Klippel-Feil Syndrome
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Klippel-Feil Syndrome
Klippel-Feil Syndrome
Dhruv B. Pateder MD
Darryl B. Thomas MD
Description
-
Klippel-Feil syndrome is part of group of disorders characterized by malformations of the axial skeleton.
-
Specifically, this syndrome is defined by the failure of segmentation of the cervical vertebrae.
-
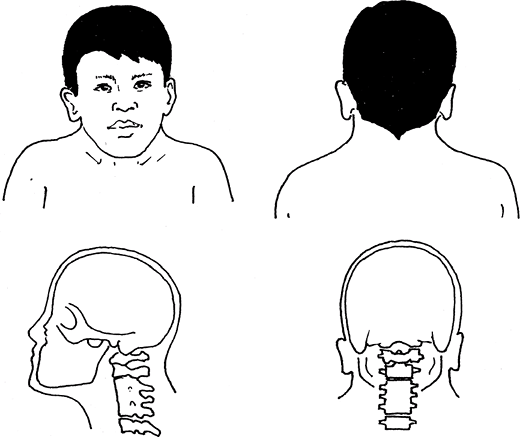
Its classic triad includes a low hairline, short neck, and limited neck motion (Fig. 1).
-
Associated conditions include congenital
scoliosis, Sprengel deformity, hearing impairment, synkinesis, and
congenital heart disease. -
Classification (1):
-
Type I: Fusions involving cervical and upper thoracic vertebrae
-
Type II: Fusions of cervical vertebrae only (several segments may be fused)
-
Type III: Type I or II with lower thoracic or lumbar vertebrae involvement
-
General Prevention
No known preventive measures
 |
|
Fig. 1. Klippel-Feil syndrome is congenital cervical fusion. It is evidenced by a short, stiff neck and a low hairline.
|
Epidemiology
-
The incidence in the general population is unknown because no screening studies have been done.
-
The anomaly develops in embryogenesis.
-
The age of presentation varies: Massive
fusions usually are noted earlier (2–4 years), whereas degenerative
changes present later (after age 4 years) (2–4). -
Female:Male ratio is 1.5:1 (2–4).
-
Most young patients are asymptomatic and present incidentally.
-
Symptomatic stenosis tends to occur in the 4th decade of life and result in sensory or motor disturbances of the extremities.
Incidence
The incidence of congenital cervical fusions is ~0.7% (2–4).
Risk Factors
-
Spina bifida
-
Congenital renal anomalies
Genetics
-
This condition is phenotypically heterogeneous and may be sporadic, but familial autosomal dominant patterns have been observed.
-
Mouse model studies suggest involvement with the PAX gene families and notch signaling pathway (2–4).
-
A chromosomal inversion—(8) (q22.2q23.3)—has been found to segregate with Klippel-Feil syndrome in some families.
Etiology
-
Although the cause is unknown, the
prevalent hypothesis suggests that Klippel-Feil syndrome results from
incomplete sclerotomal segmentation during embryologic development. -
Other nonspecific hypotheses include
abnormal facet joint segmentation, multiple or global insults to the
fetus (e.g., hypoxia), and vascular disruptions or malformations.
Associated Conditions
-
Musculoskeletal: Sprengel deformity
(failure of normal descent of the scapula), scoliosis (both congenital
and idiopathic in up to 60% of patients [2–4]), spinal stenosis, spina
bifida occulta -
Craniofacial: Hearing abnormalities, extraocular muscle palsy
-
Genitourinary: Renal abnormalities (up to 30% of patients [2–4]), including unilateral renal agenesis
-
Cardiovascular: Various congenital heart malformations
Signs and Symptoms
-
The clinical triad (low hairline, short
neck, and limited neck motion) is seen in 40–50% of patients, with
decreased neck motion in up to 75% of patients and shortening of the
neck (with resulting lowering of posterior hairline) in <50% (2–4). -
Patients also may be diagnosed after cervical spine changes are found incidentally on imaging studies.
-
Other findings may include scoliosis, deafness, and renal and cardiac anomalies.
Physical Exam
-
Careful examination of the patient
focused on the cervical spine (including resting appearance, posture,
and ROM) and a general neurologic examination -
Complete physical examination to evaluate for associated anomalies in other organ systems
P.209
Tests
Imaging
-
Radiography:
-
Conventional radiographs of the cervical
spine show various patterns and degrees of vertebral fusion ranging
from simple block vertebrae to multiple anomalies.-
Up to 50% show anterior, posterior, and lateral portions of vertebrae fused (2–4).
-
Fusion rates: Vertebral bodies alone, ~20% of cases; posterior fusions alone, 9%; and lateral fusions alone, 3% (2–4).
-
Spina bifida occulta often is seen.
-
Spinal stenosis at the level of the
segmentation defect is observed occasionally and may develop with aging
because of degenerative changes from adjacent segment hypermobility.
-
-
Flexion and extension radiographs are
important for assessing potential instability, especially before
undergoing intubation and surgery.
-
-
MRI will show any compression of neural elements.
-
CT-myelography is comparable to MRI in showing neural compression, but it is an invasive procedure.
Pathological Findings
-
Congenital cervical fusions, which may be associated with instability
-
Discs in the area of fusion are narrow or absent, and the remaining mobile discs show degeneration from overuse.
-
Degenerative joint disease
-
Spinal stenosis
-
Subluxation may occur over time.
Differential Diagnosis
-
Cervical fusion after a previous surgery
-
Torticollis from muscular causes
-
Cervical spinal stenosis
General Measures
-
Evaluation of all patients with Klippel-Feil syndrome:
-
Additional evaluation for other organ system problems, including congenital cardiac, renal, or neurologic abnormalities
-
Renal imaging (a simple renal ultrasonogram)
-
Conventional flexion and extension
lateral radiographs before any general anesthetic to rule out occult
cervical spine instability -
MRI scan if concern exists about neurologic involvement on a clinical basis and before any spine surgery
-
-
Treatment:
-
Course depends heavily on the severity of the associated renal or cardiac problems.
-
It is important to identify patients with an increased risk of neurologic injury.
-
Nonsurgical treatment includes cervical collars, bracing, and analgesics.
-
Surgical fusion is indicated when
instability results in neurologic symptoms or in patients with
documented (e.g., via MRI) stenosis. -
Patients should avoid strenuous
activities, contact sports, and occupations and recreational activities
that increase the risk of head trauma.
-
Special Therapy
Physical Therapy
Indicated for general conditioning in those patients who are symptomatic from their spinal or other systemic problems
Medication
No role for maintenance opiates
First Line
-
Anti-inflammatory medications (as long as no gastrointestinal side effects present)
-
Enteric-coated aspirin (fewer gastrointestinal side effects)
-
Acetaminophen
Second Line
-
COX-2 inhibitors (be aware of changing side-effect profile)
-
Epidural steroids
Surgery
-
Preoperative evaluation by an internist, cardiologist, and/or anesthesiologist is necessary.
-
Other than for neurologic symptoms,
surgery is indicated when nonoperative treatment fails and the patient
cannot attain a tolerable quality of life. -
Compensatory curves below the level of
primary congenital fusions, whether symptomatic or not, should be
monitored carefully and treated with bracing or fusion because these
curves are likely to progress and cause major deformities. -
Surgery may be required for associated anomalies, such as Sprengel deformity, scoliosis, or cervical rib resection.
Prognosis
Some patients develop neck pain or extremity weakness with time.
Complications
-
Spinal stenosis often is associated and may become symptomatic.
-
Paralysis or paraparesis may occur from cervical spine trauma in patients with extensive lesions.
Patient Monitoring
Patients should be followed regularly by an orthopaedic surgeon and by other specialists if other systems are involved.
References
1. Gunderson CH, Greenspan RH, Glaser GH, et al. The Klippel-Feil syndrome: genetic and clinical reevaluation of cervical fusion. Medicine 1967; 46:491–512.
2. Baba H, Maezawa Y, Furusawa N, et al. The cervical spine in the Klippel-Feil syndrome: a report of 57 cases. Int Orthop 1995;19:204–208.
3. Guille
JT, Miller A, Bowen JR, et al. The natural history of Klippel-Feil
syndrome: clinical, roentgenographic, and magnetic resonance imaging
findings at adulthood. J Pediatr Orthop 1995;15:617–626.
JT, Miller A, Bowen JR, et al. The natural history of Klippel-Feil
syndrome: clinical, roentgenographic, and magnetic resonance imaging
findings at adulthood. J Pediatr Orthop 1995;15:617–626.
4. Loder
RT. The cervical spine. In: Morrissy RT, Weinstein SL, eds. Lovell and
Winter’s Pediatric Orthopaedics, 4th ed. Philadelphia:
Lippincott-Raven, 1996:739–779.
RT. The cervical spine. In: Morrissy RT, Weinstein SL, eds. Lovell and
Winter’s Pediatric Orthopaedics, 4th ed. Philadelphia:
Lippincott-Raven, 1996:739–779.
Codes
ICD9-CM
756.16 Klippel-Feil syndrome
Patient Teaching
-
Patients should be educated about:
-
The potential for progressive motor weakness and bladder/bowel dysfunction
-
The general natural history of the condition
-
FAQ
Q: What is the classic triad of Klippel-Feil syndrome?
A: A low hairline, short neck, and limited neck motion.
Q: What are the 2 major visceral systems involved in Klippel-Feil syndrome?
A: Cardiac and genitourinary.
