Supracondylar Elbow Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Supracondylar Elbow Fracture
Supracondylar Elbow Fracture
Melanie Kinchen MD
Simon C. Mears MD, PhD
Description
-
Occurs at the metaphyseal–diaphyseal junction of the distal humerus
-
The fracture goes through the olecranon fossa of the distal humerus, which is a weak area.
-
-
The mechanism (hyperextension) usually
causes elbow dislocation in adults, supracondylar humerus fractures in
children, and fractures through the growth plate of the distal humerus
in toddlers. -
Classification:
-
By mechanism of injury:
-
Hyperextension type (95% of fractures)
-
Flexion type
-
-
The Gartland classification system is the most commonly used (1).
-
Type I: Nondisplaced
-
Type II: Displaced, but with an intact cortex; hinge or greenstick
-
Type III: Completely displaced, with no continuity between fragments; at highest risk for complications
-
-
-
Synonym: Distal humerus fracture
Epidemiology
-
These fractures affect the distal humerus
of children at a rate of 308 per 100,000, and 56% of those elbow
fractures are supracondylar (2). -
Mean age of patients at time of injury is ~8 years (2).
-
Distribution between genders is approximately even (2).
-
This fracture is rare in adults, with rates of distal humerus fractures at 5.7 cases per 100,000 (3).
Risk Factors
Fall on an outstretched arm
Etiology
-
A fall on an outstretched hand with the elbow hyperextended
-
A fall onto a flexed elbow (extremely rare)
Associated Conditions
-
Ipsilateral distal forearm fractures
-
Ipsilateral midshaft humeral fractures
-
Nerve and artery damage (Fig. 1)
Signs and Symptoms
-
Pain, swelling, and possibly instability occur after an acute traumatic event.
-
After a few hours, typically ecchymosis occurs in the antecubital region.
-
Nerve injuries are common with this fracture, signaled by lack of full active ROM.
-
Arterial injuries also are possible and produce loss of pulse, color, temperature, and later, movement.
Physical Exam
-
Swelling and tenderness are common.
-
With type III fractures, an S-shaped deformity at the elbow is common and may be mistaken for a dislocation.
-
Perform a thorough neurovascular examination of the involved extremity because a substantial risk of injury exists.
-
Document full active flexion and extension of all digits at both MCP and IP joints.
-
Substantial pain on passive stretch of the fingers may signal compartment syndrome.
-
Check pulse, color, and temperature to assess vascular status.
Tests
Imaging
-
AP and lateral radiographs usually are sufficient for diagnosing the injury.
-
For nondisplaced fractures, a posterior fat pad sign may be the only radiographic finding.
-
When ordering a radiograph of a suspected
supracondylar fracture, specify the distal humerus as the part to be
examined rather than the elbow because the patient may not be able to
straighten the elbow fully.
Differential Diagnosis
-
Elbow dislocation
-
Bicondylar humeral fracture
-
Growth plate fracture (in toddlers)
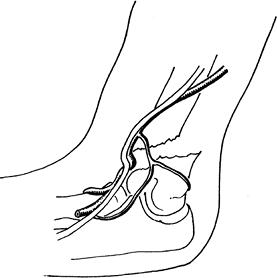 Fig. 1. A supracondylar fracture of the distal humerus may injure the brachial artery or the medial, radial, or ulnar nerve.
Fig. 1. A supracondylar fracture of the distal humerus may injure the brachial artery or the medial, radial, or ulnar nerve.
Initial Stabilization
Initial treatment should involve immobilization of the
injured elbow in 20–30° of flexion to prevent additional displacement
or neurovascular damage until an orthopaedic surgeon can evaluate the
patient.
injured elbow in 20–30° of flexion to prevent additional displacement
or neurovascular damage until an orthopaedic surgeon can evaluate the
patient.
General Measures
-
Type I injuries: Immobilization
-
Type II injuries: Closed reduction and immobilization or operative intervention
-
Type III injuries: Operative intervention
-
Immobilization should be at <90° of
flexion because flexion of >90° leads to increased compartment
pressures and risk of compartment syndrome (4).
Special Therapy
Physical Therapy
-
Physical therapy for children has not been shown to improve results (5).
-
Physical therapy is useful in adult fractures.
-
Timing depends on healing and strength of internal fixation.
-
ROM is emphasized, followed by strength.
-
Medication
Acetaminophen or acetaminophen with codeine for pain control
Surgery
-
For type II fractures angulated >5–10°
and for type III fractures, closed reduction should be attempted with
the patient under adequate analgesia or anesthesia.-
If anatomic reduction cannot be achieved by closed reduction, open reduction should be performed.
-
Fractures without vascular injury may be splinted and pinned on a delayed basis.
-
A delay of <24 hours does not seem to alter outcomes (6,7).
-
-
An unstable fracture should be stabilized with percutaneous pin fixation.
-
2 lateral PINS and crossed medial and lateral PINS give mechanical stability.
-
Use of only lateral PINS prevents possible injury to the ulnar nerve (8).
-
Flexion injuries are treated with reduction and pinning (9).
-
After surgery, the elbow is immobilized at 90° of flexion for 3–4 weeks.
-
The PINS are removed at 4–6 weeks.
-
-
Compartment syndrome:
-
May be prevented by timely recognition of arterial injury
-
If ischemia time exceeds ~6 hours, fasciotomy of the forearm probably should be included in the treatment.
-
P.433
Prognosis
-
Prognosis is excellent with anatomic reduction (10).
-
If malunion occurs, additional surgery may be needed to correct the deformity.
Complications
-
Nerve injuries: The median nerve is the most commonly injured, followed by the radial nerve.
-
It may take several months to regain normal function (11).
-
Arterial injuries: The brachial artery is the most commonly injured.
-
Compartment syndrome may result in Volkmann ischemic contracture.
-
Varus deformity of the elbow
-
Elbow stiffness: Uncommon with anatomic reduction
-
AVN of the trochlea, leading to a fishtail deformity
Patient Monitoring
-
Patients require radiographs and
examinations at 1–2 weeks and ~6 weeks after fracture to ensure
maintenance of the reduction during fracture healing. -
A small risk of malreduction exists.
-
Patients should be seen after bone healing to document good alignment and ROM.
References
1. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959;109:145–154.
2. Houshian
S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children:
analysis of 355 fractures, with special reference to supracondylar
humerus fractures. J Orthop Sci 2001;6:312–315.
S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children:
analysis of 355 fractures, with special reference to supracondylar
humerus fractures. J Orthop Sci 2001;6:312–315.
3. Robinson CM, Hill RMF, Jacobs N, et al. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma 2003;17:38–47.
4. Battaglia
TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment
pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop 2002;22:431–439.
TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment
pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop 2002;22:431–439.
5. Keppler
P, Salem K, Schwarting B, et al. The effectiveness of physiotherapy
after operative treatment of supracondylar humeral fractures in
children. J Pediatr Orthop 2005;25:314–316.
P, Salem K, Schwarting B, et al. The effectiveness of physiotherapy
after operative treatment of supracondylar humeral fractures in
children. J Pediatr Orthop 2005;25:314–316.
6. Gupta
N, Kay RM, Leitch K, et al. Effect of surgical delay on perioperative
complications and need for open reduction in supracondylar humerus
fractures in children. J Pediatr Orthop 2004;24:245–248.
N, Kay RM, Leitch K, et al. Effect of surgical delay on perioperative
complications and need for open reduction in supracondylar humerus
fractures in children. J Pediatr Orthop 2004;24:245–248.
7. Sibinski
M, Sharma H, Bennet GC. Early versus delayed treatment of extension
type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg 2006;88B:380–381.
M, Sharma H, Bennet GC. Early versus delayed treatment of extension
type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg 2006;88B:380–381.
8. Skaggs
DL, Hale JM, Bassett J, et al. Operative treatment of supracondylar
fractures of the humerus in children. The consequences of pin
placement. J Bone Joint Surg 2001;83A: 735–740.
DL, Hale JM, Bassett J, et al. Operative treatment of supracondylar
fractures of the humerus in children. The consequences of pin
placement. J Bone Joint Surg 2001;83A: 735–740.
9. De Boeck H. Flexion-type supracondylar elbow fractures in children. J Pediatr Orthop 2001;21: 460–463.
10. Mangwani
J, Nadarajah R, Paterson JMH. Supracondylar humeral fractures in
children: ten years’ experience in a teaching hospital. J Bone Joint Surg 2006;88B:362–365.
J, Nadarajah R, Paterson JMH. Supracondylar humeral fractures in
children: ten years’ experience in a teaching hospital. J Bone Joint Surg 2006;88B:362–365.
11. Ramachandran
M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated
with supracondylar fractures of the humerus in children: the experience
of a specialist referral centre. J Bone Joint Surg 2006;88B:90–94.
M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated
with supracondylar fractures of the humerus in children: the experience
of a specialist referral centre. J Bone Joint Surg 2006;88B:90–94.
Additional Reading
Storm SW, Williams DP, Khoury J, et al. Elbow deformities after fracture. Hand Clin 2006;22:121–129.
Codes
ICD9-CM
-
812.41 Closed supracondylar fracture
-
812.51 Open supracondylar fracture
Patient Teaching
Adult patients and parents of injured children should be
informed about the signs of ischemia and compartment syndrome
(increasing pain, loss of finger motion, cold fingers, and loss of
color) because compartment syndrome may (rarely) occur in the 1st few
days after reduction secondary to tight dressings or intimal injury to
the vessels.
informed about the signs of ischemia and compartment syndrome
(increasing pain, loss of finger motion, cold fingers, and loss of
color) because compartment syndrome may (rarely) occur in the 1st few
days after reduction secondary to tight dressings or intimal injury to
the vessels.
Activity
To prevent refracture, rough play should be prohibited for a month after pin removal.
FAQ
Q: Which supracondylar fractures should be treated with surgery?
A:
Type II fractures with an unsatisfactory reduction require reduction
and pinning. Type III fractures require reduction and percutaneous
pinning.
Type II fractures with an unsatisfactory reduction require reduction
and pinning. Type III fractures require reduction and percutaneous
pinning.
