Posterior Shoulder Instability: Diagnosis and Treatment
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 36 – Posterior Shoulder Instability: Diagnosis
and Treatment
the details of a dislocation in an epileptic is considered the classic
on posterior glenohumeral instability and contains a description of the
characteristic findings of loss of external rotation, an anterior void
with posterior fullness, and a detached subscapularis and reverse
Hill-Sachs lesion confirming the diagnosis on postmortem exam. Cooper
referred to this injury as “an accident which cannot be mistaken.”
Sixteen years later and still 40 years prior to the advent of x-ray
studies, Malgaigne published a report of 37 cases of posterior
dislocation, illustrating that with a thorough physical exam one can
make a proper diagnosis. Despite these early reports of posterior
instability, it remains one of the most commonly misdiagnosed and
mistreated disorders in all of orthopaedics.
includes both dislocation and subluxation and may result from trauma,
repetitive overuse or microtrauma, or without trauma. Traumatic
posterior instability may result from direct forces applied to the
humeral head or proximal shaft, or indirectly by way of a lever arm
and/or muscle imbalances. Repetitive overuse or microtrauma is most
often seen in younger athletic patients who participate in contact or
overhead sports. Atraumatic instability may result from underlying bony
and/or soft tissue abnormalities. Furthermore, it may be
unidirectional, bidirectional with a posterior component, or
multidirectional with a predominantly posterior component.
instability occurs with the shoulder in forward flexion, adduction, and
internal rotation. This position will also reproduce symptoms in
patients with recurrent instability. Axial loading through the humeral
shaft acting as a lever arm, as occurs during a motor vehicle accident,
drives the humeral head posteriorly. In cases of electrical shock or
seizure, violent muscular contraction of the adductors and internal
rotators (latissimus dorsi, pectoralis major, subscapularis, and teres
major) may overwhelm the opposing external rotators (infraspinatus and
teres minor) as well as bony and soft tissue restraints.
atraumatic posterior instability. Bony abnormalities including
excessive retroversion of the glenoid and humeral head, and glenoid
dysplasia and hypoplasia have been implicated in the development of
posterior instability. Ligamentous laxity, posterior or inferior
capsular laxity, or labral dysplasia and aplasia further predispose
patients to subluxation or frank posterior dislocation. Instability may
also occur in the setting of muscular or structural imbalance
exacerbated by certain positions. This may be further complicated by
the presence of a volitional component of the patient to sublux or
dislocate posteriorly.
5%. The incidence may in fact be higher owing to undetected and missed
cases. Posterior dislocations and subluxations are very commonly missed
in the emergency room with a reported incidence as high as 60% to 80%.
This is typically owing to inappropriate radiographs—it is critically
important to obtain 90-degree orthogonal radiographs to avoid this
preventable missed diagnosis.
of cases bilaterally. Recurrent posterior shoulder instability
primarily affects younger men between ages 20 and 30 years who
participate in competitive overhead or contact sports with only about
half of patients reporting a previous initiating injury.
in which the main component is internal rotation and the humeral head
is fixed posteriorly. The lesser tuberosity is located in glenoid, and
the greater tuberosity is no longer seen lateral to humeral head.
Although historically, posterior dislocations were associated with
shock or electroconvulsive therapy, this is now rarely the case.
 |
|
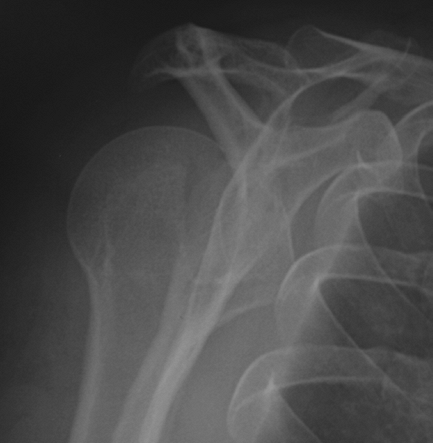
Figure 36-1 Axial computed tomogram of a 28-year-old RHD female with congenital hypoplasia and dislocation of the left shoulder.
|
stabilizers as well as arm position. Contributing factors to static
stabilization include bony, labral, ligamentous, and capsular
contributing factors. Dynamic stabilizers include the rotator cuff and
muscular attachments to the humerus. Variations in the anatomy may
predispose patients to developing instability or may be the result of a
traumatic event or series of events leading to recurrence of
subluxation or dislocation. While a number of specific individual
variations have been implicated in the development or recurrence of
instability, the cause is multifactorial.
7 degrees and varies widely among the population. Although excessive
retroversion of the glenoid, as well the humeral head, have been
implicated as primary causes of posterior instability, they may be more
accurately considered as contributing factors if present. Localized
erosion of the posterior glenoid occurring either primarily or as a
result of repeated events of instability may further contribute to
symptoms of instability. Primary or congenital glenoid
dysplasia/hypoplasia is a very rare disorder characterized by
incomplete ossification of the lower two thirds of the glenoid and
adjacent scapular neck, and may be isolated or associated with other
anomalies such as humeral head flattening or hypoplasia (Fig. 36-1).
Far more common bony abnormalities include engaging defects of the
anterior humeral head and fractures of the posterior rim of the
glenoid, which, depending on size, play a critical role in posterior
instability and require thorough evaluation to determine effective
treatment.
subdividing various types of posterior instability to assist in proper
treatment and outcome determination. To date, however, no single
classification system has been agreed on.
-
Acute: <6 weeks prior to reduction
-
Chronic: >6 weeks prior to reduction
-
Traumatic dislocation/subluxation (dislocation: trauma, convulsions, electrocution; subluxation major and minor trauma)
-
Primary dislocation/primary subluxation
-
Acute
-
Persistent
-
-
Recurrent dislocation/subluxation
-
Posttraumatic
-
Posttraumatic voluntary
-
-
-
Atraumatic dislocation/subluxation
-
Primary dislocation/subluxation
-
Acute
-
Persistent
-
-
Recurrent dislocation/subluxation
-
Atraumatic
-
Atraumatic voluntary
-
Voluntary
-
-
may not indicate a traumatic event. Patients may complain more about
stiffness or functional disability than pain at the time of
evaluation—especially if the evaluation is nonacute (past the first
several weeks following the instability event). There is often a
history of radiographs that have been interpreted as “normal.” Patients
with missed posterior dislocations often are being treated for “frozen
shoulder.” Other important components include a history of seizures (a
posterior fracture-dislocation occurring without trauma is considered
pathognomonic of seizure), diabetes (hypoglycemic seizure), alcohol or
drug use, polytrauma, and psychiatric illness. Inquiry should be made
regarding diseases or illness associated with ligamentous laxity such
as Ehlers-Danlos syndrome. In athletes complaining of shoulder pain, it
is important to ascertain details of their activities and which motions
or positions elicit or aggravate their symptoms. Activities such as
pitching, volleyball, gymnastics, swimming,
golf,
archery, and contact sports place increased physiologic stresses on the
glenohumeral joint that may lead to or exacerbate posterior
instability. Attempts to reproduce symptoms with specific movements and
positions should be made during the exam.
 |
|
Figure 36-2 Clinical photo of patient from Figure 36-1
attempting maximal external rotation of both upper extremities. Notice the fixed internally rotated position of the left shoulder. |
demonstrate difficulty with removal of coat or movements such as
touching one’s head. Attention should be paid to the symmetry and
contour of the shoulders, muscle size and tone, and the appearance of
bony prominences including the acromion, coracoid, and proximal
humerus. Active and passive range of motions should be evaluated with
the patient seated and in supine positions. The classic finding in
fixed posterior dislocation is the inability to externally rotate on
the affected side (Fig. 36-2). All patients
should be evaluated for generalized ligamentous laxity, which includes
the four standard parameters of index finger metacarpophalangeal (MCP)
hyperextension, thumb abduction with palmar-flexed wrist, knee
hyperextension, and elbow hyperextension.
instability who are reduced and/or asymptomatic at the time of exam. A
positive posterior apprehension test elicits pain (and apprehension)
with flexion, adduction, and internal rotation. The anterior and
posterior load and shift test is performed with the patient positioned
supine at the edge of the exam table, shoulder in neutral rotation,
45-degree abduction, and forward flexion. After gently loading the
humeral head with an axial force directed proximally at the elbow,
anteriorly and posteriorly translating forces are applied by directly
grasping and moving the humeral head. This test is graded in the
following manner:
-
+1 = Noticeable translation short of the glenolabral rim
-
+2 = Translation over the glenolabral rim with spontaneous reduction
-
+3 = Translation with complete dislocation requiring manual reduction
therefore requires additional attention to patient responses of pain or
apprehension with testing to properly diagnose posterior instability.
The sulcus test/sulcus sign is performed by placing downward traction
on the neutrally positioned arm and measuring the dimple or sulcus
between the lateral acromion and humeral head. Voluntarism should be
ascertained during the physical examination as it is a negative
prognostic indicator for surgical intervention.
evaluation of the shoulder in all cases should include three views: an
anteroposterior (AP) (preferably performed perpendicular to the
scapular plane), a scapular-Y or outlet view (90 degrees from the true
AP), and an axillary view. Because routine AP and lateral x-ray views
are often inadequate to establish diagnosis, it is imperative that an
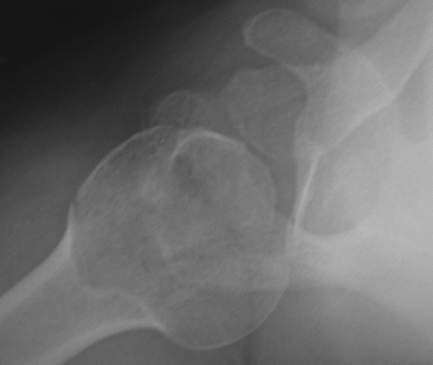
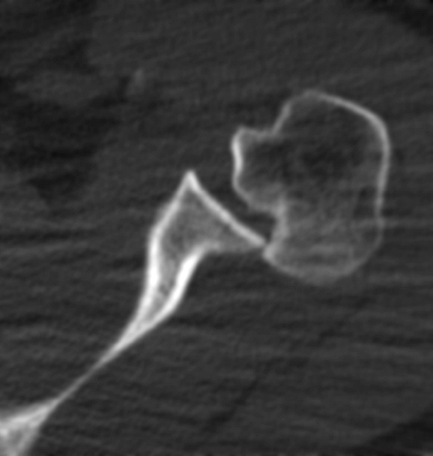
axillary view be obtained to confirm diagnosis (Figs. 36-3, Figs. 36-4 36-5).
 |
|
Figure 36-3 A 47-year-old RHD male with a missed posterior dislocation. True anteroposterior (AP) read by radiologist as “normal.”
|
occurs with the loss of normal humeral overlap on the glenoid. A
distance of >6 mm between the anterior glenoid rim and humeral head
suggests a posterior dislocation. A trough line or compression fracture of the anteromedial humeral head occurs in approximately 75% of posterior dislocations. This reverse Hill-Sachs lesion, often occurring at the time of the original injury, may enlarge with subsequent dislocations. The cystic head sign or light bulb sign
results from the fixed internal rotation of the humerus. On the
scapular-Y view with a posterior dislocation, the humeral head may be
seen posterior to the glenoid. Up to 50% of traumatic posterior
dislocations will have nondisplaced fractures, mostly of the lesser
tuberosity,
owing to avulsion of the subscapularis, and less often of the
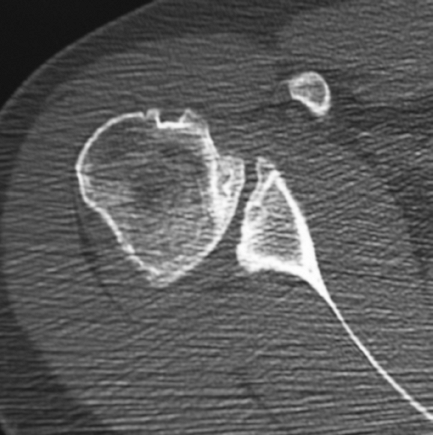
posteroglenoid rim (reverse Bankart). Computed tomography is useful for
further diagnosis and bony evaluation as well as preoperative planning
in the case of bony injury or abnormality requiring surgical
reconstruction (Fig. 36-6).
 |
|
Figure 36-4 Scapular lateral radiograph of patient from Figure 36-3 also read as “normal.”
|
 |
|
Figure 36-5 Axillary radiograph confirming the posterior dislocation in same patient from Figures 36-3 and 36-4.
|
-
Reverse Bankart: Avulsion of posterior glenoid labrum
-
POLPSA lesion: Posterior labral capsular periosteal sleeve avulsion
-
Reverse HAGL: A posterior humeral avulsion of the inferior glenohumeral ligament
-
The Kim lesion: An incomplete and concealed lesion of the posteroinferior labrum
 |
|
Figure 36-6 Axial computed tomogram in a 37-year-old RHD male following a seizure.
|
-
Traumatic, microtraumatic, atraumatic
-
Acute or chronic
-
Voluntary, involuntary; psych history
-
Associated injury, abnormality, illnesses (diabetes mellitus, alcohol abuse, seizure)
-
Previous treatment/therapy
-
Unidirectional, bidirectional, or MDI with posterior instability
-
Subluxation or dislocation
-
Reduced or fixed
-
Is there generalized ligamentous laxity?
-
Positional instability
-
Is there a frank dislocation or subluxation present?
-
Associated fractures/bony abnormalities (x-ray views, CT)
-
Bony reverse Bankart or reverse Hill-Sachs (percent/ size of defect)
-
Other fractures: tuberosity, proximal humerus
-
Glenoid hypoplasia/dysplasia
-
Excessive glenoid retroversion
-
-
Soft tissue injury or abnormality
-
Reverse Bankart (soft tissue)
-
Posterior HAGL
-
POLPSA
-
Kim Lesion
-
Redundant axillary pouch
-
Widened rotator interval
-
in much the same way as anterior dislocations, when recognized acutely.
Following satisfactory muscular relaxation and pain control, with the
patient in the supine position, longitudinal and lateral traction
should be applied with gentle internal rotation followed by external
rotation to disimpact the head and stretch and then relax the posterior
capsule. Another method of disimpaction is to flex the arm to 90
degrees and gently adduct. Pressure is then applied directly to the
posterior humeral head anteriorly to complete the reduction.
avoid creating fractures if the head is locked. Following reduction, a
sling in neutral to external rotation may be used for immobilization;
however, if there is concern for recurrent instability, a gunslinger
type brace or spica cast should be applied. The recommended position of
immobilization to optimize stability and healing of the posterior
labrum and capsule is abduction, external rotation, and extension for a
period of 4 weeks.
impaction defect or the injury is more than 6 weeks old (chronic,
“locked”). Other indications for surgery in the acute setting include
displaced tuberosity or glenoid fracture requiring reduction, or an
open injury. A deltopectoral approach is made and is usually all that
is necessary in most patients. A separate posterior incision is rarely
required to facilitate reduction.
repaired using subchondral elevation with bone grafting if the injury
is <2 weeks old. Small defects >2 weeks old may be filled using
transfer of the subscapularis (McLaughlin) or the lesser tuberosity
(Neer); however these are nonanatomic repairs that risk rotator cuff
weakness or dysfunction and can complicate future procedures. Larger
defects ≤40% to 50% can be filled with structural allograft. Repairs
should be assessed intraoperatively for stability, addressing injuries
to the labrum, capsule, rotator cuff, or glenoid if necessary. In the
case of defects >50% of the humeral head or presence of significant
osteoarthritis, a hemiarthroplasty should be performed. Total shoulder
arthroplasty is a surgical option for an older patient with significant
glenoid articular wear. Postoperatively the patient should be
immobilized in neutral rotation for 6 weeks before initiation of
therapy except in cases of simple arthroplasty, which can begin gentle
passive motion immediately.
patient with a fixed dislocation. This is recommended in cases of
prolonged dislocation, particularly in the elderly or low functional
individuals or in cases of only minor disability.
results are to be expected with increasing duration of dislocation,
increasing size of a humeral head defect, increasing degree of
deformity or arthritis, and the presence of concomitant injury.
Complications include recurrence of dislocation, osteoarthritis
secondary to trauma or abnormal joint forces from reconstruction,
osteonecrosis, and loss of motion.
the complex and multifactorial nature of recurrent posterior
instability. In almost all cases, treatment of posterior instability
begins with nonoperative measures unless symptoms of pain or
dysfunction are present to a degree that warrants more immediate
surgery. Surgery must be tailored to address each specific underlying
component of instability. Physical therapy should include rotational
and scapular strengthening with an emphasis on external rotation
strengthening (particularly the infraspinatus) while avoiding
impingement, voluntary episodes of instability, or positions that may
result in subluxation while restoring normal shoulder motion and
strength. Attention should also be given to muscular imbalances,
weakness, or disturbances of normal coordinated motion. In general,
nonoperative measures should be used for a minimum of 3 to 6 months
before considering the patient a candidate for surgery, although in
certain cases or causes of instability such as injury where
nonoperative treatment has been shown to be less effective, the
decision to proceed with surgery sooner is warranted.
instability owing to an underlying psychologic problem that is better
addressed with psychotherapy, biofeedback, and muscle retraining.
Patients with a poorly controlled seizure disorder require strict
medical management. Patients with ligamentous hyperlaxity also
represent a treatment challenge that is best addressed with extensive
nonoperative management.
determine the degree and direction of instability and identify all bony
and soft tissue abnormalities. Various procedures are available that
address bony and soft tissue abnormalities and can be performed with
either open or arthroscopic technique. Although more technically
demanding, arthroscopic procedures have the advantage of reduced
hospital stay, less postoperative pain, and improved cosmesis.
congenital posterior dislocation, glenoid hypoplasia, and posterior
bony defects. A posterior deltoid-splitting approach obviates the need
for any tendon detachment and exposes the interval between the
infraspinatus and teres minor, which is itself split, exposing the
posterior capsule. A horizontal or T-shaped capsulotomy exposes the
posterior glenohumeral
joint.
An allograft bone block is secured with two screws to the posterior
scapular neck at midlevel, projecting extracapsularly past the glenoid
margin. Bone blocks are more often used in secondary procedures when
primary soft tissue procedures have failed (Figs. 36-7, 36-8, 36-9).
 |
|
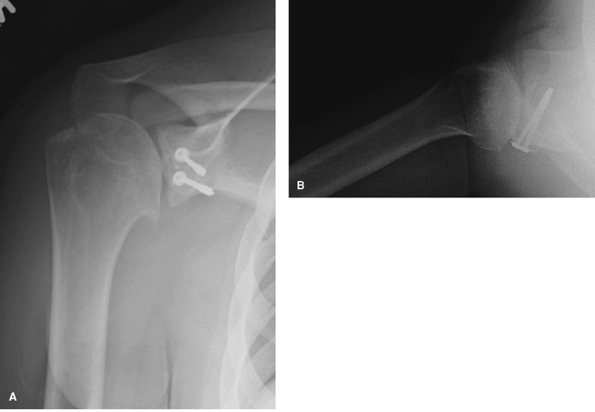
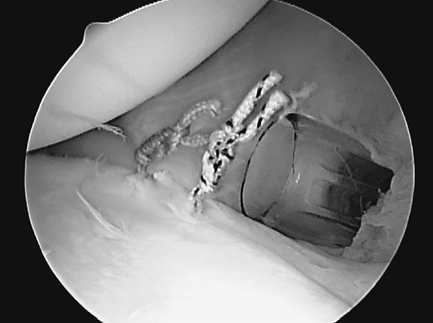
Figure 36-7
This is an axial CT scan demonstrating significant posterior glenoid bone deficiency, mild posterior subluxation, and early degenerative joint disease (DJD) in a 23-year-old RHD male who previously underwent an arthroscopic posterior labral repair, which has failed. |
 |
|
Figure 36-8
Intraoperative view of a posterior deltoid-splitting approach to the glenohumeral joint in the 23-year-old RHD male who previously underwent an arthroscopic posterior labral repair that had failed (same patient as in Fig. 36-7). |
opening wedge osteotomy of the scapular neck or glenoid plasty can be
used. This was originally performed using a posteroinferior acromion
wedge of bone to fill the defect without the use of hardware for
fixation. Results of this procedure have been mixed, partly because of
the technically demanding nature and high complication rate, which
includes glenoid articular fracture, nonunion, loss of graft position,
osteonecrosis, degenerative arthritis, and resultant impingement.
approach has been used in patients with unidirectional, bidirectional
(posterior and inferior), and multidirectional instability with a
predominantly posterior component with good to excellent results
regardless of direction or cause. Using a 60-degree oblique incision,
the deltoid is split in a posterolateral raphe extending down no
greater than 5 cm (to protect the axillary nerve) from the
posterolateral corner of the acromion, and detached medially up to 4 cm
for improved exposure. The infraspinatus is separated from the
supraspinatus and teres minor and carefully elevated off the underlying
capsule from medial to the glenoid rim out laterally to its humeral
insertion. The infraspinatus is then incised either obliquely creating
two tendon flaps or vertically, if the tendon is attenuated, leaving a
1-cm stump on the greater tuberosity. The capsule is incised 1 cm
medial to its humeral insertion, leaving a cuff parallel to the
anatomic neck with nonabsorbable mobilizing sutures placed along the
free medial edge. With increasing degrees of capsular laxity, a larger
extent of inferior dissection, capsular incision, and shifting of
inferior tissue superiorly should be performed. This is performed by
making a horizontal capsular incision (T-fashion split), creating flaps
inferiorly and superiorly. The superior flap is reattached to the cuff
on the humerus shifting it inferiorly and then reinforced with
attachment of the inferior flap shifting it superiorly and obliterating
the inferior pouch. The infraspinatus is repaired placing the lateral
portion deep to the medial portion, adding further reinforcement.
Postoperatively the patient is immobilized for 4 to 6 weeks in neutral
rotation with slight abduction prior to initiating therapy.
open technique may be performed through a posterior deltoid-splitting
approach with development of the interval between the infraspinatus and
teres minor, and a vertical capsular incision to expose the joint.
Suture anchor labral repair is then performed.
 |
|
Figure 36-9 Postoperative true anteroposterior (AP) radiograph (A) and axillary (B) showing bone graft fixed with two screws and washers (same patient as in Figs. 36-7 and 36-8).
|
and are well suited for addressing the anatomy of the capsulolabral
complex of the glenohumeral joint. Arthroscopic procedures are well
developed for the repair of pathology specific to posterior instability
and include reverse Bankart repair, capsular plication, and rotator
interval closure, when indicated. Concurrent pathology such as rotator
cuff tears, impingement, and SLAP lesions can be addressed at the same
time. Regional or general anesthesia is used with patients in the
lateral decubitus position and the arm in lateral traction.
through a standard anterosuperior portal. Dual posterior portals
provide access to the posterior inferior labrum, which can be repaired
with suture anchors. The bone beneath the labrum should be decorticated
to provide a bleeding bed, and anchors should be placed into the
glenoid rim rather than the neck. The size of the lesion dictates the
number of anchors necessary to provide secure fixation and restoration
of the labral “bumper” (Figs. 36-10 and 36-11).
 |
|
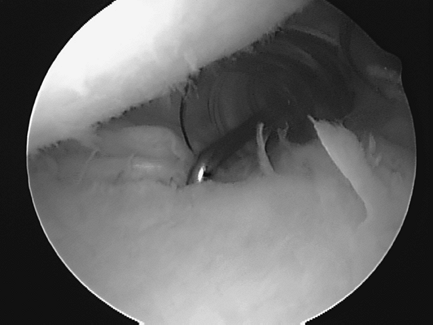
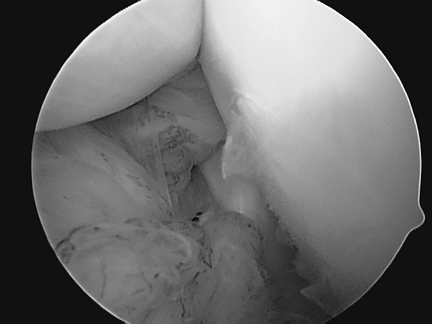
Figure 36-10
20 year-old RHD elite hockey player with right shoulder traumatic posterior labral tear. Anterosuperior viewing portal shows a posterior labral tear from 7 to 11 o’clock (probe is in tear at the 9 o’clock position). |
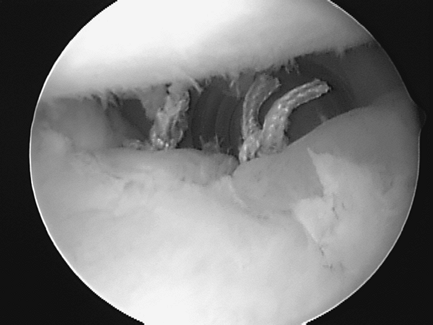
capsular plication using curved, corkscrew suture passers or crescent
hooks after first abrading the capsule with a nonaggressive shaver.
Nonabsorbable braided sutures are used, and capsular tissue is gathered
toward the glenoid labrum (Figs. 36-12 and 36-13).
Alternatively, if the posterior labrum is deficient or the capsular
plication suture is felt to be pulling the labrum away from the
glenoid, a suture anchor should be used for the plication.
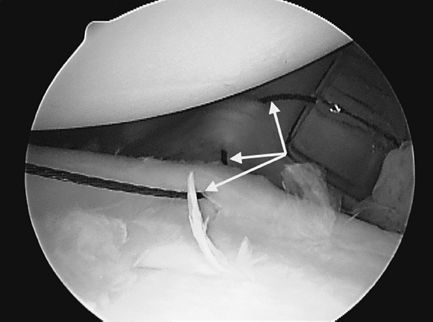
of the capsule of that region with a rasp or shaver to elicit a
bleeding response. Using a spinal needle, a braided suture is passed 1
cm medial to the humeral insertion of the supraspinatus, anterior to
its anterior edge
(superior
portion of the interval). A penetrating suture grasper is passed
through the anterior portal, positioned just outside of the joint
capsule, through capsule deep to the subscapularis (anterior portion),
and grasps the suture pulling it outside of the joint. A suture hook or
curved grasper is used to retrieve the superior suture into the portal,
and a sliding knot is tied in the cannula closing the interval (Fig. 36-14).
 |
|
Figure 36-11 Anterosuperior viewing portal showing completed labral repair from 7 o’clock to 11 o’clock in same patient as in Figure 36-10.
|
 |
|
Figure 36-12 Anterosuperior viewing portal in a 15-year-old RHD female with multidirectional/posterior instability. The arrows point to a nitinol wire as it passes through the posteroinferior capsule into the intact labrum.
|
 |
|
Figure 36-13 Anterosuperior viewing portal showing completed posterior capsular plication (same patient as in Fig. 36-12).
|
 |
|
Figure 36-14
Rotator interval closure viewed from a posterior arthroscopic portal in a 17-year-old RHD female with multidirectional instability with posterior symptoms. |
arthroscopic repairs and stabilization procedures should begin with
sling/brace immobilization with the arm in abduction and neutral to
slight external rotation worn for 3 to 6 weeks full time depending on
the type of repair and reliability of the patient. Gentle passive range
of motion exercises can begin at 3 to 6 weeks followed by gradual
strengthening with an emphasis on external rotation.
recurrence of instability, level of function and ability to perform
activities of daily living (ADLs), return to previous activity, return
to sport, pain, and general patient satisfaction. Scoring systems used
to standardize and measure outcomes include the American Society of
Shoulder and Elbow Surgeons (ASES) score, the simple shoulder test
(SST), Rowe score, UCLA score, L’Insalata score, visual analog score,
and SF-36 score.
mechanics of shoulder instability, improved diagnostic imaging, and
arthroscopic techniques tailored toward specific pathology, tremendous
strides have been made in the management of posterior instability.
FA 3rd, Titelman RM, Lippitt SB, et al. Glenohumeral instability. In:
Rockwood CA Jr, Matsen FA 3rd, Wirth MA, et al., eds. The Shoulder. Vol 2. 3rd ed. Philadelphia: WB Saunders; 2004:655–794.
