Femoral Shaft Fractures
pediatric orthopaedic injury that most orthopaedists will treat
routinely and is the most common pediatric orthopaedic injury requiring
hospitalization.64,125
When subtrochanteric and supracondylar fractures are included, the
femoral shaft represents about 1.6% of all bony injuries in children.
Fractures are more common in boys (2.6:1), and occur in an interesting
bimodal distribution with a peak during the toddler years (usually from
simple falls) and then again in early adolescence (usually from
higher-energy injury).66,84,92,117
substantial short-term disability, these injuries can generally be
treated successfully with few long-term sequelae. For generations,
traction and casting were standard treatment for all femoral shaft
fractures in children, and femoral fractures ranked high in duration of
hospitalization for a single diagnosis.87 Over the past 20 years, however, there has been a dramatic and sustained trend towards
the operative stabilization of femoral shaft fractures in school-aged
children using flexible intramedullary nails, external fixation, locked
intramedullary nails, and more recently, submuscular plates. These
advances have decreased the substantial early disability for the
children, as well as the family’s burden of care during the recovery
period.
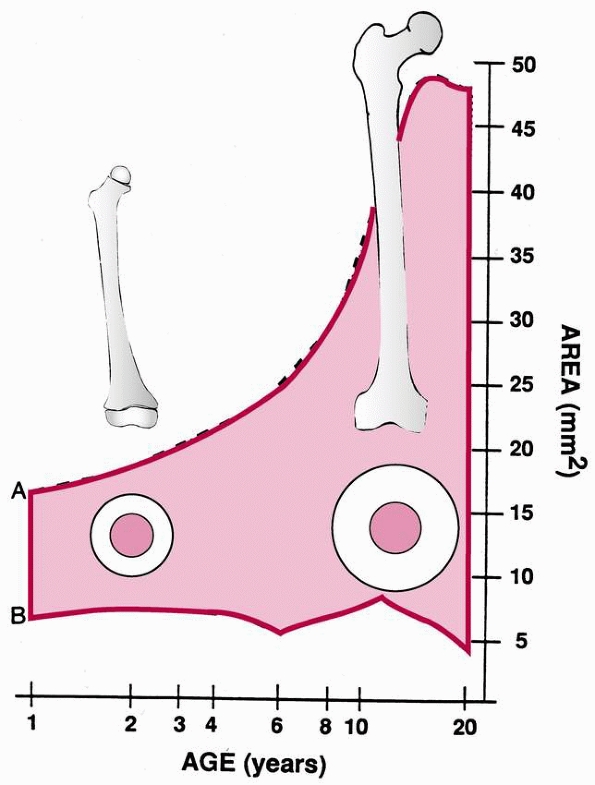
The increasing diameter and area of bone result in a markedly increased
area moment of inertia, leading to an increase in strength. This
progressive increase in bone strength helps explain the bimodal
distribution of femoral fractures. In early childhood, the femur is
relatively weak and breaks under load conditions reached in normal
play. In adolescence, high-velocity trauma is required to reach the
stresses necessary for fracture.
with the age of the child. Before walking age, up to 80% of femoral
fractures may be caused by abuse.10,18,74,183 In a study of over 5000 children at a trauma center, Coffey et al.39
found that abuse was the cause of only 1% of lower extremity fractures
in children older than 18 months, but 67% of lower extremity fractures
in children younger than 18 months.
 |
|
FIGURE 22-1
The shaded area represents cortical thickness by age group. This rapid increase in cortical thickness may contribute to the diminishing incidence of femoral fractures during late childhood. (From Netter FH. The Ciba collection of medical illustrations. Vol. 8. Musculoskeletal System. I. Anatomy, Physiology, and Metabolic Disorders. Summit, NJ: Ciba-Geigy, 1987, with permission.) |
greenstick fracture of the medial distal femoral metaphysis that occurs
when the parent falls on a child who is straddling the parent’s hip. It
is important to recognize this fracture because it occurs in infants at
an age when abuse is the leading cause of femoral fracture. The
fracture is caused by bending of the femur, which produces a
compression injury to the medial cortex. This injury is not consistent
with abuse and may confirm a parent’s description of a fall as the
cause.
fracture caused by abuse because their bone is sufficiently strong to
tolerate forceful blows and is able to resist torque without fracture.
In older children, femoral fractures are most likely to be caused by
high-energy injuries; motor vehicle accidents account for over 90% of
femoral fractures in this age-group.44,84,124
Pathologic femoral fractures are relatively rare in children, but may
occur because of generalized osteopenia in infants or young children
with osteogenesis imperfecta. Osteogenesis imperfecta should be
considered when a young child, with no history suggestive of abuse or
significant trauma, presents with a femoral shaft fracture.116
X-ray evaluation is often insufficient to diagnose osteogenesis
imperfecta; skin biopsy, collagen analysis, and bone biopsy may be
required to make a definitive diagnosis. Generalized osteopenia also
may accompany neurologic diseases, such as cerebral palsy or
myelomeningocele, leading to fracture with minor trauma in osteopenic
bone.66,111,116
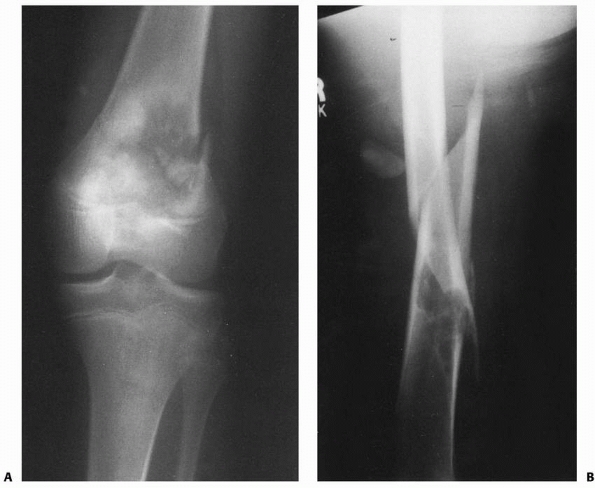
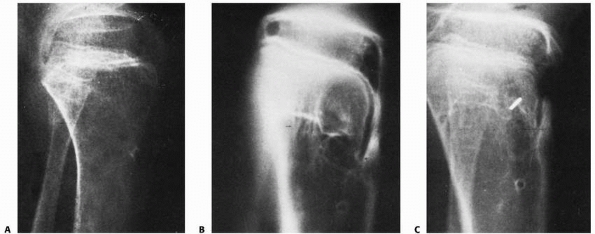
Pathologic fractures may occur in patients with neoplasms, most often
benign lesions such as nonossifying fibroma, aneurysmal bone cyst,
unicameral cyst, or eosinophilic granuloma. Although pathologic femoral
fractures are rare in children, it is essential that the orthopaedist
and radiologist study the initial injury films closely for the subtle
signs of primary lesions predisposing to fracture, particularly in
cases of low-energy injury from running or tripping. X-ray signs of a
pathologic fracture may include mixed lytic-blastic areas disrupting
trabecular architecture, a break in the cortex and periosteal reaction
in malignant lesions such as osteosarcoma, or better-defined sclerotic
borders with an intact cortex seen in benign lesions such as
nonossifying fibroma (Fig. 22-2).
In this era of high intensity, year-round youth sports, orthopaedists
are encountering more adolescents with femoral stress fractures from
running, soccer, and basketball.24
Although uncommon (4% of all stress fractures in children), femoral
shaft or femoral neck stress fractures should be considered in a child
with thigh pain because an unrecognized stress fracture may progress to
a displaced femoral fracture. A high index of suspicion is important,
because even nontraditional sports can lead to stress fractures with
extreme overuse; bilateral femoral stress fractures were reported in a
rollerblade enthusiast.199
swelling of the thigh, and obvious localized pain. The diagnosis is
more difficult in patients with multiple trauma or head injury and in
nonambulatory, severely disabled children. A physical examination
usually is sufficient to document the presence of a femoral fracture.
In patients lacking sensation (myelomeningocele), swelling and redness
may simulate infection.
 |
|
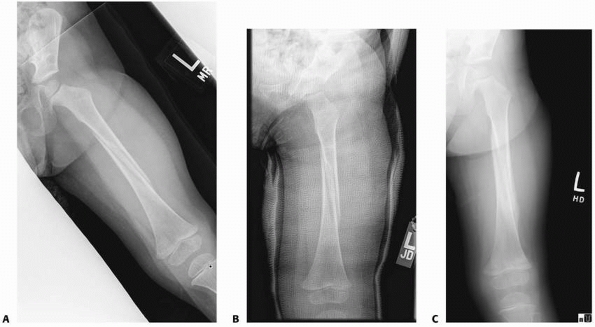
FIGURE 22-2 A. Femoral fracture through a poorly demarcated mixed, osteoblastic, osteolytic lesion—an osteosarcoma. B. Sclerotic borders of this lesion in the distal femur are typical of a pathologic fracture through a nonossifying fibroma.
|
rarely results from an isolated femoral fracture. The Waddell triad of
femoral fracture, intra-abdominal or intrathoracic injury, and head
injury are associated with high-velocity automobile injuries. Multiple
trauma may necessitate rapid stabilization of femoral shaft fractures124,165 to facilitate overall care. This is particularly true with head injury and vascular disruption.
Hematocrit levels below 30% rarely occur without multisystem injury. A
declining hematocrit should not be attributed to closed femoral
fracture until other sources of blood loss have been eliminated.37,127
including the hip and knee, because injury of the adjacent joints is
common. An anteroposterior (AP) pelvic x-ray is a valuable supplement
to standard femoral shaft views, because there may be an associated
intertrochanteric fracture of the hip, fracture of the femoral neck, or
physeal injuries of the proximal femur.13,31 Distal femoral fractures may be associated with physeal injury about the knee, knee ligament injury, meniscal tears,202 and tibial fractures.121
the diagnosis. In rare circumstances, bone scanning and magnetic
resonance imaging (MRI) may be helpful in the diagnosis of small buckle
fractures in limping children or stress fractures in athletes. The
orthopaedist should carefully evaluate x-rays for comminution or
nondisplaced “butterfly” fragments, second fractures, joint
dislocations, and pathologic fractures, as these findings can
substantially alter the treatment plan.
or short oblique; comminuted or noncomminuted; and open or closed. Open
fractures are classified according to Gustilo’s system.87
The presence or absence of vascular and neurologic injury is documented
and is part of the description of the fracture. The most common femoral
fracture in children (over 50%) is a simple transverse, closed,
noncomminuted injury.
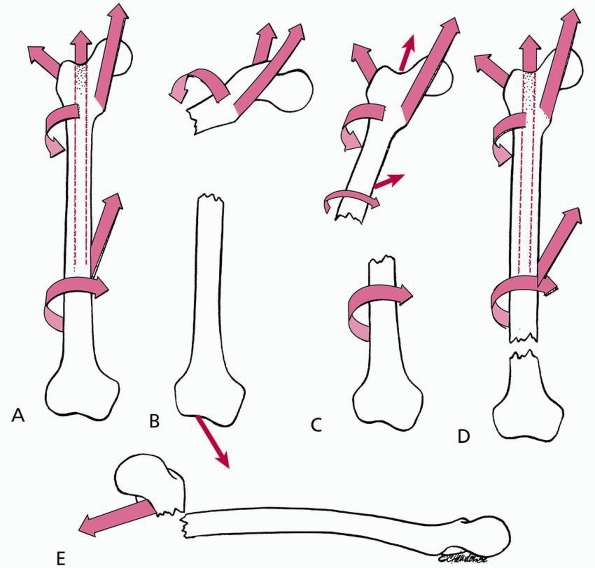
leads to characteristic displacement of the fragments based on the
attached muscles. With subtrochanteric fractures, the proximal fragment
lies in abduction, flexion, and external rotation. The pull of the
gastrocnemius on the distal fragment in a supracondylar fracture
produces an extension deformity (posterior angulation of the femoral
shaft), which may make the femur difficult to align.
 |
|
FIGURE 22-3 The relationship of fracture level and position of the proximal fragment. A. In the resting unfractured state, the position of the femur is relatively neutral because of balanced muscle pull. B.
In proximal shaft fractures, the proximal fragment assumes a position of flexion (iliopsoas), abduction (abductor muscle group), and lateral rotation (short external rotators). C. In midshaft fractures, the effect is less extreme because there is compensation by the adductors and extensor attachments on the proximal fragment. D. Distal shaft fractures produce little alteration in the proximal fragment position because most muscles are attached to the same fragment, providing balance. E. Supracondylar fractures often assume a position of hyperextension of the distal fragment due to the pull of the gastrocnemius. |
In addition to age, the orthopaedic surgeon should consider the child’s
weight, associated injuries, fracture pattern, and mechanism of injury.
Economic concerns, the family’s ability to care for a child in a spica
cast or external fixator, and the advantages and disadvantages of any
operative procedure also are important factors.
treatment of femoral shaft fractures have been evaluated by several
researchers, but no clear consensus has been reached, as charge data
are not always an accurate reflection of true costs to the patient, the
family unit, and the healthcare system. In a prospective comparative
study of 83 consecutive children and adolescents treated with either
traction and casting or titanium elastic nailing, Flynn et al.63 showed no significant difference in charges between the two methods. Newton and Mubarak154
analyzed the financial aspects of femoral shaft fracture treatment in
58 children and adolescents and determined that total charges were
lowest for those treated with early spica casting and highest for those
treated with skeletal traction or intramedullary nailing. Similarly,
Coyte et al.42 found the cost of
surgical treatment (external fixation) to exceed that of early spica
casting in all cases. Stans and Morrissy,193
in evaluating the cost of treating femoral fractures in children 6 to
16 years of age, found that all surgical treatments cost approximately
the same. Nork and Hoffinger157
showed that hospital profit was highest in the traction group, despite
charges being equivalent to the surgical group, because the actual
hospital resources required were significantly less. Wright,211
in an extensive review of the literature and meta-analysis, concluded
that immediate spica casting had a lower cost and lower malunion rate
than traction. Hedin et al.,82 in a
cost analysis comparing three methods of treating femoral shaft
fracture, found that the major determinant of cost was length of
hospital stay. Certainly, cost is a factor, but it should not be the
overriding consideration in discussions of treatment options with the
family. In addition to monetary cost to the medical system, the
treatment’s social cost to the family can vary significantly. This
social cost includes disruption of schedules, lost work, and time out
of school.
|
TABLE 22-1 Treatment Options for Isolated Femoral Shaft Fractures in Children and Adolescents
|
||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||
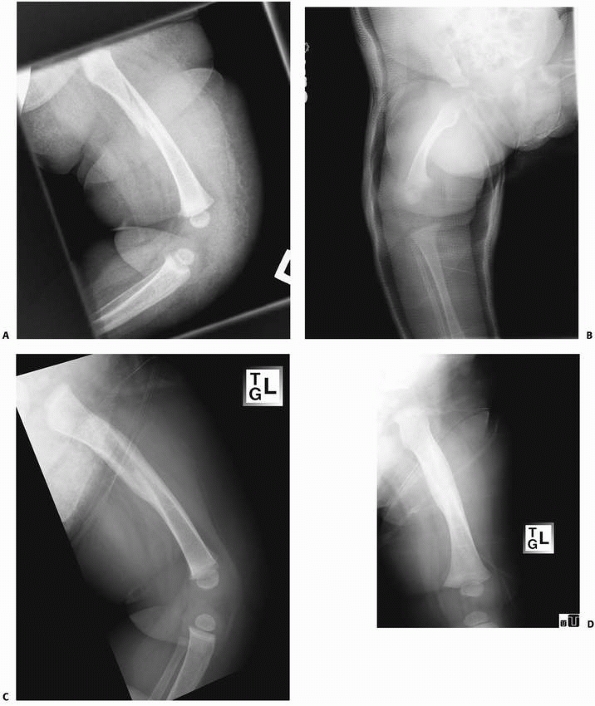
sustain stable femoral fractures. In fractures occurring in infancy,
management should include evaluation for underlying metabolic bone
abnormality or abuse. Once these have been ruled out, most infants with
a proximal or midshaft femoral fracture are comfortably and
successfully treated with simple splinting, with or without a Pavlik
harness. For the rare unstable fracture, the Pavlik harness may not
offer sufficient stabilization. Morris et al.150
reported a group of 8 birth-related femoral fractures in 55,296 live
births. Twin pregnancies, breech presentation, and prematurity were
associated with birth-related femoral fractures. The typical fracture
is a spiral fracture of the proximal femur with flexion of the proximal
fragment. With thick periosteum and remarkable remodeling potential,
newborns rarely need a formal reduction of their fracture or rigid
external immobilization.
For
femoral fractures with excessive shortening (>1 to 2 cm) or
angulation (>30 degrees), spica casting can be used. Traction rarely
is necessary in this age group.
Femoral fractures with more than 2 cm of initial shortening or marked
instability and fractures that cannot be reduced with early spica
casting require 3 to 10 days of skin or skeletal traction. In this age
group, skeletal stabilization by external fixation generally is
reserved for children with open fractures or multiple trauma.
Intramedullary fixation is used in children with metabolic bone disease
that predisposes to fracture or after multiple fractures, such as in
osteogenesis imperfecta, or following multitrauma. Flexible nailing can
be used in the normal-sized preschool child21 but is rarely necessary. Larger children (in whom reduction cannot be maintained with a spica cast) occasionally may
benefit from flexible intramedullary nailing, traction, or in rare cases, submuscular plating.
 |
|
FIGURE 22-4 A. This 7-month-old sustained a low-energy spiral femoral shaft fracture. B. Treatment was in a spica cast. C,D. Excellent healing with abundant callus at only 4 weeks after injury.
|
 |
|
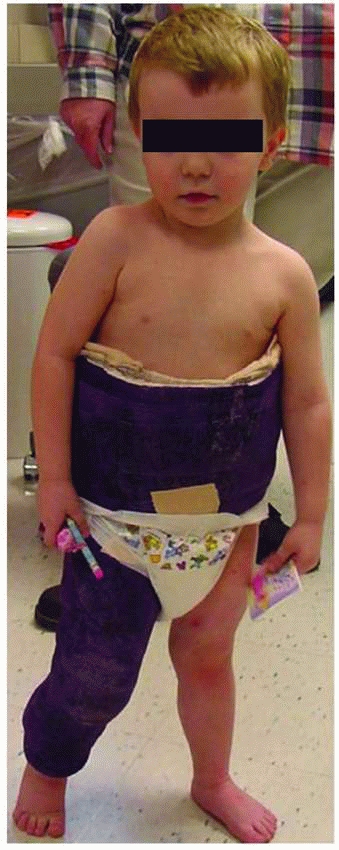
FIGURE 22-5 A. This 2-year-old sustained a low-energy spiral femoral shaft fracture, ideal for walking spica treatment. B. Immediately after reduction; note the lateral mold at the fracture site. C. Six weeks after injury, there is anatomic alignment, minimal shortening, and good callus formation.
|
 |
|
FIGURE 22-6 A 3-year-old standing in his walking spica cast (Courtesy of Howard Epps, MD.)
|
can be used successfully, depending on the fracture type, patient
characteristics, and surgeon skill and experience.64
For the rare, minimally displaced fracture, early spica casting usually
produces satisfactory results, although cast wedging or a cast change
may be necessary to avoid excessive shortening and angulation. In
children with unstable, comminuted fractures, traction may be necessary
before cast application. Although traction and casting is still a very
acceptable and successful method of managing femoral fractures in young
school-age children, the cost and the social problems related to
school-age children in casts has resulted in a strong trend towards
fracture fixation. Spica cast management is generally not used for
children with multiple trauma, head injury, vascular compromise,
floating knee injuries, significant skin problems, or multiple
fractures. Flexible intramedullary nails are the predominant treatment
for femoral fractures in 5 to 11 year olds, although submuscular
plating and external fixation have their place, especially in
length-unstable fractures or fractures in the proximal and distal third
of the femoral shaft.
to the increasing use of trochanteric entry, locked intramedullary
nailing for femoral fractures in the preadolescent and adolescent age
groups. Several studies designed to refine the indications for flexible
intramedullary nailing have concluded that although most results are
excellent or satisfactory in children older than 11, complications rise
significantly when this popular technique is used for bigger and older
children. In an international multicenter,
retrospective study, Moroz et al.149
found a statistically significant relationship between age and outcome,
with children older than 11 years or heavier than 49 kg faring worse.
Sink et al.185 found a much higher
rate of complications in length-unstable fractures. Fortunately,
surgeons can now select from several different trochanteric-entry nails
that allow a relatively safe, lateral entry point, with the stability
of proximal and distal locking. With this new information and
technology, locked intramedullary nailing is used commonly for obese
children ages 10 to 12 and most femoral shaft fractures in children
aged 13 to skeletal maturity.
 |
|
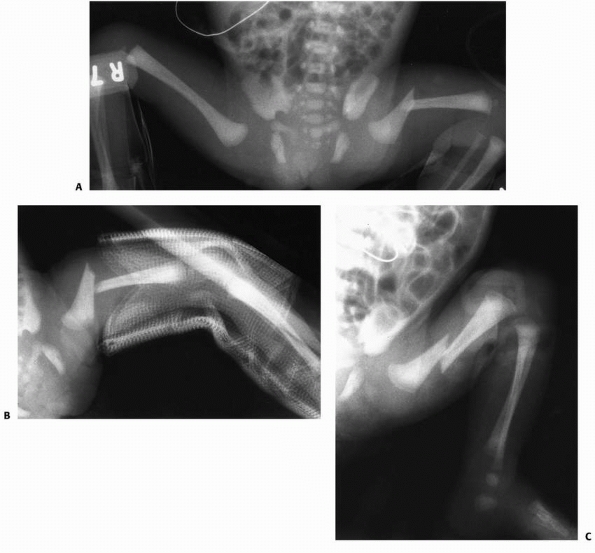
FIGURE 22-7 A. This infant had a birth-related left femoral fracture. B. An AP splint was used but ended at the fracture site, only increasing the angulation. C. A Pavlik harness reduced the fracture by flexing the distal fragment.
|
popularized the use of the Pavlik harness for femoral fractures in
infants. This treatment is ideal for a proximal or midshaft femoral
fracture that occurs as a birth-related injury. Reduction can be aided
by a wrap around the thigh if greater stability is needed. In a newborn
infant in whom a femoral fracture is noted in the intensive care unit
or nursery, the femur is immobilized with simple padding or a soft
splint. For a stable fracture, this approach may be sufficient and will
allow intravenous access to the feet if needed. The Pavlik harness can
be applied with the hip in moderate flexion and abduction. This often
helps align the distal fragment with the proximal fragment (Fig. 22-7). Evaluation of angulation in the coronal plane (varus-valgus) is difficult because of hyperflexion. Stannard et al.192 reported acceptable alignment in all patients with less than 1 cm of shortening. Morris et al.150
showed that all treatments, including traction, spica cast, and Pavlik
harness, are effective and resulted in satisfactory outcome in all
patients regardless of treatment.
harness and a small wrap around the thigh; immediate spica or traction
is reserved for the rare fracture that cannot be managed with simpler
means because of failure to align the fracture or excessive shortening
of more than 2 cm. Podeszwa et al.163
reported that infants treated with a Pavlik harness had higher pain
scores when compared to those treated with immediate spica casting;
however, none of the Pavlik patients had skin problems but one third of
the spica patients did. For this reason, some pediatric orthopaedists
prefer a single-leg Gore-tex (Gore,
Newark,
DE) spica cast, which protects the fracture site better than a Pavlik
harness and allows reasonably easy bathing and infant care.
is usually the best treatment option for isolated femoral shaft
fractures in children under 6 years of age, unless there is shortening
of more than 2 cm, massive swelling of the thigh, or an associated
injury that precludes cast treatment. The word “early” is used to imply
that the cast is placed in the first few days after injury, as opposed
to the word “immediate,” which implies that the cast is placed within
minutes of the patient’s presentation to the orthopaedist. Cassinelli
et al.35 reported on true
“immediate” spica cast application, with the cast being applied upon
arrival in the emergency department. Over an 8-year period, their group
treated 145 femoral fractures, all in children younger than 7 years of
age, with immediate spica cast application in the emergency department;
33% of the children were discharged from the emergency department (no
hospital admission). All children younger than 2 years of age and 86.5%
of children aged 2 to 5 years met acceptable alignment parameters on
final x-rays. Rereduction in the operating room was needed in 11
patients. The investigators concluded that initial shortening was the
only independent risk factor associated with lost reduction. They
concluded that if there was no associated factor requiring admission,
spica casting in the emergency department followed by immediate
discharge is safe, with a low complication rate in children younger
than 6 years of age, nearly eliminating the need for general anesthesia.
excellent safety profile, and a very high rate of good results, with
acceptable leg length equality, healing time, and motion.59,101 Hughes et al.95
evaluated 23 children ranging in age from 2 through 10 years who had
femoral fractures treated with early spica casting to determine the
impact of treatment on the patients and their families. The greatest
problems encountered by the family in caring for a child in a spica
cast were transportation, cast intolerance by the child, and hygiene.
Although most children did not attend school while in the cast, no
child was required to repeat a grade and no permanent psychologic
effects were reported by the parents. The researchers found that
overall treatment in a spica cast was much easier for families of
preschool children than for those with school-age children. In a
similar study, Kocher114 used a
validated questionnaire for assessing the impact of medical conditions
on families demonstrated that for the family having a child in a spica
cast is similar to having a child on renal dialysis. They found that
the impact was greatest for children older than 5 years and when both
parents are working. Such data should inform the decisions of
orthopaedic surgeons and families who are trying to choose among the
many options for young school-age children.
a series of 114 isolated femoral fractures in children under 6 years of
age, found that 90/90 spica casting was successful in 86% without cast
change or wedging, based on tolerance of shortening less than 1.5 cm
and angulation less than 10 degrees. Of the 20 patients requiring a
cast change, only 2 healed with unacceptable position (>2 cm of leg
length discrepancy). One of these overgrew by 1.5 cm, and the other was
lost to follow-up. Illgen et al.100
used an immediate spica regardless of initial shortening and placed the
child in traction only if unacceptable shortening occurred. Shortening
requiring spica cast change was associated with a knee flexion angle of
less than 50 degrees. Similar excellent results have been reported by
Czertak and Hennrikus43 using the 90/90 spica cast. Ferguson and Nicol59
conducted a prospective study of early spica casting in children less
than 10 years of age including 101 fractures in a 30-month period. Only
four spica casts had to be removed for unacceptable position. Age
greater than 7 years was a variable predictive of a higher risk of
failure of this technique to achieve satisfactory alignment.
described the telescope test in which patients were examined with
fluoroscopy at the time of reduction and casting. If more than 3 cm of
shortening could be demonstrated with gentle axial compression,
traction was used rather than immediate spica casting. By using the
telescope test, these researchers decreased unacceptable results
(>2.5 cm of shortening) from 18% to 5%. Martinez et al.131
reported excessive shortening and angular deformity in 26 of 51
patients after immediate spica casting, especially in comminuted
fractures. Although shortening and angulation can occur in a spica
cast, excessive deformity can be detected with weekly radiograph and
clinical evaluations during the first 2 to 3 weeks after injury.
Shortening is acceptable, but should not exceed 2 cm. This is best
measured on a lateral radiograph taken through the cast. If follow-up
radiographs reveal significant varus (>10 degrees) or anterior
angulation (>30 degrees), the cast may be wedged. However, Weiss et
al.209 noted that wedging of 90/90
spica casts can cause peroneal nerve palsy, especially during
correction of valgus angulation (a problem that rarely occurs). For
unacceptable position, the fracture can be manipulated and a new cast
applied, or the cast can be removed and the patient placed in traction
to regain or maintain length. Angular deformity of up to 15 degrees in
the coronal plane and up to 30 degrees in the sagittal plane may be
acceptable, depending on the patient’s age (Table 22-2). Finally, if shortening exceeds 2 cm, traction or an external fixator can be used (Fig. 22-8).
found that 50% (12 of 23) of closed femoral shaft fractures caused by
high-energy trauma in children under 10 years of age required repeat
reduction or other treatment to correct excessive shortening or
angulation that occurred after initial reduction; only 8% (2 of 24) of
low-energy fractures required repeat closed reduction. Wright211
showed that limb-length discrepancy and angular deformity were lower
with spica treatment than with traction treatment. The lower
cost of spica management is an added reason to pursue this method of management.
|
TABLE 22-2 Acceptable Angulation
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
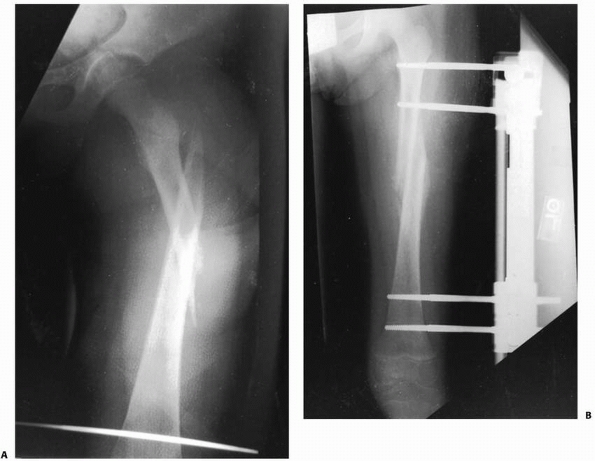
FIGURE 22-8 A. A proximal spiral femur fracture, which failed treatment with pins and plaster. B. Salvaged with an external fixator.
|
controversial. Some centers prefer a spica cast with the hip and knee
extended and the bottom of the foot cut out to prevent excessive
shortening.136 Varying the amounts
of hip and knee flexion in the spica cast based on the position of the
fracture also has been recommended: the more proximal the fracture, the
more flexed the hip should be.190
decades were taught to place children in the sitting position, with the
hips and knees set in about 90 degrees of flexion. Studies have shown
that the results from the sitting spica cast are good.135,145
The child is placed in a sitting position with the legs abducted about
30 degrees on either side. The synthetic material used for the cast
gives it sufficient strength so that no bar is required between the
legs. This not only allows the child to be carried on the parent’s hip
but also aids in toiletry needs, making bedpans unnecessary. Also, a
child who can sit upright during the day can attend school in a
wheelchair.
reported immediate single leg spica cast for pediatric femoral
diaphyseal fractures. In a series of 45 children, 90% pulled to stand
and 62% walked independently by the end of treatment; 50% of patients
were able to return to school or daycare while in the cast. Only two
children had unacceptable shortening, and two required repeat
reduction. Five children broke the cast at the hip joint. There was one
rotational malunion. The authors found that the single-leg technique
effectively treated the fracture and addressed some of the social
concerns of spica casting. Practitioners of the single-leg or walking
spica have learned to use the technique primarily on toddlers with very
stable, low-energy fractures. The cast must be extensively reinforced
at the hip. With the hip and knee much more extended, the single leg
spica not only improves function and ease of care, but also avoids a
technique that has been associated with compartment syndrome in several
children (see below).118,152
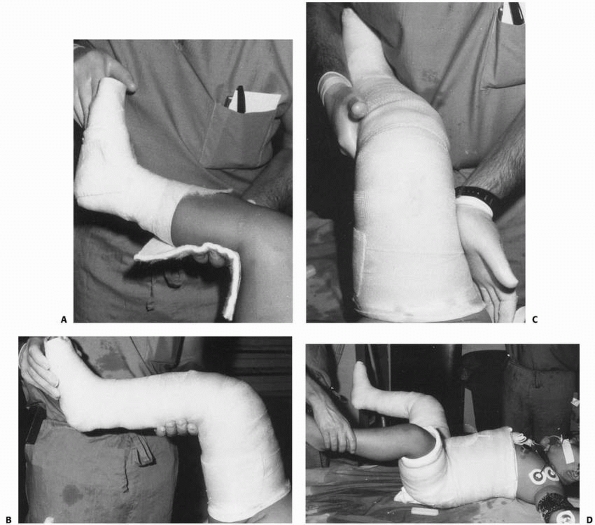
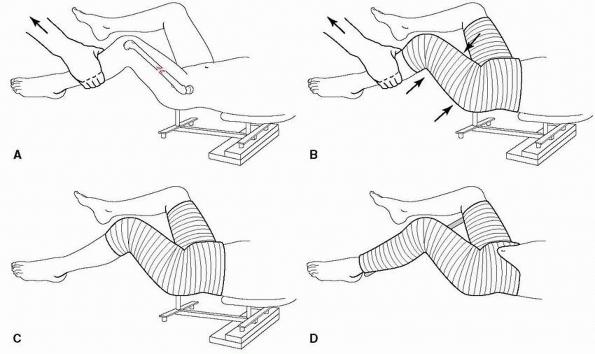
room or sedation unit. For the sitting spica cast technique, a long leg
cast is placed with the knee and ankle flexed at 90 degrees (Fig. 22-9A). Knee flexion of more than 60 degrees improved maintenance of length and reduction.100 However, if one applies excessive traction to maintain length (Fig. 22-10),
the risk of compartment syndrome is unacceptably high. Less traction,
less knee flexion, and accepting slightly more shortening is a
reasonable compromise. Extra padding, or a felt pad, is placed in the
area of the popliteal fossa. The knee should not be flexed after
padding because this may create vascular obstruction by producing a
lump of material in the popliteal fossa (Fig. 22-9B). Because most diaphyseal fractures tend to fall into varus angulation
while in a spica cast, a valgus mold is necessary (Fig. 22-9C).
The patient is then placed on a spica table, supporting the weight of
the legs with manual traction, and the remainder of the cast is applied
with the hips in 90 degrees of flexion and 30 degrees of abduction,
holding the fracture out to length (Fig. 22-9D).
It is mandatory to avoid excessive traction because compartment
syndromes and skin sloughs have been reported. The leg should be placed
in 15 degrees of external rotation to align the distal fragment with
the external rotation of the proximal fragment. After the spica cast is
in place, AP and lateral radiographs are obtained to ensure that length
and angular and rotational alignment are maintained. We observe all
patients for 24 hours after spica application to be sure that the child
is not at risk for neurovascular compromise or compartment syndrome.
Gore-tex liners can be used to decrease the skin problems of diaper
rash and superficial infection. Several centers have found that this
has been beneficial, justifying the cost of a Gore-tex liner.
 |
|
FIGURE 22-9 Application of a 90 degree/90 degree spica cast. A. A long leg cast is applied with the knee flexed 90 degrees. B.
Generous padding is applied over the foot, and a pad is placed on the popliteal fossa to prevent injury to the peroneal nerve and popliteal vessels. C. A mold is placed over the apex of the fracture, generally correcting a varus deformity into slight valgus. D. Using a standard spica table, a one and a half leg spica cast is applied with the hip flexed 90 degrees and abducted 30 degrees. |
long-leg cast is applied with approximately 50 degrees of knee flexion,
and when the remainder the cast is placed, the hip is flexed 45 degrees
and externally rotated 15 degrees. The hip should be reinforced
anteriorly with multiple layers of extra fiberglass. The pelvic band
should be fairly wide so that the hip is controlled as well as
possible. A substantial valgus mold is important to prevent varus
malangulation. Increasingly, we have been leaving the foot out,
stopping the distal end of the cast in the supramalleolar area, which
is protected with plenty of extra
padding.
Seven to 10 days after injury is the perfect window of time to wedge
the cast and correct small amounts of shortening and varus angulation
which commonly occur. Most toddlers pull to a stand and begin walking
in their walking cast about 2 to 3 weeks after injury.
 |
|
FIGURE 22-10
The dangers of pulling upward on the calf when applying a popliteal: this upward pull, which is used to reduce the fracture, can be dangerous, because it puts pressure on the gastrocnemius muscle and the other posterior leg structures, such as the popliteal artery and vein. (From Skaggs D, Flynn J.Trauma about the pelvis/hip/femur. Staying Out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins, 2006:105.) |
changed with manipulation in the operating room. Casts can be wedged
for less than 15 degrees of angulation. If shortening of more than 2 cm
is documented, the child should be treated with cast change, traction,
or conversion to external fixation, using lengthening techniques if the
shortening is not detected until the fracture callus has developed.
When conversion to external fixation is required, we recommend
osteoclasis (either closed or open if needed) at the time of the
application of the external fixator, with slow lengthening over a
period of several weeks (1 mm per day) to re-establish acceptable
length (see Fig. 22-8).
depending on the age of the child and the severity of the soft tissue
damage accompanying the fracture. Typically, an infant’s femoral shaft
fracture will heal in 3 to 4 weeks; and a toddler’s fracture will heal
in 6 weeks. After the cast hass been removed, parents are encouraged
allow their child to stand and walk whenever the child is comfortable;
most children will need to be carried or pushed in a stroller for a few
days until hip and knee stiffness gradually results. Most joint
stiffness resolves spontaneously in children after a few weeks. It is
unusual to need formal physical therapy. In fact, aggressive joint
range-of-motion exercises with the therapist immediately after cast
removal makes children anxious and may prolong rather then hasten
recovery. A few follow-up visits are recommended in the first year
after femoral fracture, analyzing gait, joint range of motion, and leg
lengths.
been used for management of femoral fractures. Vertical overhead
traction with the hip flexed 90 degrees and the knee straight was
introduced by Bryant in 1873,26,41 but this often resulted in vascular insufficiency155
and is now rarely used for treatment of femoral fractures. Modified
Bryant’s traction, in which the knee is flexed 45 degrees, increases
the safety of overhead skin traction.60
fracture is length unstable and the family and surgeon agree that
nonoperative measures are preferred. Rapid shortening in an early spica
cast can be salvaged with cast removal and subsequent traction. The
limit of skin traction is the interface between skin and tape or skin
and foam traction boot. Skin complications, such as slough and
blistering, usually occur when more than 5 pounds of traction is
applied. When more than 5 pounds of traction is required, or simply for
ease in patient management, skeletal traction can be used to maintain
alignment.5 Casas et al.34
studied a group of 41 patients between the ages of 4 and 10 years
treated with skin traction followed by spica casting. Spica casts were
applied at an average of 20.7 days. No leg-length difference or
deformity resulted. In this situation, hospital length of stay was not
thought to be a reason to reject this conservative yet clearly
effective method of management. Abandonment of traction and casting in
children younger than 10 years in many centers is in reaction to costs
and burden on the family, not because of poor outcomes.
comminuted proximal femoral shaft and intertrochanteric fractures where
secure fixation cannot be obtained without risk of vascular compromise
to the proximal femur. In general, however, skeletal traction then
spica casting is not recommended for children 12 years of age or older
because of significant incidences of shortening and angular malunion.
Also, knee ligament and meniscal injuries that sometimes accompany
femoral fractures may be aggravated by the chronic pull of traction
across the knee. The rare indication for a tibial traction pin is a
child in whom fracture configuration or skin problems prevent placement
of a femoral traction wire and in whom no knee injury is present.
the knee to the midthigh, the limb is draped in a sterile manner. The
knee is held in the position in which it will remain during traction;
that is, if 90/90 traction is being used, the traction pin should be
inserted with the knee bent 90 degrees. The patient should be sedated
and the wound treated with a local anesthetic, or general anesthesia
should be given before the traction pin is inserted. The location of
pin insertion is one finger breadth above the patella with the knee
extended or just above the flare of the distal femur. A small puncture
wound is made over the medial side of the femur. A medial-to-lateral
approach is used so that the traction pin does not migrate into the
area of the femoral artery that runs through Hunter’s canal on the
medial side of the femur. A traction pin between 3/32 inch and 3/16
inch is chosen depending on the size of the child. The pin is placed
parallel to the joint surface5 to help maintain alignment
while in traction. After the pin protrudes through the lateral cortex
of the femur, a small incision is made over the tip of the pin. The pin
is then driven far enough through the skin to allow fixation with a
traction bow. If 90/90 traction is used, a short leg cast is placed
with a ring through its midportion to support the leg. Alternatively, a
sling to support the calf can be used. If a sling is used, heel cord
stretching should be done while the patient is in traction.
 |
|
FIGURE 22-11
Tibial epiphyseal injury in association with tibial pin traction treatment for a femoral fracture. A 14-year-old boy sustained a femoral fracture that was treated by tibial skeletal traction. Two years later, the fracture was well healed but 2.5 cm short. A recurvatum deformity of the same side was apparent. A. An apparent fusion of the tibial tubercle. B. The bridge was confirmed by tomography. C. Bridge resection was performed with free fat interposition. A marker was placed to facilitate subsequent evaluation of growth. A tibial pin, if used, should be inserted posterior to the anterior aspect of the tibial tubercle. |
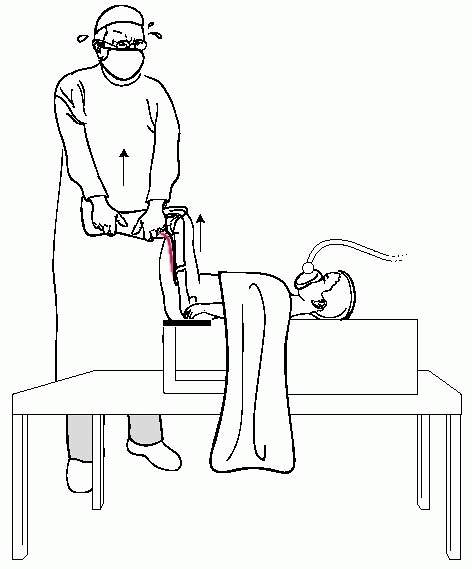
distal femur, traction is applied in a 90/90 position (the hip and knee
flexed 90 degrees) (Fig. 22-12) or in an
oblique position (the hip flexed 20 to 60 degrees). If the oblique
position is chosen, a Thomas splint or sling is necessary to support
the leg. The fracture may be allowed to begin healing in traction, and
radiographs should be obtained once or twice a week to monitor
alignment and length. In preschool-age children, traction will be
necessary for 2 to 3 weeks; in school-age children, a full 3 weeks of
traction usually are necessary before the fracture is stable enough to
permit casting. In a child under 10 years of age, the ideal fracture
position in traction should be less than 1 cm of shortening and slight
valgus alignment to counteract the tendency to angulate into varus in
the cast and the eventual overgrowth that may occur (average 0.9 cm).
If this method is used for adolescents (11 years or older), normal
length should be maintained.
 |
|
FIGURE 22-12 In 90/90 traction, a femoral pin is used and the lower leg and foot are supported with a short leg cast or a sling.
|
remove, are preferable to smooth pins because of their secure fixation
within the bone without side-to-side movement; however, they have a
slightly higher incidence of skin interface complications.
that obliquely placed femoral traction pins were associated with an
increased incidence of varus or valgus angulation. Pins for skeletal
traction should be placed parallel to the axis of the knee joint or the
articular surface, and in children over 11 years of age the fracture
should be reduced without shortening.
in a spica cast is well tolerated by young children. In older children,
maintaining the knee in 90 degrees of flexion for a prolonged period
may lead to knee stiffness and a difficult period of rehabilitation.97
72 children with femoral fractures were treated with early cast
brace/traction management. In this technique, a traction pin is placed
in the distal femur and then incorporated in a cast brace. The traction
pin is left long enough
to
be used for maintaining traction while the patient is in the cast brace
or traction is applied directly to the cast. The patient is allowed to
ambulate in the cast brace starting 3 days after application.
Radiographs are taken of the fracture in the cast brace to document
that excessive shortening is not occurring. The patient is then
returned to traction in the cast brace until satisfactory callus is
present to prevent shortening or angular deformity with weight bearing.
The technique was not effective in older adolescents with midshaft
fractures but achieved excellent results in children 5 to 12 years of
age. The average hospital stay was 17 days.
demonstrated unsatisfactory results in a small, yet significant,
percentage of patients treated with skeletal traction.90,97,113,170 Recently, increased attention has been focused on the risk of compartment syndrome in children treated in 90/90 spica cast.152 Mubarak et al.152
presented a multicenter series of 9 children with an average age of 3.5
years who developed compartment syndrome of the leg after treatment of
a low-energy femoral fracture in a 90/90 spica cast. These children had
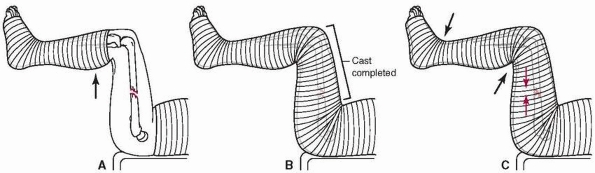
extensive muscle damage and the skin loss around the ankle (Fig 22-13).
The authors emphasized the risk in placing an initial below-knee cast,
then using that cast to apply traction while immobilizing the child in
the 90/90 position. The authors recommended avoiding traction on a
short leg cast, leaving the foot out, and using less hip and knee
flexion (Fig 22-14).
fractures, a dominant technique in Europe since the 1970s, has been
rapidly adopted throughout North America as the most popular method of
fixation for midshaft femoral fractures in children between the ages of
5 and 11 years. The flexible intramedullary nailing technique can be
done with either stainless steel nails169 or titanium elastic nails.
result of safety and efficacy. Safety and complications were a concern
with two methods of rigid fixation: solid antegrade nailing
(osteonecrosis) and external fixation (pin site infection, refracture
after external fixator removal). The flexible nailing technique offered
satisfactory fixation, enough stress at the fracture site to allow
abundant callus formation, and relatively easy insertion and removal.
The implants are inexpensive and the technique has a short learning
curve. The primary limitation of flexible nailing is the lack of rigid
fixation. Length-unstable fractures can shorten and angulate,
especially in older and heavier children. Compared to children with
rigid fixation, children who have their femoral fracture treated with
flexible nailing clearly have more pain and muscle spasm in the early
postoperative period. The surgeon should take this into consideration
in planning the early rehabilitation.
 |
|
FIGURE 22-13 Application of the 90/90 spica and pathogenesis of the resulting problem. A. Below-knee cast is applied with the patient is on the spica frame. B.
Next, traction is applied to the below-knee cast to produce distraction at the fracture site. The remainder of the cast is applied, fixing the relative distance between the leg and the torso. C. After the child awakens from general anesthesia, there is a shortening of the femur from muscular contraction which causes the thigh and leg to slip somewhat back into the spica. This causes pressure to occur at the corners of cast (arrows, e, proximal posterior calf and anterior ankle). (From Mubarak SJ, Frick S, Rathjen K, et al. Volkmann contracture and compartment syndromes after femur fractures in children treated with 90/90 spica casts. J Pediatr Orthop 2006;26(5):570.) |
popular, there have been many studies to refine the technique and
indications and to elucidate the inherent limitations of fixation with
flexible implants. Mechanical testing of femoral fracture fixation
systems showed that the greatest rigidity is provided by an external
fixation device and the least by flexible intramedullary rodding.120
Stainless steel rods are stiffer than titanium in bending tests. A
study comparing steel to titanium flexible nails found a higher
complication rate in the titanium group.206 They reported that a typical 3.5-mm stainless steel nail has the same strength as a 4.0-mm titanium nail. Lee et al.120
analyzed a group of synthetic fractured femurs instrumented with Enders
rods and determined that there was sufficient axial and torsional
stiffness to allow “touch down weight-bearing” despite fracture type.
Gwyn et al.76 similarly showed that
4-mm titanium rods imparted satisfactory torsional stability regardless
of fracture pattern. Recognizing this flexibility, the French pioneers119,123
of elastic nailing stressed the critical importance of proper implant
technique, including prebending the nails so that the apex of the bend
was at the fracture site, and so that the two implants balance one
another to prevent bending and control rotation. Frick et al.65
found greater stiffness and resistance to torsional deformation when
retrograde nails were contoured into a double C pattern than with the
antegrade C and S configuration.
 |
|
FIGURE 22-14 Authors’ recommended technique of spica cast application. A.
The patient is placed on a child’s fracture table. The leg is held in about 45-degree angle of flexion at the hip and knee with traction applied to the proximal calf. B. The one and a half leg spica cast is then applied down to the proximal calf. Molding of the thigh is accomplished during this phase. C. The x-rays of the femur are obtained and any wedging of the cast that is necessary can occur at this point in time. D. The leg portion of the cast and the cross bar are applied. The belly portion of the spica is trimmed to the umbilicus. (From Mubarak SJ, Frick S, Rathjen K, et al. Volkmann contracture and compartment syndromes after femur fractures in children treated with 90/90 spica casts. J Pediatr Orthop 2006;26(5):571.) |
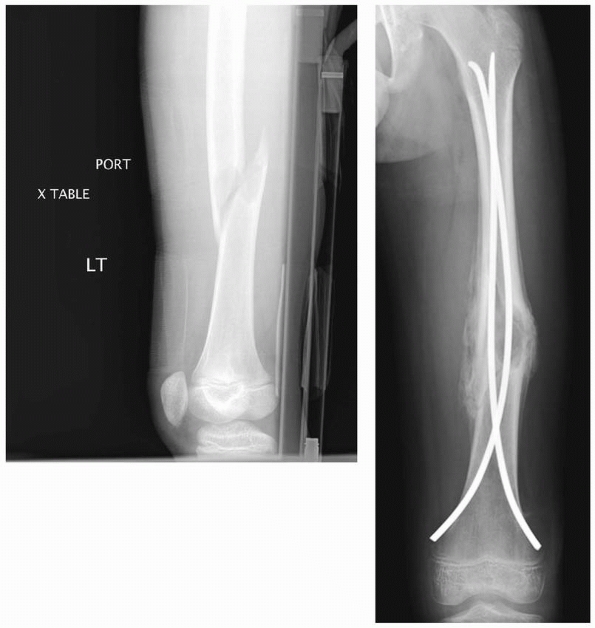
most centers throughout the world has been retrograde, with small
medial and lateral incisions just above the distal femoral physis;
however, some prefer an antegrade technique, with entry in the
subtrochanteric area. The primary advantages of a proximal insertion
site are a fewer knee symptoms postoperatively. Bourdela22
compared retrograde and antegrade (ascending and descending) flexible
intramedullary rodding in a group of 73 femoral fractures. Sixty one
fractures were treated with antegrade nails and 12 with retrograde
nails. All children with antegrade nailing had good clinical and x-ray
results; all 12 children with retrograde nails had knee pain that
impaired knee motion until the nails were removed. An antegrade
transtrochanteric approach was recommended by Carey and Galpin,32
who reported excellent results in 25 patients without growth arrest of
the upper femur and no osteonecrosis. Satisfactory alignment and
fracture healing were obtained in all patients.
recommended a 3.5-mm Ender nail in children 6 to 10 years of age and a
4.0-mm nail in children over 10 years of age. Ligier et al.123 used titanium nails ranging from 3 to 4 mm inserted primarily in a retrograde fashion. Heinrich et al.91
recommended flexible intramedullary nails for fixation of diaphyseal
femoral fractures in children with multiple system injury, head injury,
spasticity, or multiple long bone fractures. Flynn et al.62
published the first North American experience with titanium elastic
nails in 2001. In this multicenter study, 57 of 58 patients had an
excellent or satisfactory result and there was no loss of rotational
alignment, but 4 patients healed with an angular malunion of more than
10 degrees. Narayanan et al.153
looked at one center’s learning curve with titanium elastic nails,
studying the complications of 79 patients over a 5-year period. Nails
that were bent excessively away from the bone led to irritation at the
insertion site in 41. The center also had eight malunions and two
refractures. They noted that complications could be diminished by using
rods with similar diameter and contour and by avoiding bending the
distal end of the nail way from the bone. Luhmann et al.126
reported 21 complications in 43 patients with titanium elastic nails.
Most of the problems were minor, but a hypertrophic nonunion and a
septic joint occurred in their cohort. They suggested that problems
could be minimized by using the largest nail possible and leaving only
2.5 cm out of the femoral cortex.
centers; however, some surgeons choose to leave the implants
permanently. There is a theoretical concern that if flexible nails are
left in young children, they will come to lie in the distal diaphysis
as the child grows older. This may create a stress riser in the distal
diaphysis, leading to a theoretical risk of fracture (Fig. 22-15). Morshed et al.151 performed a retrospective analysis of
24 children treated with titanium elastic nails and followed for an
average of 3.6 years. The original plan with these children was to
retain their implants, but about 25% of the children had their nails
removed because of persistent discomfort.
 |
|
FIGURE 22-15 A.
A few years after titanium lasting nailing, the nails have migrated proximally with growth, creating a stress riser and the subsequent insufficiency fracture. B. The refracture was treated with removal of the old nails and replacement with longer implants. |
a child between the ages of 5 and 11 years with a length-stable femoral
fracture in the mid-80% of the diaphysis (Fig. 22-16), who has a body weight less than 50 kg.149
Unstable fracture patterns can also be treated with flexible nailing,
but the risk of shortening and angular malunion is greater,185 and supplemental immobilization during the early healing phase may be valuable.
lines that propagate proximally and distally and might be otherwise
unnoticed (Fig. 22-17). Although it is
technically difficult to obtain satisfactory fixation with a retrograde
technique when the fracture is near the distal metaphysis, a 2006
biomechanical study140 demonstrated
that retrograde insertion provides better stability than antegrade
insertion for distal femoral shaft fractures. Nail size is determined
by measuring the minimal diameter of the diaphysis, then multiplying by
0.4 to get nail diameter. For instance, if the minimal diameter of the
diaphyseal canal is 1.0 cm, 4-mm nails are used. The largest possible
nail size that permits two nails to fit into the medullary canal should
be chosen.
table, with a fracture reduced to near anatomic position before
incisions are made. Alternatively, a fluoroscopic table can be used,
but the surgeon should assure that a reduction can be obtained before
the start of the procedure, and extra assistance may be necessary.
but other devices are available and can be used with slight variations
in procedure.
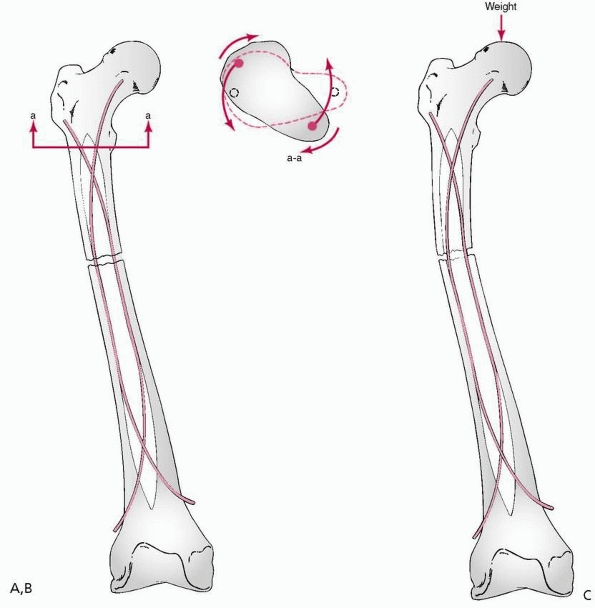
level of the fracture site is measured, and a gentle 30-degree bend is
placed
in the nail. The technique of elastic fixation of femoral fractures as described by Ligier et al.123 requires that a bend be placed in the midportion of the rod at the level of the fracture site. This produces a spring effect (Fig. 22-18)
that adds to the rigidity of the fracture fixation. The spread of the
rods in opposite directions provides a “prestressed” fixation that
increases resistance to bending. The opposite bends of the two rods at
the level of the fracture significantly increase resistance to varus
and valgus stress, as well as torsion. A second bend is sometimes
helpful near the entering tip of the nail to facilitate clearance of
the opposite cortex during initial insertion.
 |
|
FIGURE 22-16 Titanium elastic nailing of a midshaft femur fractures through a benign lytic defect.
|
Two nails of similar size should be used, and they should be as large
as possible. Using nails that are too small or mismatched in size
increases the rate of complications.153 It is very unusual to use nails smaller than 3.5 mm, except in the very youngest, smallest children.
is prepared and draped with the thigh (hip to knee) exposed. The image
intensifier is used to localize the placement of skin incisions by
viewing the distal femur in the AP and lateral planes. Incisions are
made on the medial and lateral sides distal to the insertion site in
the bone. The proximal end of the 2- to 3-cm incision should be at or
just distal to the level of the insertion site, which is about 2.5 to 3
cm proximal to the distal femoral physis (Fig. 22-19).
A 4.5-mm drill bit or awl is used to make a hole in the cortex of the
bone. The distal femoral metaphysis is opened 2.5 cm proximal to the
distal femoral physis using a drill or awl. The drill is then steeply
angled in the frontal plane to facilitate passage of the nail through
the dense metaphyseal bone.
driven up to the level of the fracture. Upon insertion, the rod glances
off the cortex as it advances toward the fracture site. Both medial and
lateral rods are inserted to the level of the fracture. At this point,
the fracture is reduced using longitudinal traction and a fracture
reduction tool. This tool is radiolucent and holds the unstable femoral
fracture in the appropriate position to allow fixation. The surgeon
should select the nail that is most difficult to pass, and pass this
one first. If the easier nail is passed first, it may stabilize the two
fragments such that the second, more difficult nail cannot be passed
easily. The two nails then are driven into the proximal end of the
femur, with one driven toward the femoral neck and the other toward the
greater trochanter. When passing the second nail across the fracture
site and rotating it, care must be taken not to wind one rod around the
other. After the nails are driven across the fracture and before they
are seated, fluoroscopy is used to confirm satisfactory reduction of
the fracture and to ensure that the nails did not comminute the
fracture as they were driven into the proximal fragment.
of each nail is cut and driven back securely into the femur. The end of
the nail should lie adjacent to the bone of the distal femoral
metaphysis, exposed just enough to allow easy removal once the fracture
is healed. The exposed to distal tip of the nail should not be bent
away from the femoral metaphysis because this will irritate surrounding
tissues.
 |
|
FIGURE 22-17 A. This high-energy, midshaft femur fracture was treated with titanium nails. B.
A large butterfly fragment was dislodged during nail insertion. Because the fracture is now length-unstable, the surgeon wisely chose to protect the child for a few weeks in a one leg spica cast. C. The fracture healed and excellent alignment. Note how the nails have wound around each other. This can make nail removal more difficult. |
site through the lateral border of the trochanter avoids creating the
stress riser that results from subtrochanteric entry.
emphasized that for insertion of titanium elastic nails, the nails have
to be bent into an even curve over the entire length, and the summit of
the curve must be at the level
of
the fracture or very close to it in comminuted fractures. The depth of
curvature should be about three times the diameter of the femoral
canal. Flynn et al.62
also stressed the importance of contouring both nails with similar
gentle curvatures, choosing nails that are 40% of the narrowest
diaphyseal diameter, and using medial and lateral starting points that
are at the same level in the metaphysis.
 |
|
FIGURE 22-18 A. Stability from flexible rods comes from proper technique. B. Torsional stability results from divergence of the rods in the metaphysis. C.
Resistance to sagittal and coronal bending results from spreading of the prebent rods through the diaphysis, as well as the size and material properties of the rods. Elastic rods return to their predetermined alignment when loaded unless plastic deformation occurs. |
 |
|
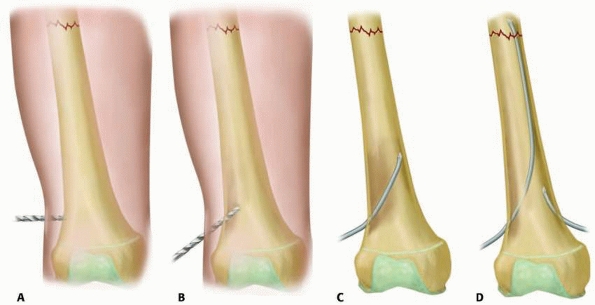
FIGURE 22-19 A.
Once the incision has been made, the entry point for the nail is identified 2 cm superior to the growth plate at the midpoint of the femur anteroposteriorly. A 4.5-mm drill bit is used to make the starting point. B. Once the cortex has been entered the drill is angled obliquely to fashion a tract. C. The first nail is inserted until it reaches the fracture line. D. Once the first nail has reached the fracture line, the second nail is inserted in the same fashion. |
postoperative course to decrease knee pain and quadriceps spasm. When
the flexible nailing technique is used for length-unstable fractures, a
walking (or one leg) spica is recommended, generally for about 4 to 6
weeks until callus is visible on x-rays. For length-stable fractures,
touchdown weight bearing can begin as soon as the patient is
comfortable. Gentle knee exercises and quadriceps strengthening can be
begun, but there should be no aggressivepassive motion of the knee,
which increases the motion at the fracture site and increases
quadriceps spasm. Postoperative knee motion does return to normal, but
this requires time. Full weight bearing generally is tolerated by 6
weeks. Ozdemir et al.162 recommended
the use of postoperative functional bracing, demonstrating its
effectiveness in a group of patients treated with elastic rodding. Such
postoperative support may occasionally be required, but in most cases
it appears not to be needed.
one nonunion, one infection, and no occurrence of osteonecrosis were
reported. Approximately 12% of patients had malunions, most often mild
varus deformities, and approximately 3% had clinically significant
leg-length discrepancies from either overgrowth or shortening. A 2007
study noted overgrowth of more than 1 cm in 8.2% of preschool children
treated with titanium elastic nailing.21
This is a much higher rate of overgrowth than seen in older children,
suggesting the technique should be used infrequently in preschool
children. Mazda et al.134 pointed
out a technique-related complication that occurred in 10 of their 34
patients: rods were left too long and caused painful bursae and limited
knee flexion. All 10 patients had the nails removed 2 to 5 months after
surgery. Flexible nails inserted in a retrograde fashion may also
penetrate into the knee joint, causing an acute synovitis.175 In a multicenter study62
that included 58 femoral fractures stabilized with titanium elastic
nails, irritation of the soft tissue near the knee by the nail tip
occurred in 4 patients (7%), leading to a deeper infection in 2
patients. This study also reported one refracture after premature nail
removal, leading to a recommendation that nail removal be delayed until
callus is solid around all cortices and the fracture line is no longer
visible. Ozdemir et al.162 measured
overgrowth with a scanogram and found that the average increase in
length was 1.8 mm, suggesting that significant femoral overgrowth is
not seen with this method of treatment.
compared traction and spica casting with titanium elastic nails for
treatment of femoral fractures in 83 consecutive school-aged children.
The three unsatisfactory results were treated with traction followed by
casting. The overall complication rate was 34% in the traction group
and 21% in the elastic nail group.
that predict a higher rate of complications after flexible nailing of
pediatric femoral shaft fractures.149
Analyzing 234 fractures in 229 patients from six different Level 1
trauma centers, the authors found significantly more problems in older,
heavier children. A poor outcome was 5 times more likely in patients
who weighed more than 108.5 pounds. A poor outcome was also almost four
times more likely in patients older than 11 years old. The authors
concluded that results were generally excellent for titanium elastic
nailing, but poor results were more likely in children older than 11
and heavier than 50 kg. Ho et al.93
reported a 34% complication rate in patients 10 years old and older,
but only a 9% complication rate in patients younger than 10 years,
emphasizing the concept that complications of flexible nailing are
higher in older, heavier children.
efficient, convenient method to align and stabilize the fractured
pediatric femur. It is the method of choice when severe soft tissue
injury is present, and may be considered in any patient where
traditional closed methods of management are not appropriate.116
In head-injured or multiply-injured patients and those with open
fractures, external fixation offers an excellent method of rapid
fracture stabilization. It is also valuable for very proximal or distal
fractures, where options for flexible nailing, plating, or casting are
limited. External fixation is particularly valuable for benign
pathologic fractures (e.g., through a nonossifying fibroma) at the
distal metaphyseal-diaphyseal junction (Fig. 22-20), where the fracture will heal rapidly, but minimal angular malunion can be tolerated.
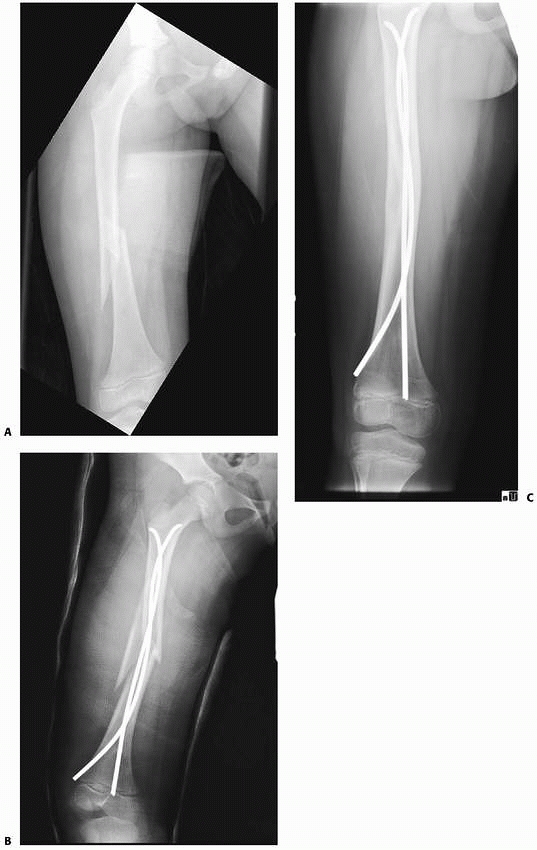
reported their early experience with 44 femoral fractures treated with
primary external fixation and early weight bearing. Most patients
returned to school by 4 weeks after fracture and had full knee motion
by 6 weeks after the fixator was removed. In this early study, end-on
alignment was the goal and overgrowth was minimal. More recently,
Matzkin et al.133 reported a series
of 40 pediatric femoral fractures treated with external fixation; 72%
of the fixators were dynamized before removal, and their refracture
rate was only 2.5%. They had no overgrowth, but one patient ended up 5
cm short.
devices, the 1990s saw waning interest in their use because of
complications with pin track infections, pin site scarring, delayed
union, and refracture. These complications, coupled with the very low
complication rate from flexible nailing, led to a decline of external
fixation for pediatric femoral shaft fractures. Data from comparison
studies also contributed to the change. Bar-On et al.9
compared external fixation with flexible intramedullary rodding in a
prospective randomized study. They found that the early postoperative
course was similar but that the time to return to school and to resume
full activity was less with intramedullary fixation. Muscle strength
was better in the flexible intramedullary fixation group at 14 months
after fracture. Parental satisfaction was also significantly better in
the flexible intramedullary rodding group. Bar-On et al.9 recommended that external fixation be reserved for open or severely comminuted fractures.
 |
|
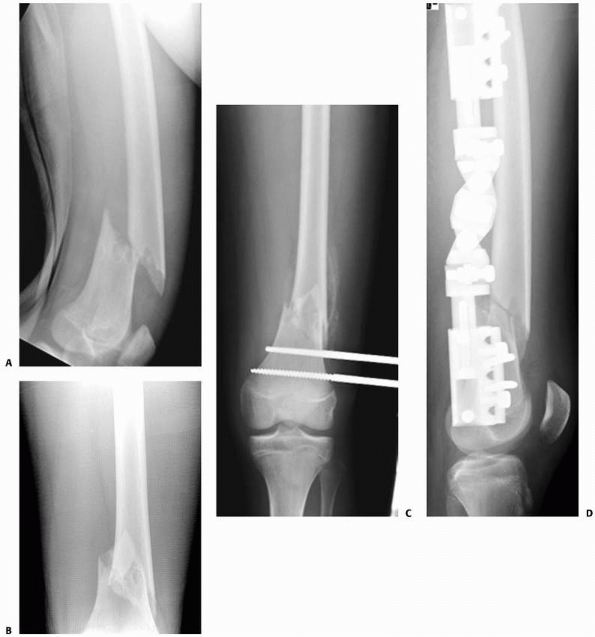
FIGURE 22-20 AP (A) and lateral (B)
x-rays a low-energy short oblique fracture through a fibrous cortical defect in the distal femur; this type of fracture is not unusual. The surgeon judged that there was enough distance between the fracture site and the growth plate to allow external fixation. AP (C) and lateral (D) x-rays 3 weeks after external fixation shows early callus and good alignment. The external fixation was removed shortly after this x-ray and the child was placed in a long leg cast, with weight bearing as tolerated. |
ever, indicated for femoral fractures in young children. One of two
types of monolateral devices are typically used. The AO system, in
which pins can be placed at any point along a bar, with a special clamp
holding the pins at a variable angle to the bar has been used at many
centers. The advantage of this system is that the stability of fixation
is increased if the two pins on each side of the fracture are spread
widely, with one pin close to the fracture and one quite distant from
it. A second longitudinal rod can be added to this system to increase
its rigidity. A second type of external fixation system has pin clamps
at the end of a telescopic tube. The pin clamps provide easy
application, but the stability of the fixation device is decreased
because the pins are widely separated from the fracture. The pin clamps
may be constrained to rotation only (Wagner) or attached with a
universal joint to the barrel of the device (Orthofix, EBI) (Fig. 22-21).
The telescoping barrel provides lengthening or “dynamization,” and the
universal joints provide adjustment. Dynamization refers to the amount
of longitudinal motion allowed by a given frame or construct. A
fracture can be dynamized before frame removal to increase strength of
healing callus. Different external fixation devices allow for varying
amounts of dynamization. Excessive rigidity is thought to relate to
poor bone healing and strength. For this reason, many pediatric trauma
experts purposely build a less stable frame to increase the forces on
the fracture site. Pins are more closely clustered and placed farther
from the fracture site, and the frame itself is placed more laterally
away
from the femur. Domb et al.52
compared static to dynamic external fixation in pediatric femoral
fractures. Average time to early callus formation was similar, and the
average time to complete healing was 70.1 days in the dynamic group and
63.1 days in the static group. The assumption that less rigid frames
decrease fracture healing remains unproven. The problem may be that
smaller, lighter children simply do not place enough force across the
dynamized fracture to stimulate callus production.
 |
|
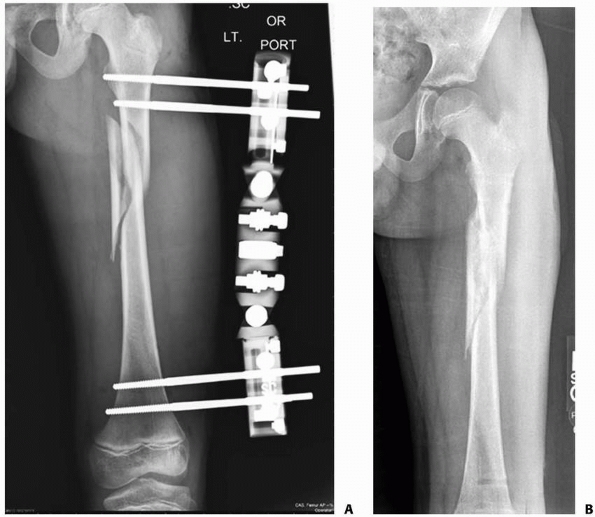
FIGURE 22-21 A.
This proximal spiral femur fracture was deemed length-unstable and a poor candidate for titanium elastic nails. The surgeon chose an external fixator, rather than a plate. B. Eight weeks after injury, the fracture is healing in excellent alignment and there is good early callus. Fixator removal is easier than plate removal. |
device can be applied make it ideal for management of a polytrauma
victim who cannot tolerate extended anesthesia. Nowotarski et al.,158
in a review of 1507 femoral fractures at a trauma center, found 59 (4%)
that were managed with urgent external fixation followed by
intramedullary rodding. The average time to rodding was 7 days, and the
infection rate was 1.7% (1 patient). They concluded that emergent
external fixation followed by early intramedullary rodding was safe.
studied carefully for comminution or fracture lines that propagate
proximally or distally. The surgeon should assure that the fixator
devices available are long enough to span the distance between the
optimal proximal and distal pin insertion sites.
table or radiolucent table can be used, although a fracture table is
much more efficient because an anatomic reduction can be obtained
before preparation and draping. First, the fracture is reduced both in
length and alignment. If the fracture is open, it should be irrigated
and débrided before application of the external fixation device. With
the fracture optimally aligned, fixation is begun. The minimal and
maximal length constraints characteristic of all external fixation
systems must be kept in mind, and the angular adjustment intrinsic to
the fixation device should be determined. Rotation is constrained with
all external fixation systems once the first pins are placed. That is,
if parallel pins are placed with the fracture in 40 degrees of
malrotation, a 40-degree malalignment will exist. Rotational correction
must be obtained before placing the pins in the proximal and distal
shafts of the femur.
device is chosen. One pin is placed proximally in the shaft, and
another pin is placed distally perpendicular to the long axis of the
shaft. Alignment is based on the long axis of the shaft, rather than
the joint surface. Rotation should be checked before the second pin is
placed because it constrains rotation but not angulation or length.
After pins are correctly placed, all fixation nuts are secured and
sterile dressings are applied to pins.
general, the pins are placed through predrilled holes to avoid thermal
necrosis of bone. Sharp drills should be used. The manufacturer’s
recommendation for drill and screw sizes should be checked before
starting the procedure. Some self-drilling and self-tapping pins are
available. At least two pins should be placed proximally and two
distally. An intermediate or auxiliary pin may be beneficial.
tension at the skin-pin interface. We recommend that our patients clean
their pin sites daily with soap and water, perhaps as part of regular
bath or shower. Showering is allowed once the wound
is
stable and there is no communication between the pin and the fracture
hematoma. Antibiotics are commonly used at some point while the fixator
is in place, because pin site infections are common and easily resolved
with antibiotic treatment, usually cephalosporin.
removal. The external fixation device can be used as “portable
traction.” With this strategy, the fixator is left in place until early
callus stabilizes the fracture. At this point, usually 6 to 8 weeks
after injury, the fixator device is removed and a walking spica cast is
placed. This minimizes stress shielding from the fixator and allows
time for the pin holes to fill in while the cast is on. The
alternative, classic strategy involves using the fixator until the
fracture is completely healed. Fixator dynamization, which is difficult
in small, young children, is essential for this strategy. The device
should not be removed until three or four cortices show bridging bone
continuous on AP and lateral radiographs, typically 3 to 4 months after
injury.
track irritation or infection, which has been reported to occur in up
to 72% of patients.147 This problem generally is easily treated with oral antibiotics and local pin site care. Sola et al.189
reported a decreased number of pin track infections after changing
their pin care protocol from cleansing with peroxide to simply having
the patient shower daily. Superficial infections should be treated
aggressively with pin track releases and antibiotics. Deep infections
are rare, but if present, surgical débridement and antibiotic therapy
are usually effective. Any skin tenting over the pins should be
released at the time of application or at follow-up.
reported a 30% major complication rate and a high minor complication
rate. Among the major complications were five refractures or fractures
through pin sites. Another comprehensive study of external fixation
complications33 found an overall rate of refracture of 4.7%, with a pin track infection rate of 33.1%. Skaggs et al.187
reviewed the use of external fixation devices for femoral fractures and
found a 12% rate of secondary fractures in 66 patients. Multivariate
linear regression analysis showed no correlation between the incidence
of refracture and the fracture pattern, percentage of bone contact
after fixator application, type of external fixator used, or
dynamization of the fracture. A statistically significant association
was found between the number of cortices demonstrating bridging callus
on both the AP and lateral views at the time of fixator removal and
refracture. Fractures with fewer than three cortices with bridging
callus at the time of fixator removal had a 33% risk of refracture,
whereas those with three or four cortices showing bridging callus had
only a 4% rate of refracture. Other reports in the literature with
smaller numbers, but still substantial experience, document refracture
rates as high as 21.6% with more significant complications.47,48,71,96,147,167,184 In 1997, in a follow-up of the original article by Aronson and Tursky,6 Blasier et al.19
reported 139 femoral fractures treated with external fixation; they
found that pin track infection was common and there was a 2% incidence
of fracture after removal of the device. El Hayek et al.54
demonstrated the benefit of modern techniques of external fixation in a
series of 28 fractures in 21 children. Despite the complications,
patients and treating physicians have found wound care and ability to
lengthen through the fracture to be of great benefit with this
technique.
patients treated with external fixation, it is relatively uncommon in
children with femoral fractures unless major soft tissue injury is
present.57
and others in the early 1990s alerting surgeons that antegrade
intramedullary nailing can be complicated by osteonecrosis of the
proximal femur, flexible nailing (either antegrade or retrograde)
quickly became more popular than standard locked, antegrade rigid
intramedullary nailing. Recently, however, locked antegrade femoral
nailing for pediatric femoral fractures has enjoyed a resurgence of
interest with the introduction of newer generation implants that allow
a very lateral trochanteric entry point. These newer implant systems
avoid a piriformis entry site, reducing (but perhaps not completely
eliminating) the risk of osteonecrosis. Others have adapted humeral
nails for pediatric femoral fractures.16
Antegrade locked intramedullary fixation is particularly valuable for
femoral fractures in adolescents. Comparative studies by Reeves et al.170 and Kirby et al.,113
as well as retrospective reviews of traction and casting, suggest that
femoral fractures in adolescents are better treated with intramedullary
fixation11,30,47,68,69,73,90,108,113,123,197,210,212 than with traditional traction and casting (Table 22-3). Kanellopoulos et al.107
reported excellent results in 20 skeletally immature patients, ranging
in age from 11 to 16 years, treated with closed, locked intramedullary
nailing through the tip of the greater trochanter. There were no
complications, including no osteonecrosis, with an average follow-up of
29 months.
from interlocking proximally and distally to maintain length and
rotational alignment.12,25,78 Beaty et al.11
reported the use of interlocking intramedullary nails for the treatment
of 31 femoral shaft fractures in 30 patients 10 to 15 years of age. All
fractures united, and the average leg length discrepancy was 0.51 cm.
No angular or rotational malunions occurred. All nails were removed at
an average of 14 months after injury; no refracture or femoral neck
fracture occurred after nail removal. One case of osteonecrosis of the
femoral head occurred, which was thought to be secondary to injury to
the ascending cervical artery during nail insertion.
proximal femoral physis must absolutely avoid the piriformis fossa, due
to the risk of proximal femoral growth abnormalities,168 the risk of osteonecrosis of the femoral head,11,143,166,194 the size of the proximal femur, and the relative success of other treatment methods. However, Maruenda-Paulino et al.131 reported good results using 9-mm Kuntscher rods in children 7 to 12 years of age, and Beaty et al.11
reported the use of pediatric “intermediate” interlocking nails for
femoral canals with diameters as small as 8 mm. Townsend and Hoffinger200 and Momberger et al.148
published reviews of trochanteric nailing in adolescents with very good
results. The combined series included 82 patients aged 10 to 17 with
follow-up of 6 years with no reported
cases of osteonecrosis and no significant alteration in proximal femoral anatomy.
|
TABLE 22-3 Results of Treatment of Femoral Shaft Fractures in Adolescents
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
treated with intramedullary rodding, either as delayed or primary
treatment, including those caused by gunshot wounds and high-velocity
injuries.15,198
Antegrade intramedullary rod insertion maintains length, prevents
angular malunion and nonunion, and allows the patient to be rapidly
mobilized and discharged from the hospital. However, other techniques
with fewer potential risks should be considered.
In a large patient approaching skeletal maturity (bone age >16
years) but with an open proximal femoral physis and an unstable
fracture pattern, this treatment might be considered as a way to avoid
the risk of osteonecrosis yet stabilize the fracture (Fig. 22-22).
If growth from the distal femur is predicted to be less than 1 cm, leg
length inequality should not be a problem. Ricci et al.172
have shown that the complication rate with this technique compares
favorably to that of antegrade nailing, with a higher rate of knee pain
but a lower rate of hip pain. The malunion rate was slightly lower with
retrograde rodding than with antegrade rodding of the femur.
decubitus position on a fracture table. The upper end of the femur is
approached through a 3-cm longitudinal incision proximal that allows
access to the lateral trochanteric entry point. The skin incision can
be precisely placed after localization on both the AP and lateral
views. Dissection should be limited to the lateral aspect of the
greater trochanter, avoiding the piriformis fossa. This prevents
dissection near the origin of the lateral ascending cervical artery
medial to the piriformis fossa. The rod should be inserted through the
lateral aspect of the greater trochanter. In children and adolescents,
it is preferable to choose the smallest implant with the smallest
diameter reaming to avoid damage to the proximal femoral insertion area.
according to the specifics of the implant chosen. In general, the
smallest rod that maintains contact with the femoral cortices is used
(generally 9 mm or less) and is locked proximally and distally (Fig. 22-23). Only one distal locking screw is necessary, but two can be used.112
Rods that have an expanded proximal cross-section should be avoided,
because they require excessive removal of bone from the child’s
proximal femur. The proximal end of the nail should be left slightly
long (up to 1 cm) to make later removal easier. The rod chosen should
be angled proximally and specifically designed for transtrochanteric
insertion (Fig. 22-24).
without extending to the capsule or midportion of the femoral neck.
Some systems provide a small diameter, semiflexible tube that can be
inserted up to the fracture site after initial entry-site reaming. This
tube is extremely helpful in manipulating a flexed, abducted proximal
fragment in proximal third femoral fractures.
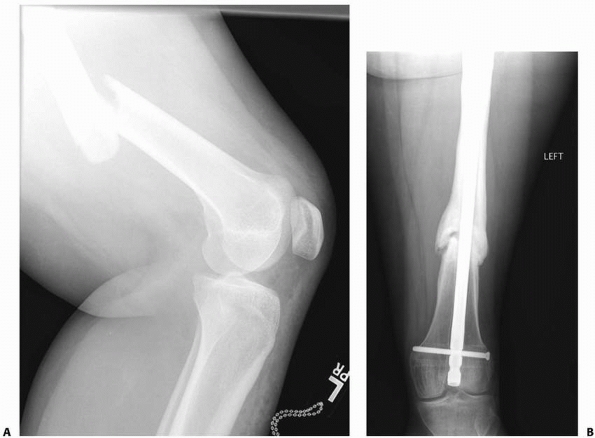 |
|
FIGURE 22-22 A. This distal femoral shaft fracture in a skeletally mature girl was treated with retrograde femoral nailing. B. There is a delayed union.
|
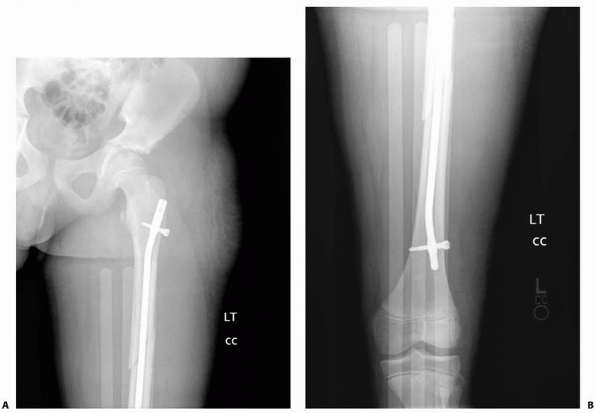 |
|
FIGURE 22-23 AP (A) and lateral (B)
x-rays immediately after internal fixation of the midshaft femur fracture in a 13-year-old with a pediatric locking nail that permits easy lateral entry and requires minimal reaming of the child’s proximal femur. |
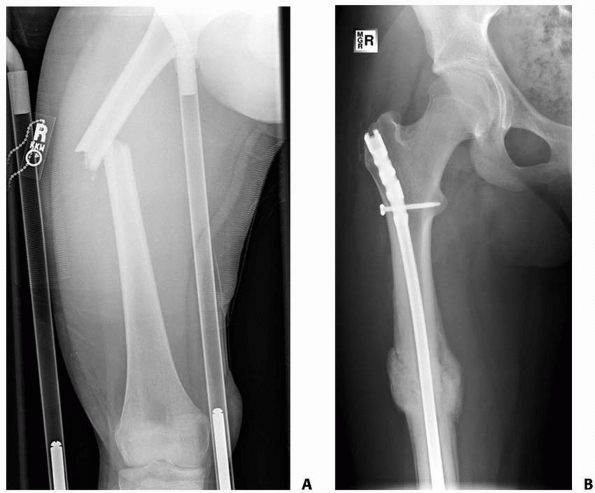 |
|
FIGURE 22-24 Preoperative (A) and postoperative (B) images showing the use of a newer generation lateral entry nail to treat a proximal third femur fracture in a 14-year-old girl.
|
prevent bony overgrowth over the proximal tip of the nail. We do not
routinely remove locked andtegrade nails from our teenage patients
unless they are symptomatic or request removal for another reason.
Dynamization with removal of the proximal or distal screw generally is
not necessary.
technique and patient satisfaction is high, problems with proximal
femoral growth, osteonecrosis, and leg-length discrepancy cannot be
ignored.
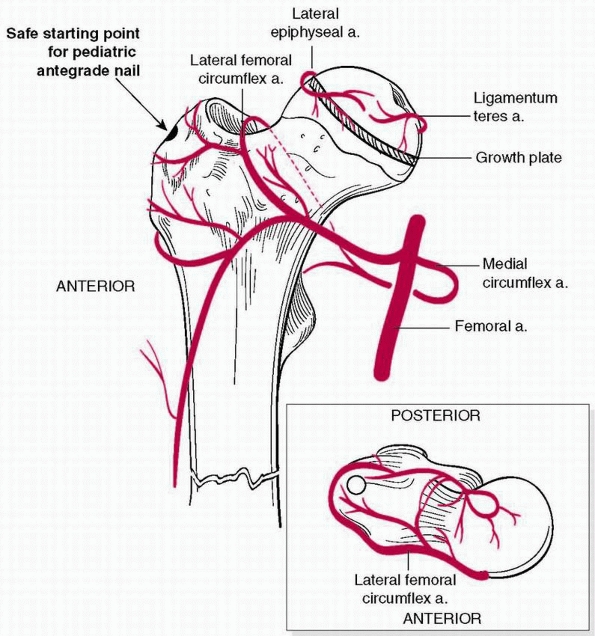 |
|
FIGURE 22-25 Trochanteric entry point for intramedullary nail indicated with arrow.
Entry here with smaller diameter nails limits the risk of avascular necrosis and ensures no awl in the piriformis fossa. (From Skaggs D, Flynn J. Trauma about the pelvis/hip/femur. Staying Out of Trouble in Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins, 2006:109.) |
reported a patient with osteonecrosis of the proximal femoral epiphysis
after a greater trochanteric fracture, suggesting that the blood supply
to the proximal femur may have been compromised by vascular disruption
at the level of the greater trochanter during rod insertion. Other
researchers have reported single patients
with osteonecrosis of the femoral head after intramedullary nailing.143,160,194
A poll of the members of the Pediatric Orthopaedic Society disclosed 14
patients with osteonecrosis in approximately 1600 femoral fractures.
Despite the use of a “safe” transtrochanteric insertion site for
antegrade femoral rodding, a case of osteonecrosis has been reported.
Buford et al.28 showed in their MRI
study of hips after antegrade rodding that subclinical osteonecrosis
may be present. Antegrade rodding through the trochanter or the upper
end of the femur appears to be associated with a risk of osteonecrosis
in children with open physes, regardless of chronologic age. Chung36
noted the absence of transphyseal vessels to the proximal femoral
epiphysis and demonstrated that the singular lateral ascending cervical
artery predominantly supplies blood to the capital femoral epiphysis (Fig. 22-27).
He stated that all of the epiphyseal and metaphyseal branches of the
lateral ascending cervical artery originate from a single stem that
crosses the capsule at the trochanteric notch. Because the space
between the trochanter and the femoral head is extremely narrow, this
single artery is vulnerable to injury and appears to be so until
skeletal maturity, regardless of chronologic age.
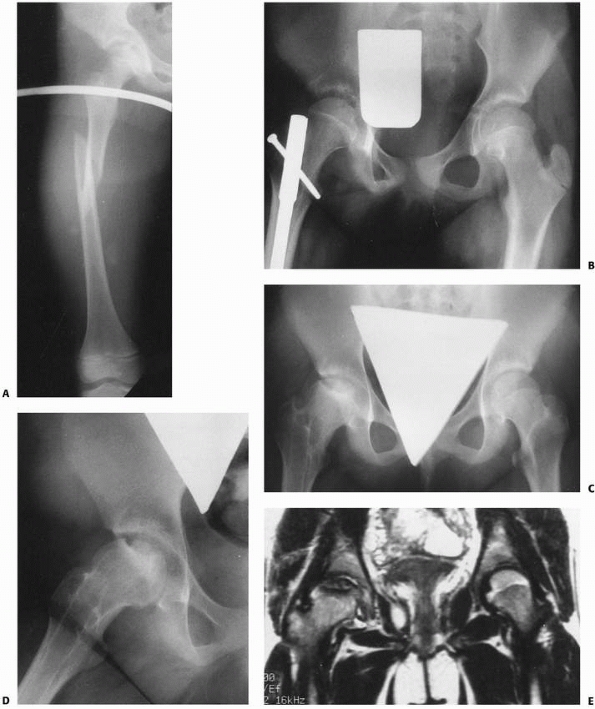 |
|
FIGURE 22-26 A. Isolated femoral shaft fracture in an 11-year-old. B. After fixation with an intramedullary nail, femoral head appears normal. C. Eight months after injury, fracture is healed; note early signs of osteonecrosis of right femoral head. D. Fifteen months after injury, segmental osteonecrosis of the femoral head is evident on x-rays. E. MRI shows extent of osteonecrosis of right femoral head. (D.
reprinted from Beaty JH, Austin SM, Warner WC, et al. Interlocking intramedullary nailing of femoral-shaft fractures in adolescents: preliminary results and complications. J Pediatr Orthop 1994;14:178-183, with permission.) |
in a long-term study of 52 children and adolescents with femoral
fractures treated with plating and intramedullary rodding, found that
excessive overgrowth was less common with nailing than with plating.
Three patients had moderate valgus deformities of the hip and one had
late arthrosis after intramedullary rodding despite using a
transtrochanteric approach. Simonian et al.184
concluded that open physes were a contraindication to antegrade rodding
even with a transtrochanteric approach. Thometz and Lamdan194 also documented an association between osteonecrosis and antegrade rodding in an adolescent.
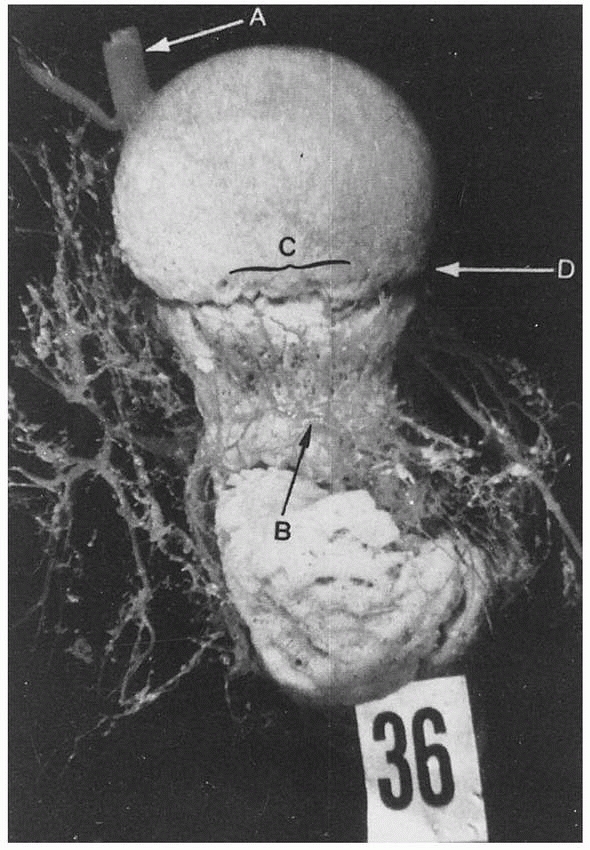 |
|
FIGURE 22-27 The single ascending cervical artery (A)
is the predominant blood supply to the femoral head. The vessel is at risk during antegrade insertion of an intramedullary rod. (From Chung S. The arterial supply of the developing proximal end of the femur. J Bone Joint Surg Am 1976;58:961, with permission.) |
arrest of the greater trochanteric physis. Although most growth from
the greater trochanter after 8 years of age is appositional, Raney et
al.168 reported 5 patients who
developed coxa valga and mild hip subluxation from trochanteric physeal
arrest after antegrade nailing. These patients ranged in age from 9 to
13 years, suggesting that even in older children greater trochanteric
physeal arrest occasionally can produce clinical problems. Beaty et al.11
reported 2 patients, boys age 13 years, with overgrowth of more than
2.5 cm that required epiphysiodesis because of leg length discrepancy.
Gordon et al.,69 in a study of the
effect of trochanteric nailing on proximal femoral anatomy, found no
significant changes in the articulotrochanteric distance, the
neck-shaft angle, or the width of the femoral neck after trochanteric
antegrade nailing. They also found no incidence of osteonecrosis.
cartilaginous plate between the greater trochanter and the proximal
femur in young children. Interference with the physis may result in
abnormal growth of the femoral neck, placing the child at a small risk
for subsequent femoral neck fracture.184
Antegrade nailing with reaming of a large defect also may result in
growth disturbance in the proximal femur as well as femoral neck
fracture (Fig. 22-28). Beaty et al.11
reported no “thinning” of the femoral neck in their patients, which
they attributed to an older patient group (10 to 15 years of age) and
design changes in the femoral nail that allowed a decrease in the cross
sectional diameter of the proximal portion of the femoral rods.
indications for traditional open reduction and plate fixation (i.e.,
full length incision, subperiosteal dissection and plate fixation,
filling most or all screw holes), except perhaps with extensile
exposure to repair an arterial injury. Ward et al.,208 Kregor et al.,115 Fyodorov et al.,67 and Hansen79 recommended open compression plate fixation in selected femoral fractures. Ward et al.208
reported the use of AO compression plates for the treatment of femoral
shaft fractures in 25 children 6 to 16 years of age, 22 of whom had
associated fractures or multisystem injuries. They recommended plate
fixation for children under 11 years of age with closed-head injuries
or multiple trauma. Disadvantages of plate fixation include the long
incision necessary and the risks of plate breakage and stress fracture
after plate removal. All the patients reported by Kregor et al.115
had multiple trauma, and this form of treatment was selected to
stabilize the femoral fracture quickly and mobilize the patient.
Fyodorov et al.67 reviewed 21
patients in whom 4.5-mm dynamic compression plates (DCPs) were used for
fixation. Patients were kept nonweight bearing on crutches for 8 weeks.
There were two plate breakages requiring revision and one requiring
spica casting to achieve healing.
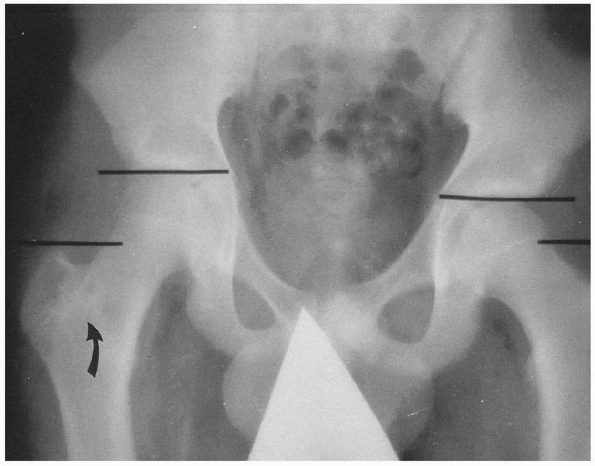 |
|
FIGURE 22-28
Fifteen-year-old boy 3 years after intramedullary nailing of the right femur. Articulotrochanteric distance increased by 1.5 cm; note partial trochanteric epiphysiodesis (arrow) with mild overgrowth of the femoral neck. (From Beaty JH, Austin SM, Warner WC, et al. Interlocking intramedullary nailing of femoral-shaft fractures in adolescents: preliminary results and complications. Pediatr Orthop 1994;14:178-183, with permission.) |
radiolucent operating table. The femur is approached laterally. The
vastus lateralis is retracted anteriorly to expose the femur. Soft
tissue attachments to the bone are preserved to the extent possible.
Fragments are lagged into place and secured with a DCP. A 4.5-mm or
larger compression plate is used in children. If the fracture is at
either end of the bone, leaving insufficient bone for cortical
fixation, fully threaded cancellous screws add to the stability of
fixation and are preferable to either cortical or partially threaded
cancellous screws. Both interfragmentary compression and dynamic
compression techniques can be used to achieve stability and anatomic
alignment. Locking screws are rarely necessary and may be difficult to
remove if they “coldweld” to the plate.
stripping should be limited, and three screws should be used proximal
and distal to the fracture site.
to tolerance. Active range-of-motion exercise of the hip and knee is
encouraged.
limiting incisions, maintaining the periosteum, using long plates, and
filling only a few selected screw holes, are being adopted by an
increasing number of pediatric orthopaedic trauma surgeons as a
valuable tool to manage length-unstable femoral fractures. Pathologic
fractures, especially in the distal femoral metaphysis, create large
areas of bone loss that can be treated with open biopsy, plate
fixation, and immediate bone grafting.
reported a series of 51 patients with submuscular bridge plating with
up to 10 year follow-up; 55% had unstable fracture patterns. There were
two significant complications: one plate breakage (3.5 mm) and one
fracture after plate removal. Functional outcome was excellent, with 8%
significant leg-length discrepancy. Hedequist et al.80
reported 32 patients aged 6 to 15 years old, most of whom had fractures
that were comminuted, pathologic, osteopenic, or in a difficult
location. Rozbruch et al.177
described modern techniques of plate fixation popularized by the AO
Association for the Study of InternalFixation that include indirect
reduction, biologic approaches to internal fixation, and greater use of
blade plates and locked plates (Fig. 22-30).
bone for fixation between the fracture and the physes, locked plating
techniques may be valuable. This technique provides greater stability
by securing the plate with a fixed-angle screw in which the threads
lock to the plate, as well as in the bone. This effectively converts
the screw-plate to a fixed-angle blade plate device. In using this type
of device, one should lock first, then compress, and finally lock the
plate on the opposite side of the fracture. The locked plate can be
used with an extensile exposure or with a submuscular plating
technique, but the latter is more difficult and should be attempted
only when the technique is mastered.
pathologic lesion, severe osteopenia, or severe comminution is present.
Locking screws can cold-weld to the plate, later turning a simple
implant removal into a very difficult procedure involving large
exposures, cutting of the implant, and possible locally destructive
maneuvers to remove the screws.
The patient is positioned on a fracture table, and a provisional
reduction is obtained with gentle traction. In most cases, a 4.5-mm
narrow, low-contact DCP plate is used. In osteopenic patients or when
there is a proximal or distal fracture, locking plates may be used. A
very long plate, with 10 to 16 holes, is preferred; the plate selection
is finalized by obtaining an image with the plate over the anterior
thigh, assuring that there are six screw holes proximal and distal to
the fracture (although in some more proximal and distal fractures, only
three holes will be available). Depending on the fracture location and
thus the position of the plate, the plate will need to be contoured to
accommodate the proximal or distal femur. The table-top plate bender is
used to create a small flare proximally for the plate to accommodate
the contour of the greater trochanter or a larger flare to accommodate
the distal femoral metaphysis. The plate must be contoured anatomically
because the fixed femur will come to assume the shape of the plate
after screw fixation. A 2- to 3-cm incision is made over the distal
femur, just above the level of the physis. Exposure of the periosteum
just below the vastus lateralis facilitates the submuscular passage of
the plate. A Cobb elevator is used to dissect the plane
between
the periosteum and the vastus lateralis. The fracture site is not
exposed, and, in general, a proximal incision is not required. The
plate is inserted underneath the vastus lateralis, and the femoral
shaft is held to length by traction. The plate is advanced slowly,
allowing the surgeon to feel the bone against the tip of the plate.
Fluoroscopy is helpful in determining proper positioning of the plate.
A bolster is placed under the thigh to help maintain sagittal
alignment. Once the plate is in position and the femur is out to
length, Kirschner wires are placed in the most proximal and most distal
holes of the plate to maintain length (Fig. 22-31).
Fluoroscopy is used to check the AP and lateral views and to be sure
the bone is at appropriate length at this point. A third Kirschner wire
can be used to provide a more stable reduction of the femoral shaft.
Although screws can be used to facilitate angular reduction to the
plate, length must be achieved before the initiation of fixation.
 |
|
FIGURE 22-29 AP (A) and lateral (B)
x-rays showing a complex spiral distal femur fracture that extends into the joint. This is a variation of Salter-Harris type IV fracture. C. The fracture was managed with submuscular plating and percutaneous lag screw fixation of the distal femoral condyle fractures. |
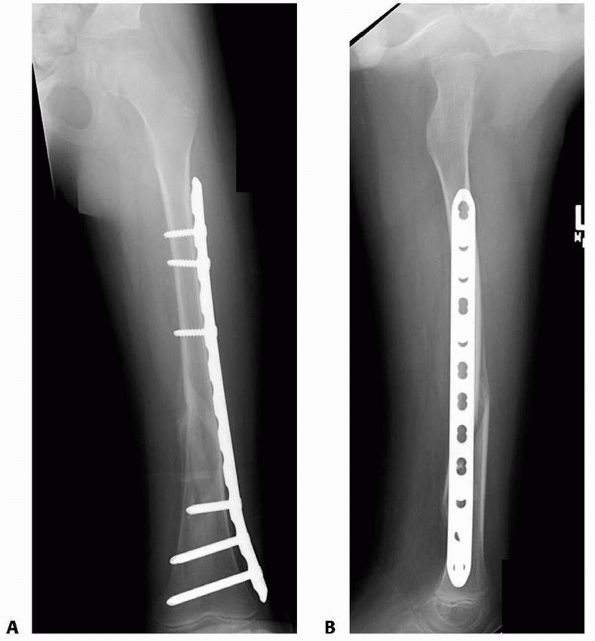 |
|
FIGURE 22-30 A.
This child with an unstable femoral fracture in osteopenic bone was managed with a submuscular locking plate providing alignment and stability. B. The lateral bow of the femur may be partially preserved despite a straight plate. |
sites for screw fixation. Greater spread of screws increases the
stability of fracture fixation. We generally place one screw through
the distal incision under direct observation. At the opposite end of
the femur, the next most proximal screw is placed to fix length and
provisionally improve alignment. Central screws are then placed, using
a free-hand technique with the “perfect circle” alignment of the plate
over the fracture fragments. Stab holes are made centrally for drill
and screw insertion. Rather than using a depth gauge directly, because
the bone will be pulled to the plate, the depth gauge is placed over
the thigh itself to measure appropriate length of the screw. When
screws are inserted, a Vicryl (Ethicon, Inc., Somerville, NJ) tie is
placed around the shank to avoid losing the screw during percutaneous
placement. Self-tapping screws are required for this procedure. Six
cortices are sought on either side of the fracture.
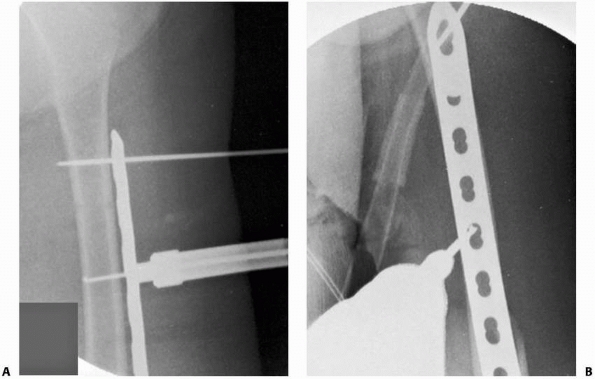 |
|
FIGURE 22-31 A. A Kirschner wire is inserted in the end holes of the plate to maintain length. B. Drill holes and screws are placed with fluoroscope imaging.
|
bearing on crutches with no need for cast immobilization, as long as
stable fixation is achieved. At times, there is benefit to a knee
immobilizer; however, in general, this is not required. Early weight
bearing in some series of plate fixation has resulted in a low but
significant incidence of plate breakage and nonunion. These
complications should be decreased by a cautious period of postoperative
management.
comminution to require a locked plate to provide secure fixation. In
using a locked plate submuscularly, a large enough incision must be
used to be sure the bone is against the plate when it is locked. The
articular fragment is fixed first to ensure that the angular
relationship between the joint surface and the shaft is perfect.
traditional compression plate application may lead to overgrowth.
Overgrowth was not a significant problem in the series of Kregor et al.,115 with an average increase in length of 0.9 cm (range 0.5 to 1.5 cm), but Ward et al.208 reported several patients with considerable overgrowth (approximately 1 inch), and Hansen79
reported overgrowth of an inch in a 12-year-old boy, suggesting that
overgrowth is possible in children over 10 years of age. Eren et al.56
reported a series of 40 children aged 4 to 10 years with significant
lengthening on the operated side in 40% of patients, averaging 1.2 cm
(0.4 to 1.8 cm).
reported implant failure in 2 of 23 femoral shaft fractures treated
with DCPs. One was treated with revision plating and the other with
spica casting; both fractures healed uneventfully. No other
complications were noted in their patients.
screw holes, and whether bone atrophy under a plate is caused by stress
shielding or by avascularity of the cortex is unknown. Although still
somewhat controversial, the plate and screws can be removed at 1 year
after fracture to avoid fracture at the end of the plate.
of age, we use a Pavlik harness. One of us gently wraps the thigh in
Webril (Kendall Health Care Products, Mansfield, MA) before placing the
harness. If the fracture is unstable, usually the proximal fragment is
flexed and a Pavlik harness is the ideal device for reducing and
holding the fracture. The use of a Pavlik harness requires an attentive
and compliant caregiver. A Gore-tex lined spica is an alternative,
especially for bigger, older babies. Traction with a spica cast is
rarely if ever needed in this group.
femoral fracture, an early spica cast is usually the treatment of
choice. In a typical low-energy toddler femoral fracture, we have noted
similar clinical results but much happier families and children when we
use a one-leg walking spica, so this has become our choice for this age
group. Some children with a walking spica benefit from cast wedging 1
to 2 weeks after injury, so we prepare families for this possibility. A
Gore-tex liner, if available, markedly improves skin care. If length or
alignment cannot be maintained in an early spica cast (this is rare in
low-energy fractures), traction followed by casting can be used. We
typically use a distal femoral traction pin and place the child in a
90/90 or oblique position in the bed for traction. We must emphasize
that over 95% of infants and toddlers can be managed without traction
with a low complication rate and low cost. In children with
multiple-system trauma, either flexible intramedullary nailing or
external fixation is often a better choice, based on the fracture
anatomy and the soft-tissue injury. Traction is rarely used in patients
with multiple-system trauma.
intramedullary nailing is generally the safest and best option for
length-stable fractures (and many length-unstable) fractures.
Submuscular bridge plating or external fixation is used for unstable
fracture patterns, comminuted fractures, and fractures with severe soft
tissue injury. Early spica casting can be used for nondisplaced or
minimally displaced fractures in this age group. In certain situations,
the family and surgeon prefer a nonsurgical option; in such cases,
spica casting, usually with traction, can be used in school-aged
children.
trochanteric-entry locked intramedullary nail or submuscular bridge
plating. Flexible intramedullary rods are also effective in this age
group (Fig. 22-32), especially for midshaft
transverse fractures in smaller children. The surgeon should be aware
that the complication rate rises with flexible nailing in this older
group.149 External fixation is
occasionally valuable in the 11- to 16-year-old group, particularly in
complex proximal or distal fractures. Healing is slow, however, and the
full treatment course may take 4 months or more. Locked plating can be
used for subtrochanteric and supracondylar fractures of the femur,
whereas intramedullary nails are ideal for midshaft fractures. If
antegrade rodding is chosen, a transtrochanteric approach is used.
There is a limited role for retrograde locked intramedullary nailing in
adolescents approaching skeletal maturity.
children is leg-length discrepancy. The fractured femur may be
initially short from overriding of the fragments at union; growth
acceleration occurs to “make up” the difference, but often this
acceleration continues and the injured leg ends up being longer. The
potential for growth stimulation from femoral fractures has long been
recognized, but the exact cause of this phenomenon is still unknown.
Growth acceleration has been attributed to age,
sex,
fracture type, fracture level, handedness, and the amount of overriding
of the fracture fragments. Age seems to be the most constant factor,
but fractures in the proximal third of the femur and oblique comminuted
fractures also have been associated with relatively greater growth
acceleration
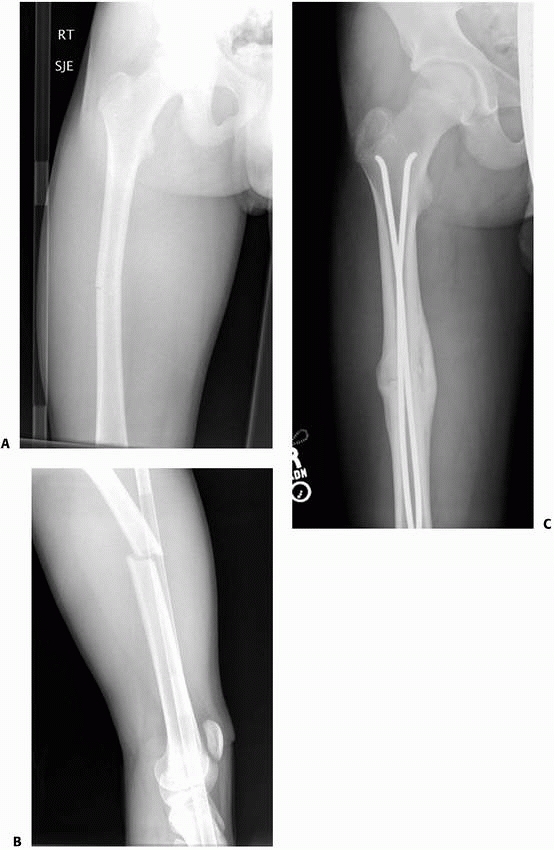 |
|
FIGURE 22-32
Successful use of titanium elastic nails in older teenager. This 15-year-old sustained a minimally displaced midshaft femur fracture AP (A) and lateral (B) views at presentation. C. This x-ray, taken 3 months after injury, shows that the fracture healed in perfect alignment with abundant callus. |
approximately 1.5 cm, shortening of 2 to 3 cm in the cast is the
maximal acceptable amount. The maximal acceptable shortening depends on
the age of the child; for example, in a 6-year-old child, 2.5 cm may be
acceptable, whereas only 1 to 2 cm should be accepted in a 14-year-old
approaching skeletal maturity.
children 2 to 10 years of age. The average overgrowth is 0.9 cm, with a
range of 0.4 to 2.5 cm.182
Overgrowth occurs whether the fracture is short, at length, or
overpulled in traction at the time of healing. In general, overgrowth
occurs most rapidly during the first 2 years after fracture and to a
much lesser degree for the next year or so.72
reported the phenomenon of overgrowth in 1921, and many researchers
since have verified the existence of growth stimulation after fracture.1,2,4,8,38,40,53,129,138,168 The relationship of the location of the fracture to growth is somewhat controversial. Staheli190 and Malkawi et al.129 reported that
overgrowth was greatest if the fracture occurred in the proximal third of the femur, whereas Henry89
stated that the most overgrowth occurred in fractures in the distal
third of the femur. Other investigators have found no relationship
between fracture location and growth stimulation.53,89,171,182
The relationship between fracture type and overgrowth also is
controversial. In general, most researchers believe that no specific
relationship exists between fracture type and overgrowth, but some have
reported overgrowth to be more frequent after spiral, oblique, and
comminuted fractures associated with greater trauma.
femoral shaft fractures in children, but this usually remodels with
growth. Angular remodeling occurs at the site of fracture, with
appositional new bone formation in the concavity of the long bone.
Differential physeal growth also occurs in response to diaphyseal
angular deformity. Wallace and Hoffman207
stated that 74% of the remodeling that occurs is physeal, and
appositional remodeling at the fracture site occurs to a much lesser
degree. However, this appears to be somewhat age dependent. It is clear
that angular remodeling occurs best in the direction of motion at the
adjacent joint.207 That is, anterior
and posterior remodeling in the femur occurs rapidly and with little
residual deformity. In contrast, remodeling of a varus or valgus
deformity occurs more slowly. The differential physeal growth in a
varus or valgus direction in the distal femur causes compensatory
deformity, which is usually insignificant. In severe varus bowing,
however, a hypoplastic lateral condyle results, which may cause a
distal femoral valgus deformity if the varus bow is corrected.
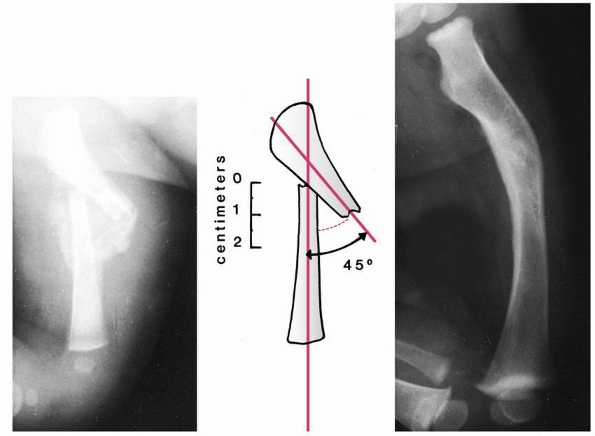 |
|
FIGURE 22-33
Remodeling potential of the femur during infancy. This infant sustained a femoral fracture during a breech delivery and was placed in a spica cast but with insufficient flexion of the hip. Left: At 3 weeks, union is evident with about 45 degrees of angulation in the sagittal plane and 1.5 cm of overriding. Center: Line drawing demonstrating true angulation. Right: Twelve months later, the anterior angulation has reduced to a level such that it was not apparent to the family, and the shortening has reduced to less than 1 cm. |
range of acceptable anterior and posterior angulation varies from 30 to
40 degrees in children up to 2 years of age (Fig. 22-33), decreasing to 10 degrees in older children and adolescents.128
The range of acceptable varus and valgus angulation also becomes
smaller with age. Varus angulation in infants and children should be
between 10 and 15 degrees, although greater degrees of angulation may
have a satisfactory outcome. Acceptable valgus angulation is 20 to 30
degrees in infants, 15 to 20 degrees in children up to 5 years of age,
and 10 degrees in older children and adolescents. Compensation for
deformity around the knee is limited, so guidelines for the distal
femoral fractures should be stricter than for proximal femoral
fractures.
proximal tibia after femoral shaft fracture has been most often
reported as a complication of traction pin or wire placement through or
near the anterior aspect of the proximal tibial physis, excessive
traction, pin track infection, or prolonged cast immobilization.203 However, proximal tibial growth arrest may complicate femoral shaft fracture, presumably as a result of occult
injury.94 Femoral pins are preferred for traction, but if tibial pins are required, the proximal anterior tibial physis must be avoided.146
Femoral traction pins should be placed one or two fingerbreadths
proximal to the superior pole of the patella to avoid the distal
femoral physis.
fracture union, corrective osteotomy should be delayed for at least a
year unless the deformity is severe enough to markedly impair function.
This will allow determination of remodeling potential before deciding
that surgical correction is necessary. The ideal osteotomy corrects the
deformity at the site of fracture. In juvenile patients, however,
metaphyseal osteotomy of the proximal or distal femur may be necessary.
In adolescents with midshaft deformities, diaphyseal osteotomy and
fixation with an interlocking intramedullary nail are often preferable.
rotational deformities of 10 degrees to more than 30 degrees occur in
one third of children after conservative treatment of femoral shaft
fractures. Malkawi et al.129 found
asymptomatic rotational deformities of less than 10 degrees in two
thirds of their 31 patients. Torsional deformity usually is expressed
as increased femoral anteversion on the fractured side compared with
the opposite side, as demonstrated by physical exam; a difference of
more than 10 degrees has been the criterion of significant deformity.
However, Brouwer et al.24 challenged
this criterion, citing differences of 0 to 15 degrees in a control
group of 100 normal volunteers. The accuracy of measurements from plain
radiographs also has been disputed, and Norbeck et al.156 suggested the use of computed tomographic (CT) scanning for greater accuracy.
another controversy in the search for criteria on which to base
therapeutic judgments. According to Davids46 and Braten et al.,23
up to 25 degrees of rotational malalignment at the time of healing of
femoral fractures appears to be well-tolerated in children. In their
patients with more than 25 degrees of rotational malalignment, however,
deformity caused clinical complaints. Davids46
found no spontaneous correction in his study of malunions based on CT
measurements, but the length of follow-up is insufficient to state that
no rotational remodeling occurs. Brouwer et al.24 and others14,77,159,204 reported slow rotational correction over time. Buchholz et al.27
documented 5 children between 3 and 6 years old with increased femoral
anteversion of 10 degrees or more after fracture healing. In 3 of the 5
children, there was full correction of the rotational deformity but the
oldest of the children the deformity failed to correct spontaneously.
rotational remodeling will occur. In infants and juveniles, some
rotational deformity can be accepted60
because either true rotational remodeling or functional adaptation
allows resumption of normal gait. Up to 30 degrees of malrotation in
the femur should result in no functional impairment unless there is
pre-existing rotational malalignment. The goal, however, should be to
reduce a rotational deformity to 10 degrees, based on alignment of the
proximal and distal femur on x-ray, interpretation of skin and soft
tissue envelope alignment, and correct positioning within a cast, based
on the muscle pull on the proximal fragment. The distal fragment should
be lined up with the position of the proximal fragment determined by
the muscles inserted on it (see Fig. 22-3).
children. The rate of healing also is related to soft-tissue injury and
type of treatment. The time to fracture union in most children is rapid
and age dependent. In infants, the fracture can be healed in 2 to 3
weeks. In children under 5 years of age, healing usually occurs in 4 to
6 weeks. In children 5 to 10 years of age, fracture healing is somewhat
slower, requiring 8 to 10 weeks. Throughout adolescence, the time to
healing continues to lengthen. By the age of 15 years, the mean time to
healing is about 13 weeks, with a range from 10 to 15 weeks (Fig. 22-34).
Application of an external fixation device appears to delay callus
formation and slow the rate of healing. Flexible nailing allows some
motion at the fracture site, promoting extensive callus formation. In
adults, there is an association between nonunion and the use of
nonsteroidal anti-inflammatory drugs (NSAIDs) after injury and delayed
fracture healing,1,60
which is very significant. Although there is not similar data for
children, perhaps patients with risk factors for delayed healing should
avoid NSAIDs.
compression plate or locked intramedullary nail are the usual treatment
for delayed union in older children and adolescents. Delayed union of a
femoral fracture treated with casting in a child 1 to 6 years of age is
probably best treated by continuing cast immobilization until bridging
callus forms or (rarely) by additional bone grafting.
They tend to occur in adolescents, in infected fractures, or in
fractures with segmental bone loss or severe soft tissue loss. Tibial
fractures
are
the most common source of pediatric nonunions; femoral fractures
account for only 15% of nonunions in children. Even in segmental
fractures with bone loss, young children may have sufficient osteogenic
potential to fill in a significant fracture gap (Fig. 22-35).142
For the rare femoral shaft nonunion in a child 5 to 10 years of age,
bone grafting and plate-and-screw fixation have been traditional
treatment methods, but more recently insertion of an interlocking
intramedullary nail and bone grafting have been preferred, especially
in children over 10 to 12 years of age. Aksoy et al.3
reported a small series of nonunions and malunions salvaged with
titanium elastic nails. Union was achieved in 6 to 9 months in most
cases.
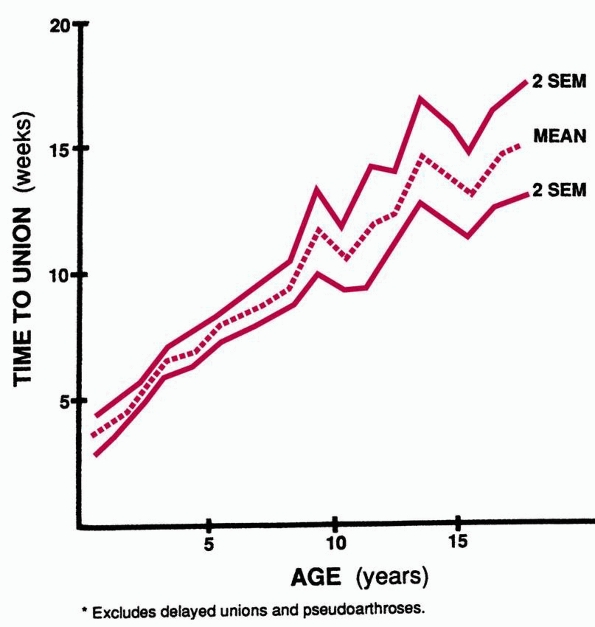 |
|
FIGURE 22-34
Time required for union of femoral shaft fractures in childhood and adolescence. (From Skak SV, Jensen TT. Femoral shaft fracture in 265 children. Acta Orthop Scand 1988;59:704-707, with permission.) |
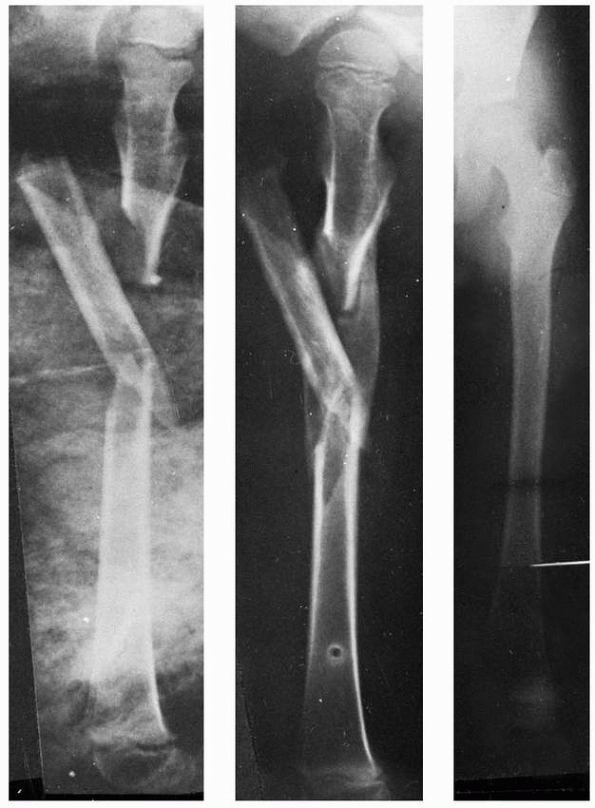 |
|
FIGURE 22-35 The effectiveness of remodeling of the femur in a child. Left:
Comminuted fracture in an 8-year-old child managed with a femoral pin incorporated in a spica cast. The midfragment is markedly angulated. Center: Fracture after union 12 weeks later with filling in of the defect and early absorption of the protruding fragment. Right: Appearance at age 12 with only a minimal degree of irregularity of the upper femur remaining. |
reported the use of external fixators in 11 open femoral fractures. The
time to union was delayed, but a satisfactory outcome occurred without
subsequent procedures. This supports the belief that the rates of
delayed union and nonunion are low in pediatric femoral fractures,
because open fractures would have the highest rates of delayed union.
the hip abductor musculature, quadriceps, and hamstrings, but
persistent weakness in some or all of these muscle groups seldom causes
a long-term functional problem. Hennrikus et al.88
found that quadriceps strength was decreased in 30% of his patients and
18% had a significant decrease demonstrated by a one-leg hop test.
Thigh atrophy of 1 cm was present in 42% of patients. These deficits
appeared to be primarily related to the degree of initial displacement
of the fracture. Finsen et al.61 found hamstring and quadriceps deficits in patients with femoral shaft fractures treated with either rods or plates.
found that hip abductor weakness was related to ipsilateral fracture
magnitude, long intramedullary rods, and, to a lesser degree,
heterotopic ossification from intramedullary rodding. Hedin and Larsson83
found no significant weakness in any of 31 patients treated with
external fixation for femoral fractures based on either Cybex testing
(Cybex International, Inc., Medway, MA) or a one-leg hop test. They
suggested that the weakness seen in other studies may be related to
prolonged immobilization.
time of femoral fracture, and long-term muscle deficits may persist in
some patients regardless of treatment. Severe scarring and contracture
of the quadriceps occasionally require quadricepsplasty.99
fracture, with hematogenous seeding of the hematoma and subsequent
osteomyelitis. Fever is commonly associated with femoral fractures
during the first week after injury,191
but persistent fever or fever that spikes exceedingly high may be an
indication of infection. One should have a high index of suspicion for
infection in type III open femoral fractures. A series of 44 open
femoral fractures98 reported no
infection in types I and II fractures, but a 50% (5 of 10) of type III
fractures developed osteomyelitis. Presumably, this occurs because of
the massive soft tissue damage accompanying this injury.
local wound care and antibiotic therapy. Occasionally, however, the
infections may lead to osteomyelitis of the femoral metaphysis or a
ring sequestrum that requires surgical débridement.
Vascular injury occurs most frequently with displaced Salter-Harris
physeal fractures of the distal femur and distal femoral metaphyseal
fractures. If arteriography indicates that vascular repair is necessary
after femoral shaft fracture, open reduction with internal fixation or
external fixation of the fracture is usually recommended first to
stablize the fracture and prevent injury of the repair. Secondary limb
ischemia also has been reported after the use of both skin and skeletal
traction. Documentation of peripheral pulses at the time of
presentation, as well as throughout treatment, is necessary.
children include those caused by direct trauma to the sciatic or
femoral nerve at the time of fracture and injuries to the peroneal
nerve during treatment. Weiss et al.209
reported peroneal nerve palsies in 4 of 110 children with femoral
fractures treated with early 90/90 hip spica casting. They recommended
extending the initial short-leg portion of the cast above the knee to
decrease tension on the peroneal nerve.
reported eight nerve palsies in 35 consecutive patients treated with
locked intramedullary rodding. The nerve injuries were associated with
delay in treatment, preoperative shortening, and boot traction.
Resolution occurred in less than 1 week in 6 of 8 patients.
shaft fractures will resolve with time. In infants, however, the
development of an early contracture of the Achilles tendon is more
likely. Because of the rapid growth in younger children, this
contracture can develop quite early; if peroneal nerve injury is
suspected, an ankle-foot orthosis should be used until the peroneal
nerve recovers. If peroneal, femoral, or sciatic nerve deficit is
present at initial evaluation of a closed fracture, no exploration is
indicated. If a nerve deficit occurs during reduction or treatment, the
nerve should be explored. Persistent nerve loss without recovery over a
4- to 6-month period is an indication for exploration.
but have been reported in patients with massive thigh swelling after
femoral fracture and in patients treated with intramedullary rod
fixation.144 If massive swelling of
thigh musculature occurs and pain is out of proportion to that expected
from a femoral fracture, compartment pressure measurements should be
obtained and decompression by fasciotomy should be considered. It is
probable that some patients with quadriceps fibrosis171 and quadriceps weakness43,196 after femoral fracture had intracompartmental pressure phenomenon. Mathews et al.132
reported two compartment syndromes in the “well leg” occurring when the
patient was positioned for femoral nailing in the hemilithotomy
position. Vascular insufficiency related to Bryant traction may produce
signs of compartment syndrome with muscle ischemia.38 Janzing et al.105
reported the occurrence of compartment syndrome when skin traction was
used for treatment of femoral fractures. Skin traction has been
associated with compartment syndrome in the lower leg in both the
fractured and nonfractured side. It is important to realize that in a
traumatized limb, circumferential traction needs to be monitored
closely and is contraindicated in the multiply injured or head-injured
child. As noted in the spica cast section, several cases of leg
compartment syndrome have been reported after spica cast treatment in
younger children with femoral fractures.
angulate into varus, and are more prone to overgrowth. These fractures
offer a challenge, as the bone available between the fracture site and
the femoral neck limits internal fixation options. In younger children,
traction and casting can be successful.50
Three weeks of traction is usually necessary. The cast should have a
good valgus mold at the fracture site, and the fracture should be
monitored closely in the first 2 weeks after casting. When the patient
returns for follow-up, if the subtrochanteric fracture has slipped into
varus malangulation, the cast can be wedged in clinic (Fig. 22-36)
or casting can be abandoned for another method. Parents should be
warned that loss of reduction in the cast is quite common, and wedging
in clinic is a routine step in management. An external fixation
strategy can be quite successful if there is satisfactory room
proximally to place pins. Once there is satisfactory callus (about 6
weeks), the fixator can be removed and weight bearing allowed in a
walking spica (long leg cast with a pelvic band and a valgus mold to
stabilize fracture in the first few weeks after external fixator
removal). Flexible nailing can be used, with a proximal and distal
entry strategy (Fig. 22-37). A pitfall in this
fracture is thinking that the proximal fragment appears too short to
use flexible intramedullary nails on the AP x-ray because the proximal
fragment is pulled into flexion by the unopposed psoas muscle. Pombo et
al.164 reported a series of 13
children, average 8 years old, with subtrochanteric fractures treated
with flexible nailing. Results were excellent or satisfactory in all
cases. Submuscular plating can also produce satisfactory results.103
In adolescents, there is insufficient experience with this fracture to
determine at what age intramedullary fixation with a
reconstruction-type nail and an angled transfixion screw into the
femoral neck is indicated. Antegrade intramedullary nail systems place
significant holes in the upper femoral neck and should be avoided.
Unlike subtrochanteric fractures in adults, nonunions are rare in
children with any treatment method.
and are difficult to treat because the gastrocnemius muscle inserts
just above the femoral condyles and pulls the distal fragment into a
position of extension (Fig. 22-38),75 making alignment difficult (see Fig. 22-3). The traditional methods of casting and single-pin traction may be satisfactory in
young children (Fig. 22-39).
As mentioned in the external fixation section, supracondylar fractures
through a benign lesion are safely and efficiently treated with a brief
period (4 to 6 weeks) of external fixation (Fig. 22-40),
followed by a walking cast until the callus is solid and the pin sites
are healed. In other cases, internal fixation is preferable, either
with submuscular plating (see Figs. 22-29 and 22-41)
and fully threaded cancellous screws (if there is sufficient
metaphyseal length) or with crossed smooth Kirschner-wires transfixing
the fracture from the epiphysis to the metaphysis, as described for
distal femoral physeal separations.181
If there is sufficient metaphyseal length, flexible nailing can be used
so long as fixation is satisfactory. The flexible nails can be placed
antegrade as originally described or retrograde if there is
satisfactory distal bone for fixation near the nail entry site.
Biomechanically, retrograde insertion is superior.140 Pathologic fractures in this area are common, and an underlying lesion should always be sought.
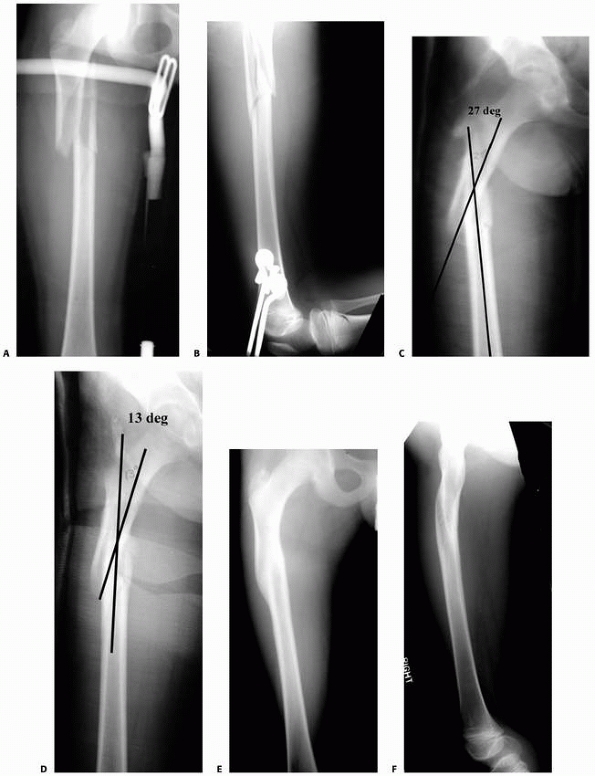 |
|
FIGURE 22-36 Comminuted spiral femur fracture in a 12-year-old treated with traction and casting. A.
This 12-year-old was struck by a car, sustaining this length-unstable proximal femur fracture. The family wanted nonoperative management. X-ray at presentation shows a subtrochanteric spiral fracture with an intact, large butterfly fragment. B. The fracture is out to length in traction. The traction pin was removed and a cast was placed about 3 weeks after injury. C. The child returns 1 week after casting (4 weeks after injury) with 27 degrees of proximal femoral varus angulation. D. The cast was wedged, correcting the deformity to 13 degrees, which was deemed acceptable. E,F. This AP and lateral view, 6 months after injury, shows quite satisfactory alignment. There was no significant limb-length inequality or deformity on physical examination. |
 |
|
FIGURE 22-37 A,B.
The combination of anterograde and retrograde titanium elastic nail insertion is a good solution for the proximal femur fracture. |
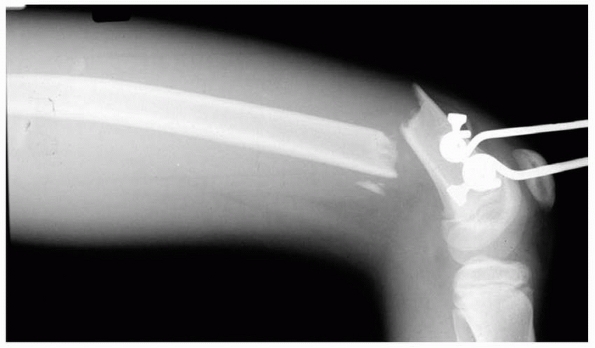 |
|
FIGURE 22-38 Treating distal femoral fractures in traction can be very difficult.
|
of the large soft tissue compartment around the femur. Proper wound
care, débridement, stabilization, and antibiotic therapy are required
to reduce the chance of infection.75 In a study by Hutchins et al.,98
70% of children with open femoral fractures had associated injuries and
90% were automobile related. The average time to healing was 17 weeks,
and 50% of the Gustillo type III injuries developed osteomyelitis.
simplifies wound care and allows early mobilization. The configuration
of the external fixator is determined by the child’s size and the
fracture pattern. Generally, monolateral half-pin frames are
satisfactory, but thin-wire circular frames may be necessary if bone
loss is extensive. External fixation provides good fracture control,
but, as always, family cooperation is required to manage pin and
fixator care.
as anatomic reduction of the femoral fracture. Wound care and treatment
of other injuries are made easier in children with multiple trauma.
However, this is an invasive technique with the potential for infection
and additional injury to the already traumatized soft tissues in the
area of the fracture. In emergency situations, plate fixation or
intramedullary fixation can be used for Gustillo-Anderson types I and
II fractures; type III fractures in older adolescents are better suited
for external fixation or intramedullary
nailing. Plate breakage can occur if bone grafting is not used for severe medial cortex comminution.
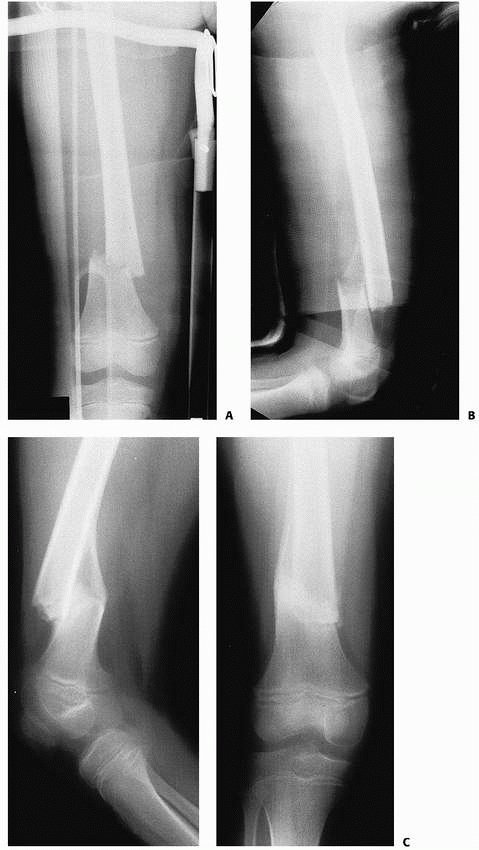 |
|
FIGURE 22-39 A. This 6-year-old patient sustained an unstable supracondylar fracture of the femur. B.
The fracture was managed with immediate spica casting with the knee in 90 degrees of flexion, mandatory in such a case to prevent posterior angulation. C. Bayonet apposition is acceptable in a child this age. |
trochanteric-entry nailing is often the optimal treatment choice.
Closed nailing after irrigation and drainage of the fracture allows
early mobilization and easy wound care in patients with
Gustillo-Anderson types I, II, IIIA, and IIIB injuries, but the risk of
osteonecrosis must be recognized.
potential for ambulation, surgical treatment with Rush, Bailey-Dubow,
or Fassier rods (see Chapter 6) is recommended
for repeated fractures or angular deformity. Cast immobilization is
minimized in patients with myelomeningocele or cerebral palsy because
of the frequency of osteoporosis and refracture in these
patients.
If possible, existing leg braces are modified for treatment of the
femoral fracture. In nonambulatory patients, a simple pillow splint is
used.
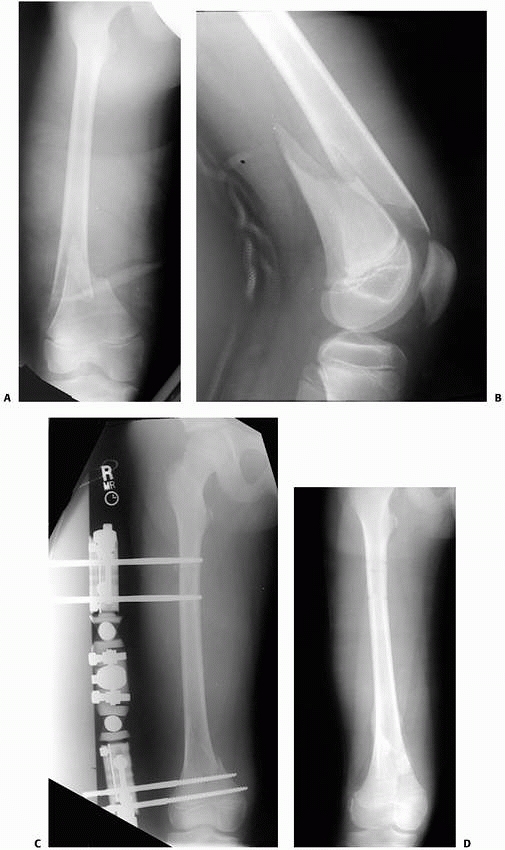 |
|
FIGURE 22-40 AP (A) and lateral (B) x-rays showing a fracture at the junction of the distal femoral metaphysis and diaphysis. C. The fractures reduced into near anatomic alignment, and an external fixator was used to control the distal fragment. D.
The fixator was removed 8 weeks after injury, and after a brief period of weight bearing is tolerated in a long leg cast, the fracture has healed in anatomic alignment with no shortening. |
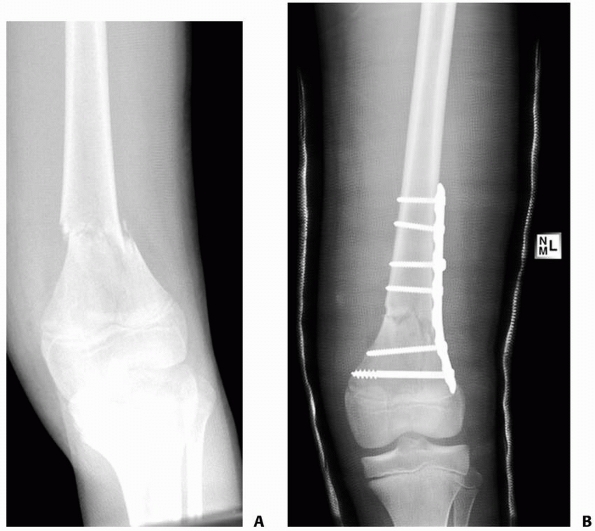 |
|
FIGURE 22-41 Preoperative (A) and postoperative (B) x-rays showing a fracture at the junction of the distal femoral metaphysis and diaphysis treated with plate fixation.
|
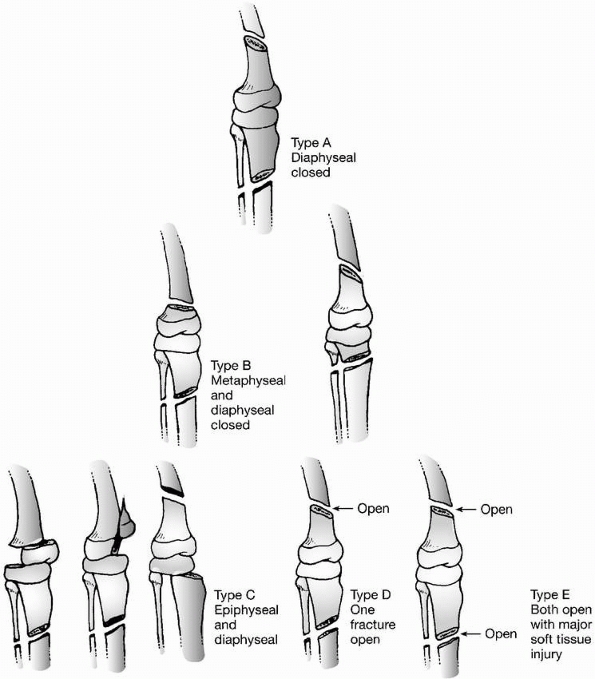 |
|
FIGURE 22-42
Classification of floating knee injuries in children. (From Letts M, Vincent N, Gouw G. The “floating knee” in children. J Bone Joint Surg Br 1986;68:442, with permission.) |
the femoral and tibial shafts leave the knee joint “floating” without
distal or proximal bony attachments. They are high-velocity injuries,
usually resulting from collision between a child pedestrian or cyclist
and a motor vehicle. Most children with floating knee injuries have
multiple-system trauma, including severe soft tissue damage, open
fractures, and head, chest, or abdominal injuries.
both fractures. If both fractures are open, external fixation of both
the tibial and femoral fractures may be appropriate. If immediate
mobilization is necessary, fixation of both fractures with external
fixation, intramedullary nails, compression plates, or any combination
of these may be indicated.
described five patterns of ipsilateral tibial and femoral fractures and
made treatment recommendations based on those patterns (Fig. 22-42). Because of the high prevalence of complications after closed treatment, Bohn and Durbin20 recommended open or closed reduction and internal fixation of the femoral fracture in older children. Arslan et al.7
evaluated the treatment of the “floating knee” in 29 consecutive cases,
finding that those treated operatively had a shorter hospital stay,
decreased time to weight bearing, and fewer complications than those
managed with splinting casting or traction. Arslan et al.7
demonstrated that open knee fracture rather than ligamentous injury was
a risk factor for poor outcome and that angulation was a predictor of
future compromise of function.
reported that of 19 patients with floating knee injuries, at long-term
follow-up 11 had limb-length discrepancy secondary to either overgrowth
of the bone after the fracture or premature closure of the ipsilateral
physis (7 patients), genu valgum associated with fracture of the
proximal tibial metaphysis (3 patients), or physeal arrest (1 patient).
Four patients had late diagnosis of ligamentous laxity of the knee that
required operation. Other complications included peroneal nerve palsy,
infection, nonunion, malunion, and refracture.
femoral fractures, the authors evaluated the effect of stabilization on
pulmonary function. Patients with severe head trauma or cervical spine
trauma are at greatest risk for pulmonary complications. Timing of
treatment of femoral fractures appears to not affect the prevalence of
pulmonary complications in children. Mendelson et al.141
similarly showed no effect of timing of femoral fixation on long-term
outcome, but early fracture fixation did decrease hospital stay without
increasing the risk of central nervous system or pulmonary
complications.
AP, Blackett CW, Cincotti JJ. Overgrowth of the femoral shaft following
fracture in childhood. J Bone Joint Surg Am 1939;21:334-338.
MC, Caglar O, Ayvaz M, et al. Treatment of complicated pediatric
femoral fractures with titanium elastic nail. J Pediatr Orthop B
2008;17(1):7-10.
M, Green WT. Lengths of the femur and the tibia: norms derived from
orthoroentgenograms of children from five years of age until epiphyseal
closure. Am J Dis Child 1948;75:279-290.
DD, Singer RM, Higgins RF. Skeletal traction for fractures of the
femoral shaft in children. A long-term study. J Bone Joint Surg Am
1987;69(9):1435-1439.
B, Christensen J. Fractures of the femoral shaft in children with
special reference to subsequent overgrowth. Acta Chir Scand
1959;116(3):235-250.
E, Sagiv S, Porat S. External fixation or flexible intramedullary
nailing for femoral shaft fractures in children. A prospective,
randomised study. J Bone Joint Surg Br 1997;79(6):975-978.
JH, Austin SM, Warner WC, et al. Interlocking intramedullary nailing of
femoral-shaft fractures in adolescents: preliminary results and
complications. J Pediatr Orthop 1994;14(2):178-183.
SK, Melder I, Henley MB, et al. Closed interlocking nailing of femoral
shaft fractures: assessment of technical complications and functional
outcomes by comparison of a prospective database with retrospective
review. J Orthop Trauma 1993;7(2): 118-122.
P, Ertresvag K, Hoiseth K. Torsion deformities after traction treatment
of femoral fractures in children. Acta Orthop Scand 1979;50(1):87-91.
M, Tornetta P, Kerina M, et al. Femur fractures caused by gunshots:
treatment by immediate reamed intramedullary nailing. J Trauma
1993;34(6):783-785.
P, Harvey EJ, Reindl R, et al. The locked flexible intramedullary
humerus nail in pediatric femur and tibia shaft fractures: a
feasibility study. J Pediatr Orthop 2004;24(6):634-637.
A, Jones DA, Daniel CL, et al. Assessment of hip abductor function in
relation to peritrochanteric heterotopic ossification after closed
femoral nailing. Injury 1993; 24(2):97-100.
LC, Loder RT, Hensinger RN. Role of intentional abuse in children 1 to
5 years old with isolated femoral shaft fractures. J Pediatr Orthop
1996;16(5):585-588.
WW, Durbin RA. Ipsilateral fractures of the femur and tibia in children
and adolescents. J Bone Joint Surg Am 1991;73(3):429-439.
L, Reinberg O, Lutz N. Femur fracture in preschool children: experience
with flexible intramedullary nailing in 72 children. J Pediatr Orthop
2007;27(3):299-303.
D. Fracture of the femoral shaft in children: advantages of the
descending medullary nailing. J Pediatr Orthop B 1996;5:110-114.
M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary
nailing of femoral shaft fractures. Measurement of anteversion angles
in 110 patients. J Bone Joint Surg Br 1993;75(5):799-803.
KJ, Molenaar JC, van Linge B. Rotational deformities after femoral
shaft fractures in childhood. A retrospective study 27-32 years after
the accident. Acta Orthop Scand 1981;52(1):81-89.
RJ, Ellison TS, Poka A, et al. Intramedullary nailing of femoral shaft
fractures: long term effects of static interlocking fixation. J Bone
Joint Surg Am 1922;74:106-112.
IM, Bolhuis HW, Broker FH, et al. Overgrowth and correction of
rotational deformity in 12 femoral shaft fractures in 3-6-year-old
children treated with an external fixator. Acta Orthop Scand
2002;73(2):170-174.
D Jr, Christensen K, Weatherall P. Intramedullary nailing of femoral
fractures in adolescents. Clin Orthop Relat Res 1998;350:85-89.
RT, Sutherland DH. Stress fracture of the femoral shaft in children:
report of two cases and discussion. J Pediatr Orthop 1984;4(5):614-616.
CD, Meek RN, Blachut PA, et al. Intramedullary nailing of the femoral
shaft: a prospective, randomized study. J Orthop Trauma
1992;6(4):448-451.
SR, Pool CJ. Traumatic separation of the proximal femoral epiphysis and
fracture of the mid-shaft of the ipsilateral femur in a child. A case
report and review of the literature. Injury 1983;15(3):156-158.
TP, Galpin RD. Flexible intramedullary nail fixation of pediatric
femoral fractures. Clin Orthop Relat Res 1996;332:110-118.
KD, Bynum J, Goucher N. Rates of refracture associated with external
fixation in pediatric femur fractures. Am J Orthop 2005;34(9):439-444;
discussion 444.
J, Gonzalez-Moran G, Albinana J. Femoral fractures in children from 4
years to 10 years: conservative treatment. J Pediatr Orthop B
2001;10(1):56-62.
EH, Young B, Vogt M, et al. Spica cast application in the emergency
room for select pediatric femur fractures. J Orthop Trauma
2005;19(10):709-716.
L, Fleisher G. Femoral fractures: are children at risk for significant
blood loss? Pediatr Emerg Care 1996;12(5):343-346.
C, Haley K, Hayes J, et al. The risk of child abuse in infants and
toddlers with lower extremity injuries. J Pediatr Surg
2005;40(1):120-123.
WH. Results of treatment of fractured femurs in children with special
reference to Bryant’s overhead traction. Arch Surg 1922;5:702-716.
PC, Bronskill SE, Hirji ZZ, et al. Economic evaluation of 2 treatments
for pediatric femoral shaft fractures. Clin Orthop Relat Res
1997;336:205-215.
DJ, Hennrikus WL. The treatment of pediatric femur fractures with early
90-90 spica casting. J Pediatr Orthop 1999;19(2):229-232.
B, Zdravkovic D. Quadriceps function following fractures of the femoral
shaft in children. Acta Orthop Scand 1974;45:756.
Sanctis N, Gambardella A, Pempinello C, et al. The use of external
fixators in femur fractures in children. J Pediatr Orthop
1996;16(5):613-620.
E, Kriz FK Jr. Slow arterial leak consequent to unrecognized arterial
laceration. Report of five cases. J Bone Joint Surg Am
1967;49(2):372-376.
JC, Clanton TO, Rockwood CA Jr. Closed treatment of subtrochanteric
fractures of the femur in a modified cast-brace. J Bone Joint Surg Am
1981;63(5):773-779.
BG, Sponseller PD, Ain M, et al. Comparison of dynamic versus static
external fixation for pediatric femur fractures. J Pediatr Orthop
2002;22(4):428-430.
P, Syversen SM. Overgrowth of the femur after fracture of the shaft in
childhood. J Bone Joint Surg Br 1976;58(3):339-342.
Hayek T, Daher AA, Meouchy W, et al. External fixators in the treatment
of fractures in children. J Pediatr Orthop B 2004;13(2):103-109.
HR, Molenaar E, O’Connor D P. Immediate single-leg spica cast for
pediatric femoral diaphysis fractures. J Pediatr Orthop
2006;26(4):491-496.
OT, Kucukkaya M, Kockesen C, et al. Open reduction and plate fixation
of femoral shaft fractures in children aged 4 to 10. J Pediatr Orthop
2003;23(2):190-193.
M, Strong ML, MacIntosh R. External fixation maintained until fracture
consolidation in the skeletally immature. J Pediatr Orthop
1993;13(1):98-101.
LH, Pankovich AM, Spero CM, et al. Closed flexible intramedullary
nailing of adolescent femoral shaft fractures. J Orthop Trauma
1989;3(2):133-141.
JM, Hresko T, Reynolds RA, et al. Titanium elastic nails for pediatric
femur fractures: a multicenter study of early results with analysis of
complications. J Pediatr Orthop 2001;21(1):4-8.
JM, Luedtke LM, Ganley TJ, et al. Comparison of titanium elastic nails
with traction and a spica cast to treat femoral fractures in children.
J Bone Joint Surg Am 2004;86-A(4):770-777.
KB, Mahar AT, Lee SS, et al. Biomechanical analysis of antegrade and
retrograde flexible intramedullary nail fixation of pediatric femoral
fractures using a synthetic bone model. J Pediatr Orthop
2004;24:167-171.
I, Sturm PF, Robertson WW Jr. Compression-plate fixation of femoral
shaft fractures in children aged 8 to 12 years. J Pediatr Orthop
1999;19(5):578-581.
JE, Swenning TA, Burd TA, et al. Proximal femoral radiographic changes
after lateral transtrochanteric intramedullary nail placement in
children. J Bone Joint Surg Am 2003;85-A(7):1295-1301.
P, Pevny T, Teague D. Early complications with external fixation of
pediatric femoral shaft fractures. J Orthop Trauma 1996;10(3):191-198.
P, Sullivan JA, Herndon WA. Adolescent femoral shaft fractures: rigid
versus flexible nails. Orthopedics 1995;18(7):645-649.
PP, Green WT. Fractures of the shaft of the femur in children:
treatment and results. Orthop Clin North Am 1972;3(1):213-224.
RH, Davidson R, Sullivan JA, et al. Cast brace management of the
femoral shaft fracture in children and young adults. J Pediatr Orthop
1983;3(5):572-582.
RH, Stranger M. Causative factors responsible for femoral fractures in
infants and young children. J Pediatr Orthop 1983;3(3):341-343.
DT, Olney BW, Dart BR, et al. Rotational control of various pediatric
femur fractures stabilized with titanium elastic intramedullary nails.
J Pediatr Orthop 2004; 24(2):172-177.
G, Hansson LI, Norman O. Correction by growth of rotational deformity
after femoral fracture in children. Acta Orthop Scand
1983;54(6):858-861.
PD, Bicknell HR Jr, Bronson WE, et al. The use of one compared with two
distal screws in the treatment of femoral shaft fractures with
interlocking intramedullary nailing. A clinical and biomechanical
analysis. J Bone Joint Surg Am 1993;75(4): 519-525.
TB. Fractures of the femoral shaft in children treated with an
AO-compression plate. Report of 12 cases followed until adulthood. Acta
Orthop Scand 1992;63(1): 50-52.
H, Borgquist L, Larsson S. A cost analysis of three methods of treating
femoral shaft fractures in children: a comparison of traction in
hospital, traction in hospital/home and external fixation. Acta Orthop
Scand 2004;75(3):241-248.
H, Larsson S. Muscle strength in children treated for displaced femoral
fractures by external fixation: 31 patients compared with 31 matched
controls. Acta Orthop Scand. 2003;74(3):305-311.
SD, Drvaric DM, Darr K, et al. The operative stabilization of pediatric
diaphyseal femur fractures with flexible intramedullary nails: a
prospective analysis. J Pediatr Orthop 1994;14(4):501-507.
SD, Drvaric D, Darr K, et al. Stabilization of pediatric diaphyseal
femur fractures with flexible intramedullary nails (a technique paper).
J Orthop Trauma 1992; 6(4):452-459.
J, Goldacre MJ, Fairweather JM, et al. Conditions accounting for
substantial time spent in hospital in children aged 1-14 years. Arch
Dis Child 1992;67(1):83-86.
WL, Kasser JR, Rand F, et al. The function of the quadriceps muscle
after a fracture of the femur in patients who are less than seventeen
years old. J Bone Joint Surg Am 1993;75(4):508-513.
WA, Mahnken RF, Yngve DA, et al. Management of femoral shaft fractures
in the adolescent. J Pediatr Orthop 1989;9(1):29-32.
D Jr, Scott DM, Behrens F, et al. The use of Ender nails in femoral
shaft fractures: what are the remaining indications? J Orthop Trauma
1992;6(3):314-317.
RY, Lincoln A, Crockett MM, et al. Fractures of the femoral shaft in
children. Incidence, mechanisms, and sociodemographic risk factors. J
Bone Joint Surg Am 1999; 81(4):500-509.
CA, Skaggs DL, Tang CW, et al. Use of flexible intramedullary nails in
pediatric femur fractures. J Pediatr Orthop 2006;26(4):497-504.
MT, Kasser JR. Physeal arrest about the knee associated with
non-physeal fractures in the lower extremity. J Bone Joint Surg Am
1989;71(5):698-703.
BF, Sponseller PD, Thompson JD. Pediatric femur fractures: effects of
spica cast treatment on family and community. J Pediatr Orthop
1995;15(4):457-460.
JB, Sanderson PL, Rickman M, et al. External fixation of children’s
fractures: use of the Orthofix Dynamic Axial Fixator. J Pediatr Orthop
B 1997;6(3):203-206.
FW, Eyring EJ. Proximal tibial 90-90 traction in treatment of children
with femoral-shaft fractures. J Bone Joint Surg Am 1969;51(3):499-504.
CM, Sponseller PD, Sturm P, et al. Open femur fractures in children:
treatment, complications, and results. J Pediatr Orthop
2000;20(2):183-188.
R 2nd, Rodgers WB, Hresko MT, et al. Femur fractures in children:
treatment with early sitting spica casting. J Pediatr Orthop
1998;18(4):481-487.
AF Jr, Albert MC, Jennings WB, et al. Immediate hip spica casting for
femur fractures in pediatric patients. A review of 175 patients. Clin
Orthop Relat Res 2000; 376:106-112.
RN, Nicholson JT, Chung SM. Long-term results in the treatment of
femoral-shaft fractures in young children by immediate spica
immobilization. J Bone Joint Surg Am 1976;58(7):945-951.
J, Louis DS, Costenbader JM. Arterial injury associated with closed
femoral-shaft fracture. Report of five cases. J Bone Joint Surg Am
1975;57(8):1147-1150.
H, Broos P, Rommens P. Compartment syndrome as a complication of skin
traction in children with femoral fractures. J Trauma
1996;41(1):156-158.
AW, Weiss CB Jr, Wheeler DL. Stress fractures of the femoral shaft in
athletes—more common than expected. A new clinical test. Am J Sports
Med 1994;22(2): 248-256.
AD, Yiannakopoulos CK, Soucacos PN. Closed, locked intramedullary
nailing of pediatric femoral shaft fractures through the tip of the
greater trochanter. J Trauma 2006;60(1):217-222; discussion 222-213.
EM, Anglen JO, Smith DG, et al. Advantages of submuscular bridge
plating for complex pediatric femur fractures. Clin Orthop Relat Res
2004;426:244-251.
M, Lehman WB, Grant AD, et al. Avascular necrosis of the femoral head
as sequela of fracture of the greater trochanter. A case report and
review of the literature. Clin Orthop Relat Res 1993;294:193-195.
RM, Winquist RA, Hansen ST Jr. Femoral shaft fractures in adolescents:
a comparison between traction plus cast treatment and closed
intramedullary nailing. J Pediatr Orthop 1981;1(2):193-197.
PJ, Song KM, Routt ML Jr, et al. Plate fixation of femoral shaft
fractures in multiply injured children. J Bone Joint Surg Am
1993;75(12):1774-1780.
C, Haas N, Walker J, et al. Treatment of femoral shaft fractures in
children by external fixation. Injury 1991;22(4):263-266.
LA. Fracture patterns in children: analysis of 8,682 fractures with
special reference to incidence, etiology and secular changes in a
Swedish urban population 1950-1979. Acta Orthop Scand Suppl
1983;202:1-109.
TM, Frick SL. Compartment syndrome of the leg after treatment of a
femoral fracture with an early sitting spica cast. A report of two
cases. J Bone Joint Surg Am 2003;85-A(11):2207-2210.
P, Haumont T, Journeau P. Use and abuse of flexible intramedullary
nailing in children and adolescents. J Pediatr Orthop
2006;26(6):827-834.
SS, Mahar AT, Newton PO. Ender nail fixation of pediatric femur
fractures: a biomechanical analysis. J Pediatr Orthop
2001;21(4):442-445.
JN, Metaizeau JP, Prevot J, et al. Elastic stable intramedullary
nailing of femoral shaft fractures in children. J Bone Joint Surg Br
1988;70(1):74-77.
RT, O’Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur
fractures in children. J Pediatr Orthop 2006;26(5):561-566.
SJ, Schootman M, Schoenecker PL, et al. Complications of titanium
elastic nails for pediatric femoral shaft fractures. J Pediatr Orthop
2003;23(4):443-447.
H, Shannak A, Hadidi S. Remodeling after femoral shaft fractures in
children treated by the modified blount method. J Pediatr Orthop
1986;6(4):421-429.
DC, Weddington J, Davenport K. Closed Ender nailing of femoral shaft
fractures in adolescents. J Pediatr Orthop 1986;6(6):651-655.
JI, Sanchis-Alfonso V, Gomar-Sancho F, et al. Kuntscher nailing of
femoral shaft fractures in children and adolescents. Int Orthop
1993;17(3):158-161.
PV, Perry JJ, Murray PC. Compartment syndrome of the well leg as a
result of the hemilithotomy position: a report of two cases and review
of literature. J Orthop Trauma 2001;15(8):580-583.
EG, Smith EL, Wilson A, et al. External fixation of pediatric femur
fractures with cortical contact. Am J Orthop 2006;35(11):498-501.
K, Khairouni A, Pennecot GF, et al. Closed flexible intramedullary
nailing of the femoral shaft fractures in children. J Pediatr Orthop B
1997;6(3):198-202.
RE. A method for early spica cast application in treatment of pediatric
femoral shaft fractures. J Pediatr Orthop 1986;6(1):89-91.
NC 3rd, Vinsant JE Jr, Sarmiento A. Functional fracture-bracing of
longbone fractures of the lower extremity in children. J Bone Joint
Surg Am 1978;60(3): 314-319.
JJ, Gregory SK. Ender nails: an alternative for intramedullary fixation
of femoral shaft fractures in children and adolescents. South Med J
1997;90(7):694-696.
RA. Overgrowth of the femur following fractures in children: influence
of handedness. J Bone Joint Surg Am 1979;61(3):381-384.
CT, Nemeth NM, Glos DL. Antegrade versus retrograde titanium elastic
nail fixation of pediatric distal-third femoral-shaft fractures: a
mechanical study. J Orthop Trauma 2006;20(9):608-612.
SA, Dominick TS, Tyler-Kabara E, et al. Early versus late femoral
fracture stabilization in multiply injured pediatric patients with
closed head injury. J Pediatr Orthop 2001;21(5):594-599.
RA, Garvin KL, Huurman WW. Avascular necrosis of the femoral head after
closed intramedullary shortening in an adolescent. J Pediatr Orthop
1995;15(1):24-26.
ME, Bramlett KW, Kissell EU, et al. Improved treatment of femoral shaft
fractures in children. The “pontoon” 90-90 spica cast. Clin Orthop
Relat Res 1987;219:140-146.
N, Stevens P, Smith J, et al. Intramedullary nailing of femoral
fractures in adolescents. J Pediatr Orthop 2000;20(4):482-484.
LA, Launay F, Kocher MS, et al. Titanium elastic nailing of fractures
of the femur in children. Predictors of complications and poor outcome.
J Bone Joint Surg Br 2006;88(10):1361-1366.
S, Cassidy N, Stephens M, et al. Birth-associated femoral fractures:
incidence and outcome. J Pediatr Orthop 2002;22(1):27-30.
S, Humphrey M, Corrales LA, et al. Retention of flexible intramedullary
nails following treatment of pediatric femur fractures. Arch Orthop
Trauma Surg 2007; 127(7):509-514.
SJ, Frick S, Sink E, et al. Volkmann contracture and compartment
syndromes after femur fractures in children treated with 90/90 spica
casts. J Pediatr Orthop 2006; 26(5):567-572.
UG, Hyman JE, Wainwright AM, et al. Complications of elastic stable
intramedullary nail fixation of pediatric femoral fractures, and how to
avoid them. J Pediatr Orthop 2004;24(4):363-369.
PO, Mubarak SJ. Financial aspects of femoral shaft fracture treatment
in children and adolescents. J Pediatr Orthop 1994;14(4):508-512.
JT, Foster RM, Heath RD. Bryant’s traction; a provocative cause of
circulatory complications. J Am Med Assoc 1955;157(5):415-418.
DE Jr, Asselmeier M, Pinzur MS. Torsional malunion of a femur fracture:
diagnosis and treatment. Orthop Rev 1990;19(7):625-629.
SE, Hoffinger SA. Skeletal traction versus external fixation for
pediatric femoral shaft fractures: a comparison of hospital costs and
charges. J Orthop Trauma 1998; 12(8):563-568.
PJ, Turen CH, Brumback RJ, et al. Conversion of external fixation to
intramedullary nailing for fractures of the shaft of the femur in
multiply injured patients. J Bone Joint Surg Am 2000;82(6):781-788.
J. Degree and frequency of rotational deformities after infant femoral
fractures and their spontaneous correction. Arch Orthop Trauma Surg
1980;97(4): 249-255.
DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated
with intramedullary nailing in an adolescent. J Pediatr Orthop
1995;15(1):21-23.
RF, DiCicco J, Lakatos R, et al. Retrograde intramedullary nailing of
femoral diaphyseal fractures. J Orthop Trauma 1998;12(7):464-468.
HM, Yensel U, Senaran H, et al. Immediate percutaneous intramedullary
fixation and functional bracing for the treatment of pediatric femoral
shaft fracture. J Pediatr Orthop 2003;23(4):453-457.
DA, Mooney JF 3rd, Cramer KE, et al. Comparison of Pavlik harness
application and immediate spica casting for femur fractures in infants.
J Pediatr Orthop 2004; 24(5):460-462.
MW, Shilt JS. The definition and treatment of pediatric subtrochanteric
femur fractures with titanium elastic nails. J Pediatr Orthop
2006;26(3):364-370.
S, Milgrom C, Nyska M, et al. Femoral fracture treatment in
head-injured children: use of external fixation. J Trauma
1986;26(1):81-84.
R, Lindsey RW, Hadley NA, et al. Refracture of adolescent femoral shaft
fractures: a complication of external fixation. A report of two cases.
J Pediatr Orthop 1993;13(1): 102-105.
EM, Ogden JA, Grogan DP. Premature greater trochanteric epiphysiodesis
secondary to intramedullary femoral rodding. J Pediatr Orthop
1993;13(4):516-520.
KE, Riccio AI, De La Garza D. Stainless steel flexible intramedullary
fixation of unstable femoral shaft fractures in children. J Pediatr
Orthop 2007;27(4):432-441.
RB, Ballard RI, Hughes JL. Internal fixation versus traction and
casting of adolescent femoral shaft fractures. J Pediatr Orthop
1990;10(5):592-595.
WM, Bellabarba C, Evanoff B, et al. Retrograde versus antegrade nailing
of femoral shaft fractures. J Orthop Trauma 2001;15(3):161-169.
KD, Sturm PF, Rosenbaum D, et al. Neurologic complications of pediatric
femoral nailing. J Pediatr Orthop 1996;16(5):606-612.
RS, Mendelson SA, Grudziak JS. Acute synovitis of the knee resulting
from intra-articular knee penetration as a complication of flexible
intramedullary nailing of pediatric femur fractures: report of two
cases. J Pediatr Orthop 2003;23(5):635-638.
JJ, Gaspar MR, Gjerdrum TC, et al. Vascular injuries associated with
fractures of the femur. Arch Surg 1975;110(5):494-499.
SR, Muller U, Gautier E, et al. The evolution of femoral shaft plating
technique. Clin Orthop Relat Res 1998;354:195-208.
PT, Chapman JR, Selznick HS, et al. Iatrogenic fractures of the femoral
neck during closed nailing of the femoral shaft. J Bone Joint Surg Br
1994;76(2):293-296.
EL, Gralla J, Repine M. Complications of pediatric femur fractures
treated with titanium elastic nails: a comparison of fracture types. J
Pediatr Orthop 2005;25(5): 577-580.
EL, Hedequist D, Morgan SJ, et al. Results and technique of unstable
pediatric femoral fractures treated with submuscular bridge plating. J
Pediatr Orthop 2006; 26(2):177-181.
DL, Leet AI, Money MD, et al. Secondary fractures associated with
external fixation in pediatric femur fractures. J Pediatr Orthop
1999;19(5):582-586.
J, Schoenecker PL, Gordon JE. External fixation of femoral shaft
fractures in children: enhanced stability with the use of an auxiliary
pin. J Pediatr Orthop 1999;19(5): 587-591.
JP, Christensen KP, Wilkins KE. Femur fractures in infants: a new
therapeutic approach. J Pediatr Orthop 1995;15(4):461-466.
AA, Morrissy RT, Renwick SE. Femoral shaft fracture treatment in
patients age 6 to 16 years. J Pediatr Orthop 1999;19(2):222-228.
JG, Lamdan R. Osteonecrosis of the femoral head after intramedullary
nailing of a fracture of the femoral shaft in an adolescent. A case
report. J Bone Joint Surg Am 1995;77(9):1423-1426.
JD, Buehler KC, Sponseller PD, et al. Shortening in femoral shaft
fractures in children treated with spica cast. Clin Orthop Relat Res
1997;338:74-78.
SA, Mahoney LJ. Volkmann’s ischaemic contracture and its relationship
to fracture of the femur. J Bone Joint Surg Br 1951;33-B(3):336-347.
A, Goshen E, Katz M, et al. Bilateral femoral stress fractures in a
child due to in-line (roller) skating. Acta Paediatr 1997;86(3):332-333.
DR, Hoffinger S. Intramedullary nailing of femoral shaft fractures in
children via the trochanter tip. Clin Orthop Relat Res 2000;376:113-118.
ED. Inequality of the lower extremities following fracture of the shaft
of the femur in children. Ann Surg 1921;74(4):498-500.
CT Jr, DeCampos J, Merritt PO, et al. Meniscal injury associated with
femoral shaft fractures. An arthroscopic evaluation of incidence. J
Bone Joint Surg Br 1993; 75(2):207-209.
Meter JW, Branick RI. Bilateral genu recurvatum after skeletal
traction. A case report. J Bone Joint Surg Am 1980;62(5):837-839.
HO. Does rotation deformity, following femur shaft fracture, correct
during growth? Reconstr Surg Traumatol 1979;17:75-81.
EJ, Jain V, Vora V, et al. Complications of titanium and stainless
steel elastic nail fixation of pediatric femoral fractures. J Bone
Joint Surg Am 2008;90(6):1305-1313.
ME, Hoffman EB. Remodelling of angular deformity after femoral shaft
fractures in children. J Bone Joint Surg Br 1992;74(5):765-769.
AP, Schenck RC Jr, Sponseller PD, et al. Peroneal nerve palsy after
early cast application for femoral fractures in children. J Pediatr
Orthop 1992;12(1):25-28.
RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral
fractures. A report of five hundred and twenty cases. J Bone Joint Surg
Am 1984;66(4): 529-539.
JG. The treatment of femoral shaft fractures in children: a systematic
overview and critical appraisal of the literature. Can J Surg
2000;43(3):180-189.
