Spondylolisthesis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Spondylolisthesis
Spondylolisthesis
Michael K. Shindle MD
David B. Cohen MD
A. Jay Khanna MD
Description
-
Spondylolisthesis is an abnormal AP translation of 2 vertebral bodies relative to each other (Fig. 1).
-
This translation is secondary to a defect
in the pars interarticularis (spondylolysis) or the posterior
ligamentous-bony restraints.
-
-
Spondylolisthesis is classified by type (Table 1) and by the severity of the slip (Table 2) (1,2).
General Prevention
-
No preventive measures except long-term
brace wear have been found to be effective in decreasing the
progression of spondylolisthesis. -
Because major progression is rare, brace treatment commonly is not recommended.
Epidemiology
-
Isthmic spondylolisthesis usually begins
in childhood, but a slight increase in incidence occurs in adolescence,
up to 6% in males (3). -
Degenerative spondylolisthesis occurs mainly in older adults.
-
Compared with males, females develop spondylolisthesis more often and develop more pronounced slips at a younger age (4).
Incidence
-
5% of the general population has spondylolysis or spondylolisthesis (3,4).
-
It does not occur until 5–6 years of age, when the incidence is 3.3% (3,4).
Prevalence
-
The prevalence is 0% at birth, 3–4% at 6 years, and 5–6% in adulthood (4).
-
Spondylolysis occurs most often at L5.
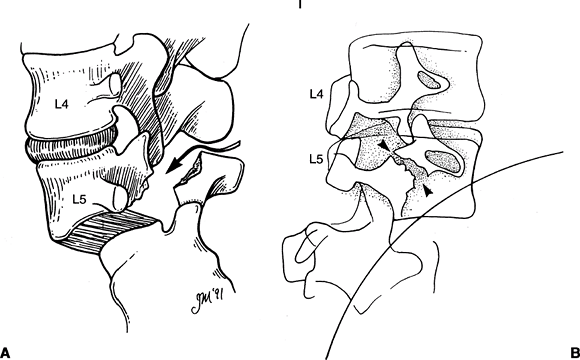 Fig. 1. Lateral (A) and oblique (B) views of spondylolytic spondylolisthesis. The arrows point to a defect in the pars interarticularis.
Fig. 1. Lateral (A) and oblique (B) views of spondylolytic spondylolisthesis. The arrows point to a defect in the pars interarticularis.
Risk Factors
-
A family history of spondylolisthesis
-
Particular physical activities in
adolescence that involve hyperextension of the spine, such as playing
the lineman position in football and participating in gymnastics, have
been associated with a high incidence of isthmic spondylolisthesis (5,6).
Genetics
-
An increased risk is associated with a positive family history.
-
~1/4 of affected patients have a positive family history of spondylolisthesis.
Etiology
-
The cause of isthmic spondylolisthesis is
a stress fracture through a thin portion of the posterior elements
(pars interarticularis). -
The causes of degenerative spondylolisthesis are degeneration and instability of the disc.
Associated Conditions
-
Most people with the condition are otherwise physically normal.
-
However, an increased risk is present if
one has a connective-tissue disorder, such as Marfan syndrome, or
neuromuscular conditions, such as athetoid cerebral palsy.
Signs and Symptoms
-
Symptoms often can be insidious, but they may follow a relatively minor injury.
-
Pain localized to the low back and thigh area may be seen in association with sciatica from an L5 radiculopathy.
-
Back or leg pain
-
Gait abnormality
-
Abnormal posture (hyperlordotic)
-
History of trauma: Acute or mild repetitive, often sports-related
Physical Exam
-
Evaluate ambulation and forward bending.
-
Perform a careful neurologic examination, including assessment of rectal sensation and function.
-
Patients may present with a hypolordotic posture.
-
Patients with a severe slip may show L5 radiculopathy.
-
Perform the limited straight-leg-raise
test: A patient with spondylolisthesis will have limited lumbar flexion
with major hamstring tightness.
Tests
Lab
Perform electromyography and nerve conduction velocities to assess L5 root compression.
Imaging
-
Conventional radiographs, including a spot lateral of L5–S1, allow assessment of the presence and degrees of spondylolisthesis.
-
Oblique views show the pars interarticularis (neck of the “Scotty dog”) and visualize the pars defect.
-
Flexion and extension views can illustrate stability, particularly for degenerative and iatrogenic slips.Table 1 Classification of Spondylolisthesis
Class Associated Risk Factors Isthmic Family history, gymnastics, football lineman Congenital Spina bifida occulta Pathologic Metastatic cancer or infection Traumatic Often associated with spinal cord injury Degenerative Seen in 6th and 7th decades of life at L4–L5 level Iatrogenic Removal of posterior restraints at prior surgery Table 2 Grade of SpondylolisthesisSpondylolisthesis Grade Percentage of Slip Grade 0 0 Grade I <25 Grade II 25–50 Grade III 51–75 Grade IV 76–100 Grade V Complete displacement
-
-
When a clear pars defect is not
visualized, and early spondylosis is suspected in an adolescent, a
technetium bone scan can be used.-
For this study, a SPECT scan should be ordered.
-
-
CT can aid in the diagnosis of occult pars interarticularis defects.
-
MRI often is not useful for identifying
spondylitic defects, but it can help in assessing the degrees of neural
compression and the hydration status of the L4–L5 disc. -
Use discography or selective blocks to assess whether the L4–L5 disc or the pars defect is a patient’s pain generator.
P.417
Pathological Findings
-
The most common finding is a defect in the pars interarticularis that resembles a fibrous union or pseudoarthrosis.
-
The fibrous mass of the pars defect sometimes PINS the L5 nerve root beneath it.
Differential Diagnosis
-
The differential diagnosis of
spondylolisthesis is extremely important because the presence of a
spondylitic defect is not necessarily the source of a patient’s pain. -
A common cause of pain in a patient with a spondylolisthesis is an L4–L5 disc herniation.
-
The differential diagnosis of back pain
should include tumor, infection, facet arthropathy, stenosis, or
degenerative disc disease.
-
General Measures
-
Children and adolescents:
-
Lumbar bracing in lordosis may be used for up to 6 months to relieve pain.
-
Nonoperative treatment: Good to excellent results in up to 91% of patients (7,8)
-
Once the patient is asymptomatic without the brace, serial radiographs may be evaluated every 1–2 years until skeletal maturity.
-
Patients for whom a 12-month regimen of
nonsurgical treatment fails or who have symptomatic high-grade slips
may require posterolateral fusions.
-
-
Adults:
-
Patients with grade 0 and grade I slips can be treated as for simple mechanical back pain.
-
Patients with more severe slips (grade II or higher) require posterior spine fusion and possible nerve root decompression.
-
Reduction of high-grade slips, the need for anterior spinal fusion, and the levels to be fused are all controversial topics.
-
Activity
-
Patients (any age) with asymptomatic grade 0 and grade I spondylolisthesis have no restrictions.
-
Symptomatic patients (any age): Activity restriction until they regain painless lumbar flexion and rotation
Special Therapy
Physical Therapy
Hamstring stretching and lumbar lordosis may relieve the
discomfort in patients with symptomatic grade 0 or grade I
spondylolisthesis.
discomfort in patients with symptomatic grade 0 or grade I
spondylolisthesis.
Medication
Medications used for children or adults should be those
typically administered for the relief of back pain: An analgesic with
or without muscle relaxant.
typically administered for the relief of back pain: An analgesic with
or without muscle relaxant.
Surgery
-
For high-grade slips and patients in whom nonoperative therapy fails, posterior spinal fusion is indicated.
-
The most common procedure is a posterolateral 1-level L5–S1 fusion (9).
-
If reduction of the spondylolisthesis is
attempted or an L5 radiculopathy is present, the L5 nerve root should
be widely decompressed. -
The addition of anterior spinal surgery:
-
Is reserved for the more severe grades
-
May increase the chance of fusion
-
May prevent postsurgical progression of the spondylolisthesis
-
Prognosis
-
Spondylolisthesis slightly predisposes an individual to problems with chronic back pain.
-
Most symptomatic low-grade slips in children and adolescents can be treated nonsurgically and lead to no long-term disability.
Complications
-
Greatly variable
-
If the slip progresses to a high grade,
compression of the cauda equina with loss of bowel and bladder function
may occur occasionally. -
Many different reduction techniques have
been described, including halo-femoral traction, cast reduction, and
open reduction and internal fixation.-
After reduction, radiculopathy secondary to L5 nerve root dysfunction can occur (10).
-
References
1. Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet 1932;54:371–377.
2. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop Relat Res 1976;117:23–29.
3. Fredrickson BE, Baker D, McHolick WJ, et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg 1984;66A:699–707.
4. Baker D, McHollick W. Spondylolysis and spondylolisthesis in children. J Bone Joint Surg 1956;38A:933–934.
5. d’Hemecourt PA, Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med 2000;19:663–679.
6. Eddy D, Congeni J, Loud K. A review of spine injuries and return to play. Clin J Sport Med 2005;15:453–458.
7. d’Hemecourt
PA, Zurakowski D, Kriemler S, et al. Spondylolysis: returning the
athlete to sports participation with brace treatment. Orthopedics 2002;25:653–657.
PA, Zurakowski D, Kriemler S, et al. Spondylolysis: returning the
athlete to sports participation with brace treatment. Orthopedics 2002;25:653–657.
8. Rubery PT, Bradford DS. Athletic activity after spine surgery in children and adolescents: results of a survey. Spine 2002;27:423–427.
9. Smith
MD, Bohlman HH. Spondylolisthesis treated by a single-stage operation
combining decompression with in situ posterolateral and anterior
fusion. An analysis of eleven patients who had long-term follow-up. J Bone Joint Surg 1990;72A:415–421.
MD, Bohlman HH. Spondylolisthesis treated by a single-stage operation
combining decompression with in situ posterolateral and anterior
fusion. An analysis of eleven patients who had long-term follow-up. J Bone Joint Surg 1990;72A:415–421.
10. Transfeldt EE, Dendrinos GK, Bradford DS. Paresis of proximal lumbar roots after reduction of L5-S1 spondylolisthesis. Spine 1989;14:884–887.
Additional Reading
King EC, Sarwark JF. Spondylolysis and spondylolisthesis. In: Sponseller PD, ed. Orthopaedic Knowledge Update: Pediatrics 2. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2002:329–339.
Puschak TJ, Sasso RC. Spondylolysis- spondylolisthesis. In: Vaccaro AR, ed. Orthopaedic Knowledge Update 8. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2005:553–563.
Codes
ICD9-CM
-
738.4 Isthmic spondylolisthesis, degenerative spondylolisthesis
Patient Teaching
-
Educate patients with a high-grade slip about looking for progressive bladder dysfunction.
-
After recovery from a symptomatic episode, new onset of bowel or bladder symptoms may indicate slip progression.
FAQ
Q: Which nerve root is most likely to be affected by a reduction and fusion of a high-grade L5–S1 spondylolisthesis?
A:
The L5 nerve root. For this reason, the L5 nerve root should be
decompressed carefully before an attempt at reduction. Also,
neuromonitoring may be used during the surgical procedure.
The L5 nerve root. For this reason, the L5 nerve root should be
decompressed carefully before an attempt at reduction. Also,
neuromonitoring may be used during the surgical procedure.
Q: What grade slip does a patient with 20% anterior translation of L4 on L5 have?
A: Grade I. (Table 2.)
