Trauma about the Elbow I: Overview, Supracondylar, and Transphyseal Fractures
– Trauma > 5 – Trauma about the Elbow I: Overview, Supracondylar,
and Transphyseal Fractures
|
|
|
|
orthopaedist with many opportunities to get in trouble. A thorough
understanding of the anatomy and development of the immature elbow is
necessary to stay out of trouble with elbow fractures.
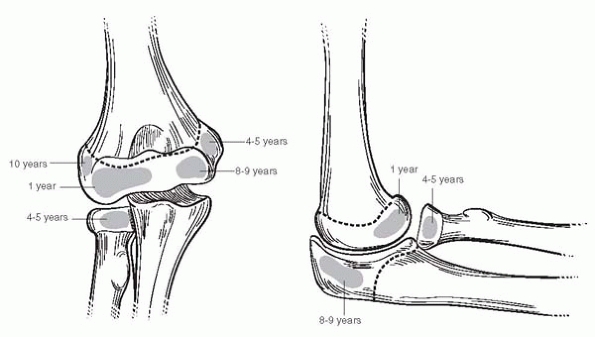
the elbow appear in a relatively predictable order, which may serve as
landmarks to define the anatomy of the largely cartilaginous elbow
during early childhood (Fig. 5-1). Easily
remembered mnemonics aid in remembering the order of ossification;
however, in our age of political correctness the most memorable ones
may only be passed on by word of mouth. As a fracture line in pediatric
elbows may travel through unossified cartilage, one often must rely on
the relationship between the ossification centers and visible bone to
define the injury. The radial head, the trochlea, and the olecranon may
appear as multiple ossification centers that may be mistaken for a
fracture.
 |
|
▪ FIGURE 5-1 Secondary ossification centers of the elbow, with range of ages of appearance.
|
the three following anatomic relationships in every radiograph of a
child’s elbow:
-
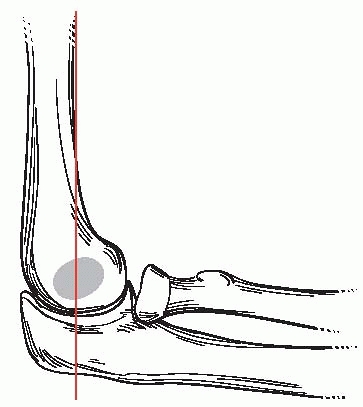
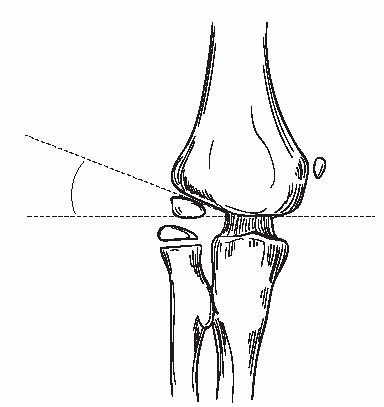
The anterior humeral line intersects the capitellum.
If the center of the capitellum is posterior to this line, an extension
type supracondylar fracture is likely, or a transphyseal fracture, seen
more commonly in the very young. If the capitellum is anterior to the
line, the less common flexion type supracondylar fracture or
transphyseal fracture is likely (Fig. 5-2). One
must be certain that the radiograph is a true lateral view of the
distal humerus because any rotation will make the capitellum appear
posterior. -
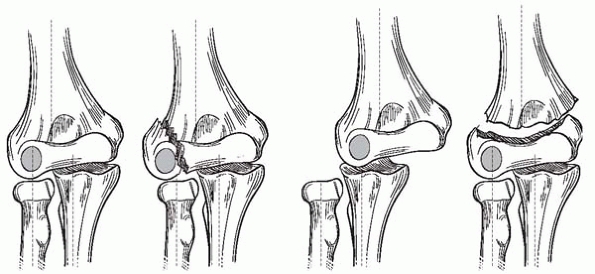
The radius should point to the capitellum in all views (Figs. 5-3 and 5-4).
If it doesn’t, a lateral condyle fracture, a radial neck fracture, a
Monteggia fracturedislocation or equivalent lesion, or an elbow
dislocation should be considered. Note that the normal radial
angulation of the neck may be up to 15° valgus and 10° anterior. -
The humeral capitellar (Baumann’s) angle should be in valgus (95% of normal elbows have an angle of 9°-26°) (Fig. 5-5). Baumann’s angle is a
P.53relatively sensitive indicator of varus angulation of the distal
humerus, and is primarily useful in assessing the adequacy of reduction
in supracondylar fractures. Angulation of the humerus to the X-ray
cassette or the X-ray beam to the humerus in the sagittal plane can
lead to significant measurement errors of this angle. Thus taking an AP
radiograph of a distal humerus may demonstrate a different Baumann’s
angle than an attempted AP of an elbow in which neither the distal
humerus nor the proximal forearm are at right angles to the X-ray beam.
In addition, the long axis of the ulna should be in line and slightly
medial to the long axis of the humerus on a true AP view (see Fig. 5-3).
If not, and the radial head and capitellum remain in correct alignment,
a transphyseal injury or displaced supracondylar fracture should be
considered. If the radius is no longer pointing to the capitellum, an
elbow dislocation must be considered.
 |
|
▪ FIGURE 5-2 In the normal elbow, a line drawn down the anterior humerus bisects the capitellum.
|
 |
|
▪ FIGURE 5-3
Relationship between the radius and capitellum, and the ulna and humerus, in normal and injured elbows, as visualized on an AP radiograph. |
 |
|
▪ FIGURE 5-4 The radius should point to the capitellum in all radiographic views.
|
A lateral radiograph of a normal elbow flexed at ninety degrees may
show a small anterior fat pad bulging from the shallow coronoid fossa,
but do not be fooled by this, as it is of no clinical significance. In
contrast, if an elevated posterior fat pad is visible, but no fracture
is appreciated on initial radiographs, an occult fracture is likely
present, and the child’s arm should be protected on the assumption an
occult fracture is present.1
proven useful in improving diagnostic accuracy by orthopaedic surgeons
or residents. However, if doubt remains, comparison views may be
helpful in individual cases. An arthrogram and/or live fluoroscopic
imaging, or even MRI, will sometimes help to establish a diagnosis when
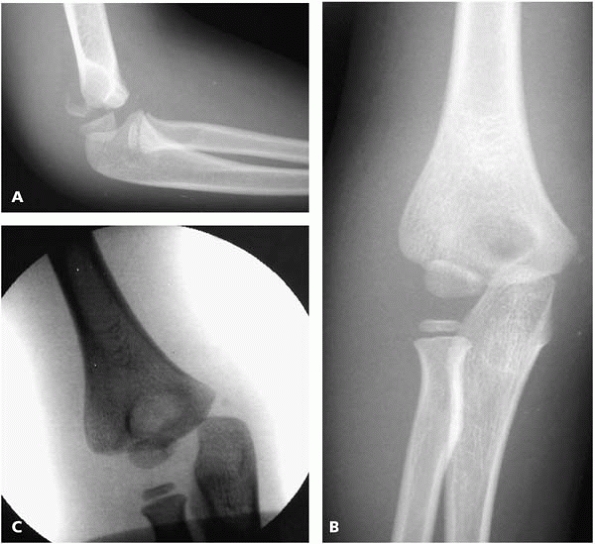
plain radiographs are inconclusive. For example, prior to ossification
of the trochlea and medial epicondyle, a lateral condyle fracture (Fig. 5-6)
may appear identical to a Salter II fracture on a plain AP radiograph.
These particular two fractures may at times be clinically
differentiated by the location of maximal swelling, which is on the
side where the periosteum is torn. This is opposite the
Thurston-Holland fragment in a Salter II fracture, or on the same side
as a lateral condyle fracture.
 |
|
▪ FIGURE 5-5 Baumann’s angle is variable, but is generally at least 11 degrees.
|
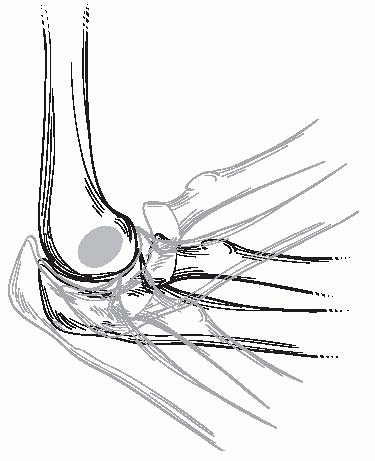
generally rich, the capitellum and the lateral portion of the trochlea
rely on end arteries entering posteriorly.
Avoid
the potentially catastrophic iatrogenic complication of avascular
necrosis of the trochlea by avoiding posterior dissection of the distal
humerus (Fig. 5-7).
 |
|
▪ FIGURE 5-6 A through C:
A Salter II fracture of the distal humerus may be mistaken for a lateral condyle fracture prior to the ossification of the trochlea and medial epicondyle. Lateral elbow radiograph of a 4-year-old boy who fell down the stairs. Preservation of the anatomic relationship of the radius to capitellum in all views, and medial translation of the capitellum on the intraoperative imaging help make the diagnosis. |
 |
|
▪ FIGURE 5-7
Avascular necrosis of the trochlea following posterior open reduction of a supracondylar humerus fracture. Patient has severely limited motion and pain. At this point there is no good treatment option. |
examination are the neurovascular and soft-tissue assessments. The
neurologic examination of a young child with an injured elbow is
difficult yet essential, as the rate of neurologic injury is about 15%
for displaced supracondylar fractures. A thorough preoperative
evaluation may avoid the uncomfortable situation of finding a nerve
injury postreduction without knowing the prereduction status.
Preoperative assessment of the ulna nerve in particular may be
challenging. However, even young children will usually pinch an
examiner’s finger, allowing the examiner to palpate contraction of the
first dorsal interosseous muscle and confirm ulnar motor function.
children undergo remodeling to the same extent as fractures in other
locations. However, since only 20% of the growth of the humerus occurs
in the distal portion, there is insufficient growth to rely upon for
angular remodeling, even in the plane joint of motion. In fractures
about the elbow, unlike most other fractures in children, one should
strive for anatomic reduction.
fracture in children requiring surgery. Though common, these fractures
are notorious for complications and litigation.
with an absent pulse. To clarify one’s thinking, consider three
clinical scenarios:
-
Hand well-perfused (warm and red), radial pulse present.
-
Hand well-perfused, radial pulse absent.
-
Hand poorly perfused (cool and blue or blanched), radial pulse absent.
urgent treatment. If practical, an immediate attempt at closed
reduction in the operating room is ideal. If this is not practical,
gentle traction and placement of the elbow in 20 to 40 degrees of
flexion should be performed. Note that the this maneuver is not
an attempt to anatomically reduce the fracture, as further injury to
neurovascular structures is possible, and an acceptable reduction is
unlikely without the use of fluoroscopy and K-wires. Vascular
compromise is usually positional, with the proximal fragment often
causing occlusion of the brachial artery. Most frequently a child with
a poorly perfused, pulseless hand, whose arm was splinted in full elbow
extension prior to arrival at the hospital, will have significant
improvement in vascular perfusion by simply flexing the arm to 20 to 30
degrees (Fig. 5-8). Arteriograms generally have
no role in preoperative evaluation of the pulseless supracondylar
fracture, as they delay treatment and most frequently contribute no
useful information.2
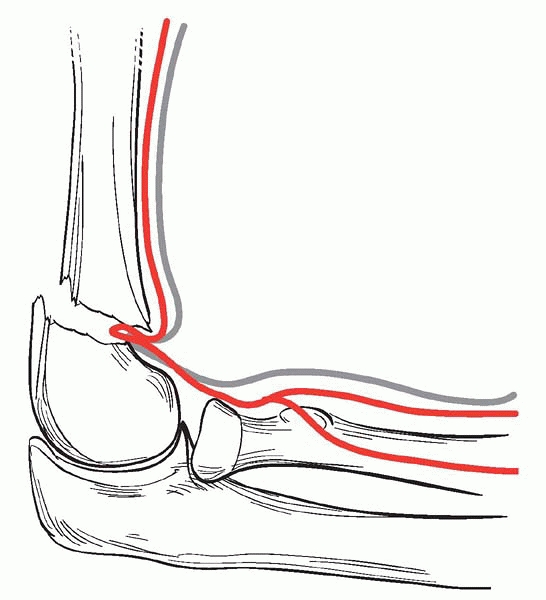
poorly perfused, pulseless hand, perfusion usually returns. If the hand
remains poorly perfused and pulseless, operative exploration is
indicated. An anterior approach is appropriate
when
the purpose of the approach is for arterial exploration. Be aware that
at times the artery itself is not trapped in the fracture site, but
soft tissue adjacent to the artery is trapped, tethering the artery
just enough to stop flow. If the hand is still poorly perfused after
exploration and removal of an entrapped or tethered artery from the
fracture site, a general or vascular surgical consult is wise (Fig. 5-9).
 |
|
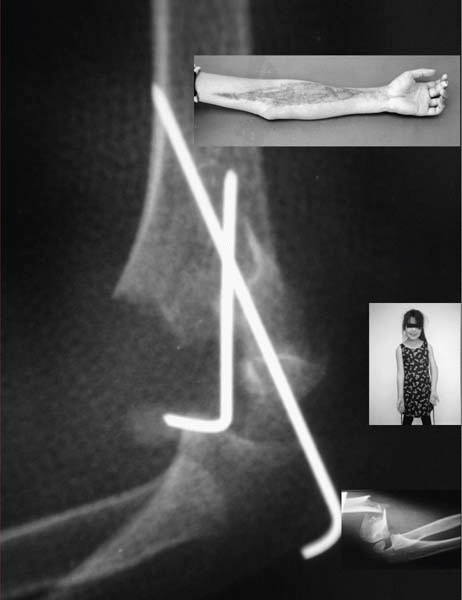
▪ FIGURE 5-8
The proximal fragment of a displaced supracondylar fracture may cause arterial occlusion, especially if the elbow is immobilized in extension. |
 |
|
▪ FIGURE 5-9
Brachial artery and median nerve may be trapped at the fracture site. If a reduction feels rubbery, and a gap at the fracture site is seen on imaging, entrapment is possible, especially in the setting of vascular compromise or median nerve or AIN injury. |
warm and well perfused management is controversial. Some favor arterial
exploration and repair if needed at that time. With such excellent
collateral circulation about the elbow, close in-hospital observation
of at least 48 hours and mild elevation is usually sufficient, with an
understanding that if the hand loses perfusion an urgent return to the
operating room may be necessary.
very infrequent. A great way to minimize the risk of compartment
syndrome is to avoid elbow flexion greater than 90 degrees (Fig. 5-10).
With the predictable efficacy and safety of closed reduction and pin
fixation, elbow hyperflexion should no longer be used to hold a
fracture reduction. As a general rule, if an elbow needs to be held in
more than 90 degrees of flexion to keep the fracture reduced, using
k-wires to maintain the reduction is probably safer. In a child with a
supracondylar fracture, as elbow flexion increases, forearm compartment
pressures increase dramatically3 and brachial artery flow decreases.4
attention. If the elbow is excessively swollen, perhaps with anterior
skin tenting (which suggests significant soft-tissue injuries),
treatment should be urgent to prevent compartment syndrome and
soft-tissue injury. Patients with a concomitant forearm fracture should
be closely watched for compartment syndrome as well. Particularly in
children, soft findings such as paresthesias are difficult to
interpret, and worsening pain is the most valuable sign of developing
compartment syndrome. As in adults, follow the golden rule for staying
out of trouble: if you are thinking about compartment syndrome, you
should probably measure compartment pressures or release the
compartments. One may want to consider avoiding narcotics for pain
management to better follow an examination in children at high risk for
compartment syndrome.
 |
|
▪ FIGURE 5-10
Avoid casting supracondylar fracture beyond 90 degrees as this position increases compartment pressures and decreases perfusion to the hand and forearm. |
compartment syndrome that was initially unrecognized in the setting of
a median nerve injury. Any child with impaired sensation, either from
local nerve injury or decreased mental status, should be closely
evaluated for compartment syndrome.
AIN (anterior interosseous nerve) injuries, posterolaterally displaced
fragments with radial nerve damage, and flexion type fractures with
ulnar nerve injury. Nerve damage at the time of injury should be
observed; it usually improves within 3 months. One exception to this is
an open fracture, for which exploration of the nerve should be
considered if it would not require extensive dissection. An ulnar nerve
palsy following fixation with a medial pin most often resolves within 4
months, and removal of the medial pin upon recognition of the nerve
injury is controversial, though probably a good idea.5 If the surgeon chooses to remove the medial pin before the fracture is healed, loss of fracture reduction
is a potential pitfall. Thus, medial pin removal in a potentially
unstable fracture should occur in the operating room only after an
additional pin has been placed to ensure maintenance of fracture
reduction after medial pin removal.
should raise the concern that the nerve may be trapped or tethered at
the fracture site (see Figure 5-9). If on the lateral x-ray there is a gap at the fracture site, surgical exploration may be indicated.
can safely wait until morning. There are now at least four studies
reporting that mean delays of 8 to 21 hours in the treatment of
supracondylar humerus fractures do not increase the risk of
complications or need for an open reduction. These studies must be
interpreted with a great deal of caution, as they are retrospective.
One interpretation of these studies is that orthopaedic surgeons’
clinical judgment in determining which fractures needed urgent
treatment was correct, and we should therefore continue to have a high
vigilance for fractures at risk. Most Type II and III fractures without
undue swelling, skin puckering from the proximal fragment, significant
vascular impairment or signs of compartment syndrome do not require
urgent surgery. Children awaiting surgery may have their arms splinted
in 20° to 50° of elbow flexion, elevated, and checked every hour or two
by someone capable of recognizing signs of trouble.
about 3 weeks. It has been recommended that in order to reduce and
maintain reduction of a type II extension supracondylar fracture
without pins, the elbow must be flexed to at least 120 degrees. While
good results are certainly possible with this technique, it is more
predictable to perform a closed reduction and pinning of any displaced
supracondylar fracture (see Figure 5-10).
Anecdotally it appears that more malpractice suits are generated from
malreduction of type II fractures than type III fractures. As there is
relatively little growth in the distal humerus, significant remodeling
can not be relied on, even in the plane of motion. Stay out of trouble
by pinning type II fractures.
mention—the apparently minimally displaced fracture with medial
comminution or impaction and a change in Baumann’s angle.6 This fracture pattern is easy to mistake for a Type I fracture and treat nonoperatively, which would result in cubitus varus (Fig. 5-11).
Operative reduction can usually be achieved by applying a significant
valgus force on a fully extended elbow, followed by flexion, pronation
(to maintain tension across the medial column), and pinning.
 |
|
▪ FIGURE 5-11
Look for medial comminution, which is indicative of the fracture being in varus, and usually requires operative reduction and pinning. |
Particularly in children with preoperative vascular compromise or AIN
palsy, beware of the reduction that feels “rubbery” as the brachial
artery or median nerve may be trapped in the fracture site. The
criteria for accepting a closed reduction are:
-
Baumann’s angle is restored.
-
The anterior humeral line intersects the capitellum.
-
The medial and lateral columns have substantial contact.
acceptable. A fair amount of rotation is also acceptable, as the
shoulder joint can make up for it. Open reductions
should
be done to remove interposed tissue, but only after a very patient
effort at closed reduction has failed. The opened elbow may be stiffer
than those treated closed, and the scar can be unsightly.
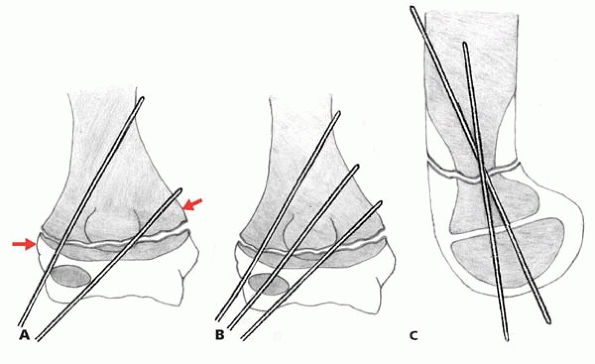
important technical points for successful lateral entry pin fixation
are: 1) maximize separation of the pins at the fracture site; 2) engage
the medial and lateral columns proximal to the fracture; 3) engage
sufficient bone in proximal and distal fragments; and 4) have a low
threshold to use a third lateral pin if there is concern over fracture
stability or pin placement following the placement of two lateral pins (Fig. 5-12).7
the frontal plane. It does not occur as a result of a medial growth
arrest, as there is too little growth in the distal humerus to cause
this deformity within months of injury. After pinning, full extension
of the arm is often not possible, so the clinical exam may be
unreliable. There is no way to avoid this complication other than being
strict in obtaining and carefully scrutinizing adequate quality
imaging, confirming that the fracture is not in cubitus varus.
in 5-6% of the two largest series of operatively treated supracondylar
fractures. This complication is predictably avoided by avoiding the use
of a medial pin.
 |
|
▪ FIGURE 5-12 Proper positioning of 2 or 3 lateral entry pins. A potential pitfall is to have insufficient bone purchase (arrows).
(Reprinted with permission from Skaggs DL, Cluck MW, Mostofi A, et al. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg. 2004;86-A(4):702-707.) |
pins that lost reduction revealed the cause was always secondary to
errors in pin placement, such as pins crossing or immediately adjacent
to each other at the fracture site (Fig. 5-13). No failures in cases fixed with 3 lateral pins were identified.7
injury to the ulnar nerve is a complex issue. One thing that is certain
is not to place a medial pin when the elbow is flexed. The Boston
Children’s group reported that in children less than five years of age,
when the elbow is flexed more than 90 degrees, the ulnar nerve migrated
over, or even anterior to, the medial epicondyle in 61% of children.8
Unfortunately, even making an incision over the medial epicondyle to
make certain the ulnar nerve is not directly injured by a pin does not
ensure protection of the nerve.9 In
a series of six cases of iatrogenic ulnar nerve injuries with early
exploration, the nerve was directly penetrated by the pin in only two
cases, with constriction of the cubital tunnel in three cases, and the
nerve fixed anterior to the
medial epicondyle in one case.10
Thus even if direct penetration of the ulnar nerve is avoided, simply
placing a medial epicondyle entry pin adjacent to the nerve may cause
injury.
 |
|
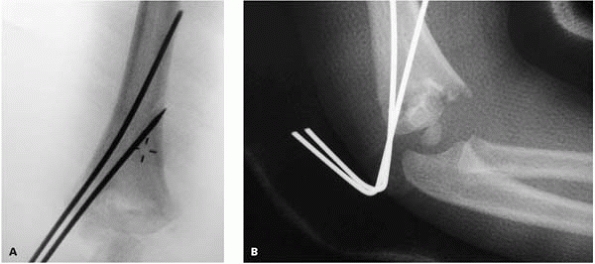
▪ FIGURE 5-13 Pins are so close that they biomechanically function as one, allowing loss of reduction. (A) Intraoperative radiograph. (B)
Postoperative loss of reduction in same patient. (Reprinted with permission from Skaggs DL, Cluck MW, Mostofi A, et al. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg. 2004;86-A(4):702-707.) |
predisposed to trouble, a detailed discussion of surgical technique is
warranted. Traction is applied in line with the humerus, with the elbow
in slight flexion. Avoid traction in full extension as this may cause
tethering of neurovascular structures over the proximal fragment. If
there is suspicion that the proximal fragment has pierced through the
brachialis muscle, persistent, gradual traction of the slightly flexed
elbow for a full minute will often reward you with a palpable freeing
of the proximal fragment. Alternatively, the proximal to distal
“milking” maneuver over the brachialis may achieve the same end.11 Freeing the proximal fragment from soft-tissue entrapment is essential for an anatomic reduction, and worth the time invested.
pushing in an anterior direction on the olecranon. Keep the elbow
hyperflexed during fluoroscopic assessment. An AP image is difficult to
interpret with the proximal ulna and radius overlying the fracture
site. However, slightly oblique views allow assessment of the
continuity of the medial and lateral columns and Baumann’s angle.
reduction with two additional maneuvers. If the distal medial column is
still posterior (most commonly internally rotated), press selectively
harder on the medial side during the reduction, and pronate the forearm
during the reduction as well. The opposite applies for an externally
rotated distal fragment. If Baumann’s angle is not clearly at least 10
degrees, or medial comminution remains, repeat the reduction while
stressing the arm in valgus.
relax, such as the author, may tape the arm with Coban in the
hyperflexed, reduced position to effortlessly maintain reduction.
Lateral entry pins are placed first by the above technique, being
certain to go through the proximal cortex, and pin position is assessed
with AP and lateral imaging. The arm is then straightened and the
carrying
angle is assessed clinically, at which point Baumann’s angle is
assessed again with AP imaging. The arm is then subjected to varus and
valgus, flexionextension and rotational stress under live AP imaging to
assess fixation. If there is any question of stability, place a third
pin, lateral or medial, depending on surgeon preference and fracture
pattern, then reassess stability by stressing the fracture under live
imaging.
in about 30 to 70 degrees of elbow flexion depending on swelling, but
certainly no less than 20 degrees of extension greater than the amount
of flexion at which the pulse disappears. Pins should be bent 90
degrees to help prevent subcutaneous migration, with the skin protected
by sterile felt or petroleum jelly-impregnated gauze. Foam padding
placed directly on skin, with no underlying circumferential bandaging,
allows for swelling, and obviates the need for splitting the cast (Fig. 5-14).
Fiberglass casting allows for better postoperative radiographs.
Alternatives such as split casts or splints are used successfully as
well.
 |
|
▪ FIGURE 5-14 Sterile foam placed directly on skin with no underlying circumferential bandages allows for swelling under the cast.
|
the distal fragment can be moved into flexion and extension. A
potential pitfall is to create this situation iatrogenically by an
overenthusiastic reduction, in which the posterior periosteum is torn,
as the hapless surgeon feels the fracture fragment move from extension
to flexion. Using the surgical technique described in the next section
for flexion-type supracondylar fractures, these completely unstable
fractures can often be treated without the need for an open reduction.
relatively rare injuries, closed reduction and pinning is technically
more challenging than extension type fractures. In order to reduce the
fracture, the elbow is extended. However, in an extended position,
K-wires are more difficult to place. In addition, when
attempting
to view the lateral image of the elbow, fracture reduction can be lost
if the arm is rotated. These difficulties have led to the belief that
open reduction is usually necessary.
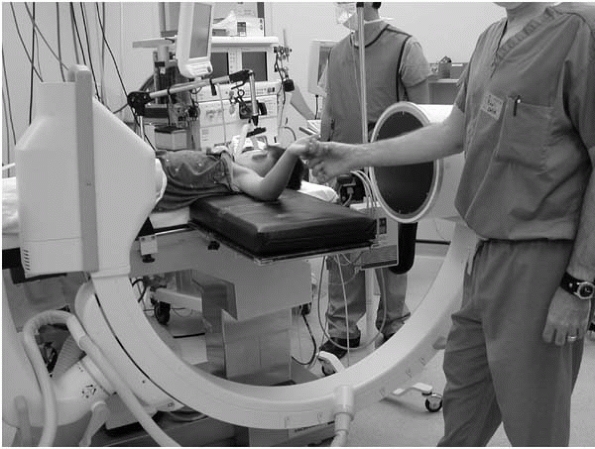
following guidelines. It is helpful to first place two lateral entry
pins in the distal fragment before the fracture is reduced. To confirm
fracture reduction, rotate the image machine between AP and lateral
positions instead of rotating the arm. This can be accomplished by
positioning the fluoroscopy unit parallel to the operating table, and
rotating the c-arm. After fracture reduction is confirmed in both
planes, drive the pins across the fracture site (Fig. 5-15).
 |
|
▪ FIGURE 5-15 Positioning of the c-arm for a lateral image of the elbow for a completely unstable or flexion type supracondylar fracture.
|
are much less common than supracondylar fractures, though the
similarities warrant inclusion in this chapter. There are two easy
opportunities for trouble with transphyseal fractures: making the
diagnosis and missing child abuse. These injuries tend to occur in
children less than 4 years old, when most of the distal humerus is
unossified. Prior to ossification of the capitellum, the appearance of
a transphyseal fracture on plain radiograph is indistinguishable from
an elbow dislocation. Elbow dislocation in this age group is
exceedingly rare, so a capitellum posterior to the anterior humeral
line is likely to be a transphyseal fracture in younger children (see Fig. 5-16 and accompanying text). An arthrogram may assist in the diagnosis and assessment of reduction.
as described above, with a few exceptions. If the fracture presents
late with callous already present, or is already healed to the point
that gentle reduction is not possible, avoid open reduction or forceful
manipulation, either of which may injure the physis. Accept the
position of the fracture and perform a supracondylar osteotomy in the
future,
if
needed. Due to the wider surface area at the level of the physes, this
fracture is inherently more stable than supracondylar fractures. A
small amount of translation will remodel, but varus/valgus angulation
will not.
 |
|
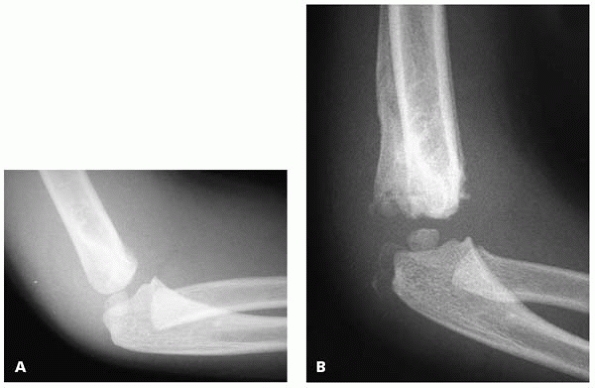
▪ FIGURE 5-16 Unrecognized acute transphyseal fracture. A:
This radiograph was considered normal at initial medical contact. Note that the capitellum is posterior to the anterior humeral line. B: Same patient two months after injury. |
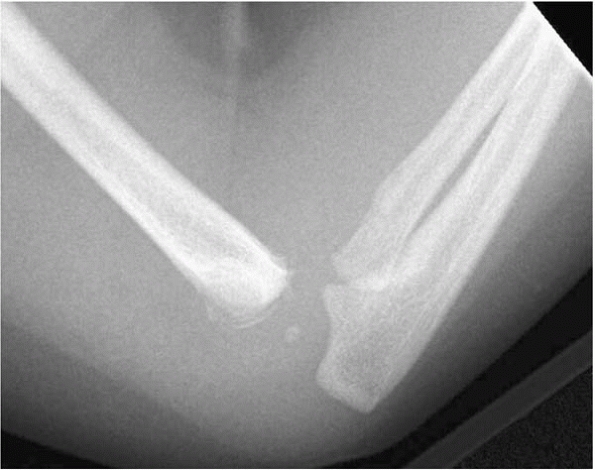
rotatory shear, consistent with the fracture’s association with child
abuse and birth injuries. Pay careful attention to the plausibility of
the parent’s description of how the fracture occurred with concern for
child abuse. In addition, a careful physical examination to uncover
other injuries is warranted (Figure 5-17).
 |
|
▪ FIGURE 5-17
Lateral elbow radiograph in a 3-month-old child at initial presentation for medical care for an acute “swollen elbow” demonstrates a transphyseal fracture. Child abuse is suspected from presence of fracture callus, suggesting a delay in seeking medical care. |
-
For every pediatric elbow radiograph, verify three points:1. The anterior humeral line intersects the capitellum.2. The radius points to the capitellum in every view.3. Baumann’s angle is in valgus.
-
For supracondylar fractures:1. A pulseless, poorly perfused hand needs an urgent reduction, not an arteriogram.2. If an elbow needs to be held in
more than 90° of flexion to keep the fracture reduced, using K-wires to
maintain the reduction is probably safer.3. If in doubt as to whether to fix a type II fracture, fix it. The chances of a good outcome achieved safely are quite high.4. Have a low threshold to place a third lateral-entry pin.
TC. Armstrong DG, Schwend RM. Factors affecting forearm compartment
pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop. 2002;22(4):431-439.
R, Hennrikus W. The effect of elbow position on the radial pulse
measured by Doppler ultrasonography after surgical treatment of
supracondylar elbow fractures in children. J Pediatr Orthop. 1998;18:441-444.
JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous
cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop. 1998;18:43-45.
DL, Hale J, Kay RM, et al. Operative treatment of supracondylar
fractures of the humerus in children: the consequences of pin
placement. J Bone Joint Surg. 2001;83-A:735-740.
MJ, Scott SM, Peters CL. Brachialis muscle entrapment in displaced
supracondylar humerus fractures: a technique of closed reduction and
report of initial results. J Pediatr Orthop. 1997;17(3):298-302.
LA, Dormans JP, et al. Vascular injuries and their sequelae in
pediatric supracondylar humeral fractures: toward a goal of prevention.
J Pediatr Orthop. 1996;16(1):99-103.
SS, Mahar AT, Miesen D, et al. Displaced pediatric supracondylar
humerus fractures: biomechanical analysis of percutaneous pinning
techniques. J Pediatr Orthop. 2002;22:440-443.
CT, Strub WM, Roy DR, et al. The effect of surgical timing on the
perioperative complications of treatment of supracondylar humeral
fractures in children. J Bone Joint Surg Am. 2001;83-A(3):323-327.