Computed Tomography
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Computed Tomography
Computed Tomography
William J. Didie MD
Laura M. Fayad MD
Description
-
CT is a noninvasive diagnostic technique that uses a rotational radiographic source to generate cross-sectional images.
-
CT is particularly advantageous for
musculoskeletal imaging when used with multiplanar, volume-rendered
reconstruction techniques.
Etiology
-
Chronology of development (1):
-
1972: Introduction
-
1974–1976: 1st clinical scanners installed
-
1980: Became widely available
-
1985–1986: Introduction of modern
applications, such as dynamic imaging, multiplanar reformatting, and 3D
CT with volume rendering and shaded surface display -
1989: Beginning of routine spiral scanning
-
-
Advantages:
-
Rapid image acquisition, particularly useful in pediatric, trauma, and very ill patients, with reduced need for sedation
-
Clear evaluation of anatomically complex
areas not always well evaluated by plain radiographs, such as the axial
skeleton and small joints (ankle and wrist) -
Multiplanar reformatted and 3D
capabilities: For 16-slice multidetector CT and beyond, acquisition in
only 1 plane is required because the data set may be reconstructed into
different planes and perspectives. -
May virtually eliminate streak artifact
secondary to metal hardware through volume rendering of a multidetector
CT axial database (Fig. 1).-
MRI evaluation in such patients often is extremely limited.
-
-
Can safely image patients with contraindications to MRI, such as aneurysm clips, pacemaker, or orbital metallic fragments
-
Cost-effective modality for a wide range of clinical problems
-
Widely available
-
-
Disadvantages:
-
Inferior to MRI for bone marrow and soft-tissue details
-
Requires ionizing radiation exposure
-
More expensive than plain radiography
-
If contrast is necessary, a risk of allergic reaction or contrast nephropathy exists.
-
Tests
-
Skeletal pathology:
-
Typically imaged with thin-section collimation (0.75 mm for a 16-slice multidetector CT).
-
Postprocessing of data into multiplanar reformatted images and 3D reconstructions is performed on a workstation.
-
-
Soft tissues:
-
Thin-section imaging is not as crucial as for the evaluation of the skeleton.
-
Reconstructed slice thickness typically is set at 2–3 mm.
-
Studies performed to evaluate a
soft-tissue mass, potential abscess, or vascular injury typically
require the administration of intravenous contrast material, requiring
injection rates of 3 mL/sec.-
Intravenous contrast should be used with caution in patients with renal insufficiency.
-
Patients with potential allergies to intravenous contrast should be identified, premedicated, or not injected.
-
-
Differential Diagnosis
-
Postoperative indications:
-
Identification of complications of hardware implantation, such as osteomyelitis or fracture
-
Identification of potential tumor recurrence in the presence of hardware
-
Detection of retained foreign body
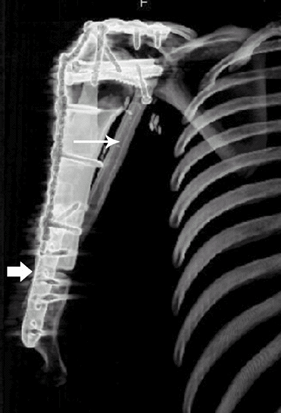 Fig. 1. Coronal oblique volume-rendered 3D CT showing reconstruction of the humerus with an allograft (thick arrow marks allograft–host junction). Healing is augmented by a vascularized fibular graft (thin arrow). Note the minimized streak artifact around the metal hardware on this 3D CT.
Fig. 1. Coronal oblique volume-rendered 3D CT showing reconstruction of the humerus with an allograft (thick arrow marks allograft–host junction). Healing is augmented by a vascularized fibular graft (thin arrow). Note the minimized streak artifact around the metal hardware on this 3D CT.
-
-
Oncology indications:
-
Detection of calcification within a
lesion: Distinction of myositis ossificans and neoplasm by detecting
pattern of mineralization -
Characterization of cortical and periosteal changes for distinguishing benign and malignant processes
-
Assessment of bone destruction and fracture risk
-
Definitive treatment of osteoid osteomas with CT-directed radiofrequency ablation of the nidus
-
Detection of compartmental and neurovascular involvement, although typically more commonly assessed by MRI
-
-
Trauma indications:
-
Definition or exclusion of a fracture
that is equivocal on plain radiograph: 3D CT and multiplanar
reconstructions are particularly useful for detecting fractures
oriented in the axial plane. -
Determination of extent of fracture, including physeal and intra-articular involvement
-
Identification of intra-articular fracture fragments
-
Identification of fracture nonunion
-
Detailed cervical spine evaluation in moderate- and high-risk trauma patients
-
-
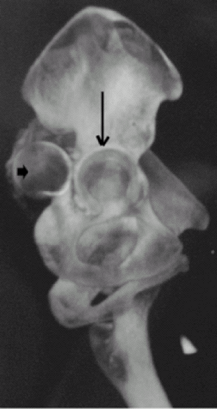
Evaluation of anatomically complex areas, such as pelvis, scapula, wrist, ankle, and spine (Fig. 2)
![]() Fig.
Fig.
2. Sagittal oblique volume-rendered 3D CT image of the pelvis shows
posterior dislocation of the right hip. The femoral head (short arrow) and empty acetabular fossa (long arrow) are marked. -
Infection indications:
-
Determination of compartments of tissue
involvement (bone, muscle, fascia, subcutaneous tissue) necessary for
patient triage as medical or surgical candidates -
Assessment of response to antibiotic therapy
-
-
Pediatric indications (2):
-
Skeletal dysplasias:
-
Useful for applications, such as
dysplasias, that require imaging of a large field of view to define the
anatomy and evaluate the skeleton postoperatively -
Such cases often are difficult to image completely by radiography or MRI.
-
-
DDH:
-
Diagnosis usually is made by physical examination, plain radiographs, and ultrasound.
-
CT may be used in difficult cases or, with low-dose scanning, as an imaging alternative.
-
CT more commonly is used to define success of reduction after cast placement.
-
-
SCFE:
-
Detection of contralateral involvement with coronal and sagittal display
-
Exclusion of other causes of hip pain, such as osteoid osteoma or septic joint
-
-
Legg-Calvé-Perthes disease:
-
Presurgical: Planning for identification of severity of disease
-
Postoperative: Assessment for determination of success of intervention or evaluation of new symptoms
-
-
Pectus deformities:
-
Surgical approach and anatomic definition, especially if initial repair was unsuccessful
-
-
Tarsal coalition:
-
CT reconstruction in multiple planes to define the different osseous and nonosseous coalitions
-
-
P.87
Alert
Pediatric Considerations
-
Children are more sensitive to radiation
than are adults and are more likely to develop radiation-induced
neoplasm over a lifetime (3–5). -
CT exposure parameters should be adjusted, and only necessary examinations performed (3–5).
-
Multiphase imaging (both with and without contrast) should be avoided.
-
Multidetector technology with volume visualization and postprocessing minimizes radiation exposure.
Pregnancy Considerations
-
Scan volume should be limited to necessary anatomy.
-
Multiphase imaging should be avoided.
-
Establish protocols that appropriately use radiation and are tested regularly by departmental medical physicists.
-
The magnitude of leukemogenic fetal risk is uncertain.
-
No long-term effects of intravenous contrast on fetus are known, but the usual dose should be reduced by 59% to 0.5 mL/kg (6).
-
Consider nonionizing alternative modalities, such as MRI or ultrasound, if possible.
-
Lead shield the abdomen and pelvis, if possible.
-
Nursing mothers should wait 24 hours after intravenous contrast administration to resume breast-feeding.
Complications
-
Contrast allergy:
-
Risk factors include history of asthma and previous reactions.
-
Option to premedicate at-risk patients with steroids and diphenhydramine
-
-
Contrast nephropathy:
-
Risk factors include pre-existing renal disease, multiple myeloma, diabetes, and dehydration
-
Aggressive hydration and use of low-osmolar agents
-
References
1. Siemens Medical. CT: Its History and Technology. (PDF file available at http://www.medical.siemens.com/siemens/en_US/gg_ct_FBAs/files/brochures/CT_History_and_Technology.pdf). Accessed 10/12/05.
2. Fayad
LM, Johnson P, Fishman EK. Multidetector CT of musculoskeletal disease
in the pediatric patient: principles, techniques, and clinical
applications. Radiographics 2005;25:603–618.
LM, Johnson P, Fishman EK. Multidetector CT of musculoskeletal disease
in the pediatric patient: principles, techniques, and clinical
applications. Radiographics 2005;25:603–618.
3. Boice JD, Jr, Miller RW. Childhood and adult cancer after intrauterine exposure to ionizing radiation. Teratology 1999;59:227–233.
4. Brenner DJ, Elliston CD, Hall EJ, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176: 289–296.
5. Boone JM, Geraghty EM, Seibert JA, et al. Dose reduction in pediatric CT: a rational approach. Radiology 2003;228:352–360.
6. Wagner
LK, Huda W. When a pregnant woman with suspected appendicitis is
referred for a CT scan, what should a radiologist do to minimize
potential radiation risks? Pediatr Radiol 2004;34:589–590.
LK, Huda W. When a pregnant woman with suspected appendicitis is
referred for a CT scan, what should a radiologist do to minimize
potential radiation risks? Pediatr Radiol 2004;34:589–590.
Additional Reading
Fishman EK, Kuszyk B. 3D imaging: musculoskeletal applications. Crit Rev Diagn Imaging 2001;42:59–100.
Karcaaltincaba
M, Akata D, Aydingoz U, et al. Three-dimensional MDCT angiography of
the extremities: clinical applications with emphasis on musculoskeletal
uses. AJR Am J Roentgenol 2004;183:113–117.
M, Akata D, Aydingoz U, et al. Three-dimensional MDCT angiography of
the extremities: clinical applications with emphasis on musculoskeletal
uses. AJR Am J Roentgenol 2004;183:113–117.
Patient Teaching
-
The patient should expect to be in the CT
scanner, motionless, for up to several minutes during the acquisition
of images, but with modern-day scanners, a typical CT examination may
require <30 seconds. -
Intravenous contrast may be administered, depending on the indication, and informed consent should be obtained.
FAQ
Q: How much time does a CT scan require?
A: Depending on the type of scanner available, as short as 10 seconds (64-slice multidetector CT) and usually <1 minute.
Q: Can I order a CT scan on a pregnant patient?
A: Yes, if clinically necessary. However, the protocol is adjusted to reduce radiation exposure.
Q: Can I order a CT scan for a patient with a pacemaker, aneurysm clips, or other metal hardware?
A: Yes. Metal is not a contraindication for CT.
Q: How does metal hardware affect CT imaging?
A: Metal creates streak artifact. This artifact can be reduced or eliminated with volume-rendered 3D CT.
Q: How do I order a 3D CT?
A:
3D CT is most effective with advanced CT technology (16-slice
multidetector CT and beyond). A discussion of imaging equipment and
techniques with the radiologist is the 1st step.
3D CT is most effective with advanced CT technology (16-slice
multidetector CT and beyond). A discussion of imaging equipment and
techniques with the radiologist is the 1st step.