Issues of the Newborn
|
|
just little children. Newborns have their own unique physiology and
pathology, hence the field of neonatology. Fortunately, there are
relatively few orthopaedic problems in this age group, but there is
adequate opportunity for the orthopaedic surgeon unaware of the unique
problems in newborns to get into trouble.
consultation in the newborn nursery is for an infant who does not move
an arm. The diagnoses that usually come quickly to mind are brachial
plexus injury or fracture. However, infection is the most important
diagnosis to make, as it can usually be treated if discovered early,
but may lead to permanent disability if the diagnosis is delayed (Fig. 10-1).
 |
|
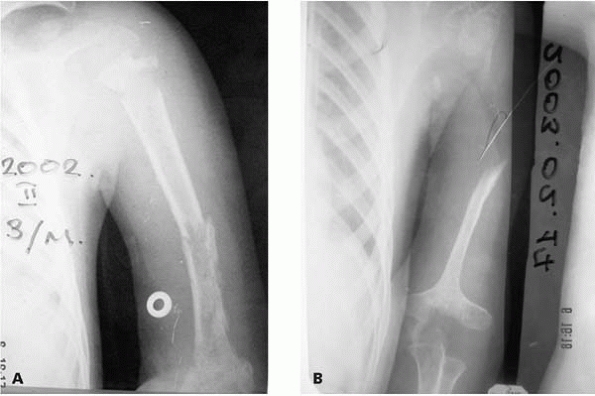
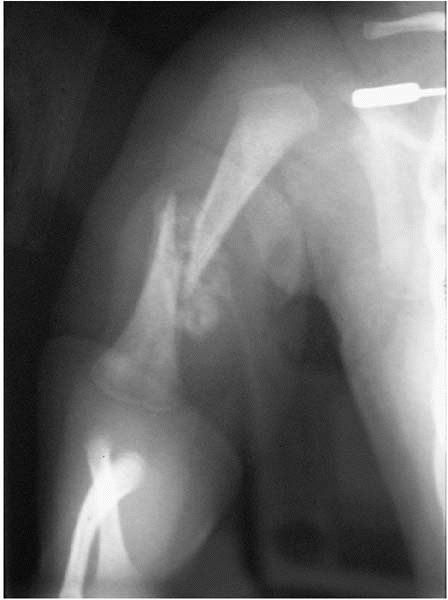
▪ FIGURE 10-1 A:
The diagnosis of neonatal infection was delayed in this child. An AP radiograph of the humerus at 3 months of age demonstrates significant osteomyelitis and subsequent fractures. B: Approximately 1 year later there is an absence of most of the proximal humerus and severe changes of the distal humerus as well. |
pseudoparalysis, and not move the limb voluntarily. To the
inexperienced, this may be misinterpreted as a true paralysis, or
brachial plexus injury. One approach to help differentiate
pseudoparalysis from paralysis is to shake the arm. If the child is
clearly in pain, the diagnosis of fracture or infection is likely. If
there is no sign of pain, the diagnosis of neurologic injury is likely.
Shaking the contralateral arm will provide a basis for comparison. A
potential pitfall of this approach is that an infant may have a
fracture and a brachial plexus injury, so
a neurologic exam is essential even in the case of a known fracture.
One series reported nearly 10% of newborns with a clavicle fracture
also had a brachial plexus palsy.1
in newborns, we enter into a different universe. In the first week of
life, normal white cell count ranges between 9000-30,000 cells/mL. A
total white cell count of <5000 cells/mL is generally considered to
be suggestive of infection, although some overlap between infected and
noninfected neonates does occur. Concerning thermoregulation,
over
half of neonates with sepsis present with fever but in 15% to 20% of
infected neonates hypothermia may be a leading sign of infection.
 |
|
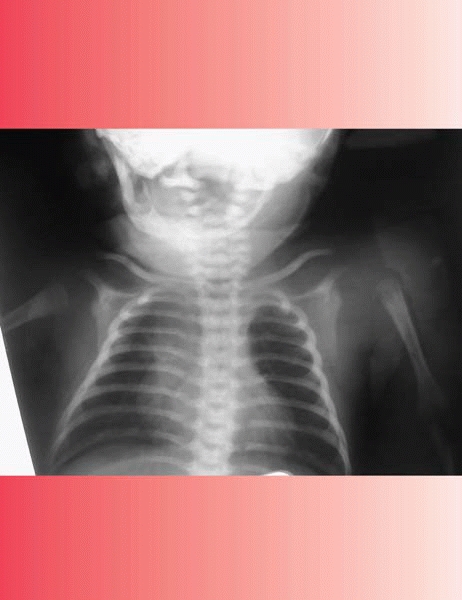
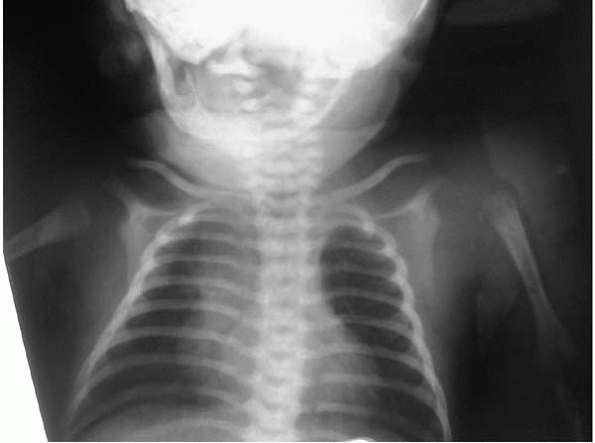
▪ FIGURE 10-2
Note lateral translation of the proximal humerus on this routine chest radiograph of a child with multiple medical problems in the NICU. The diagnosis of a septic shoulder was confirmed by ultrasound. |
examination by a limb that appears painful when moved. In the absence
of an obvious fracture on radiographs an ultrasound should be
performed, which may demonstrate a septic shoulder or subperiosteal
collection. Significant intraarticular pus may cause subluxation or
dislocation of the joint, as seen in Figure 10-2.
A septic shoulder requires urgent surgical drainage if the newborn’s
condition permits. Adjacent osteomyelitis should be expected, as
vessels cross the physis at this age. Of course many of the principles
here apply to the lower extremities as well. In particular, if there is
a septic hip, the other hip should be investigated closely with
ultrasound and/or aspiration (Fig. 10-3).
 |
|
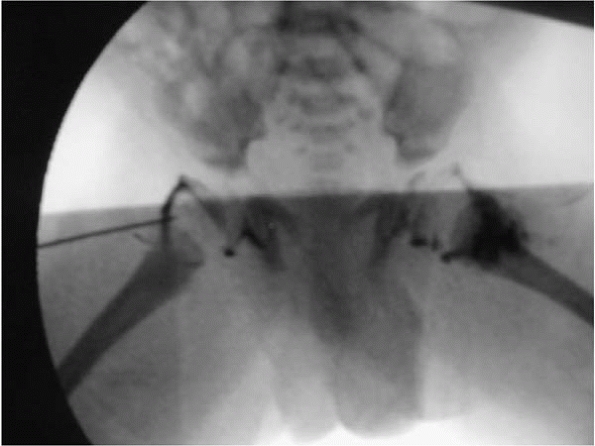
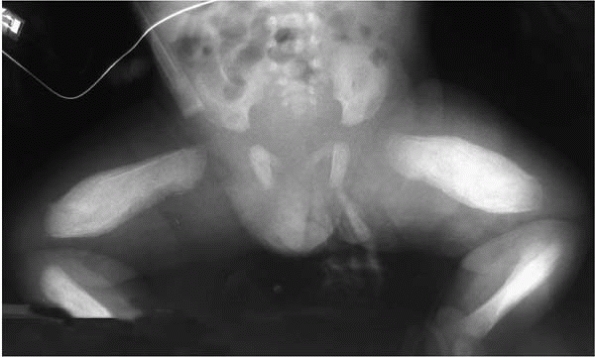
▪ FIGURE 10-3
In newborns with a septic hip, the opposite hip should be evaluated very carefully for sepsis with aspiration and/or ultrasound. |
In the most common type with upper plexus involvement, or Erb palsy,
the characteristic appearance of waiter’s tip—shoulder internal
rotation, elbow extension, forearm pronation, and wrist flexion (Fig. 10-4)—aids
in diagnosis. The surgeon should be aware that the phrenic nerve may be
involved as well as a Horner’s syndrome (ptosis, miosis and
enophthalmos). Physical therapy should be started to maintain motion,
as muscle imbalance may rapidly lead to contracture and joint
incongruence.
 |
|
▪ FIGURE 10-4 This patient with Erb palsy has the left arm in the characteristic “waiter’s tip” position.
|
The humeral head is not yet ossified, so the fracture is not easily
appreciated on plain radiographs. On exam there should be fullness and
tenderness locally, with an infection the same as for a fracture. An
ultrasound demonstrates the fracture. The following clinical algorithm
will help one make the diagnosis: arm hurts with movement, get
radiograph. If radiograph negative, get ultrasound.
more easily diagnosed on plain radiographs. Healing is very rapid, and
outcomes benign,3 usually needing immobilization for only 7 to 10 days (Fig. 10-7).
For children with multiple fractures think about osteogenesis
imperfecta, neonatal rickets, or neuromuscular disorders. Femur
fractures in newborns are commonly treated in newborns with a Pavlik
harness.
 |
|
▪ FIGURE 10-5
This transphyseal distal humerus fracture was sustained at birth. Note that this fracture may be difficult to identify on plain radiographs prior to the appearance of fracture callus. |
 |
|
▪ FIGURE 10-6
Standard slings and shoulder immobilizers do not fit the newborn with birth fractures of the upper extremity. This figure demonstrates one option of immobilization with cotton stockinette. The critical issue in treatment is to make certain a sling cannot migrate and obstruct the child’s airway. A simpler option is to pin the shirtsleeve to the torso of the shirt. |
 |
|
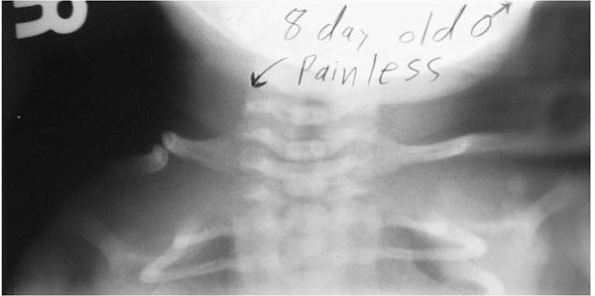
▪ FIGURE 10-7
Fracture of the humerus sustained at birth demonstrates significant callus by age 14 days, and was probably comfortable enough in 7 days to obviate the need for any immobilization. |
right, or doesn’t heal. Congenital pseudoarthrosis of the clavicle is a
rare condition in which the medial and lateral ossification centers of
the clavicle fail to unite (Fig. 10-8). Let the
parents know it is not related to birth trauma. The patient is
nontender, though a bump may be palpable, which can mislead one towards
a diagnosis of fracture. The condition almost always occurs on the
right side, and if on the left look for dextrocardia. The diagnosis is
confirmed by lack of callus on subsequent radiographs. The natural
history is often benign,5 though surgical treatment is likely successful if there is discomfort or the almost ubiquitous bump is cosmetically concerning.6
 |
|
▪ FIGURE 10-8 Pseudoarthrosis of the clavicle.
|
emergent. Consider the child’s overall health, surgeries, and problems
when deciding on timing and type of treatment. See Chapters 2 and 21 for further discussion.
and casting is probably best. Radiographs are of limited value in
newborns, but may be of assistance if the diagnosis is in question. Dr.
Sponseller warns us to be aware of underlying diagnoses: Larsen, myelo-
or lipomeningocele, arthrogryposis, Freeman-Sheldon, Mobius,
constriction band, diastrophic dysplasia, spondyloepiphyseal dysplasia
(SED). Also be aware of this look-alike condition: tibial hemimelia
(see Chapter 25).
posteromedial bowing of the tibia generally resolve spontaneously.
Gentle stretching of the foot by the parents may be helpful, though
particularly severe cases may warrant a few stretching casts.
Warn
the parents that with posteromedial bowing of the tibia a 3- to 4-cm
leg length discrepancy may result. Though scientific evidence is
lacking, severe calcaneal-valgus foot deformity has been anecdotally
associated with flat feet, external foot progression angle, and hip
dysplasia, so extra attention to these areas may be warranted.7
 |
|
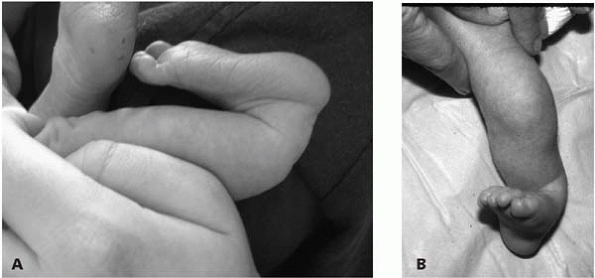
▪ FIGURE 10-9 In posteromedial bowing of the tibia the apex is in the tibia. A: Lateral view. B: AP view.
|
 |
|
▪ FIGURE 10-10 Calcanealvalgus foot. Note the apex of deformity is in the joint.
|
elbow are normal, and resolve with time. For example, one study found
the mean knee flexion contracture was 21 degrees at birth, reducing to
11 degrees at 3 months and 3 degrees at 6 months.8
If these “normal” contractures are not present, suspect trouble. Full
hip extension at birth is associated with hip dislocation.
hyperextension of the knee is more common in a subluxated knee. Early
serial casting for congenital knee dislocation/subluxation is
indicated, as earlier institution of casting
decreases the likelihood of needing surgery.9
Frequently after applying a cast to increase knee flexion, poor
circulation of the foot is noted, and the cast must be removed
immediately. We have found soft-fiberglass casting material to be
convenient and effective in this setting. Hip dislocations are present
in up to 50% of children with congenital knee dislocations,10
so all these children should have an ultrasound of the hips. Consider
Larsen’s syndrome if both pathologies are present. A Pavlik harness may
be used to treat simultaneous hip and knee dislocations.10
newborn. Although rare, immediate removal of the band to prevent
further damage to the digit or limb may be required. Dr. Walter Greene
has demonstrated that this can be done circumferentially in one stage.11
scenarios in infants. Stay out of trouble by differentiating the normal
from pathologic. Physiologic periosteal reaction of the newborn is a
common finding in about 35% of infants aged 1 to 4 months. This is
usually an incidental finding on radiographs obtained for other
reasons. The periosteal reaction is thin, even, and symmetric,
occurring along the femur, tibia, and humerus on both sides. Periosteal
reaction is potentially abnormal if the child is premature or is less
than 1 month or greater than 4 months of age. A thickness of greater
than 2 mm of subperiosteal new bone is likely to be abnormal and should
prompt further diagnostic evaluation.12 It has also been shown that newborns receiving prostaglandin infusion13 or on extracorporeal membrane oxygenation (ECMO)14
can have periosteal new bone formation. Pathologic causes of periosteal
new bone formation in infants include Caffey’s disease (most commonly
involving the mandible, ulna, and tibia) (Fig. 10-11), congenital syphilis, infection, malignancy, child abuse, and scurvy.
 |
|
▪ FIGURE 10-11 Caffey’s disease.
|
-
If a limb is not moving voluntarily, consider fracture, nerve injury, and most important, infection.
-
An ultrasound of the shoulder may help differentiate infection from a transphyseal fracture.
-
Traditional signs of
infection such as temperature, serum white cell count, and ESR are less
reliable in newborns than older children. Neutropenia (WBC count
<5,000 in a newborn) is the best to “rule in” and CRP is the best to
“rule out” infection. -
Significant flexion
contractures of the knee, hip and elbow are physiologic in the newborn,
and resolve spontaneously over the first year of life.
TY, Hung FC, Lu YJ, et al. Neonatal clavicular fracture: clinical
analysis of incidence, predisposing factors, diagnosis, and outcome. Am J Perinatol. 2002;19(1):17-21.
DA, Mooney JF, Cramer KE, et al. Comparison of Pavlik harness
application and immediate spica casting for femur fractures in infants.
J Pediatr Orthop. 2004;24:60-62.
DS, Spevak MR, Fletcher K, et al. Physiologic subperiosteal new bone
formation: prevalence, distribution, and thickness in neonates and
infants. AJR. 2002;179(4):985-988.
S, Cilliers A, Beckh-Arnold E, et al. Cortical hyperostosis in an
infant on prolonged prostaglandin infusion: case report and literature
review. J Perinatol 2004;24(4):263-265.
MS, Lovretich JO. Periosteal reaction of the long bones associated with
extracorporeal membrane oxygenation: cause and effect? Pediatric Radiology 1999;29(10):797-798.