Ultrasound Guided Lumbar Plexus Blocks
anterior rami of the L1 through L4 roots (and sometimes T12 or L5). The
lumbar plexus forms the subcostal, iliohypogastric, ilioinguinal,
lateral femoral cutaneous, genitofemoral, femoral, and obturator
nerves. Anatomic dissections have revealed that the lumbar plexus lies
within the psoas muscle, with the lateral femoral cutaneous nerve and
femoral nerve in the same fascial plane. However, the obturator nerve
can be found within a distinct muscular fold in about half of anatomic
specimens. The lumbosacral trunk is formed from the anterior rami of L4
and L5. It contributes to the sacral plexus and enters the pelvis apart
from the lumbar plexus.
 |
|
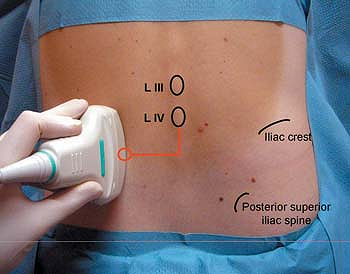
Figure 37-1.
External photograph illustrating the position of the ultrasound transducer for imaging of the lumbar transverse processes and the puncture location. |
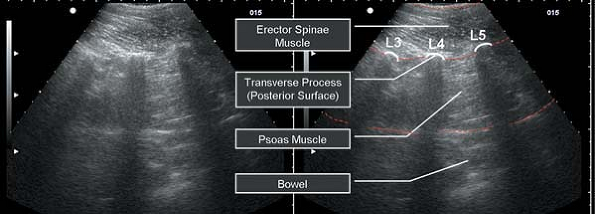
Controversy surrounds the use of ultrasound imaging to guide lumbar
plexus block. Some authors have argued that because current ultrasound
imaging does not provide direct lumbar plexus imaging in adults,
alternative methods for block guidance such as loss-of-resistance or
nerve stimulation are necessary. Other authors have used ultrasound
imaging for lumbar plexus blocks in pediatric patients where more
favorable imaging is possible. In our own clinical practice, we have
reserved the use of ultrasound for offline imaging of surrogate
landmarks of the lumbar plexus in adult patients. The usual level of
the block procedure is the intertransverse space between L4 and L5. The
best method of localization has been achieved by counting the
transverse process echoes from the sacrum upward and marking their
location with indelible ink (Fig. 37-2).
The lumbar plexus is approximately 2 cm deep to the transverse process
of L4 off its caudal edge (median value 18 mm for adults of either
gender). The lumbar nerve roots that contribute to the lumbar plexus
lie 5 to 6 mm deep to the intertransverse ligament. With the offline
technique
(scanning
prior to needle insertion), nerve stimulation is often used to confirm
correct location of the block needle tip prior to injection. Scanning
prior to offline needle insertion may be especially useful in obese
patients or those with spinal deformities.
 |
|
Figure 37-2.
Longitudinal sonogram of the intertransverse spaces from L3 to L5 with a 3 MHz transducer. Between the bright reflections of the posterior surface of the transverse process the psoas muscle and underlying bowel can be seen. |
AT, Collins AB, Schafhalter-Zoppoth I. An introduction to femoral nerve
and associated lumbar plexus nerve blocks under ultrasonic guidance. Tech Reg Anesth Pain Man 2004;8:155–163.
L, Enna B, Mitterschiffthaler G, et al. Lumbar plexus in children. A
sonographic study and its relevance to pediatric regional anesthesia. Anesthesiology 2004;101:445–450.
L, Entner T, Wissel J, et al. A study of the paravertebral anatomy for
ultrasound-guided posterior lumbar plexus block. Anesth Analg 2001;93:477–481.
