Acute Wrist and Hand Injuries
reasons for this fact stem from use of the hand as a working tool in
sometimes dangerous environs (e.g., as an object holder immediately
adjacent to a power tool) and the all too frequent use of the arm as
brake (fall onto an outstretched arm). A patient’s general health
characteristics may play an important role in determining the frequency
and outcome from such accidents (e.g., diabetics with originally
reduced sensation and ongoing reduced blood supply/immune function and
osteoporosis with reduced skeletal strength). There are several issues
to be considered with all patients:
-
Date of last tetanus immunization.
One should consider the possibility of skin compromise with injuries to
the hand and wrist. Even without obvious laceration, penetration of
infectious organisms into the subcutaneous tissue has been known to
occur. The effects of infection from one such organism (tetanus) are
largely preventable. Consequently, whenever possible, verify the status
of tetanus immunization in all patients whom you are treating for hand
or wrist trauma. -
Injury site characteristics.
These may alter your treatment choices. For example, a fracture with a
nearby clean laceration from a sharp object can often be managed as
though the skin had remained closed, whereas the same fracture
associated with a minimal but contaminated (farmyard or sewage)
puncture into the fracture hematoma must first be thoroughly irrigated.
Thus, the first key characteristic is to
establish the extent of the skin injury and to specifically determine
if any external injection of organisms deep into the skin surface is
likely to have occurred. In the case of burns (cold or hot), knowledge
of the depth of the skin injury is important. It is important to be
specific when describing wounds. Adjectives used to modify established
terminology (e.g., severe “bad” or not bad) should be avoided. Use
phrases or classification with known meaning whenever possible.Helpful adjectives used in characterizing a wound include:-
Open or closed: used most commonly in association with a fracture. If
the skin is open to a fracture, it is considered open. This same
phraseology is important in treating lacerations close to joints and
some tendon injuries. -
Clean or contaminated: generally, a kitchen knife would be considered clean as compared to a saw blade picked up from a farmyard workbench.
-
Tidy or untidy:
the margin of a laceration can be so ragged as to prevent repair. In
the hand (the same applies to the foot and face), this can preclude
tensionless wound closure and thus necessitate advanced wound
management methods.
-
-
Patient’s habits and addictions.
Without doubt, the most important habit to be aware of is the patient’s
habit of following medical advice. This is particularly important in
children, and the emergently consulted physician has a known
responsibility to enable timely follow-up care. The majority of hand
and wrist injuries requiring consultation from an orthopaedic
specialist will need early (2–14 days) follow-up, and failure to ensure
this care may result in disability. Other habits of importance include
the following:-
Tobacco use disorder.
In addition to being an established diagnosis (ICD-9 = 305.1), this
problem will impact bone healing (known) as well as other tissues
(skin, tendon, nerve) (suspected). -
Recreational drug use.
Impaired patients will place stresses on casts and dressings such that
the medical repairs may fail. In some circumstances, hospital admission
with appropriate consults is required.
-
-
Systemic illness.
Illness which compromises immune function is a common reason for
delayed recovery after hand/wrist injury. Additionally, diseases such
as rheumatoid arthritis or advanced osteoporosis will impact the result
from injury and the type of treatment that can be chosen.
-
Where and how did the injury occur?
As noted above, record the location of the injury and its mechanism.
This is important for two basic reasons. First, you need to know the
cleanliness of the wound and how much energy
was applied to the tissues. Second, you need to record the where (work,
home, motor vehicle accident, etc.) and how (an allegedly defective
tool, a reported assailant, etc.) because the first examining document
will be used henceforth as the “truth.” Thus, your written history
should contain few adjectives and only known facts. -
How did the patient become aware of the injury?
Some injuries will present after the suspected injury occurred. In
these instances, recording additional facts related to the patient’s
presentation is important. -
Pain
-
Location.
Be specific. Use anatomic descriptors. Try to avoid use of “medial and
lateral” and numbering the digits (due to misinterpretations). The
second finger is not the index but the middle. Thus, do not use number
references for fingers as too many physicians and most lay people
mistake the index for the second finger (which it is not). Use the
following terms: radial and ulnar; dorsal and volar; thumb, index,
middle, ring, and small finger. -
Qualities.
Phrases such as “really bad pain” are meaningless. Words such as
burning, radiating, and tingling may be helpful in detecting/isolating
a nerve injury, whereas words such as deep, constant, and throbbing may
be associated with an infection.
-
-
Numbness
-
Location (similar to C.1).
Describe the anatomic location of the numbness using precise words
(e.g., the radial border of the ring finger). These phrases will
hopefully be anatomically possible and serve to isolate the nerve
difference. Patients describing anatomically unlikely numbness are
occasionally seeking secondary gain. -
Qualities. As in C.2,
specificity is important. In addition, record frequency and inciting
factors (e.g., the numbness occurs when I am driving for 20 minutes or
more).
-
-
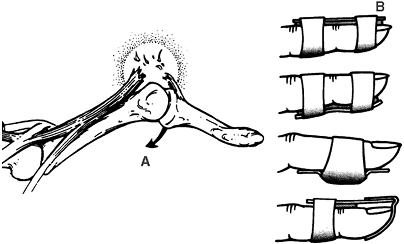
Range of motion. Specific ranges to be recorded are demonstrated in Fig. 19-1 and summarized in Table 19-1.Idealized numbers are inserted. The key to a successful exam is to measure left and right in the affected areas.
-
Active. Active motion helps to document the integrity of tendons and the stability/congruity of joints.
-
Passive.
Differences and similarities between active and passive motion can help
to document/differentiate several conditions, for example, disrupted
tendons (active will be low/absent and passive will be high/normal) and
stiff joints (active will be low and passive will be low).
-
-
Strength.
Generally, the international classification for muscle strength is
used. Thus, a muscle can be graded from 0 (flaccid and no evidence of
innervation) to 5 (normal). However, specific strengths are often
measured in the hand and forearm and compared over time.-
Pinch strength. Measured with a “pinch gauge” and recorded in pounds or kilograms.
-
Key. Thumb to side of index or middle finger (strong, used for rotation)
-
Chuck. Thumb to pulp of two fingers (strong and moderately precise)
-
Tip. Thumb to one finger pulp (weakest and most precise)
-
-
Grip strength. Measured with a “dynomometer” and recorded in pounds or kilograms.
-
Can be recorded in several diameters and useful to “quantify” malingering as well as recovery over time.
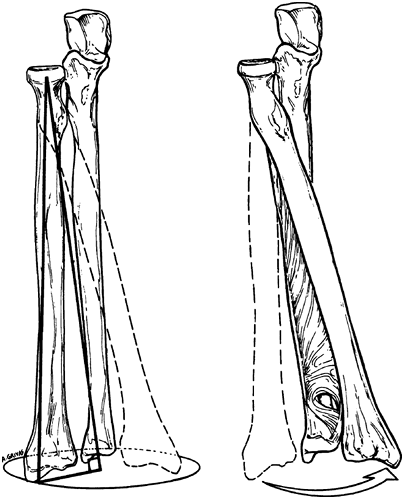
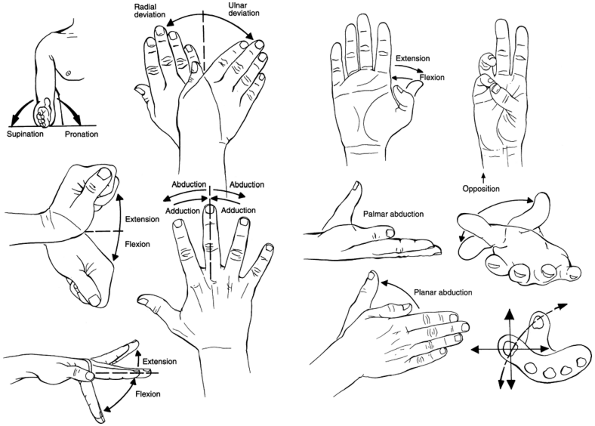 Figure 19-1. Terminology for describing forearm, hand, and digital motion. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)TABLE 19-1 Normal Hand and Wrist Motion
Figure 19-1. Terminology for describing forearm, hand, and digital motion. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)TABLE 19-1 Normal Hand and Wrist MotionMotion: Active (passive) Right Left Supination (occurs at distal radio-ulnar joint) 90 (90) Same Wrist flexion (occurs at radiocarpal and midcarpal joints 70 (90) Same Wrist extension (occurs at radiocarpal and midcarpal joints) 70 (90) Same Wrist radial deviation (occurs at radiocarpal and midcarpal joints) 20 (30) Same Wrist ulnar deviation (occurs at radiocarpal and midcarpal joints) 40 (50) Same Finger abduction and adduction (occurs at metacarpalphalangeal joint (MCPJ), index to small) 20 (20) Same Finger base extension and flexion (occurs at MCPJ, index to small) 10 (30) Same Thumb and finger individual joint extension and flexion 0 to 90 (10, extension to 100, flexion) Same Thumb palmar abduction 45 (45) Same Thumb opposition (how close to small finger base) 0 cm; able to touch base of small finger Same Thumb radial (planar) abduction 45 (45) Same
-
-
-
General. The
hand and wrist are extensions of the extremity and, as such, depend
upon an intact skin envelope to protect against systemic illness (e.g.,
septicemia).Beyond skin, the hand has three primary functions:
sensation, movement, and cosmesis. Nerves; bones and joints; and
tendons and muscles all play an important role in determining the
outcome after injury and care. -
Region specific exam
-
Distal radio-ulnar joint.
This joint works in combination with the proximal radio-ulnar joint to
guide the rotation of the distal radius around the ulnar head (distal
portion of the ulna). Fig. 19-2 demonstrates this important motion.-
Muscle. The
pronator quadratus muscle originates immediately proximal to the distal
radioulnar joint (DRUJ). It has a deep and superficial head and helps
to stabilize and pronate the forearm. The muscle is innervated by the
terminal branch of the anterior interosseous nerve. The muscle can be
injured in conjunction with distal radius fractures. -
Tendon. The
extensor carpi ulnaris and the extensor digiti minimi tendons run
alongside and dorsal to the ulnar head. Occasionally, the tendon sheath
will tear and the extensor carpi ulnaris (ECU) tendon can become
unstable. Also, a lax or irregular DRUJ can damage the extensor digit
minimi (EDM) tendons. Otherwise, no direct attachment of tendon to the
joint occurs. -
Joint/bone.
The DRUJ is interesting. It is a “roll and slide” joint. Considerable
variance in design occurs. What is universally true is that an unstable
DRUJ is uncomfortable or painful. When the joint does not work well, it
usually results in a loss of supination. An unusual but possible injury
to the joint would be dislocation without fracture in either the volar
or dorsal direction. -
Triangular fibrocartilage complex (TFCC).
First described in 1981, the TFCC is the major ligamentous stabilizer
of the distal radio-ulnar joint and the ulnar-carpus joint. Within this
triangular complex is cartilaginous material that may be injured either
acutely (e.g., from a fall onto an outstretched hand) or chronically
(e.g., from overuse with the wrist in an
P.269
ulnar-deviated
position such as with the use of a computer mouse). Patients with
ulnar-sided wrist pain that is made worse with compression (analogous
to hyperflexion of the knee when assessing for meniscal tears) may have
a TFCC injury.![]() Figure 19-2.
Figure 19-2.
The axis of rotation of the radius with respect to the ulna, with the
center of the axis of rotation being aligned beginning at the center of
the radial head and ending near the center of the distal part of the
ulna. Rotation is guided by the interosseous membrane and the
triangular fibrocartilage. (From Peimer CA. Surgery of the hand and upper extremity. New York: McGraw-Hill, 1996, with permission.) -
Nerve and vessel.
A rare but reported injury is entrapment of the ulnar nerve and/or
ulnar artery following reduction of a completely dislocated DRUJ. This
would generally require a complete separation to occur between the
radius and ulnar head but could also occur in a young child who could
fracture through the physeal plate and in combination with a fracture
just proximal to the ulnar head. In any event, the important point is
to carefully assess nerve function before and after reduction maneuvers
and carefully account for any change in function after reduction.
-
-
Wrist
-
Muscle.
Indirectly and directly, muscles arise from the wrist. Specifically,
the thenar and hypothenar muscles arise from the transverse carpal
ligament (thenars) or the hook of hamate and the pisiform
(hypothenars). Function of these muscles can be reduced in combination
with injuries to their attachments. This would include an indirect
injury to the attachments
P.270
of
the transverse carpal ligament such as would occur with a trapezial
fracture, scaphoid tubercle fracture, or pisiform fracture. -
Tendon.
Tendons do not attach directly to any of the main seven carpal bones
(the pisiform is a sesamoid and not a true carpal bone; the flexor
carpi-ulnaris does surround the pisiform). However, the flexor
carpi-radialis does appear to attach indirectly by way of a sheath to
the scaphoid tubercle and consequently transfer a flexion vector to the
scaphoid. Also, the wrist and its adjacent soft tissues act as a guide
for both the flexor and extensor tendons. Specifically, the carpal
canal guides the thumb and finger flexors as well as the median nerve.
The extensor retinaculum (Fig. 19-3,
the wrist extensor compartments 1 to 6) stabilizes the finger extensors
immediately proximal to the radio-carpal joint and acts as both a
pulley for these motors both in extension as well as radial and ulnar
deviation. Fractures or lacerations affecting tendons in this area
often result in significant stiffness. This may be the result of many
structures being injured as well as a consequence of tendons in this
area possessing a large excursion. Thus, any loss of tendon glide will
be noticeable. -
Joint/bone.
Motion of wrist depends upon ligament control of two rows of bones
affected by muscles attaching to bones at varying distances distal to
the wrist. This arrangement is similar to the ankle. However,
nonobvious ligament tears [normal x-rays and nonspecific magnetic
resonance imaging (MRI) scans] can significantly disable the normal
wrist. This is often the result of a disconnection occurring between
the proximal and distal carpal rows. This type of disconnection can
occur without obvious bone
P.271
injury.
Usually, injury to the scapho-lunate interosseous ligament (SLIL) is
the cause of such a injury. However, bone injury can produce the same
effect upon the wrist, and the most common fracture causing wrist
instability is a scaphoid waist fracture. Finally, although not
frequently causing wrist instability, distal radius fractures can cause
ligament injury in addition to causing joint surface irregularity
and/or poor fit with resultant joint capsular stiffness.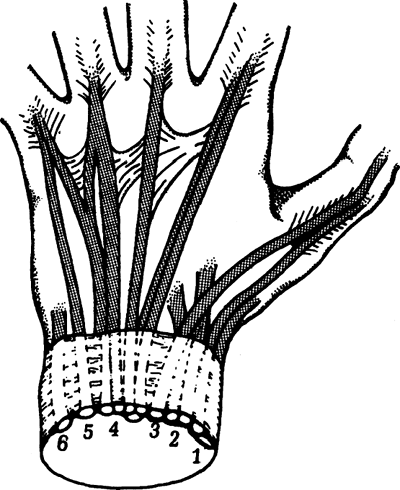 Figure 19-3. Arrangement of extensor tendons at the wrist into six compartments: dorsal and cross-sectional views. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-3. Arrangement of extensor tendons at the wrist into six compartments: dorsal and cross-sectional views. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.) -
Nerve and vessel.
Close proximity of three sensory (radial, median, and ulnar) and two
motor (median and ulnar) nerves can result in nerve compression
symptoms. Actual direct injury to the nerves is rare.
-
-
Proximal hand
-
Muscle. The
base of the hand is the site of attachment for extrinsic (muscles
originating from the forearm) wrist extensors, flexors, and deviators
as well as the thumb abductor. Also, the hand base is the origin of the
hand intrinsics. Destabilization by fracture of the hand base or
metacarpal shafts can be made significantly worse by muscle tone.
Splinting attempts to neutralize these forces. -
Tendon. The
finger extensors are adjacent to the dorsal metacarpal bone surface.
Thus, in addition to acting as a shortening force, the extensors can be
injured or entrapped by displaced metacarpal fractures. Tendons
overlying dorsally angulated mid-shaft fractures are most at risk. -
Joint/bone.
Two joints are involved in the proximal hand separated by the
metacarpal shaft. The proximal joint varies from the near universal
thumb base to the effectively immobile second and third
carpalmetacarpal (CMC) joints. The distal joint is remarkable for its
unicondylar, multiaxial shape. Distally, the bone shape allows some
radial-ulnar laxity which is reduced to none as the
metacarpalphalangeal joint (MCPJ) moves into flexion and the collateral
ligaments tighten. An interesting note: the metacarpal epiphyseal plate
is distal in the second thru fifth fingers and proximal in the thumb. -
Nerve and vessel.
Immediately distal to the volar aspect of CMC joints, the ulnar and
median nerve splits into its common digital nerve components. In this
same region, interconnections between the radial and ulnar artery via
the deep and superficial arches occur. Significant swelling,
displacement, or lacerations can result in loss of vascular injury.
-
-
Fingers
-
Muscle. The fingers do not contain any muscle tissue.
-
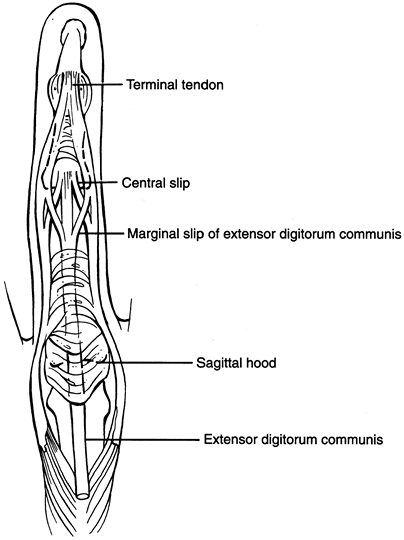
Tendon. The fingers are balanced by an intricate arrangement of flexor and extensor tendons. Fig. 19-4
depicts the complex balance achieved by the extrinsic and intrinsic
extensors. The apparent key finger extension occurs at the proximal
interphalangeal joint (PIPJ). At this level, the intrinsic tendons
transit from volar to dorsal and rely upon thin, easily injured,
retinacular structures to maintain their position. Closed injury to
these structures with progressive loss of PIPJ and increasing fixed
extension at the distal interphalangeal joint are the hallmarks of the
developing boutonierre deformity. Fig. 19-5
illustrates the anatomy of the flexor pulleys. These pulleys guide the
flexor tendon and its surrounding tenosynovial sheath during motion of
the flexor tendons. Injuries involving the flexor pulleys can result in
scarification to the tendons themselves even without tendon laceration.
Perhaps more importantly, the pulleys enclose a space which is easily
infected after a puncture wound and can serve as a path for infection
into the palm and, in the case of the small finger and thumb, into the
wrist and forearm (see V.A). -
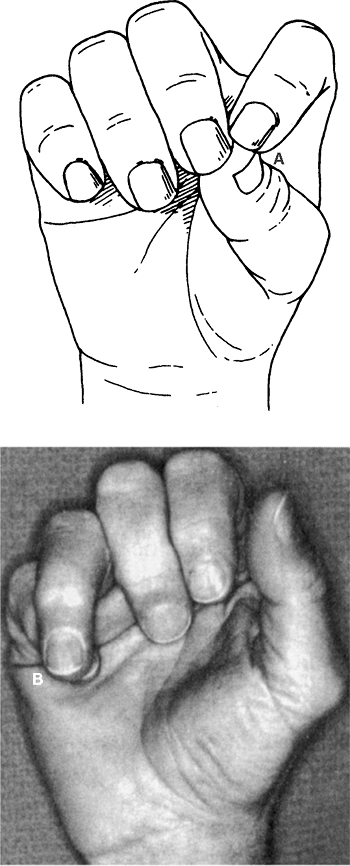
Joint/bone.
Unlike the more proximal unicondylar MCPJs, the finger interphalangeal
joints are bicondylar and uniaxial. This configuration results in a
joint which is stable throughout the axis of rotation. Theoretically,
this results in a more stable arrangement for pinch and grip
activities. However, this lack of rotational tolerance also means that
small changes in rotation of
P.272
a finger may be easily noticed and interfere with adjacent digit function. Fig. 19-6
illustrates the problem associated with rotational deformity of a
finger. Thus, the key deformity to rule out when evaluating a finger
fracture is rotational over- or underlap. Because one role of the
fingers is grasp/pinch and release, it is apparent that stable joints
are essential. But, ligament injuries to the fingers and thumb are
common. One such injury is a “gamekeepers’s” thumb. As illustrated in Fig. 19-7,
this injury may be a partial sprain or can result in complete
disruption of the ulnar collateral ligament at the MCPJ and require
surgical repair. Similar injures can occur at the PIPJ of the fingers
and occasionally overlap with complete dislocations. In all such
patients, an x-ray should be obtained and a congruent joint reduction
should be present.![]() Figure 19-4. Extensor apparatus over the dorsum of the digits. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-4. Extensor apparatus over the dorsum of the digits. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)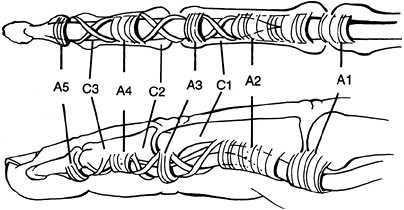 Figure 19-5. The annular and cruciate pulleys of the flexor tendon sheath. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-5. The annular and cruciate pulleys of the flexor tendon sheath. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.) -
Nerve and vessel.
The nerves and blood vessels are situated immediately adjacent to the
flexor tendons and maintained in position by dorsal (Cleland’s) and
volar (Grayson’s) fascial “ligament-like” tissue. Isolated injuries to
the nerve and vessel do occur and are sometimes described as cuts with
excessive bleeding. However, restoring blood flow is almost never an
issue because of sufficient redundancy from the remaining blood vessel,
whereas single nerve injuries can be problematic and require repair
when the injury involves pinch surfaces and or border digits. For
central digits, nerve repair is elective and oftentimes performed only
to manage painful neuromas.
P.273 -
-
-
Wrist
-
Tendon and nerve.
Nerve and tendon injuries in this region are uncommon (flexor zone 5).
Some of the injuries in this region are self-inflicted and, for this
reason, the patient’s mental status should always
be carefully evaluated. As long as blood flow to the hand is adequate,
repair of nerve and tendon tissue in this region is urgent and not
emergent. Thus, initial care should focus on wound/tetanus status, skin
closure, medical care, and mental health status clearance. -
Joint. Patients with pain and a history of significant load (e.g., fall while rollerblading) whose x-ray are normal often have a real
ligament injury. The most common of these is injury to the
scapho-lunate ligament. Obtaining an x-ray with a “clenched fist” may
demonstrate separation of these bones not seen on standard films. Close
follow-up must be ensured. Early MRI might be valuable but should be
ordered by the specialist. This is particularly true in light of the
specialist’s ability to “see” the ligament tear when completing
fluoroscopic evaluation, whereas the same tear might not be visible in
the MRI exam and, thus, ordering the MRI would be cost-inefficient. -
Bone. Three bone injuries occur commonly.
-
Dorsal triquetrial avulsion fractures.
This may be the most common wrist fracture. Fortunately, treatment is
symptomatic and fractures which have not healed and remain painful can
be excised. -
Scaphoid fractures.
Many scaphoid fractures are hard to “see” initially. Some of these
fractures are actually serious ligament sprains. Regardless, all high-energy wrist injuries, without a clear diagnosis, should be
P.274P.275P.276
splinted and follow-up should be arranged with a physician in 10 to 14
days. Original x-rays should include four views of the scaphoid
(including a specific “scaphoid view” with the wrist in ulnar deviation
to elongate the view of the bone). Follow-up x-rays would be similar.
Continued pain without diagnosis might warrant an MRI.![]() Figure 19-6. A: When the digit is flexed, the deformity is quite apparent. B: Active finger flexion generates malrotation of ring finger with digital overlapping. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-6. A: When the digit is flexed, the deformity is quite apparent. B: Active finger flexion generates malrotation of ring finger with digital overlapping. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)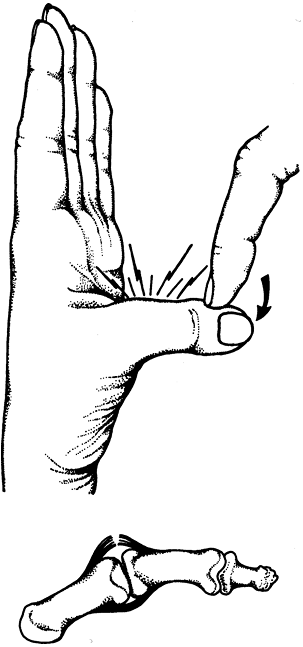 Figure 19-7. Rupture of ulnar collateral ligament of the metacarpophalangeal joint of the thumb. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-7. Rupture of ulnar collateral ligament of the metacarpophalangeal joint of the thumb. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.) -
Distal radius fractures.
Most of these fractures are obvious. During initial evaluation, the
function of the DRUJ and the median and ulnar nerve should be
evaluated. Initial-care focus is to splint the fracture with sufficient
alignment and stability so as to allow comfortable finger, elbow, and
shoulder motion. The original splint should immobilize the wrist and
the elbow with the forearm in neutral rotation and the wrist in neutral
flexion/extension. The splint should not block finger or thumb
flexion/extension. An ideal splint is the “sugar-tong” splint. This is
a dorsal and volar splint with opening at the side to allow for
swelling. Patients who cannot be pain stabilized so that home discharge
(prior to more definite care) can be accomplished may be developing
compartment syndrome or acute carpal tunnel syndrome. In either case,
emergent specialty consultation is needed.
-
-
Amputation.
Fortunately, traumatic amputation at this level is rare. Surprisingly,
results of replantation at this level are better than those seen at the
mid-palm or with multiple digits. The keys to successful management are-
Cooling (floating) the injured part in ice water. Do not place the part onto ice.
-
Antibiotics and tetanus administration
-
Systemic fluid balance
-
Transfer to a qualified specialist
-
-
-
Hand
-
Skin. Surface
burns from cold or heat exposure require tetanus and antibiotic
treatment. All blisters should be left intact. In addition to sterile
dressings, the hand should be splinted in a functional position. In the
case of frostbite, current guidelines recommend rapid rewarming.
Evolving guidelines involve antithrombolytic agents, especially for
frostbite. -
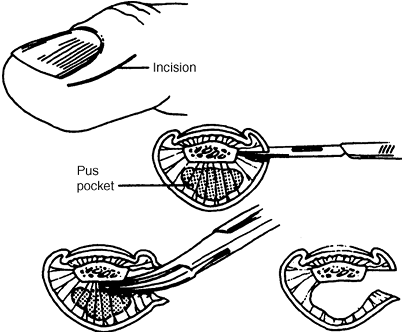
Nail plate and pulp.
Infections are common in the hand and fingernail. Do not confuse
herpetic whitlow and its vesicles with actual paronychia and associated
cellulitis. Drainage of a herpes infection can result in a
super-infection with bacteria. When herpes is suspected in an
individual in contact with others, the patient must be isolated until
the lesions have resolved. Bacterial infection in this region either is
around the nail or in the pulp tissues (felon). Felons are hardest to
treat. Fig. 19-8
depicts a felon. The need to drain the entire pulp is emphasized.
Noninfectious problems in this area include simple subungual hematomas
from trauma. Drainage of the hematoma through the nail plate usually
results in complete and immediate relief of the pressure pain. -
Tendon
-
Flexor.
Flexor tendon lacerations are surgical urgencies. Diagnosis should be
made based upon functional loss after a trauma. Some important injuries
(avulsion of the distal end of the flexor digitorum profundus) can
occur without a laceration. This may occur when a grasping hand is
suddenly pulled away from an object (jersey finger). Failure to make an
early diagnosis of a flexor tendon injury may preclude a good result. Thus,
after a finger/hand laceration or a sudden pull-away injury, the key
diagnostic step is an active motion exam at all joint levels and not
wound exploration. It is essential to test finger flexion with
the nonaffected fingers in full extension. Then test the affected
finger without further obstruction and with forced extension at the PIP
in order to isolate both the profundus tendons and the superficialis
tendon respectively. Once a flexor tendon laceration is diagnosed or
suspected, immediate referral to a hand specialist is recommended.
Almost never should a flexor repair be completed in the emergency
department. Almost always, a skin laceration
P.277
over or near a suspected tendon laceration should be closed before the patient is discharged from the emergency department.![]() Figure 19-8.
Figure 19-8.
Drainage of a felon using a midlateral incision. Complete division of
the vertical septae should be performed. (From Seiler JG III. Essentials of hand surgery, Lippincott William & Wilkins, Philadelphia, PA, 2002, with permission.) -
Extensor.
Extensor tendon lacerations must be urgently managed if they involve
the joint. Because of the close proximity of the MCPJ, PIPJ, and DIPJ
to the tendon, it is possible to contaminate the joint while only
partially disrupting the tendon’s function. Any laceration which may
have contaminated the joint deserves a tourniquet-controlled exam and
complete irrigation. Lacerations in the extensor region not involving
the joint do not always require direct repair. Occasionally,
an extensor repair can be completed in the emergency department.
Lacerations which can be seen to involve extensor tendon but which do
not alter active function (partial tendon lacerations) should be
cleaned and closed without placement of sutures into tendon. If a
definite (at least 10-degree) active extension loss distal to the
observed laceration is documented, consultation with a specialist
should be completed before discharge from the emergency department.
Almost always, a skin laceration over or near a suspected tendon
laceration should be closed before the patient is discharged from the
emergency department.
-
-
Nerve. Nerve
injuries in the distal arm region are common. Unless they are present
in conjunction with a devascularized arm, nerve injuries can be managed
on a delayed basis. The most common nerve injury by frequency is a
digital nerve laceration. When these occur, the ipsilateral digital
artery will often be damaged. In this situation, the volume of bleeding
is often the concern. Do not attempt to cauterize or “tie off” the bleeding vessel.
The close proximity of the artery to the nerve makes greater damage to
the nerve almost a certainty. Thus, in the case of a finger laceration
with bleeding uncontrolled by pressure and time, expert exploration of
the wound with proper lighting, instruments, and magnification is
appropriate. The keys to satisfactory outcome after nerve injury in the
finger are more related to not missing any associated flexor tendon
lacerations and not over-managing initial bleeding, thereby creating a
larger
P.278
nerve injury. Many digital nerve injuries are never repaired and yet the patient functions satisfactorily. -
Joint. An overlap between ligament and joint injuries in the fingers exists. The small size of the joints accounts for this fact. Fig. 19-9
depicts a common fracture pattern in the DIPJ of a finger. However, in
this injury, the fracture fragment is large enough so as to destabilize
the joint. This destabilization is obvious because a line drawn through
the diaphyses of one phalanx no longer bisects the adjacent phalanx. In
this example, the fragment must be reduced to achieve a congruent and
stable joint. A simple and universal rule is that the joint surface
must have equal space between the bony elements at any joint at any
location in both a true anteroposterior and lateral x-ray. If the
distance between bone elements is not equal, the joint is unstable. One
common exception to this statement does exist: This is the bony mallet
deformity. Such an injury is similar to Fig. 19-9
in that a portion of the distal phalanx is fractured. However, mallet
deformities (with or without a bony fragment) differ from Fig. 19-9
because they do not result in volar or dorsal migration of the
remainder of the phalanx. Initial treatment of all mallet deformities
is a neutral extension splint (Fig. 19-10). -
Bone. Overlap between bone and joint injuries is common as mentioned above. One further overlap is discussed below (fight bites in V.B). Four more common fracture conditions exist.
-
Boxer’s fracture. Fig. 19-11
depicts a common result of pugilistic activity. The fracture shown is
at the proximal margin of the metacarpal neck and is almost a
diaphyseal fracture. This is an important point. Because boxer’s
fractures occur in the neck (immediately proximal to the metacarpal
head/joint), significant flexion deformity can be accommodated. The
exception to this is in the rare cases when the digits involved are the
index or middle fingers (typically the small finger is affected). Thus,
open operative treatment is rarely indicated. There are two keys for
successful outcome when managing a boxer’s fracture:-
Do not overlook a puncture wound/open fracture.
-
Do not miss a rotational deformity. In
order to exclude rotational deformity, the finger must be gently flexed
at the MCPJ, and grip flexion posture must be examined and compared to
the adjacent digits. Figure 19-9. Bony mallet fracture with joint subluxation that will require reduction and stabilization. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-9. Bony mallet fracture with joint subluxation that will require reduction and stabilization. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)![]() Figure 19-10. A:
Figure 19-10. A:
Mechanism. Due to the extensor apparatus lesion, the distal phalanx
flexes by effect of the flexor profundus tendon. The proximal stump of
the distal conjoined extensor tendon retracts in a proximal direction
and consequently the lateral bands are slack initially and later
contract and displace dorsally. Due to the concentration of the
extension forces over the middle phalanx, the PIP joint is
progressively set in hyperextension. B:
Various splints (dorsal padded aluminum splint, volar padded aluminum
splint, concave aluminum splint). Dorsal padded aluminum splint allows
adjustable fixation of the DIP joint. (From Peimer CA. Surgery of the hand and upper extremity. New York: McGraw-Hill, 1996, with permission.)
-
-
Thumb base fracture and small finger base fracture.
Axial load applied to the border of the hand can result in
fracture-subluxation at the finger base. Any such fracture is unstable.
Almost all such fractures require operative stabilization. The key to
successful treatment is early recognition. When treated early, a closed
reduction and pinning is usually sufficient. Delay in treatment by as
little as 1 week can necessitate open reduction and a more complicated
management program. Thus, the first examiner’s job is diagnosis. In the
case of the thumb, it is easier to obtain a revealing x-ray. Along the
ulnar border of the hand, it is usually necessary to obtain several
oblique x-rays before a diagnosis can be made or excluded. -
Phalangeal fractures.
Fractures at the base or in the mid-shaft of the phalanx are tricky.
Many of these fractures have significant angular and/or rotational
differences. Oblique films in combination with standard anteroposterior
x-rays are often more helpful than lateral x-rays, which could be
confusing because of overlapping digits. Regardless, measurement of
rotational difference by clinical exam and shortening of the bony
length by x-ray exam are the key facts to be considered when planning
treatment. Unless, the fracture is essentially nondisplaced with zero rotational deformity, early referral to a hand specialist is warranted. -
Splint placement.
One of the common problems seen after initial hand fracture care by
specialist physicians is poor splint technique. The key to good splint
placement is maintaining fully lengthened ligaments. In the hand, this
is translated to 70 to 80 degrees of MCPJ flexion and no more than 10
degrees of PIPJ and DIPJ flexion. Such a splint is illustrated in Fig. 19-12. By maintaining fully lengthened ligaments, the physician reduces adjacent joint stiffness following fracture care.
P.279 -
-
Amputation.
Thankfully, amputations have become less common in conjunction with
enhanced product safety and public education. Nonetheless, they still
do occur. Single digits cut in flexor zone 2 should almost never be
replanted. A whole arm might be replanted but to do so is life
threatening. Guidelines for replantation include: Figure 19-11. A “boxer’s fracture” that can be treated with closed reduction and splinting in approximately 4 weeks. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)P.280
Figure 19-11. A “boxer’s fracture” that can be treated with closed reduction and splinting in approximately 4 weeks. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)P.280-
Almost any child (not tip injuries as these seem to reform naturally); adolescents are adults
-
Almost any thumb
-
Multiple digits
-
Whole hand
-
Digit in flexor zone 1 with clean bony injury
-
-
-
Injection injury. Fig. 19-13
depicts the mechanism of injection injury. This seemingly innocuous
original injury should not be overlooked. Failure to treat can result
in death and at least near loss of limb function. Even with emergent
care, the outcome of treatment is uncertain. Emergent care by a
specialist is mandatory. The keys to diagnosis are:-
Injury history. Use of a high pressure injector is often revealed.
-
Exam. One or several small puncture wounds with more proximal tenderness or swelling is evident.
-
Pain. The pain is seemingly greater than the wound would account for.
-
-
Fight bites.
This injury is often overlooked. Sometimes this will occur in
conjunction with a boxer’s fracture. The patient may not provide an
accurate history, and substance misuse in this situation is common.
Look for a small laceration
P.281
overlying
the joint which usually communicates to the joint if the finger is
brought into a fist position. Flexing the fist during laceration exam
is the key to identifying these patients. Treatment includes tetanus,
antibiotics, complete wound cleansing, placement of a wound drain, and
delayed closure.![]() Figure 19-12. Hand dressing: “safe” position of fingers. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-12. Hand dressing: “safe” position of fingers. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.) -
Compartment syndrome.
In addition to all the normal places, compartment syndrome can occur in
the hand. Tight fascial compartments surrounding the hand’s intrinsic
musculature can swell after injury and cause muscle ischemia. Diagnosis
is suspected when pain is increasing and passive motion is becoming
more difficult. Sensory change may not occur because of nerve anatomy
being outside of the pressurized area. Pressure monitoring and
occasional surgical release may be needed. -
Scaphoid fracture and scapho-lunate ligament tears.
Often, these are diagnoses of suspicion. Almost no patient has been
made worse by temporary splinting and early follow-up with a
specialist. Whenever a patient presents after a significant injury
mechanism (fall onto an outstretched arm), the patient should not be
discharged without follow-up even in the face of normal x-rays.
Appropriate follow-up does not require a specialist but does require a
care provider familiar with the nuances of significant wrist sprains
and scaphoid fractures mimicking a mild wrist contusion during the
first 4 to 12 weeks of recovery.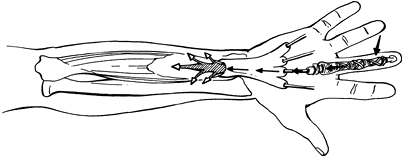 Figure 19-13. Palmar wounds at high pressure may spread into the proximal forearm. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)
Figure 19-13. Palmar wounds at high pressure may spread into the proximal forearm. (From Seiler JG III. Essentials of hand surgery, Lippincott Williams & Wilkins, Philadelphia, PA, 2002, with permission.)