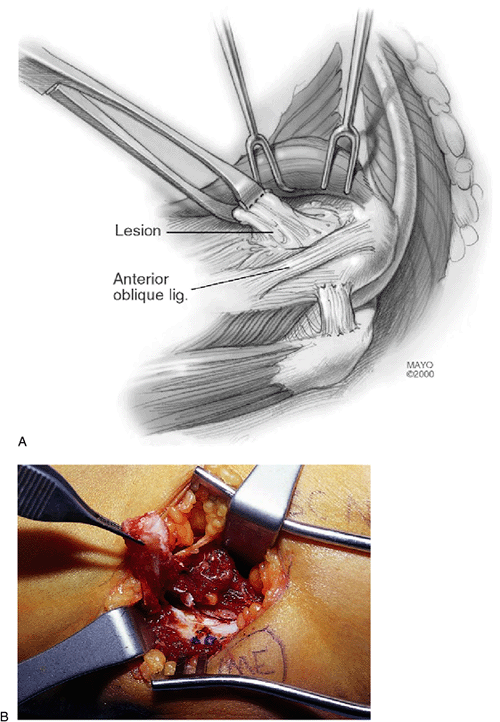
Figure 13-7. A,B:
Isolation and excision of the medial conjoint tendon. The tendon is elevated directly off the medial epicondyle with a scalpel turning distally immediately superficial to the anterior oblique ligament. The proximal 2 to 3 cm of the medial conjoint tendon should be excised. The superficial fascia of the flexor pronator mass is then closed in an anatomic fashion. |
be “freshened up” with a rongeur, and the superficial fascia of the
flexor pronator fascia is closed with a 2-0 vicryl suture side to side
and to the remnant attached to the epicondyle. Skin closure is
completed and a bulky dressing is applied, followed by application of a
single sugar tong splint with the wrist and forearm at neutral.
most common side of impingement is the so-called zone 3 of Nirschl.
Cubital tunnel release can be performed in this setting or submuscular
transposition can be elected. Cubital tunnel release is acceptable only
when the environs of the ulnar nerve at the cubital tunnel are pristine
(i.e., no prior trauma, good nerve gliding without scarring, and no
subluxation with flexion either before or following cubital tunnel
release). The procedure of debriding the medial conjoint tendon is
identical to that given earlier but is performed after the nerve status
has been assessed, and if submuscular transposition is felt to be
required, the debridement occurs with tendon origin release. The
initial skin incision is the same as that for isolated medial
epicondylar debridement. Attention is directed posteriorly to the
cubital tunnel before violating the flexor pronator fascia. The
posterior margin of the medial epicondyle is identified and the flexor
carpi ulnaris fascia is exposed (Fig. 13-8).
The fascia overlying the nerve is opened with tenotomy scissors at the
posterior/inferior corner of the medial epicondyle. The fascia is then
incised for 4 to 5 cm, exposing the two heads of the flexor carpi
ulnaris muscle. These two heads are bluntly spread apart, exposing the
deep fascia of the flexor carpi ulnaris, which lies directly on the
ulnar nerve (Fig. 13-9). This fascia layer must be released as well to complete the cubital tunnel release.
bed. If there is any structural abnormality of the cubital tunnel
(e.g., adhesions, exostoses), then conversion to a submuscular
transposition is initiated.
 |
|
Figure 13-8. Posterior dissection to expose cubital tunnel region. Identify the posterior inferior corner of the medial epicondyle.
|
 |
|
Figure 13-9.
Cubital tunnel release is performed starting at the posterior inferior corner of the medial epicondyle, incising the flexor carpi ulnaris arcade, bluntly creating the interval between the two heads of the flexor carpi ulnaris muscle and releasing the deep fascia of the flexor carpi ulnaris immediately superficial to the ulnar nerve. If examination of the nerve reveals any significant abnormality, conversion to a submuscular transposition is elected. |
translocation a 12- to 15-cm incision over the course of the ulnar
nerve is created. The medial antebrachial cutaneous nerve is identified
and protected distally in the wound. Attention is directed proximally,
incising the brachial fascia overlying the nerve posterior to the
medial intermuscular septum, proximal to the medial epicondyle. The
fascia is incised proximally, releasing the arcade of Struthers in the
process. With the elbow in relative extension to relax the nerve, the
fascia is incised distally, ultimately extending into the fascia of the
flexor carpi ulnaris. The deep flexor pronator aponeurosis within the
flexor pronator mass is bluntly decompressed by placing metzenbaum
scissors, tips up, on the ulnar nerve and gently advancing immediately
superficial to the nerve and deep to the flexor pronator aponeurosis.
This completes the decompression.
The first motor branch, to the ulnar head of the flexor carpi ulnaris,
is mobilized by performing an intramuscular neurolysis to gain 1 to 2
cm of length to allow the ulnar nerve to translate anteriorly without
kinking.
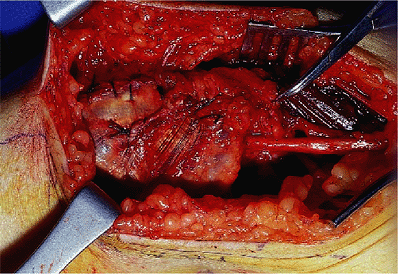
mass is elevated, leaving a 2- to 3-mm tuft of fascia attached to the
epicondyle (Fig. 13-10). The lacertus fibrosis
is incised to free up the proximal margin of the pronator teres. The
flexor pronator is elevated distally, exposing the medial conjoint
tendon within the muscle mass. The medial conjoint tendon is isolated
for its proximal 3 to 4 cm (Fig. 13-11) and
incised along the anterior margin of the anterior oblique ligament
(similar to debridement alone). It is then excised, to debride the
tendon origin, but also to prevent fascial compression of the nerve
with repair of the flexor pronator mass. Elevation of the flexor
pronator mass continues posterior to the MCT, again with care not to
violate the anterior oblique ligament. The posterior fascia of the
humeral head of the flexor carpi ulnaris is incised to allow reentry of
the ulnar nerve into the flexor pronator mass without impingement on
this fascial structure.
 |
|
Figure 13-11.
Once isolated, the proximal 2 to 3 cm is elevated, being careful to avoid the anterior oblique ligament. This portion of the tendon is resected to address the medial epicondylitis as well as to allow placement of the ulnar nerve deep to the flexor pronator mass without secondary compression. |
 |
|
Figure 13-10.
Submuscular transposition involves the standard decompression and nerve mobilization as in pure ulnar neuropathy. Flexor pronator mass elevation consists of pronator teres evaluation and isolation of the medial conjoint tendon. |
 |
|
Figure 13-12.
The flexor pronator mass is repaired with approximately 1 cm of lengthening to provide more room for the ulnar nerve as well as to functionally lengthen the muscle group (pointer is at original proximal margin of FP mass). The superficial fascia is repaired at the flexor carpi ulnaris arcade as well as at the level of the conjoint tendon. |
pronator mass and the alignment is assessed proximally and distally for
new levels of compression or acute angulation. Further release is
performed as needed to prevent new levels of compression in the nerves’
newly transposed position. The flexor pronator fascia is repaired in a
lengthened fashion repairing the fascia 1 cm distal to its anatomic
position. This allows for more room beneath the flexor pronator mass
for the ulnar nerve and minimizes the risk of recurrent impingement.
The fascial closure includes the flexor carpi ulnaris (FCU) arcade, as
the nerve is now deep to this layer and the repair allows for more
secure repair of the fascia and provides more coverage of the nerve (Fig. 13-12).
Skin closure is completed and the arm is placed into a single sugar
tong splint, well padded at the posterior elbow to prevent splint
irritation of the wound.
placed in an elbow immobilizer at 90 degrees of flexion, the forearm is
in neutral, and the wrist and hand are free. After 2 days, gentle
active assisted motion exercises are usually started (tendon and/or
tendon with nerve surgery). Intermittent immobilizer protection is
usually continued for 6 to 7 days, at which time normal activities of
daily living are resumed. Counterforce support providing protective
function is utilized until full forearm strength returns (usually 3 to
6 months). The brace is used at times of rehabilitation exercise and
more vigorous forearm activities, such as heavier household activities.
A gradual return to sports often is initiated at 8 to 10 weeks with
brace protection. For the type IIB procedure, sutures are removed at 10
days and a Muenster cast is applied for an additional 2 weeks in all
cases except if a concomitant lateral epicondylar debridement has been
performed (in which case a wrist splint is applied and noncomposite
range of motion is initiated to prevent elbow stiffness). The cast is
removed after an additional 2 weeks and noncomposite range of motion is
started, progressing to composite range of motion at week 5 or 6.
Strengthening is started at 6 weeks, if tolerated, and a flexor
pronator program is continued until symmetric pain-free strength is
gained. A counterforce brace is continued until after full strength is
restored and full-duty
status is reserved until the same point in time. This takes a minimum of 3 to 6 months on the average.
expectations of surgery for medial epicondylitis. Three recent reports
all reveal a greater than 90% satisfaction with this surgery (3,6,9).
However, both Gabel and Morrey, and Kurvers and Verlan emphasize the
poor prognosis associated with ulnar nerve involvement. Final outcome
is realized in 6 months in most but may take more than a year to fully
recover in some.
elbow is residual pain. This is not common in the Mayo or Jobe
experience and occurs in fewer than 10% of patients. However, Kurvers
et al. report a significantly worse prognosis with medial epicondylitis
than with lateral epicondylitis.
concerns. Medial antebrachial cutaneous neuropathy (MABCN) may result
from avulsion, traction, or transection of the nerve. If this is
recognized intraoperatively, the nerve should be mobilized proximally
and transposed into the brachialis muscle belly. If the neuropathy is
identified postoperatively, a desensitization program as well as
neurogenic pain medication, such as nortriptyline™ or neurontin™, is
started. A corticosteroid injection at the point of maximum Tinel’s may
be useful if the neuropathic pain persists. Sympathetic mediated pain
may result from MABCN injury, but is not synonymous. If other hallmarks
of a sympathetic mediated pain process are identified, pain management
consultation may be indicated.
is not uncommon, especially if a transposition has been performed.
Objective incomplete loss of function of the ulnar nerve is uncommon
but usually also resolves spontaneously. Complete loss of nerve
function is quite rare and may indicate compression from a hematoma,
fibrous band, or acute angulation. Complete loss of function requires
early reexploration but may be associated with no objective level of
compression, indicating a possible intraneural vascular event. Recovery
is usually seen even in these circumstances but is typically incomplete.
result in medial instability of the elbow. If this occurs, anterior
oblique ligament reconstruction may prove to be necessary to alleviate
symptoms.
prolonged recovery rather than a failure of the procedure. Symptoms
that recur or continue after 6 months should be managed in a manner
similar to that of the preoperative program. If injections are used
after a transposition procedure, they should be kept well medial on the
epicondyle to avoid intraneural injection of the ulnar nerve.
Significant epicondylar symptoms that persist beyond 18 to 24 months
may require revision, but this is the case in fewer than 2% to 3% of
medial epicondylitis cases. Persistent ulnar nerve symptoms are more
common but still rarely require revision, especially following a
submuscular transposition. Cubital tunnel release may be associated
with persistent or increased ulnar nerve symptoms and may be revised to
a submuscular transposition (2) if indicated.
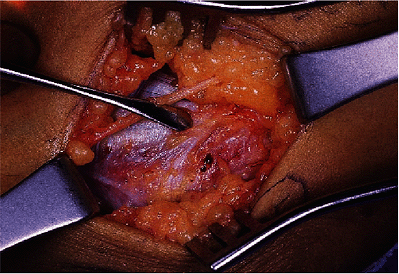
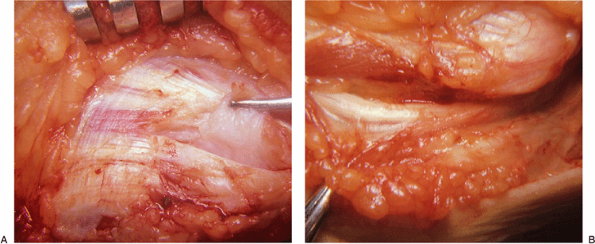
symptoms for 1 year without response to conservative management. Ulnar
nerve irritation to palpation was present in zone 3. At surgery the
pathology was identified at the interval between the flexor carpi
radialis and
pronator teres muscle origin (Fig. 13-13). The ulnar nerve was decompressed and the patient had a full recovery.
 |
|
Figure 13-13.
Exploration of flexor pronator origin revealed amorphous tissue at the medial conjoined tendon at the interval between the flexor carpi radialis and the pronator origin (A). Because ulnar nerve symptoms were present, the nerve has been decompressed distally (B). |
RJ, Goldner RD. Surgery of the medial head of the triceps and recurrent
dislocation of the ulnar nerve: anatomical and dynamic factors. J Bone Joint Surg 1998;80A:239.
