Slipped Capital Femoral Epiphysis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Slipped Capital Femoral Epiphysis
Slipped Capital Femoral Epiphysis
Paul D. Sponseller MD
Description
-
SCFE is a disorder of the hips of
adolescents or preadolescents in which the femoral head is displaced
relative to the rest of the femur (Fig. 1).-
The femoral head remains in the acetabulum.
-
Most notable features: The outward rotation of the lower femur and leg and a limp
-
-
Classification:
-
Stable versus unstable (1):
-
Stable: Weightbearing without crutches is possible; 95% of patients have satisfactory results with proper treatment.
-
Unstable: Weightbearing without crutches
is not possible; compared with stable type, this type has a higher rate
of AVN and severe slip, so only 50% have satisfactory results with
treatment.
-
-
Chronologic (1):
-
Acute (<3 weeks)
-
Chronic (>3 weeks)
-
-
Anatomic (1,2):
-
Grade 0 (preslip): Impending slip with no discernible displacement
-
Grade I (mild): 1–33% slip (Fig. 2)
-
Grade II (moderate): 33–50% slip (Fig. 3)
-
Grade III (severe): >50% slip
-
-
Epidemiology
-
80% of cases occur during the growth phase of adolescence (boys, 10–16 years; girls, 10–14 years) (1).
-
Male:Female ratio, 2.4:1 (3)
Incidence
-
2–10 per 100,000 in the general population per year (3)
-
Substantial seasonal variation (3)
-
Highest in September, lowest in March
-
Variation is presumed to be secondary to late effects of vitamin D exposure or to activity.
-
Risk Factors
-
Adolescence
-
Male gender
-
Obesity: A weight:height ratio >90th percentile in 50–75% of patients (2)
-
African American race (3)
-
Contralateral SCFE: 50% of patients eventually have a bilateral slip (25% at initial presentation) (4).
-
Delayed skeletal maturity
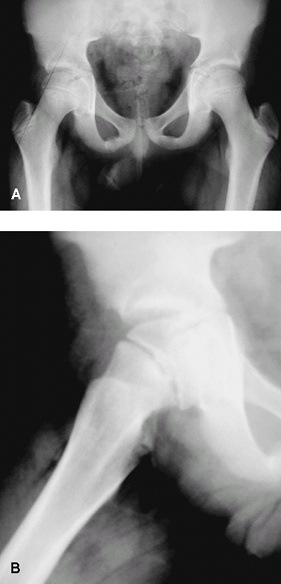
 Fig. 1. SCFE occurs through the growth plate, as seen in the right hip here.
Fig. 1. SCFE occurs through the growth plate, as seen in the right hip here.
Genetics
A 5–7% incidence is noted in family members of patients who have SCFE compared with 2–10 per 100,000 in the general population (1).
Etiology
-
Likely multifactorial, resulting in a weakened growth plate (physis) with higher-than-normal stresses placed across it
-
Endocrine factors such as hypothyroidism,
panhypopituitarism, hypogonadal conditions, and renal osteodystrophy
may weaken the physis, but such occurrences are rare (1). -
During the preadolescent or adolescent age, the growth plate is weakened by the process of rapid growth.
-
Increased shear stress may be generated by obesity or trauma.
Associated Conditions
-
Hypothyroidism
-
Hyperparathyroidism
-
Chronic renal failure
-
Radiation therapy to pelvis
![]() Fig. 2. Subtle (grade 1) SCFE. A: Note the subtle loss or epiphyseal height on the right hip and the greater lucency at the physis. B: Slip is more obvious on the lateral view.
Fig. 2. Subtle (grade 1) SCFE. A: Note the subtle loss or epiphyseal height on the right hip and the greater lucency at the physis. B: Slip is more obvious on the lateral view.
Signs and Symptoms
-
Symptom: Pain:
-
Acute (<3 weeks) or chronic (>3 weeks)
-
Occurs in the groin, medial thigh, or knee
-
-
Signs:
-
Decreased internal rotation of the hip
-
Limp
-
Trendelenburg gait
-
Antalgic gait (patient bears the weight on the affected side for as little time as possible.)
-
Externally rotated gait
-
-
Symptoms and signs of hypothyroidism or
other endocrine disorder, including cold intolerance, delayed bone age,
lethargy, coarse hair
History
-
The problem usually develops spontaneously, with no major incident, although in some patients, an episode of trauma may exist.
-
Often the pain is not severe, and the patient does not seek medical attention until late.
-
Some patients simply feel more easily tired.
-
Many patients present with a primary complaint of knee pain (a referral pattern), which often delays the proper diagnosis.
Physical Exam
-
Pain (mild) on palpation of groin or proximal femur
-
Pain greatest with internal rotation or abduction
-
Hip external rotation >internal rotation
-
The hip automatically goes into more external rotation as it is flexed.
-
Most patients have little or no internal rotation of the hip.
-
The affected limb rests in more external rotation than the contralateral limb.
-
Rule out endocrine disorders, such as
hypothyroidism, panhypopituitarism, hypogonadal conditions, and renal
osteodystrophy by history.
Tests
Lab
An endocrine workup is indicated for patients with
substantial delay in skeletal maturity or with symptoms suggesting an
endocrine problem.
substantial delay in skeletal maturity or with symptoms suggesting an
endocrine problem.
 |
|
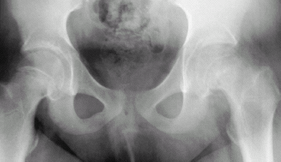
Fig. 3. This pelvic radiograph shows a grade-2 slip on the left hip and a grade-1 slip on the right.
|
P.405
Imaging
-
Radiography:
-
Plain AP and lateral views usually are adequate for diagnosis.
-
Findings are most pronounced on the lateral view.
-
-
Varus angulation of the epiphysis on the
femoral neck may be apparent, and the appearance of the epiphysis has
been likened to “ice cream falling off of its cone.” -
“Kline line” (loss of the intersection of
the epiphysis by the lateral cortical line of the femoral neck) is best
seen on a lateral view. -
Widening and blurring of the physis
-
A relative decrease in the height of the epiphysis (compared with contralateral side)
-
“Pistol-grip deformity”: In chronic stages, reactive bone forms along the inferomedial portions of the femoral neck.
-
-
CT or MRI usually shows an impending slip (also called a preslip) if the diagnosis is suspected or radiographs do not show it.
-
In a preslip, MRI shows increased edema in the region of the physis.
-
Differential Diagnosis
-
Perthes disease: Usually presents as a painless limp at a young age (4–8 years) and distinguishable on radiographs
-
Proximal femoral fractures: 90% with high-energy trauma (5)
-
A stress fracture of proximal femur is more common after skeletal maturity (5).
![]() Fig. 4. In situ fixation of SCFE with 1 cannulated screw.
Fig. 4. In situ fixation of SCFE with 1 cannulated screw.
General Measures
-
Complete avoidance of weightbearing is needed until the slip is stabilized.
-
Prevention of additional slip is the cornerstone of therapy.
-
Place the child immediately on bed rest and admit for surgery.
-
Surgery usually is done with 1 percutaneously placed screw to close the physis (Fig. 4).
-
-
Special Therapy
Physical Therapy
Postoperative instruction in ambulation with crutches or
a walker is indicated, with partial weightbearing if the slip is stable.
a walker is indicated, with partial weightbearing if the slip is stable.
Surgery
-
The goal is to prevent additional slippage by inducing closure of the physis.
-
1 guide pin is placed percutaneously from the anterior neck into the center of the femoral epiphysis.
-
The starting point is on the anterior femoral neck rather than on the lateral cortex of the proximal femur.
-
An appropriate-length 6.5- or 7.3-mm cannulated screw is placed over the guide wire.
-
Care is taken to avoid leaving a screw
that penetrates the chondral surface of the epiphysis because such
penetration likely will lead to chondrolysis. -
In severe unstable slips, some surgeons
attempt reduction of the slip by traction, gentle closed manipulation,
or open reduction. -
Osteotomies for severe slips may be performed to correct severe deformity.
-
Although controversial, prophylactic
fixation of the contralateral hip is justifiable in very young
patients, patients with known metabolic or endocrine disorders, or
patients in whom appropriate follow-up is unlikely.
-
-
Removal of the screw is not recommended.
-
For patients with degenerative joint
disease in later life resulting from SCFE, options are hip fusion in
the young patient and total hip replacement in the older patient.
Prognosis
-
Prognosis depends on the severity of the slip and the presence of complications.
-
Even without complications, a high incidence of degenerative joint disease still is possible (6).
-
If the patient is able to lose weight, it
will help decrease the risk of degeneration and increase the success of
total hip replacement.
Complications
-
Osteonecrosis:
-
Blood supply to the femoral head is lost, leading to collapse and severe degenerative joint disease.
-
Most strongly associated with unstable slip: 40% risk (5% risk for stable slips) (5).
-
-
Chondrolysis: Acute dissolution of articular cartilage with subsequent pain and stiffness
-
Degenerative joint disease: Undiagnosed
or untreated SCFE leading to degenerative joint disease is a common
cause of total hip replacement in the United States (4).
References
1. Kay
RM. Slipped capital femoral epiphysis. In: Morrissy RT, Weinstein SL,
eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:1085–1124.
RM. Slipped capital femoral epiphysis. In: Morrissy RT, Weinstein SL,
eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:1085–1124.
2. Mooney JF, III, Podeszwa DA. The management of slipped capital femoral epiphysis. J Bone Joint Surg 2005;87B:1024–1025.
3. Brown D. Seasonal variation of slipped capital femoral epiphysis in the United States. J Pediatr Orthop 2004;24:139–143.
4. Kocher
MS, Bishop JA, Hresko MT, et al. Prophylactic pinning of the
contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg 2004;86A:2658–2665.
MS, Bishop JA, Hresko MT, et al. Prophylactic pinning of the
contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg 2004;86A:2658–2665.
5. Mullins MM, Sood M, Hashemi-Nejad A, et al. The management of avascular necrosis after slipped capital femoral epiphysis. J Bone Joint Surg 2005;87B:1669–1674.
6. Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg 1991;73A:667–674.
Codes
ICD9-CM
732.2 Slipped capital femoral epiphysis
Patient Teaching
-
The child and parent must understand the
need for immediate nonweightbearing and early (usually the same day)
surgery to prevent additional slip and the need for careful
postoperative monitoring for osteonecrosis, chondrolysis, degenerative
joint disease, and (most importantly) SCFE of the contralateral hip. -
Any pain in the contralateral thigh should be reported immediately.
-
After surgery, the patient should maintain partial weightbearing to nonweightbearing for 6 weeks.
-
Vigorous sports are not allowed until the physis has closed (usually ~6 months postoperatively).
Prevention
Although controversial, prophylactic pinning of the
contralateral hip is recommended for patients in whom communication is
impaired or appropriate follow-up is unlikely (4).
contralateral hip is recommended for patients in whom communication is
impaired or appropriate follow-up is unlikely (4).
FAQ
Q: What causes the slip?
A:
It is a combination of increased forces (weight and activity) on a
physis that may be weakened by the growth spurt and other individual
factors.
It is a combination of increased forces (weight and activity) on a
physis that may be weakened by the growth spurt and other individual
factors.
Q: What is the risk of osteoarthritis?
A: It is increased to at least 25–50% at 30 years after the slip.