Discoid Meniscus
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Discoid Meniscus
Discoid Meniscus
Jason W. Hammond MD
Description
-
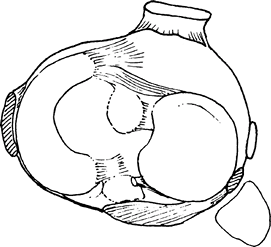
Discoid meniscus is a thickened, pancake-shaped lateral meniscus of developmental origin (Fig. 1).
-
It often causes clicking or locking of the knee in childhood or early adulthood.
-
It may be unilateral or bilateral.
-
Classification:
-
General (1):
-
Complete: Meniscus covers entire lateral tibial plateau
-
Incomplete: Meniscus larger than normal but does not cover the entire lateral plateau
-
-
Wrisberg (1):
-
Ligament type
-
Unstable
-
Lacks posterior attachment of meniscus to tibia
-
-
-
Synonym: Wrisberg meniscus
Epidemiology
Incidence
-
The approximate incidence is <1% in the United States and up to 26% in Japan (2).
-
Most cases present in late childhood or early adolescence.
Prevalence
The United States prevalence is ~4–5% (1).
Etiology
This condition is an anatomic or developmental abnormality.
 |
|
Fig. 1. A diseased lateral meniscus lacks the normal semilunar shape and covers the entire lateral side of the tibia.
|
Signs and Symptoms
-
Many patients are asymptomatic.
-
Presentation is highly variable, depending on the type of meniscus and the presence or absence of a tear.
-
The classic snapping-knee syndrome is characterized by a “clunk” at the terminal limits of flexion and extension.
-
May be associated with pain, clicking, swelling, locking, popping, and blocks to motion
-
The onset often is insidious, without a history of trauma.
-
If symptoms are acute or associated with trauma, an acute tear may be the cause.
Physical Exam
-
Usually, little to no effusion is present in the knee.
-
Mild tenderness may be present at the lateral joint line, but not as severe as that with an acute meniscus tear.
-
Often, a pop or click is noted with the McMurray test (rotating the knee while it is in a fully flexed position).
-
The examiner may note a block to full extension or the patient’s apprehension when the knee is straightened.
Tests
-
The McMurray test: Extension and rotation of a maximally flexed knee:
-
A positive test is pain or popping at the lateral joint line.
-
Imaging
-
Plain radiography:
-
Wide lateral joint space (3)
-
Lateral joint lipping
-
Cupping of the lateral tibial plateau
-
Flattening of the lateral femoral condyle
-
-
MRI:
-
3 or more contiguous 5-mm sagittal sections showing continuity between the anterior and posterior horns
-
Block “bow tie” appearance on the coronal view with increased width of the mid-AP diameter
-
Pathological Findings
-
Disc-shaped meniscus
-
Stable variant: Normal tibial ligaments
-
Unstable variant: Absence of the posterolateral tibial attachments
Differential Diagnosis
-
Acute meniscus tear
-
OATS or osteochondral fracture
-
Physeal fracture
-
Fracture of the tibial eminence
-
ACL tear
P.103
General Measures
-
Asymptomatic patients should be observed.
-
Symptomatic patients often require
surgical treatment, which varies depending on whether a tear is present
and whether the meniscus is stable or unstable. -
Nonoperative methods are rarely helpful
in the patient with symptomatic discoid meniscus, although a trial of
immobilization may be attempted in patients with acute-onset cases. -
Patients may resume normal activity when symptoms resolve.
Surgery
-
Stable meniscus: Partial meniscectomy or saucerization (trimming) to form a more normal-appearing meniscus (4)
-
Unstable meniscus:
-
Saucerization and reattachment to the posterolateral capsule in an attempt to preserve the meniscus
-
Complete meniscectomy is indicated if the patient has degenerative changes or a large meniscal tear.
-
Prognosis
Patients with a stable discoid meniscus have good results with saucerization.
Complications
-
Degenerative joint disease is possible with complete meniscectomy.
-
Recurrent meniscal tears
Patient Monitoring
Patients should be followed until symptoms resolve.
References
1. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg 1996;4:191–200.
2. Miller RH, III. Knee injuries. In: Canale ST, ed. Campbell’s Operative Orthopaedics, 9th ed. St. Louis: Mosby-Year Book Inc., 1998:1113–1299.
3. Asik M, Sen C, Taser OF, et al. Discoid lateral meniscus: diagnosis and results of arthroscopic treatment. Knee Surg Sports Traumatol Arthrosc 2003;11:99–104.
4. Youm T, Chen AL. Discoid lateral meniscus: evaluation and treatment. Am J Orthop 2004;33:234–238.
Codes
ICD9-CM
717.5 Discoid meniscus
Patient Teaching
-
Observation, if the discoid meniscus is asymptomatic
-
Increased risk of degenerative changes after total meniscectomy
FAQ
Q: Do patients with discoid lateral meniscus require surgery?
A:
If the discoid lateral meniscus is truly asymptomatic or is noted
incidentally on MRI or at the time of arthroscopy, surgical repair is
not necessary. If the discoid meniscus is symptomatic (lateral knee
pain, locking, swelling), it should be saucerized to resemble a normal
lateral meniscus. Degenerative tears should be débrided, but unstable
peripheral tears should be repaired after saucerization.
If the discoid lateral meniscus is truly asymptomatic or is noted
incidentally on MRI or at the time of arthroscopy, surgical repair is
not necessary. If the discoid meniscus is symptomatic (lateral knee
pain, locking, swelling), it should be saucerized to resemble a normal
lateral meniscus. Degenerative tears should be débrided, but unstable
peripheral tears should be repaired after saucerization.
