The Shoulder and Arm
resulting in partial or complete paralysis of the upper extremity,
usually occurring secondary to perinatal complications. These injuries
occur in 0.1 to 0.4% of live births. Development of a plexus injury may
be related to a number of factors such as intrauterine positioning,
mismatch between infant size and the vaginal outlet, and the child’s
ability to selfprotect during a difficult delivery. These scenarios may
include multiparous pregnancy, prolonged labor, large size for
gestational age, fetal hypotonia secondary to
fetal
distress or maternal sedation, shoulder dystocia in vertex deliveries,
and arm and head extractions during breech presentations.
lesion. Partial injury to the plexus is most common and occurs at the
upper roots (C5-C6) resulting in Erb’s palsy. Weakness in shoulder
abduction, external rotation, elbow flexion, and forearm supination
result in the characteristic “waiter’s tip” posture of the upper
extremity.
result of root avulsions from the spinal cord and consequently have a
poorer prognosis. In addition to the extremity paralysis, these
preganglionic lesions manifest unilateral Horner’s syndrome
(anhydrosis, miosis, ptosis) from injury to the cervical sympathetic
chain, paralysis of the hemidiaphragm from phrenic nerve injury, and
asymmetric tonic neck and Moro reflexes.
Klumpke’s paralysis involving the lower spinal roots (C7-T1). Findings
include absence of the palmar grasp reflex and weakness of hand and
wrist flexors as well as hand intrinsics resulting in a clawhand
deformity.
method of determining the nature of the injury. Gross inspection of the
infant may demonstrate partial or complete paralysis of the affected
limb. Provocative testing by eliciting neonatal reflexes to induce
elbow, wrist, and digital extension may be used. The Moro reflex is
demonstrated by placing the infant face up on a soft, padded surface.
The head is gently lifted to remove the body weight from the pad. The
head is then released suddenly but quickly supported. The infant may
have a “startled” look as the arms fling out sideways with the palms up
and the thumbs flexed. As the reflex ends, the infant draws the arms
back to the body, elbows flexed, and then relaxes. Unilateral absence
of the Moro reflex may indicate neural or bony injury. Similarly, the
asymmetric tonic neck reflex, activated by turning the head to one
side, may be used to elicit upper extremity movement. As the head
turns, the arm and leg on the same side extends while the opposite
limbs bend.
as the cause of the paralysis or as a coexisting injury. Soft tissue
swelling may indicate a fracture of the clavicle or the proximal
humeral physis. Fractures of the clavicle are often initially
unappreciated, being discovered as a lump over the site of injury at
about 10 days after birth. Findings in proximal humeral physeal
fractures can be subtle, such as irritability with attempted arm
movement or pseudoparalysis. Plain films of the shoulder should be
obtained with comparison views of the opposite side. Because the
proximal humeral ossification centers do not coalesce until about 5 to
7 years of age, other studies may be necessary to confirm the
diagnosis; arthrography, ultrasound, and magnetic resonance imaging
(MRI) have been used to help delineate the position of the largely
cartilaginous proximal humeral fragment.
attempted to differentiate between root avulsions and extraforaminal
ruptures. One study examined the results of myelography, myelography
combined with computed tomography (CT), and MRI and comparing them with
operative findings in infants. CT myelography demonstrated a
truepositive rate of 94%; similar results were obtained with MRI with
the additional advantage of permitting more distal visualization of the
plexus.
(NCV) have also been used to further define the extent of the
neurological deficit. In the early postinjury period, documentation of
nerve recovery can be performed; however, the presence of motor
activity in a given muscle unit may not accurately reflect the extent
of useful motor function. Multiple investigators in helping to predict
functional outcome have emphasized the importance of serial clinical
examinations. Gilbert and Tassin first described the importance of
monitoring the return of biceps function as an indicator of overall
neurologic recovery. They noted that if normal biceps function did not
return by 3 months of age, the outcome at 2 years of age was abnormal. Michelow et al.
found increased accuracy in predicting outcome by combining elbow
flexion with return of wrist, finger, and thumb extension and shoulder
abduction. A general consensus exists that total plexus or C5-C7
involvement, or the presence of Horner’s syndrome, predict a poorer
prognosis for spontaneous recovery.
recovery, nonsurgical treatment is directed at preserving joint motion.
Daily passive motion of all affected joints should be performed with
adjunctive splinting as necessary to prevent contracture. Conservative
measures
should be continued until sufficient motor recovery has occurred or the
child is able to cooperate with a postoperative regimen following a
reconstructive procedure.
timing of operative intervention for brachial plexus injuries. The
timing of plexus exploration with microsurgical nerve graft
reconstruction or nerve transfers for upper root avulsions is based on
the overall extent of injury and return of biceps function. Infants
with total plexus involvement with Horner’s syndrome and no return of
biceps function at 3 months or partial plexopathy with no return of
biceps function between 3 and 6 months may be considered for surgical
intervention.
may develop significant contractures impairing activities of daily
living. Upper-trunk lesions result in weak external rotators against
intact internal rotators and adductors; this imbalance may lead to
posterior glenohumeral subluxation or dislocation with secondary
glenohumeral changes. In an attempt to avert this complication, a
subscapularis muscle slide has been described to increase passive
external rotation at 1 year of age for those unresponsive to physical
therapy.
contracture, external rotator and abductor weakness, and posterior
glenohumeral subluxation without significant glenoid deformity, the
Sever-L’Episcopo procedure has been successfully performed to address
the anterior contracture in addition to providing active external
rotation. First, open release of the anterior capsule with division of
the subscapularis and pectoralis major increase passive external
rotation. Second, transfer of the teres major and latissimus dorsi
tendons to the rotator cuff permits active external rotation.
and posterior glenoid is present from chronic subluxation or
dislocation, a derotational osteotomy of the proximal humerus becomes a
reasonable option. A transverse osteotomy is performed followed by
external rotation of the distal segment to improve the utility and
function of the existing arc of motion by rotating it into a more
central position.
arthrodesis improves stability and function of the upper extremity
after brachial plexus injuries with a resultant flail shoulder. Despite
the loss of glenohumeral motion, residual scapulothoracic and elbow
motion reliably permit activities at waist and midelevation levels.
plexus injury may require prosthetic replacement. Patients suffering
from debilitating pain unresponsive to conservative measures including
anti-inflammatory medications and activity modification may benefit
from a joint replacing procedure. However, given that resultant motion
and glenohumeral stability is highly dependent on the integrity and
function of the surrounding rotator cuff and deltoid musculature, pain
relief is a more reliable surgical goal.
diarthrodial, joint that connects the distal clavicle medially to the
acromial facet laterally. Between the articular cartilaginous surfaces
is a fibrocartilaginous meniscal disc of variable size and shape and
whose biomechanical role is poorly understood.
number of surrounding ligaments. In their biomechanical study of the
capsular and ligamentous structures of the AC joint, Fukuda et al.
induced fixed displacements and rotations, and recorded the forces and
torques required to produce them. The thicker superior and thinner
inferior acromioclavicular ligaments, in conjunction with the capsule,
are predominantly responsible for AC joint stability in the
anteroposterior as well as in the superior-inferior plane with small
displacements. The coracoclavicular ligaments, consisting of the conoid
and trapezoid ligaments, provide further stability to the AC joint with
larger displacements. The conoid provides the greatest contribution to
superior translation (62%) and the trapezoid resists most (75%) of the
axial compressive loads (as in weight lifting). In all degrees of
displacement, the primary restraint to posterior clavicular translation
is the AC capsule and ligaments.
confusion with the seemingly contradictory observations of clavicular
rotation with arm elevation and the little observed motion between the
acromion and clavicle. The clavicle does, indeed, rotate 40 to 50°
during full overhead elevation; however, the scapula simultaneously
rotates during this “synchronous scapuloclavicular” motion resulting in
very little relative rotation (5 to 8°) at the AC joint.
subject to inflammatory and degenerative processes. Primary
osteoarthritis of the AC joint appears to be related to the normal
aging process. The relatively small surface area of this joint is
subject to high loads and shear stresses with disc degeneration
occurring as early as the second decade and degenerative changes by the
fourth decade in the majority of specimens obtained from 151 patients.
osteoarthritis of the AC joint is relatively uncommon. In the
evaluation of pain around the shoulder, consider other possible
coexisting conditions. AC arthrosis may be only one of a number of
pathologic disorders such as rotator cuff impingement or glenohumeral
arthritis resulting in the symptom complex. Similarly in rheumatoid
arthritis, a recent prospective study of 74 patients demonstrated that
although the AC joint was affected more often than the glenohumeral
articulation, both joints were affected in almost half (42%) of the
cohort.
arthritis. Acromioclavicular sprains and separations and fractures of
the clavicle, particularly those with intra-articular extension, can
produce a painful joint. Osteolysis following repetitive microtrauma
has gained increased recognition as a potential source of AC joint
symptoms. Most commonly associated with weight-lifting activities, the
so-called “weightlifter’s clavicle” may result from repeated injury to
the subchondral bone resulting in microfractures. The resorptive
response following this trauma produces the characteristic osteolysis.
report discomfort and aching along the anterior and superior aspect of
the shoulder. Occasionally, the pain may radiate into the trapezius,
deltoid, and down the arm; irritation of the AC joint has been shown to
mimic symptoms similar to cervical radicular pain.
Reaching overhead to high shelves, behind the back to a back pocket or
to unhook a bra, or to the opposite shoulder or axilla for daily
hygiene increase contact between the acromial and clavicular facets.
Pain at night may also occur, disrupting sleep when the patient rolls
onto the affected shoulder.
demanding heavy-load or repetitive overhead activities resulting in or
exacerbating the pain. These patients may include laborers, throwers,
golfers, swimmers, and racquet-sport athletes. Weight-training
individuals often report onset of symptoms after bench pressing, dips
on the parallel bars, and push-ups.
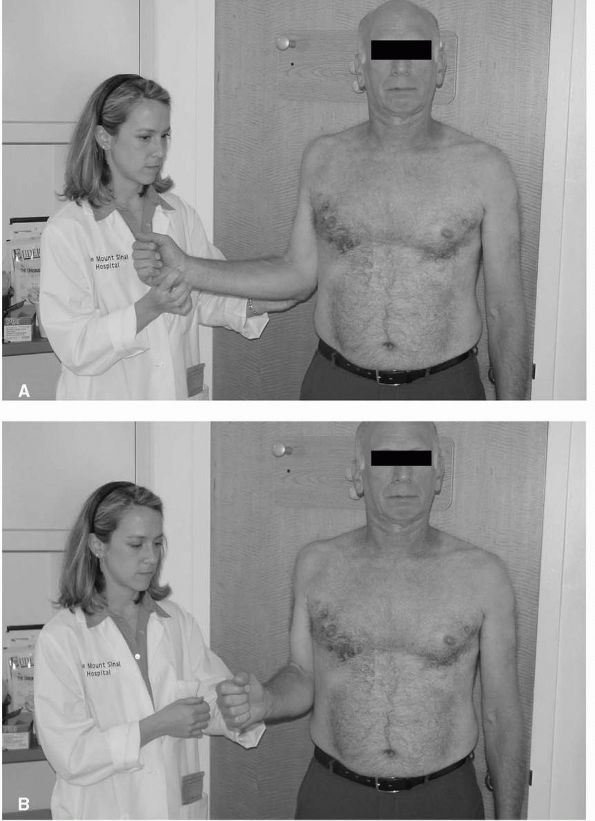
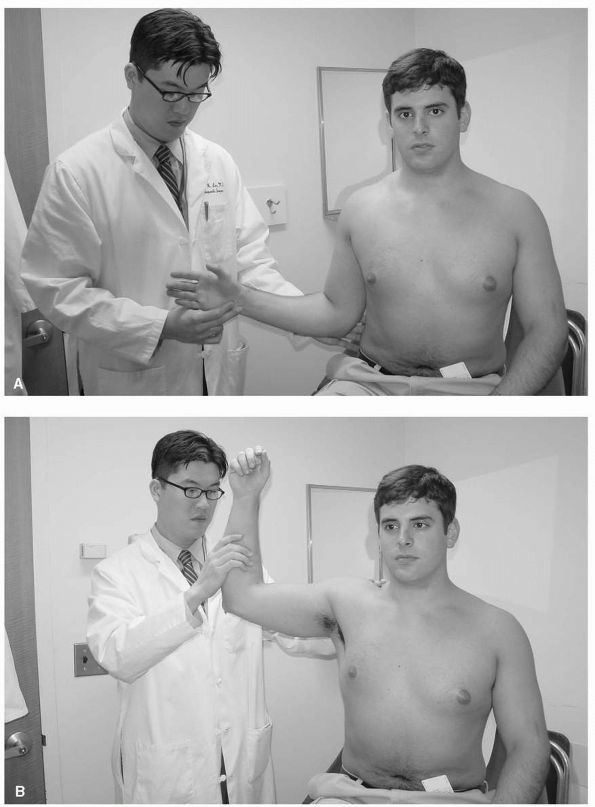
prominence and asymmetry secondary to osteophyte formation or
synovitis. Localized tenderness over the AC joint is present, and pain
may be reproduced with certain provocative maneuvers such as adducting
the arm across the body to the opposite shoulder (the cross-body
adduction test) or placing the shoulder into internal rotation with the
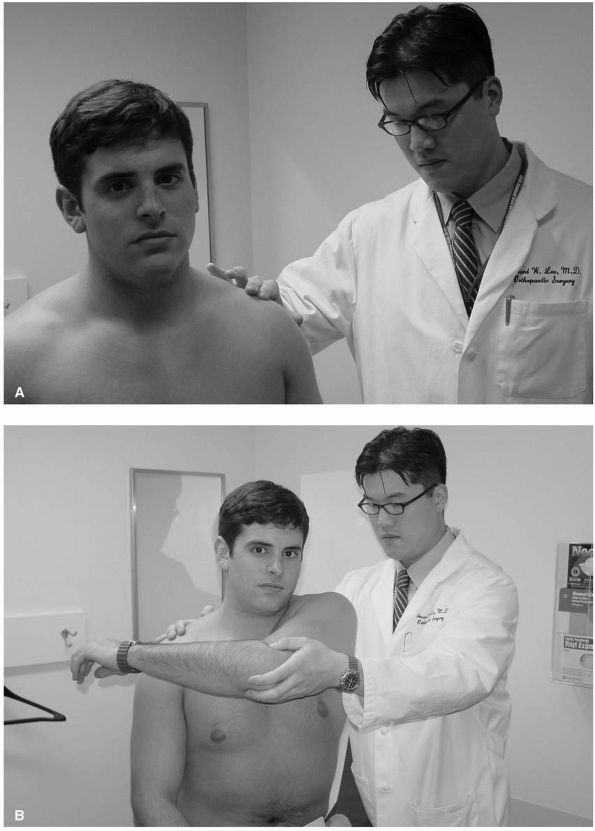
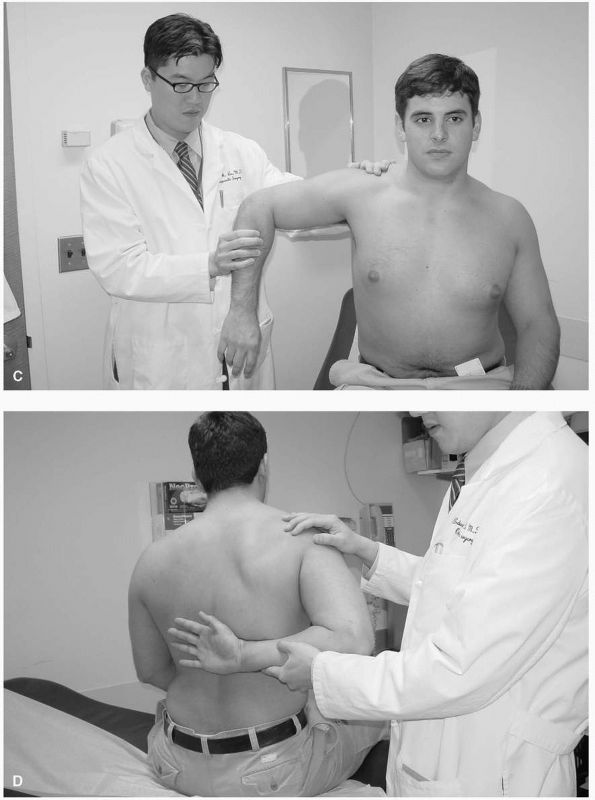
hand behind the back (Figure 12-1).
largely unaffected. With the exception of chronic cases that may
develop some loss of terminal internal rotation and cross-body
adduction, passive motion is rarely limited other than by discomfort.
Greater restrictions in motion may indicate underlying capsular
tightness or glenohumeral arthrosis.
with direct local anesthetic injection into the AC joint. Elimination
of symptoms several minutes following an injection may serve as a very
useful diagnostic tool as well as a reliable indicator of probable
success or failure with a distal clavicle excision procedure.
are usually sufficient for initial radiographic evaluation. The Zanca
view provides an unobstructed AP view of the AC joint by angling the
x-ray beam 10 to 15° cephalad. Stress views obtained with traction or
weights on the affected extremity are not routinely indicated in
evaluation of degenerative AC joint disorders but may be useful in
diagnosis of AC joint instability following trauma.
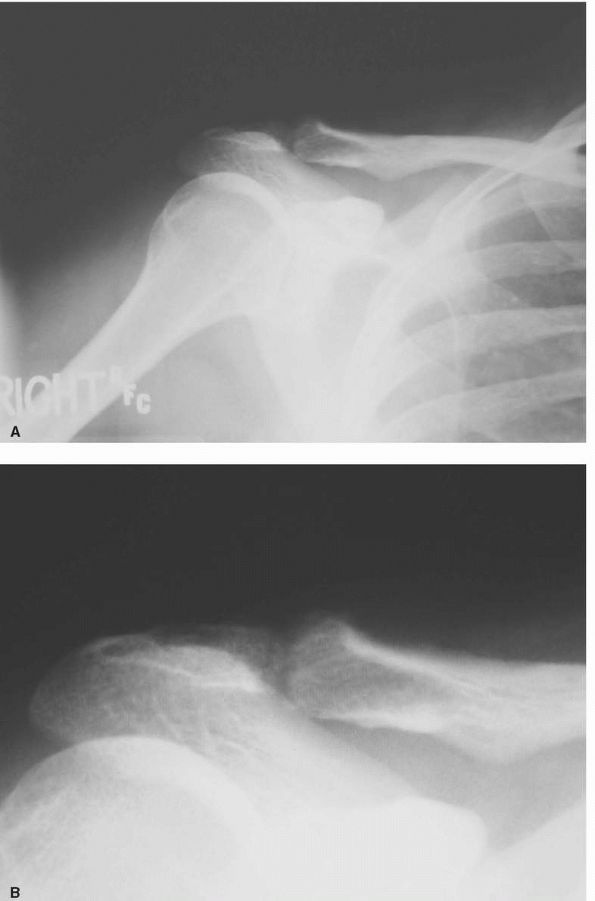
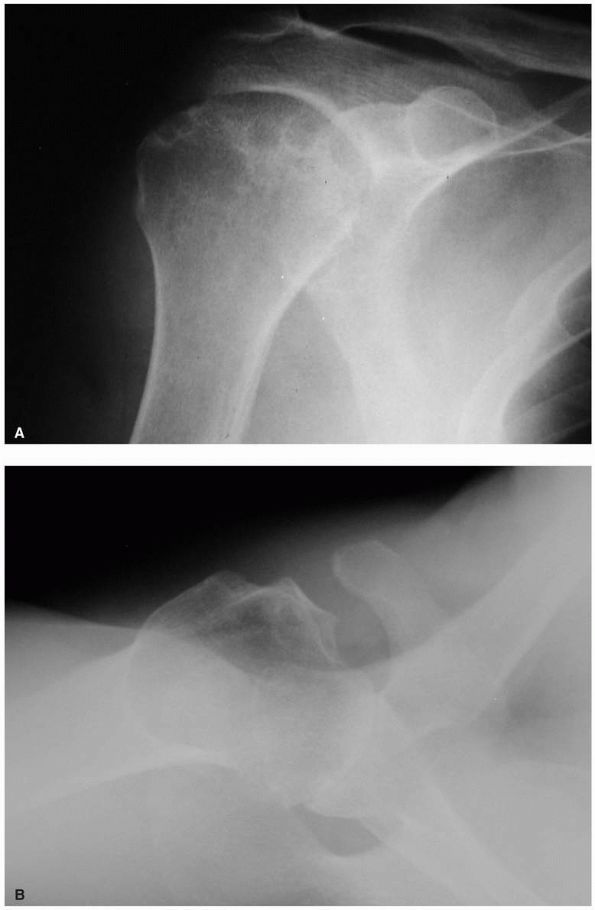
pathological process. Degenerative disease manifests itself similarly
to other joints with narrowing of the joint space, subchondral cysts
and sclerosis, and osteophyte formation (Figure 12-2).
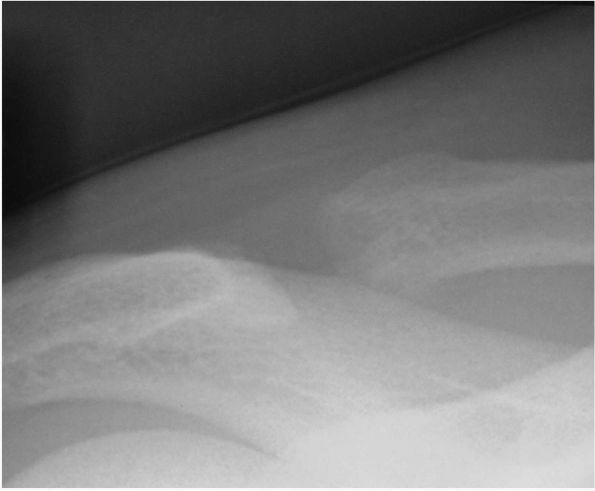
In contrast, osteolysis of the distal clavicle may demonstrate relative
osteopenia, widening or tapering of the distal clavicle, and expansion
of the joint space (Figure 12-3).
cases where plain radiographic findings do not correlate with the
clinical examination. In the active patient whose history and physical
exam are inconsistent with radiographic findings,
bone scintigraphy may detect subtle osteolysis as well as infectious or neoplastic conditions.
 |
|
FIGURE 12-1. (A) Palpation of the acromioclavicular (AC) joint; (B) cross-body adduction test elicits pain with AC arthritis and osteolysis.
|
osteolytic AC joint is nonoperative treatment. Activity modification,
heat, and nonsteroidal anti-inflammatory medications along with
judicious use of intra-articular steroid injections may adequately
alleviate symptoms. Physical therapy, while not directly addressing the
AC joint pathology, may be useful as an adjunct to decrease or prevent
restricted motion as well as address any associated rotator cuff
disease. Although some authors recommend 6 months prior to initiating
operative treatment, this must be adjusted to the patients’ activity
level, symptoms, and degree of disability.
surgical intervention may be considered. Open distal clavicle excision
was first described independently by Mumford and Gurd in 1941 and remains a reliable procedure allowing direct
visualization of the AC joint ensuring adequate bone removal.
 |
|
FIGURE 12-2. (A) and (B) Anteroposterior view of an arthritic AC joint with joint space narrowing and superior osteophyte formation.
|
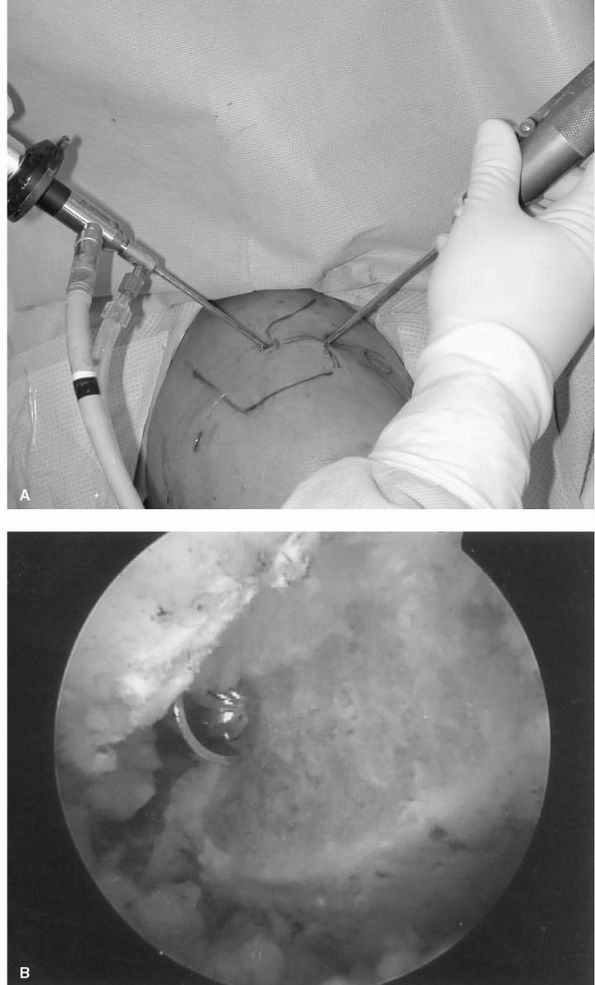
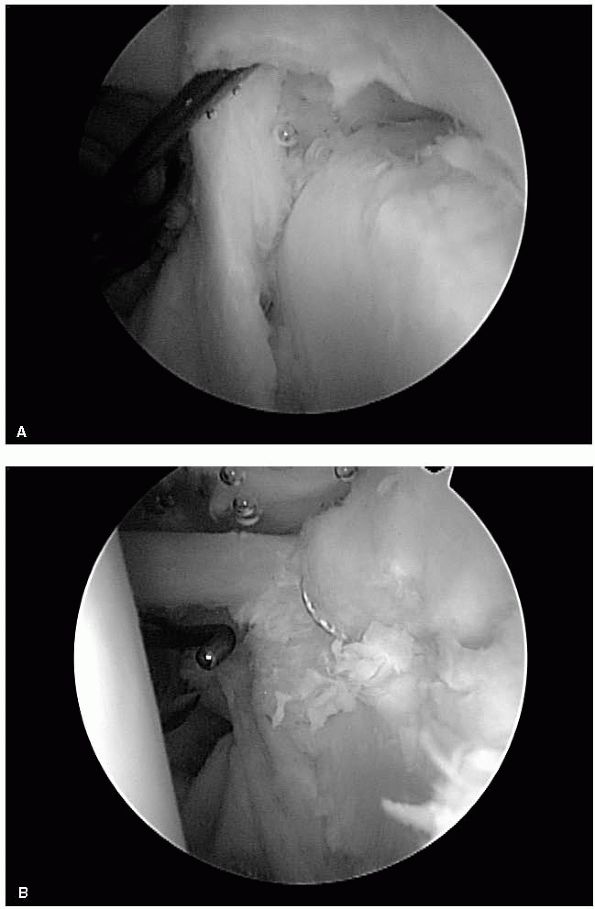
performed arthroscopically, the technique of arthroscopic distal
clavicle resection has become more common. Esch et al.
described a subacromial approach to excision of the distal clavicle in
patients undergoing a subacromial decompression procedure. A superior
direct approach to the AC joint was subsequently developed with the
theoretical advantage of preserving subacromial and capsular anatomy (Figure 12-4).
The advantages of either arthroscopic approach over open resection are
reduced morbidity with smaller incisions and avoidance of detaching the
deltoid and trapezius. However, more technical skill is required in
addition to the potentially higher risk of inadequate resection (Figure 12-5).
 |
|
FIGURE 12-3. Osteolysis of the distal clavicle demonstrating osteopenia and widening of the joint space.
|
and arthroscopic distal clavicle resection. Persistent pain or weakness
can occur and may be attributable to diagnostic error, inadequate bone
resection, or joint instability.
share the same characteristics as that of degenerative arthroses
elsewhere in the body. In all diarthrodial joints, hyaline cartilage
provides a congruent, smooth bearing surface with a coefficient of
friction 10 to 100 times less than that of ice on ice. In the
osteoarthritic shoulder, however, distortion of the articular surfaces
and joint orientation in addition to soft tissue contractures can lead
to pain and loss of function.
glenohumeral degenerative joint disease. In primary osteoarthritis, a
source cannot be identified but may result from a combination of
genetic and environmental factors resulting in articular cartilage
injury. Several secondary forms of arthritis have been described in the
shoulder including posttraumatic, rheumatoid, inflammatory,
postinstability repair, and rotator cuff arthropathy. The incidence of
shoulder osteoarthritis is higher in women and appears to increase with
age for the typical patient in the sixth or seventh decade of life.
were well characterized by Neer with the gross pathologic findings
similar across most of the patient population. Articular cartilage loss
with eburnation and sclerosis of the bone is most pronounced in the
area of the humeral head that contacts the glenoid between 60 and 100°
of abduction. Subarticular cysts may be present. Large peripheral
osteophytes occur most commonly at the inferior margin of the joint,
blocking rotation and enlarging the diameter of the head (Figure 12-6).
marginal osteophytes. These excrescences are easily palpated but
usually obscured from direct view by the overlying capsular and
ligamentous structures. Posterior glenoid wear is a common finding in
conjunction with an internal rotation contracture and posterior
subluxation of the humeral head.
 |
|
FIGURE 12-4. (A) Arthroscopic distal clavicle resection from a superior (direct) approach; (B) Resection of the distal clavicle viewed from the subacromial space.
|
pain over the course of several months to years. Pain localized to
“deep” in the joint or along the anterior and lateral deltoid is
common, although patterns vary. Symptoms may initially be merely a
nuisance but ultimately can become debilitating. Maneuvering the
affected extremity in space to perform basic activities such as daily
hygiene may become difficult, secondary to pain and loss of motion.
Interference with sleep may also occur with pain at rest and at night,
often with the patient rolling onto the affected side.
 |
|
FIGURE 12-5. (A) and (B) Postoperative anteroposterior views after distal clavicle resection.
|
restricted with a relative compensatory increase in scapulothoracic
motion. Contracture of the surrounding soft tissues, distortion of the
bony anatomy, osteochondral loose bodies, and pain may all contribute
to the loss of motion. Movement may elicit palpable and audible
crepitation or grating as the articular surfaces devoid of cartilage
rub against one another. Joint line tenderness with palpation is common
with the posterior margin usually more pronounced due to less overlying
soft tissue. Aside from weakness due to pain inhibition and disuse,
strength is usually well-preserved with a low incidence of tears of the
rotator cuff in association with osteoarthritis.
 |
|
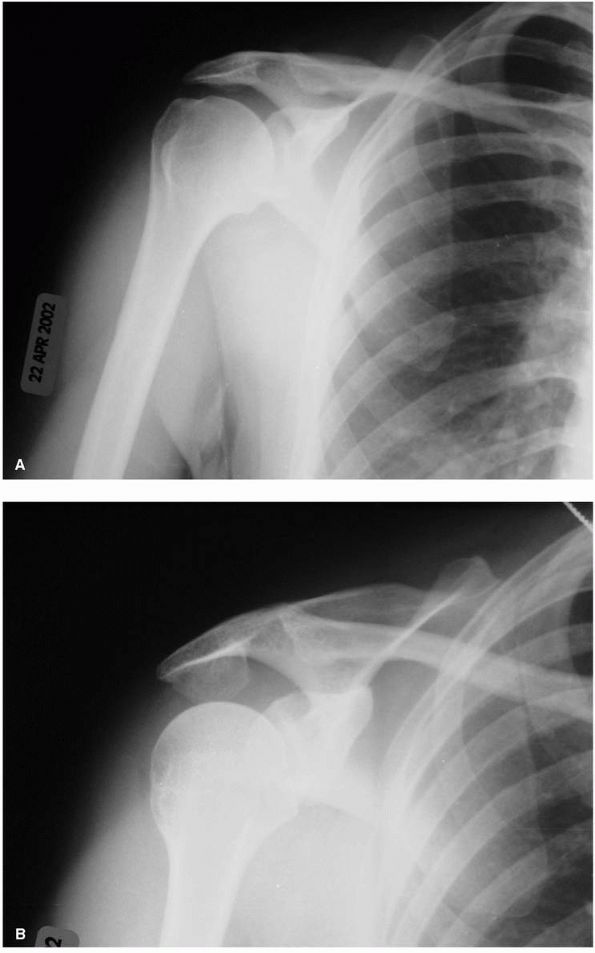
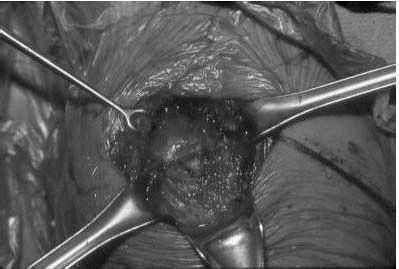
FIGURE 12-6. (A) and (B)
Intraoperative photographs of glenohumeral arthritis with flattening of the head, loss of articular cartilage, eburnation of the subchondral bone, and large peripheral osteophytes. |
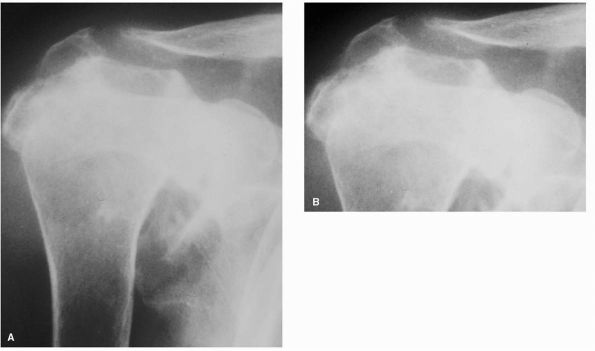
share similar roentgenographic features. Plain radiographs in the AP
and axillary planes are usually sufficient to evaluate the extent of
disease. The absence of articular cartilage manifests as a loss of the
joint space along with sclerosis of the subchondral bone and
subarticular cysts in both the humerus and glenoid. Flattening of the
humeral head and large peripheral osteophyte formation, particularly
along the anterior and inferior margins, results in an apparent
increase in the head diameter. Although rotator cuff tears are uncommon
in primary osteoarthritis, as previously mentioned, maintenance of the
subacromial space provides a simple initial indicator of rotator cuff
integrity (Figure 12-7).
preoperative planning. The AP view is useful in determining the amount
of medial glenoid bone loss. Posterior glenoid bone erosion is common
and is best visualized on the axillary view. The
combination
provides crucial information in predicting the ability to resurface the
glenoid. Although not routine in the initial workup of primary
osteoarthritis, an MRI, usually obtained to determine the status of the
rotator cuff, or CT, may also yield additional information about
glenoid alignment and bone quantity (Figure 12-8).
 |
|
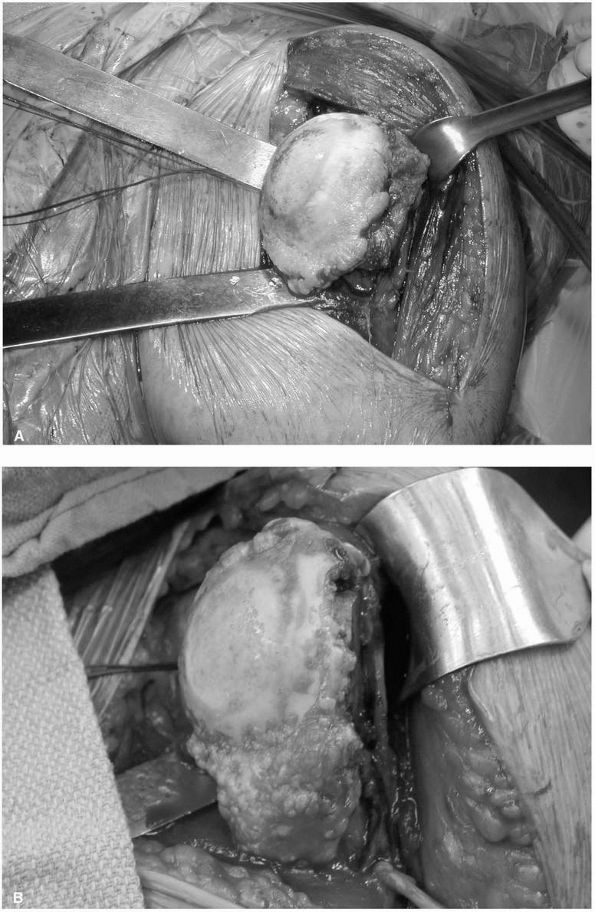
FIGURE 12-7. Glenohumeral osteoarthritis. (A) Anteroposterior radiograph demonstrating joint space narrowing (large black arrow), osteophyte formation (large white arrows), and subchondral cysts (small black arrows). (B) Axillary view showing typical posterior glenoid wear (large black arrows)
and posterior subluxation of the humeral head. The small black arrows indicate normal points of contact between the head and the glenoid. |
initial trial of conservative treatment. Judicious use of oral
anti-inflammatory medications, taken with the caveat of possible
gastrointestinal and renal side effects, may make symptoms tolerable.
Activity modification may diminish exacerbating events but can be
difficult or impossible to institute when symptoms are elicited with
activities of daily living. Intra-articular steroid injections may
provide longer lasting relief but remain unpredictable in duration and
carry the catastrophic risk of infection. Aside from maintaining
generalized strength and conditioning of the muscles, physical therapy
has no formal role in treatment and may in fact worsen symptoms.
nonoperative therapy. Several options have been described ranging from
arthroscopic debridement to prosthetic arthroplasty with distinct
indications for each intervention.
 |
|
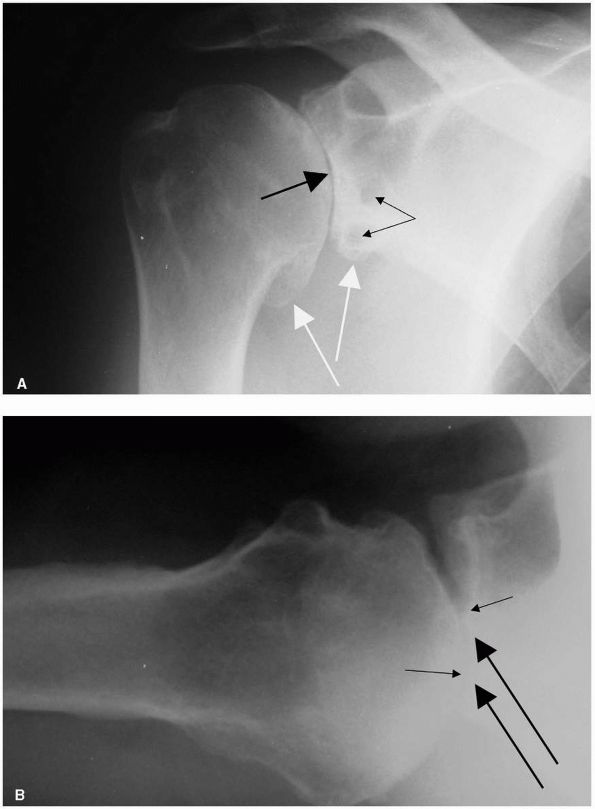
FIGURE 12-8. Axial CT image of the glenohumeral joint demonstrating posterior glenoid wear and subchondral sclerosis and cyst formation.
|
extent of disease as a primary influence on outcome. Success with this
technique has been demonstrated in patients with evidence of early
osteoarthritis. One study found arthroscopy as a reasonable option when
the humeral head remains concentric within the glenoid and where some
joint space remains on the axillary radiograph. Another group found
that patients with Outerbridge IV changes could gain significant
improvement in pain relief and function with results deteriorating with
lesions greater than 2 cm in diameter.
for glenohumeral osteoarthritis. Appropriate situations may include
painful arthritis with permanent loss of motor function (i.e., brachial
plexus injuries or insufficiency of the deltoid and rotator cuff),
chronic infection, failed revision arthroplasty, severe refractory
instability, or bone loss following tumor resection. In the young
patient who is likely to place excessive demands on a prosthesis with
heavy manual labor, consider an arthrodesis. Although it remains a
viable salvage procedure to achieve pain relief, fusion results in
significant functional limitations such as loss of internal and
external rotation and use of the extremity above shoulder level.
treatment of glenohumeral osteoarthritis. This treatment modality, now
essentially reserved for failed arthroplasty with extensive bone loss
and salvage after severe infection, results in limited motion and
variable pain relief.
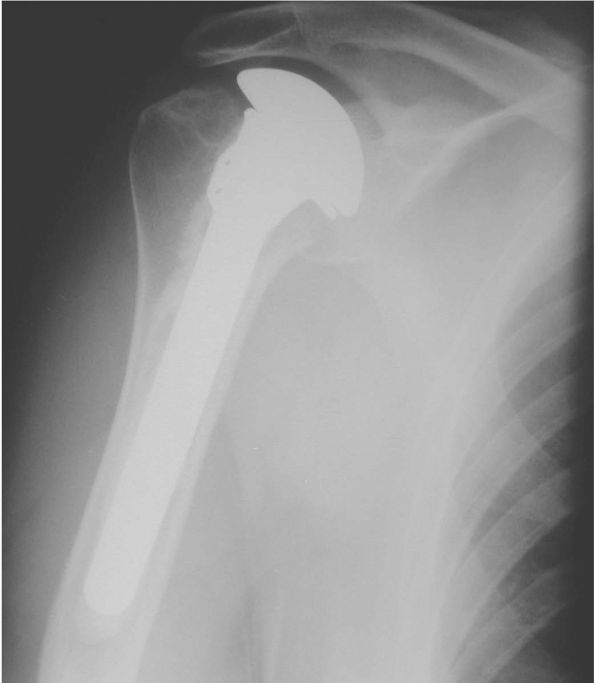
humeral head (hemiarthroplasty) or the head and the glenoid (total
shoulder replacement), remains the treatment of choice for most cases
of degenerative osteoarthritis of the glenohumeral joint. In the early
1950s, Neer introduced his technique and design for humeral head
replacement for complex shoulder fracture-dislocations. Current
technology includes a polyethylene glenoid component and adaptation of
the humeral prosthesis with most modern systems providing an array of
modular stem and head sizes (Figure 12-9).
predictable pain relief as well as functional improvement with an
intact functional rotator cuff and appropriate physical therapy. Both
total shoulder replacement and hemiarthroplasty can reliably provide
improvement in pain in more than 90% of patients; however, humeral head
replacement alone may result in less pain relief, relief that
deteriorates with time, and inferior functional outcomes (Figure 12-10).
to excellent in the vast majority of cases, potential complications are
a concern with any prosthetic reconstruction. With an overall incidence
reported to
be
approximately 14%, problems may occur, including instability, rotator
cuff tear, glenoid and humeral component loosening, intraoperative
fracture, nerve injury, and infection. Revision surgery can
successfully manage many of these causes of failed shoulder
arthroplasty, but overall results are inferior compared to primary
procedures.
 |
|
FIGURE 12-9. Modular shoulder prosthesis. (A) Multiple stem, (B) and (C) glenoid, and (D) head sizes and configurations. (Courtesy of Zimmer, Warsaw, IN)
|
necrosis, is a condition caused by a vascular insult leading to death
and collapse of the bone. Although more commonly affecting the femoral
head and similar in many respects, osteonecrosis of the proximal
humerus is a distinct entity with different clinical manifestations.
interruption of the blood supply to the humeral head can lead to
osteonecrosis. Reported causes include trauma, corticosteroid use,
alcohol abuse, radiation, dysbarism, cigarette smoking, and systemic
diseases such as Gaucher’s disease, rheumatoid arthritis, systemic
lupus erythematosus, and infection with human immunodeficiency virus.
Sickle cell hemoglobinopathy is the most common cause
of osteonecrosis worldwide. Occasionally, no cause can be identified.
 |
|
FIGURE 12-10. Total shoulder arthroplasty. (A) Anteroposterior and (B) axillary radiographs of a total shoulder prosthesis.
|
the extent of disease. Patients will typically present with pain that
is not well localized and worse with activity. Night pain and pain at
rest may occur but not as commonly as with other disorders of the
shoulder, such as osteoarthritis or rotator cuff disease. Active motion
may be affected early in the disease process by pain inhibition, but
passive motion is often preserved unless capsular contracture and
secondary osteoarthritis are present. Strength is usually preserved
except in those cases with underlying cuff pathology or systemic
disease affecting the muscles.
radiographs in orthogonal planes. Cruess’s modification of the
Ficat-Arlet classification of osteonecrosis of the femoral head is the
most widely used system for evaluation and treatment planning. The
continuum ranges from stage I where
changes
are not visible on plain radiographs; stage II characterized by focal
sclerosis; stage III with subchondral collapse and loss of the head’s
spherical contour (the crescent sign); stage IV with an area of
collapsed articular surface; and stage V with signs of secondary
arthritis on both the humeral and glenoid surfaces (Figure 12-11).
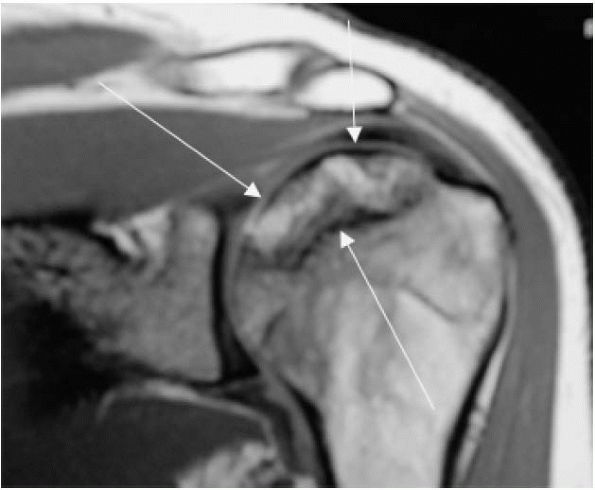
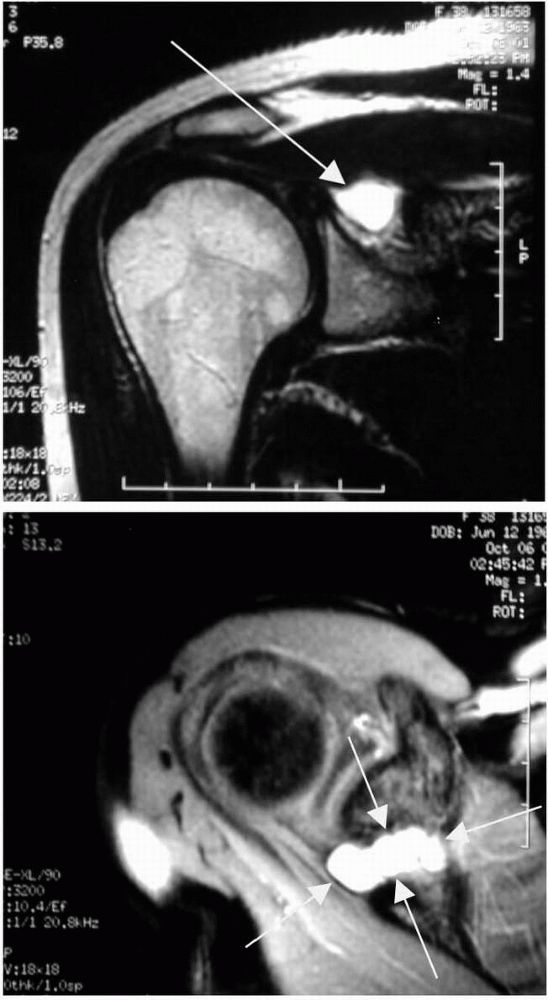
Signal intensity on MRI depends on water and fat variations and
therefore can reveal osteonecrosis prior to radiograph changes (Figure 12-12).
Bone scanning has been used for early detection of the disease, but
recent work has called its utility into question with failure to detect
more than half of the lesions identified by MRI and histology.
with relationship to etiologic factors and extent of involvement. In
general, clinical progression is slow with most patients presenting
with advanced radiographic changes. Patient with sickle cell disease
tend to have the most benign course. Corticosteroid-induced
osteonecrosis appears to fare better than posttraumatic causes with Hattrup and Cofield finding almost twice as many trauma-related cases requiring arthroplasty at 3 years after diagnosis.
 |
|
FIGURE 12-11. Avascular necrosis of the humeral head with collapse of the subchondral bone.
|
instituted with oral anti-inflammatory medication and physical therapy
for range of motion and strengthening exercises. These interventions
are often more successful in the shoulder than in the hip for several
reasons. The glenohumeral joint is not subjected to the same
weight-bearing forces, the articulation is less conforming than the
acetabulum and can tolerate greater deformity, and scapulothoracic
motion can partially compensate for lost glenohumeral motion.
operative management may provide relief of symptoms. Core decompression
has been described with some good results in earlier stages of disease.
LaPorte et al. reported their experience with
63 shoulders followed for an average of 10 years. Results demonstrated
success rates as high as 94% for stage I disease and falling
precipitously to 14% for stage IV osteonecrosis.
shoulder arthroplasty, may be appropriate in stage IV and V disease and
select patients with stage III involvement (Figure 12-13). Glenoid resurfacing is used when the glenoid is involved with substantial secondary arthritis. In a recent study, 88
shoulders followed for an average of 8.9 years were treated with either
hemiarthroplasty or total shoulder arthroplasty with 79.5% reporting
subjective improvement and 77.3% with no to moderate pain. Inferior
clinical results were noted in posttraumatic osteonecrosis and superior
results in corticosteroid-induced disease.
 |
|
FIGURE 12-12. Coronal MRI image of avascular necrosis of the humeral head (depicted by white arrows).
|
initiating operative treatment and should be based on patient function,
symptomatology, and radiographic findings. Rutherford and Cofield
reviewed the data on 33 shoulders and concluded that even with
extensive radiographic changes (stage IV and V), mild symptoms will not
necessarily progress and can be treated nonoperatively.
inflammatory disease with formation of destructive, hyperplastic
synovium or pannus. The inflammation results in erosive, symmetrical
polyarthritis with approximately 91% of patients with long-standing
disease developing shoulder symptoms.
insidious onset of pain, swelling, and loss of motion. All
synovial-lined joints may be affected including the acromioclavicular,
sternoclavicular, and glenohumeral joints, although the latter can be
the only symptomatic location in up to two-thirds of patients.
preserving passive motion. Development of soft tissue contracture and
bony destruction may eventually affect passive motion as well. Strength
may deteriorate with muscle atrophy and rotator cuff disease, which is
found in as high as 75% of patients with RA.
exhibiting only minimal findings with more extensive changes late in
the course of disease. Plain radiographs may reveal only osteopenia of
the humeral head and glenoid. Symmetrical
marginal
erosions along the inferior humeral head and subchondral cysts develop
and may eventually involve large portions of the head. Glenoid
destruction occurs with disease progression demonstrating central or
peripheral erosions (Figure 12-14).
Osteosclerosis and osteophytosis is uncommon in RA and typically
reflects quiescence of the inflammation and development of secondary
osteoarthritis.
 |
|
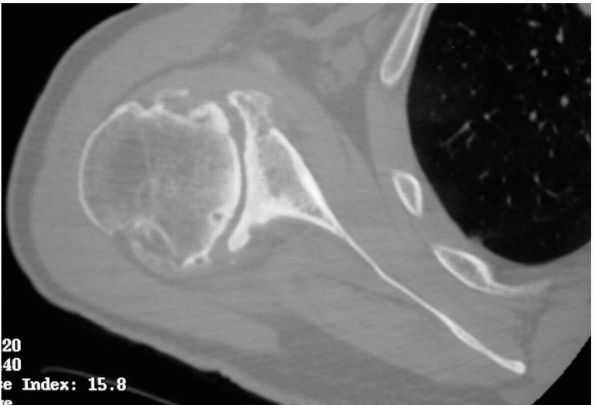
FIGURE 12-13. Intraoperative photograph of avascular necrosis of the humeral head. Note the collapse of the articular surface.
|
incompetence of the rotator cuff. Continued contact between the head
and the undersurface of the acromion can produce erosion and thinning
of the acromion process and possible fracture (Figure 12-15).
of the disease. The extent of synovial proliferation and joint effusion
can be visualized. More importantly, the integrity of the rotator cuff
can be determined with pathology ranging from mild inflammation to
full-thickness tears.
architecture is best evaluated with CT scan. In the preoperative
planning process, quantification of bone loss, particularly when
considering implantation of a glenoid component, may be necessary; CT
scan has been shown to provide superior characterization of bony
defects compared to conventional radiography.
affecting the shoulder is appropriate in the early phases of disease
with minimal bony destruction. Physical therapy may be helpful in
maintaining active and passive motion during acute exacerbations and
gradually adding resistive exercises to preserve strength.
controlling the disease process prior to development of extensive
radiographic changes
and
severe symptoms unresponsive to conservative measures. Limited trials
of corticosteroid injections may be useful in reducing the symptoms of
acute inflammation unresponsive to oral medications aimed at the
underlying disease process. Communication with the patient’s
rheumatologist is essential prior to embarking on surgical treatment.
When the rheumatologist’s medical armamentarium of nonsteroidal
anti-inflammatory medications, antimetabolic drugs, steroids, and
disease-modifying drugs has been exhausted, surgical intervention
should be considered. However, once joint destruction is demonstrated,
early replacement before loss of the rotator cuff and glenoid vault
preclude glenoid resurfacing should be considered.
 |
|
FIGURE 12-14. (A) Anteroposterior and (B)
axillary views demonstrating rheumatoid arthritis of the glenohumeral joint. Narrowing of the joint space, large subchondral cysts, and medialization of the glenoid are typical. Note the absence of large peripheral osteophytes commonly seen with osteoarthritis. |
 |
|
FIGURE 12-15. (A) and (B) Destructive rheumatoid arthritis with superior migration of the humeral head and erosion of the acromion and distal clavicle.
|
preservation of the glenohumeral articular surfaces, bursectomy and
synovectomy may be useful. Synovectomy may also help slow disease
progression in aggressive cases of synovitis.
be considered for patients with severe pain and functional limitation
unresponsive to more conservative modalities. The indications for
humeral head replacement are an irreparable rotator cuff tear or
inadequate glenoid bone stock precluding adequate fixation of the
polyethylene component (Figure 12-16). Most
patients who undergo prosthetic arthroplasty for RA can expect some
pain relief and improvement in shoulder function, but results are less
reliable than in the treatment of osteoarthritis.
can develop from a number of differing mechanisms. Commonly, arthritis
can develop as a result of a proximal humerus fracture treated
operatively or nonoperatively. Glenohumeral instability also may result
in degenerative changes either as a result of the trauma itself or,
more frequently, from the surgical treatment.
similar to other forms of degenerative arthritis of the shoulder. Pain
level is variable but is usually the primary complaint. Motion may be
restricted by pain, bone deformity, and contractures of the surrounding
capsule and rotator cuff. Strength may be compromised as well from
injury to the rotator cuff and deltoid or from alterations in rotator
cuff attachments seen in proximal humerus malunions and nonunions.
Neurologic injury should always be considered and appropriate
evaluation with an EMG should be performed if there is clinical
suspicion.
proximal humerus may demonstrate malunion or nonunion of the
tuberosities, head segment, or surgical neck or articular surface
collapse from posttraumatic osteonecrosis. Arthritis resulting from
anterior instability may show a Hill-Sachs lesion on the posterolateral
humeral head, a so-called Reverse Hill-Sachs lesion on the anteromedial
head in posterior dislocations, persistent anterior or posterior
subluxation with corresponding glenoid bone loss, or a chronic
dislocation with bony injury to the humerus and glenoid. The presence
of metallic implants used for fracture fixation or instability repair
have the potential to encroach on the glenohumeral joint and may be
evident on radiographic examination.
 |
|
FIGURE 12-16. Postoperative anteroposterior radiograph of Figure 12-14 after hemiarthroplasty.
|
preoperative planning in more complex cases where the normal anatomical
relationships have been distorted by the injury.
an initial form of treatment. Activity modification, gentle exercises,
and anti-inflammatory medications may provide enough symptomatic relief
to avoid surgical intervention.
therapy has failed. When arthritis has developed secondary to fracture
nonunion or malunion, osteotomies or soft tissue procedures alone will
not address the articular incongruity. Humeral head and glenoid
articular destruction would likely most benefit from prosthetic
replacement. In cases of arthritis following instability repair, mild
arthritic change and significant loss of external rotation due to
tightening of the anterior soft tissue structures may benefit from
anterior releases. Studies examining arthroplasty for arthritis
following instability repairs have shown reduction in pain and improved
function but high rates of revision surgery secondary to instability,
component failure, and pain due to an unresurfaced glenoid at long-term
follow-up. The difficulties following previous injury or surgery
including extensive scarring and distortion of the normal bony and soft
tissue anatomical relationships make these cases challenging for even
the most experienced of surgeons.
collapse of the subchondral bone of the humeral head are the hallmarks
of a clinical entity termed cuff-tear arthropathy
by Neer. A diagnosis of rotator cuff-tear arthropathy (RCTA) requires
the aforementioned findings in addition to progressive bone loss of the
glenohumeral joint, coracoacromial arch, and the distal clavicle.
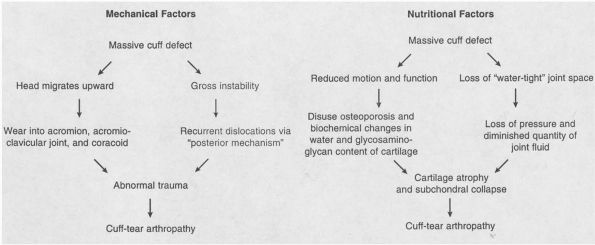
suggested that the precipitating event in RCTA was, as its name
suggests, the massive, untreated rotator cuff tear. They noted,
however, that only 4% of shoulders with full-thickness cuff tears
progressed to RCTA. Thus, aside from pure mechanical dysfunction, other
possible contributing factors must be involved to account for the
pathologic findings (Figure 12-17).
the glenoid and provides the mechanism for rotation of the glenohumeral
joint. Full-thickness tears of the cuff may disrupt these functions as
well
as provide a conduit for escape of synovial fluid essential for cartilage nutrition.
 |
|
FIGURE 12-17. Proposed mechanisms of development of rotator cuff-tear arthropathy. (From Neer CS II, Craig EV, Fukuda HA. Cuff-tear arthropathy. J Bone Joint Surg 1983;65r:1232-1244.)
|
the role of crystal deposition and the subsequent inflammatory cascade
and injury in the pathogenesis of a clinically similar disease. McCarty et al.
hypothesized that diseased synovium and cartilage release basic calcium
phosphate crystals in shoulders clinically similar to RCTA but what
they termed Milwaukee shoulder syndrome. The ensuing inflammatory
response results in injury to the rotator cuff and articular cartilage.
with predictable symptoms related to arthritis and cuff deficiency. A
long history of progressively worsening pain and stiffness is typical.
Both active and passive motion may be affected secondary to joint
incongruity, pain, and lack of a competent rotator cuff. Dislocation or
rupture of the tendon of the long head of the biceps occurs in most
patients and may be detected on exam. Many patients also exhibit
significant shoulder swelling resulting from synovial fluid
communication between the glenohumeral joint and subacromial bursa (fluid sign).
Aspiration of this fluid may reveal a bloody or blood-streaked
effusion. Large ecchymoses down the arm are not unusual, and often spur
fruitless workups for clotting abnormalities. Shoulder girdle muscular
atrophy, weakness, and loss of active and passive motion will be
evident resulting from disuse, pain, joint incongruity, and the large
rotator cuff tear.
of the shoulder are characteristic of RCTA. Early in the disease
process, radiographic changes may only reflect a large rotator cuff
tear with proximal humeral migration and abutment against the
undersurface of the acromion. Progression will involve extensive
erosion of the proximal humerus and narrowing of the glenohumeral joint
(Figure 12-18). A standard axillary radiograph may reveal subluxation or dislocation of the proximal humerus.
is typically not indicated in the evaluation of RCTA, given the drastic
changes seen on plain radiography suggestive of a massive, chronic
rotator cuff tear. Similarly, CT scan does not have specific utility in
preoperative planning aside from assessment of bone loss.
nonoperative management is reasonable. Oral nonsteroidal
anti-inflammatories, limited trials of intra-articular cortisone,
activity modification, and gentle exercises may provide some
symptomatic relief.
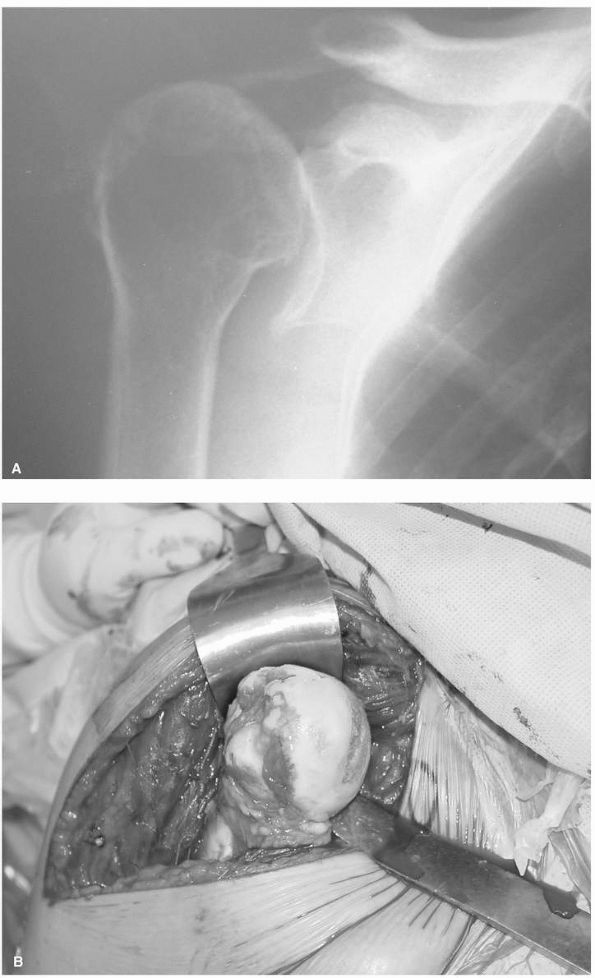 |
|
FIGURE 12-18. (A)
Anteroposterior radiograph of cuff-tear arthropathy with superior migration of the head and arthritic changes of the glenohumeral joint. (B) Intraoperative photograph with erosion of the articular surface and absence of the rotator cuff. |
Arthrodesis, now considered a salvage procedure by most surgeons, may
rarely be indicated in the setting of the arthritic shoulder with an
irreparable cuff tear and an incompetent deltoid. Constrained shoulder
arthroplasty, involving a coupled humeral and glenoid articulation,
theoretically provided a stable fulcrum around which the remaining
deltoid could rotate the humerus. However, the tremendous stresses
generated from this construct have been shown to lead to rapid
component loosening, catastrophic implant failure, and fracture.
currently the surgical treatment of choice for this patient population
with pain relief as the primary goal. Despite providing a painless
articulation with prosthetic replacement, the remaining cuff defect
will result in a persistently weak shoulder. Multiple studies examining
the results of total shoulder arthroplasty have emphasized the
importance of the rotator cuff in centering the humeral head on the
glenoid during active motion. Loss of this stabilization effect from an
unrepaired or irreparable cuff tear has been shown to result in
eccentric loading and early failure of the glenoid component. Although
every attempt should be made at reconstructing the rotator cuff, it is
now recommended that large defects with proximal humeral migration
should be treated with hemiarthroplasty alone with preservation of the
coracoacromial arch to prevent anterosuperior migration of the
component (Figure 12-19).
 |
|
FIGURE 12-19. Absence of the coracoacromial arch and injury to the deltoid leads to anterior-superior ascent of the shoulder prosthesis. (A) At rest and (B) with attempted glenohumeral motion.
|
shoulder prosthesis with a concave humeral articulation and a spherical
glenoid. Early results in Europe have been promising with respect to
stability and function, however, glenoid survival remains a concern.
Long-term experience with this prosthesis is lacking, and it has only
recently been approved for use in the United States.
disorders ranging from subacromial bursitis and tendinosis to
full-thickness tears. Proper diagnosis and treatment of these disorders
is based on an understanding of the basic anatomy and function of the
rotator cuff as well as the intrinsic and extrinsic factors associated
with cuff tendon degeneration.
ball-and-socket-type articulation with tremendous capacity for motion
in multiple planes. This motion is
obtained
through the sacrifice of joint stability. Often likened to a “golf ball
on a tee,” the humeral head articulates with the small, shallow glenoid
surface. The labral, capsuloligamentous, and musculotendinous
structures surrounding the joint provide compensation for the lack of
inherent bony restraint.
units that provide multiple functions including motion about the axis
of the joint. The subscapularis, which originates on the anterior
surface of the scapula and inserts onto the lesser tuberosity of the
humerus, provides internal rotation, particularly at the end range of
motion. The supraspinatus originates from the supraspinatus fossa of
the scapula, and inserts on the greater tuberosity of the humerus and
contributes to shoulder abduction. External rotation power is produced
solely by the infraspinatus and teres minor, both of which originate
from the scapula and insert onto the greater tuberosity.
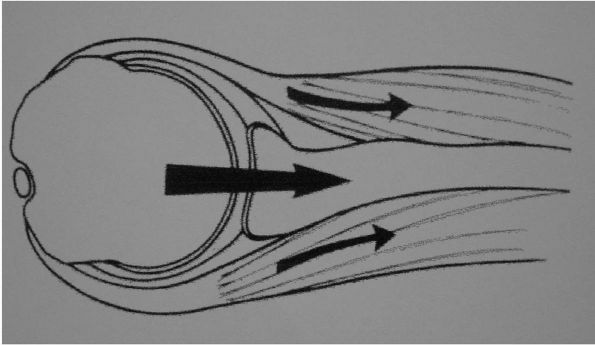
rotator cuff function has emphasized its role as a prime stabilizer of
the humeral head rather than its motor function. The cuff compresses
the joint and provides resistance to sliding and translation during
dynamic activity. In midrange positions of the shoulder when passive
soft tissue restraints are lax, almost all stability is imparted by
cuff function (Figure 12-20).
 |
|
FIGURE 12-20. Illustration depicting the role of the rotator cuff in compressing the head against the glenoid.
|
been proposed as the origin of rotator cuff disease. No one unifying
theory exists addressing their relative contributions to these
conditions.
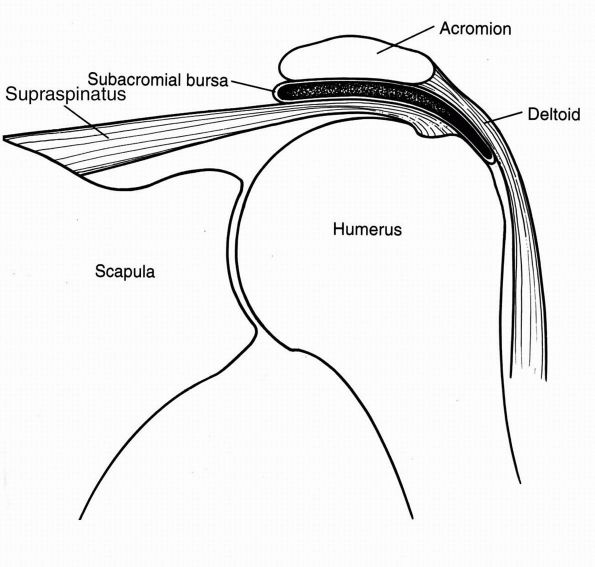
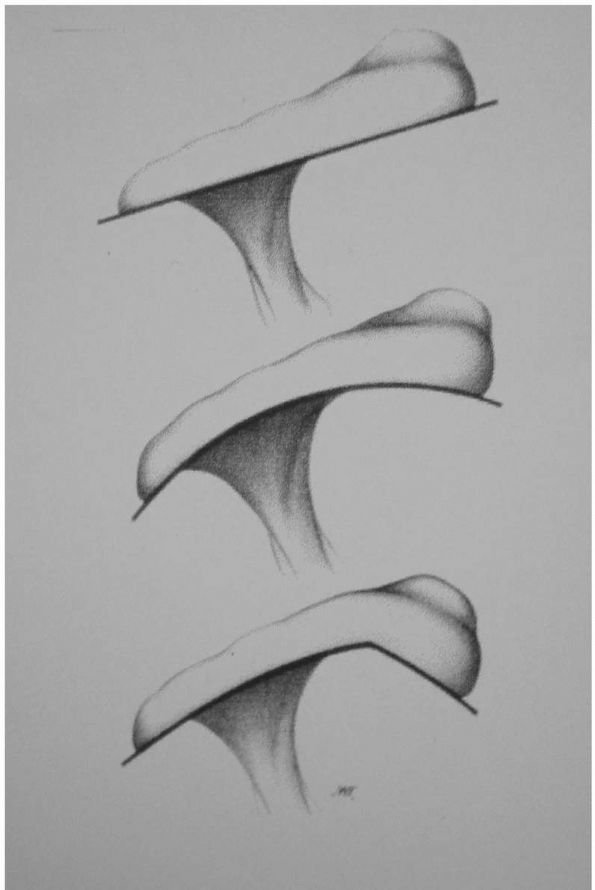
compression of the rotator cuff between the unyielding surfaces of the
humerus and coracoacromial arch, which is composed of the coracoid,
coracoacromial ligament, and the anterior acromion (Figure 12-21). Inherent morphologic variations of the acromion (flat, curved, or hooked) (Figure 12-22)
or age-related acromial spur formation may contribute to the role of
mechanicalbased pathology of the rotator cuff. Biomechanical
analysis
has demonstrated a correlation between a hooked acromion and increased
contact with the underlying cuff. Furthermore, contact of the acromial
undersurface has also been shown to occur predominantly with the
supraspinatus, consistent with the majority of pathology originating in
this location. More recent studies have described the entity of
internal impingement where the articularsided surface of the cuff
repetitively contacts the glenoid rim. Tensile overload and subtle
glenohumeral instability can result in repeated microtrauma in the
overhead throwing athlete in the absence of external, or subacromial,
impingement.
 |
|
FIGURE 12-21. Illustration depicting the normal relationship of the rotator cuff between the humeral head and the acromion.
|
focus of other studies examining the causes of rotator cuff disease.
Higher incidence of articularsided partial-thickness rotator cuff tears
may be partially explained by histologic studies demonstrating
variations in collagen with thinner, less uniform bundles near the
articular surface. Thicker, longitudinally oriented fibers found near
the bursal surface were found to have an ultimate failure stress twice
as high as those found near the articular side. Tenuous vascularity
along the articular surface of the cuff shown in injection studies has
also been suggested as a factor in the pathogenesis of undersurface
partial tears.
be somewhat variable depending on the duration and extent of tendon
involvement. The patient will typically have a history of slowly
escalating pain or pain arising acutely from a single traumatic event.
A dull ache in the anterior and lateral deltoid is typical, often with
radiation down the arm to the elbow. Occasionally, the pain may radiate
into the trapezius and parascapular musculature, but these findings
should alert the examiner to possible cervical spine pathology; an
examination of the neck is essential to rule out other causative or
potentiating sources of shoulder complaints. Symptoms may initially
occur only with vigorous activities such as lifting or sports requiring
motion above shoulder level. A painful arc of motion between 60 and
120° of elevation is present in most patients. Early in the course,
rest and occasional use of anti-inflammatory medication may provide
significant relief. Secondary stiffness can develop from inflammation
and immobility of the shoulder due to pain inhibition, although
stiffness is surprisingly uncommon with full-thickness tears.
Eventually, pain may progress to symptoms at rest or with use of the
extremity for daily activities such as brushing the teeth, combing the
hair, reaching the perineum, unhooking a bra, or even donning a coat.
Pain preventing or interrupting sleep is common, particularly when
rolling onto the affected side.
 |
|
FIGURE 12-22. Illustration depicting flat, curved, and hooked acromial morphologies.
|
assess the status of the rotator cuff. The presence and severity of
certain provocative maneuvers and signs will often aid in determining
the degree of rotator cuff injury.
girdle may be found on visual inspection. Atrophy in the supraspinatus
or infraspinatus fossae may indicate chronic massive tearing of the
associated tendons or compression of the suprascapular nerve. Loss of
the rotator cuff’s compressive function may result in anterosuperior
prominence of the humeral head. Associated proximal rupture of the long
head of the biceps is identified as a painless soft tissue bulge along
the upper arm (Popeye muscle). A discrete fluid-filled mass or swelling
around the shoulder may also become evident with full-thickness tears
as synovial fluid escapes into the subacromial space (fluid sign).
from mechanical impingement from other sources of shoulder pain. The
Neer impingement sign (Figure 12-23) (pain with forced passive forward elevation) and Hawkins sign (Figure 12-24)
(pain with internal rotation and 90 degrees of forward elevation) may
reproduce symptoms. Diminution of pain on repeat testing after
injection of 10 mL of 1% lidocaine into the subacromial space (the
impingement test) is useful not only in verifying the diagnosis as well
as discerning it from other causes of shoulder pain but also in
obtaining a more accurate measure of strength inhibited by pain.
 |
|
FIGURE 12-23.
Neer impingement sign. As one hand stabilizes the scapula, pain is elicited with forced passive elevation of the affected extremity. |
Strength is generally preserved with partial tears but can be falsely
diminished by pain. External rotation lag signs may help differentiate
partial from full-thickness tears; the inability to hold the affected
extremity in external rotation in abduction or at the side is highly
suggestive of a complete tear (Figure 12-26).
The hornblower’s sign, an inability to externally rotate the elevated
arm, is another indication of significant pathology of the posterior
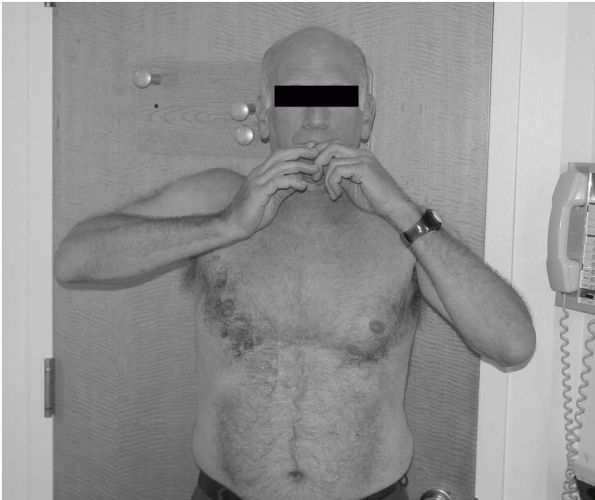
cuff (Figure 12-27). Patients with large cuff tears may also shrug the affected shoulder in an attempt to elevate the arm (Figure 12-28). Tears of the subscapularis are often missed but can be detected by noting a loss of terminal internal
rotation strength, increased passive external rotation as compared to a
normal contralateral side, and inability to perform the belly-press and
Gerber lift-off tests (Figure 12-29).
 |
|
FIGURE 12-24. Hawkins sign. Forward flexion and internal rotation elicits shoulder pain.
|
the plane of the scapula and glenohumeral joint as well as an axillary
lateral. Subtle findings suggestive of rotator cuff pathology such as
an acromial or AC joint spur, cystic changes in the greater tuberosity,
or a sourcil (or eyebrow) sign with sclerosis on the undersurface of
the acromion to unequivocal signs, such as proximal humeral migration,
may be evident on radiographs. Certain specialized views, including the
supraspinatus outlet (Figure 12-30) (10 to 15°
caudal tilt lateral scapular view) and Zanca (10 to 15° cephalic tilt
AP coronal view), may also be obtained to look specifically for outlet
narrowing and AC joint degeneration.
cuff can only be inferred from plain films, additional imaging
modalities are crucial in the evaluation of rotator cuff disease.
Arthrography has been considered the gold standard for diagnosis of
rotator cuff tears. Though highly accurate, it remains an
uncomfortable, invasive test with less utility in determining the size
of full-thickness tears or the presence of partial tears. For these
reasons, it has been largely supplanted by other techniques.
diagnosis of rotator cuff disorders. This noninvasive and relatively
inexpensive technology has been shown to be accurate in detecting and
determining the size of larger full-thickness tears. The problems have
included a high dependence on operator experience and detection of
smaller tears. However, modern equipment and addition of dynamic images
have increased the accuracy.
radiographic diagnosis of rotator cuff pathology. The advantages of MRI
are numerous and include noninvasiveness; capacity to detect
full-thickness, partial-thickness, and intrasubstance tears; and
ability to measure tear size and extent of retraction (Figure 12-31).
In addition, MRI can evaluate other associated abnormal conditions such
as degenerative acromioclavicular or glenohumeral changes, muscle
atrophy and fatty degeneration, capsular and labral pathology, biceps
rupture or dislocation, and ganglion cysts (Figure 12-32).
Through compression of the suprascapular nerve, these ganglion cysts
may produce signs and symptoms mimicking those of a rotator cuff tear.
Experience of the reader and the quality of the equipment limit the
study’s accuracy. Furthermore, long study times and the confined space
in the machine may be intolerable to some patients.
 |
|
FIGURE 12-25. Manual strength testing in (A) external rotation, (B) internal rotation, and (C) forward elevation.
|
 |
|
FIGURE 12-26. External rotation lag sign. (A) The affected extremity is held in external rotation; (B) the patient is unable to actively hold this position due to a full-thickness rotator cuff tear.
|
 |
|
FIGURE 12-27.
Hornblower’s sign. The patient is unable to externally rotate the elevated arm due to a full-thickness rotator cuff tear involving the teres minor. |
 |
|
FIGURE 12-28.
Attempted forward elevation with a large rotator cuff tear. The patient will commonly shrug the shoulder in an effort to compensate for the loss of active elevation. |
 |
|
FIGURE 12-29. Rupture of the subscapularis (left side) with loss of terminal internal rotation. (A) and (B) Gerber lift-off test: a positive test is an inability to hold the affected extremity off the back; (C)
the belly-press test: a positive test is an inability to press the hand in toward the abdomen and keeping the wrist straight. Normally, one performs this maneuver using the subscapularis to internally rotate the arm. With a subscapularis-deficient shoulder, the wrist is flexed to orient the arm and set the posterior deltoid to perform this function. |
 |
|
FIGURE 12-30. Large outlet spur impinging on the subacromial space (white arrow).
|
 |
|
FIGURE 12-31.
Coronal MRI image of a full-thickness rotator cuff tear with retraction half way to the glenoid rim. The white arrow is pointing to the tendon edge. |
full-thickness rotator cuff tears ranging from 7 to 40%. Radiographic
imaging studies of asymptomatic patients have shown that rotator cuff
tears are an age-related phenomenon with a significantly higher
prevalence in individuals older than 60 years of age. Of course, the
tears of clinical significance are those that become symptomatic.
symptoms remain unclear, recent study has suggested that many
asymptomatic tears will become symptomatic as well as demonstrate
progression of tear size (Figure 12-33).
Furthermore, studies have shown that rotator cuff tears do not heal
spontaneously. Over time, irreversible tendon and muscle degeneration
can occur with profound effects on the likelihood of success with
treatment.
 |
|
FIGURE 12-32. Coronal (A) and axial (B) MRI images of a ganglion cyst (white arrows) compressing the suprascapular nerve.
|
 |
|
FIGURE 12-33. (A) Coronal MRI image of a partial-thickness rotator cuff tear (white arrows). (B)
Three years later, MRI of the same patient demonstrating a full-thickness tear of the rotator cuff with retraction of the supraspinatus tendon (white arrow) to the glenoid rim. |
cuff disorders should be based on knowledge of the natural history of
the disease and how a particular intervention may alter its course.
intact cuffs with tendinosis or partial-thickness tears are almost
universally treated with an initial course of nonoperative therapy.
Inflammation is controlled with activity modification, oral
anti-inflammatory medication, judicious use of subacromial
corticosteroid injections, and physical therapy aimed at regaining
motion and strengthening of the rotator cuff and periscapular
musculature. Although studies have suggested that most
partial-thickness tears will continue to enlarge with time, the role of
operative treatment in modifying disease in this stage is unclear.
There is no universal agreement that surgical debridement of a
partially torn cuff relieves pain or stimulates a sufficient healing
response. Furthermore, the permanent changes in tendon and muscle
quality associated with larger, more chronic tears are not present.
Thus, although nonoperative care runs a risk of prolonged pain and
progression to larger tears, irreversible injury due to delayed
surgical intervention is unlikely.
nonoperative treatment in these early stages after a course of
approximately 6 to 12 months. Treatment includes anterior acromioplasty
for impingement lesions and debridement or tear completion and repair
of partial tears. The rationale for removal of the anterior acromial
spur is to eliminate the pathologic compression of the cuff. As
previously mentioned, tear debridement has been met with mixed results.
Tear completion and subsequent repair has been advocated in more
extensive partial tears (more than 50% of the cuff thickness) with
significantly better results reported as compared to debridement alone.
on several factors including severity and duration of symptoms, patient
activity level and goals, and tear size, chronicity, and location.
Although a trial of nonoperative treatment is not unreasonable with
smaller, minimally symptomatic tears or massive, chronic tears with
irreversible tendon and muscle degeneration, anterior acromioplasty and
rotator cuff repair remain the mainstays of treatment for most
symptomatic full-thickness lesions (Figure 12-34).
Results have been shown to be good or excellent in as many as 95% of
patients with preoperative tear size as the primary predictor of
outcome. Pain relief is a reliable goal with less consistent return of
function with larger tear sizes. Some authors have recommended the use
of tendon transfers in the presence of larger, chronic, retracted tears
with associated fatty degeneration and muscle atrophy. Transfers of the
latissimus dorsi or teres major for infraspinatus and supraspinatus
loss and pectoralis major transfer for irreparable subscapularis
ruptures have been described for massive tears and in those who have
undergone a failed primary repair with local tissue.
repair and acromioplasty remains the standard, less invasive techniques
are becoming more widely used. Arthroscopic subacromial decompression
in conjunction with arthroscopically assisted or mini-open repair or
all-arthroscopic rotator cuff repair offer distinct advantages over
traditional methods with indications identical to those for open
techniques. These advantages include smaller incisions, avoidance of
deltoid detachment, shorter hospital stays, and ability to inspect the
glenohumeral joint and treat pathologic entities such as
articular-surface partial cuff tears, labral tears, biceps lesions, and
arthritic lesions of the glenoid and humeral head. These methods are
technically demanding but early results are promising with patient
satisfaction approaching that or equal to formal open procedures (Figure 12-35).
 |
|
FIGURE 12-34. Intraoperative photograph of an open rotator cuff repair with suture fixation of the tendon to bone.
|
the success of all of the surgical treatment options. Early passive
motion is instituted and continued for approximately 6 weeks at which
time patients begin active range-of-motion exercises. Strengthening
exercises are added at about 3 months from surgery and continue until 1
year when the patient can expect maximal improvement.
heads: the short head originating from the coracoid process and the
long head from within the glenohumeral joint, both which combine at the
level of the deltoid insertion to form the muscle proper. As the long
head exits the glenohumeral joint, it traverses through the rotator
interval, a triangular portion of the shoulder capsule between the
supraspinatus and subscapularis tendons, and enters the bicipital
groove of the humerus.
kinematics of the glenohumeral joint has been extensively studied but
not entirely understood. Some authors have proposed that it acts as a
depressor of the humeral head and anterior stabilizer of the
glenohumeral joint. More recent attention has been given to lesions of
the superior labrum at the biceps origin as a source of subtle
glenohumeral joint instability and pain.
rotator cuff, degeneration of the biceps tendon is thought to occur
much in the same way as mechanical
impingement
of the cuff beneath the coracoacromial arch. The role of other factors
such as failure from tensile overload or vascular insufficiency is
unclear although pathologic findings of the distal tendon have been
found with normal segments proximally where mechanical degeneration
would be expected (Figure 12-36).
 |
|
FIGURE 12-35. Arthroscopic rotator cuff repair. (A) Retracted tendon edge (small arrow) and greater tuberosity (large arrow); (B) grasper pulling the tendon laterally to the prepared bone bed on the greater tuberosity; (C) completed repair held with sutures.
|
attention with increasing recognition of this entity using arthroscopy.
The term SLAP lesion (superior labrum anterior and posterior lesions) was introduced by Snyder et al. to characterize injuries of the superior labrum and biceps anchor (Figure 12-37).
These lesions have been postulated to occur in various ways including
sudden deceleration of the flexed elbow in the follow-through stages of
throwing and shearing of the glenoid rim from a fall on the
outstretched hand. Disruption of this complex has been shown to
increase humeral head translation and secondarily compromise important
static restraints to shoulder stability.
 |
|
FIGURE 12-36. Arthroscopic image of humeral head (HH) and fraying (black arrow) of the biceps tendon (Bi).
|
tendinopathy. Anterior shoulder pain at the bicipital groove may be
found while associated cuff disease or glenohumeral instability may
produce a vaguer, diffuse pain. Painful clicks with shoulder motion may
indicate disorders of the labrum and biceps origin.
biceps tendon. Speed’s test is performed by elevation of the extended,
supinated arm against resistance. Yergason’s test may elicit symptoms
by having the patient supinate the forearm against
resistance
with the elbow flexed to 90°. O’Brien’s test (active compression test)
is utilized to isolate SLAP lesion-related pain from other sources. The
shoulder is internally rotated, flexed to 90° and adducted 10 to 15°.
Pain that occurs with resisted elevation in this position and
diminishes with testing in external rotation signifies a positive test.
 |
|
FIGURE 12-37. (A) Arthroscopic image of a SLAP lesion. (B) Arthroscopic repair of a SLAP lesion.
|
long head of the biceps may occur with retraction of the distal segment
through the bicipital groove. The loss amounts to little more than a
cosmetic deformity in the arm (Popeye muscle) and a minimal loss in
supination and elbow flexion strength (Figure 12-38).
In fact, removal of the diseased intra-articular portion of the tendon,
either through spontaneous rupture or surgical resection, generally
results in improvement of pain.
 |
|
FIGURE 12-38. Popeye muscle. (A) and (B) Rupture of the longhead of the biceps (right side) with distal retraction of the muscle belly into the arm.
|
previously mentioned, may be associated with rotator cuff disease or
glenohumeral instability. Initial conservative treatment should address
these underlying disorders in conjunction with alleviating the acute
symptoms. Oral nonsteroidal anti-inflammatory medication and avoidance
of exacerbating activities followed by a physical therapy regimen
emphasizing shoulder and periscapular strengthening may provide relief.
Options for operative care entail debridement, tenotomy, or tenodesis
of the biceps tendon. Tenotomy simply involves transection of the
intra-articular portion of the tendon, either arthroscopically or
during an open procedure for
concomitant
pathology. This approach is particularly attractive for older, lower
demand patients who are willing to accept the resultant deformity and
prefer a faster return to activity, although tenodesis may be
preferable in the younger, more active individual.
suturing the tendon back on itself or to adjacent soft tissue
structures to locking the distal segment into the humeral head using a
bone tunnel and interference screw fixation. The effect of tenotomy on
the purported stabilizing function of the biceps is unknown. Isolated
biceps tendinopathy with no evidence of coexisting shoulder pathology,
such as impingement of glenohumeral instability, is rare. Results of
isolated biceps release (tenotomy) or tenodesis have been mixed
implying that there are various mechanisms of biceps-related pathology.
arthroscopically. Simple fraying of the labrum with a stable biceps
anchor is typically treated with debridement. Detachment of the
superior labrum and biceps origin is best treated with reattachment to
the glenoid rim with bioabsorbable tacks or suture anchors to restore
the stabilizing effect on the glenohumeral joint. Tears of the biceps
tendon extending from the labrum are debrided, but may require repair
or tenodesis if a significant portion of the tendon is torn or
degenerated.
it will be used here, has been broadly applied to a wide range of
disorders that result in a stiff and painful shoulder. Although
attempts in the literature have been made to differentiate these
entities, confusion still exists as to the proper terminology. In terms
of treatment, it may be useful to categorize the stiff and painful
shoulder into conditions that primarily result from pericapsular
scarring and adhesions in contrast to contraction of the glenohumeral
capsule, with extracapsular structures secondarily involved.
by Neviaser based on the observed pathoanatomy. The pathogenesis of
this disease remains unclear with several systemic disorders, such as
diabetes mellitus, cardiovascular disease, mastectomy, or other
operations about the chest and shoulder, found in association with this
form of stiffness. Patients with diabetes mellitus, in particular, are
more prone to bilateral involvement that is extremely resistant to all
forms of treatment.
underlying disorder such as voluntary immobilization from rotator cuff
tendonitis or tear or bicipital tenosynovitis. These forms of secondary
stiffness and pain are often difficult, if not impossible, to
clinically discern from the primary or idiopathic type.
or surgery will typically result in scarring of the extra-articular
tissues and tissue planes. Fractures of the proximal humerus, treated
operatively or nonoperatively, or surgery for instability, for example,
may cause shortening or contracture of the pericapsular tissues and
present with a clinical picture very similar to other etiologies.
usually females between the ages of 40 and 60 years with the
nondominant arm more commonly involved. As mentioned previously,
patients with diabetes mellitus tend toward bilateral involvement.
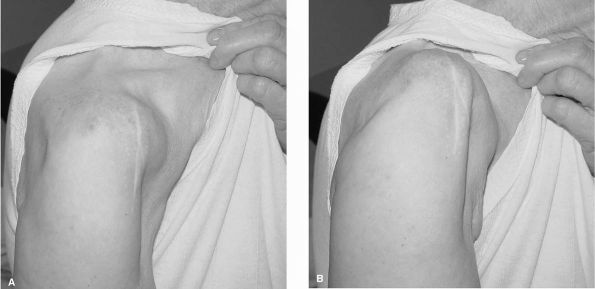
Motion loss must be carefully documented to assess severity and track
progress with both active and passive motion deficits found on
examination. Patients may exhibit compensatory increases in
scapulothoracic motion or trunk lean and should be carefully identified
to accurately measure pure glenohumeral motion loss (Figure 12-39).
disorders or potential etiologic sources. History of systemic disease,
trauma or previous surgery, or a long-standing rotator cuff tear with
pain and normal motion at a prior office visit may provide a likely
cause for the current stiffness. Similarly, in patients with a
noncontributory history, symptom patterns may suggest or mimic other
underlying disorders such as rotator cuff disease, although the
stiffness and associated pain often may mask other clinical findings.
of stiffness. Adhesive capsulitis or capsular stiffness secondary to
other processes typically result in global loss of motion. Postsurgical
or posttraumatic
stiffness
may present with motion loss in all planes or with stiffness in some
planes although sparing other ones. Discriminating between these types
will help guide specific treatment.
helpful in diagnosis or determination of cause in frozen shoulder but
may identify other associated abnormalities such as fracture,
arthritis, metal implants, or neglected dislocations, which may
contribute to the clinical findings.
 |
|
FIGURE 12-39. Passive range-of-motion exam. (A) External rotation at the side; (B) external rotation in abduction; (C) internal rotation in abduction; (D) internal rotation behind the back.
|
diagnosis of adhesive capsulitis with obliteration of the axillary fold
seen with contrast infusion. However, little correlation has been
demonstrated between arthrographic findings and motion loss. In
addition, the invasive nature of the test has decreased its utility.
are suspected. Rotator cuff or labral tears can be readily detected.
Use of MR imaging to define specific pathologic findings consistent
with capsular contracture such as capsular or synovial thickening and
decrease in capsular volume, however, has been inconclusive.
 |
|
FIGURE 12-39. (Continued)
|
described as self-limiting with resolution of symptoms occurring over 1
year. However, most patients are unwilling to endure the discomfort for
this period of time without intervention. The initial management of
most cases of frozen shoulder consists of physical therapy emphasizing
range of motion and gentle stretching every day with the majority of
patients responding to nonoperative treatment (Figure 12-40).
improvement in symptoms over several months of therapy, manipulation
and arthroscopic capsular release should be considered. Traditionally,
manipulation alone with anesthesia has been performed to rupture the
adhesions. The role of arthroscopy as an adjunct to manipulation in the
treatment of frozen shoulder has been recently described. Some authors
have adamantly discouraged its use in the treatment of this disorder
although others have had encouraging results, noting the additional
benefits of being able to release rather than tear the capsule, treat
coexisting pathology, and document the results of manipulation.
Nonetheless, essential to any operative form of intervention is the use
of adequate postoperative analgesia and aggressive therapy. Use of
interscalene brachial plexus block regional anesthesia has been used to
facilitate motion in the immediate postoperative period.
 |
|
FIGURE 12-40. Stretching exercises. (A) External rotation and abduction; (B) forward elevation using a door or (C) against the wall; (D) external rotation at the side; (E) internal rotation with cross-body adduction, (F) behind the back against a counter and (G) with a towel.
|
undergone tendon or fracture repair in the previous 3 to 6 months, or
have suspected or known extra-articular contractures (such as after
previous Putti-Platt or Bristow procedures for instability) should
undergo open release.
and realization that several months may elapse before observing
significant gains in motion.
by the orthopaedic surgeon, particularly in young, active individuals.
Better understanding of glenohumeral joint biomechanics and the role of
various anatomic structures has led to increased recognition and
advances in the treatment of instability.
stability of the shoulder. The balance between stability and permitting
a wide range of motion is provided by the interaction of dynamic and
static factors. The static stabilizers include the glenoid, labrum,
capsule, glenohumeral ligaments, and the rotator interval. The role of
the biceps tendon as a static stabilizer is unclear but is also thought
to contribute to glenohumeral joint stability.
articulate with the humeral head and provides little constraint for the
glenohumeral joint. The fibrocartilaginous labrum attaches to the
glenoid rim and increases its effective depth and surface area.
Isolated labral deficiency has been shown not to allow glenohumeral
dislocation without associated injury to the capsule, emphasizing the
crucial role of the capsuloligamentous structures in maintaining
stability.
“check-reins” toward the extremes of motion while remaining relatively
lax in the midrange to allow normal joint translation. The superior
glenohumeral ligament, coracohumeral ligament, and the rotator interval
(between the leading edge of the supraspinatus and the superior edge of
the subscapularis) restrain anterior humeral head translation in 0° of
abduction and external rotation. With increasing abduction to 45°, the
middle glenohumeral ligament provides the primary anterior restraint.
Finally, the inferior glenohumeral ligament tightens and becomes the
prime anterior stabilizer at 90° of abduction and 90° of external
rotation.
dynamic restraints in normal shoulder biomechanics. A primary role of
the rotator cuff is to resist translational forces on the joint through
compression of the humeral head into the glenoid cavity. Scapular
winging—an imbalance of the scapular stabilizing musculature—has been
implicated in pain and instability of the glenohumeral joint. Operative
intervention addressing scapulothoracic dysfunction may lead to
elimination of symptoms in select cases.
is a careful history and physical examination. The nature of the injury
surrounding the onset of symptoms should be determined and are
particularly useful in identifying the type of instability. Position of
the arm at the time of injury or circumstances that provoke symptoms
often indicates the direction of instability. Reproduction of a
patient’s symptoms in a position of abduction, external rotation, and
extension suggests anterior instability. Flexion, internal rotation,
and adduction, in contrast, would more likely point to posterior
instability. Voluntary control of instability must be carefully sought
out as this may change the ultimate course of treatment. Patients with
psychiatric disorders may utilize a concomitant ability to dislocate
the shoulder for secondary gain. Although operative intervention in
this situation would likely fail, treatment options exist for other
forms of voluntary subluxation. Surgery may benefit patients who can
subluxate the shoulder by placing the arm in provocative positions.
Biofeedback techniques, however, may help those patients who sublux
through selective muscular activation.
should ascertain whether the initial and any subsequent episodes of
instability were elicited by high-energy trauma (such as violent
twisting or fall), minimal repeated trauma (such as throwing a ball),
or no trauma (such as reaching a high shelf). The type of reduction
required (i.e., was the shoulder self-reduced or did it require
manipulation by another person?) may also provide additional
information about the extent of joint laxity.
obtained, including the type and duration of immobilization,
rehabilitative efforts, and previous surgeries. Knowledge of failed
interventions will help guide future treatment in the recurrent
dislocator.
much useful information. Anterior shoulder pain may indicate anterior
instability as well as other common disorders including subacromial
impingement. Similarly, posterior shoulder pain is nonspecific and may
represent a range of pathology from instability to cervical spine
disorders. Location of the pain in combination with provoking arm
positions and activities, however, may aid in making a diagnosis of
instability. Altered glenohumeral kinematics in throwers, for example,
may result in posterior shoulder pain during late cocking (posterior
internal impingement). Patients may also report other symptoms
consistent with subtle shoulder instability. Rowe and Zarins described
a phenomenon termed the “dead-arm syndrome,” in which paralyzing pain
and loss of control of the extremity occurs with abduction and external
rotation of the shoulder.
 |
|
FIGURE 12-41. Posterior glenohumeral dislocation (right side). Clinical photo demonstrating block to external rotation.
|
and activity level is important prior to formulating a therapeutic
plan. The different expectations of a sedentary patient with minimal
functional loss versus the high-performance athlete with pain and
apprehension may affect the type of prescribed treatment.
making an accurate diagnosis and recommending the appropriate
intervention. Both shoulders should be adequately exposed and examined
for deformity, range of motion, strength, and laxity. Unreduced
dislocations may produce an abnormal contour to the shoulder in
addition to restricting active and passive motion (Figure 12-41). Demonstration of scapular winging may accompany
instability, particularly of the posterior type, and should be
considered a potential cause of symptoms. Generalized ligamentous
laxity may also contribute to instability and can be easily elicited
with the thumb-to-forearm and metacarpophalangeal hyperextension tests (Figure 12-42).
Operative reports and evidence of healed anterior or posterior scars
from previous instability repairs indicate what has been done and may
provide a rationale for the patient’s current symptoms. Limitation of
external rotation may accompany a prior anterior tightening procedure
(i.e., Putti-Platt or Magnuson-Stack).
exception of guarding at the extremes as the shoulder approaches
unstable positions. Clinical suspicion should be raised, however, in
the patient older than 40 years of age who is unable to actively abduct
the arm after a primary anterior dislocation. It has been shown that a
high percentage of these patients have a concurrent rupture of the
rotator cuff with restoration of stability following repair.
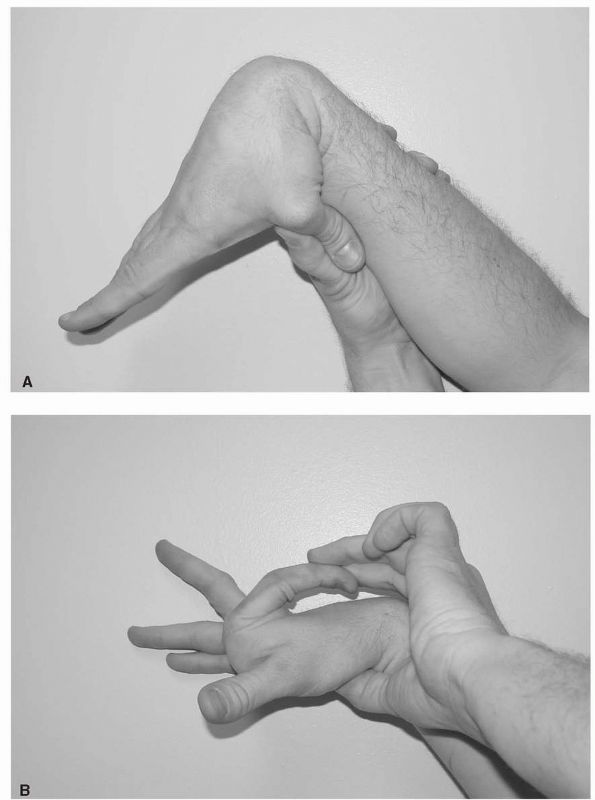 |
|
FIGURE 12-42. Ligamentous laxity. (A) Thumb-to-forearm; (B) metacarpophalangeal hyperextension.
|
the patient’s symptoms and confirm the diagnosis. In order to minimize
the effects of muscle guarding, these maneuvers should be performed
first on the unaffected side and then in succession of increasing
discomfort. The sulcus test evaluates inferior translation of the
humeral head with the arm at the side in neutral and in external
rotation. The scapula is stabilized with one hand while the other
applies a mild compressive force to
the
head in conjunction with a downward force to the arm. Significant
findings would include an increased palpable gap between the acromion
and humeral head compared to the opposite side as well as translation
below the glenoid rim. Performing the test in external rotation will
not reduce the gap when there is incompetence of the rotator interval (Figure 12-43).
posterior drawer or load-and-shift tests. The proximal humerus is
shifted in each direction while grasped between the thumb and index
fingers. Alternatively, with the patient supine, the scapula is
stabilized while the humeral head is axially loaded and translated
anteriorly and posteriorly. Translation greater than the opposite
shoulder or translation over the glenoid rim indicates significant
laxity (Figure 12-44). Only translations that reproduce the patient’s symptoms are considered to demonstrate instability.
externally rotating, abducting, and extending the affected shoulder
while stabilizing the scapula or providing an anteriorly directed force
to the humeral head with the other hand. Significant findings include a
sense of impending subluxation or dislocation, or guarding and
resistance to further rotation secondary to apprehension. Pain as an
isolated finding is nonspecific and may indicate other pathology such
as rotator cuff disease. Jobe’s relocation test is done in the supine
position, usually accompanying the apprehension test. As symptoms are
elicited with progressive external rotation, the examiner applies a
posteriorly directed force to the humeral head. A positive test is
signified by alleviation of symptoms (Figure 12-45).
 |
|
FIGURE 12-43. Sulcus sign. Downward traction of the arm will create a gap between the acromion and the humeral head.
|
stress test. As one hand stabilizes the scapula, a posteriorly directed
axial force is applied to the arm with the shoulder in 90° of flexion,
abduction, and internal rotation. Positive findings produce posterior
subluxation or symptoms of instability experienced by the patient.
elements in patient evaluation, a series of radiographic studies may be
helpful in confirming the diagnosis and defining associated pathology.
AP radiographs in internal and external rotation, a lateral view in the
scapular plane (scapular-Y view), and an axillary view should be
obtained in the initial evaluation. A Hill-Sachs lesion (posterolateral
impression fracture) of the humeral head is best seen on the AP
radiograph in internal rotation (Figure 12-46)
or on specialized views such as the Stryker Notch or West Point
Axillary. Fractures or erosions of the glenoid rim can be detected on
an axillary or apical oblique view (Garth).
obtained in the initial evaluation of instability but may be useful in
a preoperative workup. Computed tomography can assist in further
assessment of fractures and glenoid defects as well as detect subtle
subluxation of the humeral head. MRI and
MR arthrography can identify associated pathology of the labrum, glenohumeral ligaments, and the rotator cuff (Figure 12-47).
More recent radiographic modalities such as dynamic MR-imaging
currently have no defined indications but may become a useful adjunct
in evaluating glenohumeral instability.
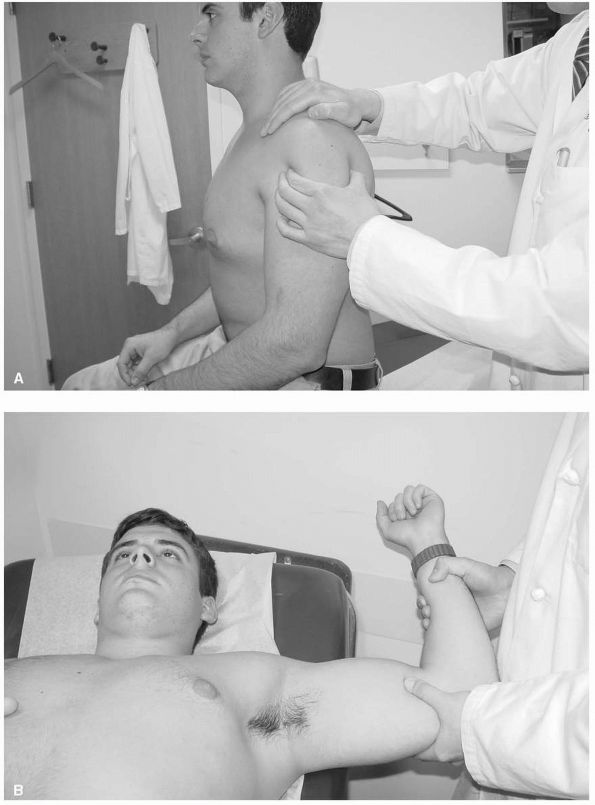 |
|
FIGURE 12-44. (A)
Anterior-posterior drawer: translation of the humeral head held between the thumb and index finger and stabilization of the scapula with the other hand. (B) Load-and-shift: simultaneous axial loading and translation of the humeral head. |
and soft tissue injury, nonoperative treatment consisting of a period
of immobilization followed by rehabilitation is typically successful in
managing the majority of patients with glenohumeral instability. Early
studies of young (less than 20 years old), athletic patients, however,
found a recurrence rate as high as 90% after a primary dislocation.
Although subsequent studies have reported lower numbers, clearly the
risk for subsequent dislocations is higher with earlier onset of
instability.
of debate. Several published series have advocated immobilization for a
few days to several weeks. However, studies by Hovelius and Simonet and Cofield
have found no difference in outcome from either the type or length of
immobilization. In general, younger patients (less than 30 years of
age) sustaining a primary dislocation are preferably immobilized for
approximately 3 to 4 weeks. Older patients, who have a smaller risk of
recurrent instability but a higher susceptibility to stiffness, may be
immobilized for shorter periods.
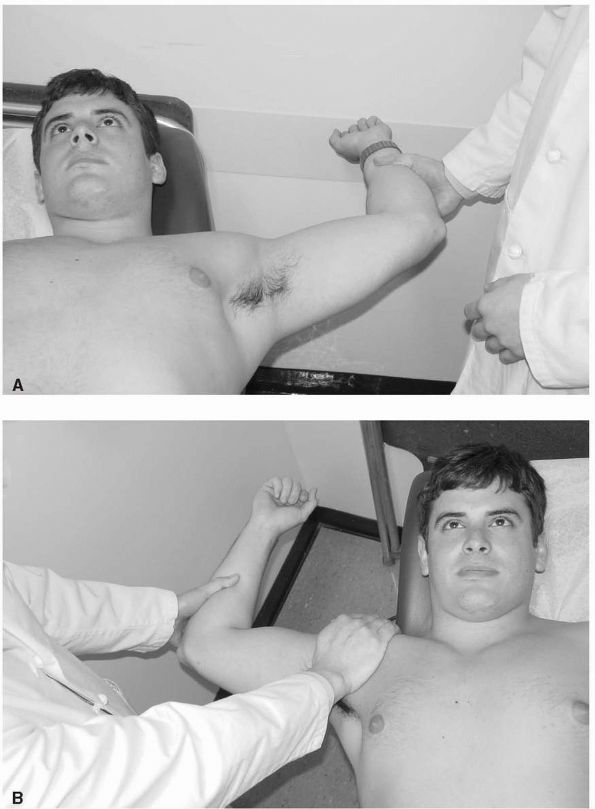 |
|
FIGURE 12-45. (A)
Apprehension test: abduction and external rotation will produce sense of impending subluxation or dislocation with anterior glenohumeral instability; (B) relocation test: posterior-directed force on the humeral head will alleviate symptoms. |
 |
|
FIGURE 12-46.
Hill-Sachs lesion. An impaction fracture of the posterolateral humeral head associated with an anterior glenohumeral dislocation is depicted by the small white arrows on this internally rotated anteroposterior radiograph. |
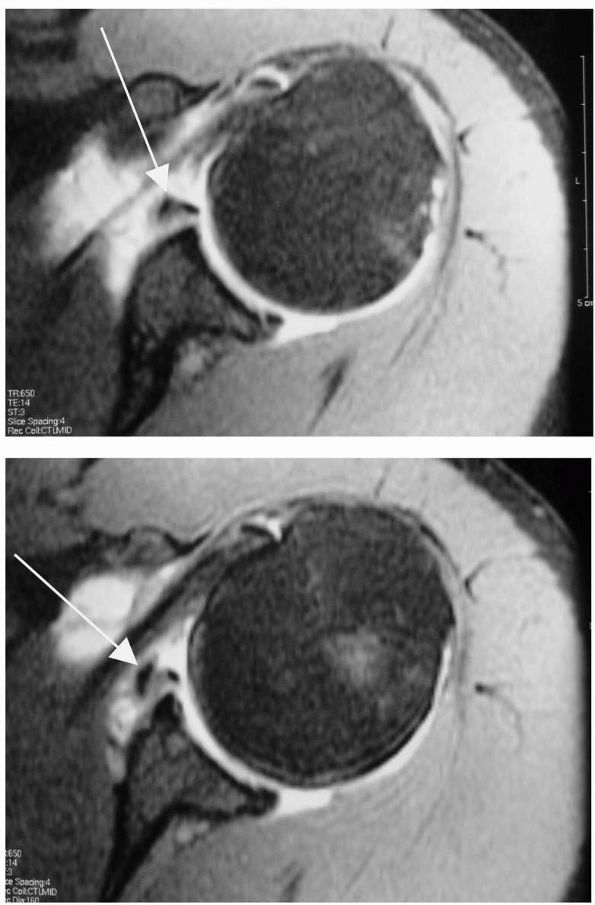 |
|
FIGURE 12-47. (A) and (B) Axial MRI images of a Bankart lesion (white arrows).
|
dynamic stabilizers and regaining motion. Progressive resistive
exercises of the rotator cuff, deltoid, and scapular stabilizers are
recommended. Stress on the static restraints (i.e., capsuloligamentous
structures) should be prevented in the immediate postinjury period by
avoidance of vigorous stretching and provocative arm positions.
instability is an indication for proceeding with operative
intervention. Open procedures are currently the gold standard for
repair of the disrupted soft tissue shoulder stabilizers. Historically,
many of these procedures treated anterior instability through
nonphysiologic shortening or transfer of muscle or bone resulting in
significant loss of motion, postoperative glenohumeral arthritis, and
complications of loose or prominent hardware in the joint.
soft tissue structures. Based on the work of Perthes in 1906, Bankart
in 1923 popularized repair of the capsule to the anterior glenoid
without shortening of the overlying subscapularis. After modifications
to his original description, reconstruction of the avulsed capsule and
labrum to the glenoid lip is commonly referred to today as the Bankart
repair. Several capsulorrhaphy procedures have also been described to
address capsular laxity and the increase in joint volume. These
procedures allow tightening of the anterior capsule in combination with
reattachment of a capsulolabral avulsion.
addresses the capsular laxity seen with this problem. Similar to the
anterior procedure, a posterior capsulorrhaphy functions to reduce
capsular laxity and address associated posterior labral injury.
Difficulty in treatment of multidirectional instability of the shoulder
is, in part, due to improper recognition. Procedures involving anterior
capsular tightening fail to address the inferior and posterior
components of instability seen in this disorder. The inferior capsular
shift procedure, described by Neer and Foster, treats multidirectional
instability by simultaneously reducing volume in the anterior,
posterior, and inferior capsule.
techniques to treat these various problems. Successful outcomes greater
than 80 to 90% can be expected; however, results have been generally
less predictable for posterior and multidirectional instability
compared to anterior instability procedures.
arthroscopic intervention. The goals of restoring the capsulolabral
anatomy and reduction of capsular volume remain the same as in open
procedures. Reduced morbidity from smaller incisions, elimination of
subscapularis detachment, avoidance of scarred and distorted tissue
planes in revision situations, and the ability to simultaneously
address multiple factors contributing to instability have made these
minimally invasive techniques more appealing.
controversial with high (up to 70%) failure rates reported for
transglenoid suture fixation. Improvements in patient selection,
technique, and implant and equipment design have decreased the
recurrence rate. Contraindications to arthroscopic repair include
patients with glenoid bone defects, engaging Hill-Sachs lesions, and
attenuated capsulolabral tissue. Athletes involved in contact sports
have been a relative contraindication, although some surgeons have
modified the exclusion criteria to include this subset of patients.
Improved surgeon technique with bone preparation and soft tissue
tensioning and the use of suture anchors have led to improved results (Figure 12-48).
repairs, in part, due to its easy application. Thermal capsulorrhaphy
may be done alone or to tighten residual capsular laxity following
capsulolabral repair or capsular plication with sutures. Complications
following its use have included neurologic injury to the axillary
nerve, capsular necrosis and loss of capsular and glenohumeral ligament
integrity, and stiffness and loss of motion. Although proponents of
thermal capsulorrhaphy have found this technique a useful adjunct for
treating instability of the shoulder, long-term follow-up studies
advocating its routine use are not yet available. Rehabilitation
following open and arthroscopic instability repairs is identical. The
shoulder is generally protected with 4 to 6 weeks of sling
immobilization in internal rotation for anterior repairs and in slight
abduction and neutral rotation following posterior and multidirectional
instability procedures. Active hand, wrist, and elbow motion is
permitted followed by progressive range of motion exercises. Resistive
exercises are started between 6 to 8 weeks with return to sports at up
to 9 to 12 months postoperatively. Although there are no strict
guidelines, the postoperative therapy regimen must be tailored to each
particular patient accounting for the quality of the tissues, the
durability of the repair, patient reliability, and future demands on
the shoulder.
 |
|
FIGURE 12-48. Arthroscopic images demonstrating (A) an avulsion of the anterior-inferior labrum (Bankart lesion) and (B) suture repair.
|
article estimated an incidence of 0.87 birth injuries to the brachial
plexus per 1,000 live births at a New Zealand hospital. Nearly 80% of
these children had made a complete recovery by the age of 13 months,
although none of those with significant residual defects has severe
sensory or motor deficit of the hand.
H, Tsuyuguchi Y, Masada K et al. Identification of the lesion in
brachial plexus injuries with root avulsion: a comprehensive assessment
by means of preoperative findings, myelography, surgical exploration
and intraoperative electrodiagnosis. Neuro-Orthop 1989;7:15-23. The
authors compared the results of myelography, myelography-CT, and MRI,
with operative findings. They found an 84% truepositive rate, 4%
false-positive rate, and a 12% false-negative rate for myelography.
Results improved with addition of CT. MRI had similar accuracy as
myelography-CT with the additional benefit of allowing more distal
visualization of the plexus.
BJ, Clarke HM, Curtis CG et al. The natural history of obstetrical
brachial plexus palsy. Plast Reconstr Surg 1994; 93:675-681. Sixty-one
of 66 patients (92%) with a brachial plexus palsy recovered
spontaneously and five patients (8%) required primary brachial plexus
exploration and reconstruction (median age 12 months), demonstrating
that most patients do well. Additional analysis was undertaken to
examine ways in which outcome might be predicted. They determined that
when elbow flexion and elbow, wrist, thumb, and finger extension at 3
months were combined into a test score, the proportion of patients
whose recovery was incorrectly predicted was reduced to 5.2% compared
to 12.8% when elbow flexion alone was used.
O, Gossé F, Wirth CJ et al. Reconstructive operations for the paralyzed
shoulder in brachial plexus palsy: concept of treatment. Injury
1999;30:609-618. In this study, 63 patients with
persistent brachial plexus palsy underwent a transfer of the trapezius
muscle and 14 patients underwent a shoulder arthrodesis. In patients
with brachial plexus palsy, trapezius transfer resulted in an
improvement of shoulder function and stability. The increase in
function was, however, less pronounced in comparison with shoulder
arthrodesis. They state that the advantages of muscle transfer are
regaining of normal passive function and the shorter duration of
surgery. However, shoulder fusion is more suitable for those patients
who require the best possible extent of function and strength in the
shoulder.
B, McAllister JW, Manske PR et al. Sever-L’Episcopo transfers in
obstetrical palsy: a retrospective review of twenty cases. J Pediatr
Orthop 1990;10:442-444. The authors
retrospectively studied 25 patients who underwent Sever-L’Episcopo
transfers for obstetrical birth palsy. A follow-up of 2 to 6 years was
possible with a retrospective review of 16 patients. Substantial
improvement in shoulder external rotation as well as subjective
functional improvement was obtained by all patients. Three transient
and one permanent axillary nerve palsies resulting from this procedure
were reported.
author reported osteolysis of the distal part of the clavicle in 46
men, none of whom had a history of acute injury to the
acromioclavicular area. All patients were athletes and 45 lifted
weights as part of their training. Pain and tenderness at the
acromioclavicular joint associated with radiographic signs of
osteoporosis, loss of subchondral bone detail, and cystic changes in
the distal part of the clavicle were present. Resection of the distal
end of the clavicle in 21 patients, 4 with bilateral procedures,
resulted in relief of symptoms in the 19 who were followed. The 25
patients who were not operated on also had improvement, but only after
activity modification with avoidance of weight training.
JC, Ozerkis LR, Helgager JA et al. Arthroscopic subacromial
decompression: results according to the degree of rotator cuff tear.
Arthroscopy 1988;4:241-249. In this article, the
authors describe their technique of arthroscopic distal clavicle
resection from a subacromial (indirect) approach performed in patients
undergoing an arthroscopic subacromial decompression.
EL. The biomechanics of the acromioclavicular, sternoclavicular, and
scapulothoracic joints. Instr Course Lect 1993;42:237-245. The anatomy and biomechanics of the acromioclavicular, sternoclavicular, and scapulothoracic joints are discussed.
EL, Cordasco FA, Bigliani LU. Arthroscopic resection of the outer end
of the clavicle from a superior approach: a critical, quantitative,
radiographic assessment of bone removal. Arthroscopy 1992;8:55-64. The
technique of arthroscopic resection of the outer end of the clavicle
through a superior approach was evaluated to determine whether adequate
bone removal could be achieved. These results were compared with open
resection. The authors determined that satisfactory bone removal was
possible arthroscopically. Comparable pain relief and function were
achieved in both groups. However, hospital stay was shortened and pain
relief was achieved on average 3.4 months earlier in the arthroscopic
group.
K, Craig EV, An KN et al. Biomechanical study of the ligamentous system
of the acromioclavicular joint. J Bone Joint Surg 1986;68A:434-440. The
ligamentous structures of the acromioclavicular joint were studied by
gross examination and quantitative measurement in 12 human cadaver
specimens. Twelve modes of joint displacement were examined. The
acromioclavicular ligament acted as a primary constraint for posterior
displacement of the clavicle and posterior axial rotation. The conoid
ligament played a primary role in constraining anterior and superior
rotation as well as anterior and superior displacement of the clavicle.
The trapezoid ligament contributed less constraint to movement of the
clavicle in both the horizontal and the vertical plane except when the
clavicle moved in axial compression toward the acromion process. The
various contributions of different ligaments to constraint changed not
only with the direction of joint displacement but also with the amount
of loading and displacement.
resection of the distal clavicle was used to treat 26 patients who had
osteoarthritis of the acromioclavicular joint and were followed for a
minimum of 2 years. The preoperative ratings for pain, activities of
daily living, work, and sports improved markedly in 17 patients. The
author concluded that arthroscopic resection was effective in the
treatment of isolated acromioclavicular joint arthritis.
is one of two simultaneous descriptions of distal clavicle excision as
surgical treatment for acromioclavicular dislocation.
BD, Galatz LM, Ramsey ML et al. Nonprosthetic management of grade IV
osteochondral lesions of the glenohumeral joint. J Shoulder Elbow Surg
2002;11:25-32. The authors examined their results
following arthroscopic debridement and capsular release in patients
with limited osteoarthritic changes of the glenohumeral joint. They
concluded that in wellselected patients with grade IV osteochondral
lesions, arthroscopic debridement can provide significant improvements
in pain relief and function. Furthermore, arthroscopic capsular release
can be added in patients with a loss of passive arcs of shoulder
motion. Osteochondral lesions greater than 2 cm2, however, were
associated with failure of this procedure.
WN, Djurasovic M, Glasson JM et al. Hemiarthroplasty for glenohumeral
osteoarthritis: results correlated to degree of glenoid wear. J
Shoulder Elbow Surg 1997;6:449-454. Thirty
patients (31 shoulders) were retrospectively reviewed after
hemiarthroplasty for glenohumeral osteoarthritis. Outcome correlated
most significantly with the status of posterior glenoid wear. They
concluded that hemiarthroplasty can be an effective treatment for both
primary and secondary arthritis but should be reserved for patients
with a concentric glenoid, which affords a better fulcrum for
glenohumeral motion.
authors expand on their earlier experience with shoulder arthroplasty
for arthritis, elaborating on indications, operative findings, and
technique.
TR, Iannotti JP. Functional outcome after shoulder arthroplasty for
primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg
2002;11:130-135. A prospective, multicenter
clinical outcome study evaluated 176 shoulders in 160 patients with
primary osteoarthritis. The authors concluded that total shoulder
arthroplasty and hemiarthroplasty for treatment of primary
osteoarthritis result in good or excellent pain relief, improvement in
function, and patient satisfaction in 95% of cases.
DM, Bucchieri JS, Pollock RG et al. Arthroscopic debridement of the
shoulder for osteoarthritis. Arthroscopy 2000;16:471-476. Twenty-five
patients underwent arthroscopic debridement to treat early glenohumeral
osteoarthritis. The operative procedure consisted of lavage of the
glenohumeral joint, debridement of labral tears and chondral lesions,
loose body removal, and partial synovectomy and subacromial bursectomy.
Overall, results were rated as excellent in 2 patients (8%), good in 19
patients (72%), and unsatisfactory in 5 (20%). The authors found this
as a reasonable procedure for treating early glenohumeral
osteoarthritis that has failed to respond to nonoperative treatment, in
which the humeral head and glenoid remain concentric, and where there
is still a visible joint space on an axillary radiograph. They did not
recommend this technique when there was severe joint incongruity or
large osteophytes.
RL. Steroid-induced avascular necrosis of the head of the humerus:
natural history and management. J Bone Joint Surg 1976;58B:313-317. Ninety-five
patients with steroid-induced avascular necrosis of the humeral head
were followed in this study. Conservative treatment consisted of
pendulum exercises and avoidance of abduction, particularly against
resistance. This led to satisfactory function with only intermittent
symptoms in 14 patients. Five humeral heads in 4 patients required
prosthetic replacement. After 1 to 7 years, the results of all 5 were
classified as excellent in terms of motion and symptoms.
article reviewed 138 patients with sickle cell disease for clinical,
radiological, and functional abnormalities of the shoulder.
Radiographic lesions, frequently bilateral, were found in 28% and only
53% of patients had normal shoulder function.
shoulders treated with prosthetic replacement for osteonecrosis with
average follow-up of 8.9 years were examined in this study. Inferior
functional results were noted in posttraumatic osteonecrosis compared
to those in steroid-induced osteonecrosis. The most common
postoperative complication was rotator cuff tearing, which was more
common in shoulders with a history of any surgery.
DM, Mont MA, Mohan V et al. Osteonecrosis of the humeral head treated
by core decompression. Clin Orthop 1998;355:254-260. Sixty-three
shoulders in 43 patients who underwent a core decompression for humeral
head osteonecrosis were followed up from 2 to 20 years (mean 10 years).
Results of core decompression according to preoperative Ficat and Arlet
stage revealed stage I disease had 15 of 16 (94%) successful outcomes
and stage II had 15 of 17 (88%) successful outcomes. stage III had 16
of 23 (70%) successful results and stage IV had 1 of 7 (14%) successful
result. They concluded that this procedure could be successful for
stages I, II, and III osteonecrosis in terms of early relief of pain
and increased function.
authors discuss the epidemiology of rheumatoid arthritis, the disease
as it affects the shoulder, the differential diagnosis, clinical and
radiographic manifestations, and treatment approaches.
Neer-type total shoulder arthroplasties were performed in 26 patients
with rheumatoid arthritis. The most significant improvement was noted
in pain relief (93% of patients). Follow-up study demonstrated poorer
results for patients with rotator cuff tears.
CJ. Painful shoulders in patients with rheumatoid arthritis:
prevalence, clinical and radiological features. Scand J Rheumatol
1986;15:275-279. The shoulders of 105 patients
with rheumatoid arthritis were examined. Ninety-six patients (91%)
reported shoulder problems with progression of destructive changes and
a decrease in the range of motion with increasing duration of the
disease.
A, Norris TR. Shoulder arthroplasty for advanced glenohumeral arthritis
after anterior instability repair. J Shoulder Elbow Surg
2001;10:539-545. Seventeen of 19 shoulders with
advanced glenohumeral arthritis after anterior instability repair were
treated with arthroplasty. Prior surgeries included four Bristow, four
Putti-Platt (two in combination with other procedures), four
Magnuson-Stack, two Bankart, and five other anterior capsulorrhaphies.
Common findings included severe internal rotation contracture and
posterior glenoid wear. There was improvement in functional use of the
upper extremity in all cases except one.
PB, Hawkins RJ, Fowler PJ et al. Release of the subscapularis for
internal rotation contracture and pain after anterior repair for
recurrent anterior dislocation of the shoulder. J Bone Joint Surg
1992;74A:734-737. Ten patients who had an
internal rotation contracture and pain after an anterior repair for
recurrent dislocation of the shoulder were treated by release of the
subscapularis muscle. Six patients demonstrated severe arthritic
radiographic changes in the shoulder. Following release, each patient
had less pain in the shoulder and an average increase of 27° of
external rotation.
JW, Antuña SA, Sanchez-Sotelo J et al. Shoulder arthroplasty for
arthritis after instability surgery. J Bone Joint Surg 2002;
84A:1775-1781. Thirty-one patients with
glenohumeral arthritis after instability surgery were treated with
shoulder arthroplasty (total shoulder or hemiarthroplasty). The group
was followed for a minimum of 2 years (mean, 7 years) or until the time
of any subsequent revision surgery. Shoulder arthroplasty was
associated with significant pain relief as well as significant
improvement in external rotation and active abduction. However, 3
patients in the hemiarthroplasty group and 8 patients in the total
shoulder arthroplasty group underwent revision surgery. Their data
suggest that shoulder arthroplasty for osteoarthritis following
instability surgery provides pain relief and improved motion but is
associated with high rates of revision surgery and unsatisfactory
results due to component failure, instability, and pain due to glenoid
arthritis.
authors discuss etiology, preoperative evaluation, treatment,
complications, and outcomes of treatment of posttraumatic glenohumeral
arthritis.
JL, Barrett WP, Jackins SE et al. Glenoid loosening in total shoulder
arthroplasty: association with rotator cuff deficiency. J Arthroplasty
1988;3:39-46. Seven cases of total shoulder
arthroplasty exhibiting loosening of the glenoid component were
evaluated to identify causative factors. Six of the patients had
severe, incompletely reconstructable rotator cuff tears present at the
time of surgery, and 1 patient developed a cuff tear within 1 year of
surgery. The amount of superior migration of the humeral component was
closely correlated with the degree of glenoid loosening. Superior
displacement of the humeral component was associated with superior
tipping of the glenoid component (a “rocking horse” glenoid). The
authors concluded that upward riding of the prosthetic humeral head in
patients with rotator cuff deficiency may contribute to loosening of
the glenoid component in total shoulder arthroplasty.
DJ, Halverson PB, Carrera GF et al. “Milwaukee shoulder”—association of
microspheroids containing hydroxyapatite crystals, active collagenase,
and neutral protease with rotator cuff defects. I. Clinical aspects.
Arthritis Rheum 1981; 24:464-473. Four women,
aged 63 to 90 years old, presented with mildly painful shoulders and
decreased mobility or stability. Radiographic evidence of a complete
tear of the rotator cuff was present in 7 of 8 shoulders.
Hydroxyapatite crystals were seen by scanning electron microscopy in 12
of 13 synovial fluid samples. All synovial fluids showed activated
collagenase and neutral protease activity. The authors designated this
constellation of findings as the “Milwaukee shoulder.”
study described the clinical and pathological findings, differential
diagnosis, and pathomechanics of cuff-tear arthropathy in 26 patients.
The authors hypothesized that nutritional and mechanical factors cause
atrophy of the glenohumeral articular cartilage and osteoporosis of the
subchondral bone of the humeral head in a minority of patients with a
massive rotator cuff tear. Their preferred method of treatment was
total shoulder replacement with rotator cuff reconstruction and special
rehabilitation.
J, Cofield RH, Rowland CM. Shoulder hemiarthroplasty for glenohumeral
arthritis associated with severe rotator cuff deficiency. J Bone Joint
Surg 2001;83A: 1814-1822. In this study of 33
shoulders with glenohumeral arthritis and a massive, irreparable
rotator cuff tear, the authors found that hemiarthroplasty provided
marked pain relief in three-quarters of the patients. They cautioned,
however, that outcomes may be complicated by instability and
progressive bone loss.
JE, Thomopoulos S, Flanagan CL et al. Rotator cuff defect healing: a
biomechanical and histologic analysis in an animal model. J Shoulder
Elbow Surg 1998;7:599-605. This study examined
healing of rotator cuff defects in rats. Seventy-eight percent of the
specimens had persistent defects after 12 weeks. There was some
evidence of healing and improved biomechanical properties; however, the
response was inadequate.
GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears
of the rotator cuff. J Bone Joint Surg 1998;80A:832-840. In
this study of arthroscopic repair of full-thickness tears of the
rotator cuff in 73 patients, the authors state the arthroscopic method
offers several advantages, including smaller incisions, access to the
glenohumeral joint for the inspection and treatment of intra-articular
lesions, no need for detachment of the deltoid, and less soft tissue
dissection. They caution, however, that these advantages must be
considered against the technical difficulty of the method, limiting its
application to experienced shoulder surgeons.
JP, Bernot MP, Kuhlman JR et al. Postoperative assessment of shoulder
function: a prospective study of full-thickness rotator cuff tears. J
Shoulder Elbow Surg 1996;5:449-457. Forty
patients underwent surgery for chronic, symptomatic, full-thickness
rotator cuff defects. The study evaluated preoperative and
intraoperative factors that influence postoperative outcome. Outcome
measurements correlated most closely with preoperative tear size.
T, Rokuuma N, Hamada K et al. Histologic and biomechanical
characteristics of the supraspinatus tendon: reference to rotator cuff
tearing. J Shoulder Elbow Surg 1994: 3:79-87. Histologic
studies were performed on clinical rotator cuff specimens to define the
cuff microstructure demonstrating that the articular surface side has
an ultimate failing stress only half that of the bursal side.
SC. Arthroscopic debridement and acromioplasty versus mini-open repair
in the management of significant partial-thickness tears of the rotator
cuff. Orthop Clin North Am 1997;28:79-82. A
comparison between patients with partial-thickness tears treated with
acromioplasty and debridement were compared to patients treated with
mini-open repair. Functional results were significantly better in the
repair group. Healing of the partial-tear was not observed.
DA, Cofield RH. Tenodesis of the long head of the biceps brachii for
chronic bicipital tendinitis: long-term results. J Bone Joint Surg
1989;71A:376-381. The authors studied 54
shoulders at an average follow-up of 13 years treated with isolated
biceps tenodesis of the long head of the biceps. Short-term results
were encouraging with all but 3 patients with satisfactory outcomes.
However, after longer follow-up, a satisfactory result was achieved in
only approximately 50% of patients.
P, Krishnan SG, Coste JS et al. Arthroscopic biceps tenodesis: a new
technique using bioabsorbable interference screw fixation. Arthroscopy
2002;18:1002-1012. Forty-three patients were
treated with the technique of arthroscopic biceps tenodesis using a
bioabsorbable interference screw and followed for at least 1 year.
There was no loss of elbow movement and biceps strength was 90% of the
strength of the other side. The absolute constant score improved from
43 points preoperatively to 79 points at review. Two patients, operated
on early in the series, presented with a rupture of the tenodesis. The
authors concluded that arthroscopic biceps tenodesis using
bioabsorbable screw fixation is technically possible and gives good
clinical results.
EM, Cofield RH, Askew LJ et al. Rupture of the tendon of the long head
of the biceps brachii: surgical versus nonsurgical treatment. Clin
Orthop 1988;228:233-239. In this comparison of
surgical versus nonsurgical treatment of proximal biceps tendon
ruptures, conservatively treated shoulders demonstrated no differences
in arm pain or shoulder range of motion. The authors did find 21% less
supination strength and 8% loss of elbow flexion strength in the
nonoperative group.
authors reported satisfactory results in 16 of 17 patients diagnosed
with isolated biceps pathology treated with biceps tenodesis.
retrospective review described a specific pattern of injury to the
superior labrum of the shoulder identified arthroscopically in 27
patients. Mechanism, clinical picture, classification, and recommended
treatment are described for this entity the authors termed a SLAP
lesion (superior labrum anterior and posterior).
JJP, McMahon PJ. The role of the long head of the biceps brachii in
superior stability of the glenohumeral joint. J Bone Joint Surg
1995;77A:366-372. The authors studied seven
patients who had isolated loss of the proximal attachment of the tendon
of the long head of the biceps brachii, documented operatively or with
magnetic resonance imaging, in order to identify and measure superior
translation of the humeral head on the glenoid. Results showed superior
migration of the humeral head relative to the contralateral (control)
shoulder supporting the role of the tendon of the long head of the
biceps brachii as a stabilizer of the humeral head in the glenoid
during abduction of the shoulder in the scapular plane.
P, Truchon R, St-Pierre A et al. Interscalene block for pain relief
after shoulder surgery: a prospective randomized study. Clin Orthop
1994;304:22-24. This prospective randomized study
of 30 patients who underwent outpatient acromioplasty demonstrated the
efficacy and safety of interscalene block postoperatively.
authors define and differentiate the stiff and painful shoulder from
true adhesive capsulitis and describe their recommended treatment for
these distinct entities.
RG, Duralde XA, Flatow EL et al. The use of arthroscopy in the
treatment of resistant frozen shoulder. Clin Orthop 1994;304:30-36. This
study describes the authors’ technique for managing resistant frozen
shoulder. A treatment regimen consisting of interscalene regional
anesthesia, manipulation, and arthroscopic release, yielded overall
satisfactory results in 25 (83%) of 30 shoulders in their series. The
subgroup with diabetes mellitus fared less well than the other groups,
with only 64% satisfactory results.
review describes the diabetic stiff shoulder, treatment, and outcomes.
The authors detail their surgical technique, which includes
manipulation followed by careful resection of capsule utilizing special
release forceps.
LU, Pollock RG, McIlveen SJ et al. Shift of the posteroinferior aspect
of the capsule for recurrent posterior glenohumeral instability. J Bone
Joint Surg 1995;77A:1011-1020. Thirty-five
shoulders in 34 patients in this study were treated with a superior
shift of the posteroinferior aspect of the capsule because of recurrent
posterior glenohumeral subluxation and dislocation. Overall, the result
for 17 of the 35 shoulders was rated as excellent; 11, as good; 1, as
fair; and 6, as poor. Four shoulders became unstable again. Six of the
7 unsatisfactory results were in shoulders that had had previous
attempts at stabilization.
GM, Roddey TS, Hammerman SM. Arthroscopic treatment of
anterior-inferior glenohumeral instability: two- to five-year
follow-up. J Bone Joint Surg 2000;82A:991-1003. This
study examined 53 patients who underwent arthroscopic treatment of
anterior-inferior glenohumeral instability with soft tissue sutures,
suture anchors, and thermal capsulorrhaphy in select patients.
Ninety-two percent (49) of the 53 patients had a rating of good or
excellent at the time of the final follow-up. Thirty-four of 38
patients returned to their desired level of sports activity following
the operation. The authors concluded that arthroscopic treatment of
anterior-inferior glenohumeral instability is better than previous
arthroscopic techniques and is equivalent to open repair.
L, Augustini BG, Fredin H et al. Primary anterior dislocation of the
shoulder in young patients: a ten-year prospective study. J Bone Joint
Surg 1996;78A:1677-1684. Two hundred and
forty-five patients who had had 247 primary anterior dislocations of
the shoulder were followed for 10 years. The ages of the patients at
the time of the dislocation ranged from 12 to 40 years. The patients
were assigned to one of three various conservative treatment groups. At
the 10-year follow-up evaluation, no additional dislocation had
occurred in 129 shoulders (52%). Recurrent dislocation necessitating
operative treatment had developed in 58 shoulders (23%): 34 (34%) of
the 99 shoulders in patients who were 12 to 22 years old, 16 (28%) of
the 57 shoulders in patients who were 23 to 29 years old, and 8 (9%) of
the 91 shoulders in patients who were 30 to 40 years old. The type and
duration of the initial treatment had no effect on the rate of
recurrence.
review provides an overview of current applications of thermal
capsulorrhaphy for the various types of glenohumeral instability. The
authors emphasize that the use of thermal capsulorrhaphy is to enhance
other arthroscopically-performed stabilization procedures.
shoulders were treated with posterior-inferior capsular shift for
recurrent instability. At follow-up averaging 5 years, 80% satisfactory
results were obtained overall. In cases of primary repair, the success
rate was 96%.
