Slipped Capital Femoral Epiphysis
disorder in adolescents. It is characterized by the anterior and
superior migration of the femoral neck. Although this shift in location
gives the femoral head the appearance of lying posteriorly and
inferiorly, it actually remains stable in the acetabulum. The average
age at presentation is 12 years for girls and 14 years for boys. The
slip occurs during the preadolescent hormonal changes of puberty.
Children with a vertical capital physis are more prone to developing a
slip. There is also an association with obesity. Most of the patients
are in the 99th percentile for weight. Patients may present with pain
for several days or many weeks, but pain is not necessarily an
indication of slip severity. The current classification used is based
on the stability of the physis. Children who have an effusion and are
unable to bear weight have an unstable slip. The children who are
bearing weight at the time of presentation have a stable slip.
occur only in skeletally immature patients. The timing of the slip
generally coincides with the beginning of puberty. The theory is that
the physis is weaker at that physiologic point, because the columnar
architecture becomes disorganized when the physis begins to fuse. The
histology of the capital physis in patients with slipped capital
femoral epiphysis shows almost total loss of the columns and is similar
to the histology of the proximal tibial physis in patients with Blount
disease. Because both types of histology have a high association with
obesity, the obesity is thought to play a role in the weakening of the
physis. In patients with known collagen problems, such as those with
Down syndrome, the fibrous septa between the columns is unable to
support the architecture.
often more vertical than normally observed. Calculating the stresses
across the physis in obese patients reveals a considerable increase in
the forces, and it is therefore not a surprise that these patients are
more susceptible to slips. There has also been reported in the
literature an association between the occurrence of slips and increased
retroversion of the femoral head. However, these studies are often
performed after the slip, and it is not clear whether the retroversion
is cause or effect.
femoral head, as the name of the disorder implies. The femoral neck
drifts anteriorly and superiorly. On radiographs, the femoral head is
located inferiorly and posteriorly. There is a rare variation known as
the valgus slip, in which the migration of the femoral neck is in the
opposite direction so that the femoral head rests more anteriorly and
superiorly. The reason for the difference in position is not known.
classified as acute, subacute, or chronic. The classification was based
solely on the amount of time symptoms were present at the time of the
initial evaluation. The timing was determined by patient history. This
classification proved not to be useful in determining outcome. Slipped
capital femoral epiphyses are now classified by the amount or degree of
the slip. This classification is beneficial in a prognostic manner. It
does not affect the decision to operate or the technique.
which the patients are unable to bear weight. Patients who walk into
the doctor’s office complaining of thigh or hip pain have a stable
slip. Stable hips have virtually no risk of avascular necrosis.
Unstable hips have a high incidence of avascular necrosis. Fortunately,
there are far more stable slips than unstable ones.
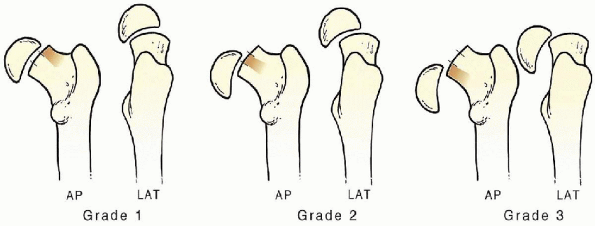
amount of slip is graded as I, II, or III or as a complete slip. If the
slip is only a few millimeters or in the first third starting from the
lateral side, the slip is a mild or Grade I slip. In a complete slip,
there is no continuity between the femoral head and the femoral neck. (Fig. 24-1).
The worse the slip, the greater the residual deformity will be. With
greater deformity, there is an increased risk of osteoarthritis.
Complete slips are associated with instability and carry a high risk of
avascular necrosis. All grades of slipped femoral capital epiphysis are treated with in situ pinning.
there is more urgency to stabilize an unstable slip. These patients are
admitted immediately and scheduled for surgical stabilization as soon
as possible. Stable slips can be scheduled over the next several days
if it is more convenient for the surgeon and patient.
 |
|
FIGURE 24-1.
The classification of a slipped capital femoral epiphysis is based on the degree of slip: Grade I, first third; Grade II, second third; Grade III, last third. |
it does not slip further. The preferred method is to percutaneously pin
the hip with a single implant. The femoral head is pinned in situ.
This technique is associated with minimal morbidity, a shortened
hospital stay, and a decreased incidence of complications. The presence
of a slip on radiographs of a patient that is skeletally mature does
not indicate surgical intervention, because there is no risk of further
slippage when the physis is fused.
epiphysis with certain metabolic disorders. The more common of these
disorders are hypothyroidism, growth hormone insufficiency, and renal
disorders. Other syndromes with known collagen deficiencies such as
Down syndrome also have an increased incidence of slipped capital
femoral epiphysis. Concomitant disorders have generally been diagnosed
before the time of presentation of a slipped epiphysis. Although it is
suspected through research that patients with slipped capital femoral
epiphysis have an unknown type of endocrine disorder, a workup is not
cost effective for each patient. A careful history and physical
examination is all that is needed. If the patient falls out of the
usual age range for slips, an endocrine workup is indicated. Patients
younger than 10 or older than 16 years of age would meet that criteria.
radiograph of the unaffected hip to check for bilateral slip
presentation. If radiographs reveal a second slip, both hips may
undergo in situ pinning at the same time.
The image intensifier is a necessity. A 6.5 mm cannulated hip pin is
used to stabilize the physis. A 7.3 mm cannulated pin may also be used.
Generally, only one pin is placed. However, in unstable slips, it may
be desirable to place two pins. In those cases, if there is not enough
room in the femoral head to place two 7.3 mm pins, 6.5 mm cannulated
pins are indicated.
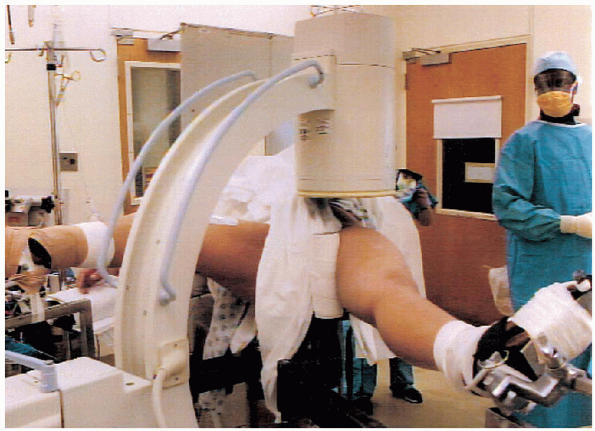
The operative leg is positioned with the hip extended, abducted, and
internally rotated. This position generally produces a gentle
reduction. A gentle reduction in this manner does not increase the
incidence of avascular necrosis.
and abducted or with the foot in a stirrup and the hip and knee flexed.
The position of the nonoperative leg is not important
as long as it does not impede the position of the image intensifier.
 |
|
FIGURE 24-2. Patient position on the table.
|
 |
|
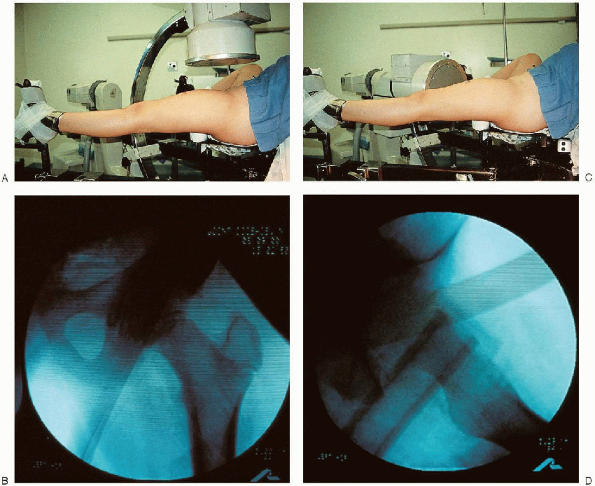
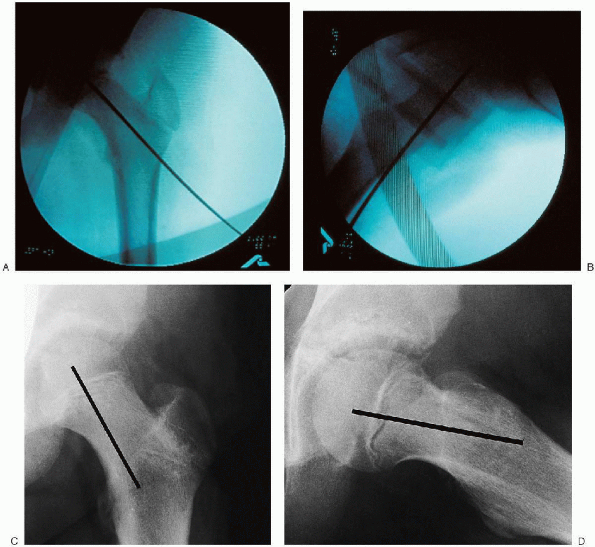
FIGURE 24-3. Image intensifier in the anteroposterior plane (A) and resultant image (B). Image intensifier in the lateral plane (C) and the image obtained (D).
|
is imperative that the image intensifier be positioned and images taken
before proceeding with the surgery. Good images of the hip are needed
in the anteroposterior and lateral planes. The physis and outline of
the femoral head must be distinctly visualized to place the pin
properly and avoid penetration of the joint. It should be possible to
obtain views in both planes by rotating the arm of the image intensifier (Fig. 24-3).

to the lateral groin and the thigh. A “shower curtain” draping is
generally used. Most starting points for the percutaneous pinning are
anterior. Care should be taken to ensure that the draping does not prevent an anterior entrance point.
head of the pin should be in the center of the femoral head and
perpendicular to the physis in the anteroposterior and lateral planes. Because
the femoral head is no longer in an anatomic position, concentrating on
the point where the pin enters the femoral neck will result in failure.
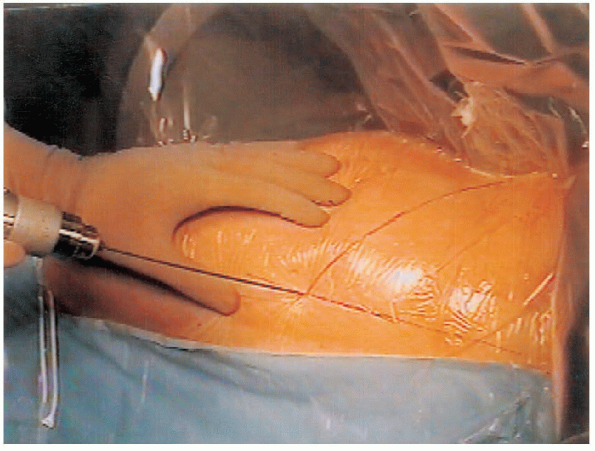
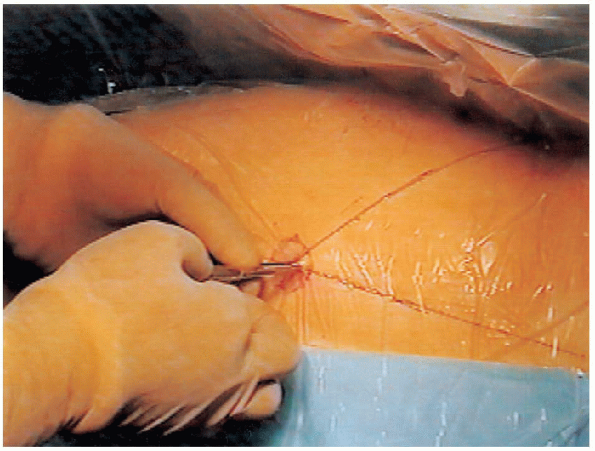
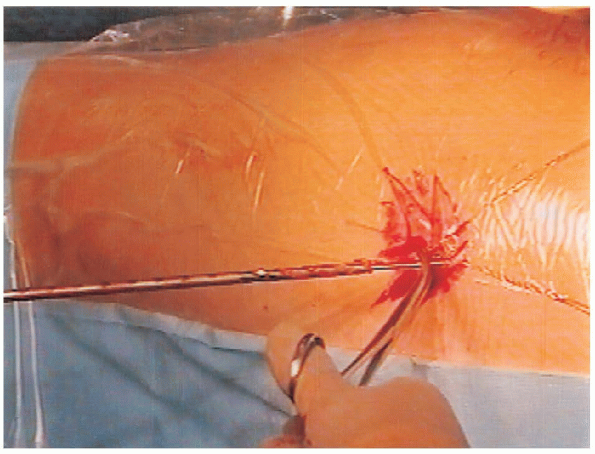
a guide wire or any other type of straight edge is placed on the
anterior groin. The guide wire is adjusted until an image is obtained
that shows the guide wire perpendicular to the physis.
A
skin marking pen is then used to draw a line on the skin along the
straight edge. The same maneuver is used with the image intensifier in
the lateral plane. A straight line is drawn on the skin. The
intersection of these two lines is the entrance point. The more severe the slip, the more anterior the entrance point will be (Fig. 24-4).
 |
|
FIGURE 24-4. A: An anteroposterior line is drawn on the skin. B: A lateral line is drawn on the skin. C: Anteroposterior and lateral lines are extended until they intersect. D: The entrance point for the pin is the intersection of lines.
|

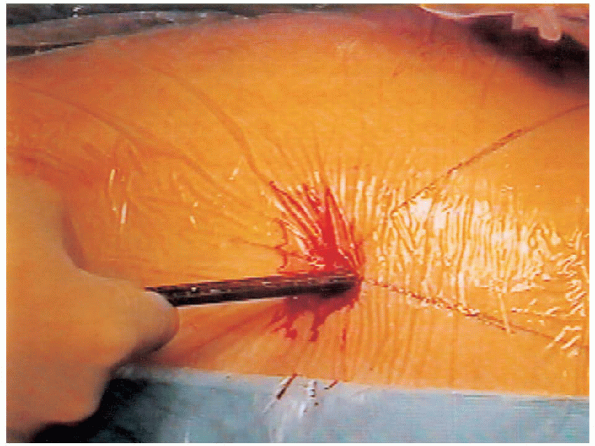
The wire is advanced onto the femoral neck a short distance (2.5 cm).
Its position is examined in the anteroposterior and lateral planes.

The surgeon looks at where the pin will be located in the femoral head,
not where it is entering the femoral neck. If the position is
satisfactory, the wire is advanced in the femoral head. The surgeon
usually feels a small amount of resistance as the guide wire crosses
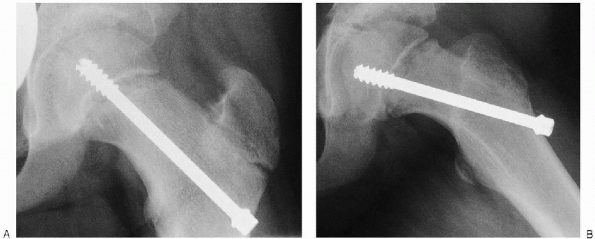
the physis. Only a few threads of the pin need to pass the physis. The pin should not go to the edge of the joint (Fig. 24-6).
 |
|
FIGURE 24-5. The guide wire enters the skin at the intersection of the drawn anteroposterior and lateral lines.
|
 |
|
FIGURE 24-6. Image intensifier views of the guide wire in the correct position in the anteroposterior (A) and lateral (B) planes. The guide wire is perpendicular to the physis and in the center of the femoral head. Radiographs (C, D) with a drawn black bar simulating the proper position of the guide wire and therefore the correct position for the hip pin.
|
 |
|
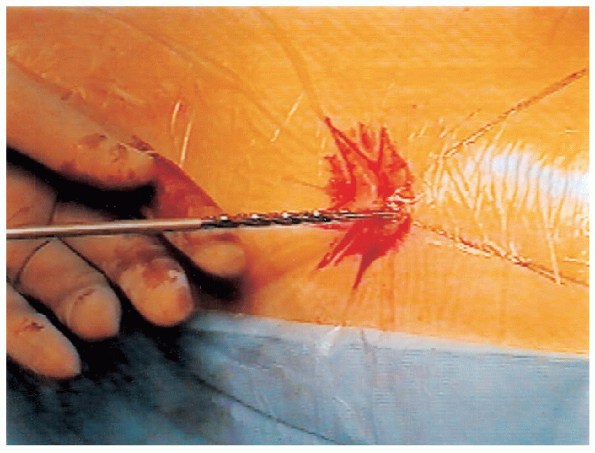
FIGURE 24-7. A 1-cm incision is made over the guide wire and continued through the fascia lata.
|
 |
|
FIGURE 24-8. The depth gauge is in place over the guide wire and in contact with the femur.
|
 |
|
FIGURE 24-9. A cannulated drill is placed over the guide wire.
|
 |
|
FIGURE 24-10. A hemostat is placed on the guide wire as the drill is withdrawn to ensure the guide wire remains in the bone.
|
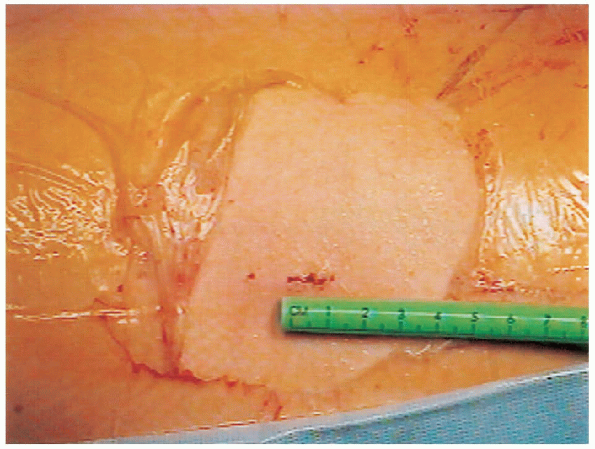
using the depth gauge supplied in the instrument set. The depth gauge
is placed over the guide wire and pushed onto the bone (Fig. 24-8). The image intensifier is used to confirm that the depth gauge is on the bone. The pins come in 0.5-cm increments.
 The drilling is done under the visual control of the image intensifier. If the guide wire catches in the drill, it may be advancing with the drill and cross the joint line.
The drilling is done under the visual control of the image intensifier. If the guide wire catches in the drill, it may be advancing with the drill and cross the joint line.This occurs when there may still debris in the drill from previous
cases or if the guide wire becomes bent. The surgeon should drill just
to the tip of the guide wire. The drill is then withdrawn. Care should
be taken not to remove the guide wire with the drill. It is helpful to use a hemostat to hold onto the guide wire as the drill is withdrawn from the incision (Fig. 24-10).
position of the pin is checked in the anteroposterior and lateral
planes. The cannulated drill is placed over the guide wire, and
drilling is started. As the drill is withdrawn, a hemostat is placed on
the guide wire so it does not come out of the wound. The hip pin is
then placed over the guide wire and advanced with the T-handle wrench. If the position is satisfactory, the guide wire is withdrawn (Fig. 24-12).
If the position is satisfactory, the guide wire is withdrawn (Fig. 24-12).
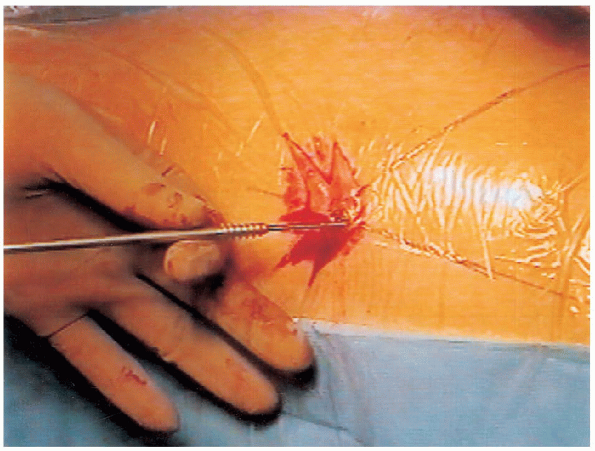
The small wound is then irrigated and closed. Only the subcutaneous and
skin layers need closure. A small dressing is then applied (Fig. 24-13).
 |
|
FIGURE 24-11. Advancement of the cannulated hip pin after positioning it over the guide wire.
|
 |
|
FIGURE 24-12. Anteroposterior (A) and lateral (B) radiographs show the pin in the correct position.
|
surgery. A criteria for discharge is independent ambulation on
crutches. Partial weight bearing is allowed. Because the pain relief is
significant postoperatively, most patients are able to ambulate with
crutches without difficulty. Patients can be weaned off their crutches
as their pain diminishes.
 |
|
FIGURE 24-13. Confirmation that only a 1-cm incision was required.
|
Avascular necrosis and chondrolysis are the two most serious
complications. The use of a single implant decreases the incidence of
both complications.
slip. One half of these cases have both hips involved at the time of
the initial presentation. The remaining patients present over the next
18 to 24 months while the physis is closing. Patients
should be followed until the capital physis fuses. Ordering an
anteroposterior and frog lateral radiograph rather than views of just
the operative side allows both hips to be evaluated.
avascular necrosis occurs and the pin is not penetrating into the
joint, the pin should be removed. Because the implant is placed
percutaneously, removal of the pin often results in a larger incision
and increased morbidity. If the pin does have to be removed, it can
often be accomplished by feeding the guide wire through the pin.
Endocrinologic and metabolic factors in atypical presentations of
slipped capital femoral epiphysis: report of four cases and review of
the literature. Clin Orthop 1983;180:188-197.
