Treatment of Acute Elbow Dislocations
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 51 – Treatment of Acute Elbow Dislocations
is now better understood. Traditional teaching stated that the
mechanism of injury was hyperextension. A fall on the outstretched hand
is the most common cause. The elbow experiences an axial compressive
force during flexion as the body approaches the ground. The body
rotates internally, with the forearm rotating externally to the trunk.
This results in a supination moment at the elbow. At that point, the
mechanical axis of the extremity is medial to the elbow, resulting in a
valgus moment. O’Driscoll and Morrey suggest that an extension varus
stress disrupts the lateral ligament complex first. If this dissipates
the force, then a perched dislocation is the result. Continued force
causes forearm rotation tearing the capsule, resulting in a complete
dislocation. This has been described as the “ring of instability”
progressing from disruption of the lateral ulnar collateral ligament
(LUCL) to the capsule, and finally injury to the medial ulnar
collateral ligament (MUCL). With a slightly flexed elbow, a tear in the
medial collateral ligament complex occurs and the elbow dislocates.
ligamentous disruption, substantial compressive and shear forces occur
on the articular surface. This can cause fractures of the proximal
radius. Dislocations treated by open procedures have documented
chondral injuries to the capitellum and trochlear surfaces at higher
rates than previously believed. Understanding the mechanism of injury
is important for appreciating classification, interpreting radiographs,
formulating a treatment plan, anticipating complications, and guiding
follow-up care.
the pediatric age group and the second most common in the adult
population. It is estimated that 6 of every 100,000 individuals will
sustain an elbow dislocation during their lifetime. Elbow dislocations
constitute 10% to 25% of all injuries to the elbow. More than one half
of dislocations involve the nondominant extremity. It has been
suggested that there is a protective instinct using the dominant side
to protect from a fall. The mean age of an individual sustaining this
injury is 30 years. There is a male predominance with 2 to 2.5 that of
females with similar ratios in children.
sports. Gymnastics, wrestling, basketball, and football are commonly
involved. Approximately 40% of dislocations have a poorly defined
causes.
from lateral to medial and can be broken into three stages. Stage 1
involves disruption of the ulnar component of the lateral collateral
ligament. This results in posterolateral rotatory subluxation of the
elbow, which reduces spontaneously. With continued force, disruption
occurs anteriorly and posteriorly allowing for an incomplete
posterolateral dislocation. This is a perched dislocation. Stage 3 has
two parts. In stage 3A, all soft tissues are disrupted including the
posterior part of the medial collateral ligament. The anterior band of
the medial collateral ligament remains intact. This allows for
posterior dislocation by the previously described posterolateral
rotatory mechanism. In stage 3B, the entire medial collateral complex
is disrupted. Varus, valgus, and rotatory instability are present.
Surgical experience suggests that the medial collateral complex is
disrupted in nearly 100% of elbow dislocations. Violation of the
anterior bundle of the medial collateral ligament is considered the
essential lesion. Disruption proximally from the humerus is most
common. Dislocation is the final of three sequential stages of elbow
instability, resulting from posterolateral ulnohumeral
rotatory subluxation, with soft tissue disruption occurring from lateral to medial.
into posterior, anterior, and divergent. Anterior dislocations are
uncommon, occurring in only 1% to 2% of incidents. Anterior
dislocations are usually seen in younger individuals. Posterior
dislocations are divided based on the final relationship between the
humerus and olecranon into posterior, posterolateral, posteromedial,
and pure lateral dislocations. Posterolateral is most common, followed
by lateral, and least commonly, posteromedial. A divergent dislocation
is a rare injury associated with high-energy trauma. Displacement of
the radius from the ulna occurs, resulting in disruption of the
interosseous membrane, annular ligament, and distal radioulnar joint
capsule.
between a perched and complete dislocation. A medial or lateral resting
position of the complete dislocation makes little difference with
regard to treatment or prognosis. A perched dislocation is one in which
the elbow is actually subluxated but the coronoid appears to impinge on
the trochlea. In this type, the ligaments are less severely injured,
and rehabilitation can be more rapid and recovery more complete.
status is mandatory. Anteroposterior and lateral radiographs should be
obtained if possible. Evaluation of associated injuries should be
reserved until reduction has been obtained. Computerized tomography and
magnetic resonance imaging are often of limited value. These are
reserved if adequate radiographs cannot be obtained, and can be used
for later reconstructive planning.
Radial head and neck fractures occur in 5% to 10% of elbow
dislocations. Avulsion fractures of the medial or the lateral
epicondyles occur in approximately 12% of the cases, and coronoid
fractures occur in 10% of dislocations. The incidence of associated
fractures in children is high, approaching 50%. With open physes, a
medial epicondyle avulsion is the most common associated injury.
Incarceration of the fragment can occur. Although prereduction and
postreduction radiographs reveal periarticular fractures in 12% to 60%
of dislocations, operative findings have revealed unrecognized
osteochondral injuries in nearly 100% of acute elbow dislocations. The
vast majority of these injuries are small fractures not requiring
operative intervention.
devastating. There are multiple case reports of brachial artery
injuries with posterior dislocation. Although it may not be necessary
to explore the brachial artery routinely if a radial pulse is present,
it is accepted that disruption of the brachial artery should be treated
with ligation and vein grafting. Median nerve entrapment has been
reported with relocation of a dislocated elbow. The median nerve may be
displaced posteriorly through a space created by avulsion of the medial
epicondyle or the common flexor origin. This can result in a tension of
the median nerve across the margin of the epicondylar flare and may
“notch” the bone, producing a late radiographic sign known as the Matev
sign.
commonly occurs. Intact structures including the forearm fascia, the
biceps tendon, and the lacertus fibrosis may exert a constricting
effect resulting in increased compartment pressures. Compartment
syndrome is possible and should be considered. Careful observation is
required, and differentiation from neurologic stretch injuries is
necessary.
often best accomplished with conscious sedation or general anesthesia
with adequate muscle relaxation. Muscle relaxation is the key to joint
reduction. Care is taken to avoid multiple reduction attempts. A prone
traction and countertraction maneuver is often successful (Fig. 51-1).
Reduction is usually achieved by extending the elbow with
countertraction on the arm and a thumb used to manipulate the coronoid
clearing the trochlea. Perched dislocation can be treated with
intra-articular analgesia and sedation whereas
a
complete dislocation may require general anesthesia and a muscle
relaxant. Uncommonly, a dislocation occurs that is irreducible by
closed reduction. This is most frequently associated with fractures.
When a dislocation is irreducible, the radial head has been shown to be
trapped in the soft tissues of the forearm or can buttonhole through
the forearm fascia. These require surgical intervention. Surgical
repair of ligaments without associated fractures in the acute
dislocation has not been shown to improve return to activity or
function.
 |
|
Figure 51-1 Prone position for traction/countertraction elbow relocation.
|
the patient under anesthesia or an anesthetized elbow. The quality of
joint reduction provides a clue to postreduction stability. Palpating a
reduction “clunk” is a favorable sign of joint stability. The elbow is
examined for valgus, varus, and posterolateral rotatory instability.
Both varus and valgus instability are performed with the elbow in full
extension and flexion up to 30 degrees. Most dislocated elbows are
unstable to a valgus stress. This is best tested with the forearm in
pronation to lock the lateral side. It is important to evaluate the
tendency for redislocation occurring in extension, which can signify a
potentially unstable joint. Posterolateral rotatory instability is
diagnosed by the lateral pivot shift test. A positive test is
manifested by a clunk that is heard and felt when the ulna and radius
reduce on the humerus.
a concentric reduction. Anteroposterior and lateral views should be
obtained. Widening of the joint space may indicate entrapped
osteochondral fragments, which must be removed surgically.
Posterolateral rotatory instability may also present as a nonconcentric
reduction.
concomitant injuries, which occur in 10% to 15% of cases. The distal
radioulnar joint and interosseous membrane should be evaluated for
tenderness and instability to rule out injury.
periarticular fractures result in medial and lateral ligament ruptures.
Rarely is surgical treatment necessary in the acute setting. Josefsson
et al. evaluated 31 acute elbow dislocations without concomitant
fractures. Under anesthesia nine were unstable with full extension.
They surgically explored all 31 elbows, finding ruptures of the medial
and lateral ligaments. The tendency of elbows to dislocate correlated
with the degree of muscular injury to the flexor-pronator and extensor
origins on the humerus. They concluded that muscular flexor and
extensor origins represent secondary stabilizers of the elbow. If they
are intact, they provide adequate stability to allow ligamentous
healing after elbow dislocation. Prospective studies have failed to
show improvement of early collateral ligament repair over early motion
after a simple elbow dislocation.
incidents. An open elbow dislocation and acute compartment syndrome
require urgent intervention. Postreduction instability requiring 50 to
60 degrees of flexion to remain stable may require intervention. Elbow
dislocations with unstable fractures require surgical stabilization.
The unstable elbow will redislocate even with a well-fitting cast or
splint (Fig. 51-2). If this occurs, rigid
external fixation with pins in the humerus and ulna are required to
maintain a stable concentric reduction. Dynamic external fixation may
be used allowing motion in the stable range of motion.
dislocation are not universally successful. Most authors recommend a
period of immobilization lasting from 3 to 10 days. Restoration of full
range of motion, especially extension, is not reliably achieved.
Nonimmobilization and early rapid motion under supervision has been
shown to achieve range of motion within 5 degrees of extension of the
contralateral elbow with an excellent functional outcome.
postinjury require additional intervention. If by 6 to 8 weeks full
motion has not been obtained, patient-adjusted static flexion and
extension splints are used to facilitate regaining motion.
Rehabilitation should be closely supervised.
dislocations. Sixty-five percent reported loss of motion especially in
extension. They found a direct correlation with the period of
immobilization. Immobilization >3 weeks resulted in a high incidence
of contractures. Uncomplicated dislocations generally have very
satisfactory results. Excellent results with full range of motion,
normal strength, absent pain, and good stability may be expected in 50%
of patients. Good results, defined as <15 degrees of motion loss,
minimal discomfort, and normal stability, may be expected in one third
of patients. Fair or poor results are generally associated with
complications and severe injuries and occur in 15% of cases.
and rarely up to 18 months. Limitations in extension are the most
common problem. Recurrent instability has not been commonly reported,
but symptoms have been noted in ≤35 percent of cases. Even long after
healing, approximately 50% of patients followed up long term complain
of discomfort or residual symptoms attributed to their elbow after a
dislocation. This is predominately reported during heavy loading of the
affected extremity. Approximately 60% of patients reported that their
elbow did not feel as “good” as the contralateral elbow. Mechanical
testing reveals a 15% average loss of elbow strength.
Symptoms range from transient paresthesia to a rare permanent ulnar
palsy. Median nerve involvement is less common. Stretching and
distortion of the anterior structures may result in spasm, intimal
damage, thrombosis, or rupture of the brachial artery. Because
dislocation involves disruption of collateral circulation, the forearm
can be placed at risk.
Ischemic myositis, myonecrosis, impaired vascularity, or claudication may result.
 |
|
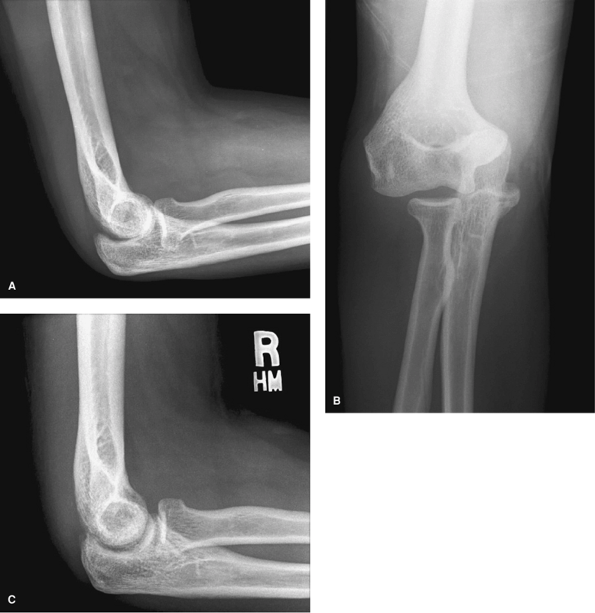
Figure 51-2 Patient with recurrent instability and dislocated 2 weeks after closed reduction. A: The redislocation was not initially recognized with only a lateral radiograph. The joint is not congruent. B: Orthogonal anteroposterior (AP) view shows the clear dislocation. C: Lateral radiograph obtained after open repair of medial and lateral ligaments with a congruent, stable joint.
|
bleeding and edema formation within the flexor compartment of the
forearm. Pain with passive finger and wrist extension out of proportion
to the injury raises clinical suspicion. Compartment pressures are
obtained when the diagnosis is in doubt, and arteriography is obtained
if arterial injury is suspected.
instability after elbow dislocation. Limitation of extension is common
with frequent loss of 10 to 15 degrees of terminal extension. Bracing
and therapy are not generally useful after 1 year. If there is
sufficient limitation of 30 degrees or more, capsulolysis may be
considered. The anterior capsule can be released via an open or
arthroscopic approach.
locations following dislocations. Ossification in the lateral and
medial collateral ligaments occurs most frequently (reported in
approximately 75% of cases) but seldom causes impairment. Ossification
occurs in the anterior capsule above the coronoid process. True ectopic
ossification that limits motion is rare, occurring in <5% of cases.
Motion-limiting ossification excision is delayed until reactive bone
has matured, generally at 1 year.
associated with distal radioulnar instability. This is a variant of the
Essex-Lopresti injury. The combined injury makes radial head
reconstruction important for both elbow stability and axial stability
of the forearm. If the radial head is not reconstructible, a metal
prosthesis or allograft radial head will provide axial support to the
radius and improve valgus stability of the elbow. Temporary pin
fixation of the distal radioulnar joint in a neutral position may be
added to resist the tendency of proximal radial migration.
|
TABLE 51-1 Elbow Dislocation Protocol
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
straightforward, and careful evaluation of radiographs should allow
classification of a complex or simple dislocation. Most injuries will
be simple, without significant associated fracture. A rapid but
complete neurovascular assessment is documented.
reduction may be performed under select conditions if indicated. This
will involve an obvious dislocation and an experienced provider at the
injury site. Most patients will require transportation to an acute care
facility for radiographic evaluation.
the degree of muscle spasm present. Analgesia may be provided with
conscious monitored sedation, or regional or general anesthesia. The
prone position with an assistant controlling the proximal humerus for
traction/countertraction has been helpful. The forearm is supinated,
and with pressure on the proximal olecranon, a successful reduction can
usually be achieved. The stability of the reduction is assessed with
range of motion, and the patient is temporarily placed in a sling for
postreduction x-ray films.
Rarely, an elbow dislocation without fracture will be grossly unstable
following reduction. In this circumstance, an early MRI, followed by
exploration and repair of the medial collateral ligament,
flexor-pronator tendon, and lateral ulnar collateral ligament can
restore stability. Our experience has been that early range of motion
is critical to ensuring a successful outcome.
PO, Gentz CF, Johnell O, et al. Surgical versus non-surgical treatment
of ligamentous injuries following dislocation of the elbow joint. J Bone Joint Surg Am. 1987;69:605–608.
I. A radiological sign of entrapment of the median nerve in the elbow
joint after posterior dislocation: a report of two cases. J Bone Joint Surg. 1976;58B:353.
