Shin Splints
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Shin Splints
Shin Splints
John H. Wilckens MD
Marc Urquhart MD
Description
-
Shin splints present with pain and
discomfort in the leg from repetitive running on hard surfaces or
forceful excessive use of foot plantarflexors. -
Synonyms: Medial tibia stress syndrome; Periostitis of the tibia; Runner’s leg
Epidemiology
Shin splints occur commonly in teens and young adults.
Risk Factors
-
Running or jogging, especially a recent increase in distance or speed (1)
-
Pronated feet
-
Training errors
Etiology
Periostitis at the origin of the posterior tibialis muscle or the soleus muscle at the medial tibia or the soleus muscle (2)
Associated Conditions
-
Usually affects conditioning athletes
-
Any deformity of the leg (e.g., pes planus) that increases stress on the leg may predispose.
Signs and Symptoms
-
Exercise-induced pain occurs along the posteromedial border of the distal tibia.
-
Pain usually is dull, but can be intense, and is present at the onset of the workout.
-
Pain may persist after the workout but eventually dissipates.
Physical Exam
-
Tenderness to palpation along the medial border of the tibia (Fig. 1)
-
Pain with resisted plantarflexion and inversion
-
The clinical presentation of medial tibia
stress syndrome may closely resemble that of stress fractures and
exertional compartment syndrome, which can carry a far worse prognosis
if undiagnosed (3). -
Exertional compartment syndrome has
characteristic physical findings of anterolateral leg pain, commonly
over the anterior compartment; fascial hernias may be present.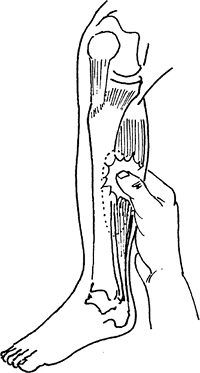 Fig. 1. Shin splints produce pain in the anterior or posterior border of the tibia over a long segment.
Fig. 1. Shin splints produce pain in the anterior or posterior border of the tibia over a long segment.
Tests
Imaging
-
Serial plain radiographs are normal but
are needed to rule out stress fractures, which usually are positive
after 2 weeks of symptoms. -
A bone scan may reveal diffuse
longitudinal uptake along the posteromedial border of the tibia,
whereas a stress fracture is a localized or transverse uptake on bone
scan. -
MRI also can be used to identify a stress fracture earlier.
Diagnostic Procedures/Surgery
Compartment pressure measurement with exercise may be
needed to diagnose exertional compartment syndrome if pain is
anterolateral.
needed to diagnose exertional compartment syndrome if pain is
anterolateral.
Pathological Findings
Inflammation at the origin of the soleus or PTT on the tibia
Differential Diagnosis
-
Stress fractures (4)
-
Chronic exertional compartment syndrome (5)
P.387
General Measures
-
Reduce training activity below symptom level
-
Ice on the area of injury
Special Therapy
Physical Therapy
-
Therapist-determined modalities
-
Strengthening and stretching exercises after acute symptoms disappear
-
Core strengthening
Complementary and Alternative Therapies
Orthotic or shoe modification to decrease pronation
Medication
First Line
-
NSAIDs
-
Analgesics
Surgery
Only after a documented trial of maximal nonoperative treatment has failed should posterior medial fascia release be considered.
Prognosis
-
Most cases respond well to nonoperative treatment.
-
Gradual return to activity can be expected.
-
Variation of the causative regimen of training and identification of training errors will help prevent recurrence.
Complications
Undiagnosed stress fracture can lead to complete fracture and displacement.
References
1. Pell RFI, Khanuja HS, Cooley GR. Leg pain in the running athlete. J Am Acad Orthop Surg 2004;12: 396–404.
2. Michael RH, Holder LE. The soleus syndrome. A cause of medial tibial stress (shin splints). Am J Sports Med 1985;13:87–94.
3. Glorioso
JE, Jr, Wilckens JH. Exertional leg pain. In: O’Connor FG, Wilder RP,
eds. Textbook of Running Medicine. New York: McGraw-Hill, 2001:181–197.
JE, Jr, Wilckens JH. Exertional leg pain. In: O’Connor FG, Wilder RP,
eds. Textbook of Running Medicine. New York: McGraw-Hill, 2001:181–197.
4. Rettig
AC, Shelbourne KD, McCarroll, Jr, et al. The natural history and
treatment of delayed union stress fractures of the anterior cortex of
the tibia. Am J Sports Med 1988;16:250–255.
AC, Shelbourne KD, McCarroll, Jr, et al. The natural history and
treatment of delayed union stress fractures of the anterior cortex of
the tibia. Am J Sports Med 1988;16:250–255.
5. Eisele SA, Sammarco GJ. Chronic exertional compartment syndrome. Instr Course Lect 1993; 42:213–217.
Codes
ICD9-CM
844.9 Shin splints
Patient Teaching
-
Identify training errors.
-
Emphasize the importance of modified activity followed by stretching and strengthening exercises.
-
Resumption of activity should be done gradually, below the level of the symptoms.
FAQ
Q: Do patients with shin splints need physical therapy?
A:
Although shin splints usually are self-limiting with rest,
identification of training errors, and gradual return to activity,
physical therapy can be helpful. Physical therapy can use modalities to
reduce the acute symptoms while identifying training errors,
flexibility, and limb alignment issues. Concentric and eccentric
strengthening of the lower extremity in addition to core strengthening
may reduce the risk of recurrence.
Although shin splints usually are self-limiting with rest,
identification of training errors, and gradual return to activity,
physical therapy can be helpful. Physical therapy can use modalities to
reduce the acute symptoms while identifying training errors,
flexibility, and limb alignment issues. Concentric and eccentric
strengthening of the lower extremity in addition to core strengthening
may reduce the risk of recurrence.
