Kienböck Disease
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Kienböck Disease
Kienböck Disease
Marc W. Hungerford MD
Dawn M. LaPorte MD
Description
-
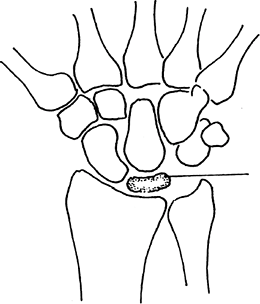
Kienböck disease is AVN of the lunate of the wrist with collapse of the bone and arthritis in the advanced stage (Fig. 1).
-
The classification system by Stahl (1), which was later modified by Lichtman et al. (2), is based on the radiographic appearance of the lunate:
-
Stage 1: Radiographically normal lunate or with small fracture lines
-
Stage 2: Sclerosis of the lunate
-
Stage 3a: Collapse of the lunate
-
Stage 3b: Lunate collapse with proximal migration of the capitate and fixed rotation of the scaphoid
-
Stage 4: Generalized wrist arthrosis
-
-
Modification (3,4):
-
Stage 0: MRI evidence of AVN of the lunate and no plain radiographic findings
-
-
Synonym: Lunatomalacia
Epidemiology
-
Most common in young adults (20–40 years old)
-
Gender predominance uncertain
-
Disease onset usually in young to middle adulthood
Incidence
~1 per 1,000
 |
|
Fig. 1. Kienböck disease is AVN of the lunate, usually followed by flattering of this bone (stippled).
|
Risk Factors
-
Ulnar-negative wrist:
-
The carpal bones of the wrist, which are supported by the distal radius and ulna, should be the same length.
-
The term “ulnar-negative wrist” refers to a short ulna, which causes more pressure to be borne by the radial side of the wrist.
-
The ulnar-negative variant wrist is thought to overload the lunate and predispose to Kienböck disease.
-
Similarly, the lunate is perfused through a single nutrient artery, so it is thought to be at higher risk (5).
-
-
Disorders leading to ischemia of the lunate, such as sickle cell anemia
-
Traumatic ligamentous disruption of the intercarpal ligaments
Genetics
No known correlation exists.
Etiology
-
Although this disease was originally described by Kienböck in 1910 (6), the precise cause has yet to be determined.
-
Theories proposing a primary ischemic or traumatic origin are supported in the literature.
-
Current consensus supports repetitive microtrauma in the lunate at risk.
Signs and Symptoms
-
Most patients complain of pain and
stiffness with tenderness over the dorsal lunate (middle of the wrist)
on physical examination. -
Alternatively, patients may have little pain but markedly decreased grip strength.
-
If untreated, the pain may increase progressively and develop into arthritis of the wrist.
History
Many patients give a history of a recent hyperextension injury of the wrist.
Physical Exam
Tenderness with palpation over the anatomic snuffbox and/or dorsal lunate is noted.
Tests
Imaging
-
Radiography:
-
Plain AP radiographs of the wrist often establish the diagnosis.
-
The lunate may show a lucent line.
-
In more advanced cases, sclerosis or collapse may be seen.
-
-
An ulnar variance view with the shoulder
in 90° of abduction, the elbow in 90° of flexion, and the wrist in
neutral rotation should be obtained.
-
Pathological Findings
-
A transverse internal fracture of the lunate has been described in 75% of cases, but it rarely is recognized clinically.
-
Changes characteristic of AVN are seen in biopsy specimens.
Differential Diagnosis
-
Scapholunate ligament tear
-
Scaphoid fracture
-
Perilunate dislocation
-
Wrist arthritis
-
Ulnar impaction syndrome
General Measures
-
The optimal treatment for patients with Kienböck disease is debated, but the following generally are accepted:
-
The wrist should be splinted and the patient referred to a hand specialist for additional treatment.
-
Untreated, the condition may follow a course of relentless radiologic progression, but the clinical course is variable.
-
Most practitioners favor some surgical intervention in the young, active patient with early-stage disease.
-
Radial shortening or ulnar lengthening may be considered if the ulna is short.
-
Proximal row carpectomy, limited fusion, arthroplasty, or another reconstructive procedure may be considered for advanced cases.
-
P.207
Special Therapy
Physical Therapy
-
Physical therapy usually is not necessary except in the postoperative period.
-
Splinting of the wrist helps relieve discomfort.
Surgery
-
Stage 1 and 2 disease:
-
Surgery is aimed at lunate load reduction or improvement of lunate perfusion.
-
Load reduction may be achieved by
joint-leveling procedures (in the case of the ulnar-negative wrist) or
limited intercarpal fusion. -
Perfusion may be improved through vascularized bone grafts.
-
-
Stage 3 disease:
-
A proximal row carpectomy may provide symptomatic relief while maintaining ROM.
-
-
Stage 4:
-
Wrist fusion is the treatment of choice.
-
Prognosis
Degenerative arthritis usually results if left untreated.
Complications
-
Increasing pain, clicking
-
Wrist arthritis
Patient Monitoring
Even if no surgery is performed initially, the patient
should be followed periodically with serial radiographs to determine
whether collapse and arthritis are progressive.
should be followed periodically with serial radiographs to determine
whether collapse and arthritis are progressive.
References
1. Stahl
F. On lunatomalacia (Kienbock’s disease): a clinical and
roentgenological study, especially on its pathogenesis and the late
results of immobilization treatment. Acta Chir Scand Suppl 1947;95:1–133.
F. On lunatomalacia (Kienbock’s disease): a clinical and
roentgenological study, especially on its pathogenesis and the late
results of immobilization treatment. Acta Chir Scand Suppl 1947;95:1–133.
2. Lichtman DM, Mack GR, MacDonald RI, et al. Kienbock’s disease: the role of silicone replacement arthroplasty. J Bone Joint Surg 1977; 59A:899–908.
3. Amadio PC, Hanssen AD, Berquist TH. The genesis of Kienbock’s disease: evaluation of a case by magnetic resonance imaging. J Hand Surg 1987;12A:1044–1049.
4. Cristiani G, Cerofolini E, Squarzina PB, et al. Evaluation of ischaemic necrosis of carpal bones by magnetic resonance imaging. J Hand Surg 1990; 15B:249–255.
5. Gelberman RH, Bauman TD, Menon J, et al. The vascularity of the lunate bone and Kienbock’s disease. J Hand Surg 1980;5A:272–278.
6. Kienbock R. Uber traumatische Malazie des Mondbeins und ihre Folgezustande: Entartungsformen und Kompressionsfrakturen. Fortschr Geb Rontgenstr 1910;16:77–103.
Additional Reading
Almquist EE. Kienböck’s disease. Hand Clin 1987;3:141–148.
Amadio PC, Moran SL. Fractures of the carpal bones. In: Green DP, Hotchkiss RN, Pederson WC, et al, eds. Green’s Operative Hand Surgery, 5th ed. Philadelphia: Elsevier Churchill Livingstone, 2005;711–768.
Weiland AJ. Avascular necrosis of the carpus. In: Hand Surgery Update. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:85–92.
Codes
ICD9-CM
732.3 Kienböck’s disease
Patient Teaching
The patient should be counseled about the natural history of the disease and the need for rest or activity restriction.
FAQ
Q: What are signs and symptoms of Kienböck disease?
A:
Patients typically present with complaints of wrist pain localized to
the region of the lunate; this pain is present at rest as well as with
activity. Decreased wrist ROM also is seen frequently in Kienböck
disease. Swelling and tenderness dorsally in the area of the lunate
also may be seen.
Patients typically present with complaints of wrist pain localized to
the region of the lunate; this pain is present at rest as well as with
activity. Decreased wrist ROM also is seen frequently in Kienböck
disease. Swelling and tenderness dorsally in the area of the lunate
also may be seen.
Q: How is the diagnosis of Kienböck disease made?
A:
The diagnosis usually is made with radiographs. In the early stages,
radiographs can be negative, and MRI or bone scan can support the
diagnosis if Kienböck disease is strongly suspected.
The diagnosis usually is made with radiographs. In the early stages,
radiographs can be negative, and MRI or bone scan can support the
diagnosis if Kienböck disease is strongly suspected.
