Pediatric Forearm
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > V – Pediatric Fractures and Dislocations > 45 – Pediatric Forearm
45
Pediatric Forearm
EPIDEMIOLOGY
-
These injuries are very common: They make
up 40% of all pediatric fractures (only 4% are diaphyseal fractures),
with a 3:1 male predominance in distal radius fractures. -
Eighty percent occur in children >5 years of age.
-
The peak incidence corresponds to the
peak velocity of growth when the bone is weakest owing to a
dissociation between bone growth and mineralization. -
Fifteen percent have ipsilateral supracondylar fracture.
-
One percent have neurologic injury, most commonly median nerve.
-
Of pediatric forearm fractures, 60% occur
in the distal metaphyses of the radius or ulna, 20% in the shaft, 14%
in the distal physis, and <4% in the proximal third.
ANATOMY
-
The radial and ulnar shafts ossify during the eighth week of gestation.
-
The distal radial epiphysis appears at
age 1 year (often from two centers); the distal ulnar epiphysis appears
at age 5 years; the radial head appears at age 5 to 7 years; the
olecranon appears at age 9 to 10 years. These all close between the
ages of 16 and 18 years. -
The distal physis accounts for 80% of forearm growth.
-
With advancing skeletal age, there is a
tendency for fractures to occur in an increasingly distal location
owing to the distal recession of the transition between the more
vulnerable wider metaphysis and the more narrow and stronger diaphysis. -
Osteology
-
The radius is a curved bone, cylindric in
the proximal third, triangular in the middle third, and flat distally
with an apex lateral bow. -
The ulna has a triangular shape throughout, with an apex posterior bow in the proximal third.
-
The proximal radioulnar joint is most
stable in supination where the broadest part of the radial head
contacts the radial notch of the ulna and the interosseous membrane is
most taut. The annular ligament is its major soft tissue stabilizer. -
The distal radioulnar joint (DRUJ) is
stabilized by the ulnar collateral ligament, the anterior and posterior
radioulnar ligaments, and the pronator quadratus muscle. Three percent
of distal radius fractures have concomitant DRUJ disruption. -
The triangular fibrocartilage complex
(TFCC) has an articular disc joined by volar and dorsal radiocarpal
ligaments and by ulnar collateral ligament fibers. It attaches to the
distal radius at its ulnar margin, with its apex attached to the base
of the ulna styloid, extending distally to the base of the fifth
metacarpal. -
The periosteum is very strong and thick
in the child. It is generally disrupted on the convex fracture side,
whereas an intact hinge remains on the concave side. This is an
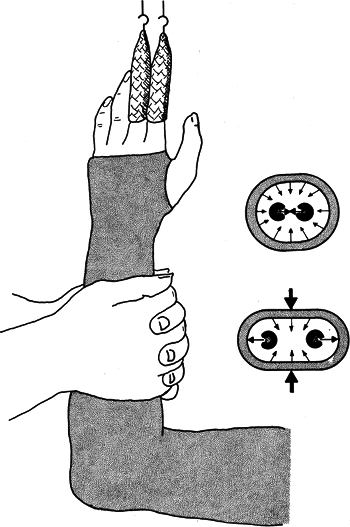
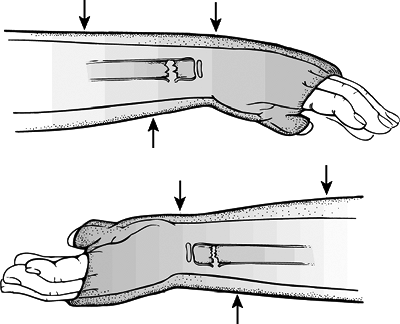
important consideration when attempting closed reduction.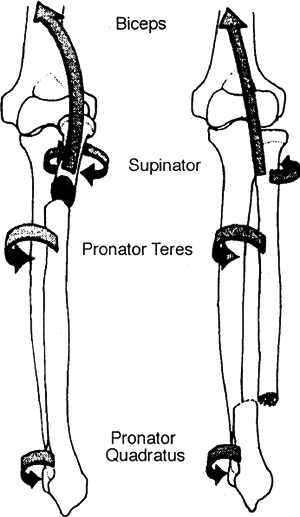 Figure 45.1. Deforming muscle forces in both bone forearm fractures.(From Cruess RL. Importance of soft tissue evaluation in both hand and wrist trauma: statistical evaluation. Orthop Clin North Am 1973;4:969.)
Figure 45.1. Deforming muscle forces in both bone forearm fractures.(From Cruess RL. Importance of soft tissue evaluation in both hand and wrist trauma: statistical evaluation. Orthop Clin North Am 1973;4:969.)
P.541 -
-
Biomechanics
-
The posterior distal radioulnar ligament is taut in pronation, whereas the anterior ligament is taut in supination.
-
The radius effectively shortens with pronation and lengthens with supination.
-
The interosseous space is narrowest in
pronation and widest in neutral to 30 degrees of supination. Further
supination or pronation relaxes the membrane. -
The average range of pronation/supination is 90/90 degrees (50/50 degrees necessary for activities of daily living).
-
Middle third deformity has a greater effect on supination, with the distal third affecting pronation to a greater degree.
-
Malreduction of 10 degrees in the middle third limits rotation by 20 to 30 degrees.
-
Bayonet apposition (overlapping) does not reduce forearm rotation.
-
-
Deforming muscle forces (Fig. 45.1)
-
Proximal third fractures:
-
Biceps and supinator: These function to flex and supinate the proximal fragment.
-
Pronator teres and pronator quadratus: These pronate the distal fragment.
-
-
Middle third fractures:
-
Supinator, biceps, and pronator teres: The proximal fragment is in neutral.
-
Pronator quadratus: Pronates the distal fragment.
-
-
Distal third fractures:
-
Brachioradialis: Dorsiflexes and radially deviates the distal segment.
-
Pronator quadratus, wrist flexors and extensors, and thumb abductors: They also cause fracture deformity.
-
P.542 -
MECHANISM OF INJURY
-
Indirect: The mechanism is a fall onto an outstretched hand. Forearm rotation determines the direction of angulation:
-
Pronation: flexion injury (dorsal angulation)
-
Supination: extension injury (volar angulation)
-
-
Direct: Direct trauma to the radial or ulnar shaft.
CLINICAL EVALUATION
-
The patient typically presents with pain, swelling, variable gross deformity, and a refusal to use the injured upper extremity.
-
A careful neurovascular examination is
essential. Injuries to the wrist may be accompanied by symptoms of
carpal tunnel compression. -
The ipsilateral hand, wrist, forearm, and
arm should be palpated, with examination of the ipsilateral elbow and
shoulder to rule out associated fractures or dislocations. -
In cases of dramatic swelling of the
forearm, compartment syndrome should be ruled out on the basis of
serial neurovascular examinations with compartment pressure monitoring
if indicated. Pain on passive extension of the digits is most sensitive
for recognition of a possible developing compartment syndrome; the
presence of any of the “classic” signs of compartment syndrome (pain
out of proportion to injury, pallor, paresthesias, pulselessness,
paralysis) should be aggressively evaluated with possible forearm
fasciotomy. -
Examination of skin integrity must be performed, with removal of all bandages and splints placed in the field.
RADIOGRAPHIC EVALUATION
-
Anteroposterior and lateral views of
forearm, wrist, and elbow should be obtained. The forearm should not be
rotated to obtain these views; instead, the beam should be rotated to
obtain a cross-table view. -
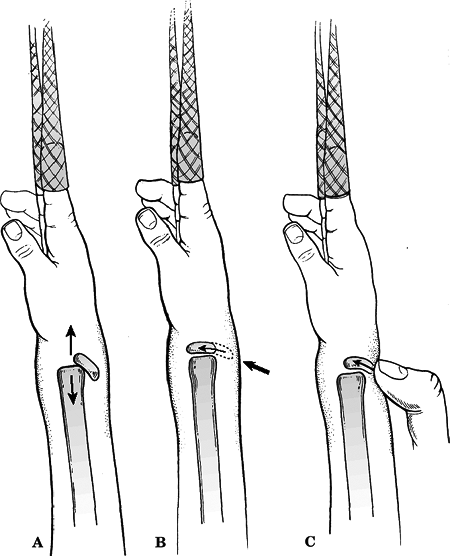
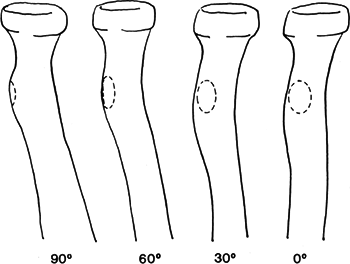
The bicipital tuberosity is the landmark for identifying the rotational position of the proximal fragment (Fig. 45.2):
-
Ninety degrees of supination: It is directed medially.
-
Neutral: It is directed posteriorly.
-
Ninety degrees of pronation: This is directed laterally.
-
In the normal, uninjured radius, the bicipital tuberosity is 180 degrees to the radial styloid.
-
RADIUS AND ULNA SHAFT FRACTURES
Classification
Descriptive
-
Location: proximal, middle, distal third
-
Type: plastic deformation, incomplete (greenstick), compression (torus or buckle), or complete
-
Displacement
-
Angulation
P.543
 |
|
Figure
45.2. The normal bicipital tuberosity from full supination (90 degrees) to midposition (0 degrees). In children, these characteristics are less clearly defined. (From Rockwood CA Jr. Wilkins KE, Beaty JH, eds. Rockwood and Green’s Fractures in Children, 4th ed, vol. 3. Philadelphia: Lippincott-Raven, 1996:515.)
|
Nonoperative Treatment
-
Gross deformity should be corrected on
presentation to limit injury to soft tissues. The extremity should be
splinted for pain relief and for prevention of further injury if closed
reduction will be delayed. -
The extent and type of fracture and the
child’s age are factors that determine whether reduction can be carried
out with sedation, local anesthesia, or general anesthesia. -
Finger traps may be applied with weights to aid in reduction.
-
Closed reduction and application of a
well-molded (both three-point and interosseous molds) long arm cast or
splint should be performed for most fractures, unless the fracture is
open, unstable, irreducible, or associated with compartment syndrome.-
Exaggeration of the deformity (often
>90 degrees) should be performed to disengage the fragments. The
angulated distal fragment may then be apposed onto the end of the
proximal fragment, with simultaneous correction of rotation (Fig. 45.3). -
Reduction should be maintained with pressure on the side of the intact periosteum (concave side).
-
-
Because of deforming muscle forces, the level of the fracture determines forearm rotation of immobilization:
-
Proximal third fractures: supination
-
Middle third fractures: neutral
-
Distal third fractures: pronation
-
-
The cast should be molded into an oval to
increase the width of the interosseous space and bivalved if forearm
swelling is a concern. The arm should be elevated (Fig. 45.4). -
The cast should be maintained for 4 to 6 weeks until radiographic evidence of union has occurred. Conversion to a short
P.544
arm cast may be undertaken at 3 to 4 weeks if healing is adequate.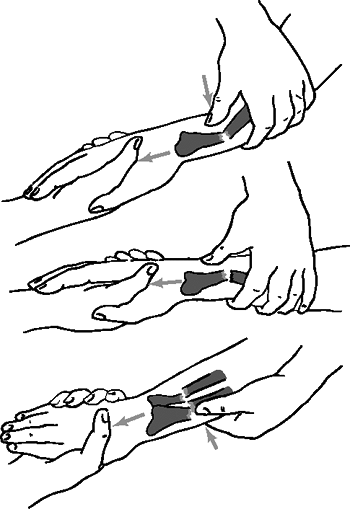 Figure
Figure
45.3. Top: Traction and counteraction of the thumb is used to increase
the deformity. Center: With traction still maintained, the thumb slips
farther distally to correct the angulation. It is best to avoid
disrupting the periosteum, but on occasion this is necessary. Bottom:
Ulnar or radial deviation can also be corrected by traction and thumb
pressure.(Redrawn from Weber BG, Brunner C, Freuler F. Treatment of Fractures in Children and Adolescents. New York: Springer-Verlag, 1980.) -
Acceptable deformity:
-
Angular deformities: Correction of 1
degree per month, or 10 degrees per year results from physeal growth.
Exponential correction occurs over time; therefore, increased
correction occurs for greater deformities. -
Rotational deformities: These do not appreciably correct.
-
Bayonet apposition: A deformity ≤1 cm is acceptable and will remodel if the patient is <8 to 10 years old.
-
In patients >10 years of age, no deformity should be accepted.
-
-
Plastic deformation: Children <4 years
or with deformities <20 degrees usually remodel and can be treated
with a long arm cast for 4 to 6 weeks until the fracture site is
nontender. Any plastic deformation should be corrected that (1)
prevents reduction of a concomitant fracture, (2) prevents full
rotation in a child >4 years, or (3) exceeds 20 degrees.P.545-
General anesthesia is typically necessary, because forces of 20 to 30 kg are usually required for correction.
![]() Figure
Figure
45.4. While the cast hardens, it is pressed together by both hands to
form an oval. This increases the width of the interosseus space.
Traction should be released gradually while this is done.(Redrawn from Weber BG, Brunner C, Freuler F. Treatment of Fractures in Children and Adolescents. New York: Springer-Verlag, 1980.) -
The apex of the bow should be placed over
a well-padded wedge, with application of a constant force for 2 to 3
minutes followed by application of a well-molded long arm cast. -
The correction should have less than 10 to 20 degrees of angulation.
-
-
Greenstick fractures: Nondisplaced or
minimally displaced fractures may be immobilized in a well-molded long
arm cast. They should be slightly overcorrected to prevent recurrence
of deformity.-
Completing the fracture decreases the
risk of recurrence of the deformity; however, reduction of the
displaced fracture may be more difficult. Therefore, it may be
beneficial to carefully fracture the intact cortex while preventing
displacement. A well-molded long arm cast should then be applied.
-
P.546
Operative Indications
-
Unstable/unacceptable fracture reduction after closed reduction
-
Open fracture/compartment syndrome
-
Floating elbow
-
Refracture with displacement
-
Segmental fracture
-
Age (girls >14 years old, boys >15 years old)
Surgical stabilization of pediatric forearm fractures is required in 1.5% to 31% of cases.
Operative Treatment
-
Intramedullary fixation: Percutaneous
insertion of intramedullary rods or wires may be used for fracture
stabilization. Typically, flexible rods are used or rods with inherent
curvature to permit restoration of the radial bow.-
The radius is reduced first, with
insertion of the rod just proximal to the radial styloid after
visualization of the two branches of the superficial radial nerve. -
The ulna is then reduced, with insertion
of the rod either antegrade through the olecranon or retrograde through
the distal metaphysis, with protection of the ulnar nerve. -
Postoperatively, a volar splint is placed
for 4 weeks. The hardware is left in place for 6 to 9 months, at which
time removal may take place, provided solid callus is present across
the fracture site and the fracture line is obliterated.
-
-
Plate fixation: Severely comminuted
fractures or those associated with segmental bone loss are ideal
indications for plate fixation, because in these patterns rotational
stability is needed. Plate fixation is also used in cases of forearm
fractures in skeletally mature individuals. -
Ipsilateral supracondylar fractures: When
associated with forearm fractures, a “floating elbow” results. These
may be managed by conventional pinning of the supracondylar fracture
followed by plaster immobilization of the forearm fracture.
Complications
-
Refracture: This occurs in 5% of patients and is more common after greenstick fractures and after plate removal.
-
Malunion: This is a possible complication.
-
Synostosis: Rare complication in
children. Risk factors include high-energy trauma, surgery, repeated
manipulations, proximal fractures, and head injury. -
Compartment syndrome: One should always bivalve the cast after a reduction.
-
Nerve injury: Median, ulnar and posterior
interosseous nerve (PIN) nerve injuries have all been reported. There
is an 8.5% incidence of iatrogenic injury in fractures that are
surgically stabilized.
MONTEGGIA FRACTURE
-
This is a proximal ulna fracture with associated dislocation of the radial head.
-
Comprises 0.4% of all forearm fractures in children.
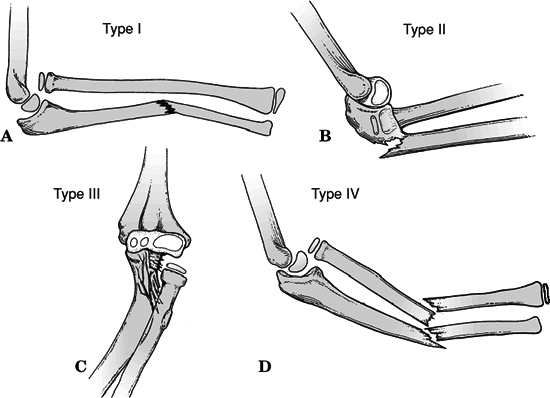 Figure
Figure
45.5. Bado classification. (A) Type I (anterior dislocation): The
radial head is dislocated anteriorly and the ulna has a short oblique
or greenstick fracture in the diaphyseal or proximal metaphyseal area.
(B) Type II (posterior dislocation): The radial head is posteriorly and
posterolaterally dislocated; the ulna is usually fractured in the
metaphysis in children. (C) Type III (lateral dislocation): There is
lateral dislocation of the radial head with a greenstick metaphyseal
fracture of the ulna. (D) Type IV (anterior dislocation with radius
shaft fracture): The pattern of injury is the same as with a Type I
injury, with the inclusion of a radius shaft fracture below the level
of the ulnar fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The peak incidence is between 4 and 10 years of age.
-
Ulna fracture is usually located at the junction of the proximal and middle thirds.
-
Bado classification of Monteggia fractures (Fig. 45.5):
P.547
| Type I: | Anterior dislocation of the radial head with fracture of ulna diaphysis at any level with anterior angulation; 70% of cases; may occur from a direct blow, hyperpronation, or hyperextension |
| Type II: | Posterior/posterolateral dislocation of the radial head with fracture of ulna diaphysis with posterior angulation; 3% to 6% of cases; a variant of posterior elbow dislocation when the anterior cortex of the ulna is weaker than the elbow ligaments |
| Type III: | Lateral/anterolateral dislocation of the radial head with fracture of ulna metaphysis; 23% of cases (ulna fracture usually greenstick); occurs with varus stress on an outstretched hand planted firmly against a fixed surface |
| Type IV: | Anterior dislocation of the radial head with fractures of both radius and ulna within proximal third at the same level; 1% to 11% of cases |
P.548
MONTEGGIA FRACTURE EQUIVALENTS (FIG. 45.6)
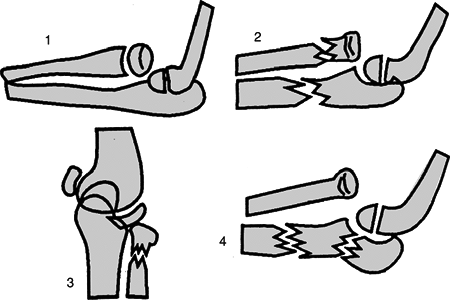 |
|
Figure 45.6. Type I Monteggia equivalents: 1, isolated anterior radial head dislocation; 2, ulnar fracture with fracture of the radial neck; 3, isolated radial neck fractures; 4, elbow (ulnohumeral) dislocation with or without fracture of the proximal radius; 5, supracondylar fracture in association with type I injury.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
| Type I: | Isolated radial head dislocation |
| Type II: | Ulna and proximal radius (neck) fracture |
| Type III: | Isolated radial neck fracture |
| Type IV: | Elbow dislocation (ulnohumeral) |
-
Treatment: Based on the type of ulna
fracture rather than on the Bado type. Plastic deformation is treated
with reduction of ulnar bow. Incomplete fractures are treated with
closed reduction and casting (Types I and III are more stable with
immobilization in 100 to 110 degrees of flexion and full supination).
Complete fractures are treated with Kirschner wires or intramedullary
fixation if one is unable to reduce the radial head or ulna. -
Ten degrees of angulation are acceptable in children <10 years old, provided reduction of radial head is adequate.
-
Complications:
-
Nerve injury: There is a 10% to 20% incidence of radial nerve injury (most common in Types I and III).
-
Myositis ossificans occurs in 7% of cases.
-
P.549
GALEAZZI FRACTURE
 |
|
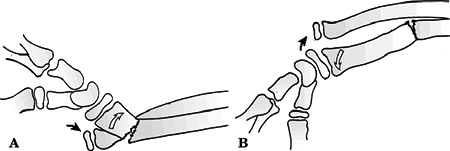
Figure
45.7. Walsh classification. (A) The most common pattern, in which there is dorsal displacement with supination of the distal radius (open arrow). The distal ulna (black arrow) lies volar to the dorsally displaced distal radius. (B) The least common pronation pattern. There is volar or anterior displacement of the distal radius (open arrow), and the distal ulna lies dorsal (black arrow). (From Walsh HPJ, McLaren CANP. Galeazzi fractures in children. J Bone Joint Surg Br 1987;69:730–733.)
|
-
A middle to distal third radius fracture,
with intact ulna, and disruption of the DRUJ. A Galeazzi equivalent is
a distal radial fracture with a distal ulnar physeal fracture (more
common). -
This injury is rare in children; 3% of distal radius fractures have concurrent DRUJ disruption.
-
Peak incidence is between ages 9 and 12 years.
-
Classified by position of radius (Fig. 45.7)
Type I: Dorsal displacement of distal
radius, caused by supination force. Reduce with forced pronation and
dorsal to volar force on the distal radius.Type II: Volar displacement, caused by pronation. Reduce with supination and volar to dorsal force on the distal radius. -
The operative indication is a failure to
maintain reduction. This is treated with cross pinning, intramedullary
pins, or plating. -
Complications:
-
Malunion: This results most frequently from persistent ulnar subluxation.
-
Ulnar physeal arrest: Occurs in 55% of Galeazzi equivalent fractures.
-
DISTAL RADIUS FRACTURES
Physeal Injuries
-
Salter-Harris Types I and II: Gentle
closed reduction is followed by application of a long arm cast or sugar
tong splint with the forearm pronated (Fig. 45.8);
50% apposition with no angular or rotational deformity is acceptable.
Growth arrest can occur in 25% of patients if two or more manipulations
are attempted.
P.550
Open reduction is indicated if the fracture is irreducible (periosteum or pronator quadratus may be interposed).![]() Figure
Figure
45.8. Acceptable method of closed reduction of distal physeal fractures
of the radius. (A) Position of the fracture fragments as finger trap
traction with countertraction is applied (arrows). (B) Often with traction alone the fracture will reduce without external pressure (arrows).
(C) If the reduction is incomplete, simply applying direct pressure
over the fracture site in a distal and volar direction with the thumb
often completes the reduction while maintaining traction. This
technique theoretically decreases the shear forces across the physis
during the reduction process.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Salter-Harris Type III: Anatomic
reduction is necessary. Open reduction and internal fixation with
smooth pins or screws parallel to the physis is recommended if the
fracture is inadequately reduced. -
Salter-Harris Types IV and V: Rare
injuries. Open reduction and internal fixation is indicated if the
fracture is displaced; growth disturbance is likely. -
ComplicationsP.551
-
Physeal arrest may occur from original
injury, late reduction (>7 days after injury), or multiple reduction
attempts. It may lead to ulnar positivity. -
Ulnar styloid nonunion is often indicative of a TFCC tear. The styloid may be excised and the TFCC repaired.
-
Carpal tunnel syndrome: Decompression may be indicated.
-
|
Table 45.1. Acceptable angular corrections in degrees
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
Metaphyseal Injuries
-
Classified by the direction of
displacement, involvement of the ulna, and the biomechanical pattern
(torus, incomplete, complete). -
Treatment
-
Torus fractures: If only one cortex is
involved, then the injury is stable and may be treated with protected
immobilization for pain relief. Bicortical injuries should be treated
in a long arm cast. -
Incomplete (greenstick) fractures (Table 45.1):
These have a greater ability to remodel in the sagittal plane than in
the frontal plane. Closed reduction with completion of the fracture is
indicated to reduce the risk of subsequent loss of reduction. The
patient should be placed in supination to reduce the pull of the
brachioradialis in a long arm cast. -
Complete fractures: Finger traps may
hinder reduction because the periosteum may tighten with traction. The
patient should be placed in a well molded long arm cast for 3 to 4
weeks (Fig. 45.9). Indications for percutaneous
pinning include loss of reduction, excessive local swelling preventing
placement of a well-molded cast, floating elbow, and multiple
manipulations. Open reduction is indicated if the fracture is
irreducible (<1% of all distal radius fractures), if the fracture is
open, or if the patient has compartment syndrome.
-
-
Complications
-
Malunion: Loss of reduction may occur in
up to 30% of metaphyseal fractures with bayonet opposition. Residual
malangulation of more than 20% may result in loss of forearm rotation. -
Nonunion: This rare complication is usually indicative of an alternate pathologic state.
 Figure
Figure
45.9. Three-point molding. Top: Three-point molding for dorsally
angulated (apex volar) fractures, with the proximal and distal points
on the dorsal aspect of the cast and the middle point on the volar
aspect just proximal to the fracture site. Bottom: For volar angulated
fractures, where the periosteum is intact volarly and is disrupted on
the dorsal surface, three-point molding is performed with the proximal
and distal points on the volar surface of the cast and the middle point
just proximal to the fracture site on the dorsal aspect of the cast.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Refracture: Usually results from an early return to activity (before 6 weeks).
-
Growth disturbance: The average
disturbance of growth is 3 mm (either overgrowth or undergrowth) with
maximal overgrowth in 9 to 12 year olds. -
Neurovascular injuries: One needs to avoid extreme positions of immobilization.
P.552 -