Staying Out of Trouble while Caring for the Injured Child
|
|
The outcome from the injuries is primarily related to the severity and
management of the head and musculoskeletal injuries.1
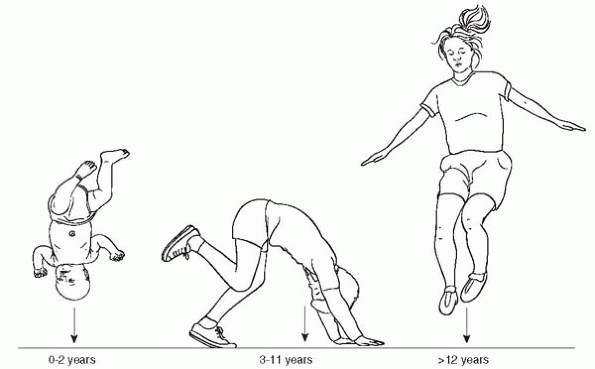
To stay out of trouble treating injured children, it is important to
understand the different mechanism of injuries in children and how they
can result in different constellations of injuries. A classic example
is the fact that children who fall from heights have age-related injury
patterns2 (Fig. 4-1).
Although historically many children’s fractures have been treated with
closed management alone, specific periarticular injuries and physeal
injuries are especially appropriate for internal fixation. Likewise,
the value of mobilizing injured children is increasingly being
appreciated. Recognize that certain injuries are sentinels for other
types of injuries. Examples of this include rib fractures, pelvic
fractures, facial injuries, and a lap belt sign (Fig. 4-2) on the anterior aspect of the abdomen or chest.
 |
|
▪ FIGURE 4-1
Mechanism of injury is a key component of the history and physical exam. For instance, the constellation of injury after a fall from a significant height varies based on the age of the child. Infants have large heads and are not able to right themselves—they often fall head first. School-aged children are able to partially right themselves, so they get combined extremity injuries, but fewer head injuries. Older teens usually land feet-first, sustaining foot, ankle, tibia and femoral injury. (Reprinted with permission: Sawyer JR, Flynn JM, Dormans JP, et al. Fracture patterns in children and young adults who fall from significant heights. J Pediatr Orthop. 2000;20-2:197-202.) |
children results from the family’s perspective and expectations. When
they arrive with their injured child, the family may be overwhelmed and
shocked by the traumatic event. The relationship with the healthcare
team is quickly established. As the surgeon, you may find yourself cast
in one of two lights: part of the problem or part of the solution. Some
families quickly look for someone to blame for the calamity, and if
there is no one outside the hospital, they look for someone inside the
hospital— and who better than the surgeon, the captain of the ship. The
surgeon becomes solely responsible for “making it all like it was
before the accident” and anything different is grounds for a
malpractice suit. To stay out of trouble, use those first few minutes
with the family to establish the optimal relationship: a partnership,
you and the family against the injuries. It is fair for you to describe
the extent of the problem in graphic detail, the outcome if untreated,
the prolonged length of recovery (yes, many children do limp for a year
or more after a serious lower extremity injury) and the numerous
complications that have been described in the literature. Although they
can expect your best effort, they must understand the things you can’t
control. In a multi-trauma situation, explain that it is common to
discover some injuries in the days and weeks that follow1. Discuss findings again immediately after any surgery, and reinforce recovery, complications and hurdles
you and the parents may encounter in the months to come. The more
untrusting the family, the more you should see them, both inpatient and
outpatient. After many weekly clinic visits, such families often thank
you, rather than complain about the hassle of such close followup.
 |
|
▪ FIGURE 4-2 The lapbelt sign is a classic sentinel injury. When this skin finding is present, a lumbar spine injury should be sought.
|
that make a child’s injury unique, and may alter treatment. Ligaments
may attach to the epiphysis. Because the ligaments are stronger than
the physis, a force to such a joint leads to physeal injury rather than
ligamentous disruption. It is easy to forget about plastic deformation
as an injury pattern in children. Such plastic deformation can lead to
loss of motion or deformity, such as in a diaphyseal forearm fracture,
or make reduction of an associate fracture difficult, such as in a Type
III Monteggia fracture.
 |
|
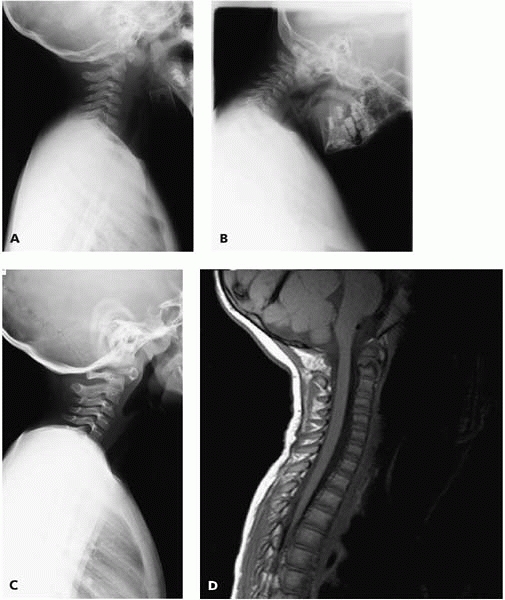
▪ FIGURE 4-3
Increasingly over the past decade, MRI has become an important tool to avoid trouble when caring for a child with a possible occult cervical spine injury. MRI is particularly valuable to clear the cervical spine of a child who cannot cooperate with voluntary flexion and extension radiographs. This image allowed the diagnosis of ligamentous disruption at the occipitocervical junction (red arrow). |
victims are head injury and intraabdominal hemorrhage. One of the most
important ways to stay out of trouble as an orthopaedist caring for
severely injured children is establishing a good relationship with your
general surgeon and your neurosurgeon. Children have a smaller blood
volume and become hypovolemic quite quickly. This is particularly
problematic in femur fractures associated with splenic injury or other
internal bleeding. Because of their amazing ability to compensate with
an increased pulse, children may not show a drop in blood pressure due
to hypovolemia until they are in a very critical range. Blood loss is
easily underestimated because most pediatric trauma is blunt and the
bleeding is internal. Partnering with a general surgeon and a
neurosurgeon, and using a careful physical exam with liberal use of
imaging (Fig. 4-3), are valuable ways to optimally collaborate care when there are both skeletal injuries and multiple internal injuries.
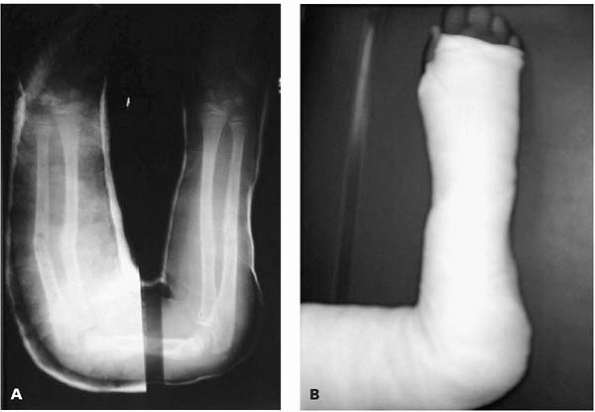
high-energy trauma. The most common areas are the forearm and tibia, or
an open fracture of the foot and ankle when the foot is run over by a
car or school bus (Fig. 4-4). As in adults, the
wound should be inspected once in the Emergency Department (ED),
classified, and covered with Betadine gauze. Repeated evaluation of
these wounds can lead to increased blood loss and the risk of
nosocomial infections. Antibiotics and tetanus should also be given
upon arrival in the ED. Studies in both the adult and
pediatric
trauma literature have found no reduction in infection rates for open
fractures that make it to the operating room within 8 hours, as long as
appropriate antibiotics are given upon arrival in the ED.3
Although there may be other reasons to rush an open fracture to the
Emergency Room, such as a neurovascular injury, soft-tissue injury, or
severe contamination, many clean open fractures in children can have
their operative debridement within 24 hours with no increased risk of
infection. Because of the better microvascular supply, soft-tissue
injuries seem to recover much better in children. To stay out of
trouble, leave questionably damaged tissue at the first debridement and
reassess at a second operation. In many cases more extensive
soft-tissue coverage can be avoided if the surgeon is conservative in
the initial debridement.
 |
|
▪ FIGURE 4-4
Most open fractures in children are grade 1 open injuries to the forearm or leg. Unfortunately, open ankle and foot injuries are also common in urban areas when young feet are under moving car tires. |
syndrome. To stay out of trouble, don’t ignore the signs of acute
compartment syndrome thinking that “a fasciotomy has been done by the
injury.” Compartment syndrome creates lots of trouble in children
because its diagnosis is more difficult. It can be harder to
differentiate normal trauma pain from abnormal compartment pain in
children. Children may be slow to complain of increasing pain. An
increased narcotic requirement may be the only sign of compartment
syndrome in some children.4 Another
source of trouble with compartment syndrome is hesitation to stick the
compartments due to the pain and anxiety children experience with
standard compartment measurement. If at all in doubt, use conscious
sedation or even compartment syndrome measurement in the operating
room. Finally, be alert that compartment syndrome may be quite delayed
in children. Although the reason for this delay is not clear, the first
diagnosis is often 20-40 hours after fracture.5
Even when a compartment syndrome is diagnosed this late in children,
often the results are good, with lower risk of devitalized muscle and
other complications seen in adults.
that a child can recover from severe multi-trauma, particularly head
and spinal cord injury. The orthopaedist may be reluctant to operate on
a child with severe closed head injury given the fact that fracture
alignment seems to be the least of the child’s problems. The
inexperienced orthopaedist may expect that the child’s chance of
survival is low and allow the injuries to go untreated. The same
surgeon may then have to face this child’s malunion in his office 6
weeks later, when the child presents accompanied by his physical
therapist and parents. The 72-hour Glasgow coma score motor response is
the best predictor of permanent disability after head injury. Operative
stabilization may be necessary if spasticity develops in the days
following head injury. Because the healing rates are faster with head
injury, the decision for stabilization should be made early.
Emergency departments that accept children for care should have
pediatricians or emergency room doctors with the training and
experience necessary to safely administer narcotics, sedatives, and
anesthetics, as well as do the monitoring afterwards. The orthopaedist
should be able to work with these other experts to keep the child
comfortable during orthopaedic evaluations and procedures. Nitrous
oxide is sometimes used, typically as a self-administered sedative.
Children usually have to be older than 4 years old in order to do the
self administration. Unfortunately, pain relief is not very good with
nitrous oxide. If nitrous oxide is the only agent available, consider
supplementing this with a hematoma block if appropriate.
fractures. To stay out of trouble, counsel the parents at your first
discussion with them about the risk of growth arrest. Current
statistics indicate that the risk of growth arrest is about 25% to 30%
in the distal femur and distal tibia, about 60% for the distal ulna and
about 4% for the distal radius. Physeal fractures tend to heal more
quickly than metaphyseal and diaphyseal fractures. Therefore, the
window for remanipulation of a physeal fracture is quite short. Most
authorities agree that a physeal fracture should not be subject to
manipulative reduction more than 3-5 days after injury.
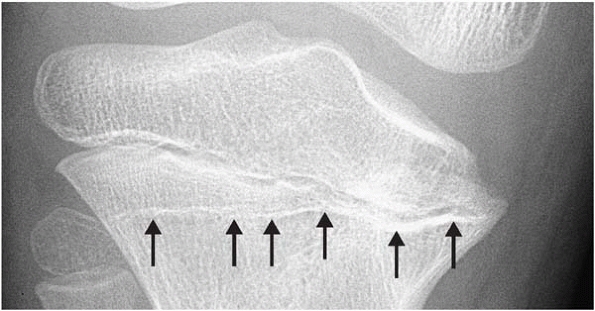
at high risk for physeal arrest should be followed for 6 to 12 months
beyond healing. The Park-Harris line is valuable (Fig. 4-5). An MRI8
can typically demonstrate a physeal arrest by approximately 6 months
after injury. Beware of the occult physeal fracture. These are complete
physeal fractures that are barely displaced on initial presenting
radiographs. The typical case is a distal femoral physeal fracture that
is dismissed as a sprain. The radiographs may be read by an uninformed
radiologist as normal. Physical exam is essential in these cases. Be
aware that physes adjacent to diaphyseal fractures (the distal femoral
physis adjacent to an ipsilateral tibial shaft fracture) may sustain an
unrecognized injury.9
 |
|
▪ FIGURE 4-5 Medial growth arrest of the proximal tibia. Note the value of the Park Harris growth arrest line in making this diagnosis (arrows).
|
and the orthopaedist the license to practice. To stay out of trouble,
the orthopaedist should get a social worker, pediatricians, and other
appropriate experts and consultants involved as soon as nonaccidental
injury is suspected. The history should include a thorough discussion
of how the child was hurt and who was present at the time of injury.
Family history of osteogenesis imperfecta or other multiple-fracture
problems should be sought. About 95% of children can be diagnosed with
osteogenesis imperfecta based on a family history and a physical
examination of the child. The physical examination of a child
suspicious for nonaccidental injury should
include
a full evaluation of the skin, trunk and other parts of the body, in
addition to the particular injured limb. Remember that the age of the
child is a very important consideration in nonaccidental injury (Fig. 4-6).
Abuse is the cause of about 60% of fractures in children less than 1
year old and approximately 90% of fractures in children less than 6
months old. Nearly half of all femur fractures that occur in children
before they reach walking age are thought to be due to nonaccidental
injury. There is no pathognomonic fracture pattern in abuse. Rather,
the age of the child, the overall injury pattern, the stated mechanism
of injury, and pertinent psychosocial factors must all be considered in
each case.10 Classically, corner
fractures, especially of the distal femur, and multiple rib fractures,
skull fractures or fractures in multiple stage of healing are
considered highly suggestive of nonaccidental injury. Any long bone
spine fracture or skull fracture can be related to child abuse. To stay
out of trouble, prepare all records as though everything you write will
be reviewed by lawyers and read aloud in court.
 |
|
▪ FIGURE 4-6
Understanding mechanism of injury is essential. This “floating elbow”—a combination of a distal humeral epiphyseal fracture and a Monteggia fracture—is caused by hyperextension, such as when a child falls on an outstretched hand. However, this 3 month old does not even have the reflex yet to break a fall with an outstretched hand. Understanding the mechanism produces the conclusion that this injury resulted when someone (in this case a parent) forcibly hyperextended the baby’s arm in anger. |
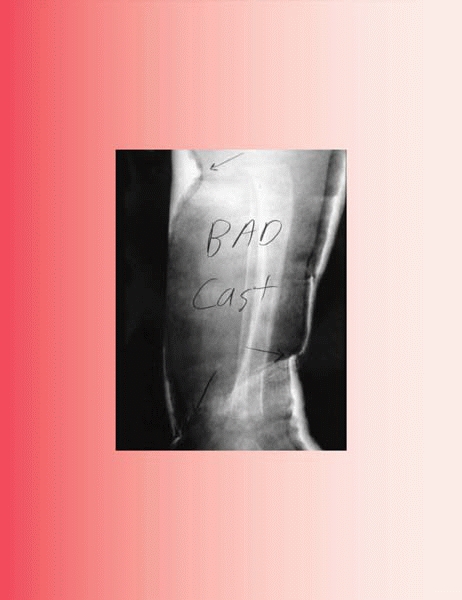
orthopaedics. Trouble comes from improperly applied casts, ignored
cast-related symptoms (Fig. 4-7), and injury inflicted from the children themselves (Fig. 4-8).
If pain in a cast is increasing in minutes to hours after injury, think
of compartment syndrome. If pain in a cast is increasing in days to
weeks after injury, think of skin problems. Many wise orthopaedists
follow the dictum: “worsening pain in a cast means that the cast should
be removed and the limb should be examined.” Fractures can always be
remanipulated, but full thickness skin loss is difficult to manage.
this art are being lost as pediatric orthopaedists increasingly use
internal and external fixation to manage
children’s
fractures. Trouble, such as loss of reduction, malalignment in the
cast, or skin problems, result when standard principles are forgotten.
One common mistake is placing the molds of a 3-point mold too close
together such that they all act in the same region. This is
particularly common for young orthopaedists managing pediatric wrist
and forearm fractures (Fig. 4-9).
The cast index is a valuable tool for managing forearm fractures. The
cast should be oval, such that the diameter in the radial/ulnar
direction is longer than the diameter in the anterior/posterior
direction. The ratio should be about 0.7. In forearm fractures, the
interosseous membrane is at maximum stretch at neutral to 30° of
supination. Postreduction x-rays should be examined closely for signs
of potential cast trouble (Fig. 4-10). At the
joint creases, particularly the anterior aspect of the ankle and elbow,
look for creases in the cast that may result in skin breakdown. In
infants and toddlers, study the relationship between the cast, the
joints, and the soft tissue. If the cast is not well molded and applied
above the knee and elbow, toddlers and infants can often wiggle their
way out of the cast, or pull their hand or foot far enough into the
cast to lead to trouble. If a child reports that something’s stuck down
into the cast, take this complaint seriously. Objects such as coins,
pen caps, and other toys can lead to full thickness skin breakdown. Wet
casts are a nuisance for families and orthopaedists, because they lead
to an embarrassing visit at which the orthopaedist has to change the
cast and scold the child and family (Fig. 4-11).
The transgression by the child can be something as simple as not
sealing the cast well during a bath or shower. Although these wet cast
visits are annoying, stay out of trouble by changing a wet cast
promptly. Prolonged time in a wet cast can lead to skin maceration, and
even clinically important infections (Fig. 4-12).
 |
|
▪ FIGURE 4-7 A classic cast pressure ulcer (red arrow).
If mom calls because the child is complaining of heel pain in the cast, instruct the family to come in as soon as possible for cast removal. |
 |
|
▪ FIGURE 4-8
Some of the kid’s scratching implements can break off and get stuck. Here a plastic knife handle created pressure ulcers. Education may be the only hope to limit the amount of this trouble. Our cast techs do their teaching about wet casts and sticking things in casts as they apply the cast. However, nothing is foolproof with such ingenious fools. |
 |
|
▪ FIGURE 4-9 Sometimes it takes a crooked cast to make the bone straight. A:
This before-and-after composite picture shows the importance of a well formed cast. The radiograph on left shows midshaft angulation, because the forearm is sagging in the poorly molded cast. The new cast (image on right) has a molded ulnar border, which has corrected the malalignment. B: Photograph of the cast. |
 |
|
▪ FIGURE 4-10
A poster child for a bad cast, creating a set-up for iatrogenic fracture care complications. Cast material is creasing into the popliteal fossa and the anterior distal leg. Padding is too thick in some places and too thin in others. This often results when the child is anxious and in pain due to inadequate sedation. |
 |
|
▪ FIGURE 4-11
A wet cast seems like nothing more than a nuisance, but it should be changed promptly. A prolonged period in a wet cast can lead to skin maceration, skin breakdown, and infection. |
 |
|
▪ FIGURE 4-12 Take the wet or foul-smelling cast seriously. This child had full-blown staph sepsis.
|
Certainly in some scenarios—such as when there is significant swelling
or the need to repeatedly evaluate a wound or perform neurovascular
exams—this is true (Fig. 4-13). However,
splints cause a lot of trouble themselves. In many EDs, the emergency
medicine physician applies some prefabricated splint material, wraps it
on nice and tight with an ace wrap, and informs the family to go to the
orthopaedic clinic the next morning. For many reasons, these families
don’t arrive in clinic for days or even weeks. The ace wraps roll up,
creating rows of blisters, ecchymosis, and distal swelling (Fig. 4-14).
Lack of sufficient padding in the prefabricated splints creates the
risk for pressure sores, especially on the heel. The best way to stay
out of trouble is by educating the referring physicians and seeing
these reportedly minor injuries as soon as possible.
 |
|
▪ FIGURE 4-13
A carefully applied, well-padded cast is the optimal immobilization for most pediatric fractures. In some cases, however, swelling or the need for repetitive physical exams (as in this case) make splinting the best option. |
 |
|
▪ FIGURE 4-14 Splints can cause a heap of trouble, especially when followup is days or weeks after application. This prefabricated splint (A)
was applied by the ED physician and the family was instructed to follow up with Orthopaedics the next day. The family presented 3 weeks later to Orthopaedics. The child had been running on the splint. The ace wrap was rolled up, creating a crease at the front of the ankle. Clinical photos (B, C) taken after splint removal show ecchymosis and skin blistering, a heel ulcer, and swelling of the foot distal to the rolled-up ace wrap (red arrows). |
potentially catastrophic in its implications. In the setting of
high-energy or multiple trauma, the child should be assumed to have a
spine injury until proven otherwise. The initial history and physical
examination is essential to staying out of trouble. Learn as much
detail
as
possible about the mechanism of injury, and search for signs of head
injury or skin findings such as a lap belt sign across the abdomen. A
history of loss of consciousness or head injury should raise concern
about a possible cervical spine injury. If there is a potential spinal
cord injury, document a good neurologic exam. In particular, stay out
of trouble by looking for sacral sparing, as it may indicate a good
prognosis for neurologic recovery.
 |
|
▪ FIGURE 4-15 Don’t immediately attribute a wide retropharyngeal space (red arrow) to trauma and swelling—it may be due to crying, as seen in this image.
|
trauma evaluations. If these initial films are normal, but the child
has neck pain or concern of injury and is awake and cooperative,
flexion/extension lateral cervical spine radiographs should be the next
step. Don’t be fooled by certain false positives in children—that
retropharyngeal “swelling” due to crying (Fig. 4-15) and C2-3 pseudosubluxation. A CT scan
may be valuable to clarify a suspected upper cervical spine injury in
children. An MRI has shown to be an effective method for clearing the
cervical spine in obtunded children.11,12
 |
|
▪ FIGURE 4-16 This 3 year old presented after a fall with a minor concussion. The radiographs, including the lateral (A) and full flexion lateral (B)
were read as normal by a very capable and respected pediatric radiologist. No further imaging was performed. The boy was lost to followup, then returned nearly 2 years later because of intermittent neck pain. The lateral (C) shows an odontoid nonunion, read as “os odontoidium.” The nonunion is clearly visualized on the MRI (D). The lesson? Even in the best of hands, some cervical spine injuries in young children cannot be detected on plain radiographs. Use MRI or CT if there is concern for an occult injury. |
 |
|
▪ FIGURE 4-17
SICWORA. This patient came into the ED with no neurologic deficits. Initial plain radiographs were read as normal. Paraplegia developed the next morning. MRI (A, B) increased 2 vertebral fractures and signal in the spinal cord, confirming injury (red arrow). |
lethal. This injury occurs more often in children due to the laxity of
the ligamentous structures anchoring the occiput to the axial skeleton.
The mechanism of action usually involves a sudden
acceleration-deceleration force on the head of the child. The
dislocation usually severs the spinal cord at the foramen magnum,
resulting in acute respiratory arrest.13
To stay out of trouble, understand that these injuries may often not be
appreciated on the initial presentation of the child to the trauma
center. Some occiput C-1 injuries reduce in the field or on transport
to the trauma facility, and then are not discovered until radiographs
are done in a different position, especially traction. When discovered,
an occiput C-1 disruption should be treated with an occiput C-2 fusion.
atlanto-dense interval (ADI). The ADI in children has an upper limit of
normal of 5 mm. If the atlanto-dens interval is greater than 5 mm on
flexion/extension lateral radiographs in the setting of trauma, a
C-1/C-2 fusion is recommended.
fracture in children. The injury usually occurs at the synchondrosis,
leading to a pattern similar to a type II odontoid fracture in adults.
Many pediatric odontoid fractures will heal with reduction and halo
vest immobilization.14 To stay out
of trouble, be certain to get a satisfactory reduction, and document
maintenance of reduction over the first 2-4 weeks. A halo vest
treatment in children is associated with well-documented trouble. In
younger children with thinner skulls, more pins at lower torque should
be used.15 Most pediatric odontoid
fractures will heal readily with immobilization, but they should be
followed for at least a year. Some cases of os odontoidium are
nonunions of early childhood odontoid fractures that either did not
present at the time of injury, were missed, or were unsuccessfully
treated (Fig. 4-16).
 |
|
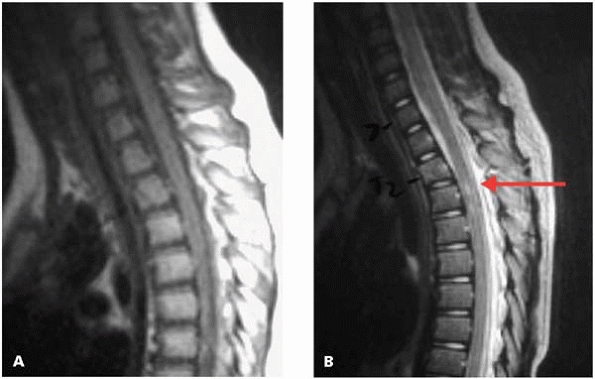
▪ FIGURE 4-18 L1 compression fracture without neurologic injury. On initial CT (A) the collapse and retropulsion can be appreciated. After posterior instrumented spinal fusion (B), the CT scan (C) shows reconstitution of vertebral height and correction of the local kyphosis.
|
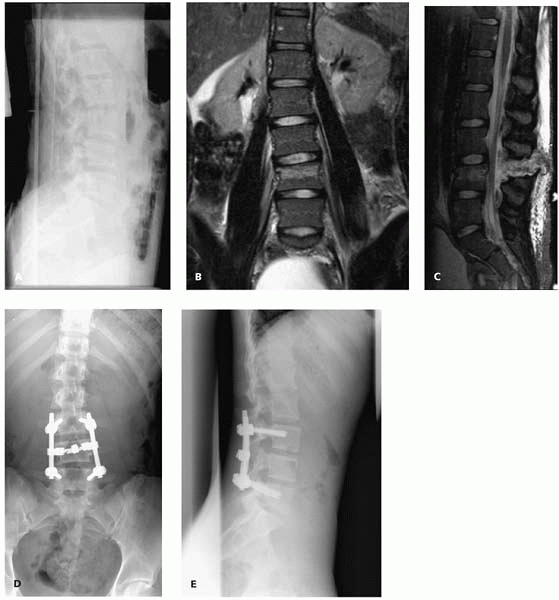
children than adults. Beware of the constellation of injuries
categorized as SCIWORA (spinal cord injury without radiographic abnormality) (Fig. 4-17).
In young children, be certain that the injury was not caused by child
abuse. Generally, it takes a significant amount of force to create
these injuries in children; if the mechanism of the spine
fracture
is said to be a “simple fall,” investigate the story thoroughly. An MRI
has become the standard for evaluating these injuries. Stable injuries,
usually compression fractures near the thoracolumbar junction, can be
satisfactorily managed with brace treatment. Injuries with significant
deformity (Fig. 4-18) and/or instability (Fig. 4-19) are usually treated with posterior instrumented spinal fusion.
 |
|
▪ FIGURE 4-19 L4 chance fracture without neurologic injury (A). The MRI (B, C) shows both a bony component and complete ligamentous disruption, requiring a posterior instrumented spinal fusion (D, E).
|
-
Recognize that
certain injuries are sentinels for associated injuries. Examples of
this include rib fractures, pelvic fractures, facial injuries, and a
lap belt sign on the anterior aspect of the abdomen or chest. -
Upon first meeting
the family, use the first few minutes to establish the optimal
relationship: a partnership, you and the family against the injuries. -
Discuss findings
again immediately after any surgery, and reinforce recovery,
complications and hurdles you and the parents may encounter in the
months to come. The more untrusting the family, the more you should see
them, both inpatient and outpatient. -
Partnering with a
general surgeon and a neurosurgeon, and using a careful physical exam
and liberal use of imaging, are valuable ways to optimally collaborate
care when there are both skeletal injuries and multiple internal
injuries. -
Don’t ignore the signs of acute compartment syndrome in open fractures thinking that “a fasciotomy has been done by the injury.”
-
Be alert that
compartment syndrome may be quite delayed in children. Although the
reason for this delay is not clear, the first diagnosis is often 20 to
40 hours after fracture. -
Don’t underestimate
the extent that a child can recover from severe multi-trauma,
particularly head and spinal cord injury. Treat fractures expecting
recovery. -
The orthopaedist
should get a social worker, pediatricians, and other appropriate
experts and consultants involved as soon as nonaccidental injury is
suspected. -
Worsening pain in a cast means that the cast should be removed and the limb should be examined.
-
Postreduction
radiographs should be examined closely for signs of potential cast
trouble. At the joint creases, particularly the anterior aspect of the
ankle and elbow, look for creases in the cast that may result in skin
breakdown. -
Although wet cast
visits are annoying, stay out of trouble by changing a wet cast
promptly. Prolonged time in a wet cast can lead to skin maceration, and
even clinically important infections. -
In the setting of high-energy or multiple trauma, the child should be assumed to have a spine injury until proven otherwise.
RM, Luhmann JD, Luhmann SJ. Emergency department management of pain and
anxiety related to orthopedic fracture care: a guide to analgesic
techniques and procedural sedation in children. Paediatr Drugs. 2004;6-1:11-31.
RM, Porter FL, Miller JP, et al. Comparison of fentanyl/midazolam with
ketamine/midazolam for pediatric orthopedic emergencies. Pediatrics. 1998;102-4 Pt 1:956-963.
JM, Closkey RF, Mahboubi S, et al. Role of magnetic resonance imaging
in the assessment of pediatric cervical spine injuries. J Pediatr Orthop. 2002;22-5:573-577.
T, Langlais J, Glorion C, et al. Fractures of the odontoid process: a
report of 15 cases in children younger than 6 years. J Pediatr Orthop. 1999;19-1:51-54.