Injuries to the Shafts of the Radius and Ulna
Because of numerous differences in both treatment and prognosis, shaft
fractures are considered to be clinically distinct from fractures of
the distal (metaphyseal fractures and physeal fractures) and proximal
(radial neck fractures and physeal fractures) ends of the same bones.72,144,281,322,326,329 Most shaft injuries require nothing more than skillful closed fracture care.161,254,356
The remainder are a subset of malaligned fractures that raise concerns
with the orthopaedist and parents about remodeling potential, loss of
motion, and long-term outcome. Issues regarding reduction,
remanipulation, recasting, open treatment, and refracture must be
mastered. Shaft fractures of the forearm also are the most common
reason for orthopaedic surgery of the forearm in children.62,128 Thus, it is very important for orthopaedic surgeons who treat children to skillfully manage the cognitive
and technical aspects of both nonoperative and operative treatment for injuries to the shafts of the radius and ulna.
contemporary and ancient terms. In one of the oldest examples, the
remains of a 15-year-old from the Paleolithic period (the Stone Age)
demonstrate posttraumatic forearm deformity.106
Among the skeletons of children from medieval England (circa 950 A.D.)
acute trauma and new bone formation were most common in 6- to
10-year-olds.190 Other archeological
reports from the medieval period (circa 1100-1550 A.D.) indicate that
forearm fractures were not only common but also presumably well
treated, based on absence of substantial deformity.126 This latter finding may simply be an early testament to pediatric remodeling potential.
care bears the marks of many orthopaedic icons. The Austrian surgeon
Lorenz Böhler (1885-1973) had a world-wide impact on fracture care.239,309 In the late 1920s, he published his important book The Treatment of Fractures,
and it flourished for nearly three decades. It was translated into 8
different languages and published in 13 German and 5 English editions.309
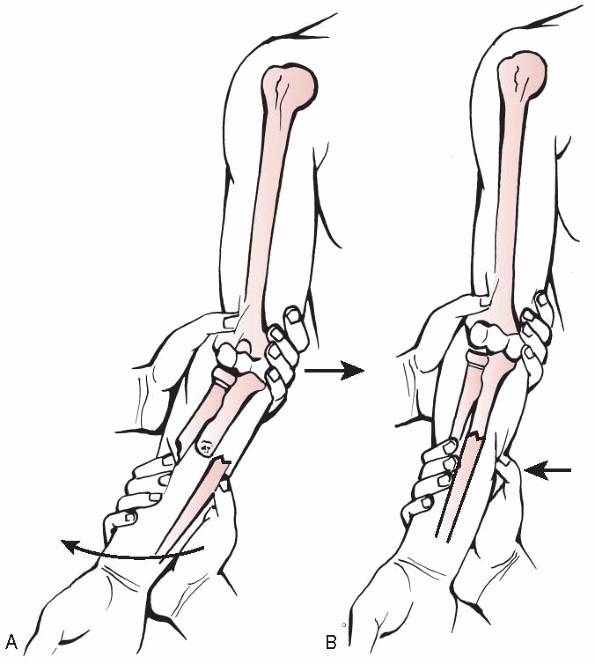
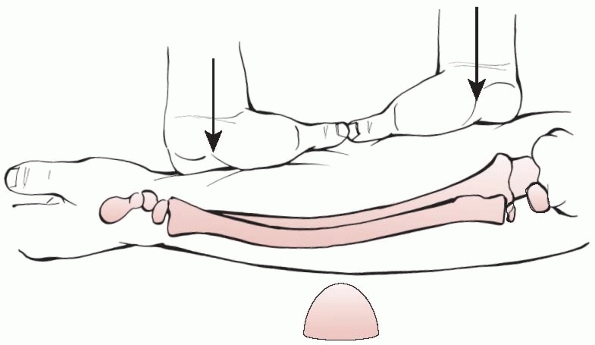
Böhler recognized that reduction tactics that used exaggeration of the
deformity and re-engagement of the bone ends often were effective in
distal-third forearm fractures, but longitudinal traction was his main
tool for reducing fractures in the middle and proximal thirds (Fig.10-1).23
His protocol for forearm fracture reduction included belted
countertraction of the humerus above the flexed elbow while exerting
“steady (not jerky) strong traction by pulling on the thumb with one
hand and on the second to fourth fingers with the other hand. Traction
on the thumb must be stronger than that on the other fingers” (Fig. 10-2).23
Böhler believed that forearm fracture reduction would occur within 5 to
10 minutes when using this technique, and he favored skin-tight
plasters (i.e., form-fitting casts with little to no padding) for
immobilization.264,309
He stated that “it is unimportant whether lateral displacement of half
or even of the entire width of the diaphysis is corrected, because such
displacement usually disappears within a year. The same is true of
angulation up to 10 or 15 degrees. More marked angulation and rotation
must be corrected. Shortening is of no importance. There is never any
necessity in adolescents to reduce closed forearm fractures
operatively, or to unite the fragments with nails, wires or plates and
screws.”23 Böhler’s outspoken
criticism of pediatric forearm surgery continued, “Operative treatment,
as bourne out by x-ray pictures in the literature, is very often
practiced in children, and consists of osteosynthesis of different
types as well as open reduction. It is superfluous, because
conservative treatment is always successful. Moreover, operative
treatment is dangerous in that infection with all its consequences may
ensue. Pseudarthroses have also been reported following operative
treatment, which are unknown in children.”23
 |
|
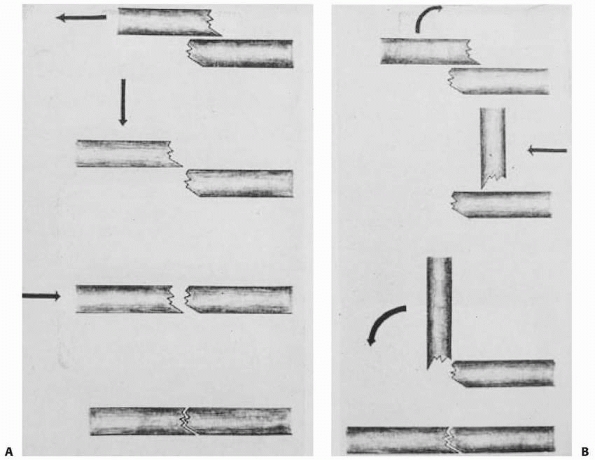
FIGURE 10-1 Fracture reduction techniques for complete fractures from Böhler’s original textbook. A. Longitudinal traction method. B.
Exaggeration of deformity method. (Reproduced from Böhler L. The Treatment of Fractures. 5th English ed. New York: Grune & Stratton, 1956.) |
 |
|
FIGURE 10-2 Böhler’s horizontal traction/countertraction method.
|
for internal fixation in children grew, reflecting the resurgent
interest in osteosynthesis in adults that occurred in the late 1930s.286 With the publication of his highly regarded textbook Operative Orthopaedics
in 1939, the American Willis Campbell (1880-1941) tacitly approved
operations on children’s forearm fractures by illustrating open
reduction and internal fixation of a distal-third forearm shaft
fracture in a patient who was perhaps as young as 11 or 12 years of age
(Fig. 10-3). He stated, “When satisfactory
alignment or fixation in fractures of both bones of the forearm is not
possible by conservative measures, skeletal traction or open reduction
is required. This is particularly true of oblique or spiral fractures.
Internal fixation, preferably by a vitallium plate, should be applied
to prevent bowing.”50 Later
advocates of osteosynthesis such as the Belgian Jean Verbrugge
(1896-1964) also reported on internal fixation for fractures in
children, listing forearm fractures as one of the most common
indications.336 The rather
indiscriminate application of surgical techniques (by some surgeons of
the day) to children helps explain the criticism from Böhler and other
authors who followed.23,24,33,36,152
forearm fracture care. The Englishman Sir John Charnley (1911-1982) in
his textbook The Closed Treatment of Common Fractures
challenged the utility of Böhler’s horizontal traction approach to
forearm reduction and advocated his preferred method of vertical
traction (Fig. 10-4).61 Charnley did not accept Böhler’s concept of skin-tight plasters and favored padded plasters with three-point molding instead (Fig. 10-5). This concept was embodied by Charnley’s maxim: “A curved plaster is necessary in order to make a straight limb.”61
 |
|
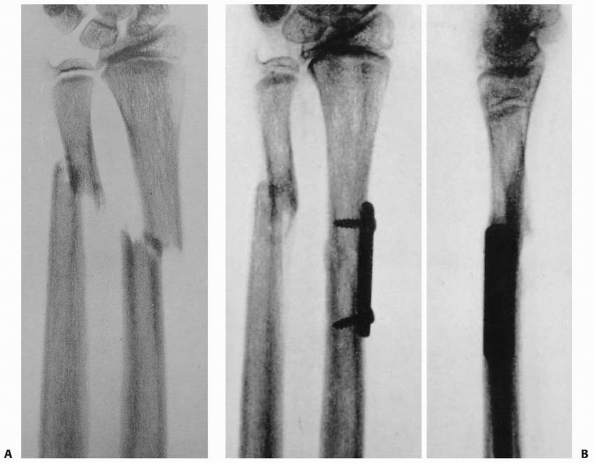
FIGURE 10-3 Original illustration from Campbell’s 1939 textbook. A. An approximately 12-year-old patient with distal-third radius and ulna shaft fracture. B. Postoperative radiographs after plate fixation of radius.
|
offered strong recommendations for nonoperative treatment of nearly all
children’s fractures (especially fractures of the middle third of the
forearm). He was an outspoken critic of most surgical treatment of
children’s fractures and offered impressive illustrations of successful
nonoperative care of forearm shaft fractures in children (Fig. 10-6).34
Blount’s frustration regarding the state of affairs of children’s
fractures is captured in this 1967 quote: “The ever-changing crop of
fledgling surgeons of trauma must learn anew that fractures in children
are different from those in adults. This is particularly true of
fractures of the forearm.”33 The
reduction technique he advocated was one of manually exaggerating the
fracture deformity while simultaneously applying traction and using the
surgeon’s thumbs as a fulcrum. Regarding forearm fractures in children
Blount also stated, “Bayonet apposition in good alignment is not to be
confused with angular deformity… . Too many men treat roentgenograms
instead of children.”34
the world of pediatric fractures: the Englishman Mercer Rang
(1933-2003). Rang first published a book entitled The Growth Plate and Its Disorders, which was aimed at orthopaedists who cared for children, and later his classic text Children’s Fractures, in which he highlighted many of the practical aspects of caring
for children’s fractures, including forearm fractures. Contrary to the
forearm shaft fracture rotational dogma of others, Rang said,
“Immobilize the fracture in the position—any position —in which the
alignment is correct and the reduction feels stable.”262
He also discussed the value of single-bone internal fixation with a
Kirschner wire in selected patients when open reduction was preferable
to malunion.262 The bulk of his
discussion of reduction techniques and casting techniques was not new
(it reflected the work of those who had come before him), but it was
effectively illustrated (with his own artwork) and communicated to
generations of orthopaedic surgeons around the world.220
 |
|
FIGURE 10-4 Charnley’s vertical traction.
|
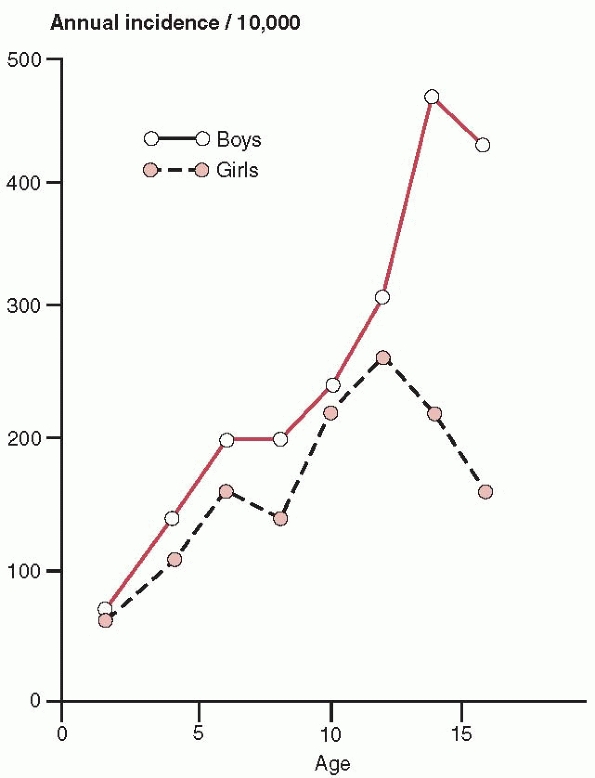
has shown that the overall risk of fracture in children slowly
increases for both males and females until they are 11 or 12 years old
and then drops for females and increases further for males (Fig. 10-7).
This risk difference is starkly illustrated by the fact that males who
are 13 or older have approximately double the fracture rate of their
female peers.181 Forearm fractures have been reported to be the most common pediatric fracture associated with backyard trampoline use28 and the second most common one (supracondylar humeral fractures were first) associated with monkeybars.345 Using a national database, Chung and Spilson64
looked at the frequency of upper extremity fractures in the United
States and found that the single largest demographic group was
fractures of the radius and ulna in children aged 14 years or less,
with a rate approaching 1 in 100.
 |
|
FIGURE 10-5 Charnley’s three-point mold illustration.
|
from forearm shaft fractures indicate that overall, radial shaft
injuries rank as the third most common fracture of childhood (behind
distal radial and supracondylar humeral fractures).62 Open fractures in children are most often fractures of the shaft of the radius and ulna or tibial shaft fractures.62 Among pediatric fractures, forearm shaft injuries are the most common site of refracture.181
Forearm shaft fractures have been shown to occur most commonly in the
12- to 16-year-old age group, a challenging age group to treat.62
who showed that the rate of forearm shaft fractures in school-age
children (more than 5 years old) is more than double that in toddlers
(1.5 to 5 years old). Age also may have an effect on injury severity.
Many experienced clinicians have pointed out the increasing level of
treatment difficulty as the level of forearm fracture moves proximally,72,144,241,326,329 and more proximal fractures tend to occur in older patients.72
and ulnar shaft fractures is a fall on an outstretched hand that
transmits indirect force to the bones of the forearm.3,70,165
Biomechanic studies have suggested that the junction of the middle and
distal thirds of the radius and a substantial portion of the shaft of
the ulna have an increased vulnerability to fracture.150
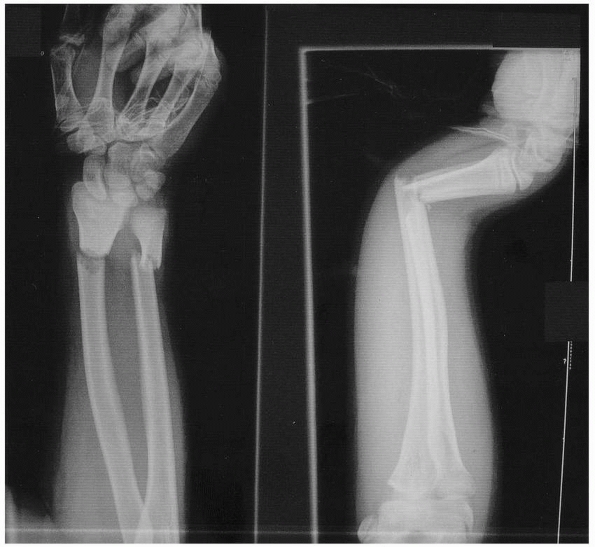
Often, a significant rotational component is associated with the fall,
causing the radius and ulna to fracture at different levels (Fig. 10-8).93,207 If the radial and ulnar fractures are near the same level, a minimal torsional component can be inferred (Fig. 10-9). If comminution is present, higher-energy trauma should be suspected.85
Significant hyperpronation forces are associated with isolated shaft
fractures of either the radius or the ulna and concomitant dislocation
of either the distal or the proximal radioulnar joint. Thus, in any
single-bone forearm shaft fracture, these important joints need to be
closely scrutinized. Galeazzi and Monteggia fracture-dislocations are
discussed in Chapters 9 and 12, respectively.
baseball bat) can fracture a single bone (usually the ulna) without
injury to the adjacent distal or proximal radioulnar joints.36
Isolated ulnar shaft fractures have been referred to as “nightstick
fractures.” Alignment of the radial head should be confirmed in
any child with such a fracture to avoid a “missed Monteggia” injury.148 Isolated radial shaft fractures are rare but notoriously difficult to reduce with closed methods.68,92 Rang263
referred to apex volar greenstick fractures of the distal radial shaft
near the metaphysis as “the slipper” because of its annoying tendency
to lose position after otherwise satisfactory reduction.
 |
|
FIGURE 10-6 Case illustration from Blount’s original work showing dramatic remodeling. A. Six-year-old male with both-bone forearm fracture. B. Six months after injury. Comparison of AP (C) and lateral (D) radiographs of both forearms at 5-years follow-up.
|
 |
|
FIGURE 10-7
Annual incidence of all fractures in children. (From Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B 1997;6: 79-83.) |
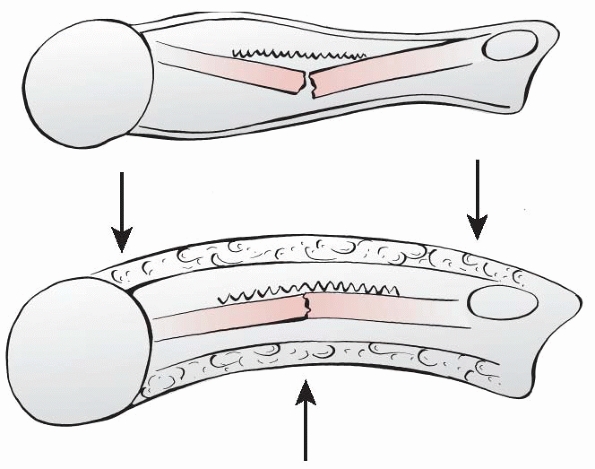
fracture patterns, traumatic bowing (also known as bow fractures or
plastic deformation)263 and
greenstick fracture, also bear mentioning. Bone behaves differently
based on the direction of the forces applied to it. This is the
so-called anisotropic property of bone, and it can be simply explained
as follows: bone is more resistant to axial forces than to bending and
rotational forces.54 Pediatric bone
also is much more porous than its adult counterpart and behaves
somewhat differently from a biomechanic standpoint.57,232 Because of its porosity, pediatric bone absorbs significantly more energy prior to failure than does adult bone.75
When relatively slowly applied, longitudinal forces bend immature bone
beyond its elastic limits and into its plastic zone, resulting in
traumatic bowing.40,198
Thus, when a bending force is applied relatively slowly, many
microfractures occur along the length of the bone, leading to
macroscopic deformity without discernible radiographic fracture. This
bending can usually be seen radiographically if suspected.
 |
|
FIGURE 10-8 Radius and ulna shaft fractures occurring at different levels, implying rotational mechanism.
|
On anteroposterior (AP) and lateral radiographs, greenstick fractures
show cortical violation of one, two, or three of their radiographic
cortices, and thus some bony continuity is preserved. Rotational
deformity is considered to be intimately related to the clinical
deformity seen with greenstick fractures of the forearm, and the
analogy of a cardboard tube that tends to bend as it is twisted has
been offered by Holdsworth.144
Specifically, hyperpronation injuries usually are associated with
apex-dorsal greenstick fractures of the forearm, and hypersupination
injuries usually are associated with the opposite, apex-volar injuries.92,220 The treatment of these greenstick fractures requires a derotation maneuver in addition to correction of any angulation.55,133
of the radius and ulna usually are not subtle. Deformity and pain are
the classic findings. Patients typically experience exquisite pain
emanating from the involved area. Decreased pronation and supination
motion are also usually noted.308
Neither practitioners nor parents are always reliable assessors of
children’s pain, and ideally patients should rate their own pain.170,301 Significant anxiety and muscle spasm almost always amplify a child’s painful experience.49,116
It has been suggested that muscle spasm is a protective effort by the
body to splint or otherwise protect the injured body part.116
When such muscle spasm occurs in association with certain fracture
patterns (e.g., a radial shaft fracture proximal to the pronator teres
insertion), it produces
predictable fracture displacement (e.g., a pronated distal radial fragment and a supinated proximal fragment).
 |
|
FIGURE 10-9 Radial and ulnar shaft fractures occurring at same level, implying no significant rotation.
|
challenges. Certain pathologic fractures of the forearm may occur in
the absence of overt trauma.156,178
Many minimally displaced fractures of the shafts of the radius and ulna
can be mistaken for a “sprain” or “just a bruise” for several days to
several weeks. This usually occurs in young children who continue to
use the fractured arm during low-level play activities. As a general
rule, a fracture should be suspected if the child has not resumed all
normal arm function within 1 or 2 days of injury.
occur as isolated injuries, but wrist and elbow fractures may occur in
conjunction with forearm fractures, and the elbow and wrist region
needs to be included on standard forearm radiographs.27,76,165,353,313,359
If clinical suspicion is high, then dedicated wrist and elbow films are
necessary. The so-called floating elbow injury (fracture of the bones
of the forearm along with ipsilateral supracondylar humeral fracture)
is a well-described entity that must not be missed.27,272,313,353
Surgical stabilization of both the supracondylar fracture and the
forearm fractures has been recommended by multiple authors in recent
years31,138,271,272,318,321
to avoid the risk of a compartment syndrome. Galeazzi and Monteggia
fracture-dislocations also must be ruled out. Compartment syndrome also
can occur in conjunction with any forearm shaft fracture.74,363
This rare but potentially devastating complication can lead to a
Volkmann ischemic contracture, which has been shown to occur after
forearm shaft fractures almost as often as it does after supracondylar
humeral fractures in children.221
Patients with severe pain unrelieved by immobilization and mild
narcotic medication should be reassessed for excessive swelling and
tight forearm compartments. If loosening of the splint, cast, and
underlying cast materials fails to relieve pain, then measurement of
compartment pressures and subsequent fasciotomy may be necessary.
that occur in conjunction with forearm fractures must be carefully
evaluated because they may be an indication of an open fracture. Clues
to the presence of an open fracture include persistent slow bloody ooze
from a small laceration near the fracture site and subcutaneous
emphysema on injury films. Careful evaluation and, in some situations,
sterile probing of suspicious wounds will be necessary. Open forearm
fractures are discussed later in this chapter.
with forearm shaft fractures, but the consequences of such injuries are
far-reaching. Serial neurovascular examinations should be performed and
documented. Radial and ulnar pulses along with distal digital capillary
refill should be routinely evaluated. Davis and Green80
reported nerve injuries in 1% (5/547) of their pediatric forearm
fracture patients, with the most commonly injured nerve being the
median nerve. Combined data from three large series of pediatric open
forearm fractures reveal an overall nerve injury rate at presentation
of 10% (17/173), with the median nerve once again being the one most
commonly injured.128,135,195
To screen for these rare but significant injuries, every child with a
forearm fracture should routinely have evaluation of the radial, ulnar,
and median nerves.68 Nerve injuries occurring at the time of injury must be differentiated from treatment-related or iatrogenic neurologic deficits.
function. The extended fingers and wrist depict paper and test radial
nerve function. Fully flexed small and ring fingers, an adducted thumb,
and spreading the index and ring fingers mimic scissors and test ulnar
nerve function. Further focused testing should also be done on two
important nerve branches: the anterior interosseous nerve (branch of
median nerve) and the posterior interosseous nerve (branch of radial
nerve). The anterior interosseous nerve provides motor function to the
index flexor digitorum profundus, the flexor pollicis longus, and
pronator quadratus and is best tested by having the patient make an
“OK” sign. The posterior interosseous nerve typically innervates the
extensor carpi ulnaris, extensor digitorum communis, extensor digiti
minimi, extensor indicis, and the three out-cropping muscles of the
thumb (abductor pollicis longus, extensor pollicis brevis, and extensor
pollicis longus).45
Its function is best documented by full extension of the phalangeal and
metacarpophalangeal joints. This is especially difficult to test in a
patient in a cast or splint that partially covers the fingers. Most
injuries that occur in association with forearm fractures are true
neurapraxias and typically resolve over the course of days to weeks.74,80
 |
|
FIGURE 10-10 Upper extremity motor nerve physical examination. A. Rock position demonstrates median nerve motor function. B. Paper position demonstrates radial nerve motor function. C. Scissor position demonstrates ulnar nerve motor function. D. “OK” sign demonstrates function of anterior interosseus nerve.
|
described in rather imprecise terms such as “both-bone forearm
fracture” and “greenstick fracture.” Radiographs confirm the diagnosis
of forearm shaft fracture and are the basis for most classification
systems. The most comprehensive classification of forearm fractures is
the one adopted by the Orthopaedic Trauma Association (OTA).12 Although this system is sound in concept, its 36 discrete subtypes12 make it impractical for everyday clinical use, and it has not been widely used by clinical researchers.269
Despite its complexity, the OTA classification does not account for one
of the most important prognostic factors in pediatric forearm shaft
fracture: location of the fracture in the distal, middle, or proximal
third of the shaft.
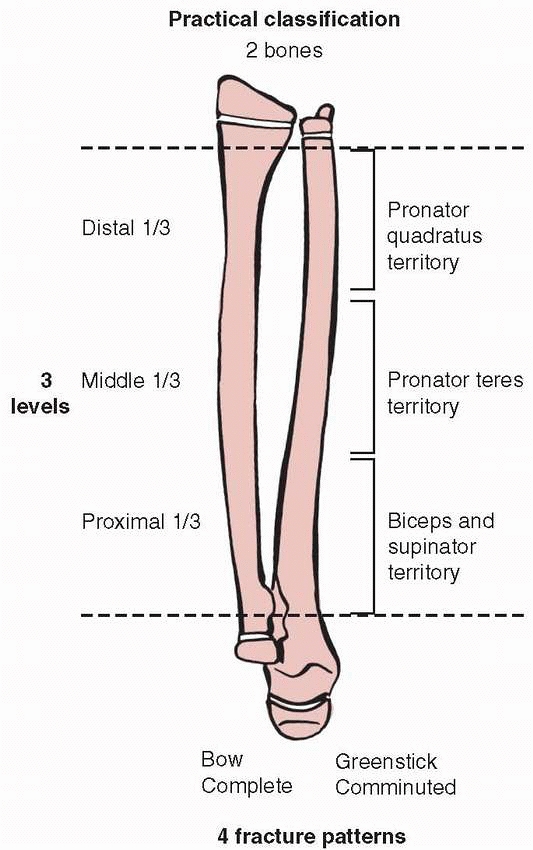
descriptions of forearm shaft fractures. An orderly and practical
approach to forearm shaft fracture classification should provide
information about the bone (single bone, both bones), the level
(distal, middle, or proximal third), and the pattern (plastic
deformation, greenstick, complete, comminuted). Bone involvement is
important because it not only indicates the severity of injury but also
influences suspicion regarding additional soft tissue injury (e.g.,
single-bone injury increases the likelihood of a Monteggia or Galeazzi
injury)335 and affects reduction tactics (unique single-bone fracture reduction strategies can be used) (Fig. 10-11).
Single-bone shaft fractures occur, but both-bone fractures are more
common. Level is important for anatomic reasons relative to muscle and
interosseous ligament attachments,
as
well as differences in prognosis for distal-, middle-, and
proximal-third shaft fractures. Pattern is important because it
significantly alters the treatment approach. For example, the primary
reduction strategy is very different for greenstick fractures
(rotation) compared to that for complete fractures (vertical traction).
Certain comminuted fractures (e.g., comminution of both bones) may
preclude reduction and casting and require plate fixation.103,104
Fortunately, comminuted fracture patterns are rare in children. For all
practical purposes, the buckle fracture pattern that is common in the
distal radial metaphysis never occurs in isolation in the shaft region.
The typical buckle fracture “speed bump” may accompany either plastic
deformation or greenstick fractures. Thus, there are two bones, three
levels, and four common fracture patterns (Fig. 10-12). We believe this is a practical and clinically relevant way to describe forearm shaft fractures.211
 |
|
FIGURE 10-11
Isolated ulnar shaft reduction technique (Blount). Valgus force applied to fracture site and direct thumb pressure over distal ligament. |
terms of this practical classification, fracture displacement must be
evaluated. Fracture displacement can occur as angulation, rotation,
shortening, or translation. Angulation is important in treatment
decision-making and can be measured with reasonable reliability.185,319 Rotation is a simple concept, but it is difficult to assess clinically.93,255 The best that usually can be done is to roughly estimate rotation within a 45-degree margin of error.72,255
Based on available clinical studies, it appears that less than 1 cm of
shortening should be accepted in either single-bone or both-bone
fracture patterns.53,81,86,213,273
It also has been suggested that the shortening that accompanies
displaced fractures may help preserve future motion through
interosseous membrane relaxation.255 Translation also is a simple concept and can be easily measured. Completely (100%) translated fractures of the middle third72,255 and distal third86,213,273
of the forearm have been shown to reliably remodel. Certain situations
may raise concern regarding complete translation, such as isolated
middle-third radial fractures with medial (ulnar) displacement that
significantly narrows the interosseous space and translation in
children who have less than 2 full years of growth remaining, because
remodeling of the translated fracture site is less predictable than in
younger children.230,232
 |
|
FIGURE 10-12
Practical classification of forearm shaft fractures. (Distal dotted line defined by proximal extent of Lister’s tubercle and proximal dotted line defined by proximal extent of bicipital tuberosity.) |
shafts of the radius and ulna relates to the likelihood of bad results
in the absence of adequate care. Data from certain developing countries
may be as close as we come to natural history studies of untreated
fractures. Archibong and Onuba14
reported on 102 pediatric fracture patients treated in southeastern
Nigeria. Their patients most commonly had upper extremity fractures,
and they frequently experienced significant delays in seeking medical
treatment, which led to high rates of malunion requiring surgical
treatment.14 Other Nigerian authors
have found that young age was not protective against fracture malunion
(more than 50%) and nonunion (25%) following traditional bonesetter
treatment.236
It is unclear whether children treated in this fashion are better or
worse off than if they had received no treatment at all. The rationale
for treating pediatric forearm shaft fractures is thus based on the
premise that the results of modern orthopaedic treatment will exceed
“pseudonatural histories” such as these.
Despite their great concern to parents, cosmetic issues have not been
formally studied, and as a result the practitioner must interpret
forearm cosmetic issues on a case-by-case basis. Clinical experience
has shown that the ulna appears to be less forgiving from a cosmetic
standpoint because of its long subcutaneous border. Early and repeated
involvement of the parents (or other legal guardians) in an informed
and shared decision-making process is essential.
implicated as causes of limited forearm motion after forearm shaft
fractures.143,229 Limited forearm pronation and supination can have significant effects on upper extremity function.27,243,255
Inability to properly pronate often can be compensated for with
shoulder abduction, but no easy compensatory mechanism exists for
supination deficits.68,144,243,255 Daruwalla76
identified a nearly 53% rate of limited forearm rotation (subtle in
some, dramatic in others) in his series of 53 children with forearm
fractures and attributed it to angular deformity and rotational
malalignment. Several patients in Price’s255
classic series of pediatric forearm malunions had severe forearm
range-of-motion losses that significantly limited vocational and
avocational activities. Trousdale and Linscheid329
reported range-of-motion losses severe enough to prompt corrective
osteotomies in many of their predominantly pediatric (less than 14
years old at time of injury) patients with forearm malunions. Meier214 also reported significant range-of-motion deficits in association with pediatric forearm malunion.
 |
|
FIGURE 10-13 Effect of forearm malunion on forearm motion. A. Normal arc of forearm motion. B.
Angulated radius leads to diminished arc of forearm motion. (Ogden JA. Skeletal Injury in the Child. Philadelphia: Lea & Febiger, 1982.) |
studied by numerous authors using adult cadaveric forearm specimens.
Matthews et al.206 studied 10- and
20-degree midshaft angular deformities of the radius and ulna in 10
forearm specimens. They found that 10-degree deformities of either bone
individually resulted in little or no measurable motion loss (in the
range of 3 degrees or less). When both bones were angulated 10 degrees
dorsal, volar, or toward the interosseous membrane, larger motion
losses were documented (approximately 10 degrees pronation and 20
degrees supination). Significantly greater losses of motion occurred
when one or both bones were angulated 20 degrees (approximately 40
degrees for both pronation and supination). Some of the 10-degree
angulated specimens demonstrated “cosmetically unacceptable deformity.”206 These findings indicate that relatively small angular deformities can be clinically significant.
fracture level on forearm motion was provided by a series of
experiments conducted by Sarmiento et al.280,320
They found that fracture angulation of 15 to 30 degrees led to greater
supination losses when the deformity was in the middle third of the
forearm (40 to 90 degrees) and greater pronation losses when in the
distal third (30 to 80 degrees).320
Fracture angulation of 10 degrees or less in the proximal or middle
forearm rarely resulted in more than 15 degrees of motion loss,280,320 but the same angulation in the distal third of the forearm was at times
(usually with isolated radius fracture) associated with pronation losses of 20 degrees.280,320
These findings challenge commonly held beliefs that the distal third of
the forearm is the most forgiving. These same authors asserted that
rotational malalignment led to rotational motion losses that usually
were equal in magnitude and opposite in direction to the deformity
(e.g., a 10-degree pronation deformity led to a 10-degree loss of
supination).320
 |
|
FIGURE 10-14 A 6-year-old male who suffered a right forearm shaft malunion. A. Radiograph one week after fracture showing complete midshaft ulnar and proximal third radial fractures. B. Healed fractures at 6-month follow-up. C. Twenty month follow-up. D. Twenty-six month follow-up. (continues)
|
 |
|
FIGURE 10-14 (continued) E. Symmetrical pronation. F. Limited supination on the right G. Axial alignment with palms together. H. An effort at supination. I. Axial alignment in pronation.
|
In isolated midshaft radial fractures, more than 30 degrees of
malrotation was a threshold for significant losses in motion
(approximately 15 degrees).167
Isolated midshaft ulnar fracture malrotation did not alter the total
arc of forearm motion but did change the set point (e.g., a 30-degree
pronation deformity took away 30 degrees of pronation and added 30
degrees of supination).331 Larger ulnar axial malalignment of 45 degrees decreased overall forearm rotation by no more than 20 degrees.331 Large residual ulnar shaft translation has similarly been found to have little impact on forearm rotation.209 Simulated combined radial and ulnar midshaft rotational
malunions resulted in the worst motion (more than 50% losses of
pronation and supination when 60-degree rotational malunions were in
opposite directions).88 Rotational malunions that approximated recommended limits in the literature (45 degrees)255 produced less extreme but real limitations of motion (Table 10-1).88
From these studies and our clinical experience, it appears that the
radius is more sensitive to rotational problems and less sensitive
regarding cosmetic issues, while the ulna is exactly the opposite.
|
TABLE 10-1 Condensed Range-of-Motion Information
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
taught that 50 degrees of pronation and 50 degrees of supination
represent adequate forearm motion.219
It must be remembered that this classic study performed by Morrey and
his Mayo Clinic colleagues involving 33 normal subjects (18 female, 15
male) from 21 to 75 years of age is not the only study that addresses
forearm motion. The average arc of normal forearm motion for the Mayo
group (68 degrees pronation to 74 degrees supination)219
was approximately 20 degrees less than that measured in 53 healthy male
subjects who were no older than 19 years old (77 degrees pronation to
83 degrees supination) by Boone and Azen39 and 35 degrees less than that reported by Rickert et al.270
(75 degrees pronation to 100 degrees supination) in 141 subjects of
both sexes between 20 and 30 years of age. Contemporary
three-dimensional motion analysis has revealed that maximal pronation
occurs when pouring liquid from a pitcher and maximal supination
commonly occurs during personal hygiene activities.261 Thus, it seems clear that the forearm motion “goals” reported by Morrey et al.219
are not necessarily ideal or even optimal, but rather they may be
considered as the minimal limits of forearm function. Stated another
way, losing 20 degrees or 30 degrees of either pronation or supination
carries the potential for significant functional impact upon important
activities of daily living.
of the forearm injury within established anatomic and functional
guidelines while also taking into account the reasonable degree of
remodeling that can be expected in growing children.154
Most of the time, these goals can be achieved with closed fracture
care, and little or no radiographic or clinical abnormality can be
detected following healing. A paradox exists in pediatric forearm
fractures whereby anatomic radiographic alignment is not always
associated with normal motion, and normal motion often is associated
with nonanatomic radiographic healing.143,225,229,320 Herein lies the inherent controversy between operative and nonoperative treatment approaches (Table 10-2).
In patients with anatomic radiographs, range-of-motion problems usually
have been attributed to scarring of the interosseous membrane.168,243,255
With nonanatomic radiographs (incomplete remodeling), range-of-motion
deficits usually are attributed to the radiographic abnormalities.
Thus, treatment of forearm shaft fracture must balance the risk of
allowing stiffness to occur secondary to malunion against the risk of
creating stiffness secondary to surgical procedures.
but knowledge of the limits of remodeling must be taken into
consideration. Established reduction criteria state that complete
(100%) translation is acceptable,213,255 as well as up to 15 degrees of angulation and up to 45 degrees of malrotation.255
Because important forearm fracture treatment decisions frequently are
based on radiographic measurement of angular deformities, it must be
remembered that these angles are projected shadows that are affected by
rotation.102 If angulation is
present on both AP and lateral views (commonly called two orthogonal
views), the true deformity is out of the plane of the radiographs, and
its true magnitude is greater than that measured on each individual
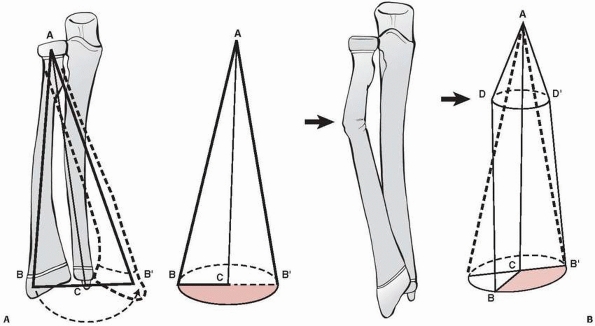
view. Certain forearm shaft fracture deformities are clearly “twoplane
deformities” whose maximal angular magnitude is in some plane other
than the standard AP or lateral plane (Fig. 10-15).17 Bär and Breitfuss17
produced a table (based on the Pythagorean Theorem) that predicts the
true maximal angulation. Accurate deformity measurement can be made
when angulation is seen on only one view and there is no angulation on
the other orthogonal view. A cast change with molding, remanipulation
under analgesia or anesthesia, or surgical fixation may become
necessary, but even with anatomic reduction patients may not regain
full pronation and supination.229,243 Most series of pediatric forearm fractures document excellent subjective results, and
only with special goniometric testing is a decreased range of motion detected objectively.72
|
TABLE 10-2 Pros and Cons of Cast versus Surgical Treatment
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 10-15 Underestimation of true angulation. A. “Out of the AP and lateral plane” underestimates angulation at 30 degrees. B. True AP and lateral demonstrates that true maximal angulation is 40 degrees.
|
forearm shaft fractures have great remodeling potential that occurs
through several mechanisms.289 The
distal radial epiphysis will redirect itself toward normal at about 10
degrees per year. As long as the physis is open, this rate is
independent of age. Although the epiphysis will return to normal
direction, it will have much less effect on correcting an angular
deformity at the midshaft compared to fractures at the subphyseal
level. Remodeling also occurs with lengthening of the bone through
growth, which produces an apparent decrease in angulation, especially
if measured as the difference between the proximal and distal ends of
the bone. Bone also remodels by intramembranous apposition on the
concave side and resorption on the convex side.75,154,289 This occurs throughout life, but more rapidly when driven by the thick periosteum found in children. Larsen182
found that although the epiphyseal angle realigns quickly, children
older than 11 years correct bone angulation less than the younger
children. Thomas stated the following regarding pediatric forearm
remodeling potential: “We should not fail to recall that the remodeling
capabilities of the bones of children have not changed in the last
million years and that open reduction and internal fixation must be
undertaken only after due deliberation.”322 Others such as Ashok Johari157
would state that if one critically evaluates the limits of forearm
shaft remodeling capacity you will find a much higher rate
(approximately 50%) of incomplete remodeling in children over 10 years
of age.
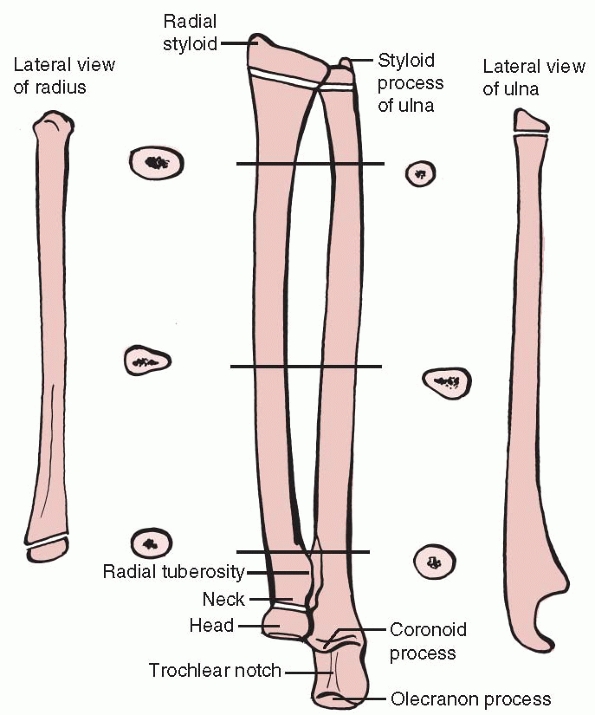
180-degree arc of motion. Its bones, the radius and ulna, are not
simple straight bony tubes. The shaft of the radius is a three-sided
structure with two prominent curvatures. One major gradual convexity
(approximately 10 degrees with its apex lateral-radial) is present
along its midportion; a second, more acute curve of approximately 15
degrees with its apex medial occurs proximally near the bicipital
tuberosity.100,127,277
The deviation along the midportion is commonly referred to as the
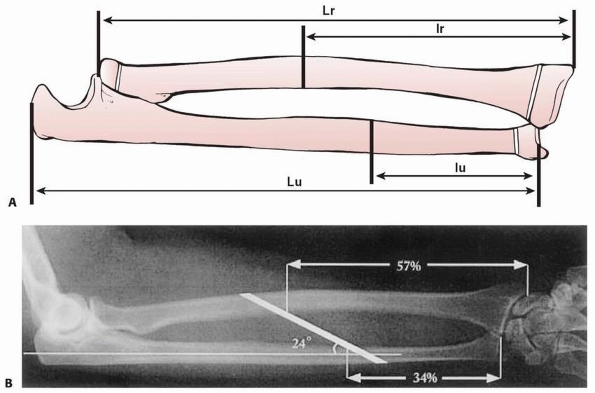
radial bow, and maintenance of this normal contour is a goal of forearm
shaft fracture care.259,284,285
The most important bony landmarks of the radius are the radial styloid
(lateral prominence) and the bicipital tuberosity (anteromedial
prominence), which are oriented somewhat less than 180 degrees away
from each other (Fig. 10-16).217 Anthropologists consider a full 180-degree relationship to be characteristic of Neanderthal osteology.327
Maintenance of the styloid-tuberosity rotational relationship is
another forearm shaft fracture principle. The nutrient artery of the
radius enters the bone in its proximal half and courses anterior to
ulnar (medial).119 Such nutrient
vessels typically are seen on only one orthogonal view and should not
be confused with fracture lines. In cross section, most of the shaft of
the ulna also is shaped like a classic three-sided prism, while its
more distal and proximal portions are much more circular. The most
important bony landmarks of the ulna are its styloid process (distally)
and its coronoid process (proximally). These two landmarks are oriented
nearly 180 degrees from one another, with the styloid aimed in a
posterior (dorsal) direction and the coronoid in an anterior (volar)
direction.217 Tracking
styloid-coronoid rotational alignment of the ulna is another part of
forearm shaft fracture care. The ulnar shaft has mild curvatures in
both its proximal (apex lateral/radial) and distal (apex medial/ulnar)
portions but is otherwise relatively straight.127,277 The nutrient artery to the ulna enters the bone in its proximal half and courses anterior to radial (lateral).119
deformity associated with fractures of both bones of the forearm.94,207,263
Evans stated, “The orthodox position in which to immobilize these
fractures is that of full supination for the upper third, and the
midposition for fractures of the middle and lower thirds, these
positions being based on the anatomical arrangement of the pronators
and supinators of the forearm. However, it is unreasonable to suppose
that all fractures at a given level will present the same degree of
rotational deformity.”94 He pointed
out the importance of tracking the rotational alignment of the
free-moving radial fragment by ascertaining the relative location of
the bicipital tuberosity. This was a major step forward in refining the
orthopaedic care of these forearm injuries. On a fully supinated AP
radiograph of an unfractured forearm, the bicipital tuberosity points
predominantly in a medial direction (nearly 180 degrees opposite of the
radial tuberosity).94 The radius and
ulna also are nearly parallel to each other on such a view. On a fully
pronated AP radiograph of an unfractured forearm, the bicipital
tuberosity points in a lateral direction and the radial tuberosity is
situated medially.94 The radius also crosses over the ulna in a pronated AP view. Rang262 noted that in an unfractured limb, the bicipital tuberosity tended to align with a point near the thenar eminence (Fig. 10-17),
more nearly a 165-degree relationship than a true 180-degree one. These
relationships are best assessed on standard radiographs that include
the entire forearm on one film76,255,329 rather than the specialized bicipital tuberosity view originally suggested by Evans.94
 |
|
FIGURE 10-16 Radial and ulnar anatomy.
|
of secondary ossification centers of the radius and ulna should be kept
in mind because these growth areas must be respected during both
surgical and nonsurgical fracture care.244,256,364,365 The secondary center (epiphysis) of the distal radius is the first to appear at around 1 year of age.32,233 Next are the epiphyses of the proximal radius and distal ulna, which appear by about 4 to 6 years of age.299 The proximal ulna is last and appears at around 9 years of age.298
Physeal closure occurs in two stages, with the proximal radius and
proximal ulna closing by about 15 years of age and the distal radius
and ulna by about 18 years of age.231 It must be remembered that females’ physes close 1 to 2 years before their male counterparts.
restraints: the proximal radioulnar joint (PRUJ), the distal radioulnar
joint (DRUJ), and the interosseous membrane complex, all of which have
important stabilizing and load-transferring functions. These structures
allow rotation of the radius about the ulna along an axis that runs
approximately from the center of the radial head to the center of the
distal ulna.145,243 The PRUJ and DRUJ are discussed elsewhere in this book (Chapters 9 and 11).
The structure and biomechanic function of the interosseous membrane
have been studied extensively in recent years. Hotchkiss et al.149
showed that the central band of the interosseous membrane (the
interosseous ligament) courses from a point near the junction of the
proximal and middle thirds of the radius to a point near the junction
of the middle and distal thirds of the ulna. It is an important
longitudinal stabilizer of the forearm in that 71% of forearm
longitudinal stiffness is provided by the interosseous ligament after
radial head excision.149 Transverse vectors also have been identified246
and reflect the stabilizing effect of the interosseous ligament during
pronation and supination movements. The interosseous ligament
demonstrates tensile properties comparable to the patellar tendon and
the anterior cruciate ligament,247 indicative of the magnitude of the arm forces to which this structure is subjected.
multiple studies have shown that the most strain in the central band of
the interosseous membrane is generated when the forearm is in the
neutral position.203,204,304 These findings of maximal strain in neutral in cadaver studies also are consistent with radiographic measurement studies72
and dynamic magnetic resonance imaging studies of the forearm showing
that the interosseous space is maximal near a neutral position.226 This may help explain certain pathologic situations such as the fixed supination deformity of neonatal brachial plexus palsy208 as well as limitations of pronation and supination due to encroachment on the interosseous space from malangulated fractures (Fig. 10-18).360
The interosseous membrane also serves as an important anchoring point
for several forearm muscles: the flexor digitorum profundus, flexor
pollicis longus, extensor indicis, and the outcropping muscles
(extensor digitorum brevis, abductor pollicus longus).
have an unbalanced number of muscular connections. The ulna typically
has 14 attached muscles and the radius only 10 (Tables 10-3 and 10-4).87,127
Powerful supinators attach to the proximal third of the forearm, while
important pronators attach to its middle and distal thirds (Fig. 10-19).
The accompanying vasculature of the forearm is complex: these muscles
are supplied by more than 248 vascular pedicles arising from the
brachial artery, its branches, or other collateral vessels.268 The radial, ulnar,
and median nerves (or their branches) along with the musculocutaneous
nerve provide all of the key innervations to the motors that attach to
the forearm bones. As mentioned earlier, the median nerve is the most
commonly injured nerve with forearm fractures.79,80,128,135
 |
|
FIGURE 10-17
Rang’s illustration depicting the position of the bicipital tuberosity on AP and lateral views with the forearm in pronation, supination, and neutral position. (From Rang M. Children’s Fractures. Philadelphia: JB Lippincott, 1974.) |
 |
|
FIGURE 10-18 Anatomy of interosseous ligament. A. Central oblique orientation of interosseous ligament. B.
Interosseous ligament attachment in terms of percentage forearm length. (From Skahen JR 3rd, Palmer AK, Werner FW, et al. Reconstruction of the interosseous membrane of the forearm in cadavers. J Hand Surg Am 1997;22:986-994.) |
|
TABLE 10-3 Ten Muscles That Attach to the Radius (and Their Innervation)
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
direction and enters the forearm after passing the lateral epicondyle
between the brachialis and brachioradialis muscles. Near this same
level, it divides into superficial and deep terminal branches. The deep
motor branch of the radial nerve also is known as the posterior
interosseous nerve. In addition to its routine innervation of the
brachioradialis and extensor carpi radialis longus, most commonly (55%
of the time) a motor branch arises from the radial nerve proper or its
superficial terminal branch to innervate the extensor carpi radialis
brevis, while the rest of the time (45%) this motor branch comes from
the posterior interosseous nerve.2
The superficial branch travels along with and beneath the
brachioradialis. The posterior interosseous nerve enters the supinator
muscle, passing the fibrous thickening called the arcade of Frohse
shortly after branching from the radial nerve proper. It courses within
the supinator past the proximal radius, later exiting this muscle
dorsally (posteriorly) near the junction of the proximal and middle
thirds of the radius. Following its emergence from the supinator, the
posterior interosseous nerve branches repetitively to the superficial
extensors and the deeper outcropping muscles. The ulnar nerve enters
the forearm between the two heads of the flexor carpi ulnaris.121
It traverses the forearm between the flexor carpi ulnaris and the
flexor digitorum profundus. In the distal forearm, it lays just beneath
the flexor carpi ulnaris. The median nerve enters the forearm as it
passes between the two heads of the pronator teres.59
It next passes beneath the archway created by the two heads of the
flexor digitorum superficialis. The median nerve then continues down
the course of the forearm nestled between the flexor digitorum
superficialis and the flexor digitorum profundus. It becomes much more
superficial as it nears the level of the carpal tunnel. The anterior
interosseous branch arises from the median nerve at the level of the
pronator and travels deep with the anterior interosseous vessels.
Abundant muscle shields the radial, ulnar, and median nerves from the
shafts of the radius and ulna through most of the forearm.
|
TABLE 10-4 Fourteen Muscles That Attach to the Ulna (and Their Innervation)
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
 |
|
FIGURE 10-19 Muscle forces acting in proximal, middle, and distal thirds.
|
pediatric forearm fractures can be achieved with three surgical
approaches: the Henry (anterior) and Thompson (posterior) approaches to
the radial shaft and the direct (medial) approach to the ulnar shaft.73,223 Compartment syndrome release usually requires the serpentine incision of McConnell’s combined approach.141 These approaches and their variations are well described and illustrated in detail elsewhere.5,19,90,147,296
For open reduction of both the radius and the ulna, most authors favor
separate incisions to minimize the possibility of communicating
hematoma and the development of a radioulnar synostosis.180,259,333 The Thompson approach to the radius generally is used for fractures of its proximal third358 but requires special care to protect the posterior interosseous nerve.84,215,317 Other authors have emphasized the utility of the Henry approach for plating of the proximal radius.215
When open reduction is done in conjunction with other internal fixation
techniques (e.g., intramedullary fixation), limited versions of the
same surgical approaches are used.
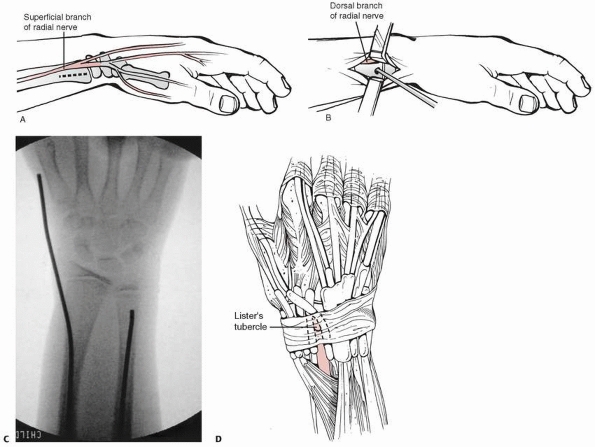
fractures requires knowledge of appropriate physeal-sparing entry
portals about the distal and proximal forearm. Because of the relative
inaccessibility of its proximal end, the radius usually is approached
only distally through either a dorsal or radial entry point. The dorsal
entry point is near the proximal base of Lister’s tubercle or just
lateral to it in a small bare area between the second and third dorsal
compartments. This location is a short distance proximal to the physis
of the distal radius. Another dorsal alternative is pin entry just
medial to Lister’s tubercle, between the third and fourth dorsal
compartments,275 but this may entail
greater tendon risk. The most commonly used radial entry point is
located in line with the styloid process just proximal to the physis.356
Entry in this area passes adjacent to the first dorsal compartment, and
thus the tendons of abductor pollicis longus and extensor pollicis
brevis (as well as branches of the superficial radial nerve) must be
protected (Fig. 10-20). Because of its
extensive branching pattern, portions of the superficial branch of the
radial nerve may be at risk when dorsal or radial intramedullary entry
points are used.1,16
 |
|
FIGURE 10-20 Distal radial entry. A. Distal radial incision in proximity to superficial branch of radial nerve. B. Distal radial entry position for intramedullary rod placement in relationship to superficial branch of radial nerve. C. Radiograph of lateral starting point for intramedullary nail. D. Alternate entry point just proximal to Lister tubercle between second and third dorsal compartment.
|
In the distal portion of the ulna, an entry site can be made proximal
to the physis and in the interval between the extensor carpi ulnaris
and flexor carpi ulnaris tendons. Care must be taken to avoid branches
of the dorsal cutaneous sensory nerve. Ulnar entry is most easily
accomplished in the proximal portion of the bone along its lateral
metaphyseal border (just distal to the olecranon apophysis),
piercing peripheral fibers of the anconeus (Fig. 10-21).48,184,191
This anconeus entry site described by the Nancy group avoids the physis
and avoids the painful bursa that tends to form over “tip of the
olecranon” pins.
 |
|
FIGURE 10-21 Proximal ulnar entry. A. Anconeus entry point. B. Radiograph of proximal ulnar entry point.
|
have been suggested by some authors. Significant growth potential
exists at the distal radius (approximately 10 mm per year), while there
is proportionately less from the olecranon apophysis (approximately 2
mm per year). There is an unnecessary risk to the radial physis and few
if any technical advantages to transphyseal entry of the radius in
diaphyseal level fracture fixation. The ulna apophyseal entry site is
used in many centers.
Low-energy, undisplaced, and minimally displaced forearm fractures can
be immediately immobilized in a properly molded (three-point mold
concept of Charnley) above-elbow cast.10
If posttraumatic tissue swelling is a concern, noncircumferential
splint immobilization (e.g., sugar tong splint) can be used initially.68,324,362
For fractures in the distal third of the forearm, below-elbow casting
has been shown to be as effective as above-elbow casting in maintenance
of satisfactory fracture alignment.63,112
Appropriate follow-up is important for these undisplaced fractures (an
initial follow-up radiograph usually is taken 7 to 14 days after
injury) because displacement may still occur for a variety of reasons:
new trauma to the extremity, male gender, and poor casting technique.68,113,290,362
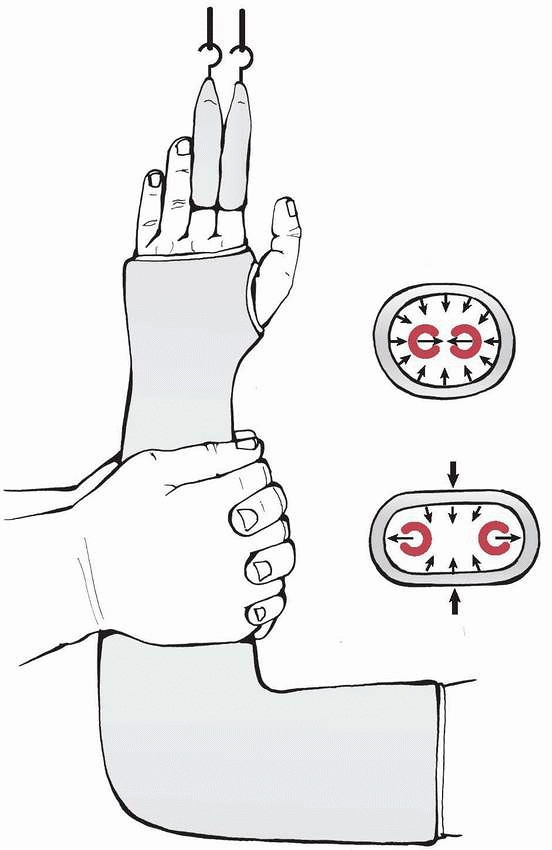
contemporary orthopaedic textbooks and sometimes is underemphasized
during orthopaedic residency training. The principles of good forearm
casting technique include: (a) interosseous molding, (b) supracondylar
molding, (c) appropriate padding, (d) evenly distributed cast material,
(e) straight ulnar border, and (f) three-point molding (Fig. 10-22).
The risk of excessive cast tightness can be minimized through the use
of the stretch-relax fiberglass casting technique described by Davids
et al.77 Chess et al.63
described a cast index for distal radial fractures defined as the
sagittal cast width divided by the coronal cast width at the level of
the fracture site; a normal ratio is considered to be 0.70. The cast
index has not been validated for forearm shaft fractures, but it
embodies the sound concept of good interosseous molding. Advanced
techniques such as pins and plaster and cast wedging also have a role
to play.18,89 Cast wedging is almost always done with an opening wedge technique because this entails less risk of soft tissue impingement.169
After informed consent for the sedation and reduction is obtained,
monitored sedation can be used in the emergency department with a
combination of narcotics and anxiolytics.173 This typically requires a dedicated nurse to administer oxygen and perform appropriate monitoring functions
(vital signs, continuous electrocardiogram, and pulse oximetry).8,9,142 Ketamine protocols also are being used with increased frequency.120,173
Young children with less than 5 or 10 degrees of angulation in the
plane of wrist and elbow motion probably do not require the additional
trauma, time, expense, and sedation risk involved in a formal reduction
because of the predictable remodeling in this age group.14
It has been shown that the more displaced the fracture, the more likely
that formal monitored sedation techniques will be used for pediatric
forearm fracture reduction as opposed to other techniques.334
 |
|
FIGURE 10-22 Interosseous mold technique.
|
pediatric forearm injuries in terms of their common fracture patterns:
bow (plastic deformation), greenstick, complete, and comminuted.
show no obvious macroscopic fracture line or cortical discontinuity,
but they do demonstrate multiple microfractures (slip lines) along the
length of the bow.279 At times, a
nearly classic buckle fracture (torus fracture) coexists with a bow
fracture. The most common clinical scenario is a plastically deformed
ulna along with a more typical fracture of the radius.198
subsequent authors stressed the importance of natural remodeling
potential in these injuries but voiced concern about this approach in
older children (especially those over 10 years of age).40,198,279 Vorlat and DeBoeck340
reported incomplete remodeling in 3 of 11 children at long-term
follow-up (average 6.7 years) after traumatic bowing of the forearm.
Because these three children were between the ages of 7 and 10 at the
time of injury, the authors recommended more aggressive efforts at
reduction in all patients with clinically significant deformity (more
than 10 degrees) older than 6 years of age.340 Traumatic bowing that causes cosmetically or functionally unacceptable angular deformity276
must be manipulated under general anesthesia or deep sedation because
strong (20 to 30 kg) gradual force applied over 2 to 3 minutes is
required to obtain acceptable alignment (Fig. 10-24).279
Application of this reductive pressure over a rolled towel, block, or
surgeon’s knee fulcrum followed by a three-point molded cast can
substantially (although at times still incompletely) correct the
deformity. Care must be taken to avoid direct pressure over adjacent
epiphyses for fear of creating a physeal fracture.
 |
|
FIGURE 10-23 Bow fracture: approximately 15 degrees of apex dorsal bowing of radius and ulna shaft.
|
diagnosis and treatment. Angulated greenstick fractures of the shafts
of the radius and ulna at different levels indicate a significant
rotational component to the injury (see Fig. 10-8).
Evans, Rang, and others have stated that the apex-volar angulation
pattern usually is associated with a supination-type injury mechanism,
while most apex-dorsal greenstick fractures involve a pronation-type
injury mechanism (Fig. 10-25),92,94,230,262 although exceptions certainly occur.92,132
Often, the apparent angular deformity can be corrected by simply
reversing the forearm rotational forces (e.g., reducing an apex-dorsal
pronation-type injury with supination).
Noonan and Price230
observed that it is difficult to remember whether to use pronation or
supination reductive forces and suggested that most fractures can be
reduced by rotating the palm toward the deformity. They also noted that
most greenstick fractures are supination injuries with apex-volar
angulation and thus can be reduced by a pronation movement.230
 |
|
FIGURE 10-24
Reduction technique of bow fracture over fulcrum. (From Sanders WE, Heckman JD. Traumatic plastic deformation of the radius and ulna: a closed method of correction of deformity. Clin Orthop 1984;188:58-67.) |
probably have little to no rotational component and are best corrected
by manipulative reduction and three-point molding techniques (see Fig. 10-9).
Charnley believed that greenstick fractures of the forearm in children
perfectly illustrated his dictum that “A curved plaster is necessary in
order to make a straight limb.”61 He
also stated that “The unsuspected recurrence of angular deformity in
greenstick fractures of the forearm, while concealed in plaster, is an
annoying event if it takes the surgeon by surprise and is not
discovered until the plaster is removed. Parents, quite understandably,
may be more annoyed about this happening to their children than if it
had happened to themselves, and do not easily forgive the surgeon.”61
Despite these concerns, it is clear from large published reports that
greenstick fractures can almost always be successfully treated with
nonoperative methods.365
 |
|
FIGURE 10-25 Shaft fractures at different levels implies rotational mechanism. A. Apex-volar angulation with supination deformity of the forearm. B. Apex-dorsal angulation with pronation deformity of forearm.
|
regarding greenstick fracture reduction: one in which the greenstick
fracture is purposely completed and another in which it is not. Those
who favor completing the fracture (dating back at least to the 1859
work of Malgaigne) cite concerns about lost reduction and recurrent
deformity that can be prevented only by converting the greenstick into
a complete fracture.24,36,103,152 Others prefer to maintain and perhaps exploit some of the inherent stability of the greenstick fracture.6,63,80,92,322
In addition to the traditional view that loss of reduction is less
likely if a greenstick fracture is completed, there also is the
theoretical advantage of a lower refracture rate because of more
exuberant callus formation.63,230 To the best of our knowledge, these theories have not been validated in any controlled clinical studies. Davis and Green80
advocated a derotational approach to greenstick fracture reduction and
reported a 10% (16/151) reangulation rate in their series of patients
with greenstick fracture. They compared this to the 25% (12/47)
reangulation rate in patients with complete fractures and questioned
the wisdom of routinely completing greenstick fractures.80 In a prospective study, Boyer et al.44 showed statistically that greenstick fractures maintain their reduction better than complete forearm fractures.
the forearm behave differently from a clinical perspective and have
classically been divided into distal-, middle-, and proximal-third
fractures. Single-bone complete fractures usually are caused by direct
trauma (nightstick fracture) and are difficult to reduce. Blount
described a reduction technique that may be effective for reduction of
a displaced single-bone shaft fracture.34
The intact bone is used as a lever to re-establish length of the
fractured bone, and then transverse forces are applied to realign the
bone ends (see Fig. 10-11). Both-bone complete
fractures (often with bayonet shortening) are common and are best
treated with finger-trap or arm traction applied over 5 to 10 minutes.
This stretches out the soft tissue envelope and aids in both reduction
and cast or splint application. Traction allows complete fractures to
“seek their own level of rotation” and allows correction of rotational
malalignment.80
been an area of debate since the days of Hippocrates.36
Theoretically, the position of forearm rotation in an above-elbow cast
or splint affects rotational alignment of complete fractures at all
levels; however, a study of distal-third forearm fractures found no
significant effect of forearm rotation position on ultimate alignment.44
We are aware of no similar studies analyzing the effects of forearm
position on middle- or proximal-third shaft fractures, and treatment is
influenced by certain anatomic considerations. Because of the strong
supination pull of the biceps, aided by the supinator, complete
proximal radial fractures may be best immobilized in supination so that
the distal forearm rotation matches that of the proximal forearm (see Fig. 10-19).
The position of immobilization of fractures in the middle third of the
forearm commonly is dictated by whether the radial fracture occurs
distal or proximal to the insertion of the pronator teres. Fractures
proximal to its insertion are best treated by fully supinating the
distal fragment, while those distal to its insertion are probably best
treated in a neutral position.
first 2 to 3 weeks because most position loss can be recognized and
corrected during this time.179,341
Any significant shift in position between visits necessitates cast
wedging or a cast change, with remolding and possible fracture
remanipulation if unacceptable displacement is present. Voto et al.341 found that, in general, 7% of forearm fractures redisplace; this can occur up to 24 days after the initial manipulation. Davis80
reported a 25% reangulation rate in complete fractures. Remanipulation
can be done in the office following administration of oral analgesics.
Judicious use of benzodiazepines may also be valuable because of their
anxiolytic effects.
changed to a below-elbow cast after 3 to 4 weeks, this is unnecessary
in most children because they heal more quickly and permanent elbow
stiffness is rare.171 A cast change
at week 3 or 4 also can be traumatic to a young child and carries the
additional small risk of cast saw injury. Once the fracture shows good
callus formation, the cast can be removed. Because shaft fractures of
the radius and ulna in children have a significant rate of refracture,15,181,326 they should be splinted for an additional period of time.67 Parents should be warned of the risk of refracture.
suggested for some complete fractures of the middle and proximal thirds.293,344,348 The supination moment exerted by the biceps has been shown to be diminished when the elbow is extended.224 Walker and Rang344
reported successful treatment of 13 middle- or proximal-third forearm
shaft fractures with this method (some following failed flexed-elbow
casting). They suggested that the “short fat forearms” of some young
children prevented successful flexed-elbow casting.344 Shaer et al.293
also reported 20 children treated with this method and emphasized full
supination of the forearm. Three of their patients required cast
wedging, but at final follow-up 19 of the 20 patients had excellent
results.293 One patient who was lost to follow-up for 6 months (presumably removing his own cast) did suffer “mild residual deformity.”293 Walker and Rang344
recommended that benzoin be applied to the skin, in addition to
creation of an adequate supracondylar mold, to further secure the cast.
Casting the thumb in abduction with extra padding may prevent the cast
from sliding. Turco330 suggested
that reduction should be obtained with horizontal traction applied to
the extended upper extremity, followed by additional steps outlined in Table 10-5. Based on published clinical results, concerns related to cast slippage and elbow stiffness appear to have been overstated.293,344 The main drawback of this technique is its awkwardness as compared to flexed-elbow casting.344
|
TABLE 10-5 Turco Technique for Extended Elbow Cast Treatment
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
Comminuted forearm fractures deserve special attention because they
often require specially tailored treatment approaches. If satisfactory
reduction cannot be achieved or maintained by closed methods, then
other treatment alternatives should be considered.
this may help maintain motion through interosseous membrane slackening.
Shortening of more than 1 cm is unacceptable in either single-bone or
both-bone comminuted patterns. Standard closed fracture treatment
generally is unsuccessful when both bones are comminuted, and surgical
stabilization may be necessary.103 Bellemans and Lamoureux25
reported intramedullary nailing of all comminuted forearm fractures in
their pediatric series. Other reported fixation methods for comminuted
forearm fractures in children include plate-and-screw devices,103,104 flexible intramedullary nailing for single-bone comminution,269 and pins-and-plaster techniques.342 Bone grafting is rarely if ever indicated in acute comminuted forearm features in children.
cited an “aggressive surgical mentality” as the reason for frequent
operative treatment of pediatric forearm fractures, and Wilkins352 expressed concern about “impetuous” surgeons who are too eager to operate. Cheng et al.62
documented a more than 10-fold increase in the rate of operative
treatment of forearm shaft fractures in children, but it is unclear as
to whether this increase in operative treatment has led to a
commensurate improvement in clinical outcomes.
usually is reserved for open fractures, those associated with
compartment syndrome, floating elbow injuries, and fractures that
develop unacceptable displacement during nonoperative management.
Residual angulation after closed treatment is much better tolerated by
younger children than older adolescents and adults because of the
increased remodeling potential in the younger age group.168
As a consequence, adolescents are more likely to benefit from surgical
treatment of their forearm fractures than are younger children.
Although internal fixation is the standard of care for displaced
forearm fractures in adults, the success of nonoperative methods and
the complications associated with internal fixation have tempered
enthusiasm for its application to pediatric forearm fractures. Compared
to closed treatment methods, healing is slower after open reduction and
internal fixation,25 no matter what type of implant is used.103
Crossed Kirschner wire fixation techniques that often are used
successfully in the distal radius are technically difficult in the
shaft region of the radius and ulna. In rare situations, external
fixation has been used for pediatric forearm fixation.291
surgical technique is chosen. Assessment of the fracture, including
rotation and the presence or absence of comminution, is important.
Bone-plate mismatch (due to narrow bones and wide plates) and extensive
soft tissue dissection are risks when adult-sized plates are applied to
pediatric bones.356 Before
intramedullary nailing of fractures, the forearm intramedullary canal
diameter should be measured, especially at the narrowest canal
dimension; typically this is the central portion of the radius305
and the distal portion of the ulna near the junction of its middle and
distal thirds. Precise canal measurement can be difficult,277,306
and the consequences of a nail or pin that is too large are probably worse than those of a nail or pin that is too small.234,288 Modern digital radiography systems have made these measurements easier.242
forearm shaft fractures with plates and screws is a well-documented
procedure in both pediatric series240,310,323,333 and adult series that include patients as young as 1360 and even 760 years of age. In one of the early series of pediatric forearm fractures fixed with plates,83
dynamic compression plates and one-third tubular plates applied with
standard atlas orthogonal technique (six cortices above and below the
fracture site) obtained good results.227 Four-cortex fixation on either side of the fracture site has been shown to be equally effective in pediatric forearm fractures.358
technique except that smaller plates (2.7-mm compression and stacked
one-third tubular), fewer screws, and single-bone fixation often are
acceptable.358 Plate fixation may
allow more anatomic and stable correction of rotational and angular
abnormalities and restoration of the radial bow than with noncontoured
intramedullary rods; however, the larger incisions and extensive
surgical exposures required for plate fixation have raised concerns
regarding unsightly scars275,333,356 and muscle fibrosis with consequent motion loss.358
While the cosmetic concerns seem valid, ultimate forearm motion is
similar with the two techniques, with only minor losses reported in the
literature after both plating and intramedullary nailing.74,168,297,332 Fernandez et al.97
recently documented these precise issues very nicely in that they found
no significant differences in functional outcome in their plate
fixation versus intramedullary nailing patients, but they noted the
longer operating room time and inferior cosmesis of the plated patients.
screws may be appropriate in the management of fractures with delayed
presentation or fractures that angulate late in the course of cast care,135,358
when significant fracture callus makes closed reduction and
percutaneous passage of intramedullary nails difficult or impossible.13 Other indications for plate fixation include shaft fractures with significant comminution103 and impending or established malunion329 or nonunion.136,189,234 Several authors have reported good results with plate fixation of the radius only50,105,240,262 or the ulna only (Fig. 10-26).26 Bhaskar and Roberts26
compared 20 children with both-bone plate fixation to 12 with ulna-only
fixation and found significantly more complications in the dual plating
group, although motion was equal at 1-year follow-up. Single-bone
fixation requires satisfactory reduction of both bones. Flynn and Waters105
stated that they would preferentially plate the radius only when the
fracture could not be reduced by closed means. Two patients in Bhaskar
and Roberts’26 study required open
reduction and internal fixation of the radius when it was not
adequately reduced after plate fixation of the ulna.
Intramedullary fixation of children’s forearm fractures dates back at
least to Fleischer’s 1975 report in the German literature in which he
called it “marrow wiring.”101 Closed
intramedullary nailing (also known as indirect reduction and internal
fixation) of diaphyseal forearm fractures in adolescents was later
reported in the English language literature by Ligier et al.,191 Amit et al.,10 and others.30,184,356
A variety of implants have been used for forearm intramedullary
nailing, including Kirschner wires, Rush rods, and Steinmann pins.
Continued favorable reports from around the world (e.g., England,
Germany, New Zealand, Turkey, and the United States) have established
intramedullary fixation as the surgical treatment of choice.56,115,162,188,267
plate fixation, including improved cosmesis because of smaller
incisions and less deep tissue dissection, potentially leading to a
lower risk of stiffness.74,180,297,356 Contoured pins are used in the radius to preserve its natural anatomic bow10,74,259,267,346; contoured pins are not necessary for the ulna.10
Although the rotational stability of pediatric forearm fractures
treated with intramedullary fixation has been questioned, Blasier and
Salaman30 suggested that the strong
periosteum in children resists torsional stresses. In a cadaver study
of the rotational stability of fractures of the ulna and radius treated
with Rush rods, Ono et al.238 found that intramedullary fixation of both bones reduced fracture rotation to one eighth of that in unfixed fractures.
with small-diameter (1.5- to 2.5-mm) contoured implants.191 No effort was made to fill the medullary canal as with other intramedullary nailing techniques,269 and the “summit of the curve must be calculated preoperatively to lie at the level of the fracture.”184
The prebent flexible rods (known as Nancy nails) were reported to
maintain satisfactory fracture alignment while encouraging development
of normal physiologic fracture callus.191,216,251
Biomechanically, these implants have been shown to act as internal
splints provided the nails extend three or more diameters beyond the
fracture site.158 Good results with this technique have been reported by numerous authors (Figs. 10-27 and 10-28).131,225,269,287,294,325,328,357
 |
|
FIGURE 10-26 Single-bone plate fixation (radius only). A. A 12-year-old female with both-bone forearm fracture (AP and lateral). B. Immediate postoperative images. C. Two-year follow-up images. (Courtesy of Tom Welle, DO.)
|
bones are internally fixed.184
It also is dependent on anchorage of the nails in the upper and lower
metaphyseal portions of the bone to produce an internal three-point
fixation construct.184 Technique
principles include fixing first the bone that is easiest to reduce,
using physeal-sparing entry points, and using small nails varying in
diameter from 1.5 to 2.5 mm.184 A nail that is too large may lead to nail incarceration and distraction at the fracture site, especially in the ulna.234 Contouring of both nails is recommended, with particular attention to restoration of the appropriate radial bow (Fig. 10-29).
Initially, nails were removed by about the fourth postoperative month,
but several refractures led the originators of the technique to delay
nail removal until 1 full year after surgery.184 Pin ends should be cut short and buried to maintain prolonged fixation.
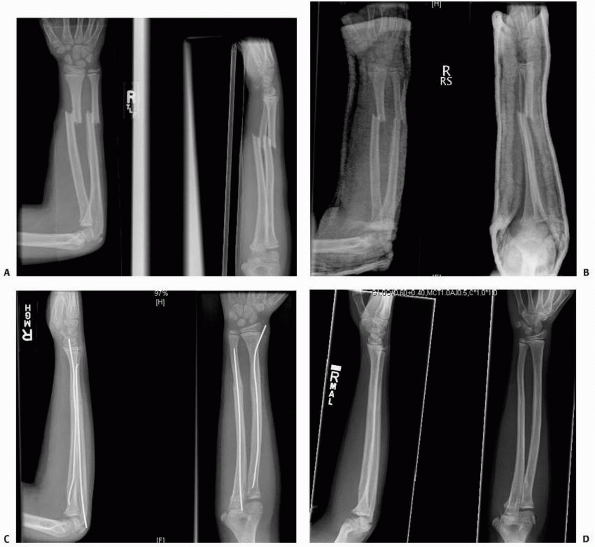 |
|
FIGURE 10-27
A 10-year-old male whose both-bone complete forearm fracture near the junction of the middle and distal thirds was treated with elastic stable intramedullary nailing. A. Injury radiographs demonstrating completely displaced radial and ulnar shaft fractures. B. Postreduction radiographs reveal unsatisfactory angular alignment as well as significant loss of radial bow. C. Anatomic appearance following ESIN. D. One and a half year follow-up radiographs. Nails were removed 6 months postoperatively. (continues) |
considered displaced oblique or comminuted midshaft forearm fractures
in children older than 7 years of age to be an indication for ESIN.
They considered bayonet apposition (overriding) to be unacceptable at
any age because of concerns about rotational malalignment and frequent
narrowing of the interosseous space.25 Their fixation technique
involved passage of the intramedullary nails followed by rotation of
each nail until the greatest distance between the two bones was
achieved in full supination.25
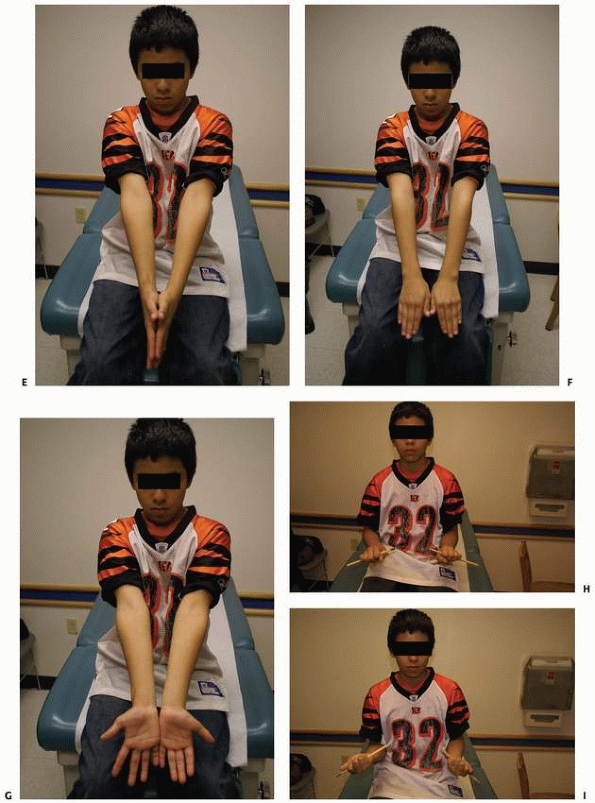 |
|
FIGURE 10-27 (continued) E. Clinical appearance with extended elbows and forearm midposition. F. Clinical appearance with extended elbows and pronated forearms. G. Clinical appearance with extended elbows and supinated forearms. H. Symmetrical pronation. I. Symmetrical supination.
|
 |
|
FIGURE 10-28
An 11-year-old male whose both-bone midshaft complete forearm shaft fracture was treated with elastic stable intramedullary nailing. A. Injury AP radiograph. B. Injury lateral radiograph. C. Postreduction radiographs demonstrating unacceptable angular alignment. D. Improved alignment status ater ESIN. E. Clinical appearance with extended elbows and forearm midposition. (continues) |
 |
|
FIGURE 10-28 (continued) F. Clinical appearance with extended elbows and pronated forearms. G. Clinical appearance with extended elbows and supinated forearms. H. Symmetrical pronation. I. Symmetrical supination. (continues)
|
shafts of the radius and ulna and open tibial shaft fractures occurred
with equal frequency, making them the most common open fractures in
children.62 Although the infection
rate is extremely low for open fractures, even grade I open forearm
fractures in children have been associated with serious complications
such as gas gangrene.96 Early irrigation and débridement212,302 are indicated for open forearm fractures, and care should be taken to inspect and properly clean the bone ends.165 Roy and Crawford275 recommended routinely inspecting both of the bone ends for the presence of intramedullary foreign material (Fig. 10-30).
Once débrided, open forearm fractures can be stabilized by any of the
available internal fixation methods without undue risk of infection (Fig. 10-31).128,135,195
Open fractures tend to be more unstable than closed fractures (because
of soft tissue stripping and comminution) and more commonly require
internal fixation. Internal fixation also may facilitate soft tissue
management and healing.358 Professor Lim192 and his co-authors
from the KK Children’s Hospital in Singapore recently reminded us that
internal fixation is not an absolute prerequisite and many children
with such open fractures may still be successfully managed with casting
alone.
 |
|
FIGURE 10-28 (continued) J. Thirty-nine month follow-up AP wrist radiograph and lateral (K) wrist radiograph (taken due to new trauma) demonstrating normal bony anatomy. Nails were removed 6 months postoperatively.
|
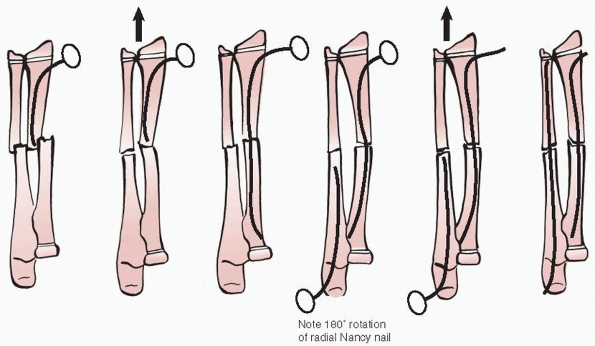 |
|
FIGURE 10-29
Metaizeau elastic stable intramedullary nailing technique. The radial rod is twisted 180 degrees in step 4 to re-establish the radial bow. |
 |
|
FIGURE 10-30 Intramedullary organic contamination of an open forearm fractures.
|
body reaction associated with open forearm fractures may produce an
unusual radiographic appearance: the “ruffled border sign” (Fig. 10-32).
Usually, this seems to represent a normal healing response in growing
children, but occasionally it is an early sign of osteomyelitis. The
infection rate ranges from 0% to 33% for open fractures in children.128,74,128,135,179,195,230,240,255,358
Even grade I open forearm fractures in children can be complicated by
gas gangrene or osteomyelitis, and therapeutic amputation has been
reported.80,96,152
Open fracture grade does not appear to correlate with the infection
rate in childhood forearm fractures, with most of the serious forearm
infections reported in the literature occurring after grade I fractures.
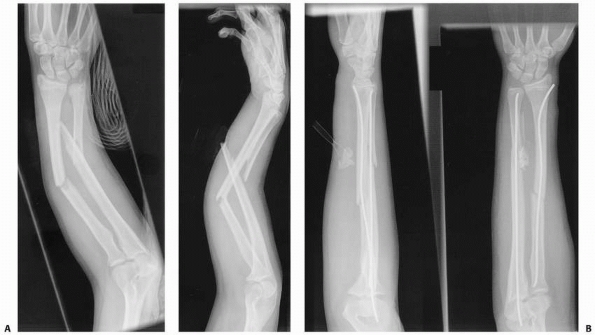 |
|
FIGURE 10-31 A 13-year-old female with open forearm fracture. A. AP and lateral radiographs; note extrusion of ulna on lateral view. B. After irrigation and débridement and flexible nail internal fixation. Note the Penrose drain in the ulnar wound.
|
still remains the gold standard for closed isolated pediatric forearm
fractures.”161 Most nondisplaced and
minimally displaced radial and ulnar shaft fractures can be splinted in
the emergency department and referred for orthopaedic follow-up within
1 week. Radiographs are repeated at the first orthopaedic visit, and a
cast is applied. During warmer weather, when fracture incidence peaks,
we tend to use waterproof cast liners. We avoid flexing the elbow past
80 to 90 degrees in waterproof casts because the soft tissue crease
that forms in the antecubital fossa tends to trap moisture. Because
waterproof cast lining alone does not shield the skin from cast saw
cuts and burns as well as traditional padding does, specialized
material may be added along the anticipated
course
of the cast saw to protect the skin during cast removal. Two such
materials are blue cast strips (De-Flex Strip Cast Removal Aid, WL Gore
& Associates, Flagstaff, AZ) and a plastic zipstrip (inserted
between the skin and cast liner).
 |
|
FIGURE 10-32 Ruffled border sign at the site of previous open fracture of ulna; same patient from Figure 10-28 at 1-month follow-up.
|
in children under the age of 4 years, because young children tend to
lose or remove a below-elbow cast due to soft tissue differences (baby
fat) common to the age group.86 Most
older children with forearm shaft fractures also are treated with
above-elbow casting, except for those with stable distal-third
fractures. Good forearm casting technique should focus on the
principles outlined earlier in this chapter. Patients with nondisplaced
fractures usually are re-evaluated radiographically in 1 to 2 weeks
after initial immobilization to check for fracture displacement.
Forearm shaft fractures heal more slowly than metaphyseal and physeal
fractures of the distal radius and ulna.15,80
The cast is removed in 6 to 8 weeks if adequate healing is present on
radiographs. Because of the significant refracture rate after forearm
shaft fractures, we splint these fractures for another several weeks
until all transverse lucency of the original fracture disappears and
all four cortices are healed. Fractures that heal in bayonet apposition
(complete translation and some shortening) can take longer to heal than
those with end-to-end apposition and may require prolonged splinting to
prevent refracture.86,273
usually manipulated in the emergency department using a conscious
sedation protocol. After obtaining informed consent for conscious
sedation and fracture manipulation, an intravenous line is started, and
the child’s blood pressure, pulse, respirations, electrocardiogram, and
peripheral oxygen level are monitored during the procedure and for
about 30 minutes after the procedure. We use ketamine and midazolam
administered intravenously in divided doses. Although many children
moan or cry briefly during the manipulation, very few recall pain.
Reductions are done under mini-C-arm (fluoroscopy) control. The initial
position of forearm rotation is based on the level of the fracture, and
the final position is based on the best reduction under fluoroscopy.
Small portable fluoroscopy units save time and money (estimated to be
10% of the cost of conventional radiographs) and lessen radiation
dosage to patient and clinician compared to traditional fluoroscopy.
Finger-trap traction with 10 to 15 pounds of counterweight frequently
is used for completely displaced both-bone forearm fractures
(especially those with shortening). We do not complete greenstick
fractures because the partial bone continuity adds stability.
manipulated fractures are placed into a plaster sugar-tong splint
(incorporating the elbow). Before manipulation, the sugar-tong splint
is prepared by laying out 7 to 10 layers of appropriate-length 3-inch
plaster casting material on top of a work surface. A four-layer matched
length of cotton cast padding also is laid out and will form the inner
padding (skin side) of the splint. A final single layer of cast padding
is laid out and will form the outer layer of the splint to prevent
elastic wrap adherence to the plaster. Once manipulation is completed,
the plaster is dipped, wrung out, smoothed, and then sandwiched between
the dry four-ply and one-ply cotton padding. This splint is then placed
with the four-ply cotton side against the skin and secured with an
elastic bandage. We prefer to avoid the circumferential application of
cotton padding because it may limit splint expansion during follow-up
swelling. If necessary, parents also can unwrap and loosen the elastic
bandage at home to relieve pressure if swelling makes the splint too
tight. Patients are given discharge instructions and a prescription for
mild narcotic analgesics.
repeat radiographs and clinical assessment. Provided that satisfactory
alignment has been maintained, we remove the elastic wrap but leave the
plaster sugar-tong splint in place. The splint is “boxed in” by
applying cotton cast padding over the splint and the exposed upper arm,
and by wrapping with fiberglass to convert the splint into an
above-elbow cast. Follow-up radiographs are taken of manipulated
fractures at about 1-week intervals for the next 2 weeks. Fractures
that are losing position but are still in acceptable alignment usually
require removal and remolding of a new cast to prevent further position
deterioration. Minor remanipulations can be done in the office after
appropriate administration of oral analgesics and anxiolytics. Major
remanipulations are best done with general anesthesia. The decision
regarding remanipulation may be aided by the viewing of the cosmetic
deformity by the parents and physician after all splint and cast
materials are removed.
above-elbow casts can be converted to below-elbow casts (often a
waterproof cast in warm weather). This step may be omitted in younger
children because of their faster healing and their
minimal inconvenience from temporary elbow immobilization.171
Patients can return to sports after conversion to a below-elbow cast as
long as the cast is padded during play and league rules allow casts.
Patients usually are required to have a physician’s note allowing
sports participation with a cast. This decision is made with the
patient’s and parents’ understanding of potential increase in
refracture risk. Adequate fracture healing (bridging callus of four
cortices) usually has occurred after several more weeks of cast
treatment but should be confirmed by radiographic and physical
examination before unlimited athletic participation. Older children are
given home elastic band strengthening exercises and allowed to
participate in normal activities while they continue to be protected in
either a removable Velcro fracture brace or a customized thermoplastic
forearm gauntlet brace. Formal physical therapy rarely is required.
This fracture protocol is aimed at minimizing refracture risk.
approximately 20 degrees of angulation in distal-third shaft fractures
of the radius and ulna, 15 degrees at the midshaft level, and 10
degrees in the proximal third (provided the child has at least 2 years
of growth remaining).361 We accept
100% translation if shortening is less than 1 cm. Although other
authors recommend accepting up to 45 degrees of rotation, we find this
is extremely difficult to measure accurately using the bicipital
tuberosity and radial styloid as landmarks because of the lack of
anatomic distinction in younger children. Plastic deformation fractures
seem to have less remodeling potential than other fractures, and
radiographically or cosmetically unacceptable angulation may require
gradual, forceful manipulation under sedation or general anesthesia.
Children approaching skeletal maturity (less than 2 years of remaining
growth) should be treated using adult criteria because of their reduced
remodeling potential. Parents should be cautioned that even mild
angulation of the ulna, especially posterior sag, will produce an
obvious deformity after cast removal because of the subcutaneous
location of the bone (Fig. 10-33). This
cosmetic deformity is exacerbated by abundant callus formation, but it
will ultimately remodel if it falls within acceptable angulation
criteria. Ulnar sag may be countered by placing the child in an
extended elbow cast. Mild to moderate angulation of the radius usually
produces much less cosmetic deformity but may limit motion more (Fig. 10-34).
treated with closed methods at our institution. Our top two indications
for surgical treatment of these injuries are open shaft fractures and
shaft fractures that exceed our stated reduction limits. If surgical
treatment is deemed necessary, intramedullary fixation is preferred
over plate fixation because of reduced soft tissue disruption. We
occasionally fix one bone when both bones are fractured if overall
forearm alignment is acceptable and stable after single-bone fixation.
treated first because of its more benign entry site, subcutaneous
location, and relatively straight canal compared to the radius. Our
preferred intramedullary ulnar entry site is just distal to the
olecranon apophysis (anconeus starting point), just anterior to the
subcutaneous border of the proximal ulna on its lateral side. Care is
taken not to enter the ulna more than 5 mm anterior to its subcutaneous
crest to avoid encroachment into the region of the proximal radioulnar
joint. Pins placed directly through the tip of the olecranon apophysis
have a strong tendency to cause bursitis and pain until removal. We
prefer to open the cortex with an awl because it tends to wander less
than motorized drills and it allows ulnar entry with little or no
formal incision. The awl technique also simplifies operating room setup
in that no pneumatic hose hookups or battery packs are necessary.
 |
|
FIGURE 10-33 Ulnar sag on serial radiographs. Note the prominent ulnar fracture callus.
|
fixed first as it is usually more difficult. The distal radial entry
site can be either through a physeal-sparing direct lateral approach
through the floor of the first dorsal compartment or dorsally near the
proximal extent of the Lister tubercle between the second and third
dorsal compartments. Both of these entry points are approximately 1 cm
proximal to the physis of the distal radius. We insert the radial nail
through a 1- to 2-cm incision, protecting the superficial radial nerve
and the dorsal tendons with small blunt retractors. An awl is used to
gain intramedullary access to the radius. We typically use small
intramedullary nails (2.0 to 2.5 mm in diameter) to maintain some
flexibility at the fracture site and stimulate appropriate callus
formation. Larger nails may become incarcerated in either the narrow
central canal of the radius or that of the distal third of the ulna.
Care must be taken
to
not overbend the tip of the nail as this effectively increases the
diameter of the implant and may impede its intramedullary passage.
Failure to pass the intramedullary nail across the fracture site after
several attempts may necessitate a limited open reduction through a 1-
to 2-cm incision to directly pass the rod across the fracture site (Fig. 10-35). Persistence in attempting to achieve closed reduction and rodding has been associated with compartment syndrome.363
We are sensitive to both time and attempts during ESIN of forearm shaft
fractures in our pediatric patients and recommend adherence to the
17-minute rule (taught to us by our senior partner Alvin Crawford) and
the three strikes and you are out rule. If either closed reduction
attempts for a particular forearm bone exceed 17 minutes or if three
low-amplitude efforts to pass the intramedullary nail across the
fracture site have been unsuccessful, then rapid conversion to a small
open reduction is suggested.
 |
|
FIGURE 10-34 A 7-year-old female with left both-bone complete forearm fracture. A. AP and lateral injury radiographs. B. Two-month follow-up radiographs. C. Two-year follow-up radiograph shows mild residual deformity. D. Pronation. (continues)
|
 |
|
FIGURE 10-34 (continued) E. Supination. F. Axial alignment at 2-year follow-up. G. Five-year follow-up radiographs of left forearm with mild loss of radial bow. H. Comparison radiographs of right forearm. (continues)
|
 |
|
FIGURE 10-34 (continued) I. Pronation. J. Supination. K. Axial alignment at 5-year follow-up.
|
because complete fracture healing takes at least 2 months, often more.
Because refracture can even occur with nails in place, we protect
children for at least the first month with a removable fracture brace.
If a single bone of a both-bone fracture is fixed, above-elbow cast
immobilization usually is necessary instead of a below-elbow cast or
brace, as is used after dual-bone fixation. After the appearance of
satisfactory callus, splint and activity restrictions are progressively
relaxed. We recommend nail removal after complete four-cortex healing
of each bone (6 to 12 months in some patients).
early malunion is present and callus formation is noted
radiographically. Plating allows open osteoclasis and reduction. The
plating technique is similar to that used in adults, except that
smaller plates can be used and fewer cortices (often only four cortices
above and below the fracture) are required for adequate fixation. In
children with both-bone forearm fractures, plating of a single bone may
be adequate and reduce the morbidity associated with dual-bone plating.26 Significant comminution of both bones also may be an indication for plate fixation.
fracture treatment is loss of satisfactory reduction in a previously
well-reduced and well-aligned fracture, a complication that occurs in
10%58,65,80,161,342 to 25% of patients.58,80 Initial follow-up radiographs are a screening test aimed at identifying redisplacement. Kramhoft and Solgaard179
recommended that children with displaced diaphyseal forearm fractures
have screening radiography at 1 and 2 weeks after reduction. Voto171
also pointed out that most fractures that redisplace do so within the
first 2 weeks after injury. Inability to properly control fracture
alignment with closed methods is the most commonly reported indication
for operative intervention.188,259,275,297,365
reduction are cast related (poor casting technique, no evidence of
three-point molding).63,342 The more experienced the surgeon, the greater the likelihood of successful reduction.58 Other factors that have been found to be associated with forearm fracture redisplacement are quality of initial reduction,362 missed follow-up appointments,68 proximal-third fractures,72 and failure of the doctor to respond to early warning signs such as slight loss of reduction at 1-week follow-up.113 Strategies for dealing with redisplacement include allowing the deformity to remodel,143 cast wedging,18,152,169 rereduction and recasting,80,342 pins and
plaster,33,89,342 indirect reduction and internal fixation,10 and open reduction and internal fixation.358
Reports in the literature suggest that most forearm shaft fractures
that redisplace can be successfully managed with repeat closed
reduction and casting.80,342
 |
|
FIGURE 10-35 A 12-year-old female with midshaft both-bone complete forearm fracture. A. AP and lateral injury radiographs. B. Two-month follow-up radiographs. C. Six-month follow-up radiographs (ulnar nail removed). (continues)
|
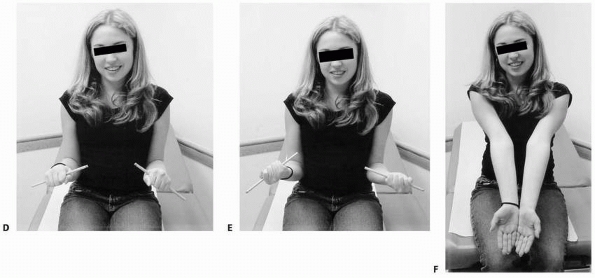 |
|
FIGURE 10-35 (continued) D. Pronation. E. Supination. F. Axial alignment.
|
highamplitude motion as its main function. The most common long-term
complication of forearm shaft fracture treatment is significant forearm
stiffness,143 with pronation loss occurring almost twice as frequently as supination loss.144 Loss of pronation or supination motion sometimes occurs despite perfectly normalappearing radiographs.168,229,255 Abnormal bony alignment of the forearm bones leads to predictable motion deficits.166 Stiffness that exceeds that expected from bony malalignment alone166
and stiffness that occurs with normal radiographs are indications of
fibrosis of the interosseous membrane or contracture of the
interosseous ligament.168,255
of patients show at least some minor deficits after nonsurgical
treatment. Most minor deficits are not even noticed by patients and
rarely are associated with functional limitations.52,76,229 More severe losses of forearm rotation have far greater impact.219 In their series of malunited forearm fractures (thus strongly weighted to demonstrate forearm stiffness), Price et al.255
reported a 15% (6/39) rate of mild stiffness (up to 25-degree loss) and
an 8% (3/39) rate of severe forearm stiffness (loss of 45 degrees or
more of either pronation or supination). Holdsworth’s144 series of malunited pediatric forearm fractures had a similar rate (6%) of severe forearm stiffness. Holdsworth144
told the classic story of a female whose inability to properly pronate
caused her to elbow her neighbors when eating at the table. Patrick243
pointed out that it is possible to compensate for pronation losses with
shoulder abduction, but no similar compensation mechanism exists for
supination losses. Such severe motion loss is a very undesirable
outcome. For surgical treatment of these injuries to be a rational
choice, the rates of stiffness after surgery must be lower than those
after cast treatment.130
published one of the only studies of plated pediatric forearm fractures
to report goniometric pronation and supination data. Both their
single-bone (ulna) and both-bone plated patients showed mild forearm
motion losses (maximal 18% loss of pronation).26 Variable rates of mild forearm range-of-motion losses have been reported after intramedullary fixation. Amit et al.10
reported a 40% rate of mild stiffness (5 to 10 degrees) in 20 pediatric
patients after Rush rod fixation of forearm fractures. Combined data
from five series of the flexible intramedullary nailing (Kirschner
wires, Steinmann pins, Nancy nails) reveal a 1.6% rate (2/128) of mild
forearm stiffness (up to a 20-degree loss) and a 0% (0/128) rate of
severe motion loss (40 degrees or more loss of either pronation or
supination).10,25,98180,297,365
No published series of nonoperatively treated forearm shaft fracture
patients has exceeded these results relative to preservation of forearm
motion.
found that forearm refractures occurred at an average of 6 months after
original injury and were more common in males (3:1) and in older
children (approximately 12 years old). Refracture rates of 4%98 to 8%193 have been reported in pediatric diaphyseal forearm fractures. Bould and Bannister43
reported that diaphyseal forearm fractures were eight times more likely
to refracture than metaphyseal fractures. Schwarz et al.292
found that 84% (21/28) of the forearm refractures in their series had
initially presented as greenstick fractures. Based on the stage of bony
healing, refractures may occur through the original fracture site,
through both the original site and partially through intact bone or
completely through intact bone,350 but most seem to occur through the original fracture site.
17 patients with refractures. Closed reduction also has been shown to
be effective for forearm refractures that occur with flexible nails in
place (Fig. 10-36).222
The best treatment of refracture is prevention, and patients should be
splint-protected (removable forearm splint or thermoplastic gauntlet)
for a period of 2 months depending on activity after initial bone
healing.230,255
Refracture is rare during splint wear. Parents must be cautioned about
the risk of refracture despite apparently adequate bone healing on
radiographs.
The main strategies aimed at decreasing the risk of refractures after
implant removal are documentation of adequate bony healing before
implant removal, and an additional period of splint protection after
implant removal until the holes have filled in.
 |
|
FIGURE 10-36 A 14-year-old ESIN patient who suffered refracture with the nails in place. A. Injury AP radiograph. B. Injury lateral radiograph. Skateboard mechanism. C. Early postoperative radiographs status post ESIN. D. Two months postoperative AP radiograph. (continues)
|
remodeling potential. Thus, a malunion of 30 degrees may become less
than 10 degrees during the course of follow-up. The level of the
malunited fracture also must be considered, because the consequences of
malreduction vary according to level.280,361
More deformity in the predominant plane of motion is acceptable in
fractures near physes of long bones than in diaphyseal fractures.
Normal motion can be preserved despite persistent radiographic
abnormality (Fig. 10-37).
 |
|
FIGURE 10-36 (continued) E. Two months postoperative lateral radiograph. F. Refracture at 2.5 months postoperative. G. Refracture elbow radiograph. H. Closed reduction of titanium nails and angulated radius and ulna fractures. (continues)
|
 |
|
FIGURE 10-36 (continued) I. Five months after refracture. J. AP radiograph 1 year after refracture. K. Lateral radiograph 1 year after refracture. L. Clinical appearance with extended elbows and forearm midposition. (continues)
|
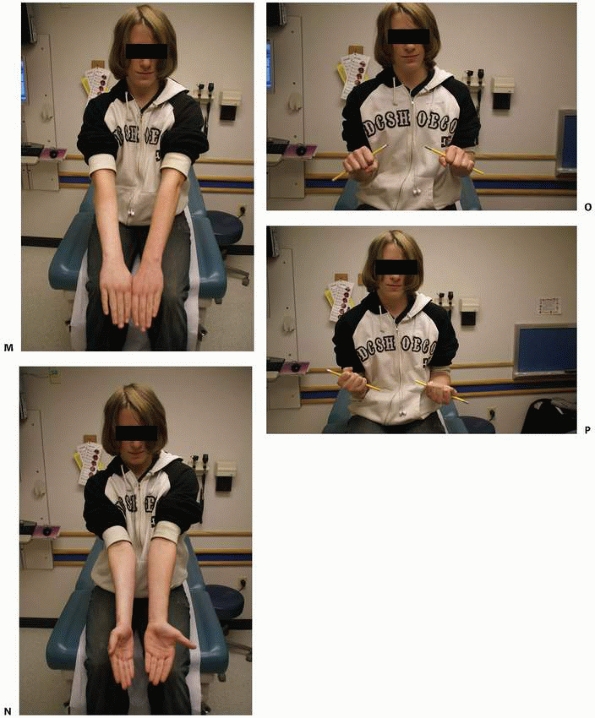 |
|
FIGURE 10-36 (continued) M. Clinical appearance with extended elbows and pronated forearms. N. Clinical appearance with extended elbows and supinated forearms. Note mild supination loss on right. O. Symmetrical pronation. P. Asymmetrical supination. Approximately 15 degree loss on right.
|
cosmetic deformity and loss of motion; however, significant loss of
function occurs in only a small percentage of patients.52,76,229 Some authors have recommended more aggressive efforts at correction of forearm fracture malunions.214,253
Early malunions (up to 4 or 5 weeks after injury) can be treated with
closed osteoclasis under anesthesia. If closed osteoclasis fails to
adequately mobilize the fracture, a minimally invasive drill
osteoclasis can be done.29 A small-diameter drill (or Kirschner wire) is used to make multiple holes in the region of the malunion
before forcefully manipulating the bone back into alignment.29 Internal fixation is rarely, if ever, needed.
 |
|
FIGURE 10-37 An 11-year-old with midshaft both-bone complete forearm fracture. A. AP and lateral injury radiographs. B. One-month follow-up radiographs. C. Two-year follow-up radiogaphs. D. Pronation. E. Supination. (continues)
|
and internal fixation with flexible intramedullary nails can be
difficult or impossible because the fracture site is now blocked with
callus. Thus, established or impending malunions that cannot be
adequately controlled with a cast may require formal open reduction and
plate fixation (Figs. 10-38 and 10-39).
Many fractures that heal with angulation or rotation of more than the
established criteria regain full motion and have an excellent cosmetic
outcome. Fractures may require corrective osteotomy if they fail to
remodel after an adequate period of observation or if adequate motion
fails to return.214,329 Such corrective osteotomies have been done long after injury (up to 27 years) and additional motion has still been regained.329 There is a minor subset of malunions that
do not remodel, that have functional limits (especially when there is
limited supination deformity), and therefore, are candidates for
osteotomy.
 |
|
FIGURE 10-37 (continued) F. Axial alignment. G. Six-year follow-up radiographs with substantial remodeling of radius and ulna fractures.
|
 |
|
FIGURE 10-38 An 8-year-old male who underwent corrective osteotomy for forearm shaft malunion. A. Radiographs demonstrating significant angular malunion. B. Preoperative clinical appearance (dorsal view). (continues)
|
 |
|
FIGURE 10-38 (continued) C. Preoperative clinical appearance (volar view). D. Preoperative demonstration of full passive supination. E. Preoperative demonstration of marked limitation in passive pronation. F.
Early postoperative radiographs following corrective osteotomies (note intraosseous Kirschner wire tip from provisional fixation). G. Clinical appearance with extended elbows and forearm midposition. (continues) |
 |
|
FIGURE 10-38 (continued) H. Clinical appearance with extended elbows and pronated forearms. I. Clinical appearance with extended elbows and supinated forearms. J. Symmetrical pronation. K. Symmetrical supination. L. AP radiograph 18 months after osteotomies (plates and screws have been removed). (continues)
|
 |
|
FIGURE 10-38 (continued) M. Lateral radiograph at 18 month follow-up. N. AP radiograph uninjured left forearm. O. Lateral radiograph uninjured left forearm.
|
 |
|
FIGURE 10-39 A 16-year-old male who underwent corrective osteotomy for forearm shaft malunion. A. AP radiograph at time of presentation. B.
Lateral radiograph at time of presentation. Note rotational malunion of radius in addition to angular abnormalities of both bones. C. Clinical deformity (bump). D. Relatively symmetrical pronation noted preoperatively. (continues) |
 |
|
FIGURE 10-39 (continued) E. Dramatic lack of supination on the right noted preoperatively. F. One-year postoperative radiographs following osteotomies. Note improved rotational alignment of radius. G. Uninjured left forearm radiographs. (continues)
|
 |
|
FIGURE 10-39 (continued) H. Clinical appearance with extended elbows and forearm midposition. I. Clinical appearance with extended elbows and pronated forearms. J. Clinical appearance with extended elbows and supinated forearms. K. Symmetrical pronation. L. Symmetrical supination.
|
stated that normal healing of closed pediatric forearm shaft fractures
occurs at an average of 5.5 weeks (range 2 to 8 weeks). Delayed union
can be practically defined as a failure to demonstrate complete healing
(four cortices) on sequential radiographs by 12 weeks after injury,
which exceeds the upper limit of normal healing by about 1 month.
Nonunion can be defined as absence of complete bony union by 6 months
after injury, which exceeds the upper limit of normal healing by about
4 months.
In six large series of pediatric diaphyseal forearm fractures treated
by closed methods, a less than 0.5% rate (1/263) of delayed union and
no nonunions were reported.255,144,76,52,168,179
Delayed unions and nonunions are more common after open reduction and
internal fixation and open fractures. Particular concern has been
raised about the potential of antegrade ulnar nailing (olecranon
starting point) to distract the fracture site.234 Combined data from four series of plated pediatric forearm fractures indicated a 3% (3/89) nonunion rate26,227,333,358; 24% (21/89) of these were open fractures and at least one358 of the three nonunions occurred after a grade III open fracture.227,333
Large series of open pediatric forearm fractures (treated by a variety
of internal fixation methods) reported comparable numbers: 5% (8/173)
delayed union rate and 1% (2/173) nonunion rate.79,128,135 In a series of 30 nonunions in children, only 6 were in the forearm, and half of these were after open fractures.189
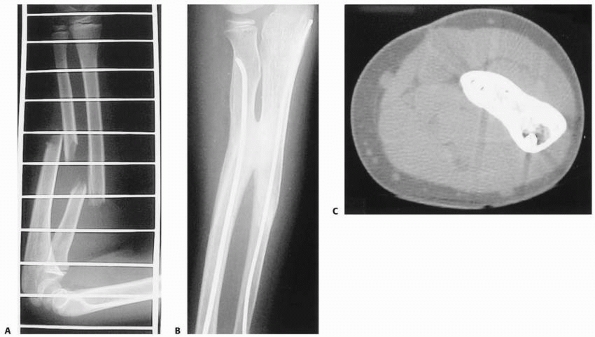 |
|
FIGURE 10-40 Radioulnar synostosis following closed injury. A. Injury radiographs. B. Plain radiographs showing synostosis. C. CT scan showing synostosis. (Courtesy of Alan Aner, MD.)
|
the possibility of unusual diagnoses such as neurofibromatosis must be
considered.69,71,155,202
After open injury or surgical intervention for other reasons, the
possibility of septic nonunion must be ruled out. In the absence of
such extraneous factors, nonunion of pediatric forearm fractures seems
to be related to surgical treatment.69,71,155,202,307 Weber and Cech349
divided nonunions into atrophic and hypertrophic types. Atrophic
nonunions probably are best treated with bone grafting and compression
plating. Compression plating or other stable internal fixation without
grafting usually is sufficient for hypertrophic nonunions.186
loss of forearm rotation. Most cross-unions that form after pediatric
forearm shaft fractures are type II lesions (diaphyseal crossunions),
as described by Vince and Miller (Fig. 10-40).338 Although some series of adult forearm fractures reported synostosis rates of 6% to 9%,22,316 posttraumatic radioulnar synostosis is a rare complication of pediatric forearm shaft fractures.338 In children, it usually is associated with high-energy injuries,338 radial neck fractures,274 and surgically treated forearm fractures.74,235 Some have suggested a familial predisposition to this complication.199 Postoperative synostosis after forearm fractures in children is almost exclusively associated with plate fixation.354,358
The risk of cross-union is increased when open reduction and internal
fixation of both-bone fractures are done through one incision.22,68
but the more common type is osseous. After a synostosis matures (6 to
12 months), it can be excised along with any soft tissue interposition.231,338 The results of synostosis resection may be better in adults than children,338 perhaps because
of the more biologically active periosteum in children.85,338
Interposition of inert material (such as Gore-tex [W. L. Gore &
Associates, Inc., Elkton, MD] or bone wax) has been used to decrease
the chances of recurrent synostosis.11,20,235,338
Nonsteroidal anti-inflammatory drugs and radiation treatment have been
reported after synostosis excision in adults, but their use in children
remains undefined. An alternative treatment is corrective osteotomy if
the patient is synostosed in a position of either extreme pronation or
supination. If the patient is stuck in a neutral position after
posttraumatic synostosis, surgical intervention is usually not
recommended.
shaft fractures and open fractures. Appropriately timed preoperative
antibiotic prophylaxis is believed to diminish the risk of infection.
Children with open forearm fractures are considered to be at high risk
for infection, and early (usually less than 24 hours)302 irrigation and débridement in the operating room is indicated.275
Whether in the backyard, the barnyard, the football field, or the hay
field, open forearm fractures that occur in organic settings are best
treated with early irrigation and débridement with inspection of the
intramedullary canal of both bone ends, where soil contamination tends
to occur during injury (see Fig. 10-30). Soil
contamination has been reported to lead to gas gangrene and subsequent
upper extremity amputation in children with grade I open forearm
fractures.96 Emergency room
irrigation and débridement is not recommended and is considered
inadequate with increased risk of serious infection.
fractures (25% open fractures), deep infection (osteomyelitis) occurred
in 5% (4/83).219,227,333,358
Such deep infections usually require extensive additional surgical
treatment to eradicate them. Combined data from 12 series of similar
pediatric forearm fractures (15% open fractures) treated with
intramedullary Kirschner wires, Steinmann pins, or Rush rods revealed a
deep infection rate of 0.46% (2/437)10,48,74,180,194,259,260,297,346,365
and a superficial infection rate of 2.5% (11/437). Six studies of ESIN
fixation reported a 0.2% (1/370) deep infection rate and a 3% (12/370)
superficial infection rate.48,131,184,201,269,337 Superficial infections may require oral antibiotics, pin removal, or both.
infection. Most (96%) open forearm fractures in children are Gustilo
and Anderson134 grade I or II.128,135,195
Two studies specifically investigated the relationship between the time
from injury until irrigation and débridement and the risk of later
infection. Luhmann et al.195
reported on 65 fractures (52 type I, 12 type II, 1 type III) that were
irrigated and débrided an average of 5.6 hours (range 1.5 to 24 hours)
after injury, and Greenbaum et al.128
reported 62 fractures (58 type I, 4 type II) that were irrigated and
débrided an average of 14.6 hours (range 1.7 to 37.8 hours) after
injury. No statistically significant association was found in either of
these studies; however, most (87%) of these fractures were grade I
injuries. Pooled data revealed an overall 1.2% rate (2/173) of deep
infection and a 0.6% rate (1/173) of superficial infection after
current open fracture treatment protocols.128,135,195
nerve exploration, decompression, and possible nerve repair should be
considered. If signs of progressive nerve recovery (e.g., advancing
Tinel sign, return of function) are not present by the end of the third
month after injury, further diagnostic work-up (electromyography with
nerve conduction studies) is indicated. Prolonged waiting can be
harmful to long term outcome.
concern. Operative treatment of pediatric forearm fractures by either
indirect reduction and internal fixation techniques or classic open
reduction and internal fixation techniques requires fracture
manipulation and soft tissue retraction, which have the potential to
worsen existing subclinical nerve injury or to create a new injury.
Such injuries are rare and may be underreported. Nerve injury after
pediatric forearm plate fixation has been alluded to but not discussed
extensively.180 Luhmann et al.194
reported an 8% (2/25) iatrogenic nerve injury rate after fixation with
intramedullary Kirschner wires or Rush rods: Both were ulnar nerve
injuries that resolved in 2 to 3 weeks. Cullen et al.74
reported one ulnar nerve injury that took 3 months to resolve in a
group of 20 patients treated with Kirschner wires or Rush rods.
damage during surgical forearm fracture treatment, especially the
superficial branch of the radial nerve.48,194,314
Pooled data from six series that included 370 ESIN procedures revealed
a 2% (7/370) rate of injury to the superficial branch of the radial
nerve.48,131,184,201,269,337
The branching pattern of this sensory nerve is complex, and efforts
must be taken to protect it during insertion of intramedullary nails
through distal radial entry points.1,16
Often, interposed tissue can be effectively removed during standard
fracture reduction, but the muscle may become an obstacle to successful
closed reduction. Much of the volar aspects of the shafts of the radius
and ulna are covered by the flexor pollicis longus and flexor digitorum
profundus, respectively. Many displaced forearm shaft fractures also
have apex volar angulation.230 As a result, portions of these muscles (or their tendons) are particularly prone to fracture site incarceration (Fig. 10-41).
The pronator quadratus also is vulnerable to fracture site entrapment
in the distal third of the radius and ulna, and it can block reduction
of distal-third forearm fractures.146
shaft fractures has been reported. Entrapment of the flexor digitorum
profundus typically causes an inability to fully extend the involved
finger (usually index, long, or ring fingers alone or in combination).139,295 Even if identified early, this complication rarely responds to occupational or physical
therapy. Surgical intervention is the preferred treatment and requires
only a small incision (usually over the ulna) through which the
adherent tissue is elevated with a blunt instrument from the bone at
the site of the fracture. Excellent restoration of finger motion can be
achieved, even when the release is done up to 2 years after the
fracture.266
 |
|
FIGURE 10-41 Muscle/tendon incarceration. A. Injury radiograph showing mild apex-volar fracture angulation. B. Flexor digitorum profundus entrapment in the ulnar fracture site required surgical extirpation.
|
Primary tendon disruption may be caused by direct trauma during either
nail insertion or extraction. Delayed tendon disruption may be caused
by slow erosion of the tendon as it glides past a sharp nail edge. The
possibility of this complication can be minimized by using surgical
incisions large enough to allow insertion of small blunt retractors to
protect adjacent tendons during nail insertion and extraction.
Avoidance of tendon erosion requires pin lengths that extend beyond the
tendon level into either the subcutaneous tissues74,297 or through the skin (external pins).259
Conceivably, the pins could be buried completely within the bone, but
this would require either accepting them as permanent implants
(something not commonly practiced at this time) or significantly
increasing the level of difficulty of nail removal. The extensor
pollicis longus is more at risk near Lister’s tubercle and may require
a late tendon reconstruction with extensor indicis proprius transfer.
reported no compartment syndromes in their series of 730 closed forearm
injuries. A single compartment syndrome that developed during cast
treatment of a 12-year-old female with a closed both-bone forearm
fracture was reported by Cullen et al.74 Because the diagnosis of compartment syndrome can be difficult in children,265 the index of suspicion must be high.
who is not reasonably comfortable 3 to 4 hours after adequate reduction
and immobilization of a forearm fracture.66 The risk of compartment syndrome is higher with open fractures135,363 and fractures that are difficult to reduce and require extended operative efforts.363 Yuan et al.363
voiced concern that the 10% (3/30) rate of compartment syndrome in
their patients with closed fractures might be due to multiple passes or
“misses” with intramedullary devices during efforts at indirect
reduction and internal fixation. Compartment syndrome was reported by
Haasbeek and Cole135 in 5 (11%) of
46 open forearm fractures in their series. The so-called floating elbow
injury has been associated with a rate of compartment syndrome as high
as 33%.363 Forearm compartment
syndrome is best treated with fasciotomy, releasing both the
superficial and deep volar compartments and the mobile wad. Both the
lacertus fibrosis and the carpal tunnel should be released as part of
the procedure.
sympathetic dystrophy are uncommon complications after pediatric
forearm shaft fractures.333 Paradoxically, relatively minor injuries seem to place patients at greatest risk.315,351
The most reliable sign in children is true allodynia: significant
reproducible pain with light touch on the skin. Swelling and other
vasomotor changes often are accompanying signs.187 The diagnosis in children is
made based almost exclusively on the history and physical examination, with little reliance on studies such as bone scans.315 These pain syndromes are best treated initially with physical therapy aimed at range of motion and desensitization.315,351 Failure to respond to physical therapy may warrant a referral to a qualified pediatric pain specialist.172,187
has increased dramatically in the United States: 33% higher for males
and 56% higher for females.175
Certain risk-taking behaviors demonstrated by children, as well as
increased use of motorized vehicles like all-terrain vehicles, may be
at least partly to blame.47,197 Increased general physical activity patterns and decreased calcium intake also have been suggested as explanations,175
but gaps persist in our epidemiologic understanding. Preventing these
injuries remains an admirable but elusive goal. Two main avenues of
research have been explored: optimizing safety during activities known
to be associated with forearm fractures, and investigating biologic
mechanisms related to fracture risk.
relative to forearm fractures. Children who avoid drinking milk have
been shown to have increased fracture risk,125 as well as those who prefer to drink fruit juice and soda.245 Several studies have shown an increased risk of fractures in females aged 3 to 15 years with low bone density.122,124
Diet, nutrition, and exercise are being explored as causative factors,
but the precise reason for the low bone density has not been confirmed.
Too little physical activity (as measured by television, computer, and
video viewing) has been associated with increased fracture risk,
presumably because of decreased bone mineral density.196
Caution also must be exercised when obtaining dual-energy x-ray
absorptiometry data in children, as up to 88% of scans may be
misinterpreted.110 Childhood obesity is a growing problem in our society.114,153
Increased body weight and decreased cross-sectional dimensions of the
forearm bones also have been found in females who fracture their
forearms.303 Other researchers have found an increased risk of forearm fracture in obese children.123,160
pediatric emergency department procedures. Several studies on chest
tubes, intravenous cannulation, lumbar puncture, and urethral
catheterization have shown increased parental satisfaction when parents
are allowed to stay for these procedures.21,137,250
Parental presence during induction of anesthesia also has been shown to
have favorable effects on children older than 4 years of age.164
To the best of our knowledge, there are no published studies on
parental presence during orthopaedic procedures performed in the
emergency department setting. There also are no parental presence
studies on any emergency department procedures performed on children
who are under sedation, when the child is probably not aware of the
parent’s presence.
invasiveness and parental presence have been borne out in the
literature. Four hundred parents from the Indiana area were surveyed,
and with increasing invasiveness, the parents’ desire to be present
decreased.38 A survey of academic
emergency medicine attendings, residents, and nurses from across the
country also showed that there is an inverse relationship between
increasing invasiveness and support for parental presence.23
Boudreaux et al. published their critical review of the parental
presence literature and concluded that “randomized controlled trials
are mixed regarding whether family presence actually helps the patient.”42
mentioned studies to pediatric orthopaedic settings should be done with
caution. We typically allow parents to be present for the induction of
sedation, and once the patient is sedated the parents are asked to wait
in a designated area. If parents are allowed to be present, we strongly
recommend a dedicated employee to attend to the parent or parents (a
“spotter”). Several parents (typically fathers) have fainted during
such orthopaedic procedures and injured themselves. Parents who stay
for a reduction also should be counseled that the patient may moan or
cry during reduction but will not remember it. Parents who are not
present during reduction should be asked to wait far enough away from
the procedure room so they cannot hear the child.
priceless teaching and constructive feedback afforded us by our senior
partner, Alvin H. Crawford, MD, FACS, as well as the skilled assistance
of Ms. Kelli Israel and Ms. Tiffany Whatley in the preparation of this
chapter.
RA, Brown RA, Botte MJ. The superficial branch of the radial nerve: an
anatomic study with surgical implications. J Hand Surg Am
1992;17:1037-1041.
RA, Ziets RJ, Lieber RL, et al. Anatomy of the radial nerve motor
branches in the forearm. J Hand Surg Am 1997;22:232-237.
S, Saridogan K, Moralar U, et al. Patterns of single segment nonphyseal
extremity fractures in children. Int Orthop 1999;23:345-347.
MM, Clarke HM, Zimmer P. Radiological signs of entrapment of the median
nerve in forearm shaft fractures. J Hand Surg Br 1994;19:713-719.
Academy of Pediatrics Committee on Drugs. Guidelines for monitoring and
management of pediatric patients during and after sedation for
diagnostic and therapeutic procedures. Pediatrics 1992;89:1110-1115.
Academy of Pediatrics Committee on Drugs. Guidelines for monitoring of
pediatric patients during and after sedation for diagnostic and
therapeutic procedures: addendum. Pediatrics 2002;110:836-838.
Y, Salai M, Chechik A, et al. Closing intramedullary nailing for the
treatment of diaphyseal forearm fractures in adolescence: a preliminary
report. J Pediatr Orthop 1985;5:143-146.
A, Singer M, Feldbrin Z, et al. Surgical treatment of posttraumatic
radioulnar synostosis in children. J Pediatr Orthop 2002;22:598-600.
Fracture and dislocation compendium: Orthopaedic Trauma Association
Committee for Coding and Classification. J Orthop Trauma 1996;10:1-153.
V, Gál P, Skotáková J, et al. Treatment of redislocated fragments of
long bones using plaster cast wedging. Rozhl Chir 2002;81:415-420.
G, Arand M, Mutschler W. Posttraumatic synostosis after forearm
fracture osteosynthesis. Arch Orthop Trauma Surg 1991;110:142-145.
AW, Sloan BK, Moore GP, et al. Should parents be present during
emergency department procedures on children and who should make the
decision? A survey of emergency physician and nurse attitudes. Acad
Emerg Med 2002;9:154-158.
M, Lamoureux J. Indications for immediate percutaneous intramedullary
nailing of complete diaphyseal forearm shaft fractures in children.
Acta Orthop Belg 1995;61(suppl I):169-172.
AR, Roberts JA. Treatment of unstable fractures of the forearm in
children: is plating of a single bone adequate? J Bone Joint Surg Br
2001;83:253-258.
A, Gupta SP, Sharma JC. Ipsilateral supracondylar fractures of the
humerus and forearm bone in children. Injury 1989;20:203-207.
RD, Salamon PB. Closed intramedullary rodding of pediatric adolescent
forearm fractures. Oper Tech Orthop 1993;3:128-133.
LC, Cooperman DR, Thompson GH, et al. Compartment syndrome in
ipsilateral humerus and forearm fractures in children. Clin Orthop
Relat Res 2000;376: 32-38.
ET, Moore GP, Brummett C, et al. Do parents want to be present during
invasive procedures performed on their children in the emergency
department? A survey of 400 parents. Ann Emerg Med 1999;34:70-74.
S. Roentgen recognition of acute plastic bowing of the forearm in
children. Am J Roentgenol Radium Ther Nucl Med 1975;125:524-530.
ED, Francis JL, Loyacano T. Family presence during invasive procedures
and resuscitations in the emergency department: a critical review and
suggestions for future research. Ann Emerg Med 2002;40:193-205.
BA, Overton B, Schraeder W, et al. Position of immobilization for
pediatric forearm fractures. J Pediatr Orthop 2002;22:185-187.
G, Hanson M, Cash R, et al. The innervation of the radial nerve at the
elbow and in the forearm. J Hand Surg Br 1998;23:167-169.
HD, Eyres RL, Cole WG. Randomized double-blind trial of low- and
moderatedose lidocaine regional anesthesia for forearm fractures in
childhood. J Pediatr Orthop 1996;16:660-663.
RL, Koepplinger ME, Mehlman CT, et al. All-terrain vehicle and bicycle
crashes in children: epidemiology and comparison of injury severity. J
Pediatr Surg 2002;37: 375-380.
PR, Achan P, Barry M. Diaphyseal forearm fractures in children treated
with intramedullary fixation: outcome of K-wires versus elastic stable
intramedullary nail. Injury 2003;34:278-282.
ML, Sponseller PD, Rossberg MI. Pediatric analgesia and sedation for
the management of orthopedic conditions. Am J Orthop 2000;29:665-672.
L, Muratli HH, Doğan O, et al. The results of intramedullary nailing in
children who developed redisplacement during cast treatment of
both-bone forearm fractures. Acta Orthop Traumatol Turc 2007;41:175-182.
C, Feugas C, Guillem P, et al. Innervation of the medial epicondylar
muscles: an anatomic study in 50 cases. Surg Radiol Anat
1999;21:165-168.
MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute
fractures of the diaphysis of the radius and ulna. J Bone Joint Surg Am
1989;71:159-169.
JC, Ng BK, Ying SY, et al. A 10-year study of the changes in the
pattern and treatment of 6,493 fractures. J Pediatr Orthop
1999;19:344-350.
DG, Hyndman JC, Leahey JL, et al. Short arm plaster cast for distal
pediatric forearm fractures. J Pediatr Orthop 1994;14:211-213.
KC, Spilson SV. The frequency and epidemiology of hand and forearm
fractures in the United States. J Hand Surg Am 2001;26:908-915.
JE, Omer GE Jr. Congenital proximal radioulnar synostosis: natural
history and functional assessment. J Bone Joint Surg Am 1985;76:539-545.
AH. Orthopedic injury in children. In: Callaham ML, ed. Current
Practice of Emergency Medicine. 2nd ed. Philadelphia: BC Decker,
1991:1232-1233.
AH. Orthopedics. In: Rudolph CD, Rudolph AM, Hostetter MK, et al., eds.
Rudolph’s Pediatrics. 21st ed. New York: McGraw Hill, 2002:2451.
AH, Cionni AS. Management of pediatric orthopedic injuries by the
emergency medicine specialist. In: Pediatric Critical Illness and
Injury: Assessment and Care. Rockville: Aspen System Publications,
1984:213-225.
C, Zaleske DJ, Ehrlich MG. Analyzing forearm fractures in children: the
more subtle signs of impending problems. Clin Orthop Relat Res
1984;188:40-53.
AH Jr. Surgical approaches. In: Canale ST, ed. Campbell’s Operative
Orthopaedics. 10th ed. St. Louis, CV Mosby, 2003:107-109.
MC, Roy DR, Giza E, et al. Complications of intramedullary fixation of
pediatric forearm fractures. J Pediatr Orthop 1998;18:14-21.
JS. A study of radioulnar movements following fractures of the forearm
in children. Clin Orthop Relat Res 1979;139:114-120.
JR, Frick SL, Skewes E, et al. Skin surface pressure beneath an
above-theknee cast: plaster casts compared with fiberglass casts. J
Bone Joint Surg Am 1997;79: 565-569.
AJ, Eyres RL, Cole WG. A comparison of prilocaine and lidocaine for
intravenous regional anaesthesia for forearm fracture reduction in
children. Paediatr Anaesth 2002;12:146-150.
Pablos J, Franzreb M, Barrios C. Longitudinal growth pattern of the
radius after forearm fractures conservatively treated in children. J
Pediatr Orthop 1994;14: 492-495.
LE, Li G, Zayontz SJ, et al. A minimally invasive method for the
determination of force in the interosseous ligament. Clin Biomech
2001;16:895-900.
PA, Lindsey RW, Ruwe PA. Refracture of bones of the forearm after the
removal of compression plates. J Bone Joint Surg Am 1988;70:1372-1376.
T, Botte MJ, Abrams RA. Anatomical considerations regarding the
posterior interosseous nerve during posterolateral approaches to the
proximal part of the radius. J Bone Joint Surg Am 2000;82:809-813.
T. Forearm. In: Cramer KE, Scherl SA, eds. Orthopaedic Surgery
Essentials. Philadelphia: Lippincott Williams & Wilkins,
2004:125-130.
TT, Strub WM, Foad SL, et al. Reduction versus remodeling in pediatric
distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop
B 2003;12:109-115.
JR, Botte MJ. Surgical Anatomy of the Hand & Upper Extremity.
Philadelphia: Lippincott Williams & Wilkins, 2003:34-40.
CE, Thalmann R, Macy JC. The effect of rotational malunion of the
radius and ulna on supination and pronation. J Bone Joint Surg Br
2002;84:1070-1074.
EM. Pronation injuries of the forearm with special reference to the
anterior Monteggia fracture. J Bone Joint Surg Br 1949;31:578-588.
JK, Buckley SL, Alexander AH, et al. Analgesia for the reduction of
fractures in children: a comparison of nitrous oxide with intramuscular
sedation. J Pediatr Orthop 1995;15:73-77.
NF, Dobranski A, Bisla RS. Gas gangrene complicating open forearm
fractures: report of five cases. J Bone Joint Surg Am 1977;59:135-138.
FF, Egenolf M, Carsten C, et al. Unstable diaphyseal fractures of both
bones of the forearm in children: plate versus intramedullary nailing.
Injury 2005;36: 1210-1216.
EA, Bartal E. Delayed union of the distal ulna in a child after
both-bone forearm fracture. J South Orthop Assoc 1998;7:113-116.
JM. Pediatric forearm fractures: decision making, surgical techniques,
and complications. Instr Course Lect 2002;51:355-360.
JM, Sarwark JF, Waters PM, et al. The surgical management of pediatric
fractures of the upper extremity. Instr Course Lect 2003;52:635-645.
V, Pontrandolfi A, Svoboda J. The Upper Paleolithic Triple Burial of
Dolní Vestonice: pathology and funerary behavior. Am J Phys Anthropol
2001;115:372-379.
JP, Alioto RJ, Marquardt JD. The efficacy and safety of the hematoma
block for fracture reduction in closed isolated fractures. Orthopedics
1997;20:423-426.
MT, Pfaeffle HJ, Stabile KJ, et al. Passive strain distribution in the
interosseous ligament of the forearm: implications for injury
reconstruction. J Hand Surg Am 2004; 29:293-298.
RI, Baron J. Overdiagnosis of osteoporosis in children due to
misinterpretation of dual-energy x-ray absorptiometry (DEXA). J Pediatr
2004;144:253-257.
BJ, Olson S. Combined entrapment of the median and anterior
interosseous nerves in a pediatric both-bone forearm fracture. J Orthop
Trauma 1990;4:197-199.
RD, Webb GR, Armstrong DG, et al. A comparison of short and long-arm
plaster casts for displaced distal-third pediatric forearm fractures: a
prospective randomized trial. Paper presented at: Annual Meeting of the
Pediatric Orthopaedic Society of North America; April 27-May 1, 2004;
St. Louis, MO.
RK, Wilson P, Mason Brown JJ, et al. Spontaneous correction of
deformity following fractures of the forearm in children. Br J Surg
1962;50:5-10.
NK, Ballal MS, Malek IA, et al. Use of elastic stable intramedullary
nailing for treating unstable forearm fractures in children. J Trauma
2008;65:109-115.
WB, Fernandez DL, Graca R. Anterior interosseous nerve palsy
complicating a forearm fracture in a child. J Hand Surg Am
1990;15:44-47.
F, Karlbauer AF, Gasperschitz F. Greenstick fracture of the forearm
with median nerve entrapment. J Emerg Med 1988;6:381-385.
GD, Meyer C, Koebke J, et al. Arterial supply of forearm bones and its
importance for the operative treatment of fractures. Surg Radiol Anat
1997;19:149-153.
SA, Elliot V, Matheny D, et al. Comparison of propofol/fentanyl versus
ketamine/midazolam for brief procedural sedation in a pediatric
emergency department. Pediatrics 2003;112:116-123.
MH, Lotfi P, Bendre A, et al. The ulnar nerve at the elbow and its
local branching: an anatomic study. J Hand Surg Br 2001;26:142-144.
A, Cannan R, Williams SM, et al. Bone mineral density in girls with
forearm fractures. J Bone Miner Res 1998;13:143-148.
A, Jones IE, Taylor RW, et al. Bone mineral density and body
composition in boys with distal forearm fractures: a dual-energy x-ray
absorptiometry study. J Pediatr 2001;139:509-515.
A, Jones IE, Taylor RW, et al. More broken bones: a 4-year double
cohort study of young girls with and without distal forearm fractures.
J Bone Miner Res 2000; 15:2011-2018.
A, Rockell JE, Black RE, et al. Children who avoid drinking cow’s milk
are at increased risk for prepubertal bone fractures. J Am Diet Assoc
2004;104:250-253.
AL, Roberts CA. Paleoepidemiology, healing, and possible treatment of
trauma in the medieval cemetery population of St. Helen-on-the-Walls,
York, England. Am J Phys Anthropol 1996;100:531-544.
PR, Sullivan JA. Nitrous oxide compared with intravenous regional
anesthesia in pediatric forearm fracture manipulation. J Pediatr Orthop
1996;16:187-191.
RM, Mehlman CT, Moon E, et al. Stiffness following displaced pediatric
both-bone forearm fractures: a meta-analysis. Paper presented at:
Annual Meeting of the Orthopaedic Trauma Association; October 5-7,
2006; Phoenix, AZ.
RP, Danielsson LG. Dorsally angulated solitary metaphyseal greenstick
fractures in the distal radius: results after immobilization in
pronated, neutral, and supinated position. J Pediatr Orthop
1990;10:90-92.
RB, Anderson JT. Prevention of infection in the treatment of 1025 open
fractures of long bones: retrospective and prospective analyses. J Bone
Joint Surg Am 1976;58: 453-458.
MP, Richter D, Muhr G, et al. Pediatric forearm fractures: diagnosis,
therapy, and possible complications. Unfallchirurg 1997;100:760-769.
Y, Amir J, Harel L, et al. Parental presence during lumbar puncture:
anxiety and attitude toward the procedure. Clin Pediatr (Phila)
1996;35:2-4.
P, Sharif I, Fogarty EE, et al. Management of the floating elbow injury
in children. Arch Orthop Trauma Surg 2000;120:205-208.
D, Aner A. Entrapment of the flexor digitorum profundus of the ring
finger at the site of an ulnar fracture: a case report. Ital J Orthop
Traumatol 1992;18:417-419.
WL, Shin AY, Klingelberger CE. Self-administered nitrous oxide and a
hematoma block for analgesia in the outpatient reduction of fractures
in children. J Bone Joint Surg Am 1995;77:335-339.
GM, Nowakowski R, Troshynski TJ, et al. Risk reduction in pediatric
procedural sedation by application of an American Academy of
Pediatrics/American Society of Anesthesiologists process model.
Pediatrics 2002;109:236-243.
H, Nilsson BE, Willner S. Correction with growth following diaphyseal
forearm fracture. Acta Orthop Scand 1976;47:299-303.
AM, Gellman H, Waters RL. The relationship of the interosseous membrane
to the axis of rotation of the forearm. Clin Orthop Relat Res
1994;298:272-276.
JR, Louis DS. Entrapment of pronator quadratus in pediatric distal
radius fractures: recognition and treatment. J Pediatr Orthop
1994;14:498-500.
RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the
interosseous membrane of the forearm: pathomechanics of proximal
migration of the radius. J Hand Surg Am 1989;14:256-261.
ES, Patwardhan AG, Meade KP, et al. Cross-sectional geometrical
properties and bone mineral content of the human radius and ulna. J
Biomech 1993;26:1307-1318.
K, Pun WK, Coleman S. Entrapment and transection of the median nerve
associated with greenstick fractures of the forearm: a case report and
review of the literature. J Trauma 1998;44:1101-1102.
TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely
overweight adolescents: concerns and recommendations. Pediatrics
2004;114:217-223.
FS, Crawford AH. Complications in neurofibromatosis. In: Epps CH, Bowen
JR, eds. Complications in Pediatric Orthopaedic Surgery. Philadelphia:
JB Lippincott, 1995:678-680.
CW, Carmichael KD, Morris RP, et al. Biomechanical study of flexible
intramedullary nails. J Pediatr Orthop 2009;29:44-48.
IE, Williams SM, Goulding A. Associations of birth weight and length,
childhood size, and smoking with bone fractures during growth: evidence
from a birth cohort study. Am J Epidemiol 2004;159:343-350.
A, Andermahr J, Isenberg J, et al. Outcomes and complications of
elastic stable intramedullary nailing of forearm fractures in children.
J Pediatr Orthop B 2005;14: 375-380.
PJ, Mazur JM, Cummings RJ, et al. Low-dose lidocaine intravenous
regional anesthesia for forearm fractures in children. J Pediatr Orthop
1992;12:633-635.
ZN, Mayes LC, Caramico LA, et al. Parental presence during induction of
anesthesia: a randomized controlled trial. Anesthesiology
1996;84:1060-1067.
P, Krefft M, Hesselbach J, et al. Computer simulation of forearm
rotation in angular deformities: a new therapeutic approach. Injury
2002;33:807-813.
P, Krefft M, Hesselbach J, et al. How does torsional deformity of the
radial shaft influence the rotation of the forearm? A biomechanical
study. J Orthop Trauma 2003; 17:57-60.
WNW, Clegg J. Intraoperative wedging of casts: correction of residual
angulation after manipulation. J Pediatr Orthop 1995;15:826-829.
AM, Powell CV, Williams A. Parent visual analogue scale ratings of
children’s pain do not reliably reflect pain reported by child. Pediatr
Emerg Care 2002;18:159-162.
JP, Zionts LE. Economic considerations in the treatment of distal
forearm fractures in children. Paper presented at: Annual Meeting of
the American Academy of Orthopaedic Surgeons; February 28-March 4,
2001; San Francisco, CA.
KJ, Sarah R, Silver-Highfield E, et al. On pins and needles? Pediatric
pain patients’ experience with acupuncture. Pediatrics 2000;105:941-947.
RM, Porter FL, Miller JP, et al. Comparison of fentanyl/midazolam with
ketamine/midazolam for pediatric orthopedic emergencies. Pediatrics
1998;102: 956-963.
J, Kröger H, Bowditch M, et al. Bone mineral density after removal of
rigid plates from forearm fractures: preliminary report. J Orthop Sci
2003;8:772-776.
S, Melton LJ III, Dekutoski MB, et al. Incidence of childhood distal
forearm fractures over 30 years: a population-based study. JAMA
2003;290:1479-1485.
WW, Sherman R, Succop P, et al. Fractures and rickets in very
low-birth-weight infants: conservative management and outcome. J
Pediatr Orthop 1989;9:326-330.
M, Solgaard S. Displaced diaphyseal forearm fractures in children:
classification and evaluation of the early radiographic prognosis. J
Pediatr Orthop 1989;9: 586-589.
M, Kabukcuoglu Y, Tezer M, et al. The application of open
intramedullary fixation in the treatment of pediatric radial and ulnar
shaft fractures. J Orthop Trauma 2002;16:340-344.
E, Vittas D, Torp-Pedersen S. Remodeling of angulated distal forearm
fractures in children. Clin Orthop Relat Res 1988;237:190-195.
P, Prevot J, Ligier JN, et al. Elastic stable intramedullary nailing in
forearm shaft fractures in children: 85 cases. J Pediatr Orthop
1990;10:167-171.
S, Bergerault F, Saidani N, et al. Roentgenographic measurement of
angle between shaft and distal epiphyseal growth plate of radius. J
Pediatr Orthop 2002;22: 751-753.
DG. Delayed union and nonunion of fractures. In: Canale ST, ed.
Campbell’s Operative Orthopaedics. 10th ed. St. Louis: Mosby,
2003:3125-3127.
BH, Scharff L, Sethna NF, et al. Physical therapy and
cognitive-behavioral treatment for complex regional pain syndromes. J
Pediatr 2002;141:135-140.
S, Nicol RO, Stott NS. Intramedullary fixation for pediatric unstable
forearm fractures. Clin Orthop Relat Res 2002;402:245-250.
ME. Impact of industrialization: comparative study of child health in
four sites from medieval and postmedieval England (A.D. 850-1859). Am J
Phys Anthropol 2002;119:211-223.
JN, Metaizeau JP, Prévot J, et al. Elastic stable intramedullary
pinning of long bone shaft fractures in children. Z Kinderchir
1985;40:209-212.
YJ, Lam KS, Lee EH. Open Gustilo 1 and 2 midshaft fractures of the
radius and ulna in children: is there a role for cast immobilization
after wound débridement? J Pediatr Orthop 2007;27:540-546.
SJ, Gordon JE, Schoenecker PL. Intramedullary fixation of unstable
both-bone forearm fractures in children. J Pediatr Orthop
1998;18:451-456.
SJ, Schootman M, Schoenecker PL, et al. Complications and outcomes of
open pediatric forearm fractures. J Pediatr Orthop 2004;24:1-6.
D, Jones G. Television, computer, and video viewing; physical activity;
and upper limb fracture risk in children: a population-based case
control study. J Bone Miner Res 2003;18:1970-1977.
D, Morley R, Jones G. Risk-taking coordination and upper limb fractures
in children: population-based case-control study. Osteoporos Int
2004;15:633-638.
DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in
2650 long-bone fractures in children aged 0 to 16 years. J Pediatr
Orthop 1990;10:713-716.
DC, Schnabel M, Baacke M, et al. Results of elastic stable
intramedullary nailing (ESIN) in forearm fractures in childhood.
Unfallchirurg 2003;106:102-109.
TT, Pfaeffle HJ, Herdon JH, et al. Forearm rotation alters interosseous
ligament strain distribution. J Hand Surg Am 2000;25:1058-1063.
KL, Lamey D, Yang S, et al. Radioulnar load-sharing in the forearm: a
study in cadavers. J Bone Joint Surg Am 1998;80:879-888.
J, Marsh JL, Nepola JV, et al. Radiographic fracture assessments: which
ones can we reliably make? J Orthop Trauma 2000;14:379-385.
LS, Kaufer H, Garver DF, et al. The effect on supination-pronation of
angular malalignment of fractures of both bones of the forearm: an
experimental study. J Bone Joint Surg Am 1982;64:14-17.
JC, Hopgood BC, Gaughan JP, et al. Forearm and elbow injury: the
influence of rotational position. J Bone Joint Surg Am
2003;85:2403-2409.
TP, Pierce WA, Lais RL, et al. Effect of displacement of ulna-shaft
fractures on forearm rotation: a cadaveric model. Am J Orthop
2002;31:420-424.
CT. Forearm, wrist, and hand trauma: pediatrics. In: JS Fischgrund, ed.
Orthopaedic Knowledge Update 9. Rosemont, IL: American Academy of
Orthopaedic Surgeons, 2008:669-680.
CT, Crawford AH, Roy DR, et al. Undisplaced fractures of the distal
radius and ulna in children: risk factors for displacement. Paper
presented at: Annual Meeting of the American Academy of Orthopaedic
Surgeons; February 13-17, 2001; Dallas, TX.
CT, O’Brien MS, Crawford AH, et al. Irreducible fractures of the distal
radius in children. Paper presented at: Annual Meeting of Pediatric
Orthopaedic Society of North America; May 1-5, 2001; Cancun, MX.
R, Prommersberger KJ, Lanz U. Surgical correction of malunited
fractures of the forearm in children. Z Orthop Ihre Grenzgeb
2003;141:328-335.
AO, Ebraheim NA, Jackson WT, et al. Vulnerability of the posterior
interosseous nerve during proximal radius exposures. Clin Orthop Relat
Res 1995;315: 199-208.
JP, Ligier JN. Surgical treatment of fractures of the long bones in
children: interference between osteosynthesis and the physiological
processes of consolidations: therapeutic indications. J Chir (Paris)
1984;121:527-537.
OJ, Regauer MP. Closed reduction of forearm refractures with flexible
intramedullary nails in situ. J Bone Joint Surg Am 2003;85:2152-2155.
ME, Allgöwer M, Schneider R, et al. Manual of Internal Fixation:
Techniques Recommended by the AO-ASIF Group. 3rd ed. Berlin:
Springer-Verlag, 1991:454-467.
GJC, Gibbons PJ, Glithero PR. Nancy nailing of diaphyseal forearm
fractures: single bone fixation for fractures of both bones. J Bone
Joint Surg Br 2004;86:581-584.
T, Yabe Y, Horiuchi Y. In vivo MR studies of dynamic changes in the
interosseous membrane of the forearm during rotation. J Hand Surg Br
1999;24:245-248.
BE, Obrant K. The range of motion following fracture of the shaft of
the forearm in children. Acta Orthop Scand 1977;48:600-602.
JA. Uniqueness of growing bones. In: Rockwood CA, Wilkins KE, King RE,
eds. Fractures in Children. Philadelphia: JB Lippincott, 1991:10-14.
JA, Beall JK, Conlogue GJ, et al. Radiology of postnatal skeletal
development, IV: distal radius and ulna. Skeletal Radiol 1981;6:255-266.
L, Wong-Chung J, Wray R, et al. Delayed union and nonunion of the ulna
following intramedullary nailing in children. J Pediatr Orthop B
2004;13:330-333.
TC, Sarlak A, Arazi M, et al. Posttraumatic distal radioulnar
synostosis and distal radial epiphyseal arrest. Ulus Travma Derg
2002;8:59-61.
DA, Oladiran IO, Adeniran A. Complications of fracture treatment by
traditional bonesetters in southwest Nigeria. Fam Pract 2001;18:635-637.
M, Bechtold JE, Merkow RL, et al. Rotational stability of diaphyseal
fractures of the radius and ulna fixed with Rush pins and/or fracture
bracing. Clin Orthop Relat Res 1989;240:236-243.
R, Loder RT, Louis DS. Open reduction and internal fixation of forearm
fractures in children. J Pediatr Orthop 1996;16:651-654.
PA, Richter D, Mecklenburg K, et al. Pediatric forearm fractures:
indications, technique, and limits of conservative management. J Orthop
Trauma 2000;14:73.
SN, Brody AS, Crawford AH. Use of a picture archiving and communication
system (PACS) and computed plain radiography in preoperative planning.
Am J Orthop 2004;33:62-64.
J. A study of supination and pronation with especial reference to the
treatment of forearm fractures. J Bone Joint Surg 1946;28:737-748.
AS, Kay PR, Haines JF. Distal ulnar growth plate arrest following a
diaphyseal fracture. J R Coll Surg Edinb 1992;37:347-348.
E, Karpathios T, Dessypris N, et al. The role of dairy products and
nonalcoholic beverages in bone fractures among schoolage children.
Scand J Soc Med 1997; 25:119-125.
HJ, Kischer KJ, Manson TT, et al. Role of the forearm interosseous
ligament: is it more than just longitudinal load transfer? J Hand Surg
Am 2000;25:680-688.
HJ, Tomaino MM, Grewal R, et al. Tensile properties of the interosseous
membrane of the human forearm. J Orthop Res 1996;14:842-845.
M, Jawish R. Stable flexible nailing of fractures of both bones of the
forearm in children [Article in French]. Chir Pediatr 1989;30:117-120.
KS, Rubenstein JS. Family presence during invasive procedures in the
pediatric intensive care unit: a prospective study. Arch Pediatr
Adolesc Med 1999;153:955-958.
J, Guichet JM. Elastic stable intramedullary nailing for forearm
fractures in children and adolescents. J Bone Joint Surg 1996;20:305.
J, Lascombes P, Guichet JM. Elastic stable intramedullary nailing for
forearm fractures in children and adolescents. Orthop Trans 1996;20:305.
CT, Mencio GA. Injuries to the shafts of the radius and ulna. In: Beaty
JH, Kasser JR, eds. Rockwood & Wilkins Fractures in Children. 5th
ed. Philadelphia: Lippincott Williams & Wilkins, 2001:452-460.
IR, De Sena L, Cáceres EP. Entrapment of the median nerve in a
greenstick forearm fracture: a case report and review of the
literature. Bull Hosp Jt Dis 1999;58: 220-223.
DM, Galpin RD, Carey TP. Intramedullary Steinmann pin fixation of
forearm fractures in children: long-term results. Clin Orthop Relat Res
2000;376:39-48.
P, Rettig O, Wolf S, et al. Range of motion of shoulder and elbow in
activities of daily life in 3D motion analysis. Z Orthop Unfall
2007;145:493-498.
M, Armstrong P, Crawford AH, et al. Symposium: management of fractures
in children and adolescents, parts I & II. Contemp Orthop
1991;23:517-548, 621-644.
GM, Hayes M. Entrapment of the flexor digitorum profundus in the ulna
with fracture of both bones of the forearm: report of a case. J Bone
Joint Surg Am 1986; 68:1102-1103.
KR, Feldman DS, Green DW, et al. Comparison of intramedullary nailing
to plating for both-bone forearm fractures in older children. J Pediatr
Orthop 2008; 28:403-409.
MP, Lantieri L, Loy S, et al. Vascular anatomy of the forearm muscles:
a study of 50 dissections. Plast Reconstr Surg 1991;88:1026-1033.
D, Ostermann PA, Ekkernkamp A, et al. Elastic intramedullary nailing: a
minimally invasive concept in the treatment of unstable forearm
fractures in children. J Pediatr Orthop 1998;18:457-461.
M, Bürger A, Günther CM, et al. Forearm rotation in healthy adults of
all ages and both sexes. J Shoulder Elbow Surg 2008;17:271-275.
A, Reis M, Molina M, et al. Supracondylar fractures of the humerus
associated with ipsilateral fractures in children: a report of
forty-seven cases. J Pediatr Orthop 2001;21:307-312.
DR, Crawford AH. Operative management of fractures of the shaft of the
radius and ulna. Orthop Clin North Am 1990;21:245-250.
FP. Medullary fixation of fractures of the forearm: a study of the
medullary canal of the radius and a report of 50 fractures of the
radius treated with a prebent triangular nail. J Bone Joint Surg Am
1959;41:1489-1516.
WE, Heckman JD. Traumatic plastic deformation of the radius and ulna: a
closed method of correction of deformity. Clin Orthop Relat Res
1984;188:58-67.
HD, Mommsen U, Bethke K, et al. Fractures of the proximal and middle
third of the lower arm in children. Z Kinderchir Grenzgeb
1980;29:357-363.
RA, Branche-Dorsey CM, Ryan GW, et al. Risk factors for injuries from
in-line skating and the effectiveness of safety gear. N Engl J Med
1996;335:1630-1635.
EH, Jones D, Henley MB, et al. A comparison of malreducation after
plate and intramedullary nail fixation of forearm fractures. J Orthop
Trauma 1995;9:8-16.
EH, Richards RR. The effect of malunion on functional outcome after
plate fixation of fractures of both bones of the forearm in adults. J
Bone Joint Surg Am 1992; 74:1068-1078.
W, Salm R. Indications for intramedullary stabilization of shaft
fractures in childhood: what is reliable and what is an assumption?
Kongressbd Dtsch Ges Chir Kongr 2001;118:431-434.
PP, Fitze G, Gödeke J, et al. Delayed healing of forearm shaft
fractures in children after intramedullary nailing. J Pediatr Orthop
2008;28:303-306.
PJ, Fagg PS. Undisplaced fractures of the distal third of the radius in
children: an innocent fracture? Injury 1992;23:165-167.
SD, Comstock CP, Mubarak SJ, et al. Intramedullary Kirschner wire
fixation of open or unstable forearm fractures in children. J Pediatr
Orthop 1999;19:329-337.
PT, Hanel DP. Traumatic plastic deformity of an adult forearm: case
report and literature review. J Orthop Trauma 1996;10:213-215.
AJ, Gulla J, Thode HC Jr. Parents and practitioners are poor judges of
young children’s pain severity. Acad Emerg Med 2002;9:609-612.
DL, Kautz SM, Kay RM, et al. Effect of delay of surgical treatment on
rate of infection in open fractures in children. J Pediatr Orthop
2000;20:19-22.
DL, Loro ML, Pitukcheewanont P, et al. Increased body weight and
decreased radial cross-sectional dimensions in girls with forearm
fractures. J Bone Miner Res 2001;16:1337-1342.
JR III, Palmer AK, Werner FW, et al. Reconstruction of the interosseous
membrane of the forearm in cadavers. J Hand Surg Am 1997;22:986-994.
GA. Injuries to children in the United States related to trampolines
1990-1995: a national epidemic. Pediatrics 1998;101:406-412.
KS, Kim HK. Nonunion as a complication of an open reduction of a distal
radial fracture in a healthy child: a case report. J Orthop Trauma
2003;17:231-233.
MP, Moore DC, Akelman E, et al. The effect of wrist guards on bone
strain in the distal forearm. Am J Sports Med 1999;27:500-506.
S, Rozen N, Michaelson M. Ulnar nerve injury following midshaft forearm
fractures in children. J Hand Surg Br 1997;22:788-789.
CL, Micheli LJ. Simultaneous ipsilateral fractures of the arm and
forearm in children. Clin Orthop Relat Res 1980;153:218-222.
EA. Treatment of midshaft fractures of the radius and ulna utilizing
percutaneous intramedullar pinning. Orthop Trans 1996;20:305.
RP, Malcolm JR, Wesdock KA, et al. Reflex sympathetic dystrophy in
children: an orthopaedic perspective. Orthopedics 1993;16:773-780.
RJ, Rosenwasser MP, Glazer PA. Surgical exposure of the dorsal proximal
third of the radius: how vulnerable is the posterior interosseous
nerve? J Shoulder Elbow Surg 1996;5:342-346.
AY, Celebi L, Murath HH, et al. Closed reduction and percutaneous
fixation of supracondylar fracture of the humerus and ipsilateral
fracture of the forearm in children. J Bone Joint Surg Br
2003;85:1169-1172.
S, Doherty S. The accuracy of length and angle measurement in
videoconferencing teleradiology. J Telemed Telecare 2002;8(Suppl
2):85-87.
RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational
deformities of both bones of the forearm: an in vitro study. J Bone
Joint Surg Am 1984;66:65-70.
PA, Graham HK. The “floating elbow” in children: simultaneous
supracondylar fractures of the humerus and of the forearm in the same
upper limb. J Bone Joint Surg Br 1995;77:791-796.
GH, Wilber JH, Marcus RE. Internal fixation of fractures in children
and adolescents: a comparative analysis. Clin Orthop Relat Res
1984;188:10-20.
H, Hüttl B, Knorr P, et al. Elastic stable intramedullary nailing
(ESIN) provides good long-term results in pediatric long-bone
fractures. Eur J Pediatr Surg 2000;10: 319-322.
D, Vanderlinden C, Bremen J. Stable elastic nailing applied to
diaphyseal fractures of the forearm in children. Acta Orthop Belg
1991;57:147-153.
MC, Fornalski S, McMahon PJ, et al. The effects of ulnar axial
malalignment on supination and pronation. J Bone Joint Surg Am
2000;82:1726-1731.
S, Bostman O, Pätiälä H, et al. Internal fixation of forearm fractures
in children. Acta Orthop Scand 1987;58:121-123.
der Reis WL, Otsuka NY, Moroz P, et al. Intramedullary nailing versus
plate fixation for unstable forearm fractures in children. J Pediatr
Orthop 1998;18:9-13.
BL, Mehlman CT, Foad SL, et al. The use of conscious sedation for
forearm fracture reduction in children: does race matter? Paper
presented at: Annual Meeting of the American Academy of Pediatrics;
October 31-November 5, 2003; New Orleans, LA.
J. Clinical survey of 163 cases of internal fixation with metal in
fractures in children. J Bone Joint Surg Am 1956;38:1384-1385.
L, DeIronge G, Lamoureux J. Shaft forearm fractures in children:
intramedullary nailing with immediate motion: a preliminary report. J
Pediatr Orthop 1988;8: 450-453.
D, Larsen E, Torp-Pedersen S. Angular remodeling of midshaft forearm
fractures in children. Clin Orthop Relat Res 1991;265:261-264.
P, De Boeck H. Bowing fractures of the forearm in children: a long-term
follow-up. Clin Orthop Relat Res 2003;413:233-237.
SJ, Weiner DS, Leighley B. Redisplacement after closed reduction of
forearm fractures in children. J Pediatr Orthop 1990;10:79-84.
SJ, Weiner DS, Leighley B. Use of pins and plaster in the treatment of
unstable pediatric forearm fractures. J Pediatr Orthop 1990;10:85-89.
L, Mehlman CT. Tarsal coalition. eMedicine Orthopaedics. Available at:
http://www.emedicine.com/orthoped/topic326.htm. Accessed September 1,
2005.
M, Paton RW. Percutaneous intramedullary elastic wiring of displaced
diaphyseal forearm fractures in children. A modified technique. Injury
1999;30:21-24.
PA, Blair W. Entrapment of the index flexor digitorum profundus tendon
after fracture of both forearm bones in a child. Iowa Orthop J
1999;19:127-128.
KE. Operative management of children’s fractures: is it a sign of
impetuousness or do the children really benefit? J Pediatr Orthop
1998;18:1-3.
JC Jr, Krueger JC. Fractures of the proximal and middle thirds of the
radius and ulna in children: study of the end results with analysis of
treatment and complications. Am J Surg 1966;112:326-332.
AM, Voigt A, Linke F, et al. New aspects in the treatment of complete
and isolated diaphyseal fractures of the forearm in children.
Unfallchirurgie 1995;21: 70-76.
B, Mencio GA, Green NE. Open reduction and internal fixation of
pediatric forearm fractures. J Pediatr Orthop 1996;16:644-650.
MN, Talwalkar SC, Henderson JJ, et al. Segmental radius and ulna
fractures with scaphocapitate fractures and bilateral multiple
epiphyseal fractures. Am J Orthop 2008; 37:214-217.
T, Nakatsuchi Y, Koike H, et al. Mechanism of limitation of
pronation/supination of the forearm in geometric models of deformities
of the forearm bones. Clin Biomech (Bristol, Avon) 2002;17:456-463.
AS, Tredwell SJ, Mackenzie WG, et al. Accurate prediction of outcome
after pediatric forearm fracture. J Pediatr Orthop 1994;14:200-206.
AS, Tredwell SJ, Mackenzie WG. Factors affecting fracture position at
cast removal after pediatric forearm fracture. J Pediatr Orthop
1997;17:332-336.
PS, Pring ME, Gaynor TP, et al. Compartment syndrome following
intramedullary fixation of pediatric forearm fractures. J Pediatr
Orthop 2004;24:370-375.
SH, Lam CY, Choi KY, et al. Percutaneous intramedullary Kirschner
wiring for displaced diaphyseal forearm fractures in children. J Bone
Joint Surg Br 1998;80:91-94.
PS, Lam CY, Ng BK, et al. Percutaneous transphyseal intramedullary
Kirschner wire pinning: a safe and effective procedure for treatment of
displaced forearm fracture in children. J Pediatr Orthop 2004;24:7-12.
LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced both-bone
forearm fractures in older children and adolescents. J Pediatr Orthop
2005;25:507-512.
