Ultrasound Guided Infraclavicular Block
Supine, with ipsilateral arm abducted 120° with the elbow flexed 90°.
This position rotates the plexus away from the pleura and closer to the
surface of the skin.
The axillary artery and axillary vein lie just beneath the
clavipectoral fascia. Adjacent to the artery are found the cords of
brachial plexus: the lateral cord (cephaloanterior), posterior cord
(cephalad), and medial cord (cephaloposterior). The pleura and second
or third rib are seen deep to the axillary artery, vein, and plexus (Fig. 35-1).
Sterile prep of skin. Place a sterile cover over the probe or sterilize
the probe itself. Use sterile ultrasound gel on the field. Subcutaneous
local anesthetic is injected at the superior margin of the transducer.
The block needle is inserted at this site, at a 45° angle, and advanced
in-plane parallel to the long axis of the transducer, so that the
entire needle remains in view on the ultrasound machine screen. The
steep downward angle makes keeping the needle image intact on the
screen more challenging than with more
superficial
nerves. The needle is directed toward the cords in sequence, and as
each cord is contacted, the peripheral nerve stimulator is turned on,
with current set to 0.5 to 1 mA, if stimulation is desired for
confirmation. When sensory or motor stimulation confirms the
appropriate cord has been contacted, local anesthetic is delivered in
small aliquots, observing spread of local anesthetic around each cord
and any branches. This confirms that the needle tip is not
intravascular. For contact of the medial cord, wrist or finger flexion,
with ulnar deviation, is typical, as is thumb adduction. When the
lateral cord is contacted, wrist or finger flexion, or elbow flexion,
is expected. Finally, for stimulation of the posterior cord, elbow,
wrist, or finger extension is typical. At each cord, 5 mL of local
anesthetic is injected in small increments, creating a “halo” around
each one.
 |
|
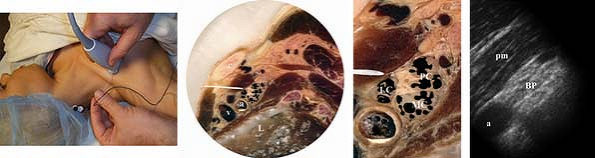
Figure 35-1.
a, axillary artery; BP, brachial plexus; c, clavicle; L, lung; LC, lateral cord; MC, medial cord; PC, posterior cord; pm, pectoralis minor; v, axillary vein. |
-
Innervation patterns vary and stimulation
may vary from the classic patterns described for the three cords. In
addition, some patients have only two cords, or very rarely, one cord. -
Some authors have reported good results
for ultrasound guided infraclavicular block by simply delivering a
circumferential bolus of local anesthetic around the entire axillary
artery. -
Note that the artery is usually cephalad
to the vein. It may be difficult to collapse the vein with chest wall
pressure, due to its depth. Color-flow Doppler can be helpful to
distinguish the two vessels, along with changes in caliber of the vein
with respiration. Both the artery and vein give rise to small branches
at this level, and it is imperative to look for these with ultrasound
as well as aspirating frequently during local anesthetic injection. -
The pleura and lung are only a few
millimeters deep to the posterior cord and vessels. Care must be taken
to keep the tip of the needle in view with ultrasound at all times in
order to avoid pneumothorax. -
Some authors advocate visualizing the cords and delivering local anesthetic to each without stimulation.
-
If the patient’s upper extremity is
fractured, or if the patient’s shoulder is frozen, the block can be
performed with the patient’s upper extremity adducted to the side. The
probe and needle approach are the same as described above. -
Some practitioners prefer to perform the
block at a more distal position along the plexus. In this case the
probe should be placed inferior to the coracoid process. The plexus
lies deeper here and may be more difficult to visualize. In this
location, the medial cord may lie posterior to the axillary artery, or
may be sandwiched in between the axillary artery and vein (Fig. 35-2).
 |
|
Figure 35-2.
a, axillary artery; cn, cutaneous nerve; m, median nerve; pma, pectoralis major; pmi, pectoralis minor; LC, lateral cord; mc, musculocutaneous nerve; MC, medial cord; PC, posterior cord; r, radial nerve; u, ulnar nerve; V, axillary vein. |
