Leg Length Inequality
problem encountered in children. The treatment is complicated by the
need to consider the growth of the limb and estimate discrepancies at
skeletal maturity.
shortening or absence of the femur, fibula or tibia, hemihypertrophy,
hemiatrophy, and skeletal dysplasias. The congenital causes may have
associated anomalies that complicate management (i.e., foot
abnormalities with fibular hemimelia; knee anomalies with tibial
dysplasias). Other etiologies include Ollier disease, multiple
hereditary exostoses, developmental dysplasia of the hip, clubfoot,
Blount’s disease, Legg-Calvé-Perthes disease (LCP), and slipped capital
femoral epiphysis (SCFE).
|
TABLE 8-1 ETIOLOGY OF LEG LENGTH INEQUALITY
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
irradiation, tumors, and mechanical causes. Trauma may cause direct
shortening, overgrowth, or growth-plate injuries. Infections and tumors
may retard or stimulate growth.
appropriate interventions may be planned. In addition, hemihypertrophy
and hemiatrophy are associated with Wilms tumor and hepatic neoplasms,
necessitating screening ultrasounds of the abdomen and pelvis
throughout childhood.
careful clinical and radiographic evaluation over extended periods of
time. Clinical assessment requires gross inspection of the discrepancy,
as well as evaluation for other anomalies including
angular
deformities, joint contractures, joint instability, spine deformities,
and vascular malformations. Gait must be assessed and compensatory
mechanisms considered. Children are quite adept at compensating for leg
length discrepancies. Compensation mechanisms include toe-walking on
the shorter limb, flexing the hip or thigh of the longer limb, and
circumducting or vaulting over the longer limb.
|
TABLE 8-2 RADIOGRAPHIC METHODS OF ASSESSMENT OF LEG LENGTH INEQUALITY
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
(measured from anterosuperior iliac spine to the tip of the medial
malleolus) and apparent leg length (measured from umbilicus to the tip
of the medial malleolus). Blocks are used to measure leg length
discrepancy by placing incrementally larger blocks under the shorter
limb until the pelvis is level.
 |
|
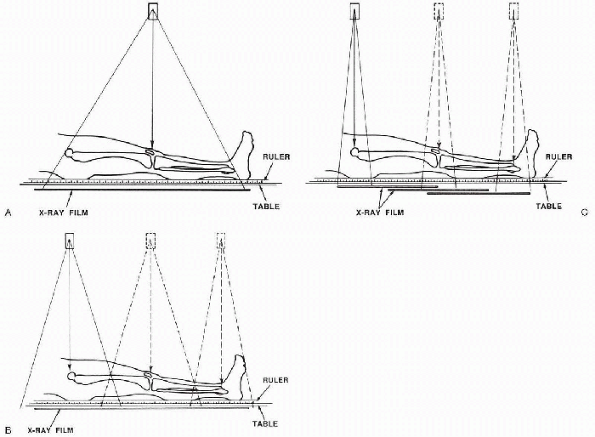
Figure 8-1 (A)
Diagram of teleroentgenogram technique. This technique shows angular deformity but is subject to errors of magnification. It is probably the best technique for children who cannot reliably comply with instructions to remain still for multiple exposures. (B) Diagram of orthoroentgenograph technique. This technique exposes each joint individually, ensuring that the beam through each joint is perpendicular to the x-ray film, thereby avoiding errors of magnification. (C) Diagram of scanogram technique. This technique avoids magnification error in the same manner as does the orthoroentgenograph and is the preferred technique for children who cannot remain still for three exposures. (From Mosley CF. Leg length discrepancy. In: Morrissey RT, Weinsten SL, eds. Lovell and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1106-1150.) |
is a single exposure of both legs on a long film with a ruler. Its
advantages include visualization of angular deformities and the
requirement of only a single exposure
(making
it easier to obtain in small children who have difficulty remaining
still during the procedure). However, the single exposure introduces a
magnification error that decreases the accuracy.
is similar to the teleoradiograph but it uses three separate exposures
over the hips, knees, and ankles on one long film with a ruler. This
results in less magnification error, but requires a cooperative patient.
acquired by moving the radiographic tube and the film for the three
exposures. This again diminishes magnification error and results in
smaller, more manageable films, but does require the patient to be
cooperative and still. It also does not allow for assessment of overall
limb alignment. A flexion contracture may diminish its accuracy.
 |
|
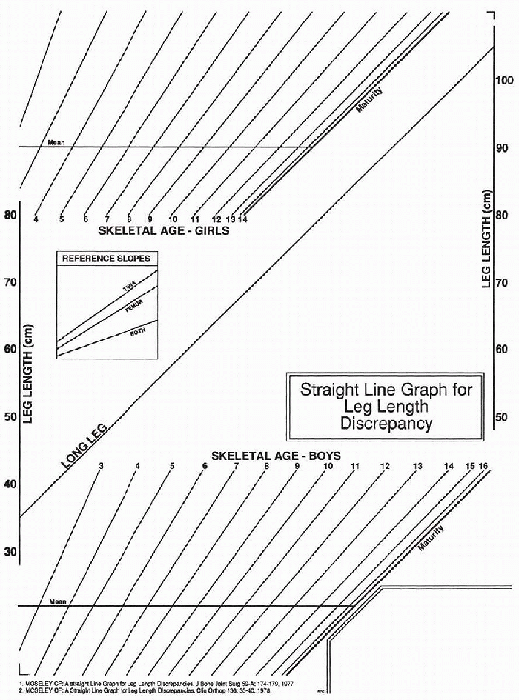
Figure 8-2
The straight-line graph consists of three parts: the leg-length area with the predefined line for the growth of the long leg, areas of sloping lines for the plotting of skeletal ages, and reference slopes to predict growth after epiphysiodesis. (From Mosley CF. Leg length discrepancy. In: Morrissey RT, Weinstein SL, eds. Lovell and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1106-1150.) |
measuring leg length discrepancy. They use decreased radiation and are
less sensitive to errors secondary to positioning or contractures and
measurements in the lateral plane can be obtained. They also visualize
the entire limb, allowing for assessment of other deformities.
length discrepancy. It is more popular in Europe, and a primary reason
for its popularity is that it does not use ionizing radiation.
several assumptions. The first is that boys grow until age 16 and girls
until age 14. The second is that the distal femur contributes 3/8-inch
per year to growth and the proximal tibia contributes ¼-inch per year.
The third is that the discrepancy increases by 1/8-inch year. These
assumptions allow for mathematical calculations of growth and
estimation of timing for epiphysiodesis (surgical closure of the growth
plates).
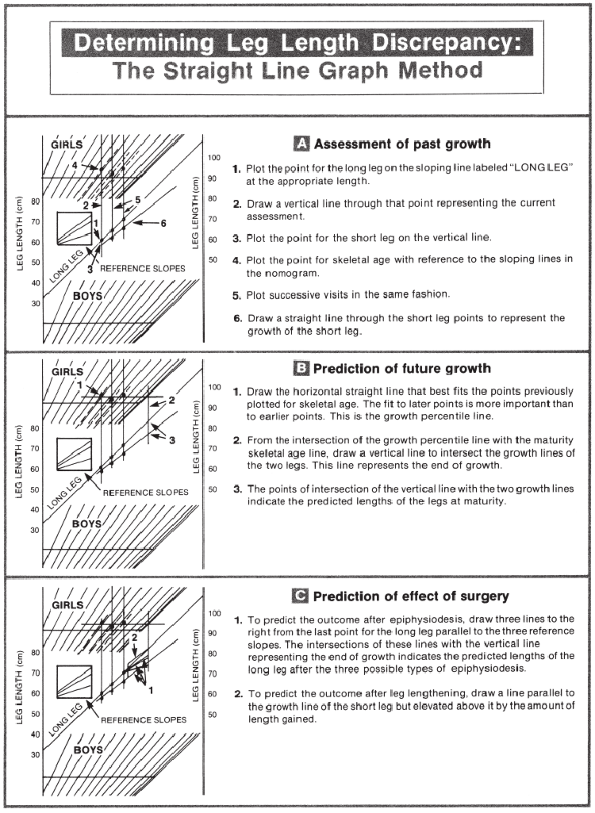
predicts future growth based on skeletal age rather than chronologic
age. Graphs are used to determine growth percentile of the child,
future growth of the long leg, and the effects of epiphysiodesis.
Information required for these calculations includes the length of the
limbs, skeletal age, chronologic age, and percent of growth inhibition.
The Moseley graph relies on the assumptions that the growth of legs can
be represented graphically by straight lines and that the leg length
discrepancy is the vertical difference between the two lines. The
percentage of inhibition of growth is the difference between the slopes
of the two lines, with the slope of the normal leg equal to 100%. A leg
that is lengthened is represented by a straight line of the same slope
displaced upward by the amount lengthened. After epiphysiodesis, the
straight line will have a decrease in slope equal to the percent
contribution that the growth plate would have made, with the proximal
tibia contributing 28% and the distal femur contributing 37% (Fig. 8-3).
This method enables better prediction of the effects of surgery,
enabling timing to be planned. It is the most commonly used method, and
there are now computer programs available to perform the calculations.
Observation is the best treatment for small discrepancies under 2 cm.
Most of these patients do well with a lift, although some adolescents
and teenagers will reject this. The parents should be reassured that,
in general, small discrepancies do not cause significant spine or hip
problems. A lift up to 1/2-inch can be fit inside the shoe, making it
more cosmetically pleasing for the patient.
treatment may consist of epiphysiodesis or shortening of the long side.
With an epiphysiodesis, the growth charts must be consulted and the
patient evaluated at least 3 times at 6-month intervals. The growth
charts can assist in the determination of where and when the procedure
is to be done. For example, a larger discrepancy may require a distal
femoral and proximal tibial epiphysiodesis at 1 to 2 years before the
end of growth, while a smaller discrepancy may need only a proximal
tibial ablation in the last year of growth. The surgery itself is not
overly challenging but the timing is crucial. Poor timing may result in
a persistent limb length inequality. Because the procedure is
irreversible, the surgical decision must be made carefully. Overall
growth and stature of the patient and the patient’s parents must be
given consideration. For example, a child with small stature may not
want a shortening procedure, whereas a tall child may be more accepting
of this. A short child with tall parents may have more growth potential
than realized. Again, one is faced with shortening the overall stature
and operating on the normal, longer, lower extremity.
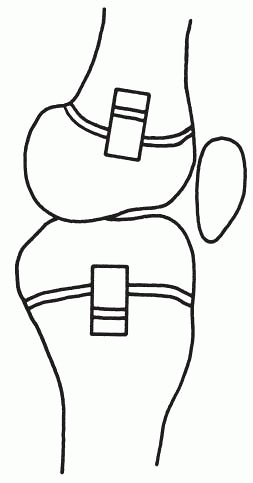
closed method on the long side. The open method involves cutting a
piece of bone out from each side of the growth plate, turning it, and
reinserting in a manner to produce a bony bridge (Fig. 8-4).
A postoperative cast is required for about 6 weeks. The closed or
percutaneous method is done under the C-arm using a small incision with
a drill or burr being inserted to ablate the growth plate. Both medial
and lateral sides must be ablated or an angular deformity may result.
The epiphyseal plate is undulating rather than horizontal in contour so
care must be taken to burr its entirety. A knee immobilizer is used
postoperatively for about 4 weeks and partial weightbearing is allowed.
Serial outpatient radiographs are taken to follow the closure of the
growth plate.
epiphysiodesis due to age and cessation of growth, a femoral or tibial
shortening may be performed. This may also be done in either a closed
or open method. In the open technique, a midshaft approach is made to
either the femur or tibia, the desired amount of bone is removed, and
the ends are brought together and held with a plate and screws. The
closed technique is more technically demanding, requiring
intramedullary reaming, cutting, and rodding for stability. However,
the patient has less morbidity and a smaller scar. Surgical shortening
of greater than 2 inches may result in clumping of the soft tissues,
giving a bulky appearance and possibly weakness of the underlying
muscles due to the shortening.
procedure should not be made lightly. The patient and family must be
carefully evaluated as to whether this is the best procedure for them
and are they prepared, physically and psychologically, to deal with the
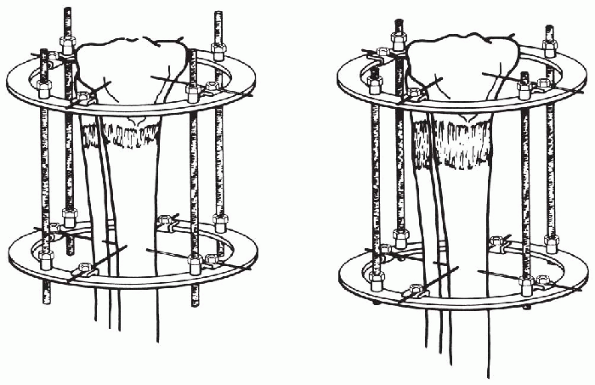
long and involved procedure. The general principle consists of making
an osteotomy in the bone to be lengthened, stabilizing it with an
external frame, and then gradually distracting the two ends of ends of
the bone to allow the bone to lengthen as it heals (Fig. 8-5).
Each lengthening takes about 1 year to complete, with 6 months in the
frame, and 6 months consolidating in an orthosis. The patient and
family must be
able
to perform the distractions, pin care, and therapy. Complication almost
always arise and include pin site infections, broken wires, loss of
range of motion, fractures, angulation, lack of consolidation, and
pain. A careful clinical, psychological, and social evaluation of the
patient and family prior to planning and scheduling this type of
procedure is performed. Potential complications and treatment are
outlined to the family.
 |
|
Figure 8-3
Step-by-step instructions for using the straight-line graph in determining remaining growth. Data used are an example. (From Mosley CF. Leg length discrepancy. In: Morrissey RT, Weinsten SL, eds. Lovell and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1106-1150.) |
|
TABLE 8-3 TREATMENT OF LEG LENGTH INEQUALITY
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 8-4
Epiphysiodesis by the Phemister method. A rectangular bone block is replaced in reversed position to produce a bar across the growth plate. (From Mosley CF. Leg length discrepancy. In: Morrissey RT, Weinsten SL, eds. Lovell and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1106-1150.) |
 |
|
Figure 8-5
Metaphyseal lengthening. Elongation through the metaphysis promotes osteogenesis in the lengthening gap because metaphyseal bone is so active, and it promotes strength by the large cross-sectional area. (From Mosley CF. Leg length discrepancy. In: Morrissey RT, Weinsten SL, eds. Lovell and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1106-1150.) |
lengthening surgical techniques in detail. However, the basic
principles are outlined in Box 8-1. Once the
decision has been made to lengthen the extremity, there are several
techniques available. One may use either a circumferential frame such
as an Ilizarov device or a unilateral lengthener. Each one will yield
the same type of results. The circumferential frame provides more
stability and allows angular correction concurrently with the
lengthening. The unilateral device may also provide angular correction,
although in many cases not as much. It may be easier to apply to the
femur since one does not have to deal with pins and rings extending
medially. An advantage of the circular frame is that it can be
constructed in a manner to provide both
compression and distraction if needed (i.e., in a short limb with a pseudarthrosis).
-
Evaluate length discrepancy
-
Patient/family evaluation and education
-
Proper pin placement; frame stability
-
Maintain joint mobility
-
Corticotomy vs. osteotomy
-
Latency period (for edema), then distract
-
Four-times-a-day distractions
-
Compress—for pseudarthrosis, poor regenerate bone
-
Physical therapy, pin care, pain control
equal distractions, which will result in an inch of growth per month.
This can be slowed if there is poor callous/regenerate bone formation.
In cases of persistent poor regeneration, one can alternately compress
and lengthen to stimulate the new bone formation. Distractions should
be held for the first 5 to 7 days postoperatively to allow the edema to
decrease. At that point, the periosteal new bone formation commences.
The osteotomy should be atraumatic to preserve the periosteum and its
function. A corticotomy has been recommended by various authors to help
preserve the osseous intramedullary circulation. Others have
recommended cutting with a Gigli saw.
pain management are important adjuncts to treatment. Range of motion of
the joints above and below the lengthening are crucial and lengthening
may have to be slowed or stopped temporarily if range is significantly
lost. Orthotics attached to the frame enhance joint position and
prevent loss of motion. Pin care is taught to the patient and family to
avoid pin tract infections. Many pins develop drainage which is not a
true infection; however, with significant drainage or purulence I
prescribe oral antibiotics. Pin care is done with simple soap and water
cleansing and salinesoaked sponges. Pain control is dealt with on a
team approach at our hospital. Various techniques are used including
oral medications, transdermal analgesic patches, and diversion
techniques. A combination of these techniques generally results in
adequate pain control.
consolidation period. This is generally 2 to 3 months after the
cessation of lengthening. The patient is placed in an orthosis after
removal for about 6 months, until the regenerate bone appears mature.
During this period the patient works on range of motion and
strengthening. Full weightbearing is allowed and encouraged. This whole
process may be repeated after a few years for larger discrepancies,
when there is adequate osseous healing.
-
Infection—pin tract
-
Neurovascular injury
-
Joint subluxation/dislocation
-
Joint contracture—loss of range of motion
-
Fracture
-
Delayed union/nonunion
-
Pain
-
Skin compression from fixator
-
Psychosocial issues
-
Inability to obtain desired length
pediatric orthopaedist. An understanding of the condition and the
ability to predict ultimate discrepancy enables one to formulate a
treatment plan. The treatment must be suited to the patient and the
family. Treatment may include shoe lift, epiphysiodesis, shortening, or
lengthening. A team approach and well-informed and involved family
result in the best outcome.
CF. Leg length discrepancy. In: Morrissey RT, Weinsten SL, eds. Lovell
and Winter’s pediatric orthopaedics, 5th ed. Philadelphia: Lippincott
Williams & Wilkins, 2001:1106-1150.
