SURGICAL MANAGEMENT OF TORSIONAL DEFORMITIES OF THE LOWER EXTREMITIES
IX – PEDIATRIC DISORDERS > CHAPTER 168 – SURGICAL MANAGEMENT OF
TORSIONAL DEFORMITIES OF THE LOWER EXTREMITIES
evaluation, except perhaps for trauma, is for suspected torsional or
angular deformities of the lower extremities. Most of these children
are normal. Studies have shown that measurements of torsion and
angulation in children have wide ranges of normal values and that these
values change spontaneously with age until they reach the narrower
adult normal ranges (3,15,17,21,22).
true torsional or angular deformities, as well as to identify disease
entities that mimic or resemble these deformities. Do this with a
careful history and clinical assessment. Perform the torsional profile
examination and document it for all children who are referred for
evaluation of their lower extremities or gait abnormalities (18).
Clinical photographs are helpful for documentation, especially for
serial evaluations. Accurate anatomic diagnosis can be made by routine
radiographs for angular deformities and biplane radiographs or computed
tomography (CT) scan for torsional deformities. These studies are
reserved for severe deformities and for preoperative planning.
entities, convince the parents (and grandparents) that the apparent
deformity is a normal finding, although it may not represent the
average value. Point out that the apparent deformity will probably
become “more normal” with time. There is no convincing evidence that
orthotic management of torsional or angular variations or deformities
has any beneficial effect over simple observation of the natural
history alone (4,10). Therefore, the management decision is between observation with parent education, and surgery.
appearance. Education about natural history, the uselessness and
expense of orthotic devices, and the cost–benefit ratio of
surgery
establishes a rational basis for the observational approach. If the
parents are not convinced, see their child yearly and review the
torsional or angular profile with them. Clinical photographs are most
helpful in this setting. Also stress that even if full spontaneous
correction of torsional variations does not occur, the child may be
able to volitionally change the foot-progression angle when
self-appearance takes on increased meaning during adolescence.
study has shown that severe medial femoral torsion appears to adversely
affect running, but a moderate amount of torsion does not (23). Marked genu valgum appears to adversely affect running performances as well, but this has not been documented.
some variations, only the concurrence of lateral tibial torsion with
medial femoral torsion in late childhood has been documented (5). Likewise, genu valgum is often associated with foot pronation, but a cause-and-effect relationship has not been documented.
No documentation to date proves a cause-and-effect relationship between
such variations or deformities and arthritis of the hip or
patellofemoral joint.
surgery for torsional or angular variations or deformities are
extremely narrow. Because of the natural tendency for rotational
deformities to remodel and improve with growth, surgical treatment is
not indicated in children under 10–12 years of age. The decision hinges
primarily on cosmetic concerns in the adolescent.
and often at more than one level; for example, medial femoral torsion
often accompanies lateral tibial torsion. Surgical correction at one
level frequently necessitates surgical correction at the other level.
Staged unilateral surgery prolongs the period of temporary disability.
Simultaneous bilateral surgery increases the extent of temporary
disability.
15% complication rate was found in a review of operative treatment for
medial femoral torsion alone (20). In another
study, a 13% incidence of peroneal nerve palsy was reported following
proximal tibial rotational osteotomies if the fibula was not
osteotomized (16).
individualized. The patient’s general body habitus, the torsional and
angular profile at all levels, the patient’s emotional and psychologic
makeup, and the torsional and angular variations of other family
members must be considered. With these parameters carefully evaluated
and in perspective, consider surgical correction when (a) femoral
rotation values are more than three standard deviations from the mean,
(b) tibial rotation values are more than four standard deviations from
the mean, or (c) there is more than 25° of genu valgum in a child older
than 8 years. A busy, full-time pediatric orthopaedist may find one or
two torsional or angular variations or deformities per year that
require surgery. The operations to be described are used much more
frequently to correct the anteversion and coxa valga in cerebral palsy,
the lateral tibial torsion with ankle valgus in myelodysplasia, and the
angular deformities from old infection, partial physeal arrest,
metabolic disorders, ischemia, ionizing irradiation, or genetic
conditions.
proximally, in the mid shaft, or distally. The intertrochanteric region
of the femur is the preferred site for proximal osteotomies (19).
Osteotomy at this level is safe, heals rapidly, and leaves an
acceptable cosmetic scar. The intertrochanteric region is usually the
site of the pathology and is easily accessible. The essence of the
problem is torsional malalignment of the femoral neck and shaft, and it
is in the intertrochanteric region that these two anatomic structures
meet. If proximal femoral angulation is a problem in addition to
torsion, simultaneous corrections can be made with osteotomy at this
level. The technique and instrumentation for intertrochanteric
osteotomy are simple and no special training or equipment is required.
Early partial weight bearing is possible when rigid internal fixation
is used.
of the femur is an alternative for the older adolescent in whom there
is adequate intramedullary shaft diameter and little concern about
iatrogenic arrest of the greater trochanter (26,27).
The utility of this operation in the immature child, however, is
limited both by its complexity and by the small but real risk of
avascular necrosis of the femoral head related to the proximal
insertion site for the nail. The scar is acceptable cosmetically and
the patient may bear weight immediately. Special expertise and
equipment are required, and after surgery the femur may tend to
derotate around the rod unless a locked nail is used. Some angular
deformities can be corrected simultaneously (see Chapter 30).
gives the least acceptable scar, runs the highest risk of potential
injury to growth plates, is more likely to leave residual angulation,
and is farthest from the site of pathology, unless there is an
associated marked patella-tracking problem (7).
to determine which blade-plate angle will permit entrance of the blade
just distal to the greater trochanteric apophysis, and to determine
seating of the tip of the blade in the inferior proximal femoral neck.
-
Place the patient supine on a radiolucent
operating table extension to permit use of the image intensifier. Place
folded towels under the buttocks in such a way as to allow the lateral
soft tissues of the buttocks and thigh to overhang the edge of the
towels. Isolate the perineum with an adherent plastic drape. Prepare
both lower extremities from the iliac crests over most of the
hemipelvis down to the toes. -
Make a straight lateral longitudinal
incision extending distally from the greater trochanter. Incise the
fascia lata longitudinally. Incise the vastus lateralis transversely
just distal to the vastus ridge, and then longitudinally just anterior
to the linea aspera. Bring the transverse cut in the vastus lateralis
anteromedially, sufficient to see the base of the femoral neck. This
creates an L-shaped flap of the muscle that can be easily reattached at
the completion of the procedure. -
Expose the femur subperiosteally.
Carefully incise the linea aspera with a scalpel at the proposed level
of the osteotomy. Attempts at blunt elevation are difficult and may
result in plunging into highly vascularized soft tissues. Using image
intensification, internally rotate the extremity until the femoral neck
is in the horizontal plane. Place a Steinmann pin along the anterior
femoral neck in the proposed position of the blade and use the image
intensifier to confirm the appropriateness of the chosen angle (Fig. 168.1).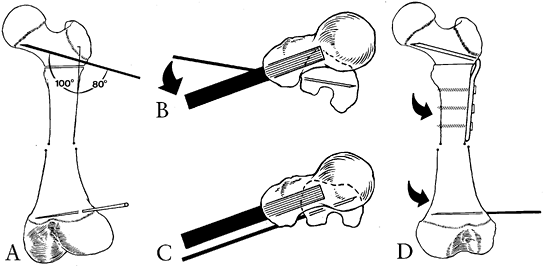 Figure 168.1. Proximal femoral rotational osteotomy with blade plate. A: Steinmann pin confirms appropriateness of 100° blade plate. Notice placement of distal femoral alignment pin. B: Initial position of distal pin and chisel. Angle represents degree of desired correction. C: Pin and chisel (which is actually the plate holder) aligned parallel after osteotomy. Note residual average amount of torsion. D: Final position with blade-plate fixation after intertrochanteric osteotomy.
Figure 168.1. Proximal femoral rotational osteotomy with blade plate. A: Steinmann pin confirms appropriateness of 100° blade plate. Notice placement of distal femoral alignment pin. B: Initial position of distal pin and chisel. Angle represents degree of desired correction. C: Pin and chisel (which is actually the plate holder) aligned parallel after osteotomy. Note residual average amount of torsion. D: Final position with blade-plate fixation after intertrochanteric osteotomy. -
Introduce the seating chisel (13),
mounted on the seating chisel guide, distal to the vastus ridge and in
the anterior half of the greater trochanter when viewed laterally. Hold
the chisel in the horizontal plane (which is the plane of the femoral
neck as positioned earlier) and angled away from the femoral shaft by
180° minus the predetermined blade-plate angle. Most importantly,
rotate the chisel until the flap of the seating chisel guide is exactly
in line with the long axis of the femur. Incorrect alignment of this
position will result in flexion or extension at the osteotomy site when
fixing the plate to the shaft. The proximal femoral shaft must be well
exposed to make this alignment possible. Insert the chisel to the
desired depth under image intensifier control. Check the frog-leg
lateral view as well as the anteroposterior view to guide your chisel
correctly. -
Insert a smooth Steinmann pin in the
distal femoral metaphysis perpendicular to the long axis of the femur
and rotated away from the chisel (in the direction of the rotational
deformity) by the desired degree of correction. Perform the osteotomy
with an oscillating saw beginning 5–10 mm distal to the entrance point
of the chisel and perpendicular to the long axis of the femur. -
Use a bone-holding clamp to stabilize the
proximal fragment as the chisel is removed. Carefully insert the blade
plate on the plate holder. It is vital to maintain your attention and
orientation during this maneuver or the blade plate could easily find a
new seat in the femoral neck. Confirm the position in two planes with
the image intensifier. -
Rotate the femoral shaft until the
Steinmann pin and plate holder are aligned parallel. Then clamp the
plate firmly on the shaft and rotate the extremity with a finger on the
osteotomy site to ensure that there is no false rotation at this level.
If the arc of rotation of the extremity is as desired, the side plate
can be attached to the shaft with cortical screws in the usual fashion.
Make sure that the side plate sits squarely on the shaft prior to
making drill holes. An oblique orientation will create undesired and
uncalculated additional rotation as the screws are tightened. It is
better to accept a few millimeters of translation than to accept an
oblique plate. Once again, check rotation and confirm final position of
instrumentation by image intensification. -
Reattach the vastus lateralis with 0
Vicryl sutures. Repair the fascia lata with the same suture material.
Use an absorbable subcuticular suture for the skin. -
A soft sterile dressing is all that is
required. Rigid external immobilization is not needed. The child may
begin touch-down weight bearing with crutches when comfortable, usually
within several days of surgery. If both femurs have been osteotomized,
weight bearing is not permitted. Continue this for 6–8 weeks, at which
time healing should be sufficient for full weight bearing. Remove
P.4282
the blade plate 1 year after surgery, with 6 weeks of protected weight bearing after plate removal.
-
The patient can be either lateral or
supine on a fracture table. Make a longitudinal incision just proximal
to the greater trochanter. Incise the abductors in the direction of
their fibers to expose the trochanteric recess just medial to the
greater trochanter. Open the medullary canal and then pass a
bulb-tipped guide down the canal. Ream the canal up to the desired
diameter. -
Place a smooth Steinmann pin
percutaneously in the lateral cortex of the proximal femur. Place a
second pin through the lateral cortex of the distal femur rotated
internally from the plane of the first pin by the desired amount of
rotational correction. -
Introduce the intramedullary saw down to the mid diaphysis under image intensifier control and make the osteotomy (Fig. 168.2).
Rotate the distal fragment until the two Steinmann pins are parallel;
then drive the intramedullary nail. Statically lock the intramedullary
nail with the osteotomy in compression. This guarantees that rotational
correction will not be lost. Immediate weight bearing with assistive
devices is usually possible.![]() Figure 168.2.
Figure 168.2.
Closed femoral rotational osteotomy with an intramedullary saw. (From
Winquist RA. Closed Shortening of the Femur: Utilizing a New Type of
Intramedullary Saw. In: Hempel D, Fischer S, eds. Intramedullary Nailing. New York: Thieme-Stratton, 1982;214.) -
Begin crutch-assisted weight bearing when
tolerated and continued for 6 weeks. Remove the nail approximately 1
year after the operation or when healing is solid (see Chapter 30).
-
Prep the entire leg and hip area free so
the limb is free to move in space. Make a longitudinal incision over
the posterolateral distal femur, but do not extend distally beyond the
lateral epicondyle of the femur. Lift the vastus lateralis fibers from
the posterior fascia lata, and incise the muscle along its femoral
insertion. Take time to carefully identify and cauterize the two or
three perforating vessels before dividing or tearing them. -
Strip the periosteum and retract it using
a Bennett or Hohmann retractor. As the periosteum is gently stripped
distally, a point of resistance will be felt; this is the region just
above the physis, and dissection should not be carried more distally.
An image intensifier may be used to confirm this position. -
Place a six-hole, 3.5 mm AO plate
longitudinally along the femur with the distal portion just at the end
of this subperiosteal dissection. Predrill, measure, record, and tap
the distal three holes. Steinmann pins may be inserted proximally and
distally to mark the desired rotational correction, as described before
for proximal femoral osteotomy. Do not put the pins where they will
interfere with the plate after derotation. -
Using an oscillating saw, make a
transverse saw cut just above the proximal hole. Fix the plate to the
distal three holes and rotate the femur into its corrected position,
using a Lowman clamp to fix the proximal plate into place. Check
clinical rotation, and, if correct, complete the fixation by attaching
the proximal screws in compression. It is unnecessary to contour the
plate to the minor bend of the lateral femur, since it will elastically
conform, enhancing medial compression. Check rotation again, and close
using absorbable sutures and subcuticular technique. -
Place the limb in a knee immobilizer and
protect from weight-bearing until callus is seen medially (usually 4–6
weeks). At this time, allow weight bearing. Knee function spontaneously
returns, and the plate may be electively removed at 1 year after the
surgery.
femoral rotational osteotomy other than those that accompany any
surgical procedure—superficial and deep wound infections, anesthetic
risk, and bleeding.
malrotation. When using the blade plate, clamp the side plate on the
femoral shaft and check rotation before inserting the screws. Also,
recheck rotation after the screws have been inserted. The position may
shift during screw insertion. Guide pins are not precisely accurate and
final
confirmation by intraoperative range of motion is required.
described steps are followed, and the final position is checked by
image intensification and by range of motion on the table. Angular
malunion can occur if the osteotomy is not precisely perpendicular to
the femoral shaft. Should either occur, the same careful assessment
used for the initial surgical decision should be made to determine if
repeat osteotomy is indicated.
intertrochanteric region is extremely rare. However, this could result
from failure to achieve reasonable apposition of bone, or from
distraction of the osteotomy by the hardware. In cases of delayed
union, prolonged external immobilization or prolonged partial weight
bearing is usually all that is necessary to achieve union.
easily miss the track left by the chisel. Maintain precise orientation
during the switch and insert it by pushing manually. Check final
position with the image intensifier.
potential stress risers for fractures. If a blade plate has been used,
there are multiple stress risers and temporary (6–8 weeks) partial
weight bearing with crutches must be enforced after removal of the
hardware.
intertrochanteric or subtrochanteric fracture—that is, by skin or
skeletal traction followed by spica casting. Internal fixation may be
used but is reserved for fractures that cannot be reduced or held well
in a spica cast.
narrower than for femoral rotational osteotomies. They are perhaps most
commonly performed in conjunction with femoral osteotomies in the case
of medial femoral torsion with lateral tibial torsion. Cosmesis is the
prime indication.
thigh–foot angle must be assessed to determine that the rotational
problem is in the tibia and not in the foot. Tibial rotational
osteotomy is reserved for tibial torsion problems. Transverse or
coronal plane deformities of the foot should be managed by appropriate
surgery on the foot.
accessibility, simplicity, safety, rapid healing, and cosmetically
acceptable scar. It is also versatile in cases where rotational
abnormalities are accompanied by distal angular abnormalities.
potential injury to the common peroneal nerve and the popliteal artery
at its trifurcation, as well as damage to the tibial apophysis. There
is a greater risk of compartment syndrome. Scars at the knee are
perhaps less cosmetically acceptable than scars at the ankle.
advantages of distal osteotomy over proximal or mid-shaft osteotomy are
overwhelming. We therefore feel there are no reasonable alternatives.
-
Position the patient supine on a
radiolucent operating table extension. Prepare both limbs from the toes
to the tourniquets on the proximal thighs (Fig. 168.3).
The distal thigh and knee must be exposed in the surgical field. In the
skeletally immature child, identify the distal tibial physis with the
image intensifier and mark its level on the skin.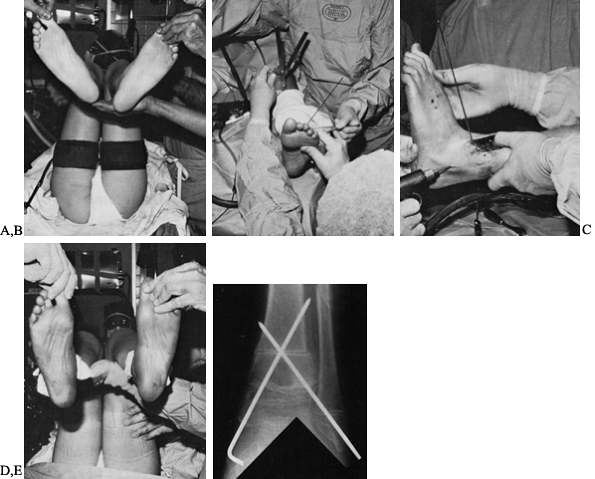 Figure 168.3. Distal tibial rotational osteotomy. A: Both limbs prepped and exposed up to tourniquets. B: Initial axial rotation between alignment pins checked with goniometer. C: Pins aligned parallel after osteotomy. Fixation pins enter malleoli and cross osteotomy. D: Final thigh–foot angle checked with hip and knee flexed 90° and also with joints in extension. E: Good early healing. Notice fibular osteotomy.
Figure 168.3. Distal tibial rotational osteotomy. A: Both limbs prepped and exposed up to tourniquets. B: Initial axial rotation between alignment pins checked with goniometer. C: Pins aligned parallel after osteotomy. Fixation pins enter malleoli and cross osteotomy. D: Final thigh–foot angle checked with hip and knee flexed 90° and also with joints in extension. E: Good early healing. Notice fibular osteotomy. -
Make a 5 cm longitudinal incision 1–2 cm
lateral and parallel to the tibial crest ending at the physeal line.
Retract the anterior compartment tendons laterally and protect the
anterior tibial neurovascular bundle. Incise the periosteum
longitudinally down to, but not across, the physis, and expose the
tibial metaphysis subperiosteally. -
Through the same skin incision, make an
extrafascial approach to the fibula between the lateral and anterior
compartments. Expose the fibula subperiosteally at a level 1–2 cm
proximal to the anticipated osteotomy of the tibia. Make a long oblique
osteotomy with an osteotome. -
Drill a smooth 3/32-inch
Steinmann pin into the anterior proximal tibia in the sagittal plane.
Drill a second smooth pin into the distal metaphysis just proximal to
the physis. This pin should be perpendicular to the long axis of the
tibia and axially rotated away from the first pin (in the direction of
the deformity) by the amount to be corrected. The goal is a
transmalleolar axis of +20° and a corresponding thigh–foot angle of +
10°. -
Perform the osteotomy 1–1.5 cm proximal
to and parallel with the physis using an oscillating saw. Then rotate
the distal fragment until the two Steinmann pins are aligned parallel.
Fix the osteotomy with crossed smooth 3/32-inch
Steinmann pins that enter each malleolus, cross the osteotomy, and
engage the tibial cortex of the proximal fragment. Occasionally a third
Steinmann pin will be needed for fixation across the osteotomy. Check
fixation and bone apposition with the image intensifier. Check the
angle of the transmalleolar axis and the thigh–foot angle with the hip
and knee flexed 90° and again with these joints in extension. -
Perform a blind, prophylactic,
subcutaneous fasciotomy of the anterior and lateral compartments with
Metzenbaum scissors. Be certain that the fascia is cut. -
Loosely reapproximate the tibial
periosteal edges with 2-0 Vicryl sutures. Following irrigation and
hemostasis, approximate the subcutaneous tissues with 3-0 Vicryl
sutures, and approximate the skin with running subcuticular 4-0 Vicryl
sutures. Bend the fixation Steinmann pins at the point they exit the
skin and cut them long. -
Apply a well-padded, bent-knee, long-leg
cast. A long-leg cast with 5° to 10° of knee flexion can be applied 3
weeks after surgery so partial weight bearing can begin. Remove the
pins at approximately 6–8 weeks. Use radiographs to determine the need
for further immobilization in a short-leg cast.
exposure of the fibula is necessarily limited. To avoid damage to the
superficial peroneal nerve or the peroneal vascular structures, perform
the fibular osteotomy with an osteotome.
distal tibial osteotomy, prophylactic subcutaneous anterior and lateral
compartment fasciotomy is advised. Nevertheless, frequent careful
postoperative assessment is
mandatory to detect impending compartment syndrome early. Perform four-compartment fasciotomy if it occurs.
intraoperatively, as described. The decision for repeat osteotomy
should be made as carefully as the initial decision to operate.
bearing in a cast with or without pins in place should effectively
treat delayed union.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
GM, Staheli LT. The Natural History of Torsion and Other Factors
Influencing Gait in Childhood: A Study of the Angle of Gait, Tibial
Torsion, Knee Angle, Hip Rotation, and Development of the Arch in
Normal Children. Clin Orthop 1974;99:12.
MM, Prietto C, Koffman M. Supracondylar Derotational Osteotomy of the
Femur for Internal Rotation of the Thigh in the Cerebral Palsied Child.
J Bone Joint Surg Am 1981;63:389.

