IMAGING MODALITIES IN ORTHOPAEDICS
new imaging modalities have significantly improved our capabilities for
diagnosing orthopaedic conditions. Although conventional radiography
remains the primary diagnostic tool, ancillary techniques are used to
characterize the abnormality more accurately, to predict possible
complications, and to monitor postoperative recovery. The newer imaging
modalities, however, are expensive (e.g., magnetic resonance imaging,
or MRI), may expose the patient to radiation (e.g., computed
tomography, or CT), and are frequently employed unnecessarily or
inappropriately.
of current imaging modalities, and sets guidelines for choosing
particular modalities. Time and cost considerations should discourage
redundant studies. The surgeon familiar with these techniques can
confidently order the least number of tests necessary to dictate a
course of therapy.
concerned about which modality they should use for a particular
problem. Although there are numerous algorithms for evaluating various
problems at different anatomic sites, the answer cannot always be
succinctly stated (22). The choice of techniques for imaging bone and soft-tissue
abnormalities is dictated by the clinical presentation, equipment
availability, expertise, cost, and restrictions referable to individual
patients. For example, allergy to ionic or nonionic iodinated contrast
agents may preclude the use of arthrography; the presence of a
pacemaker may preclude the use of MRI; and physiologic states such as
pregnancy may preclude the use of ionized radiation, favoring instead
sonography.
film must be available for comparison. The choice of imaging technique
is usually dictated by the type of suspected abnormality. If
osteonecrosis is suspected, for example, and the radiographs are
normal, the physician should proceed immediately to MRI examination,
the most sensitive modality. It can detect necrotic changes in bone
long before plain films, tomography, CT, or scintigraphy can provide
positive evidence.
obtain plain films first; if the abnormality is not obvious, proceed
with MRI, because this modality provides an exquisite contrast
resolution of the bone marrow, articular cartilage, ligaments, menisci,
and soft tissues. In evaluating rotator cuff abnormalities,
particularly partial or complete tears, arthrography and MRI are
currently the most effective procedures. Although ultrasound can also
detect rotator cuff tears, because of its low sensitivity (68%) and low
specificity (75% to 84%) it is seldom used as the definitive diagnostic
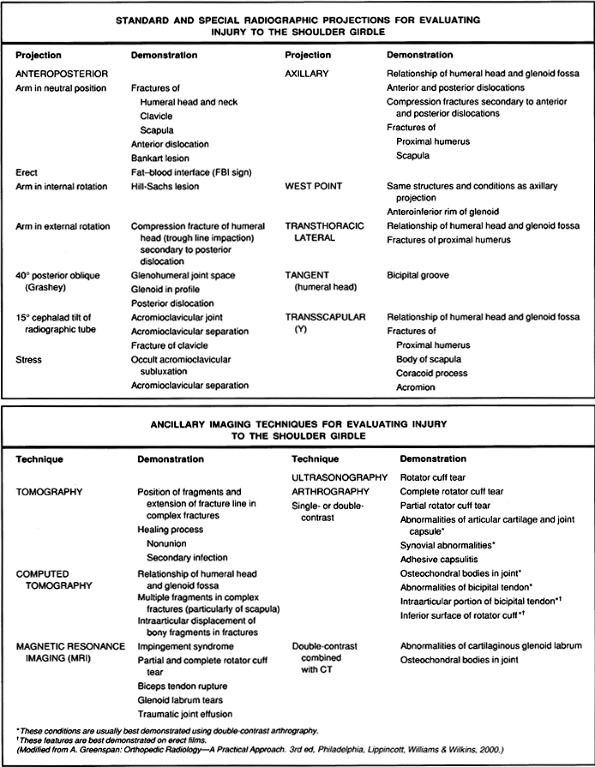
procedure (9,36,60). Figure 4.1
depicts the gamut of standard and special radiographic projections and
various ancillary imaging techniques currently available for evaluating
injury of the shoulder girdle.
 |
|
Figure 4.1. Standard, special, and ancillary imaging techniques used to evaluate injury to the shoulder girdle.
|
radiographs and trispiral tomography before proceeding to
arthrotomography or CT-arthrography. In this case, MRI is a less
desirable technique, because it is less sensitive and specific than
CT-arthrotomography in detecting abnormalities of the triangular
fibrocartilage and various intercarpal ligaments, particularly if
three-compartment injection is used (40,41).
If one suspects carpal tunnel syndrome, however, MRI is preferred
because it provides inherent high-contrast differences among muscles,
tendons, and ligaments. Similarly, if osteonecrosis of the carpal bones
is suspected and the plain films are normal, MRI is the preferred
method. In evaluating fractures and fracture healing of carpal bones,
trispiral tomography is still the procedure of choice because it gives
a high degree of spatial resolution.
tomography are still the gold standard for diagnostic purposes. To
evaluate intraosseous and soft-tissue extension of tumor, however, use
CT or the more accurate MRI. In evaluating results of treatment of
malignant tumors by radiotherapy and chemotherapy, dynamic MRI using
gadolinium diethylenetriamine penta-acetic acid (Gd-DTPA) for contrast
enhancement is much superior to scintigraphy, CT, or even plain MRI.
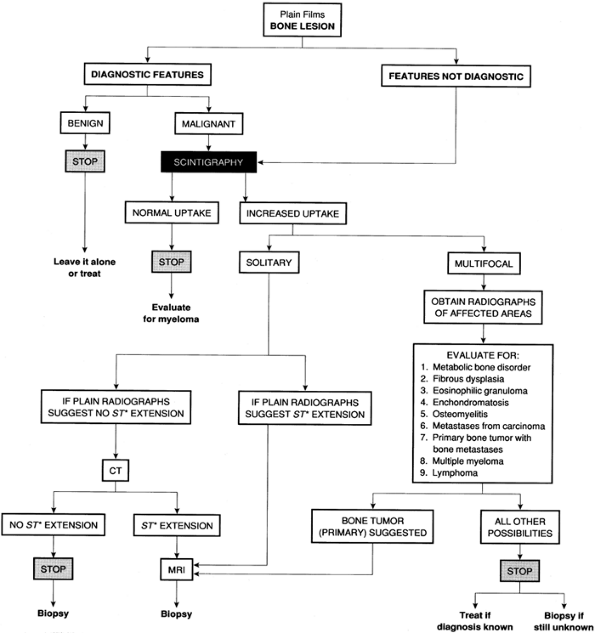
helpful in evaluating bone lesions discovered on standard radiographs.
Notice that the proper order for employing various imaging modalities
depends on two factors: whether the plain film findings are diagnostic
for any particular tumor, and the lesion’s uptake of a tracer on the
bone scan. Scintigraphy plays a crucial role in dictating the use of
different techniques. The use of CT or MRI may depend on the features
found on conventional radiographs. If there is no evidence of
soft-tissue extension, CT is superior to MRI for detecting subtle
cortical erosions and periosteal reaction, and it provides an excellent
means to determine the intraosseous extension of the tumor. If,
however, the radiographs suggest cortical destruction and a soft-tissue
mass, MRI is the preferred modality because it provides exquisite
soft-tissue contrast and can determine the extraosseous extension of
the tumor better than CT can.
 |
|
Figure 4.2. Algorithmic evaluation of bone lesion discovered on the standard radiographs. *ST, soft tissue.
|
and joint disorders, particularly traumatic conditions, is conventional
radiography. Obtain at least two views of the involved bone at 90°
angles to each other, with each view including the two joints adjacent
to the injured bone; this decreases the risk of missing an associated
fracture, subluxation, or dislocation at a site remote from the
apparent primary injury. In children, it is frequently necessary to
obtain a radiograph of the normal, unaffected limb for comparison. The
standard films usually comprise the anteroposterior and lateral views;
occasionally, oblique and special views are necessary, particularly in
the evaluation of fractures of complex structures, such as the elbow,
wrist, ankle, and pelvis. A weight-bearing view may be of value for
dynamic evaluation of the joint space during weight bearing.
glenoid to be seen in profile. To obtain this view, place the patient
in a 40° posterior oblique position with the central beam directed
toward the glenohumeral joint. The film in this projection shows the
glenoid in true profile, and the glenohumeral joint space is clearly
visible. This is particularly effective in demonstrating suspected
posterior dislocation (4).
Point view may be similarly effective. To obtain this view, position
the patient prone on the radiographic table, and place a pillow under
the affected shoulder to raise it about 8 cm. Position the film
cassette against the superior aspect of the shoulder. Angle the
radiographic tube toward the axilla at 25° to the patient’s midline and
25° to the table’s surface. On the film in this projection, the
relationship of the humeral head and the glenoid can be evaluated as
well as it can be evaluated on the axillary view, but the
anteroinferior glenoid rim, which is seen tangentially, is better
visualized.
special low-kilovoltage technique with the central beam directed 15°
cephalad toward the clavicle. Reduce exposure factors to about 33% to
50% of those used in obtaining the standard anteroposterior view of the
shoulder. The film in this projection shows the acromial end of the
clavicle, acromion, and acromioclavicular joint (4).
is very effective for evaluation of the scapula. Have the patient stand
erect, with the injured side against the raised radiographic table.
Rotate the trunk about 20° from the table to allow separation of the
two shoulders. Slightly abducted the arm on the injured side and flex
the elbow, with the hand resting on the ipsilateral hip. Direct the
central beam toward the medial border of the protruding scapula. The
film in this projection provides a true lateral view of the scapula as
well as an oblique view of the proximal humerus.
elbow joint. It is a variant of the lateral projection that overcomes
the major limitation of the standard lateral view by projecting the
radial head ventrad, free of overlap by the coronoid process (Fig. 4.3).
It has proved to be a particularly effective technique to demonstrate
the capitellum, the coronoid process, and the humeroradial and
humeroulnar articulations (32).
 |
|
Figure 4.3.
A special 45° angle view of the elbow projects the radial head ventrad, free of the overlap of coronoid process. The capitellum is also well demonstrated. |
hand and the wrist (i.e., the “allstate” or ball-catcher’s view)
effectively demonstrates the radial aspects of the metacarpal heads and
the base of the proximal phalanges in the hand and the triquetrum and
pisiform bones in the wrist (10).
patella known as the Merchant view is helpful in evaluating the
patellofemoral joint. This view is particularly effective in detecting
subtle subluxations of the patella (46).
radiographic table, with the knee flexed about 45° at the table’s edge.
A device keeping the knee at this angle also holds the film cassette.
Direct the central beam caudally through the patella at a 60° angle
from the vertical. On the film in this projection, the articular facets
of the patella and femur are well demonstrated.
projections to demonstrate the details of the subtalar joint. To
demonstrate the posterior and middle facets of this joint, use the
posterior tangential view (i.e., the Harris-Beath). To demonstrate the
posterior facet, talofibular joint, and tibiofibular syndesmosis, use
the Broden view (Fig. 4.4) (4).
 |
|
Figure 4.4.
A special view of the ankle obtained at 30° cephalad angulation (Broden view) demonstrates the posterior facet of the subtalar joint, talofibular joint, tibiofibular syndesmosis, and sustentaculum tali. |
odontoid process if its upper half is not clearly shown on the
open-mouth view (4). For this view, position the patient supine on the radiographic table, with the neck hyperextended.
Direct the central beam vertically to the neck just below the tip of
the chin. The radiograph obtained in this projection clearly reveals
the odontoid, especially its upper half.
enhance the bony details not well delineated on the standard
radiographic projections. This technique involves a special screen–film
system and geometric enlargement that yields magnified images of the
bones and joints with increased sharpness and bony detail (28).
The technique is particularly effective for demonstrating early changes
in some arthritides and metabolic disorders. It may be useful for
demonstrating subtle fracture lines not seen on routine projections.
ligamentous tears and joint stability. In the hand, obtain
abduction-stress film of the thumb if gamekeeper’s thumb, resulting
from disruption of the ulnar collateral ligament of the first
metacarpophalangeal joint, is suspected. In the lower extremity, the
stress views of the knee and ankle joints are frequently obtained.
Evaluation of knee instability due to ligament injuries may require
this technique in cases of suspected tear of the medial collateral
ligament, and less frequently for evaluating insufficiency of the
anterior and posterior cruciate ligaments.
of the medial collateral ligament, position the patient supine with the
knee flexed about 15° to 20°. With the thigh fixed, apply pressure
against the medial aspect of the leg below the knee, forcing the knee
into valgus. The films thus obtained show the anteroposterior
projection. To obtain a stress film of the knee joint for evaluation of
the anterior cruciate ligament, position the patient on his side, with
the knee flexed 90°. Apply pressure against the posterior aspect of the
upper leg (anterior-drawer stress). The films show the lateral
projection.
stress films are most frequently obtained; only rarely is an eversion
(abduction) stress examination required. To obtain an inversion stress
film of the ankle joint, position the patient supine with the lower leg
fixed, and apply pressure on the lateral aspect of the foot, adducting
the heel and forcing the foot into varus position. For anterior-drawer
stress examination, position the patienton her side with the lower leg
fixed, and apply posterior stress to the heel. The films show the
lateral projection.
 |
|
Figure 4.5.
The anteroposterior view of the ankle after application of inversion stress shows widening of the lateral compartment of the ankle joint, indicating a tear of the lateral collateral ligament. |
of limb lengths. This technique requires a slit-beam diaphragm with a
1.5 mm opening attached to the radiographic tube, and a long film
cassette. The radiographic tube can move in the long axis of the
radiographic table. During the exposure, the tube traverses the whole
length of the film, scanning the entire extremity. This technique
allows the x-ray beam to intersect the bone ends perpendicularly, and
limb lengths can be compared (4,52).
A modified technique may be used with three separate exposures over the
hip joints, knees, and ankles if a motorized radiographic tube is not
available. In this technique, an opaque tape measure is placed
longitudinally down the center of the radiographic table (4).
indicated. For this technique, position the patient supine with the
lower limbs on a 3-ft-long cassette and a long ruler at one side. Make
a single exposure, centered at the knees and including the entire
length of both limbs and the ruler.
radiologic procedures, including arthrography, tenography, bursography,
arteriography, and percutaneous bone or soft-tissue biopsy. Fluoroscopy
combined with videotaping is useful in the evaluation of the kinematics
of joints. Because it delivers a high dose of radiation, it is used
only occasionally (e.g., in evaluating joint movement and detecting
transient subluxation). It occasionally is used in follow-up
examination of the healing process after fractures to evaluate the
degree of bone union. Fluoroscopy is still used in conjunction with
myelography if it is important
-
to observe the movement of the contrast column in the subarachnoid space,
-
to check proper placement of the needle and monitor the flow of contrast medium,
-
to assess intraoperatively the reduction of a fracture or the placement of hardware.
image acquisition using an x-ray detector. The detector comprises a
photostimulable phosphor imaging plate and image reader/writer that
processes the latent image information for laser printing on film. A
major advantage of computed radiography over conventional film and
screen radiography is that, once acquired, the digital image data are
readily manipulated to produce alternative renderings. In addition,
energy subtraction imaging may be acquired: Two images, acquired either
sequentially or simultaneously with different filtration, are used to
reconstruct a soft tissue–only image or a bone-only image.
and a digital disk added to a fluoroscopy imaging system to provide
on-line viewing of subtraction images (23).
This technique is most widely used to evaluate the vascular system; it
is occasionally used in conjunction with arthrography. Use of
high-performance video cameras with low-noise characteristics allows a
single video frame of precontrast and postcontrast images to be used
for subtraction. Spatial resolution can be maximized using a
combination of geometric magnification, electric magnification, and a
small anode-to-target distance. The subtraction technique removes
surrounding anatomic structures and isolates the opacified vessel or
joint, making it more conspicuous.
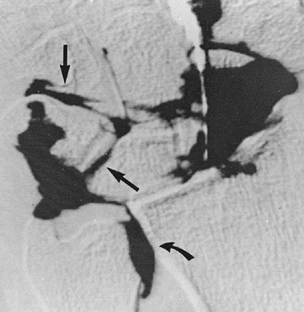
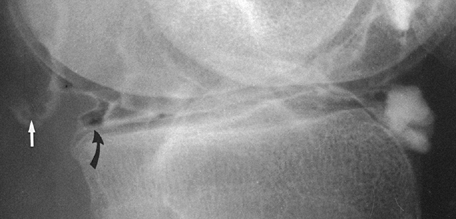
abnormalities and, in conjunction with contrast injection (i.e.,
digital arthrography), to evaluate subtle abnormalities of the joints,
such as tears of the lunate-triquetral ligament or the abnormalities of
the triangular fibrocartilage in the wrist (Fig. 4.6).
Use it also to evaluate the stability of a prosthesis. Digital
radiography offers improved image quality, contrast sensitivity, and
exposure latitude. It is also an efficient mode in which to store,
retrieve, and transmit radiographic image data. Digital images can be
displayed on film or on a monitor. A significant advantage of image
digitization is its ability to produce data with low noise and a wide
dynamic range. Image digitization is suitable for window-level analysis
in a manner comparable to that employed in a CT scanner (56).
 |
|
Figure 4.6. Digital subtraction wrist arthrogram demonstrates a leak of contrast into the proximal intercarpal articulation (arrows) through the perforation in the lunate-triquetral ligament. Notice a leak of contrast into the distal radioulnar joint (curved arrow), indicating a tear of the triangular fibrocartilage complex. (Courtesy of BJ Manaster, MD, Salt Lake City, UT.)
|
frequently used variant of digital radiography, to evaluate trauma and
tumors of the bone and soft tissue, and to view the vascular system. In
trauma to the extremity, DSA is effectively used to evaluate arterial
occlusion, pseudoaneurysms, arteriovenous fistulas, and transection of
the arteries (30). The advantage of DSA over
conventional film techniques is the rapidity of the study with the
ability to obtain multiple repeated projections. Bone subtraction is
useful in clearly delineating the vascular structures. In evaluating
bone and soft-tissue tumors, DSA is an effective tool for mapping tumor
vascularity.
visualization of lesions too small to be seen on conventional
radiographs. It is also effective for demonstrating anatomic detail
that is obscured by overlying structures. It employs continuous motion
of the radiographic tube and film cassette in opposite directions
throughout exposure, with the fulcrum of the motion located in the
plane of interest. The technique blurs structures above and below the
area being examined, thereby sharply outlining the object to be studied
on a single plane of focus. The newly developed tomographic units can
better localize the image and can detect lesions as small as 1 mm in
diameter.
radiographic tube and film cassette moving on a straight line in
opposite directions. This linear movement has little application in the
study of bones because it creates streaks that often interfere with
radiologic interpretation. Resolution of the plane of focus, much
clearer if there is uniform blurring of undesired structures, requires
a multidirectional movement, as in zonography or circular tomography.
In this type of tomography, the radiographic tube makes one circular
motion at a preset angle of inclination. More complex multidirectional
hypocycloidal or trispiral movements increase the distance of excursion
of the tube and create a varying angle of projection of the x-ray beam
during exposure. These complex movements are advantageous because they
produce even greater blurring outside the field of interest and yield
the sharpest focal plane images.
It is also useful in evaluating tumor and tumorlike lesions (e.g., the
nidus of an osteoid osteoma, a calcific matrix in an enchondroma or
chondrosarcoma). Small cystic and sclerotic lesions and subtle erosions
are well demonstrated. Tomograms are better interpreted with plain
radiographs for comparison.
 |
|
Figure 4.7. Trispiral tomography obtained in the carpal tunnel projection demonstrates a fracture of the hook of the hamate (arrows).
|
evaluation of many traumatic conditions and various bone and
soft-tissue tumors because of its cross-sectional imaging capability.
In trauma, CT is extremely useful because of its abilities to define
the presence and extent of fracture or dislocation, to evaluate such
intra-articular abnormalities as damage to the articular cartilage or
presence of noncalcified and calcified osteocartilaginous bodies, and
to evaluate adjacent soft tissues. CT is important in the detection of
small bony fragments displaced into the joints after trauma, in the
detection of the small displaced fragments of the fractured vertebral
body (Fig. 4.8), and in the assessment of concomitant injury to the cord or thecal sac (14).
 |
|
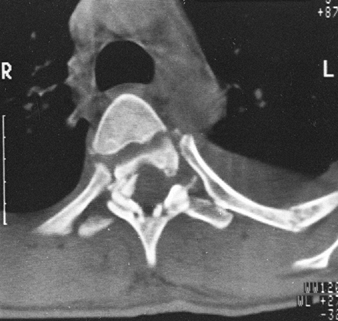
Figure 4.8.
CT section through the level of T3 accurately demonstrates the comminuted fracture of the vertebral body and laminae. Notice small bony fragment encroaching on the spinal cord. |
measurement of the tissue attenuation coefficient, and direct
transaxial images. Another advantage is its ability to image the bone
in coronal, sagittal, and oblique planes, using reformation technique.
This multiplanar reconstruction is particularly helpful in evaluating
vertebral alignment (Fig. 4.9),
demonstrating horizontally oriented fractures of the vertebral body,
and evaluating complex fractures of the pelvis or calcaneus,
abnormalities of the sacrum and sacroiliac joints, sternum,
sternoclavicular joints, temporomandibular joints, and wrist.
 |
|
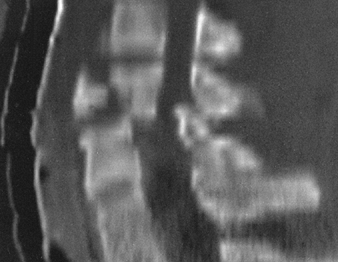
Figure 4.9.
Sagittal CT reconstructed image effectively shows the flexion tear-drop fracture of C5. Malalignment of the vertebral bodies and narrowing of the spinal canal are well demonstrated. |
only at the tissue layer under investigation. Recently developed spiral
(helical) scanning permits three-dimensional reconstruction for
analysis of regions with complex anatomy, such as the face, pelvis,
vertebral column, wrist, foot, and ankle (Fig. 4.10) (11,27,42).
The CT data may be used to create three-dimensional plastic models of
the area of interest, which can facilitate operative planning and allow
rehearsal of complex reconstructive procedures.
 |
|
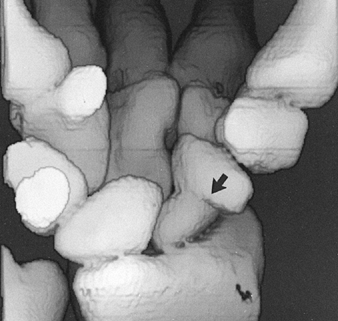
Figure 4.10. Three-dimensional CT reconstruction of the wrist demonstrates a nonunited fracture of the scaphoid (arrow) complicated by osteonecrosis of the proximal fragment.
|
specific diagnosis of bone and soft-tissue tumors, it can provide a
precise evaluation of the extent of the bone lesion and may demonstrate
a break through the cortex and the involvement of surrounding soft
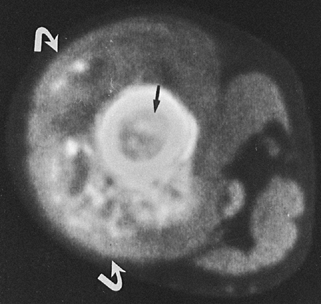
tissues (Fig. 4.11). Moreover, CT is helpful
for delineating a tumor in bones having complex anatomic structures,
such as the scapula, pelvis, and sacrum, which may be difficult to
image fully with conventional radiographic techniques or even
conventional tomography. CT examination is crucial in determining the
extent and spread of a tumor in the bone and surrounding soft tissues
if limb salvage is contemplated, allowing a safe margin of resection to
be planned. It is also useful for monitoring the results of treatment
and evaluating recurrence of resected tumor.
 |
|
Figure 4.11. CT section through the proximal thigh of a patient with osteosarcoma of the femur. The tumor involves the bone marrow (arrow) and is breaking through the cortex, producing a large soft-tissue mass (curved arrows).
|
successful aspiration or biopsy of bone or soft-tissue lesions because
it provides visual guidance for precise placement of biopsy needles
within the lesion.
coefficients of each pixel provides a basis for accurate quantitative
bone mineral analysis in cancellous and cortical bone (8,26).
Evaluation of bone mass measurement underscores continuing progress in
our understanding of bone metabolism and provides valuable insight into
improvement of evaluation and treatment of osteoporosis and other
metabolic bone disorders (55).
effect, which results from insufficient resolution to describe
inhomogeneities of the tissue. Because of this, the Hounsfield’s units
represent average values of the different components of the tissue.
This effect becomes particularly important if normal and pathologic
processes interface within a section under investigation.
characterization. Despite the ability of CT to discriminate some
density differences, a simple analysis of attenuation values does not
permit precise histologic characterization. Moreover, if the patient
moves at all, the result is artifacts that degrade the image quality.
Similarly, metal (e.g., prosthesis, rods, screws) produces significant
artifacts. Finally, the radiation dose may occasionally be high,
particularly if contiguous and overlapping sections are obtained during
an examination.
contrast refers to air. Despite the evolution of newer diagnostic
imaging modalities, such as CT and MRI, arthrography has retained its
importance in daily radiologic practice (25). Arthrography is technically simple, and interpretation is much easier than interpretation of ultrasound, CT, or MRI (33).
Although virtually every joint can be injected with contrast,
arthrography is most frequently performed in the shoulder, wrist,
ankle, and elbow.
arthrographic procedure, because contrast may obscure some joint
abnormalities (e.g., osteochondral body) that can be easily detected on
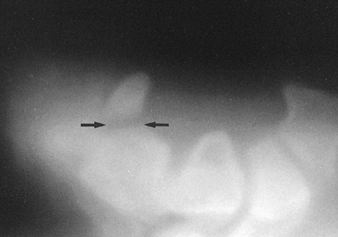
the plain film. Arthrography is particularly effective in demonstrating
rotator cuff tear (Fig. 4.12) and adhesive
capsulitis in the shoulder, osteochondritis dissecans, osteochondral
bodies, and subtle abnormalities of the articular cartilage in the
elbow joint. In the wrist, it is still a very effective procedure for
evaluating abnormalities of the triangular fibrocartilage complex (53).
The introduction of three-compartment injection techniques combined
with digital technique and postarthrographic CT examination has made
this modality almost always the procedure of choice in evaluating a
painful wrist (40).
 |
|
Figure 4.12.
After injection of contrast agent into the shoulder joint, there is opacification of the subacromial-subdeltoid bursae complex (arrow), indicating a rotator cuff tear. |
completely replaced by MRI, it still may be used to demonstrate
injuries to the soft-tissue structures, such as the joint capsule,
menisci, and various ligaments (Fig. 4.13).
It also provides important information on the status of the articular
cartilage, particularly if the surgeon suspects subtle chondral or
osteochondral fracture or requires confirmation of osteochondral bodies
(e.g., osteochondritis dissecans).
 |
|
Figure 4.13. Double-contrast arthrogram of the knee demonstrates a bucket-handle tear of the posterior horn of medial meniscus (curved arrow) and a popliteal cyst (straight arrow).
|
combined with tomography (i.e., arthrotomography), with CT (i.e.,
arthro-CT), or with digitization of an image (i.e., digital subtraction
arthrography) to provide additional information (Fig. 4.6) (43).
arthrography. Even hypersensitivity to iodine is only a relative
contraindication, because a single contrast study using only air can be
performed.
tendon sheath to evaluate the integrity of a tendon, in a procedure
known as a tenogram. CT and MRI have superseded this procedure, but it
is still used, mainly to evaluate traumatic or inflammatory condition
of tendons of the lower extremity, such as peroneus longus and brevis (Fig. 4.14),
tibialis anterior and posterior, and flexor digitorum longus, and to
outline the synovial sheaths within the carpal tunnel in the upper
extremity.
 |
|
Figure 4.14.
Tenogram demonstrates irregular accumulation of the contrast in the proximal portion of the sheath of the peroneus brevis tendon (arrow), indicating tenosynovitis. Notice the normal appearance of the tendon of the peroneus longus (open arrow). |
into bursae. This procedure has mostly been abandoned, and only
occasionally the subacromial-subdeltoid bursae complex is directly
injected with contrast agent to demonstrate partial tears of the
rotator cuff.
arteries and films are obtained, usually in a rapid sequence. In
venography, contrast is injected into the veins. The technique is used
most frequently to detect vascular trauma.
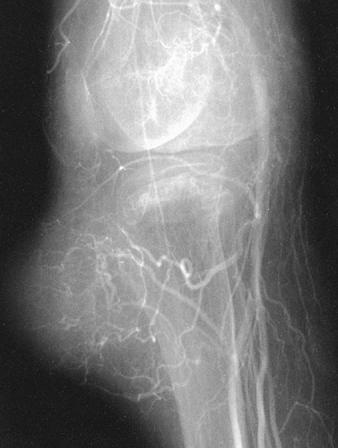
map bone lesions, to demonstrate the vascularity of the lesion, and to
assess the extent of disease (Fig. 4.15). It is
also used to demonstrate the vascular supply of a tumor and to locate
vessels suitable for preoperative intraarterial chemotherapy. It is
useful in demonstrating the area suitable for open biopsy, because most
vascular parts of a tumor contain the most aggressive component of the
lesion. Occasionally, arteriography can be used to demonstrate abnormal
tumor vessels, corroborating findings with plain film radiography and
tomography. Arteriography is often extremely helpful in planning
limb-salvage procedures by demonstrating the regional vascular anatomy
and permitting a plan to be drawn for the resection procedure. It is
sometimes used to outline the major vessels before resection of a
benign tumor. It can be combined with an interventional procedure, such
as embolization of hypervascular tumors, before surgery. It also plays
a major role in assessing the effectiveness of chemotherapy in the
treatment of malignant bone and soft-tissue tumors.
 |
|
Figure 4.15. Femoral arteriogram demonstrates feeding vessels and vascularity of a large paratibial liposarcoma.
|
injected into the subarachnoid space, mixing freely with the cerebral
spinal fluid to produce a column of opacified fluid with a higher
specific gravity than the clear fluid. Tilting the patient allows the
opacified fluid to run up or down the thecal sac under the influence of
gravity. The puncture usually is done in the lumbar area, at L2–L3 or
L3–L4 levels. For examination of the cervical area, a C1–C2 puncture is
performed. Myelographic examination has been almost completely replaced
by high-resolution CT and high-quality MRI.
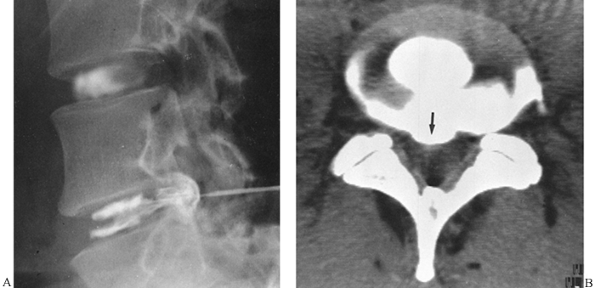
the nucleus pulposus. Although many surgeons have abandoned the use of
this controversial procedure, under tightly restricted indications and
immaculate technique a discogram can yield valuable information (29,59).
Discography is a valuable aid for determining the source of a patient’s
low-back pain. It is not a pure imaging technique, because the symptoms
produced during the test (e.g., pain during the injection) are
considered to have even greater diagnostic value than the radiographs
obtained (66). Always combine it with CT examination (Fig. 4.16).
According to the official position statement on discography by the
Executive Committee of the North American Spine Society in 1988, this
procedure “is indicated in the evaluation of patients with unremitting
spinal pain, with or without extremity pain, of greater than 4 months
duration, when the pain has been unresponsive to all appropriate
methods of conservative therapy” (21).
According to the same statement, before discography is performed, the
patient should have undergone investigation with other modalities
(e.g., CT, MRI, myelography), and surgical correction of the patient’s
problem should be anticipated.
 |
|
Figure 4.16. A: Discogram demonstrates herniation of the nucleus pulposus at the L4–L5 level. Normal disc is outlined at the L3–L4 interspace. B: CT scan at the L4–L5 level after discography confirms the posterior central disc herniation (arrow).
|
on the interaction of propagated sound waves with tissue interfaces in
the body. Whenever the directed pulsing of sound waves encounters an
interface between tissues of different acoustic impedance, reflection
or refraction occurs, which is then recorded with a sensitive
transducer
and
converted into images. An advantage of this technique is that, because
it does not use ionized radiation, it is safe to use on pregnant women
and infants. Modern probe technology, development of real-time imaging,
and color Doppler imaging have extended to some degree the use of
ultrasound in orthopaedic radiology. Higher-frequency transducers of
7.5 and 10 MHz have excellent spatial resolution and are ideal for
imaging of the appendicular skeleton. Some applications of ultrasound
in orthopaedics include evaluation of the rotator cuff and injured
tendons (e.g., Achilles tendon) (7,24,60,64). Ultrasound is occasionally used during surgery to assess reduction of spinal fractures (65). It is also used to image soft-tissue tumors (e.g., hemangioma) (15).
evaluation of the infant hip. In this case, ultrasound has become the
imaging modality of choice, because of the hip’s cartilaginous
composition, ultrasound’s real-time capability for studying motion and
stress, the absence of ionizing radiation, and the relative cost
effectiveness. The newest development in this area is the introduction
of three-dimensional ultrasound for evaluation of developmental
dysplasia of the hip. Three-dimensional sonography provides functional
utility in the evaluation of the joint in the added sagittal plane
(section image) and craniocaudal projection (revolving spatial image).
This technique permits excellent demonstration of the femoral
head–ace-tabulum relationship and femoral head containment.
rheumatic disorders, in particular to differentiation of popliteal
fossa masses (e.g., aneurysm, Baker’s cyst, hypertrophied synovium).
More recent ultrasound techniques such as Doppler ultrasound or
colorflow imaging, which expresses motion from moving red blood cells
in color, have found limited applications in orthopaedic radiology.
This modality is used mainly to detect arterial narrowing and venous
thrombosis. Also, there have been a limited number of reports regarding
the use of this technology in measuring tumor vascularity within soft
tissue masses.
(i.e., radionuclide bone scan) over all other imaging techniques is its
ability to image the entire skeleton at once. A bone scan can confirm
the presence of the disease, demonstrate the distribution of a lesion (Fig. 4.17),
and help to evaluate the activity of a pathologic process. Indications
for skeletal scintigraphy include traumatic conditions, tumors (primary
and metastatic), arthritides, infections, and metabolic bone disease.
The detected abnormality may consist of decreased uptake of
bone-seeking radiopharmaceutical (e.g., early stage of osteonecrosis)
or increased uptake (e.g., fracture, neoplasm, focus of osteomyelitis).
Some
structures under normal conditions may show increased activity (e.g., sacroiliac joints or normal growth plates).
 |
|
Figure 4.17.
Bone scan obtained after injection of 15 mCi of technetium-99m methylene diphosphonate demonstrates increased uptake of the radiopharmaceutical at the site of multiple rib fractures. The increased uptake at the level of L1 is secondary to the compression fracture of the vertebral body (arrows). |
lacks specificity. It is impossible to differentiate between various
processes that can cause increased uptake. Occasionally, however, the
bone scan may yield very specific information and even suggest the
diagnosis, as in multiple myeloma or osteoid osteoma. In the search for
myeloma, scintigraphy is helpful for differentiating bony metastases.
In most cases of myeloma, there is no significant increase in the
uptake of the radiopharmaceutical; in skeletal metastases, however,
invariably the uptake of the tracer is significantly elevated. In
osteoid osteoma, there is a typical appearance of the bone scan that
demonstrates a “double-density sign.” There is more increased uptake in
the center, due to the nidus, and less increased uptake at the
periphery, related to the reactive sclerosis surrounding the nidus.
turnover; because there is usually an enhanced deposition of
bone-seeking radiopharmaceuticals in areas of bone undergoing change
and repair, a bone scan is useful in localizing tumors and tumor-like
lesions in the skeleton. This is particularly helpful in fibrous
dysplasia, eosinophilic granuloma, or metastatic cancer, in which more
than one lesion develop. It also plays an important role in localizing
small lesions, such as osteoid osteoma, which may not always be seen on
the plain film studies. In most instances, radionuclide bone scan
cannot differentiate benign lesions from malignant tumors, because both
conditions have an increased blood flow with resultant increased
isotope deposition and increased osteoblastic activity. It may,
however, permit differentiation of benign lesions, such as bone
islands, that usually do not absorb the radioactive isotope.
helpful in the early diagnosis of stress fractures, which may not be
seen on conventional radiographs or tomographic studies. It also has
value in diagnosing fractures of the scaphoid or the femoral neck in
elderly patients if the routine radiographic examinations appear normal
(13,39).
helpful in establishing the extent of skeletal involvement in Paget’s
disease and assessing the response to treatment. Although it is of no
use in the evaluation of patients with generalized osteoporosis, it may
occasionally be helpful in differentiating osteoporosis from
osteomalacia and in differentiating multiple vertebral fractures
resulting from osteoporosis from those occurring in metastatic
carcinoma.
leukocytes accumulate in active bone marrow, and this tendency limits
their sensitivity for the detection of chronic osteomyelitis. To
improve the diagnostic ability of this technique, some advocate a study
that combines 99mTc-sulfur colloid bone marrow with 111In-labeled leukocytes. In chronic osteomyelitis, imaging with 67gallium (67Ga) citrate is more accurate in detecting the response or lack of response to treatment than 99mTc-phosphate
bone imaging. A three-phase technique can be effectively used to
differentiate soft-tissue infection (cellulitis) and osseous infection
(osteomyelitis).
metastasis is probably the most common indication for skeletal
scintigraphy. It also is frequently used to determine the extent of a
lesion or the presence of skip lesions or intraosseous metastases. It
is not the method of choice to determine the extent of the lesion in
the bone. Scintigraphy alone cannot diagnose the type of the tumor, but
it may
be useful in detecting and localizing some primary tumors and multifocal lesions (e.g., multicentric osteosarcoma).
determine whether a lesion is monostotic or polyostotic, information
essential in the staging of a bone tumor. Although the degree of
abnormal uptake may be related to the aggressiveness of the lesion,
this finding does not correlate well with histologic grade. Gallium-67
may be taken up in a soft-tissue sarcoma and may help to differentiate
a sarcoma from a benign soft-tissue lesion.
extent of the primary malignant tumor in bone, it is not as accurate as
CT or MRI. It may be useful in the detection of local recurrence of
tumor and occasionally may indicate the response or lack of response to
radiotherapy or chemotherapy.
demonstrate the distribution of the lesion in the skeleton; this method
has completely replaced the previously used radiographic joint survey.
Scintigraphy can determine the distribution of arthritic changes in
large and small joints and in areas usually not detected by standard
radiography, such as the sternomanubrial and temporomandibular joints (38).
radionuclide imaging. The radiopharmaceuticals currently in use in bone
scanning include the organic diphosphonates, ethylene diphosphonates,
methylene diphosphonates (MDP), and methane hydroxydiphosphonates, all
labeled with 99mTc, a pure gamma-ray emitter with a 6-hour
half-life. MDP is more frequently used, particularly in adults,
typically in a dose that provides 15 mCi of 99mTc
radiation. After intravenous injection of the radiopharmaceutical,
approximately 50% of the dose localizes in bone. The remainder
circulates freely in the body and eventually is excreted by the kidneys.
three-phase isotope bone scan. The first phase, the radionuclide
angiogram, is the first minute after injection, when the serial images
demonstrate the radioactive tracer in the major blood vessels. In the
second phase, the blood-pool scan, which lasts from 1 to 3 minutes
after injection, isotope is detected in the vascular system and in the
extracellular space in the soft tissues before being taken up by bone.
The third phase, or static bone scan, usually occurs 2 to 3 hours after
injection and discloses the presence of radiopharmaceutical in the
bone. This phase may be divided into two stages. In the first stage,
the isotope diffuses passively through the bone capillaries. In the
second stage, the radionuclide is concentrated in bone. The most
intense localization occurs in the first and second phases in areas
with increased blood flow and in the third phase in areas with
increased osteogenic activity, increased calcium metabolism, and active
bone turnover.
for abscess detection varies from 58% to 100% and specificity from 75%
to 99%. The images are usually obtained 6 and 24 hours after the
injection of 5 mCi of this radiopharmaceutical. These images have been
shown to be extremely accurate in monitoring response to therapy of
chronic osteomyelitis and infectious arthritis. The changing activity
of 67Ga uptake parallels the patient’s clinical course in septic arthritis more closely than the images obtained after injection of 99mTc-diphosphonate. A gallium scan is also used to differentiate sarcomas from benign soft-tissue lesions.
oxine-labeled leukocytes over other bone-seeking radiopharmaceuticals
for detecting inflammatory abnormalities in the skeletal system (45). Because 111In-labeled
leukocytes are not usually incorporated into areas of increased bone
turnover, indium imaging presumably reflects inflammatory activity
only, and early experience has shown it to be specific in the detection
of abscesses or acute infectious processes, including osteomyelitis and
septic arthritis. The sensitivity varies from 75% to 90%, and
specificity is approximately 91% (57).
False-negative results often occurred for patients with chronic
infections in which there was reduced inflow of circulating leukocytes.
False-positive results were seen for patients who had an inflammatory
process without infection (e.g., rheumatoid arthritis mistaken for
septic arthritis).
of human serum albumin were tried as a bone marrow imaging agent. About
86% of these particles are 30 nm or smaller, and the remainder are
between 30 and 80 nm. When this “nanocolloid” is used for detection of
osteomyelitis in the extremities, it has a sensitivity equal to that of
111In-leukocytes.
characteristic, nonuniform distribution of administered
radiopharmaceutical tracers. Imaging the distributions yields
information about the functional status of bony tissues. A perfect
image of such an object would be an exact, three-dimensional replica of
the distribution of activity within
the area of interest (6).
This goal has been partially achieved through the tomoscanner and dual
Anger-type scintillation cameras operated in the conjugate counting
mode, or single photon emission computed tomography (SPECT).
tomography (SPET) and SPECT has tremendously increased diagnostic
precision in evaluating bone and joint abnormalities. The efficiency of
instrumentation for SPECT is improving with multiple crystal detectors,
fan beam and cone beam collimators, detection of a greater fraction of
photons, and improved algorithms. Compared with planar images, SPECT
provides increased contrast resolution, using a tomographic mode that
eliminates the noise from tissue outside the plane of imaging; in this
regard, it is similar to conventional tomography. It provides
quantitative and qualitative information on the uptake of bone-seeking
radiopharmaceuticals.
an absorbed radiofrequency signal while the patient is in a strong
magnetic field (31). An external magnetic field
is usually generated by a magnet with field strengths of 0.2 to 1.5
tesla. The system includes a magnet, radiofrequency coils (transmitter
and receiver), gradient coils, and a computer display unit with digital
storage facilities.
intrinsic spin of atomic nuclei with an odd number of protons or
neutrons (e.g., hydrogen), which generates a magnetic moment. Nuclei of
tissues placed within the main magnetic field tend to align along the
direction of that field. Application of radiofrequency (rf) pulses
induces resonance of particular sets of nuclei. The required frequency
of the pulse is determined by the strength of the magnetic field and
the nucleus under investigation. The energy absorbed during the
transition from the induced high-energy state to the normal low-energy
state is released; this can be recorded as an electrical signal, which
provides the data from which digital images are derived (58).
relaxation time is a term used to describe the return of protons to
equilibrium after application and removal of the rf pulse. T2
relaxation time is a term used to describe the associated loss of
coherence or phase between individual protons immediately after the
application of rf pulse. A variety of rf pulse sequences can be used to
enhance the differences in tissue relaxation times T1 and T2, providing
the necessary image contrast.
recovery, inversion recovery, and fast scan technique. Inversion
recovery sequences can be combined with multiplanar imaging to shorten
scan time. Spin echo short pulse repetition (TR ≤ 0.5 sec) and short
echo delay (TE ≤ 40 msec) sequences (or T1) provide good anatomic
detail. Long TR (≥1.5 sec) and long TE (≥≥90 msec) pulse sequences (or
T2) provide good contrast, sufficient for evaluation of pathologic
processes. With a short inversion time in the range of 100 to 150 msec,
the effects of prolonged T1 and T2 relaxation times are cumulative, and
the signal from fat is suppressed. This technique is short time
inversion recovery (STIR), and it has been useful for evaluating bone
tumors (3).
because they provide advantages compared with much slower spin echo
imaging. In particular, gradient recalled echo (GRE) pulse sequences
using variable flip angles (5° to 90°) have gained rapid acceptance in
orthopaedic radiology because they represent the most effective means
of performing fast MR imaging.
each of which relies on using a reduced flip angle to enhance the
signal with short TR. These techniques are known by a variety of
acronyms such as FLASH (fast low-angle shot), FISP (fast imaging with
steady procession), GRASS (gradient-recalled acquisition), and MPGR
(multiplanar gradient recalled).
and coronal or sagittal); for many injuries, all three planes are
necessary. For adequate MR imaging, surface coils are necessary because
they provide improved spatial resolution. Most surface coils are
designed specifically for different areas of the body, such as knee,
shoulder, wrist, and temporomandibular joints.
evaluation by MRI because different tissues display different signal
intensity on T1- and T2-weighted images. The images displayed may have
a high, intermediate, or low signal intensity. High signal intensity of
fat planes and differences in signal intensity of various structures
allow separation of the different tissue components. Fat, bone marrow,
and hematoma display relatively high signal intensity on T1- and
T2-weighted images; cortical bone, air, ligaments, tendons, and
fibrocartilage display low signal intensity on T1- and T2-weighted
images; muscle, nerves, and hyaline cartilage display intermediate
signal intensity on T1- and T2-weighted images. Most tumors display low
to intermediate signal intensity on T1-weighted images, and high signal
intensity on T2-weighted images.
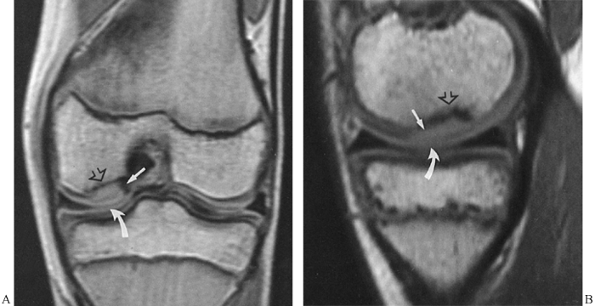
knee, particularly meniscal and ligamentous abnormalities, has high
negative predictive value (16). This test can
be used to screen patients before surgery and avoid unnecessary
arthroscopies. Some types of meniscal tears may be difficult to detect,
such as bucket-handle tears, tears of the free edge, and peripheral
detachments. Medial and lateral collateral ligaments, anterior and
posterior cruciate ligaments, and tendons around the knee joint are
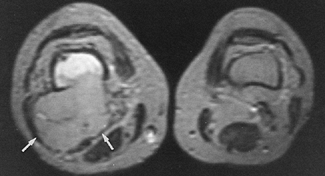
well visualized on MRI (5). Abnormalities of these structures can be diagnosed with high accuracy (37). Osteochondral fractures and lesions of osteochondritis dissecans can also be effectively imaged (Fig. 4.18). In the shoulder, impingement syndrome and most complete and incomplete rotator cuff tears can be accurately diagnosed (Fig. 4.19).
 |
|
Figure 4.18. Coronal (A) and sagittal (B) MR images of the knee demonstrate a necrotic segment of bone (arrow),
separated from the medial femoral condyle by a low-signal-intensity band, representing a sclerotic margin of reactive tissue at the interface between necrotic and viable bone (open arrow). The articular cartilage is intact (curved arrow), indicating an in situ lesion of osteochondritis dissecans. |
 |
|
Figure 4.19.
Oblique coronal MR image of the shoulder (multiplanar gradient, TR = 500, TE = 20, flip angle = 30°) demonstrates a complete tear of the supraspinatus tendon (arrow). Areas of high signal intensity (curved arrow) represent accumulation of fluid in the subacromial–subdeltoid bursae complex. |
cartilaginous labrum. Traumatic lesions of the tendons, such as biceps
tendon rupture, can easily be diagnosed with this technique. MRI
effectively delineates traumatic joint effusions and hematomas, as well
as the changes of osteonecrosis at various sites (Fig. 4.20) (47).
This modality can detect the early changes of osteonecrosis, even when
conventional radiography, tomography, and radionuclide bone scan are
normal (12). MRI of the ankle and foot has been
used in diagnosing tendon ruptures and posttraumatic osteonecrosis of
the talus. In the wrist and hand, MRI has been successfully used in the
early diagnosis of
posttraumatic
osteonecrosis of the scaphoid. Nevertheless, it is not the technique of
choice for evaluating abnormalities of triangular fibrocartilage
complex, for which arthrography is preferred, particularly with the
combination of CT and digital imaging.
 |
|
Figure 4.20. Coronal MR image of the pelvis (spin echo, TR = 600, TE = 20) demonstrates advanced osteonecrosis of the right femoral head.
|
in recent years. The diagnostic accuracy of this technique may exceed
that of conventional MRI. It better demonstrates the intra-articular
structures because they can be separated by capsular distention. Such
distention can be achieved with intra-articular injection of contrast
material such as diluted gadopentate dimeglumine (gadolinium
diethylenetriamine penta-acetic acid, or Gd-DTPA) or saline. The
generated images are very similar to those obtained of the joint with
preexisting joint fluid (joint effusion). In clinical practice, MRA is
used predominantly in the evaluation of shoulder abnormalities, such as
internal derangement, glenohumeral joint instability, rotator cuff
disorders, or articular cartilage and cartilaginous labrum
abnormalities. Indirect MRA is a procedure in which, prior to the MRI
examination of the joint, an intravenous injection of gadolinium is
given. Like direct MRA, this technique may improve detection of rotator
cuff tears, labral pathology, and adhesive capsulitis.
visualize blood vessels. Unlike conventional contrast angiography, it
does not demonstrate the blood volume itself, but rather it depicts a property
of blood flow. One of its advantages lies in fact that after a
three-dimensional MR angiography data set is collected, the physician
may choose any number of viewing directions. This feature also
eliminates vascular overlapping.
angiographic contrast. Some rely on the rapid inflow of relaxed blood
into the region in which the stationary tissue is saturated. These
methods are time-of-flight (TOF) or flow-related enhancement (FRE).
Others, which rely on the velocity-dependent change of phase of moving
blood in the presence of a magnetic field gradient, are the
phase-contrast methods. Some methods involve the subtraction of
flow-dephased images from flow-compensated images. The application of
MR angiography in orthopedic radiology includes evaluation of the
vascular structures in patients with trauma to the extremities, and in
assessment of vascularity of musculoskeletal neoplasms.
spinal cord, the thecal sac, and nerve roots, and in the evaluation of
disc herniation (34). MRI is also useful in
evaluating spinal ligament injury. Demonstration of the relationship of
vertebral fragments to the spinal cord with direct sagittal imaging is
extremely helpful, particularly in the cervical and thoracic areas.
evaluating bone and soft-tissue tumors. Particularly in the evaluation
of soft-tissue masses, MR offers distinct advantages over CT. Tissue
planes surrounding the lesion can be more adequately visualized, and
neurovascular involvement can be evaluated without the use of
intravenous contrast (62).
musculoskeletal tumors. These include spin-echo (SE) sequences,
inversion recovery (IR) sequences, STIR sequences, GRE sequences, and
fast T2 or fat-suppression T2-weighted sequences. SE sequences are the
most effective for identification and staging of most skeletal tumors.
The signal intensity for normal tissues is predictable using these
sequences. On T1-weighted images, fat and bone marrow have a high
signal intensity that changes to intermediate intensity on T2
weighting. Muscles have intermediate signal intensity on both T1 and T2
sequences. Cortical bone and fibrocartilage have low signal on both
sequences. Fluid has intermediate signal on T1-weighted and high signal
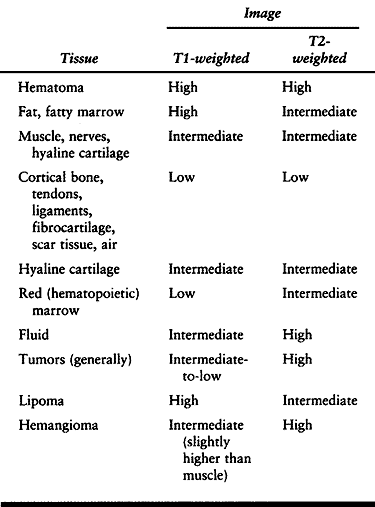
intensity on T2-weighted images (Table 4.1).
Most bone tumors have increased T1 and T2 relaxation times compared
with normal tissue and therefore are imaged as areas of low or
intermediate signal intensity on T1-weighted SE sequences and high
signal intensity on T2-weighted sequences.
 |
|
Table 4.1. MRI Signal Intensities of Various Tissues
|
MRI in many instances is superior to CT, particularly in the coronal
plane, in delineating the extraosseous and intramedullary extent of the
tumor and its relationship to surrounding structures. Showing sharper
demarcation between normal and abnormal tissue than CT, especially in
evaluating the extremities, MRI reliably identifies the spatial
boundaries of tumor masses, encasement
and
displacement of major neurovascular bundles, and the extent of joint
involvement. T1-weighted spin echo images enhance tumor contrast with
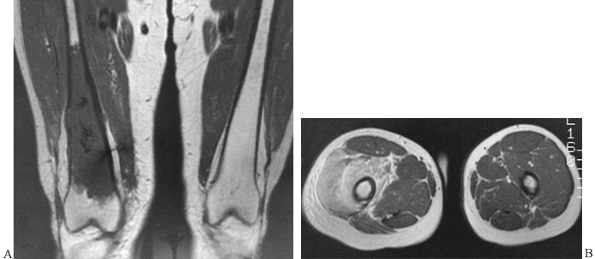
bone, bone marrow, and fatty tissue (Fig. 4.22A), and T2-weighted spin echo images enhance tumor contrast with muscle and accentuate peritumoral edema (Fig. 4.22B).
Axial and coronal images have been employed in determining the extent
of soft-tissue invasion in relation to important vascular structures.
Compared with CT, MR images do not clearly depict or allow
characterization of calcification in the tumor matrix; large amounts of
calcification or ossification are occasionally undetectable. Moreover,
MRI has shown itself less satisfactory than CT, and even less
satisfactory than plain films and tomography, in demonstrating cortical
destruction and periosteal reaction.
 |
|
Figure 4.21.
On the MR axial image (T2-weighting), the involvement of the bone marrow is demonstrated by high signal intensity of the tumor (Ewing’s sarcoma). The soft-tissue extension of the tumor displaying intermediate signal intensity is well demonstrated (arrows). |
 |
|
Figure 4.22. A:
T1-weighted coronal MR image demonstrates good contrast between the tumor in the right femur (dedifferentiated chondrosarcoma), which displays low signal intensity, and normal bone marrow, which displays high signal intensity. B: T2-weighted axial MR image of the same patient enhances the contrast between tumor, displaying high or intermediate signal intensity, and normal muscles, displaying low signal intensity. |
enhancement of MR images using intravenous injection of Gd-DTPA.
Enhancement was found to give better delineation of the tumor in richly
vascularized parts, in compressed tissue immediately surrounding the
tumor, and in atrophic but richly vascularized muscle (50). The contrast studies also improved the differentiation of necrotic tissue from viable areas in various malignant tumors (18).
additional application in evaluating tumor response to irradiation and
chemotherapy and in evaluating local recurrence (54).
Although static MRI was of little value for assessment of response to
the treatment, dynamic MR imaging using Gd-DTPA had a higher degree of
accuracy (85.7%) and was superior to scintigraphy, particularly in
patients who were receiving intra-arterial chemotherapy (19,20). The latest observation suggests that MR spectroscopy may also be useful in evaluating patients undergoing chemotherapy (17,61).
establishing the precise nature of a bone tumor, and too much faith has
been placed in MRI as a method for differentiating benign from
malignant lesions (63). Trials using combined 1H MRI (proton imaging) and 31P MR spectroscopy failed to differentiate most benign lesions from malignant tumors (49).
Despite the use of various criteria, the application of MRI to tissue
diagnosis has rarely brought satisfactory results, because the small
number of protons in calcified structures renders MRI less useful in
evaluation of bone lesions (1). The physician
can miss valuable evidence related to the production of the tumor
matrix using this modality, because it is unsatisfactory for
demonstrating small calcified structures. Moreover, MRI has been an
imaging modality of low specificity. T1 and T2 measurements are
generally of limited value for histologic characterization of
musculoskeletal tumors.
proved to be clinically valuable in identifying tumor types, although
it has proved to be an important technique in the staging of
osteosarcoma or chondrosarcoma (63). T2-weighted
images are a crucial factor in delineating extraosseous extension of
tumor and peritumoral edema and assessing the involvement of major
neurovascular bundles. Necrotic areas change from low-intensity signal
in the T1-weighted image to a very bright, intense signal in the
T2-weighted images and can be differentiated from viable, solid tumor
tissue.
tumors, it is a useful tool for differentiating round cell tumors and
metastases from stress fractures and medullary infarcts in symptomatic
patients with normal radiographs. It can occasionally differentiate
benign from pathologic fractures (3,63).
include the contraindications of scanning patients with cardiac
pacemakers or cerebral aneurysm clips, and those who are
claustrophobic. The presence of metallic objects, such as ferromagnetic
surgical clips, causes focal loss of the signal with or without
distortion of image. Metallic objects create “holes” in the image, but
ferromagnetic objects cause more distortion (48).
MRI still lacks high resolution for evaluating osseous anatomy and
fractures compared with CT and conventional tomography. As in CT, an
average volume effect may be observed in MR images, rendering
occasional pitfalls in the interpretation. Motion artifacts can be
eliminated using fast imaging techniques.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
Sheikh W, Sfakianakis GN, Mnaymneh W, et al. Subacute and Chronic Bone
Infections: Diagnosis Using In-111, Ga-67, and Tc99m MDP Bone
Scintigraphy and Radiography. Radiology 1985;55:501.
LL, Goodman SB, Perkash I, et al. Benign versus Pathologic Compression
Fractures of Vertebral Bodies: Assessment with Conventional Spin-Echo,
Chemical-Shift, and STIR MR Imaging. Radiology 1990;74:495.
J, Kerr E, Sartoris DJ, et al. Quantitative Dual-energy Radiographic
Absorptiometry of the Lumbar Spine: In Vivo Comparison with Dual-photon
Absorptiometry. Radiology 1989;170:129.
MW, Sostman HD, Leopold KA, et al. Soft-Tissue Sarcomas: MR Imaging and
MR Spectroscopy for Prognosis and Therapy Monitoring. Radiology 1990;174:847.
R, Sciuk J, Bosse A, et al. Response of Osteosarcoma and Ewing Sarcoma
to Preoperative Chemotherapy: Assessment with Dynamic and Static MR
Imaging and Skeletal Scintigraphy. Radiology 1990;175:791.
CR, Schils JP, Resnick D, Sartoris DJ. Arthrography of the
Post-Traumatic Knee, Shoulder, and Wrist. Current Status and Future
Trends. Radiol Clin North Am 1989;27:957.
DG, Rao VM, Dalinka MK, et al. Femoral Head Avascular Necrosis:
Correlation of MR Imaging, Radiographic Staging, Radionuclide Imaging,
and Clinical Findings. Radiology 1987;162:709.
WG, Crowley MG, Ryan JR, et al. Bone and Soft-Tissue Lesions: Diagnosis
with Combined H-1 MR Imaging and P-31 MR Spectroscopy. Radiology 1989;173:181.
H, Eliasson J, Egund N, et al. Gadolinium-DTPA Enhancement of Soft
Tissue Tumors in Magnetic Resonance Imaging—Preliminary Clinical
Experience in Five Patients. Skeletal Radiol 1988;17:319.
G, Mutschler W. Detection of Local Recurrent Disease in Musculoskeletal
Tumors: Magnetic Resonance Imaging versus Computed Tomography. Skeletal Radiol 1990;19:85.
HD, Charles HC, Rockwell S, et al. Soft-Tissue Sarcomas: Detection of
Metabolic Heterogeneity with P-31 MR Spectroscopy. Radiology 1990;176:837.
