Pediatric Orthopaedic Conditions
physician’s office or an urgent/emergency care center. There is a long
list of possible causes to be considered. Important components of the
evaluation include a thorough history and a careful physical
examination (7).
-
History.
Acuteness of onset, pain, history of trauma or injury, constitutional
symptoms such as fever, malaise, chills; early morning stiffness and
motor milestone development (walked by 15–18 months). -
Past medical history. Birth history and any previous surgery, injuries, or illnesses.
-
Family History. Family history of childhood lower extremity conditions such as developmental dysplasia of the hip (DDH).
-
Physical examination.
The child should be undressed to an appropriate state. Older children
and teenagers should be provided with a gown or shorts. Toddlers and
small children can be examined in their diaper or underwear. The
physical exam should be tailored to each patient depending on the
symptoms at presentation. The physical exam of a child with a recent or
sudden onset of a painful limp or refusal to walk will be very
different from an examination of a child with a chronic, painless limp.-
An antalgic
gait is characterized by a decreased stance period on the affected limb
as well as a trunk shift over the affected limb during stance. -
Evaluation for limb length difference:
palpate the anterior superior iliac spine (ASIS) with the patient
standing. Then, with the patient supine, compare lengths of the lower
extremities with the legs extended. Also, compare lengths of the femurs
by flexing the hips and comparing the relative heights of the knees. -
Physical exam should also include the back, sacroiliac (SI) joints, and abdomen as well as the entire extremity involved.
-
Palpate the entire length of the limb.
-
Range of motion of the hip, knee, and
ankle joints. Particular attention should be paid to any erythema,
warmth, joint effusion, or focal tenderness. -
A thorough neurologic examination should also be completed.
-
-
The differential diagnosis
encompasses a broad range and depends on many factors including age,
symptoms, severity, acuteness of onset, and clinical findings on
physical exam (1,2).-
0 to 5 years old
-
Septic arthritis
-
Osteomyelitis
-
Transient hip synovitis
-
DDH
-
Legg-Calvé-Perthes disease/osteochondroses-related conditions
-
Toddler’s fracture
-
“Nonaccidental injury” (child abuse)
-
Neurologic disorders (cerebral palsy, Duchenne’s Muscular Dystrophy)
-
Tumor [neuroblastoma, acute lymphocytic leukemia (ALL), benign tumors]
-
Discitis
-
Juvenile rheumatoid arthritis
-
Congenital limb deficiency (femur, fibula, tibia)
P.68 -
-
5 to 10 years old
-
Septic arthritis
-
Osteomyelitis
-
Transient synovitis
-
Osteochondroses conditions such as Perthes, Kohler, and Osgood-Schlatter disease
-
Limb length difference
-
Tumor (ALL, Ewing sarcoma, benign bone tumors)
-
Neurologic disorders (hereditary motor sensory neuropathy)
-
Discitis
-
Juvenile rheumatoid arthritis
-
Discoid meniscus
-
-
10 to 15 years old
-
Osteomyelitis
-
Slipped capital femoral epiphysis (SCFE)
-
Osteochondroses conditions such as Perthes and Sever disease
-
Hip dysplasia
-
Patellofemoral pain syndrome
-
Tumor (osteosarcoma, Ewing’s sarcoma, benign bone tumors)
-
Osteochondritis desiccans
-
Idiopathic chondrolysis
-
-
-
Radiographic evaluation.
Anteroposterior (AP) and lateral plain radiograph (x-ray) of the entire
length of bone involved, including joint above and below the area of
concern. Referred pain describes pain
attributed to one site or location by the patient but the source of the
pain is at a different site (e.g., knee pain in a patient with an SCFE
involving the hip joint). Referred pain is frequently seen with some
childhood conditions. -
Laboratory studies.
Complete blood count (CBC) with differential, erythrocyte sedimentation
rate (ESR), and C-reactive protein (CRP). If rheumatologic conditions
or spondyloarthropathies are being evaluated, include rheumatoid factor
(RF), antinuclear antibody (ANA), anti-streptolysin (ASO) titer, Lyme
titer, and HLA B-27. -
Additional imaging studies.
-
Three-phase bone scan. Useful when source of pain is not easily localizable; sensitive but not specific.
-
Magnetic resonance imaging (MRI).
Very sensitive and specific. Able to identify areas of bone marrow
edema, soft tissue edema, or fluid collections such as abscesses. -
Ultrasound.
Useful to look for hip joint effusions, subperiosteal or soft-tissue
abscesses. May also help guide aspiration of hip joint or soft tissue
abscess.CAUTION: If septic arthritis is suspected, a joint aspiration should be performed without wasting time waiting for the availability of other additional imaging studies.
-
-
History
-
Fever, lethargy, malaise, or other constitutional symptoms
-
Pain: location, severity, duration
-
Trauma/injury
-
Onset (sudden, gradual, etc.)
-
-
Physical evaluation
-
Observe posture of patient/posture of limb
-
Inspect swelling, redness, deformity
-
Palpate entire length of extremity, abdomen, spine for sites of pain, mass, warmth
-
Range of motion (ROM) active/passive, hip, knee, ankle joints
-
-
Radiograph. Obtain AP and lateral radiographs of the area identified as the location of the patient’s pain on physical examination.
-
Laboratory examination. EXTREMELY IMPORTANT:
-
CBC with differential (may be normal)
-
C-reactive protein (CRP) (most sensitive)
-
ESR
-
Blood culture (particularly in setting of fever/sepsis)
-
-
Differential Diagnosis.
When evaluating a patient with a fever, significant pain with attempted
range-of-motion, and/or refusal to bear any weight or to walk, the
primary physician should immediately notify the orthopaedic surgeon
with whom they wish to consult. As soon as the laboratory studies and
x-rays are available, the appropriate disposition of the child can be
determined.-
Septic arthritis.
Frequently affects the hip joint in toddlers and young children; may
also affect other joints of the lower extremity (knee, ankle) or the
upper extremity (shoulder, elbow, wrist). (See VIII.B for additional information.)-
Symptoms: fever, joint pain, restricted range of motion
-
Laboratory tests: CBC may be normal, CRP and ESR are elevated
-
Radiographs: frequently normal, may suggest hip joint effusion
-
Treatment plan: immediate referral to orthopaedist for evaluation and aspiration and/or surgical drainage as well as admission/intravenous (IV) antibiotics
-
-
Transient/toxic synovitis (see VIII.C for additional information)
-
Symptoms: severity of hip pain may vary, patient usually afebrile
-
Laboratory tests: normal or minimal elevation of CBC, ESR, and CRP
-
Radiographs: normal
-
Hip ultrasound: hip effusion
-
Treatment: nonsteroidal anti-inflammatory drugs (NSAIDs)/bed rest and re-evaluate in 24 to 48 hours
-
-
Osteomyelitis. A bacterial infection of the bone (see VIII.A for more information).
-
Symptoms: fever, pain localized over long
bone adjacent to joint, pain with joint ROM is less severe than that
seen with septic arthritis -
Laboratory tests: CBC may be normal, ESR and CRP elevated
-
Radiographs: early on, normal; later
(after 10–14 days), may show a lytic lesion in area of infection. This
is frequently adjacent to the physis (growth plate). -
Treatment:
-
Admission to hospital for intravenous antibiotic therapy
-
Additional imaging (nuclear medicine vs. MRI)
-
Possible aspiration of painful area for culture
-
-
-
Fracture or other injury. If patient is too young to provide history, consider possible fracture or other significant injury.
-
History: patient fell or found lying on floor if injury unwitnessed
-
Physical exam: area of swelling, deformity, tenderness
-
Radiograph: look for fracture or physeal
separation. Children’s x-rays can be difficult to interpret because of
the presence of growth plates (physes). If necessary, consider
comparison x-rays of opposite limb. -
Treatment: splint injured limb and consult orthopaedic surgeon
-
-
SCFE (unstable/acute) (see VII.C)
-
Symptoms: adolescent child with sudden
onset of severe hip pain, inability to walk or bear weight on affected
limb. (For stable SCFE, the adolescent patient may complain of hip or
thigh pain but may be able to bear weight.) -
Physical exam: patient lies with hip flexed and externally rotated. Severe pain with any attempted ROM.
-
X-ray: obtain AP pelvis x-ray and cross-table lateral x-ray of affected hip. Femoral epiphysis is displaced relative to femoral neck.
-
Treatment: immediate referral to orthopaedic surgery for surgical stabilization.
-
-
-
Intoeing
-
Definition.
An internal foot progression angle during gait. The foot turns in
relative to the line of forward progression during walking. Intoeing is
a frequent cause for parental concern. An important part of the
evaluation should be listening to the concerns expressed by the parents
and answering their questions.
-
-
Physical examination. The patient should be undressed adequately to visualize the lower extremities.
-
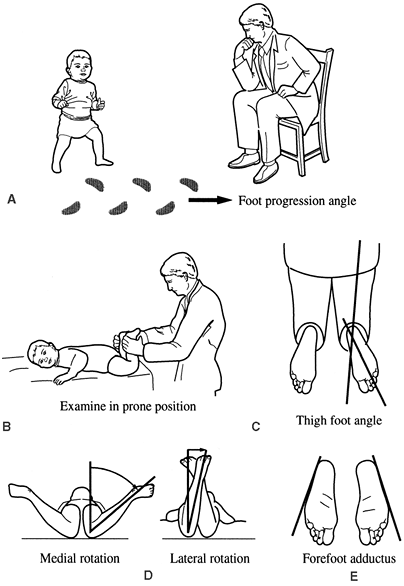
Observation: observe child walk in hallway. Note position of feet relative to line of forward progression (Fig. 5-1).
-
Examination: evaluate rotational profile. Position patient prone on examination table.
-
Hip internal (medial) and external (lateral) rotation (see Fig. 5-1D).
With patient prone and knees flexed to 90 degrees, rotate hip
internally and externally until you can feel the position of rotation
at which the greater trochanter of the hip is most prominent. Estimate
the angle between the tibia and a vertical position in order to
estimate femoral neck anteversion. -
Estimate thigh-foot axis and bimalleolar axis in order to assess tibial torsion.Thigh-foot axis: (see Fig. 5-1C) angle formed by line down the middle of the foot relative to line down length of thigh.Bimalleolar axis: angle
formed by a line passing through center of lateral malleolus and medial
malleolus relative to line perpendicular to long axis of thigh. -
Examine the plantar surface of the foot with the patient still in the prone position. Metatarsus adductus is defined as a curvature of the lateral border of the foot (see Fig. 5-1E).
-
-
-
Causes
-
Increased femoral anteversion: rotational twist in femur turns leg in while walking.
-
Internal tibial torsion: twist in tibia turns lower leg inward.
-
Metatarsus adductus: curvature of foot turns toes/forefoot inward.
-
-
Discussion.
For the majority of children, treatment of these conditions consists of
education of the parents, reassurance, and observation. Intoeing is
frequently seen in young patients and is a normal part of skeletal
development for many children. The most frequent causes are increased
femoral anteversion, internal tibial torsion, or metatarsus adductus.
Normal femoral anteversion in the newborn
is 40 to 45 degrees. For most children, this gradually remodels with
growth over time and will have improved by age 6 to 8 years old. At
skeletal maturity, normal femoral anteversion is approximately 10 to 15
degrees. Increased femoral anteversion is
femoral anteversion that persists longer than usual and is frequently
associated with increased ligamentous laxity. Children with
developmental delays or abnormal motor developmental conditions such as
cerebral palsy will also frequently exhibit increased femoral
anteversion. There are no forms of bracing, shoe-wear, or therapy that
will help femoral anteversion resolve. For the vast majority of
patients, it does not cause functional nor painful conditions later in
life and should simply be observed (3). -
Internal tibial torsion
is frequently seen as a cause of intoeing in infants and toddlers and
also gradually corrects with time. It will correct more quickly than
femoral anteversion and usually has improved by age 2 to 3 years. -
Metatarsus adductus
refers to a curvature of the lateral border of the foot. This is a
frequent finding in newborn children and is often flexible. Simple
massage and stretching can be performed by the parents for the first 6
months of life. If no improvement is seen, one may then consider a
course of treatment with reverse-last shoes or bracing. If the foot
does not appear flexible, a course of serial casting may be considered.
 |
|
Figure 5-1. Rotational profile. A: Observation of foot-progression angle. B: Examination of child in prone position to evaluate torsional deformity of the lower extremities. C: Thigh-foot angle. D: Hip internal (medial) rotation and external (lateral) rotation. E: Forefoot (metatarsus) adductus.
|
-
Terminology
-
Genu varum (“bowed legs,” genu-knee, varum/varus): the distal segment of the lower leg is aligned toward or close to the midline.
-
Genu valgum (“knock knees,” genu-knee, valgum/valgus): the distal segment is aligned away from the midline.
-
-
Physical examination.
The child should be undressed appropriately so that both lower
extremities can be evaluated. The child should be assessed standing and
again supine on the examination table. The amount of angulation at the
knee can be assessed in two ways.-
Femoral-tibial angle: angle between thigh and lower leg
-
One can also measure and record the distance between bony landmarks.
-
Intercondylar distance (genu varum): the distance between the medial femoral condyles of the knees.
-
Intermalleolar distance (genu valgum): the distance between the medial malleoli of the ankles.
-
-
-
Radiographic evaluation. For either genu varum or genu valgum, standing AP hip to ankle radiographs of both lower extremities should be obtained. The mechanical axis as well as the anatomic axis of the lower extremity is measured. In young children with genu varum, the metaphyseal-diaphyseal angle is measured.
-
Causes
-
“Physiologic”: part of the normal
development. Most children who are referred for evaluation have a
physiologic form of bowing. Children undergo an evolution of their
lower extremity alignment during the first 6 years of life.-
Birth to age 2: genu varum
-
Age 2 to age 4: genu valgum
-
Age 4 to age 6: continued gradual correction into relatively “mature” alignment of mild genu valgum anatomically (4).For children who do not fit this pattern, are of
adolescent age, or appear to have asymmetric alignment of their lower
extremities, other possible causes should be explored.
-
-
Tibia vara (Blount disease)
is an abnormal varus alignment of the knee due to altered growth of the
medial portion of the proximal tibial physis. There is an infantile form for children older than age 2 years and an adolescent form, frequently associated with obesity. -
Other causes could include:
-
Coxa vara (a congenital varus deformity of the proximal femur)
-
One of the various forms of skeletal dysplasia.
To help evaluate this, obtain additional radiographs. An x-ray of the
hands, shoulders, spine, hips, and knees can help evaluate other
potential sights of growth abnormalities. -
One of the forms of rickets
(such as familial hypophosphatemic rickets). To evaluate this further,
consider obtaining laboratory studies including vitamin D; parathyroid
hormone (PTH); alkaline phosphotase; calcium, magnesium, and phosphorus
levels; and consider obtaining an endocrinology consultation.
-
-
-
Treatment
-
For
physiologic conditions, treatment usually consists of observation.
Inform the patient’s parents of the expected course and communicate the
findings and recommendations to the patient’s primary physician.
Continued observation can be performed during routine well-child
checks. If the child’s alignment varies from what is expected, the
child can return for reevaluation. -
Children
with conditions which do not fit the typical “physiologic” pattern
should be referred for further evaluation. Further treatment consists
of establishing the underlying cause as well as developing an
appropriate treatment plan. After the diagnosis has been determined,
treatment may consist of:-
Observation
-
Hemiepiphyseal stapling
-
Hemiepiphysiodesis
-
Tibial and/or femoral osteotomyThese should be performed by physicians who are well
experienced in planning and performing the appropriate procedures and
are able to provide follow-up care.
-
-
-
Clubfoot (talipes equinovarus)
-
Description.
A congenital deformity of the foot comprised of ankle equinus, hindfoot
varus, and adduction and supination of the midfoot and forefoot. The
foot “turns in” and “curves under” compared with the normal. -
Incidence.
1 in 1,000 live births, unilateral in 60% of patients, and the ratio of
boys to girls is 2:1. There may be a positive family history. -
Etiology. Multiple theories exist with the most likely cause being multifactorial.
Theories include arrested fetal development, abnormal intrauterine
forces, abnormal muscle fiber type, abnormal neuromuscular function,
and germ plasm defects. -
Prenatal considerations include breech position, large birth weight, and oligohydramnios.
-
Associated conditions include arthrogryposis, myelodysplasia, congenital limb anomalies, and various syndromes.
-
Physical examination.
A careful evaluation should include not only examination of the child’s
feet, but also the child’s upper extremities, back, spine, and hips in
order to look for other associated conditions. Examination of the foot
should include evaluation of the ankle dorsiflexion, the hindfoot
position, curvature of the lateral border of the foot, and the forefoot
position as well as an assessment of the degree of flexibility of the
foot. Deep posterior and medial creases are usually present. -
Radiographic evaluation.
Radiographs in the newborn period are not useful because the tarsal
bones are not well ossified. Radiographs may be useful after age 3
months for planning or evaluating surgical treatment. They are ordered
less often in nonoperative treatment as the physical examination is
more useful for clinical decision making. When x-rays are ordered, the
most useful images are an AP view and a lateral view in a position of
maximum dorsiflexion. Kite angle is the
angle subtended by the long axes of the calcaneus and the talus on the
AP view. This angle is normally between 20 and 40 degrees. In the
clubfoot, this angle is less than 20 degrees with relative parallel
alignment of the talus and calcaneus. The relationship of the talus and
calcaneus should also be assessed on the lateral view. Again, in the
clubfoot, this shows relative parallel alignment compared with the
normal foot. -
Treatment.
The goals of treatment are to achieve a plantigrade, flexible, painless
foot. In the early half of the 20th century, Kite published high levels
of satisfactory results with his casting technique. The later half of
the 20th century saw the emergence and rise in popularity of the
surgical treatment of clubfoot as described by such authors as Turco,
Carroll, Crawford, Simmons, and McCay (5). The
dawn of the 21st century has seen renewed interest in the role of
nonoperative treatment using the method developed by Ponseti. His
experience has produced impressive results at long-term follow up and
is gaining more widespread acceptance and support (6).
-
-
Flat feet (pes planus)
-
Definition. Feet in which the medial longitudinal arch is absent resulting in hindfoot valgus and forefoot supination.
-
Presentation
-
Parental concerns regarding the appearance and shape of the foot
-
Pain
-
Difficulties with shoe wear
-
-
Patient history.
It is important to note when the foot position was first noticed,
whether the foot condition causes problems with function or pain, and
any family history of ligamentous laxity or flatfeet. -
Physical examination
-
Observe the foot while the patient stands and walks. Note presence or absence of medial longitudinal arch.
-
Inspect the foot for calluses and pressure areas over bony prominences.
-
When the patient is standing, have him or
her stand on tiptoe to assess mobility of the hindfoot. If the hindfoot
moves from valgus when plantigrade to varus with standing on tiptoe and
the foot forms an arch when on tiptoe, then the foot is “flexible.” If it does not correct, it is considered “rigid.” -
Assess the length of the Achilles tendon by examining the range of ankle dorsiflexion.
P.74 -
-
Radiographic examination.
For young children with a painless, flexible flat foot, no radiographs
are indicated. If the flat foot is painful or rigid, then standing AP,
lateral, and oblique radiographs of the foot should be obtained. -
Flexible flat feet.
The flexible flat foot is a relatively common condition, although the
true incidence is unknown. Most young children start with a flexible
flat foot before developing a medial longitudinal arch during the first
decade of life. Most children are symptom-free, and no treatment is
warranted. For the older child or adolescent with a flexible flat foot
who experiences aching or discomfort associated with particular
activities, one may wish to use an orthotic to support the arch. If the
foot is flexible but there is a contracture of the Achilles tendon, one
should prescribe a course of physical therapy for a heelcord stretching
program. If the patient with an Achilles tendon contracture remains
symptomatic despite physical therapy, one may consider injection of
Botox into the calf muscle, possibly in conjunction with a stretching
cast. For patients that fail conservative therapy, some authors support
surgical correction of the hind foot valgus deformity in conjunction
with lengthening the tight gastrocnemius (7). This is rarely necessary in the growing child with a flexible flat foot deformity. -
Rigid flat feet. The most common cause for a rigid flat foot is a tarsal coalition. This is an incomplete separation of the tarsal bones during fetal development. The two most common types are the calcaneonavicular and the talocalcaneal
coalition. The calcaneonavicular coalition may be best seen on the
oblique foot radiograph. The talocalcaneal coalition may be seen on an
axial (Harris) radiograph of the foot. If further radiographic imaging
is required, a computed tomography (CT) scan of both feet is the study
of choice. -
If tarsal coalition has been excluded as the cause for the rigid flat foot, other possible causes include a congenital vertical talus, juvenile rheumatoid arthritis (JRA) involving the subtalar joint, osteochondral fractures of the subtalar joint, or neuromuscular conditions.
-
Treatment of
the rigid flat foot. The goal of treatment is to achieve a pain-free,
asymptomatic foot. Approximately 75% of patients with tarsal coalitions
are asymptomatic. Frequently, the onset of pain coincides with the
transition of the coalition from a fibrous or cartilaginous junction to
a bony bar. For the calcaneonavicular bar, this occurs around ages 8 to
12 years old; for the talocalcaneal bar, this usually occurs between 12
and 16 years of age. Nonoperative treatment consists of applying a
short-leg walking cast for 6 weeks followed by use of a molded
orthotic. This results in a resolution of the patient’s symptoms in a
large number of patients. For patients who do not respond to casting
treatment or for whom the symptoms recur, surgery is indicated.
Operative treatment usually consists of excision of the coalition along
with interposition of fat, muscle, or tendon to prevent recurrence. For
patients with a talocalcaneal coalition that comprises more than 50% of
the subtalar joint surface, some authors have questioned the role of
resection of the coalition. For patients with severe degenerative
arthrosis of the subtalar joint or persistent pain following previous
resection, a triple arthrodesis should be considered (8,9).
-
-
Bunions (hallux valgus)
-
Definition.
An abnormal bony prominence of the medial eminence of the first
metatarsal associated with a hallux valgus deformity of the great toe.
It is frequently associated with a medial deviation of the first
metatarsal (metatarsus primus varus). -
Patient history.
These patients are most often adolescent or teenage girls with
complaints of pain over the medial eminence, difficulty with shoe wear,
or concerns regarding appearance. There may be a positive family
history. -
Physical examination.
Clinically assess presence of hindfoot valgus and presence of a
coexisting flat foot in addition to presence and severity of hallux
valgus deformity. Evaluate degree of angulation as well as rotation of
great toe. -
Radiographic evaluation.
Standing AP and lateral radiographs of the foot are recommended. On the
AP radiograph, one can assess the following parameters:-
First-second intermetatarsal angle (normal is <9 degrees)
-
First metatarsal-phalangeal angle (normal is <15 degrees)
-
Length of the first metatarsal
-
Congruency of first metatarsophalangeal (MTP) joint
-
-
Treatment. It is important to distinguish the functional
problems that the patient is experiencing as well as the patient’s and
the parents’ concerns. In the adolescent patient in whom the primary
concern is the appearance of the foot, every effort should me made to
educate and counsel the family. For patients with a symptomatic hallux
valgus deformity, strong consideration should be accorded to postponing
any surgical treatment until skeletal maturity is reached because there
is a high recurrence rate of bunions in adolescent patients. If surgery
is considered, careful examination of the foot is necessary to correct
all of the underlying deformities, thus decreasing the risk of
recurrence and increasing the likelihood of patient satisfaction. For
patients with an underlying flexible flat foot condition, initial
treatment should consist of a custom-molded, flexible medial-arch
supporting foot orthotic. This will frequently correct the foot
deformity and improve the hallux valgus deformity as well. -
Surgical options. There are numerous surgical options.
-
Soft-tissue procedures
-
Medial capsule advancement of first MTP joint
-
Excision of the medial eminence of the metatarsal head
-
Adductor hallucis release
-
-
Bony procedures
-
Distal first metatarsal osteotomy (Chevron, Mitchell)
-
Proximal first metatarsal osteotomy
-
First metatarsal double (proximal and distal) osteotomy as described by Peterson (10)Geissele reported that the reduction of the
intermetatarsal angle is the factor that correlates most highly with
both decreased risk of recurrence of angular deformity and with patient
satisfaction (11).
-
-
P.75 -
-
History
-
Trauma/injury
-
Swelling of joint
-
Locking/buckling of knees
-
Location of pain
-
Association of pain with specific activities (running, descending stairs, sitting)
-
-
Physical evaluation
-
Knee ROM
-
Hip ROM (remember referred pain from hip)
-
Effusion of knee joint
-
Joint line tenderness
-
Tenderness over patella/tibial tubercle
-
Assess ligamentous stability
-
-
Radiograph examination.
Obtain AP/lateral radiographs of knee to evaluate for any bony
abnormalities. For evaluation of patella alignment or patella-related
pain, obtain AP/lateral and “merchant” view or “sunrise” view of knee.
For concern regarding possible locking or catching of the knee such as
with osteochondritis dessicans (OCD) (see below), obtain AP/lateral and
“notch” view radiographs of knee. -
Differential Diagnosis
-
Patellofemoral pain syndrome
-
Definition.
Previously termed “chondromalacia patellae” or “anterior knee pain
syndrome,” it describes a condition in which the pain is attributed to
the patellofemoral joint. It typically is characterized by pain
localized to the front of the knee. -
Patient history.
Adolescent girls are affected more often than boys. Symptoms may occur
gradually or after previous knee injury; usually not associated with
specific trauma. There are no symptoms of locking or buckling. Pain is
frequently associated with activities such as walking, running,
descending stairs, and sitting for prolonged periods. -
Physical examination.
One should include a thorough examination of the knee, paying
particular attention to evaluate tracking of the patella, patella
mobility medially and laterally, and Q-angle (alignment of extensor
mechanism measured by angle of line from ASIS to patella and line from
patella to tibial tubercle). Also assess the lower extremity rotational
profile (see III.C.2) -
Radiographs.
AP, lateral, and patella views should be obtained to evaluate for
evidence of patellar tilt as well as to rule out other potential
sources of knee symptoms such as OCD and bony lesions. -
Treatment.
Most patients with patellofemoral knee pain respond to a course of
conservative treatment consisting of hamstring stretching in addition
to closed-chain quadriceps [specifically vastus medialis obliquus (VMO)
strengthening]. This may be augmented by use of a patellar-taping
program or a patella-stabilizing neoprene knee sleeve in some patients.
-
-
Acute patella dislocation
-
Patient history.
Patients may have experienced a traumatic or a nontraumatic patella
subluxation or dislocation. The patella dislocates laterally. The
patient may be tender over the medial retinaculum and a joint effusion
may be present. -
Radiographic evaluation.
AP/lateral/patella views of the knee should be closely evaluated for
any evidence of osteochondral fragments. The patella may knock off an
osteochondral fragment from the lateral femoral condyle within the
process of dislocating or relocating. -
Treatment. If
osteochondral fragments are present, the knee should be evaluated
arthroscopically. Very large fragments may need to be replaced and
internally fixed; smaller fragments may simply be removed. If no
osteochondral fracture is identified, treatment may consist of a short
period of immobilization with a soft-sided knee immobilizer followed by
a program of quadriceps strengthening exercises.
-
-
Chronic patella instability
-
Patient history.
Some patients may have recurrent patella subluxation/ dislocation
episodes. The initial course of treatment should consist of physical
therapy for quadriceps strengthening exercises. If these are not
successful in achieving improvement of the instability, surgical
stabilization may be indicated (12).
-
-
Osgood-Schlatter disease
-
Presentation.
One in the family of conditions known as “osteochondroses,” this is an
inflammation at the junction of the patellar tendon to the tibial
tubercle. It most often occurs in girls aged 10 to 12 and boys aged 12
to 14. The patient usually complains of painful swelling over the area
of the tibial tubercle as well as pain associated with activities such
as running or jumping sports. Sinding-Larsen-Johansson syndrome is a related condition arising at the proximal or distal ends of the patella. -
Treatment. Consists of hamstring and quadriceps stretching, NSAIDs, periodic ice to the area, and modification of activities.
-
-
Discoid meniscus
-
Presentation.
Patients with a discoid meniscus may have knee pain as early as age 4
years. Most patients are first seen between ages 6 and 12 years or
older. The incidence varies and is estimated to be from 3% to 5% in
Anglo-Saxons and as much as 20% in Japanese. The majority of cases
involve the lateral meniscus. Patients usually have complaints of
snapping or popping of the knee. -
Physical examination. Examination of the knee may reveal snapping with flexion of the knee. Unstable menisci may snap or pop in extension.
-
Classification.
There are three principal types. Type I is stable, complete. Type II is
stable, incomplete. Type III is unstable because of the absence of the
meniscotibial ligament. -
Treatment.
For stable discoid lateral meniscus, arthroscopic sculpting of the
meniscus to a normal configuration is indicated. If it is unstable,
stabilization with a capsular suture is recommended (13).
-
-
Ostochondritis Dessicans (OCD)
-
Definition.
This is a condition of unknown etiology that results in vascular
changes of the subchondral bone in the femoral condyle which may lead
to fragmentation or separation of the fragment along with the overlying
cartilage. It most often occurs in adolescents and is more often in
boys than in girls. -
History
-
Nonspecific knee pain
-
Knee swelling after activities
-
No history of acute trauma or injury
-
With or without catching or locking of knee
-
-
Physical examination. Mild swelling may be present, tenderness over femoral condyle.
-
Radiographic examination.
AP/lateral/notch views of knee; notch view may show lesion most
effectively. Lateral view may also show lesion on posterior aspect of
femoral condyle. -
MRI: assess “stability” of fragment based on continuity of articular cartilage and subchondral bone.
-
Treatment depends on age of patient and stability of fragment.
-
Skeletally immature patient with stable lesion:
-
brief period of immobilization
-
restriction of activities
-
-
Patient near or at skeletal maturity or
unstable lesion: consider arthroscopic evaluation, possible drilling
and internal stabilization.
-
-
-
Miscellaneous
-
Referred pain
-
Definition. Pain originating in one location but localized by the patient as arising from a nearby, different location.
-
Many children complain of lower extremity
pain, and the clinician’s challenge is to determine the source of the
symptoms. Children and adolescents (as well as adults) may have
referred pain in which disorders occurring at one site present with
pain at a distal location. A classic example is the overweight
adolescent boy with knee pain. An exhaustive evaluation of the knee
reveals no obvious cause of his symptoms. However, a careful and
thorough examination of the entire lower extremity reveals a SCFE of
the hip. To avoid the common pitfalls, one must consider all of the
diagnostic possibilities and complete a thorough evaluation.
-
-
Tumors
-
Definition.
Patients with leukemia or bone tumors often present with bone or joint
pain. If history and physical exam are not consistent with other causes
of pain, consider possible malignancies including
P.78
Ewing
sarcoma, osteogenic sarcoma, leukemia, lymphoma, neuroblastoma, etc.
Obtain laboratory tests and radiographs/imaging studies appropriately.
-
-
P.77 -
-
Developmental Dysplasia of the HIP (DDH)
-
Definition. A
spectrum of disorders ranging from complete dislocation of the femoral
head to a reduced hip joint with acetabular dysplasia. -
Incidence. Approximately 1 in 1,000 live births.
-
Risk factors:
include first born, female, breech position in utero, oligohydramnios,
and a positive family history. It has also been associated with other
congenital conditions including congenital muscular torticollis,
metatarsus adductus, and clubfeet. -
Physical examination.
In the newborn child or young infant, physical examination should start
with a careful evaluation of the other parts of the child other than
the hips, including the spine, neck, and upper and lower extremities.
Then, focus examination on the hips, trying to detect any evidence of
instability. The clinical tests performed include the Barlow/Ortolani
and Galeazzi tests. The Barlow and Ortolani
tests are performed with the clinician stabilizing the pelvis with one
hand and grasping the child’s femur with the other, placing the thumb
over the medial femoral condyle and the long finger over the greater
trochanter. The hip is flexed to 90 degrees and held in neutral
abduction. The Ortolani maneuver consists of abducting the hip and
trying to detect the “clunking” sensation of the dislocated femoral
head relocating into the acetabulum. Likewise, the Barlow test consists
of two maneuvers. The first consists of adducting the hip with gentle
longitudinal pressure to provoke the hip to dislocate or subluxate. The
second maneuver is the same as that described for the Ortolani maneuver
to achieve reduction of the dislocated hip. The Galeazzi
test consists of comparing the height of the knees with the hips flexed
to discern any apparent femoral shortening. One should also check for
symmetric degrees of hip abduction as well as for asymmetry of the
perineal skin folds. Finally, DDH can be bilateral, which can be easily
missed clinically because there is no apparent asymmetry. These
children may first come to attention after walking age, with increased
lumbar lordosis, limb length difference, or a “waddling gait.” -
Radiographic evaluation.
In the young infant, ultrasound is the modality of choice to detect any
evidence of hip abnormality. The ultrasound allows a static assessment
of acetabular development (alpha and beta angles) and percentage of
femoral head coverage as well as dynamic assessment of femoral head
stability with stress maneuvers. In children older than 6 months, plain
AP radiographs are sufficient. -
Treatment
-
Age 0 to 6 months. In the newborn child up to 6 months of age, treatment consists of abduction bracing, usually performed with a Pavlik harness.
This is usually applied at the time the instability is noted. It may
also be used for children with a clinically stable hip but who have
significant acetabular dysplasia noted on ultrasound. Moreover, the
adequacy of the reduction or positioning in the Pavlik harness can be
evaluated with ultrasound. There have been several reports in the
literature of “Pavlik harness disease” in which the femoral head was
not adequately reduced in the acetabulum while in the harness, leading
to progressive deformation of the posterior wall of the acetabulum and
exacerbation of the dysplasia. If an adequate, concentric reduction of
the femoral head cannot be achieved by 4 weeks after the harness has
been applied, treatment with the Pavlik harness should be abandoned (14,15). -
Age 6 to 18 months or the child who fails Pavlik harness treatment.
Treatment for this group is aimed at achieving a satisfactory,
congruent, stable reduction. This is achieved by performing either a closed or an open reduction. Historically, traction has been employed preoperatively in
P.79
order to decrease the risk of avascular necrosis of the femoral head
after closed reduction. An arthrogram is frequently performed at the
time of the closed reduction. If the hip is noted to have a narrow
“stable zone,” a limited adductor release may be performed to improve
stability. If a concentric reduction is not achievable or if excessive
force is required to maintain the reduction, then an open reduction may
be performed. Popular methods for performing the open reduction include
an anterolateral approach and the medial approach (14). -
Age older than 18 months.
Some authors still advocate a trial of preoperative skin traction
followed by attempted closed reduction. Alternatively, one can consider
open reduction performed in conjunction with femoral shortening to
reduce soft-tissue tension and thereby decrease risk of avascular
necrosis. If significant acetabular dysplasia is present, a pelvic
osteotomy may also be performed (16). -
Secondary procedures.
For older children with persistent acetabular dysplasia or persistent
hip subluxation, secondary procedures may take the form of femoral or
pelvic osteotomies. Adolescents or young adults may present with hip
pain from previously undiagnosed dysplasia. They may be candidates for
a redirectional pelvic osteotomy.
-
-
-
Legg-Calvé-Perthes disease
-
Definition. Idiopathic avascular necrosis to the femoral head in children.
-
Presentation.
Most often affects children aged 4 to 8 years; however, it may affect
children as young as 2 or as old as 12 years. The ratio of incidence in
boys to girls is 4:1. The disease may be bilateral in 10% of patients.
Patients frequently have younger skeletal age than cohorts. Frequently,
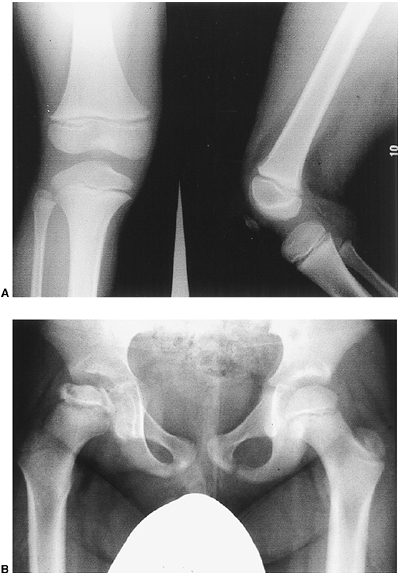
the disease presents as a painless limp (Fig. 5-2). -
Etiology: idiopathic. It has been associated with abnormalities of thrombolysis as well as deficiencies of protein C, protein S, or thrombolysin.
-
Differential diagnosis.
If bilateral hip involvement is present on radiograph, then other
possible etiologies should be excluded, including renal disease,
hypothyroidism, multiple epiphyseal dysplasia or spondyloepiphyseal
dysplasia, systemic corticosteroid use, storage disorders, and
hemoglobinopathies. -
Stages.
Waldenström originally described evolutionary stages that the disease
course follows. These have been modified from the original description
to include the following:-
Initial stage. Femoral head appears sclerotic early in the course of the disease.
-
Fragmentation stage.
Presence of subchondral fracture (Salter sign) is hallmark of onset.
The femoral head develops “fragmented” appearance on radiograph as
necrotic bone undergoes resorption. -
Reossification stage. There is evidence of healing; coalescence of femoral head fragmentation begins to occur.
-
Healed stage. Reossification is complete. Femoral head returns to predisease density. Any remaining deformity is permanent.
-
-
Classification systems. To describe and to compare the results of treatment, various classification systems have been described.
-
Catterall. Four-part system (I–IV) based on the amount of femoral head involvement
-
Salter-Thompson. Two part system (A, B) simplified to less than 50% or greater than 50% involvement of femoral head.
-
Herring:
Recently revised to a four-part system (A, B, BC, C) based on height of
lateral “pillar” (lateral one third of femoral epiphysis).
-
-
Treatment.
For patients with Legg-Calvé-Perthes disease, it is important to
determine which patients will benefit from treatment as well as how to
treat them.Risk factors for a poor prognosis include:-
Older age at presentation (>8 years old)
-
Greater degree of involvement of the femoral head using any of the above classification systems.
![]() Figure 5-2. A 6-year-old boy with a 1- to 2-month history of limping and right knee pain. A: Radiographs of the knee are normal. B: An AP pelvis radiograph reveals changes in the right hip consistent with Legg-Calvé-Perthes disease.P.80P.81The hallmarks of treatment consist of:
Figure 5-2. A 6-year-old boy with a 1- to 2-month history of limping and right knee pain. A: Radiographs of the knee are normal. B: An AP pelvis radiograph reveals changes in the right hip consistent with Legg-Calvé-Perthes disease.P.80P.81The hallmarks of treatment consist of:-
Maintaining hip range of motion
-
“Containment” of the femoral head in the acetabulum.For younger patients or patients with less involvement
of the femoral head, treatment may consist primarily of NSAIDs,
physical therapy, and restriction of activities to maintain hip range
of motion. For older children, especially those who have more
involvement of the hip (and therefore a worse prognosis), treatment may
consist of surgical containment of femoral head by femoral and/or
pelvic osteotomies (17). Abduction bracing was used historically but now is used very rarely.
-
-
-
-
Slipped Capital Femoral Epiphysis (SCFE)
-
Definition. A
disorder of the upper femur in which there is a separation (acutely or
chronically) of the femoral epiphysis from the femoral neck through the
region of the physis (growth plate). The femoral head becomes
positioned posterior and inferior relative to the femoral neck. -
Incidence.
Approximately 3 in 100,000; boys more frequently than girls. Bilateral
involvement occurs in between 20% and 60% of cases. SCFE is seen most
frequently in boys aged 12 to 16 years and in girls aged 10 to 14
years. SCFE is associated with obesity, with more than half of affected
individuals weighing greater than the 95th percentile. (Note: Not all
patients with SCFE are obese.) Patients with an underlying hormonal or
endocrine disorder have an associated increased risk for development of
SCFE. For patients with an unusual presentation such as atypical age
(before age 10), bilateral involvement at presentation, or with other
signs of possible endocrine abnormalities, a careful evaluation for
endocrine disorders including hypothyroidism, hypopituitarism or
hypogonadism should be conducted. -
Classification
-
Temporal. One
method of classification is based on duration of symptoms. Acute is
less than 3 weeks, chronic is greater than 3 weeks, and
acute-on-chronic is a sudden exacerbation of subclinical symptoms of
long-standing duration. -
Stability. This classification system has gained greater popularity because it appears to be clinically more useful. A patient with a stable SCFE is able to walk without assistance, with mild pain, or a slight limp. Patients with an unstable SCFE are unable to walk or to bear weight. Unstable SCFEs are associated with a higher rate of complications (18).
-
Displacement.
Classified according to the amount of displacement of the femoral head.
This may be represented as a percentage of the femoral neck width or as
an angular value measured by the lateral head-shaft angle.
-
-
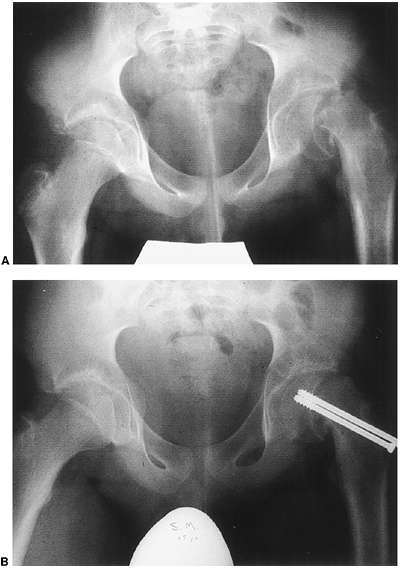
Treatment. The most widely recommended form of treatment is surgical stabilization with percutaneous pinning in situ. For a stable SCFE, this can usually be accomplished with a single, cannulated screw inserted under fluoroscopic control (19).
The aim of the procedure is to insert the screw perpendicular to the
femoral head in both the AP and lateral planes with close attention to
avoid penetrating the femoral head and entering the hip joint. In cases
of an unstable SCFE, a second screw may be inserted to further
stabilize the femoral head (Fig. 5-3). -
Complications. The primary complications associated with SCFE are avascular necrosis and chondrolysis. Avascular necrosis is uncommon with stable SCFE treated with pinning in situ.
There is a greater incidence of avascular necrosis associated with
unstable SCFE. A vigorous attempt at reduction of an unstable SCFE
should NOT be performed. Chondrolysis is a
gradual loss of the joint space following stabilization of the SCFE. It
has been associated with treatment with one or more pins as well as
with a spica cast in which no internal fixation was used.
-
 |
|
Figure 5-3. Slipped capital femoral epiphysis. A: A 13-year-old boy with a severe, unstable left SCFE. B: Two cannulated screws were inserted for stabilization.
|
-
Osteomyelitis
-
Definition. A bacterial infection of the bone.
-
Etiology.
Bacterial seeding can occur through several methods: direct inoculation
(open fractures, penetrating wounds), local extension from adjacent
sites, or hematogenous spread from distant sites. Children are
skeletally immature and have physes at the ends of their long bones.
The metaphyseal region of the bone just below the physis is a frequent
location for osteomyelitis to occur. -
Presentation.
Patients may present with pain, limping, or refusal to walk or bear
weight on the affected lower extremity. Constitutional symptoms of
fever, malaise, and flu may or may not be present. One should inquire
about immunization status as well as history of recent illnesses [e.g.,
otitis media, chicken pox, strep pharyngitis, upper respiratory tract
illness (URTI)]. -
Physical examination.
Site of involvement may or may not be easy to identify, particularly in
younger patients. Careful palpation of entire extremity and the
metaphyseal regions in particular is important. All joints should be
placed through a range of motion. Inspect for areas of redness,
swelling, or warmth. -
Laboratory studies.
CBC with differential, ESR, CRP, and blood cultures are helpful in
making the diagnosis. The CRP has been recognized as a more rapidly
responsive test than the ESR, increasing more quickly early in the
evolution of the condition and declining more rapidly in response to
treatment. If the diagnosis remains unclear, consider other diagnostic
possibilities such as JRA, Lyme arthritis, and poststreptococcal
arthritis. -
Radiographic studies.
Plain radiographs of the affected area should be obtained. In
osteomyelitis they may frequently be normal for the first 7 to 14 days.
However, the radiographs may also be useful to rule out other
diagnostic possibilities. In patients with normal radiographs in whom
the diagnosis is still unclear, a technetium bone scan is a sensitive
test for acute osteomyelitis. It is particularly helpful in cases
involving the pelvis, proximal femur, and spine. MRI is also very
sensitive and has the added benefit of having greater soft-tissue
detail allowing assessment of marrow involvement, soft-tissue extension
or abscess formation, and presence of joint effusions. However, an MRI
may require significant sedation or anesthesia for younger patients. -
Aspiration.
In patients with an identified focus of infection, an attempt at
aspiration is recommended by many authors to identify the organism.
This may be done with sedation in the emergency department or the
fluoroscopic suite or, alternatively, under anesthesia in the operating
room. -
Organisms. On the basis of patient age:
-
Younger than 1 year old
-
Staphylococcus aureus
-
Group B Streptococcus
-
Escherichia coli
-
-
1 to 4 years old
-
S. aureus
-
Haemophilus influenzae
-
-
Older than 4 years old
-
S. aureus
-
-
Adolescent
-
S. aureus
-
Neisseria gonorrhoeae
-
-
-
Treatment.
Appropriate intravenous antibiotic based on culture or most likely
organism. Duration of antibiotic coverage is typically 6 weeks. After 2
to 3 weeks of IV treatment, the patient may be switched to oral
antibiotics if the following criteria are met: (a) the organism has
been identified, (b) there is
P.84
a
satisfactory oral antibiotic to which the organism is sensitive, (c)
the child will take the oral antibiotic, and (d) satisfactory serum
levels can be achieved with oral therapy (20). -
Surgical treatment.
If the patient does not respond to antibiotic treatment after the first
24 to 48 hours, consider the possibility of a subperiosteal or
intraosseous abscess as well as other diagnostic possibilities.
Consider surgical drainage of abscess or intramedullary canal if
necessary (21).
-
-
Septic arthritis (22)
-
Definition. An infectious arthritis of a joint, usually bacterial in nature.
-
Etiology.
Most frequently, it occurs as a result from adjacent osteomyelitis in
which the metaphyseal portion of the bone is intraarticular (e.g., hip,
shoulder, elbow, ankle). When pus from metaphysis decompresses itself
through cortex, joints can become infected. Infection is also possible
through hematogenous spread or direct inoculation. -
Joints most commonly involved: knee (41%), hip (23%), ankle (14%), elbow (12%), wrist (4%), and shoulder (4%).
-
Presentation.
Young children usually refuse to walk or bear weight on the lower
extremity. The child will usually be febrile and may show signs of
sepsis. If infection is in the upper extremity, children refuse to use
the affected extremity. Septic arthritis may also occur in the newborn
child; babies in the neonatal intensive care unit (NICU) may present
with pseudoparalysis of the affected limb with failure or refusal to
move it. -
Physical examination.
If the joint involved is superficial, classic signs of joint redness,
swelling, and warmth are present. However, if the joint is not
superficial (hip, shoulder), no visible abnormality may be detectable.
However, the patient will hold the affected limb in a position of
maximum comfort (e.g., keep the hip in flexion and external rotation).
Any attempt at passive range of motion is painful and restricted
because of guarding. -
Laboratory studies
include CBC with differential, ESR, CRP, and blood culture. The CRP and
ESR will become significantly elevated. The CBC may remain normal. -
Radiographic studies.
Plain radiographs of the affected joint should be obtained to look for
any evidence of bony destruction or erosions. For patients with
suspected hip pain, an ultrasound of the hip may confirm the presence
of a hip joint effusion. In some institutions, aspiration is performed
under ultrasound guidance. -
Joint aspiration
is mandatory to confirm the diagnosis. Joint fluid should be sent for
cell count, Gram stain, and culture and, if quantity permits, glucose
and total protein. If the patient is a teenager in whom gonococcal
infection is suspected, the laboratory should be notified in order to
perform cultures on chocolate agar in addition to the routine media.
The Gram stain may be positive for bacteria in only approximately 50%
of patients. The cell count most often has greater than 50,000 white
blood cells (WBCs) and/or greater than 90% polymorphonuclear
neutrophils (PMNs). -
Organisms. On the basis of patient age:
-
Younger than 1 year old
-
S. aureus
-
Group B Streptococcus
-
E. coli
-
-
1 to 4 years old
-
S. aureus
-
H. influenzae (less common now with H. influenzae B vaccination)
-
Group A Streptococcus
-
Streptococcus pneumoniae
-
-
Older than 4 years old
-
S. aureus
-
Group A Streptococcus
-
-
Adolescent
-
S. aureus
-
N. gonorrhoeae
-
-
Less common organisms include Kingella kingae, Salmonella, and Neisseria meningitidis.
P.85 -
-
Treatment. In
patients suspected of septic arthritis, treatment consists of surgical
incision and drainage of the affected joint. Surgical decompression of
the adjacent bone may also be indicated if there is evidence of an
intraosseous abscess. Intravenous antibiotics should be administered
once intraoperative cultures have been obtained. Empiric coverage
should be started initially based on the most likely organism involved.
Once culture and sensitivities have been identified, antibiotic
coverage can be tailored accordingly. The duration of antibiotics is
usually 4 to 6 weeks. An initial course of intravenous antibiotics is
followed by oral therapy until the patient’s symptoms and laboratory
studies have returned to normal.
-
-
Transient synovitis
-
Definition. An inflammatory, noninfectious process resulting in joint swelling and pain.
-
Presentation.
Transient synovitis most frequently occurs in young children aged 3 to
8 years. Patients often may have had a recent upper respiratory tract
illness or other viral illness in the 2 to 3 weeks before onset of
symptoms. Patients are usually afebrile with a history of several days
of pain or limping. The physician must differentiate between transient
synovitis and a truly infectious process such as septic arthritis or
osteomyelitis. -
Laboratory studies. CBC with differential, ESR, and CRP are usually within the normal range.
-
Radiographic studies.
Plain radiographs are usually normal or may show evidence of a joint
effusion. Ultrasound is helpful for confirming the presence of a joint
effusion. -
Aspiration.
Because the clinician is often confronted with having to exclude septic
arthritis, joint aspiration can be helpful in order to examine the
joint fluid. A Gram stain, cell count, and culture should be obtained.
The Gram stain should be negative and the cell count should have
between 5,000 and 15,000 WBCs with less than 25% PMNs. -
Treatment.
The primary treatment objective in the treatment of transient synovitis
is to ensure that septic arthritis has been excluded. Once septic
arthritis is excluded, then the condition can be treated expectantly
with reduction in activity, NSAIDs, and careful observation (23).
-
-
Evaluation of the patient with back pain
-
History
-
Location of pain (neck/thoracic/lumbar)
-
Radiation of pain into lower extremities
-
Associated symptoms such as numbness, tingling, weakness, change in bowel or bladder function, pain at night, etc.
-
Onset of pain (acute/gradual)
-
Frequency and duration of symptoms
-
Any improvement with NSAIDs/aspirin
-
Is patient involved in athletic
activities that are associated with repetitive hyperextension of back
such as figure skating, gymnastics, dance, football (particularly
lineman) or hockey?
-
-
Physical exam. Have patient dressed in examination gown or other appropriate clothing.
-
Back ROM: flexion/extension/side bending/rotation
-
Pain with palpation along spine
-
Radicular pain associated with straight-leg test
-
Complete neurologic exam including:
-
Adam’s forward bending test (see below)
-
Hip ROM: possible referred pain from hip pathology
-
-
Radiologic tests.
If pediatric patient describes significant back pain and/or any
abnormal findings are present on physical exam, it is appropriate to
obtain plain radiographs.-
AP and lateral radiograph of thoracic and
lumbar spine if pain is localized to thoracic or thoracolumbar region
or any findings to suggest scoliosis. -
AP/lateral and oblique images of lumbar
spine if patient localizes pain to lumbar region of back or pain
radiates into lower extremities. -
Evaluate radiographs for signs of:
-
Scoliosis
-
Spondylolysis/spondylolisthesis
-
Loss of disc space
-
Vertebral end-plate changes (erosions, Schmorl nodes)
-
Other bony changes (absent pedicle, curvature without rotation, etc.)
-
-
-
Additional imaging tests.
If neurologic abnormalities are identified on physical exam, consider
MRI of spinal canal. If no neurologic findings are present but pain
presentation is worrisome for underlying bone tumor or structural
abnormality, consider three-phase nuclear medicine bone scan. -
Differential diagnosis
-
Mechanical low-back pain
-
Spondylolysis/Spondylolisthesis
-
Discitis
-
Lumbar Scheuermann disease
-
Herniated intervertebral disc
-
Spine-related bone tumors
-
-
Mechanical low-back pain
-
Definition: back pain usually localized
to the lower back without radiation to lower extremities and without
neurologic findings on physical exam or radiographic abnormalities.
Previously thought to be rare in children, it remains less common in
children than in adults but can be a source of back pain if other
causes have been excluded. Symptoms most often occur after sitting for
long periods of time, tend to be vague or non-specific, and occur
sporadically. -
Physical exam: notable for lack of abnormal findings.
-
Radiographic exam: plain radiographs are
normal. No specialized radiographic studies are recommended at the time
of the initial evaluation. -
Treatment:
-
Referral to physical therapy for home-based exercise program of back strengthening and posture retraining.
-
Prescription for NSAIDs.
-
Return to clinic in 1 to 2 months for follow-up. If symptoms not improved or have changed, reconsider diagnosis.
-
-
-
Spondylolysis/spondylolisthesis.
-
Spondylolysis:
a structural defect in the bone in the posterior elements of the spine.
Most often in the “pars interarticularlis” region of the L5 vertebra.
Associated with hyper-extension activities such as dance, gymnastics,
figure skating; presents as low-lumbar back pain without radiation into
the lower extremities but exacerbated by hyperextension activities. -
Spondylolisthesis:
a translation or slippage of one vertebra on the next lower vertebra.
The most common cause in children is an “isthmic spondylolisthesis” in
which a lesion or defect in the pars interarticularis permits forward
slippage of the superior vertebra.
-
-
Discitis. A
condition in which children develop back pain that arises from a
presumed bacterial infection of the intervertebral disc. They may
present
P.87
with
gradual onset of pain, loss of lumbar lordosis, and progressive decline
in activity level potentially to the point of refusing to walk. The
child may remain afebrile. Current theories of etiology suggest it may
start as a vertebral osteomyelitis that spreads to the adjacent disc
space. If suspected, laboratory tests should be obtained including CBC
with differential, ESR, CRP, and blood cultures. The CBC may be normal
but some elevation of the ESR and CRP is frequently present. Initial
radiographs may be normal or may show vertebral end-plate
irregularities. Later radiographs may show a narrowing of the disc
space involved. The diagnosis may be confirmed with specialized imaging
tests such as nuclear medicine bone scan, CT, or MRI. Treatment
consists of antibiotic therapy and, when appropriate, back
immobilization with a removable spinal orthosis for symptomatic support. -
Lumbar Scheuermann disease.
A condition in which patients present with lumbar back pain without
radicular symptoms. There are end-plate changes termed “Schmorl nodes”
in the lumbar vertebra on plain radiographs. In contrast to
Scheuermann’s disease of the thoracic spine (see below), which is
associated with significant thoracic kyphosis and vertebral wedging,
these changes are not found in the lumbar spine. -
Herniated intervertebral disc.
A herniation of the central portion of the disc, the “nucleus
pulposus,” into the spinal canal. Occurs in adolescent and teenage
patients. Symptoms usually have an acute, specific onset and are
associated with radicular symptoms of pain radiating down into the
lower extremity. Neurologic exam is helpful to look for signs of motor
weakness. An avulsion fracture of the vertebral ring apophysis
may also present with sudden onset of back pain with radicular-type
symptoms radiating into the lower extremities. This may be visible on
plain films as a small triangular fragment of bone displaced from the
lower end plate of the vertebra. If a herniated disc or a vertebral
ring apophysis avulsion-type fracture is suspected, an MRI scan can
help confirm diagnosis. -
Bone tumors involving the spine.
There are a number of bone tumors that may arise from the vertebral
body or the posterior elements of the spine. They may present with
pain, particularly night pain, deformity, or other associated symptoms.
Physical exam may reveal findings of scoliosis, however, radiographs
may reveal a curvature of the spine without any rotational component
present. This suggests that the curvature is postural, due to the
painful process, rather than a structural, scoliosis-type curve. Benign
tumors that arise in the spine most frequently include osteoid osteoma,
osteoblastoma, and hemangioma. Primary malignant tumors of the bone
that arise in the spine are relatively rare.
-
-
Idiopathic adolescent scoliosis
-
Definition. A
deformity of the spine consisting of a lateral curvature measuring
greater than 10 degrees on a spine radiograph that also has a
rotational component. The word “idiopathic” suggests no identifiable,
underlying cause. There may be a genetic component. -
Presentation.
Most often patients are adolescent girls who have been detected either
on school screening examination or by an observant primary physician.
Boys are affected less often and have a lower incidence of progressive
curves. The deformity may occasionally be seen in younger children.
Family history is frequently positive. Idiopathic scoliosis should be painless.
The examiner should inquire about any neurologic symptoms including
weakness, numbness, radicular symptoms, or bowel or bladder changes. -
Incidence.
For curves greater than 10 degrees, the overall incidence is 2%.
However, for curves measuring greater than 20 degrees and requiring
treatment, the incidence is 0.2%. -
Physical examination. All patients should be examined in a gown so that the back can be well visualized. Inspect pelvic height for evidence of limb
P.88
length difference. Examine shoulder height and trunk position for
evidence of asymmetry or truncal imbalance. With the patient standing,
have the patient bend forward at the waist. Observe the patient’s back
for evidence of rib hump deformity. This is the Adam forward bending test.
Finally, complete a thorough neurologic examination, including
abdominal reflexes and tests for long tract or upper motor neuron
lesions. -
Radiographic evaluation.
PA and lateral spine radiographs on a long cassette to include the
thoracic, lumbar, and sacral regions of the spine. The curvature of the
spine can be measured using the COBB method. -
Characteristics. For true idiopathic scoliosis, the curve is most often:
-
Painless
-
Convex to the right in the thoracic spine
-
Not associated with any neurologic changesIf a curve does not fit this pattern, one must exclude
other possible causes. If the curve is convex to the left, painful, has
associated neurologic changes, or is rapidly progressive, one should
consider obtaining an MRI scan in order to rule out possible underlying
spinal cord abnormalities such as syringomyelia, tethered cord,
diastematomyelia, or spinal cord tumor.
-
-
Risk factors for progression
include young age, female gender, prepubertal status, and curve greater
than 11 degrees. The spine curve is at greatest risk for progression
during periods of accelerated skeletal growth (24). -
The goal of treatment is to prevent further progression of the curve.
-
Treatment of
idiopathic scoliosis depends on the size of the curve as well as the
age of the patient at the time of detection. Typically, for curves
greater than 11 degrees and less than 20 degrees, treatment consists of
observation with repeat spine radiographs
obtained in 4 to 6 months. The younger the child at the time of curve
detection, the greater the risk for future progression of the curve. If
the curve is greater than 20 to 25 degrees in a skeletally immature
patient, brace treatment is indicated.
Brace treatment is most effective in moderate-sized and flexible curves
in growing adolescent patients. The goal of brace treatment is to
arrest any further progression of the curve. For patients in whom a
large curve of greater than 45 to 50 degrees is already present or for
whom the curve progresses despite brace treatment, treatment is surgical spinal fusion with instrumentation.
-
-
Kyphosis
-
Definition.
An increased curvature of the thoracic spine in the sagittal plane,
either from the side or on the lateral radiograph, producing a
rounded-back appearance. -
Characteristics. Normal thoracic kyphosis is 20 to 45 degrees. Scheuermann disease
is a condition in which the thoracic curve on the lateral radiograph is
greater than 45 degrees and associated with wedging of three adjacent
central vertebral bodies of 5 degrees or more. It may be associated
with end-plate changes of the vertebral bodies such as Schmorl nodes.
It should be distinguished from postural kyphosis, in which the
vertebral bodies do not exhibit changes and the curvature resolves with
improvement of the patient’s posture. -
Presentation. Patients usually have one of two complaints: pain or concerns regarding appearance.
-
Physical examination.
Careful examination of the back with the patient standing, on forward
bending, and with hyperextension in the prone position can help
determine the flexibility of the kyphosis. Increased thoracic kyphosis
is frequently associated with increased lumbar lordosis. The
possibility of hip flexion contractures should be assessed. A careful
neurologic examination should also be performed. -
Radiographs. Standing PA and lateral thoracolumbar spine radiographs should be obtained.
-
Treatment.
Options include observation, bracing, and surgery. For patients who are
asymptomatic with a relatively small curve, one may consider
P.89
continued
observation. For symptomatic patients who are skeletally immature with
curves greater than 45 to 50 degrees, one may consider brace treatment.
The indications for surgical treatment include kyphosis greater than 70
degrees, progressive deformity, recalcitrant pain, and concerns
regarding patient appearance in the setting of significant deformity (25).
-
-
Lordosis
-
Definition. An increase in “swayback” appearance of the lower lumbar spine.
-
Presentation. The patient may complain of low back pain, concern regarding appearance, or both.
-
Etiology.
Possible causes include posture (especially in younger patients),
bilateral congenital dislocation of the hip, hip flexion contracture,
hamstring weakness, increased thoracic kyphosis,
spondylolysis/spondylolisthesis, and congenital spinal deformity. -
Physical examination
should include careful evaluation of the back, hips, and lower
extremities and should also include a thorough neurologic evaluation. -
Radiographs. PA and lateral thoracolumbar spine radiographs should be obtained.
-
Treatment.
Careful exclusion of underlying abnormalities should be undertaken. If
other underlying causes have been excluded and the cause is thought to
be postural, then treatment may consist of further observation.
-
-
Cerebral palsy (26,27)
-
Definition. A
nonprogressive disorder resulting from an injury to the brain, usually
within the first year of life, and resulting in impairment in motor
function. -
Classification can be geographic (part of body most affected) or by type of motor dysfunction.
-
Geographic
-
Hemiplegia. Arm and leg on one side only affected
-
Diplegia. Major spasticity in lower limbs, less in upper
-
Triplegia. Three-limb involvement
-
Quadriplegia. All four limbs, “total body involved”
-
-
Motor type
-
Spastic. Increased stretch reflexes (pyramidal)
-
Athetoid. Fluctuating motor tone, often with spontaneous, involuntary rhythmic motor movements (extrapyramidal)
-
Dystonia. Similar to athetoid; intermittent or inconsistent tone
-
Mixed. A combination of spasticity and dystonia
-
-
-
Causes
-
Prenatal.
Intrauterine infection, for example, TORCH (toxoplasmosis, rubella,
cytomegalovirus, and herpes simplex), genetic or chromosomal
abnormalities -
Perinatal. Premature birth, low birth weight, asphyxia, erythroblastosis fetalis
-
Postnatal. Infection, stroke, cardiac arrest, near drowning
-
-
Hierarchical approach to problems
-
Primary problems include abnormal muscle tone, poor selective muscle control, and poor balance.
-
Secondary problems
include muscle and joint contractures and bony deformities (increased
femoral anteversion, tibial torsion, and foot deformities). -
Tertiary problems include compensatory mechanisms for primary and secondary problems.
-
-
Treatment
-
Physical therapy
-
Orthotics
-
Assistive devices: wheelchair, walker, crutches
-
Tone-reducing agents or medications: oral (e.g., baclofen, Valium, dantrolene) or focal (e.g., Botox, phenol)
-
Neurosurgical options: selective dorsal rhizotomy, intrathecal baclofen pump
-
Orthopaedic surgery: soft-tissue lengthening procedures, bony realignment procedures
P.90 -
-
Nonambulatory patients.
The principal difficulties that affect patients with total body
involvement are hip dislocation and neuromuscular scoliosis. These are
important issues for these patients because they are wheelchair bound
and frequently mentally handicapped. Painful sitting or difficulty with
sitting balance resulting from scoliosis or pelvic obliquity can
interfere significantly with their activities of daily living, personal
care, and activity level. Patients should be monitored regularly for
early detection of either hip dislocation or scoliosis. -
Ambulatory patients.
If children have independent sitting balance by age 2 years old, then
there is approximately a 95% chance that they will eventually be able
to ambulate. Children with cerebral palsy who can ambulate usually have
difficulty because of increased motor tone, poor selective motor
control, which results in co-contracture of muscle groups, and poor
balance. Frequently, muscle contractures and bony deformities develop
over time. Three-dimensional gait analysis is useful to assess walking
in these children in order to identify a problem list of orthopaedic
issues or deformities that are contributing to the patients difficulty
in walking. Orthopaedic surgery usually consists of muscle lengthening
or transfer procedures combined with bony realignment procedures for
underlying torsional deformities of the lower extremities. Most often,
these are combined in one surgical setting to minimize recovery time
and to speed the child’s return to activities. The selective dorsal rhizotomy
is a procedure to decrease lower extremity tone by cutting
approximately 30% to 40% of the dorsal afferent sensory nerve rootlets.
It is indicated for children with spastic diplegia who have pure
spasticity, no contractures, and good balance. It is usually performed
in children between the ages of 4 and 8 years old. For children with
cerebral palsy, optimum treatment consists of a combined approach
involving the physiatrist, the neurosurgeon, the orthopaedic surgeon,
the physical and occupational therapists, and the orthotist.
-
-
Spina bifida (28)
-
Definition. A
malformation of the spine, resulting from incomplete closure of the
posterior elements of the spine as well as of the neural tube in which
the meninges and neural elements are exposed at birth. -
Etiology is
multifactorial. There is a genetic component in that there is increased
risk for first-degree relatives of patients with spina bifida. There is
also an environmental role linked to insufficient dietary folic acid
for women of childbearing age. -
Classification is based on the level of neurologic deficit.
-
Associated disorders
include hydrocephalus requiring ventriculoperitoneal shunting, tethered
spinal cord, Arnold-Chiari malformations, syringomyelia, and urologic
problems. -
Orthopaedic conditions
include scoliosis for patients with high thoracic level deficits,
excessive spinal kyphosis, hip dislocation, and foot deformities. -
Ambulatory function
is determined primarily by level of deficit. Patients who ambulate are
usually patients who maintain active control of knee flexion and
extension. Many children ambulate when young, but as they get older, it
takes greater energy and oxygen consumption, and many resort to using a
wheelchair.
-
HA, Newman SR. Adolescent bunion deformity treated with double
osteotomy and longitudinal pin fixation of the first ray. J Pediatr Orthop 1993;13:80–84.
RG, Birch JG, Herring JA, et al. Use of the Pavlik harness in
congenital dislocation of the hip, an analysis of failures of
treatment. J Bone Joint Surg (Am) 1990;72:238–244.
MS, Mandiga R, Murphy JM, et al. A clinical practice guideline for
treatment of septic arthritis in children: efficiency in improving
process of care and effect on outcome of septic arthritis of the hip. J Bone Joint Surg (Am) 2003;85:994–999.