MANAGEMENT OF THE ARTHRITIC HAND
III – THE HAND > Reconstructive Procedures > CHAPTER 70 –
MANAGEMENT OF THE ARTHRITIC HAND
the most common disease processes leading to deformity in the hand. It
is important for the surgeon to be familiar with them and with some of
the less typical arthritides, as well. Gout and psoriatic arthritis,
for example, have certain unique characteristics with which the hand
surgeon must deal (Table 70.1).
 |
|
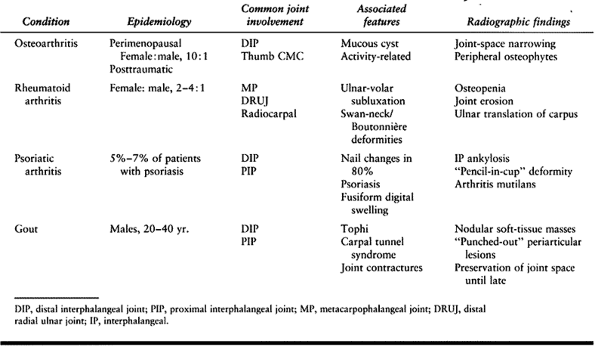
Table 70.1. Hand Arthritis—Differential Diagnosis
|
interphalangeal (IP) and thumb carpometacarpal (CMC) joints. It is most
common in perimenopausal and postmenopausal women. While OA of the
thumb basal CMC joint can occur as an isolated entity, arthritis of the
distal interphalangeal (DIP) joint often involves multiple digits, and
arthritis of the proximal interphalangeal (PIP) joint usually occurs in
conjunction with OA of the DIP joint. Interphalangeal OA in a single
digit is often a sequela of trauma or sepsis. Symptoms of primary OA
include gradual swelling and stiffness with minimal to mild pain.
Marginal osteophytes appear in the DIP joint (Heberden’s nodes) and PIP
joint (Bouchard’s nodes). With progression, the joint develops a mild
flexion deformity and may deviate radially or ulnarly with collateral
ligament involvement. A mucous cyst is a ganglion arising from the DIP
joint via a pedicle, which often develops in conjunction with OA (33).
can affect the IP joints and is more likely to occur in middle-aged
women (42,53). Erosive
osteoarthritis causes pain, synovitis, and stiffness; radiography
reveals progressive destruction of the IP joints. This condition may be
differentiated from RA by the absence of systemic manifestations and
certain radiographic characteristics (osteoporosis, more proximal joint
involvement) (42).
idiopathic condition in women; previous trauma is the usual etiology in
men. Patients complain of pain at the base of the thumb and thenar
eminence, with occasional radiation distally into the
metacarpophalangeal (MP) joint and proximally into the wrist and
forearm. Swelling, crepitus, weakness of pinch, and dorsoradial
subluxation occur as arthritis and instability progress (Table 70.2).
Tenderness over the palmar-radial aspect of the CMC joint and a
positive axial grind test aid in diagnosis. Other causes of pain in
this region that must be considered in the differential diagnosis
include carpal tunnel syndrome, de Quervain’s tenosynovitis, flexor
carpi radialis (FCR) tendinitis, radiocarpal and triscaphe
(scaphotrapeziotrapezoid) arthritis, and volar wrist ganglion.
Radiographic evaluation should include Robert’s hyperpronation view and
the stress view as described by Eaton (Fig. 70.1) (22,56).
 |
|
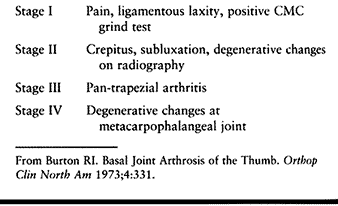
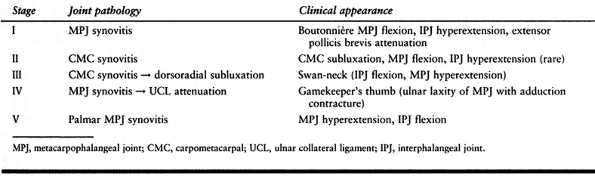
Table 70.2. Classification of Thumb Carpal Metacarpal (CMC) Osteoarthritis
|
 |
|
Figure 70.1. Osteoarthritis of the thumb, carpometacarpal (CMC) joint. A: Posteroanterior (PA) view demonstrates loss of joint space, subchondral sclerosis, and periarticular osteophyte. B: Robert’s hyperpronation view displays the entire trapezium and its borders. C:
Application of ulnarly directed stress on the radial side of the distal phalanx demonstrates subluxation of the thumb CMC joint associated with ligamentous laxity and arthritis. |
joints of the hand is much less common, and it is usually secondary to
fracture, ligamentous instability, or sepsis. OA of the second or third
carpometacarpal joints is called a carpal boss.
This dorsal osteophyte develops gradually as a firm, tender mass on the
dorsum of the hand. Symptoms may be aggravated by tendinitis of the
overlying extensor carpi radialis brevis and longus. Some cases are
associated with small dorsal ganglions. The carpal boss is best
demonstrated on a lateral radiograph with the hand supinated 30°.
Arthritis of the small-finger CMC joint is usually a result of trauma.
This joint is best viewed on an anteroposterior (AP) radiograph with
the forearm pronated 30°.
ligamentous injury, malunited or nonunited fractures, Kienbøck’s
disease, or crystal pyrophosphate deposition disease. Reviewing a large
series of wrist radiographs, Watson and Ballet reported a 5% incidence
of wrist OA (73). Of these cases, 57% involved
a pattern that they termed scapholunate advanced collapse (SLAC).
Arthritis first develops between the scaphoid and radius, followed
sequentially by degenerative changes in the capitolunate and
lunotriquetral joints (Fig. 70.2). It is most
commonly a sequela of chronic scapholunate ligamentous instability or a
scaphoid nonunion. Patients may complain of stiffness, pain,
intermittent swelling, and clicking.
 |
|
Figure 70.2.
Scapholunate advanced collapsed pattern of wrist arthritis secondary to chronic scaphoid nonunion. Degenerative changes are seen between the scaphoid and radial styloid, as well as in the scaphocapitate and capitolunate joints. There is no evidence of the proximal migration of the capitate associated with later stages of this disease. |
involve the triscaphe joint alone or a combination of triscaphe and
SLAC patterns (74). Triscaphe arthritis is
characterized by pain at the base of the thumb; it may coexist or be
confused with arthritis of the CMC joint of the thumb.
synovial tissues of joints, tendon sheaths, and bursae. The hallmark of
this disease is proliferation of inflamed synovium that leads to
progressive joint destruction and deformity. This disease is often
symmetric and occurs two to four times more often in women than in men.
remember that it is a systemic disease; examination of the hand begins
with the cervical spine and encompasses the entire upper extremity.
Rheumatoid nodules, tenosynovitis, nerve compression, acute synovitis,
and damage to periarticular soft tissues and articular cartilage
secondary to chronic synovitis may lead to pain and dysfunction in the
rheumatoid hand.
ulnar subluxation of the carpus with radial deviation of the hand.
Dorsal subluxation of the distal ulna often occurs concomitantly.
Because the finely balanced forces of intrinsic and extrinsic muscles
are disrupted, these proximal deformities often result in palmar and
ulnar subluxation of the MP joints, with secondary deformities of the
IP joints.
interfere with function because of the direct pressure they apply or
their location over a joint or tendon. They may erode through skin, and
occasionally they can become infected. Rheumatoid nodules occur in 20%
to 25% of RA patients, usually in association with an aggressive form
of the disease.
tendons. Early in the course of the disease, symptoms of flexor
tenosynovitis include pain and crepitus over the tendons. Digital range
of motion becomes limited. Carpal tunnel syndrome is very common in RA
patients, secondary to compression of the median nerve in the wrist by
hypertrophic flexor tenosynovium. Involvement of digital flexor tendon
sheaths results in fusiform swelling of the digits, limited finger
flexion, and triggering. In later stages, tendons may rupture. Flexor
pollicis longus (FPL) and index flexors are the most common tendons to
rupture on the palmar side, often secondary to attrition over a palmar
scaphoid osteophyte (23). Further ruptures may progress sequentially in a radial-to-ulnar direction.
obvious swelling distal to the extensor retinaculum. Direct synovial
invasion or attrition over the distal ulna (Vaughan-Jackson syndrome)
may cause extensor tendon rupture (71). The
extensor digiti quinti is usually the first tendon affected; remaining
tendons rupture progressively from ulnar to radial. Because of the
already limited motion in their hands, many patients will not be aware
of ruptured extensor tendons; the physician must look closely for loss
of active MP joint extension. This condition must also be
differentiated from subluxating extensor tendons and from posterior
interosseous nerve palsy. With ulnar subluxation of the extensor
tendons over the MP joint, passive extension of the MP joint allows
centralization of the tendons; the patient will then be able to
maintain MP joint extension. In the presence of posterior interosseous
nerve palsy, passive MP joint extension can be demonstrated by a
tenodesis effect, in which passive wrist palmar flexion tightens intact
digital extensors, resulting in subtle MP joint extension.
transient stiffness; radiographs are normal. The presence of joint
crepitus, permanent limitation of motion, and joint narrowing or
erosion on radiographs indicates articular destruction secondary to
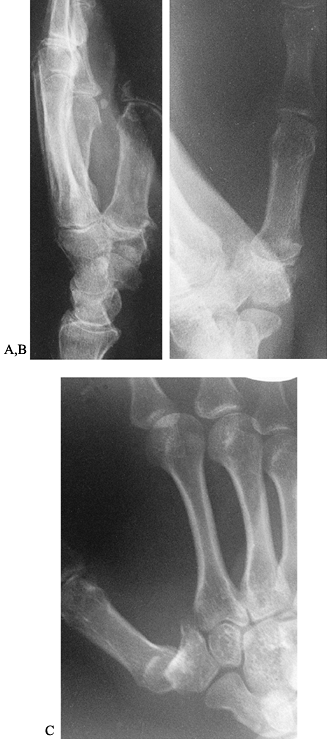
long-standing synovitis (Fig. 70.3 and Fig. 70.4).
The physician needs to look for subtle signs of fullness in the wrist
and point tenderness over the radiocarpal or distal radioulnar joints
(DRUJ). Arthritis of the DRUJ or more proximally at the elbow may limit
forearm rotation.
 |
|
Figure 70.3. PA (A) and lateral (B)
radiographs of the hand and wrist demonstrate generalized osteopenia, dorsal subluxation of the distal radioulnar joint, and ulnar translation of the carpus with loss of all contact between the radius and lunate. |
 |
|
Figure 70.4. PA (A) and lateral (B)
radiographs of another patient with rheumatoid arthritis. There is mild involvement of the proximal interphalangeal joints, more significant involvement of the metacarpophalangeal joints with bony destruction, and severe involvement of the wrists with marked bony destruction and loss of carpal height. |
ulnar-deviation deformities as continued synovitis causes extensor
tendon subluxation, intrinsic tightness, and actual subluxation of the
joint (Fig. 70.4). Chronic synovitis of IP
joints can lead to digital deformities that can occur in many
conditions but have come to be associated with RA. Primary mallet
deformity occurs rarely when the terminal extensor tendon is stretched
by dorsal synovitis of the DIP joint. Attenuation of the central slip
caused by PIP joint dorsal synovitis may lead to a boutonnieère
deformity. Swan-neck deformity can be caused by intrinsic tightness,
palmar synovitis leading to attenuation of the palmar capsule, flexor
digitorum sublimis (FDS) rupture, or overpull of the extensor secondary
to a mallet deformity. The thumb may be similarly involved; these
deformities are classified I through V on the basis of symptoms and
primary joint of involvement (Table 70.3) (49).
 |
|
Table 70.3. Classification of Rheumatoid Thumb Deformities
|
polyarthritis that occurs in 5% to 7% of patients with psoriasis. Skin
lesions usually precede the arthritis by months to years (36). Eighty percent of patients demonstrate nail changes, especially in association with arthritis of the DIP joint (76). This form of arthropathy differs from RA in that inflammation occurs without significant synovitis (46). It often leads to stiffness and spontaneous fusion rather than to the instability seen in RA (6). The hand may be involved in as many as 84% of patients with PA (70).
destruction (“arthritis mutilans”) have been described as pathognomonic
for PA. However, only 10% of patients with hand involvement have such
symptoms (46). Most patients exhibit varying
degrees of arthropathy affecting multiple joints. Clinically, PIP joint
involvement is most severe; radiographically, however, DIP, PIP, and MP
joints are affected with similar frequencies (6,70).
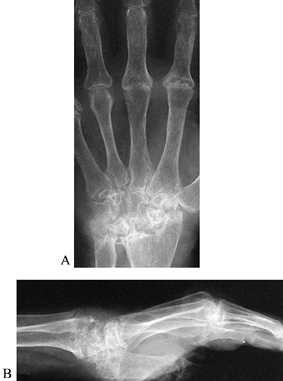
joints often develop significant flexion contractures and spontaneous fusion, while the MP joint often stiffens in extension (Fig. 70.5).
This finding does not occur in those 5% of patients with psoriatic
arthritis mutilans, in which severe osteolysis of the phalanges and
metacarpals leads to significant digital shortening and instability of
IP and MP joints (36,46,72). This collapse and telescoping of the phalanges has been called main en lorgnette (opera glass deformity) (41).
Fusiform swelling of the digits, acute dactylitis psoriatica, may be
confused with flexor tenosynovitis. Fusiform swelling, however,
involves the soft tissues of the entire digit and is often intermittent
in nature. In wrists of moderately to severely affected patients,
narrowing or obliteration of joint spaces and bony erosions often lead
to stiffness or spontaneous fusion in functional positions (6).
 |
|
Figure 70.5.
Radiographic appearance of psoriatic arthritis in the hand. Distal interphalangeal joints as well as proximal interphalangeal joints of the small finger have undergone spontaneous fusion. There is bony destruction of the proximal interphalangeal joints of the long and ring finger with severe shortening of the ring finger (opera glass deformity). There is less significant involvement of the metacarpophalangeal joints. Clinically, this patient’s wrists were asymptomatic. |
joint-space narrowing, erosions, and subchondral osteopenia. More
advanced stages reveal acro-osteolysis, “pencil-in-cup” deformities, IP
joint ankylosis, and severe joint destruction.
seen in men in the second to fourth decades. Tophaceous gout occurs in
50% to 70% of untreated patients, often many years after the initial
episode of acute arthritis (32). More recent
experience indicates that approximately 10% of patients under stable
medical management will develop clinically significant tophi (32,64).
Urate crystals may be deposited in cartilage, periarticular soft
tissues, and subcutaneous tissues. Progressive stiffness and aching of
joints often develops into destruction and deformity by insidiously
enlarging tophi. DIP and PIP joints are involved much more frequently
than are MP joints. Symptoms of gout in the hand include median nerve
compression; joint contractures; and chronic tenosynovitis, tendon
ruptures, and digital flexion contractures secondary to flexor tendon
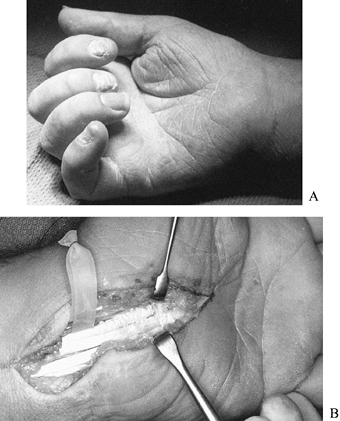
involvement (Fig. 70.6) (14,17,29,47,51,64).
 |
|
Figure 70.6. A: Tophaceous gout has caused progressive flexion contractures of the digits as well as carpal tunnel syndrome in this patient. B:
Carpal tunnel release and flexor tenosynovectomy were performed in this patient. Tophaceous deposits were also seen within the tendon substance. |
gout (67).
Extra-articular tophi may erode into bony cortex, creating the
“punched-out” lesions typically associated with gout. Intraarticular
erosions begin in the periphery of the joint and proceed centrally; the
joint space is usually preserved until late in the course of the
disease (55).
judicious combination of medical management, splinting, and hand
therapy (Table 70.4). A multidisciplinary
approach is needed, with participation of the surgeon, the hand
therapist, and, in the inflammatory arthritides, the internist or
rheumatologist. Knowledge of a patient’s goals, expectations, vocation
and avocations, social situation, and limitations of activities of
daily living is necessary to formulate an individualized treatment plan.
 |
|
Table 70.4. Management of Hand Arthritis
|
patient, because many of these conditions involve more than just the
hand. Arthritis of the more proximal joints of the upper extremity,
cervical and lumbar spine, and lower extremities must be diagnosed. For
successful restoration of hand function, the patient must have enough
elbow and shoulder motion to properly position the hand in space.
Lower-extremity disease may need to be controlled first to dispose of
ambulatory aids that may be exacerbating upper-extremity symptoms.
Alternatively, management of severely involved hands may take
precedence in anticipation of rehabilitation following lower-extremity
reconstruction.
Extraarticular
manifestations of inflammatory arthropathies (e.g., rheumatic cardiac
or pulmonary disease) may affect the decision to treat a patient
conservatively or with reconstructive surgery.
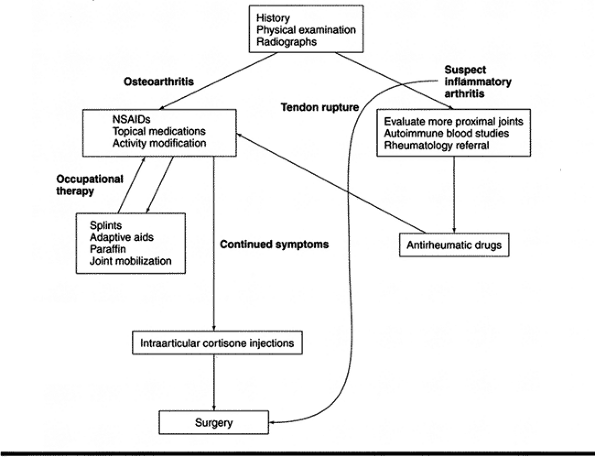
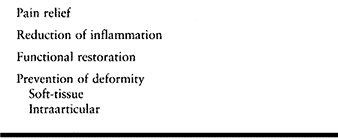
of pain, reduction of inflammation, restoration of function, prevention
of deformity, and a slowdown of the inevitable progression to joint
destruction (Table 70.5). In the patient with
inflammatory arthritis or gout, medical management by an internist (or
rheumatologist) is crucial in alleviating acute episodes and bringing
the entire disease process under control; therapy may take 3 to 4
months before it is effective (45).
 |
|
Table 70.5. Treatment Goals for Hand Arthritis
|
first line of treatment for early hand arthritis. I do not hesitate to
combine this therapy with splinting and rest of the affected joints.
Together, these are helpful in minimizing pain and inflammation.
Resting splints may be used prophylactically for activities that
exacerbate a patient’s symptoms. In certain instances, such as a
flare-up of OA of the DIP or the thumb basal joints, I often recommend
continuous use of a splint for 2 to 3 weeks, followed by nighttime use
for another 2 weeks.
prescribing the appropriate splint. A palmar splint with the wrist in
neutral to 20° of extension is effective for treating arthritis of the
wrist and carpal tunnel syndrome. The thumb with basal joint arthritis
is best immobilized with a long opponens splint, leaving the IP joint
free; a hand-based splint does not provide sufficient leverage to
immobilize the CMC joint.
effective in early stages of the inflammatory arthritides. Resting
splints to immobilize the wrist can be used to treat flare-ups of acute
synovitis or tendinitis of wrist flexors and extensors. A splint
incorporating the MP joints may be helpful for acute synovitis or to
treat early palmar and ulnar subluxation of these joints. IP joints may
be included when treating exacerbations of flexor tenosynovitis. The
physician or therapist should be aware of the increased susceptibility
of rheumatoid skin to breakdown under these splints. Development of
psoriatic skin lesions due to irritation beneath splints may also
occur. Psoriatic dermatitis, known as the Koebner phenomenon, also has
been observed at surgical incision sites and other wounds. Treat these
lesions with daily application of topical steroid (58).
as MP joint ulnar deviation and swan-neck and boutonnieère deformities,
may improve overall function by realigning the hand and digits in
patients who may not be ideal surgical candidates. Adaptive aids may be
instrumental in improving specific activities of daily living (ADL).
The therapist can provide individualized exercise programs and guidance
in performing ADL, based on the patient’s current stage of disease and
her specific limitations. An appropriate exercise program will prevent
joint stiffness and muscle atrophy.
by the physician. Inject joints (excluding the DIP joints), tendon
sheaths, peritendinous insertions, and carpal tunnels that have not
responded initially to an appropriate period of splinting and oral
NSAIDs. A 1:1 ratio of 1% lidocaine and betamethasone sodium phosphate,
using a 25- or 27-gauge needle, is preferred. Injections must be used
judiciously because excessive intraarticular or peritendinous steroid
administration can hasten cartilage degeneration (40) or lead to tendon ruptures (3).
More effective responses can be expected when steroid injections are
combined with 3 weeks of continuous splinting, as they maximize
anti-inflammatory effects (28,75). In many cases, this combination of methods has been successful when previous steroid injection alone was not.
in limited clinical use: COX-2 inhibitors, glucosamine and chondroitin
sulfate, intraarticular hyaluronic acid substitutes, and antirheumatic
biological agents. The indications for these agents in hand and wrist
arthritis have not yet been established.
conservative therapy is no longer effective. The surgeon and patient
must be aware of the goals and relative priorities of surgical
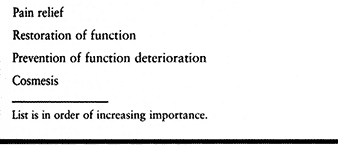
treatment of arthritis of the hand, described by William Souter (63). Although Souter was writing about RA, these principles are applicable to any type of hand arthritis (Table 70.6).
 |
|
Table 70.6. Goals of Surgery for Hand Arthritis
|
For instance, a patient whose RA leads to relatively painless
destruction of the wrist and rupture of one or two extensor tendons
needs immediate surgical intervention to prevent further tendon
rupture. Deformity alone, however, is not
an
indication for surgery. Severe deformities in debilitated patients or
in individuals with preservation of function may not require surgery.
As stressed earlier, the physician must examine and talk with the
patient several times to assess that person’s impairment, expectations,
and prognosis adequately. It is essential that patients be cooperative
and motivated before complicated, staged reconstructive procedures are
performed.
 |
|
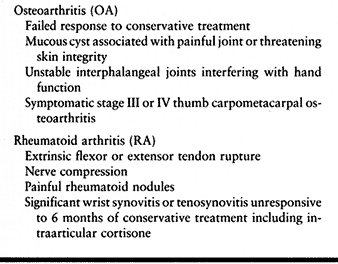
Table 70.7. Surgical Indications
|
inflammatory arthritis, the physician needs to take other factors into
consideration. Be aware of possible involvement of the cervical spine;
take appropriate radiographs and alert the anesthesiologist. Patients
on maintenance doses of steroids may need perioperative parenteral
corticosteroid supplementation. High doses of chronic steroids may
interfere with wound healing. Discontinue use of aspirin and other
NSAIDs 1 week before surgery to minimize platelet dysfunction. Other
antirheumatic medications may adversely affect immunologic or
hematopoeitic function; take appropriate precautions on the basis of
preoperative laboratory studies.
excision and marginal osteophyte debridement. Excision of mucous cysts
alone has a 25% to 50% recurrence rate (20,33). Cyst aspiration similarly has a high recurrence rate and may lead to an increased incidence of septic arthritis (59). Arthrodesis is the preferred treatment for an unstable, painful DIP joint.
osteoarthritic PIP joint remains a problem. Arthrodesis of index and
long fingers is superior to arthroplasty in restoring pinch strength.
Arthrodesis provides more consistent results in the ulnar digits at the
expense of grip strength and dexterity. Although silicone arthroplasty
of these PIP joints may provide improved function, a recent report
noted 20% to 35% bone resorption around these implants at 2 to 4 years
after surgery (53).
joint can be significantly disabling, in part because of the normal
mobility of this joint. Excessive laxity secondary to chronic
subluxation may be treated by arthrodesis; take care to maintain the
metacarpal arch by fusing this joint in adequate flexion (30).
Painful malunions of small-finger CMC fracture–dislocations also may be
treated with arthrodesis, or with partial resection arthroplasty (7).
commonly treated surgically for osteoarthritis. The severity of
arthritis has been classified into four stages based on clinical and
radiographic involvement (Table 70.2) (10).
Patients with stage I disease are most likely to respond to
conservative treatment, including splinting, NSAIDs, injection,
activity modification, and thenar strengthening exercises. If symptoms
continue after an adequate trial of conservative management, or in
later stages of arthritis, surgical intervention may be indicated. A
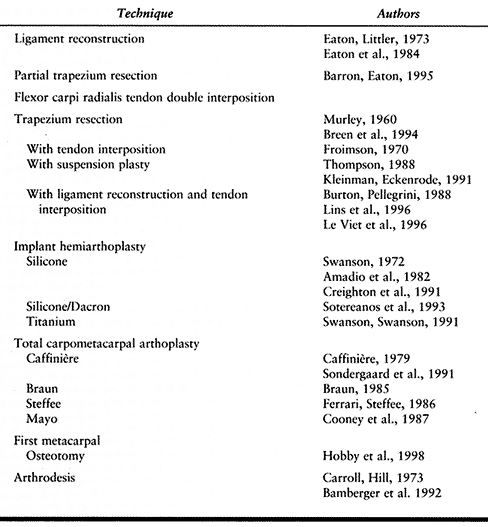
wide range of surgical techniques for the arthritic thumb CMC joint
have been described (Table 70.8).
 |
|
Table 70.8. Thumb CMC Joint Reconstruction
|
More advanced CMC arthritis requires partial or total trapezium
excision combined with a reconstructive procedure. Trapezial excision
alone (48), silicone implant arthroplasty (52), and soft-tissue interposition arthroplasty (1,43,44)
result in residual weak pinch and proximal metacarpal migration.
Another problem with silicone implants is fragmentation and
foreign-body giant-cell synovitis occurring in patients who use their
thumbs a great deal (52,60).
Various resurfacing arthroplasties have been advocated, but proceed
cautiously because rates of 10% to 35% of subluxation and dislocation
are reported (19,54,66).
laborers who require a strong, pain-free thumb and are willing to
sacrifice some mobility (including the ability to flatten the hand) (4). This procedure is contraindicated in patients with scaphotrapezial or pantrapezial arthritis.
-
Approach the osteophyte and associated ganglion through a transverse wrist incision over the bump.
-
Retract the digital extensor tendons ulnarly and the wrist extensors radially.
-
Excise the ganglion with its stalk and attached capsule.
-
Approach the CMC joints through separate longitudinal incisions.
-
With sharp osteotomes, excise any osteophytes down to normal cartilage.
-
Reapproximate the capsule and periosteum.
-
Immobilize the hand in a splint or cast for 4 to 6 weeks.
reconstruction described by Burton and Pellegrini has resulted in a
high percentage of satisfied patients (12,22).
The ligament reconstruction, tendon interposition (LRTI) arthroplasty
uses autogenous tissue, restores strength, and minimizes metacarpal
migration. With complete trapezium excision, this procedure may be used
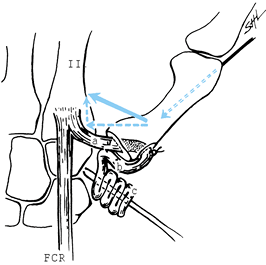
for all stages of basal joint arthritis. The LRTI arthroplasty, as
originally described, uses a split FCR tendon to reconstruct the palmar
oblique ligament and function as a tendon spacer (Fig. 70.7). More recently, I have used the entire FCR tendon,
as advocated by Burton (11): It is easier to harvest, and no adverse effects on recovery have been reported.
 |
|
Figure 70.7.
Ligament reconstruction, tendon interposition arthroplasty. The forces producing proximal migration and radial subluxation of the metacarpal are neutralized by ligament reconstruction as indicated in the vector diagram. a, ligament reconstruction; b, metacarpal resurfacing; c, tendon arthroplasty spacer. (From Burton RI, Pellegrini VD Jr. Surgical Management of Basal Joint Arthritis of the Thumb. Part II. Ligament Reconstruction with Tendon Interposition Arthroplasty. J Hand Surg [Am] 1986;11:324.) |
-
Expose the CMC joint through a
longitudinal incision along the radial border of the thumb metacarpal.
Curve the proximal incision ulnarly into the distal wrist crease to
expose the FCR tendon. -
Identify and protect the sensory branch
of the radial nerve, the radial artery, and the palmar cutaneous branch
of the median nerve. -
Reflect the thenar muscles distally and ulnarly from the metacarpal and trapezium.
-
Longitudinally incise the fibro-osseous canal of the FCR to expose the tendon distal to the trapezium.
-
Longitudinally incise the palmar-radial capsule to expose both the carpometacarpal and scaphotrapezial joints.
-
Split the trapezium into two or four
pieces with an osteotome or saw and remove them with a rongeur. Avoid
injury to the joint capsule and FCR tendon. -
Excise the base of the thumb metacarpal
perpendicular to its longitudinal axis. Place a hole in the metacarpal
base between the extensor pollicis brevis (EPB) and the extensor
pollicis longus (EPL) tendons with a gouge or drill positioned
perpendicular to the plane of the thumbnail. -
Harvest 10–12 cm of the FCR tendon
through two to three short transverse incisions in the forearm,
transecting it proximally at its musculotendinous junction. -
Free the distally based tendon from its
insertion and pass it into the metacarpal medullary canal and out of
the dorsal cortical hole. -
Place a nonabsorbable figure-of-eight
stitch in the deep capsule for later use. With the thumb in palmar
abduction, stabilize the metacarpal by inserting two 0.045 in.
Kirschner wires (K-wires) into the index metacarpal and trapezoid. -
While applying tension to the FCR tendon,
suture it to the lateral metacarpal periosteum and then back to itself.
Fold the remainder of the tendon on itself and suture it into the
trapezial fossa with the previously placed deep capsular stitch (Fig. 70.7). -
Close the capsule with nonabsorbable suture. Close skin incisions and immobilize the arm in short-arm thumb spica for 4 weeks.
K-wires at 4 weeks. Apply a removable thumb spica splint, which the
patient should wear for another 2 to 4 weeks except when performing
gentle assisted range-of-motion (AROM) exercises. Begin strengthening
exercises at 6 to 8 weeks.
postoperatively. More than 80% of patients undergoing this or similar
ligament reconstruction procedures demonstrate pain-free function and
improved grip strength (12,21,69).
of the wrist include various intercarpal arthodeses, proximal row
carpectomy, and total wrist arthrodesis (see Chapter 41, Chapter 42, and Chapter 72).
Posttraumatic arthritis of the DRUJ may require surgical intervention
if conservative therapy is ineffective. The historically popular
Darrach procedure has fallen out of favor with many surgeons as
increasing numbers of complications are recognized and as the
biomechanics of the DRUJ are better understood. Alternative operations
have been developed that attempt to maintain the integrity of the
radioulnar and ulnocarpal ligaments while revising the painful DRUJ.
These include hemiresection–interposition arthroplasty, matched distal
ulna resection, and the Sauveé-Kapandji procedure. Each has its
advocates and adversaries; there are no good studies documenting
long-term results. Treatment decisions must be based on personal
experience and theoretical advantages. See Lichtman, Ganocy, and Kim’s
comparative review of these procedures for a more in-depth discussion (38) (see also Chapter 43).
mild swan-neck and boutonnieère deformities. A variety of
reconstructive procedures are available for patients with more severe
impairment. Similarly, significant involvement of MP and wrist joints
may require surgical intervention.
Although
distal ulna resection has been more successful in the rheumatoid
population, a Sauveé-Kapandji procedure is more appropriate in certain
patients. This operation is preferable for younger, more active
patients who require a stable radioulnar surface (for arthroplasty
support), who demonstrate ulnar translocation of the carpus (less than
50% radiolunate contact), or who require augmentation of radiolunate
fusion (68).
from those for patients with RA because of the fixed soft-tissue
contractures and spontaneous joint fusions that accompany PA. MP
arthroplasties for extension contractures may restore some function,
but recurrent stiffness is not unexpected. Arthrodesis of PIP joints
that have spontaneously fused in severe flexion allows more functional
positioning of these digits (see Chapter 72).
Arthritis mutilans may require more complex reconstruction, including a
combination of arthrodesis and lengthening, to replace resorbed
phalanges (26,57,72).
deformity, because these become fixed in functional positions. The
surgeon should also be aware of the increased infection rates reported
in patients with PA (6). Preoperative betadine washing of the involved extremity has been suggested as a means to decrease perioperative infections.
Five percent to 10% of patients require surgical intervention.
Indications for surgery include nerve compression, tendon involvement
(entrapment or rupture), diagnosis and control of infection,
significant joint destruction, and cosmetically unacceptable tophi (35,47,64).
judicious excision of tophi, tendon debulking, and synovectomy. Tendon
rupture may be managed with side-to-side repair or tendon transfers. It
is best to treat isolated ruptures of FDS tendons nonoperatively if
there is no functional impairment. Unstable, painful joints may require
arthroplasty or arthrodesis.
occasions before deciding to perform thumb CMC arthroplasty on an
arthritic CMC joint. Some patients with stage III and IV radiographic
changes have few symptoms and remain surprisingly functional.
trapezium during exposure. Radiography does not reveal degenerative
changes of the scaphotrapezial joint in one third of cases (50).
If there is no scaphotrapezial arthritis or thumb web-space
contracture, the proximal one half of the trapezium may be left in
place; most surgeons prefer a total trapeziectomy.
hyperextension instability greater than 30°, stabilize the joint with a
volar plate advancement or MP arthrodesis.
instability of the end of the proximal ulna. Ulnar instability is most
likely to occur in patients with significant preoperative DRUJ
instability; neither this procedure nor other excisional arthroplasties
of the distal ulna adequately addresses this problem. In these cases,
continue above-elbow immobilization for 3 to 4 weeks before instituting
gentle active range-of-motion exercise.
subsequent development of erythema, warmth, pain, and drainage of
thick, opaque fluid. Differentiation of acute tophaceous gout from
infection may require aspiration and crystal analysis or occasional
incision and drainage.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
OA, Eaton RG. Save the Trapezium: Double Interposition Arthroplasty for
Stage 4 Degenerative Arthritis. Presented at the annual meeting of the
American Society for Surgery of the Hand, San Francisco, CA. September
15, 1995.
T, Balcom W, Morgan WJ, et al. Functional Outcome of Resection
Arthroplasty vs LRTI for Basal Joint Arthritis. Presented at the annual
meeting of the American Society for Surgery of the Hand, Cincinnati,
OH. October 27, 1994.
RI, Pellegrini VD Jr. Surgical Management of Basal Joint Arthritis of
the Thumb. Part II. Ligament Reconstruction with Tendon Interposition
Arthroplasty. J Hand Surg [Am] 1986;11:324.
RG, Lane LB, Littler JW, Keyser JJ. Ligament Reconstruction for the
Painful Thumb Carpometacarpal Joint: A Long-term Assessment. J Hand Surg [Am] 1984;9:692.
WN, Fox IR, Palella TD. Gout and Related Disorders of Purine
Metabolism. In: Kelley WN, Harris ED Jr, Ruddy S, Sledge CB, ed. Textbook of Rheumatology, 3rd ed. Philadelphia: WB Saunders, 1989:1395.
Viet D, Kerboull L, Lantieri LA, Collins DE. Stabilized Resection
Arthroplasty by an Anterior Approach in Trapeziometacarpal Arthritis:
Results and Surgical Technique. J Hand Surg [Am] 1996;21:194.
R, Gelberman R, McKeown L, et al. Basal Joint Arthritis: Trapeziectomy
with Ligament Reconstruction and Tendon Interposition Arthroplasty. J Hand Surg [Am] 1996;21A:202.
VD Jr, Burton RI. Surgical Management of Basal Joint Arthritis of the
Thumb. Part I. Long-term Results of Silicone Implant Arthroplasty. J Hand Surg [Am] 1986;11:309.
L, Konradsen L, Rechnagel K. Long-term Follow-up of the Cemented
Caffiniere Prosthesis for Trapeziometacarpal Arthroplasty. J Hand Surg [Br] 1991;16:428.
RL, Brown RE, Giansiracusa DF. Psoriatic Arthritis Mutilans: Digital
Distraction Lengthening: Pathophysiologic and Current Therapeutic
Review. J Hand Surg [Am] 1988;13:510.
J, Pess G, Gelberman RH. Treatment of de Quervain Tenosynovitis. A
Prospective Study of the Results of Injection of Steroids and
Immobilization in a Splint. J Bone Joint Surg Am 1991;73:219.
