Rotational Deformities of the Lower Extremities
common presenting complaint of children in a pediatric orthopedic
office. The vast majority of deformities are a normal variation and
resolve spontaneously. However, parental concern is high, especially
among those who recall the use of splints and orthotics that “cured” a
similar deformity in a relative in the past. A complete physical
assessment of the rotational profile and ruling out more serious
diagnoses is only the first step. Parental education and reassurance
are necessary. In rare cases of severe or persistent deformity,
surgical intervention is warranted.
changes significantly as the child grows. In general, intrauterine
molding causes a lateral contracture of the soft tissues about the hip
and internal rotation about the tibia and foot. As the hip soft tissue
contracture resolves, for the most part the femoral anteversion
determines an internal rotation at the hip. At birth, the femoral
anteversion is around 30 degrees; it gradually decreases to 10 degrees
by maturity. Similarly, the tibia is most internally rotated in a
newborn child. It will also gradually externally rotate as the child
matures, from about 5 degrees of internal rotation to 10 degrees of
external rotation by 8 years of age. Despite wide individual variation,
an understanding of these general trends is important in following the
natural history of most rotational deformities.
gait. The deformity can occur at one anatomic level, or a combination
of levels. Rotation within two standard deviations (SD) from an average
value at a given anatomic level is termed version. Outside of 2 SD, the rotational alignment is defined as pathologic and called torsion.
Most cases of torsion represent the extremes of natural variability,
without a clear cause other than heredity. Intrauterine forces may play
a role in some cases of tibial torsion, particularly those associated
with metatarsus adductus. In both cases the in-toeing will usually
resolve spontaneously. Some other conditions can present as in-toeing and out-toeing.
Cerebral palsy and tibia vara (Blount’s disease) can present with
associated increased tibial torsion. Slipped capital femoral epiphysis
should be suspected in an obese adolescent presenting with out-toeing.
-
Foot progression angle
-
Hip rotation
-
Thigh-foot angle
-
Tibial torsion
-
Foot morphology
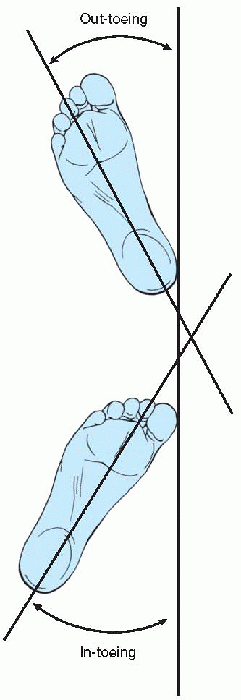
is the angle between the long axis of the foot and a line of the
direction of gait. Generally, the foot is slightly externally rotated,
about 5 to 10 degrees. By convention, external rotation is recorded as
a positive value, and internal rotation as a negative angle. The foot
progression angle is the summation of rotational alignment of the limb.
The remainder of the exam attempts to identify the level of pathology.
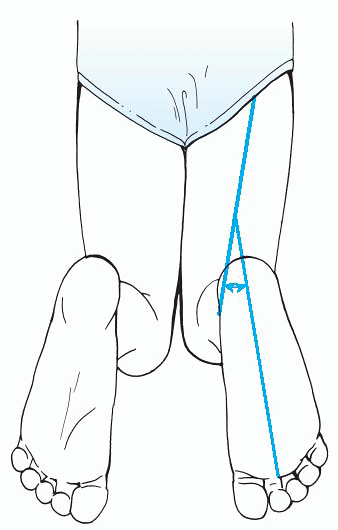
For hip rotation and thigh-foot angle exam the child is positioned
prone on the exam table. The tibial torsion and foot morphology could
be assessed in this same position or with the child sitting on the edge
of the examination table.
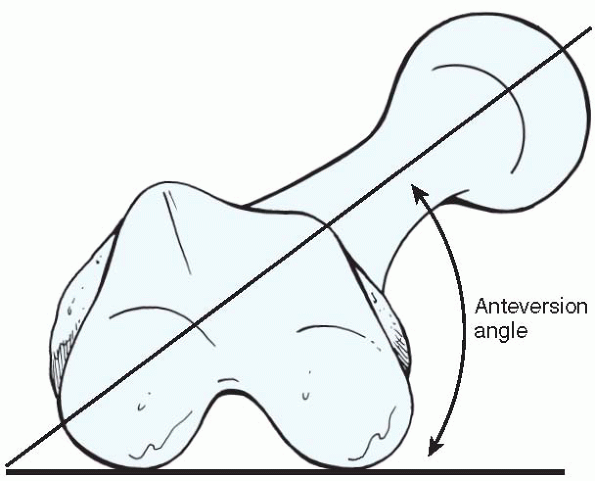
amount of femoral anteversion. The femoral anteversion angle is created
between the long axis of the femoral neck and a line drawn through the
medial and lateral condyles of the femur (Fig. 2-2). The amount of rotation is assessed by measuring the
angle between the exam table and lower legs with bent knees at a right angle (Fig. 2-3).
The amount of internal rotation decreases as a child’s anteversion
decreases with age. Concomitantly, the external rotation improves.
However, children with abnormally increased anteversion, or femoral
torsion, may continue to have abnormal internal rotation and might lack
external rotation. Femoral torsion usually begins to be noticeable in a
child as the lateral soft tissue contracture resolves after 2 or 3
years. Internal rotation approaching 90 degrees and external rotation
less than 15 degrees are abnormal. These are children frequently
described as sitting comfortably with their legs in a “W” or “TV”
position. Unusual gait patterns identified in these children have been
described as “eggbeater” gait. Patellar tracking problems can result,
particularly when associated with increased compensatory external
tibial torsion.
 |
|
Figure 2-1 The foot progression angle is the angle between the long axis of the foot and the direction of gait.
|
 |
|
Figure 2-2
The femoral anteversion angle is the angle between the long axis of the femoral neck and a line drawn through the medial and lateral condyles of the femur. |
 |
|
Figure 2-3
With the patient lying supine on the examination table, hip rotation is assessed by measuring the angle between the table and the lower legs. |
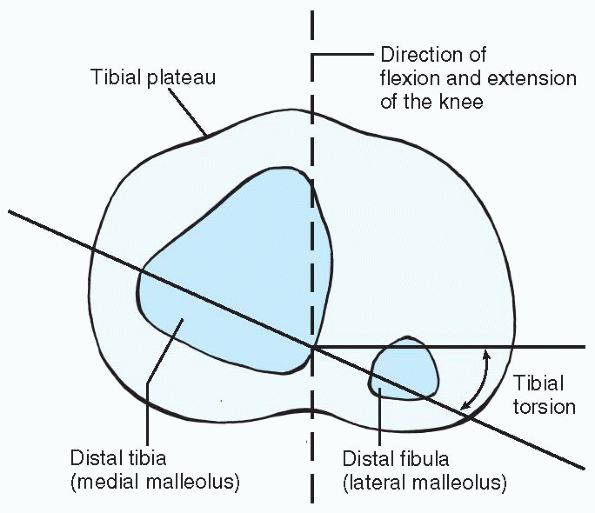
estimated by examining the thigh-foot angle. The angle formed between
the thigh and the long axis of the foot approximates the transverse
alignment of the tibia (Fig. 2-4), assuming the foot does not present with increased forefoot abduction/adduction. More
precisely this alignment is defined by the angle between the line
perpendicular to the axis of knee flexion/extension and the tibial
transmalleolar axis (Fig. 2-5).
Persistence of internal torsion through the tibia is called internal
tibial torsion, a common cause of in-toeing in the toddler age group.
 |
|
Figure 2-4
The thigh-foot angle is the angle formed between the thigh and the long axis of the foot, which approximates the transverse alignment of the tibia. |
 |
|
Figure 2-5
Tibial torsion is defined as the angle between the line perpendicular to the axis of knee flexion/extension and the tibial transmalleolar axis. |
 |
|
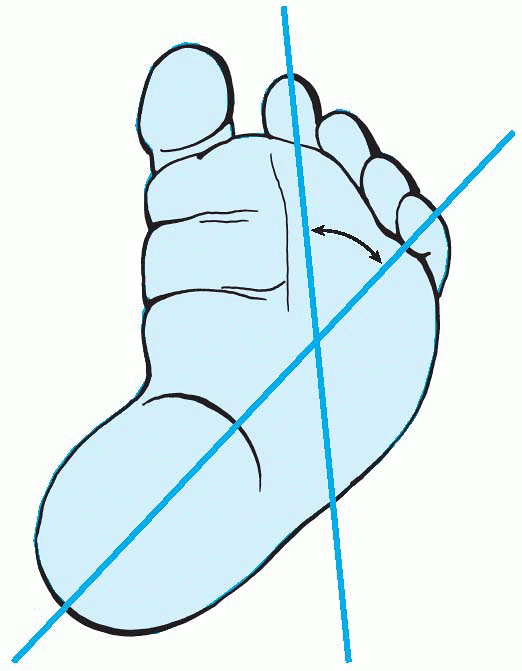
Figure 2-6 Metatarsus adductus.
|
is the final component of the rotational profile. Most commonly,
metatarsus adductus or other foot deformities can independently cause
in-toeing (Fig. 2-6). These tend to present
earlier than femoral or tibial deformities, since foot deformities are
apparent prior to ambulation. Deformities of the foot are discussed
specifically in a different chapter.
workup of a child with a rotational abnormality. The possibility of
neurologic disorders, skeletal dysplasias, joint or ligamentous laxity,
and metabolic disorders should be evaluated. The deformity can occur at
more than one level as well, either exaggerating or compensating for
another deformity.
conditions, and repeat follow-up over time may be necessary to evaluate
patients and the progression of the deformity. The following factors
raise clinical suspicion and require additional follow-up:
-
Unilateral conditions
-
History of progression
-
Deformities causing functional symptoms
-
Pain
-
Asymmetry
-
Trend not as suspected.
Spontaneous resolution is the norm. Only persistent deformity that
fails to resolve with growth and produces functional or cosmetic
concerns warrants further investigation. Ultimately, when treatment is
indicated, the only solution is a surgical correction. There has not
been any proven benefit to brace therapy of any kind for tibial or
femoral rotational deformities.
torsion was thought to protect against early arthrosis of the hip due
to abnormal forces across the joint. This has not been substantiated.
The indication for surgical treatment of persistent increased anterior
femoral torsion is functional or cosmetic deformity in a child older
than 8 years. Usually the residual femoral anteversion has to be
greater than 50 degrees to create significant functional/cosmetic
problems. Intertrochanteric or supracondylar derotational femoral
osteotomy is the treatment of choice, with use of K-wires to determine
the exact amount of angular correction intraoperatively.
children. Disability rarely comes from increased/decreased tibial
torsion, since there is such a wide range of normal values. Once
indicated by individual functional or cosmetic deformity, surgical
correction should be delayed until at least 8 years of age. Most
advocate a supramalleolar osteotomy stabilized with pins or a dynamic
compression plate and a short- or long-leg cast.
This “malignant malalignment syndrome” tends to induce patellofemoral
maltracking and pain, and is more likely to require intervention than
single level deformity. Again, no brace or nonoperative treatment has
shown any benefit. These patients are surgical candidates from about
the time that the patellofemoral symptoms are increasing with their
activities, usually around 10 years of age. In most cases, both
deformities must be addressed surgically for a successful outcome. This
can be best achieved by two-level osteotomy of the distal femur and
proximal tibia. Improvement in knee pain, gait patterns, and cosmetic
appearance can be expected.
ED, Schoenecker PL, Rich MM, et al. Treatment of severe torsional
malalignment syndrome. J Pediatr Orthop 1996;16: 484-488.
L. Rotational problems in children: an instructional course lecture,
the American Academy of Orthopaedic Surgeons. J Bone Joint Surg
1993;75A:939-949.
