Prepatellar Bursitis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Prepatellar Bursitis
Prepatellar Bursitis
John J. Carbone MD
John H. Wilckens MD
Description
-
Prepatellar bursitis is an inflammation of the bursa in front of the patella.
-
Bursae are located between structures to reduce friction.
-
These sacs are lined with a membranous
synovium that produces and absorbs fluid; they are subject to acute or
chronic trauma or infection and to low-grade inflammatory conditions
such as gout, syphilis, tuberculosis, and rheumatoid arthritis (1).
-
-
Classification:
-
Traumatic
-
Septic
-
Inflammatory
-
-
Synonyms: Housemaid knee; Carpenter knee; Carpet-layer knee
Epidemiology
-
Particularly common in middle and old age
-
Occurs equally in males and females
Incidence
Common
Risk Factors
Occupations that create repetitive pressure and trauma to the anterior aspect of the knee
Genetics
No known Mendelian pattern
Etiology
-
Acute injury such as from a fall or motor vehicle accident (2)
-
Repetitive minor trauma (2)
Signs and Symptoms
-
Pain, worse with motion of and pressure over the knee
-
Erythema
-
Obvious swelling over the anterior patella (Fig. 1)
Physical Exam
-
Examine the knee carefully and compare the affected with the contralateral side.
-
Check for joint effusion.
-
Palpate the quadriceps and patellar tendons and check for knee extension with the knee flexed 90°.
-
Palpate the patella for tenderness.
-
Check for erythema and local warmth.
Tests
Lab
-
Routine tests:
-
Complete blood cell count
-
ESR
-
-
If the bursa is aspirated:
-
Culture
-
Cell count
-
Gram stain
-
Crystal analysis
-
Imaging
AP and lateral radiographs to rule out an intra-articular or bony process
Pathological Findings
Usually, Gram-positive organisms (Staphylococcus aureus) (3)
Differential Diagnosis
-
Intra-articular disorders of a similar nature:
-
Sepsis
-
Low-grade inflammatory process
-
Trauma
-
-
Cellulitis
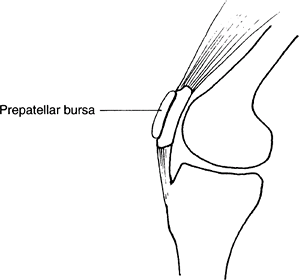 Fig. 1. Prepatellar bursitis produces swelling in the bursa directly over the kneecap.
Fig. 1. Prepatellar bursitis produces swelling in the bursa directly over the kneecap.
General Measures
-
Immobilize the joint in extension (knee immobilizer).
-
Treat traumatic and inflammatory bursitis symptomatically with NSAIDs.
-
Aspirate the bursa if a septic process is suspected.
-
Traumatic injuries often heal spontaneously with:
-
Immobilization
-
NSAIDs
-
Heat or ice for symptomatic relief
-
-
Septic injuries:
-
Immobilize the joint.
-
Aspirate the bursa to identify the infectious organism.
-
Administer parenteral antibiotics.
-
Begin with empiric gram-positive coverage while awaiting culture and sensitivity results.
-
-
Perform incision and drainage of bursa if no improvement occurs in 36–48 hours.
Special Therapy
Physical Therapy
Therapy is given as needed to regain ROM lost as a result of immobilization and to restore quadriceps strength.
Medication
-
NSAIDs (traumatic injuries)
-
Parenteral antibiotics (septic injuries)
Surgery
-
Indicated for fibrosis or synovial thickening with painful nodules that fails to respond to medical treatment
-
Indicated for septic prepatellar bursitis that does not respond to antibiotics
P.347
Disposition
Issues for Referral
Ascending lymphangitis requires hospitalization and intravenous antibiotics.
Prognosis
Most patients do well with immobilization and NSAIDs.
Complications
Infection and chronic drainage may occur after repeated aspirations.
References
1. Dlabach
JA. Nontraumatic soft tissue disorders. In: Canale ST, ed. Campbell’s
Operative Orthopaedics, 10th ed. St. Louis: Mosby, 2003:885–904.
JA. Nontraumatic soft tissue disorders. In: Canale ST, ed. Campbell’s
Operative Orthopaedics, 10th ed. St. Louis: Mosby, 2003:885–904.
2. Safran MR, Fu FH. Uncommon causes of knee pain in the athlete. Orthop Clin North Am 1995;26: 547–559.
3. McAfee JH, Smith DL. Olecranon and prepatellar bursitis. Diagnosis and treatment. West J Med 1988;149:607–610.
Codes
ICD9-CM
726.65 Prepatellar bursitis
Patient Teaching
-
Patients are instructed to avoid provocative activities such as prolonged kneeling.
-
Protective coverings over the knee are helpful for patients with occupational exposures.
FAQ
Q: How can you differentiate bursal swelling and knee joint effusion?
A:
Prepatellar bursitis has swelling on top of the patella, making it
difficult to palpate the patella. With even a large knee joint
effusion, the patella is palpated easily and is ballottable; direct
pressure on the patella makes it “bob” on the effusion.
Prepatellar bursitis has swelling on top of the patella, making it
difficult to palpate the patella. With even a large knee joint
effusion, the patella is palpated easily and is ballottable; direct
pressure on the patella makes it “bob” on the effusion.
Q: How can you tell if a prepatellar bursitis is septic?
A:
The bursa is fluctuant with overlying cellulitis, and it usually is
more painful than traumatic or inflammatory bursitis. Definitive
diagnosis is made with aspiration of the bursa and analysis of the
fluid.
The bursa is fluctuant with overlying cellulitis, and it usually is
more painful than traumatic or inflammatory bursitis. Definitive
diagnosis is made with aspiration of the bursa and analysis of the
fluid.
