SURGERY FOR DEVELOPMENTAL DYSPLASIA OF THE HIP
dysplasia of the acetabulum and subluxation or dislocation of the
femoral head from the acetabulum, if present at birth, have been known
in the past as dysplasia or dislocation of the hip. Westin et al. (30)
reported on late dislocation of the hip in children with apparently
normal neonatal clinical and radiographic examinations, which they
termed developmental dysplasia of the hip (DDH). Since then, the term DDH
has come to be used to describe all dysplasias of the hip, reflecting
the uncertainty about the exact time of onset and detection of the
condition. Many mechanisms for DDH have been proposed, including the
following:
live births. Involvement of the left hip alone or bilateral involvement
is more common than involvement of the right hip alone.
of treatment is important to avoid the severe disability that results
in late diagnosis, particularly after 5 years of age. Physicians and
other paraprofessionals involved in delivering children must be
competent in routine clinical screening with Ortolani’s test and
Barlow’s provocative maneuver.
False-positive sonography is common in the first 10 weeks of life;
practitioners should take this into account when making treatment
decisions.
dislocated hip was missed at birth or who subsequently dislocate a
dysplastic hip, reduction of the hip or dislocation of the hip by
Ortolani’s test and Barlow’s maneuver becomes impossible. Important
clinical findings in this age group include asymmetry in abduction of
the hip because of adductor muscle contractures, asymmetric skin folds
with gathering on the dislocated side, and Galeazzi’s sign showing
apparent shortening of the femur on the side of the dislocation.
Bilateral dislocations are more difficult to detect because they are
symmetrically abnormal. If affected children reach walking age, they
will usually demonstrate a waddling (Trendelenburg) gait.
because the lack of ossification of the proximal femur makes detection
difficult. Indications of DDH in newborns include the following:
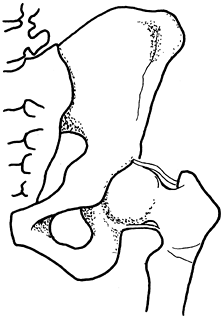
outside the inner lower quadrant of the grid formed by the vertical
line of Perkins and the horizontal line of Hilgenreiner (Fig. 166.1)
 |
|
Figure 166.1.
Radiographic signs of subluxation and dysplasia on an AP view. The proximal femoral ossification center has been drawn but may be absent before age 6 months (H, Hilgenreiner’s line; P, Perkins’ line; S, Shenton’s line (broken on left); AI, acetabular index). Note the subluxation in the left hip. |
nonoperative methods if the condition is detected in the first 6 months
of life. Pavlik harness treatment in this age group has a high rate of
success, and I have been able to achieve reduction of hips in some
children up to 9 months of age with this harness.
shoulder harness portion should be tight enough to cover the chest at
the nipple line. The anterior (medial) foot straps are tensioned enough
so that the hips are flexed greater than 90°. The posterior (lateral)
straps are tensioned enough so that the knees cannot touch in the
midline; they must not be too tight.
a child in 1–2 weeks and readjust the device, which is often necessary
because it is confusing to parents. After it is accepted by the family
and properly adjusted, the harness will rapidly produce a reduction of
the hip if Pavlik treatment is going to be successful. If the hip
reduces, the device should be worn for 3 or more months until stable
reduction is accompanied by resolution of acetabular dysplasia (e.g.,
normal acetabular index, appearance of proximal femoral ossific
nucleus).
weeks of wear after the initial readjustment, it should be
discontinued, as it will not be effective if utilized longer. When
Pavlik-harness treatment fails to achieve congruent reduction, closed
reduction and casting must be considered. Prereduction traction, long
considered to reduce the incidence of avascular necrosis, is now
controversial; I personally do not use it.
indicated. Open reduction is a delicate, specialized operation with
complications that can affect a patient for a lifetime, and it should
not be undertaken by an inexperienced surgeon. Surgery for the residual
dysplasia that can follow closed or open treatment of DDH also requires
adequate follow-up and experienced judgment in its applications and
execution. The techniques described in this chapter are those that I
have found most effective in surgical management of this condition, but
they are not exclusive and
many alternatives can be found in the literature (3,4,7,8,13,16,18).
closed reduction fails or when closed reduction would result in such
extremes of position that avascular necrosis would be a likely
consequence. It is also indicated in children older than 12–18 months,
when it is frequently combined with femoral shortening to decrease the
overall time of immobilization required to achieve remodeling of the
hip. Open reduction is indicated in a subluxated hip when abduction
fails to reposition the femoral head deeply into the true acetabulum;
in this instance, osteotomy of the pelvis or proximal femur is usually
performed simultaneously.
obviously do not allow the femoral head to be centered in the
acetabulum or that result in extremes of position are easy to detect
and should be followed with prompt open reduction, preferably as a
continuation under the same anesthetic. In children younger than 12
months, closed reduction that results in a reduction that is stable but
not deep and concentric may be accepted initially. Follow these
reductions by arthrography in 8–12 weeks; if soft-tissue remodeling has
not occurred and the reduction is not congruent and deep, proceed with
open reduction.
Standard open reduction can be performed with relative safety in some
children, but many surgeons (including myself) elect femoral shortening
in a walking child because it allows prompt open reduction without
preoperative traction and with an extremely low incidence of avascular
necrosis. It also permits derotation of the anteverted femur, thus
stabilizing the reduction. This allows early ambulation and may speed
hip remodeling; both of these goals are admirable in a child who has
never had a reduced hip joint before surgery. Open reduction is
occasionally useful in diseases other than congenital hip dysplasia,
such as cerebral palsy or reconstruction following trauma or infection.
I personally no longer use it. In general, open reduction and its
variants should be done without the use of blood transfusions. This
requires great care on the surgeon’s part. The use of X or 3X loupes is
valuable in the dissection, and electrocautery greatly facilitates
dissection without excessive bleeding. All tissues must be handled
extremely gently, and the surgeon should have a thorough knowledge of
hip anatomy. For children younger than 2–3 years, attempt a closed
reduction immediately before proceeding with an open procedure because
occasionally a stable reduction can be achieved with good long-term
prognosis for resolution of the dysplasia.
because capsulorrhaphy and other reconstructive procedures can easily
be accomplished. Open reduction from a medial (adductor) approach does
not give sufficient exposure for these essential parts of the operation
and is indicated only in very young children who will undergo prolonged
casting to maintain reduction while the capsulotomy heals and remodels.
The medial approach is not described here; see Chapter 3 and Ferguson’s (7) description for details.
Smith–Petersen approach, I prefer a skin incision that falls in, or is
parallel and superior to, the inguinal crease. Inguinal incisions can
be extended medially and laterally, and they allow excellent deep
longitudinal exposure with a nearly undetectable scar that is hidden
beneath standard clothing. If open reduction and femoral shortening are
combined, the use of an inguinal incision for the open reduction and a
lateral incision for the femoral shortening yields a more cosmetic
appearance and permits simple removal of internal fixation devices
later through the lateral incision.
flex, lift, and abduct the femur with the knee flexed until reduction
is felt. In older children, the reduction is usually either definite or
unobtainable, but younger children may not have distinct stability.
Arthrography and fluoroscopy greatly improve assessment of the
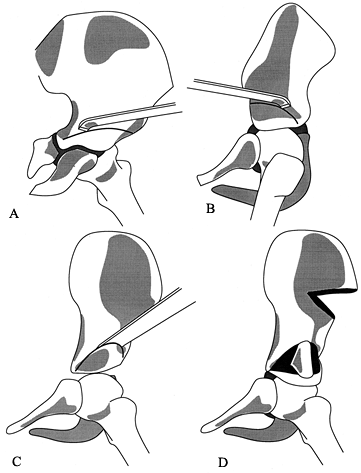
reduction (Fig. 166.2). Occasionally,
percutaneous adductor-longus tenotomy enhances stability. If the hip is
unstable in less than 55° of abduction, strongly consider open
reduction. Full double-spica casting is safest in 90° to 100° of
flexion, neutral rotation, and less than 55° of abduction, which is
Salter’s (18,19) “human” position.
 |
|
Figure 166.2. Arthrography during closed reduction can delineate anatomic features and aid in assessment of stability.
|
demonstrates stability in the weight-bearing position. Usually, 12–18
weeks in a spica cast is required. Abduction bracing may be used
long-term, although there is no scientific evidence of its value in
this circumstance.
-
Drape the affected limb and hip free with the pelvis elevated on a small towel.
-
Make a transverse inguinal incision directly in the most prominent flexion crease of the hip (Fig. 166.3A). After incising the skin, use electrocautery to expose the fascial layer.
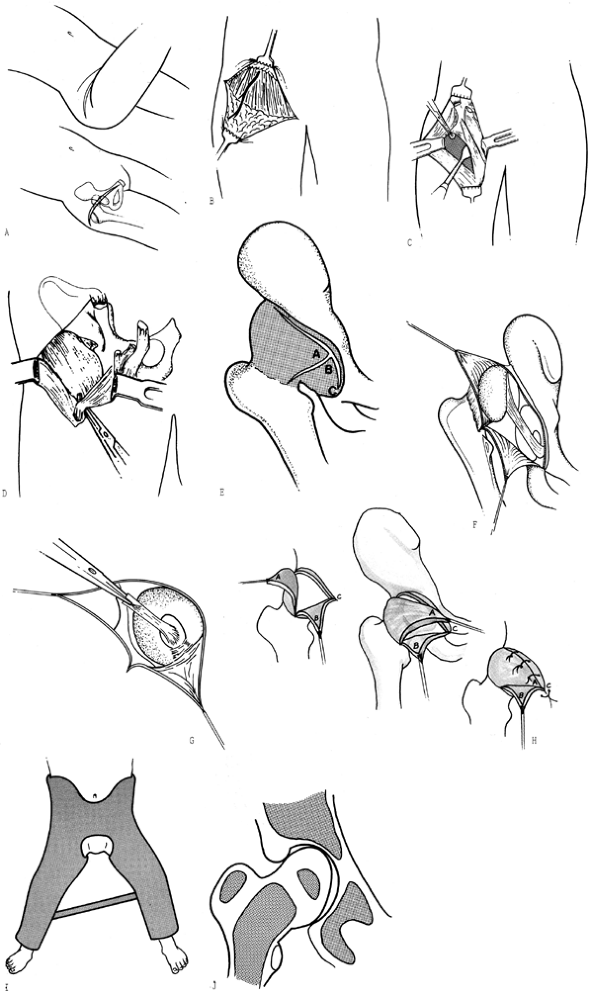 Figure 166.3. Surgical technique for open reduction of the hip through an anterior approach. See the text for a full description. A: Skin incision. B: Subcutaneous dissection and lateral femoral cutaneous nerve. C: Deep dissection exposes the hip joint capsule. D: Isolation and section of the iliopsoas tendon. E: Capsular incisions. F: Intra-articular pathology. G: Use of the sectioned ligamentum teres to locate the true acetabulum. H: Repair and reefing of the joint capsule. I: Double-hip spica cast. J: The hip and its ossific nuclei as seen on an AP radiographic view after reduction.
Figure 166.3. Surgical technique for open reduction of the hip through an anterior approach. See the text for a full description. A: Skin incision. B: Subcutaneous dissection and lateral femoral cutaneous nerve. C: Deep dissection exposes the hip joint capsule. D: Isolation and section of the iliopsoas tendon. E: Capsular incisions. F: Intra-articular pathology. G: Use of the sectioned ligamentum teres to locate the true acetabulum. H: Repair and reefing of the joint capsule. I: Double-hip spica cast. J: The hip and its ossific nuclei as seen on an AP radiographic view after reduction. -
Dissect subcutaneously both proximally to
the iliac crest and sufficiently distally to mobilize the skin and
subcutaneous tissue and allow a longitudinal incision of the deeper
layers of the wound. -
Identify the lateral femoral cutaneous nerve as it emerges from the sartorius. Isolate and protect it with Silastic tape (Fig. 166.3B).
-
If an innominate osteotomy is to be done,
now split the apophysis, but for standard open reduction, it is
unnecessary to dissect the proximal iliac apophysis. -
Carefully develop the interval between
the sartorius and the tensor fasciae latae. Retract the sartorius
me-dially and the tensor laterally to expose the rectusfemoris. -
Using a Kidner dissector, identify, tag,
and transversely section the tendinous attachment of the rectus femoris
to expose the reflected head of the rectus femoris, which is the key to
the anterior capsule (Fig. 166.3C). -
Expose the capsule, using gentle blunt
dissection with a periosteal elevator and a Kidner dissector. Use
electrocautery for any bleeders. The capsule will be found to be large,
redundant, and extending superiorly and posteriorly. -
Carry the capsular exposure medially
under the adherent iliopsoas muscle and distally until the lesser
trochanter can be palpated with a fingertip. -
At the medial border of the capsule,
identify the iliopsoas muscle, hook its tendon with a right-angle
clamp, and bring it into the wound, where it is sectioned (Fig. 166.3D). -
Next, divide the capsule in a fashion, taking care to avoid damage to the underlying femoral head (Fig. 166.3E).
The vertical limb of the lies parallel to the femoral neck, with the
cross of the lying parallel and 0.5 cm distal to the labrum of the hip
joint. Scissors may be used to extend the superior border of the cross
part of the around to the upper and posterior portions of the hip
capsule. At this point, place suture tags in the two corners of the
capsulotomy for later use in repairing the capsule. -
Now inspect the hip joint (Fig. 166.3F).
Unless the patient is older, the ligamentum teres will be seen as a
large, hypertrophic, flattened structure. Carefully excise it sharply
from its attachment on the femoral head. Leave its acetabular
attachment intact, and follow the ligament into the acetabular fovea to
locate the true acetabulum (Fig. 166.3G). With
external rotation or flexion and adduction, the femoral head can be
pulled out of the way to allow full exposure of the acetabulum. After
the fovea has been clearly identified, cut the remaining stump of the
ligamentum teres. Clean any fibro-fatty tissue from the acetabulum,
using rongeurs and Kidner dissectors, being careful to avoid damage to
the articular surface. Sometimes, the anterior capsule is adherent to
the acetabulum and must be painstakingly dissected free to expose the
entire “horseshoe” of the acetabular surface. In nearly every case, the
transverse acetabular ligament (a capsular thickening that lies across
the base of the horseshoe of the acetabular surface) will need to be
sectioned. This ligament is hypertrophic
P.4245
and prevents the descent of the femoral head into the depths of the true acetabulum.
the labrum may actually be inverted, but more often it is rolled and
hypertrophic. If an actual inversion can be demonstrated and it cannot
be adequately dissected to allow placement of the femoral head, use
axial (radial) incisions to allow part of the labrum to be teased out
of the acetabulum. This is rarely necessary. Do not excise the labrum
because it contributes to future growth of the acetabular rim.
-
Now reduce the hip by traction,
abduction, and internal rotation. The femoral head is often flattened
on its medial border and somewhat bullet-shaped; this is usually not a
problem if the hip is abducted and the apex of the femoral head can be
brought inside the acetabular labrum. If any force is required to bring
the femoral head into the acetabulum, perform a femoral shortening
osteotomy. If the hip reduces but is stable only when the hip is flexed
and abducted, consider performing an innominate osteotomy (usually
Salter osteotomy), especially if the child is near 3 years of age. In
addition, if severe internal rotation is required in an older child,
consider a derotation osteotomy through a lateral incision. -
With the hip held in internal rotation, close the capsulotomy (Fig. 166.3H). Bring the superior flap corner (tagged A in Fig. 166.3H)
into the inferomedial portion of the capsule, at the lower end of the
T. The redundant lower flap can then be either excised or sewn over the
superior flap (tagged B in Fig. 166.3H). After
additional capsular repair, the hip joint should be stable. Close the
wound by reattaching the tendons of the rectus femoris and by
subcutaneous and subcuticular skin closure with absorbable 5-0
synthetic suture. Drainage is usually unnecessary.
legs in 30° of abduction, 20° of flexion, and gentle internal rotation (Fig. 166.3I).
The position is safe if the femur has been shortened and the iliopsoas
lengthened. After open reduction in older children, this extended
internally rotated position is more appropriate than the flexed “human”
position used after closed reduction.
head, although the small ossific nucleus is often seen to be somewhat
inferior to its expected position. This results from the misshapen
femoral head and the hypertrophic labrum, and will remodel (Fig. 166.3J).
Casting for 6 weeks is usually sufficient to allow healing of any
osteotomy and development of satisfactory joint stability after open
reduction. Ambulation with or without abduction bracing, as the
clinical situation dictates, may begin immediately.
hip to minimize the compressive force across the joint (thus decreasing
the risk of avascular necrosis) and to avoid preoperative traction in
older children. It is also done in combination with derotation
osteotomy to stabilize the reduction in the weight-bearing position (5,20,22).
This lateral approach is more cosmetic and facilitates plate removal,
if desired. However, the proximal femoral shaft can, with more
difficulty, also be reached anterolaterally through the lower arm of an
extended standard Smith–Petersen incision.
 |
|
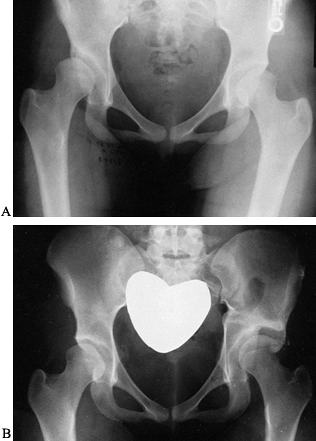
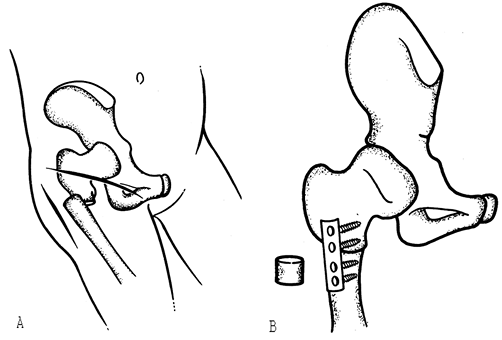
Figure 166.4. Surgical technique for femoral shortening derotation osteotomy combined with open reduction of the hip. A: Surgical incisions and osteotomy. B: Resection of a femoral segment and plate fixation.
|
-
Carry the lateral approach longitudinally through the fascia lata distal to the trochanteric apophysis.
-
Free the proximal origin of the vastus
lateralis from the trochanter, and dissect the muscle from its
posterior attachment longitudinally along the shaft of the femur. This
avoids denervation of the vastus lateralis, but take care to cauterize
perforating vessels that enter the muscle posteriorly. Then reflect the
entire muscle subperiosteally anteriorly to expose the proximal femoral
shaft. -
Select a small plate for internal fixation; I use a four-hole 1/3-tubular small-fragment plate. Place the plate along the lateral shaft of the femur just below the trochanteric flare.
-
Drill, measure, and tap the two proximal
screw holes (because the shaft is so small, this is more easily done
before the osteotomy). -
Between the second and third holes of the plate, make a transverse osteotomy with a small, sharp oscillating saw.
-
After completion of the osteotomy, the
proximal femur can easily be reduced into the hip joint through the
anterior incision. Gently pull the thigh, and observe the bayonet
overlap of the femoral fragments; this determines the amount of
shortening to be done (usually 2 cm). Remove the selected length of
shaft by a second transverse osteotomy of the distal fragment (Fig. 166.4B). -
Secure the plate to the proximal femoral
fragment, and temporarily fix the plate to the distal fragment with a
small bone clamp. Adjust anteversion by putting the hip through the
full range of motion while observing the joint through the anterior
incision. Derotation should not be excessive; usually there should be
15° to 20° of residual anteversion after the osteotomy is fixed. I do
not routinely increase varus; however, varus derotation osteotomy with
shortening is an alternative at this point. -
Once the three-dimensional position of the fragments
P.4246P.4247
is satisfactory, fix the distal two holes of the plate to the distal shaft with screws (Fig. 166.5). Figure 166.5. A:
Figure 166.5. A:
Radiographic appearance of complete congenital dislocation of the hip
treated with primary open reduction and femoral shortening using plate
fixation of the osteotomy (B). -
After a final check of hip coverage by
the acetabulum during motion, close the lateral wound with fine,
absorbable synthetic suture.
including a second lateral incision (if done), down to the skeletal
structures. Leave the plate in place if a femoral shortening osteotomy
was done. Thoroughly irrigate and debride the wound. The hip capsule
may be opened if necessary to irrigate the joint, but it must be
repaired in the same fashion as the original capsulorrhaphy. The wounds
may be packed open or closed over suction drains, depending on the
severity of infection and the surgeon’s preference. Cast immobilization
is mandatory. Administer appropriate antibiotic therapy.
has failed. If it is detected early, simple manipulation under general
anesthesia and application of a spica cast should suffice to restore
reduction. Late redislocation is often associated with residual
stiffness. It may occur because of insufficient immobilization,
capsulorrhaphy failure, or excessive derotation. Rarely, it can be
secondary to severe ligamentous laxity, even when appropriate surgery
has been done, usually in an older child with a markedly dysplastic
acetabulum. Management of late redislocation must be based on careful
radiographic studies to
determine
the cause. Sometimes, fluoroscopy or arthrography is helpful. A proper
diagnosis will suggest the most appropriate treatment.
occur, particularly in older children. Assessment is almost always
radiographic. If subluxation is subtle and mild, I postpone additional
surgical treatment for 6 months to allow complete rehabilitation of the
hip girdle musculature and joint remodeling; abduction bracing during
this period may be appropriate.
was performed, subluxation is usually best treated by an innominate
osteotomy. Repeat open reduction may be required. Unless the surgeon is
extremely experienced in all aspects of congenital hip surgery, it is
safer to perform such acetabular procedures as secondary treatment,
even if it is initially thought that both femoral and acetabular
surgery will be necessary. If previous femoral surgery was not done,
the surgeon may elect either pelvic or femoral osteotomy, especially if
the child is younger than 5 years.
stiff, even if open reduction was required. Stiffness is almost always
a sign of subluxation or avascular necrosis. Make every attempt to
accurately diagnose the problem; fluoroscopy and arthrography can be
helpful.
or irregular ossification in a clinically normal joint) and require
observation only. More extensive avascular necrosis may lead to
temporary subluxation, which should be managed by casting, ambulatory
abduction bracing, or surgical treatment. Severe subluxation associated
with avascular necrosis may require reorientation of the acetabulum by
innominate osteotomy (1), although it is safe
to wait and observe if the hip is reduced in an abduction brace.
Arthrography to visualize cartilaginous structures is recommended
before surgical treatment for avascular necrosis. Avascular necrosis is
a potential complication of all additional treatment options for
patients and reduces the success of reconstructive surgery. It can also
lead to early osteoarthrosis of the hip.
will be followed by leg-length discrepancy and deformity of the
proximal femur. These deformities (head deformity, coxa breva, coxa
valga) may appear late. Initiate a regular program of leg-length
evaluation and x-ray observation to detect these complications and plan
long-term management (11,27).
usually occurs as a result of vascular damage to the proximal femoral
physis (14). In most children (except very
short ones), the appropriate management is properly timed
epiphysiodesis of the contralateral limb, based on routine yearly
leg-length measurements through childhood. Occasionally, femoral
lengthening may be necessary (see Chapter 171).
The slight temporary discrepancy that accompanies femoral shortening
osteotomy is usually followed by slight femoral overgrowth, so
treatment is unnecessary.
be continued until remodeling has eliminated the secondary dysplastic
features of the acetabulum and the proximal femur. Monitor dysplasia
and residual subluxation both radiographically (acetabular index,
center–edge angle) (21) and clinically (subtle
loss of abduction, Trendelenburg gait). The use of casts, abduction
braces, and surgery for residual dysplasia is somewhat arbitrary and
should be based on the patient’s age, the parents’ wishes, and the
surgeon’s experience. However, failure of significant remodeling of
dysplasia by 5 years of age makes additional surgery worth considering
because there is good evidence that excellent remodeling can occur if
correction is achieved by that age. Obvious subluxation warrants a more
aggressive surgical approach because prompt treatment improves the
dysplasia and the prognosis. Both femoral and pelvic osteotomies can be
done for residual dysplasia.
indicated in subluxation or dysplasia of the hip when reorientation can
stabilize a reduction, resolve mild subluxation, or stimulate
remodeling of the joint (4,5,12,22,25).
Often, it is used to achieve a congruent joint in the weight-bearing
position after closed or open reduction to allow a child of walking age
to ambulate with less risk of subluxation. When acetabular dysplasia
persists after reduction, femoral osteotomy can stimulate remodeling of
the acetabulum, if done by 5 years of age (12).
The choice of femoral or pelvic osteotomy in this situation is often a
matter of the surgeon’s personal preference; I prefer the pelvic
procedure.
dysplasia is excessive anteversion. This contributes to anterolateral
subluxation in the weight-bearing position and encourages superolateral
subluxation in the sitting position. Femoral derotation alone is
generally sufficient to correct the deformity. This becomes obvious
when radiographs are taken with the legs internally rotated and a
normal neck–shaft angle (135°) is seen. If abduction is also necessary
to produce a congruent reduction, then varus can be added, as well.
Take great care not to overcorrect the femoral deformity. Avoid
retroversion; increased varus of greater than 20° is rarely indicated.
If a varus osteotomy is done, the hip must have an adequate range of
abduction to allow functional motion after surgery. In my opinion, the
prerequisites for femoral osteotomy in hip dysplasia are critical and
should be the same as those for innominate osteotomy: congruent
reduction of the hip and a full range of motion.
Some have advocated single-screw fixation or multiple smooth pins, but
I strongly prefer rigid fixation with a small plate (for derotation
alone) or a pediatric blade plate (for a varus osteotomy in an older
child). This allows more accurate control of position during healing.
-
Perform the operation with the hip and
leg draped free, the patient on a radiolucent table, and an image
intensifier available positioned anteroposteriorly. This allows testing
of range of motion and reduces the chance of overcorrection, compared
to the more conventional fracture table. -
Make a longitudinal lateral incision from
the greater trochanter to a point distant enough to accommodate the
fixation device selected. Incise the fascia lata and reflect the vastus
lateralis anteriorly from its posterior femoral insertion, taking care
to cauterize perforating vessels. Expose the proximal femoral shaft
subperiosteally to the apophysis of the greater trochanter. -
The osteotomy site is critical. It must
be intertrochanteric because internal rotation of the proximal fragment
would otherwise increase iliopsoas tension (Fig. 166.6). If a subtrochanteric osteotomy is preferred, expose and release the tendinous portion of the iliopsoas insertion.![]() Figure 166.6.
Figure 166.6.
Proper intertrochanteric level for femoral derotation osteotomy. This
allows relaxation rather than tightening of the iliopsoas muscle. -
Position the guide pins for a blade
plate, using anteroposterior (AP) and frog-lateral image
intensification. Use appropriate reamers or blade chisels according to
the manufacturer’s directions, depending on the specific fixation
system being used. Drill and tap any proximal fixation holes before
cutting the femur. -
Perform the osteotomy with a saw, taking
an appropriate wedge out medially if varus positioning is desired. Fix
the plate to the proximal fragment, externally rotate the distal
fragment, and temporarily clamp the plate to the shaft. Now put the hip
through a full range of motion while studying the joint with
fluoroscopy, making special note of anteversion (which should not be
less than 15°). Readjust the position until you are satisfied that
subluxation has been adequately treated, and fix the plate to the
distal fragment. Close the wound with fine, absorbable suture,
including
P.4250
the
skin; I prefer 5-0 undyed polyglycolic acid subcuticular suture. Apply
a double-spica cast. Remove the cast at 8 weeks postoperatively or
after radiographic union. Allow ambulation as tolerated. Physical
therapy is unnecessary. Warn the family that the perineum will appear
wide until the child grows and that a limp may persist for 2–3 months
but will eventually disappear.
acetabular dysplasia, residual subluxation of the hip, or failure of
gradual improvement of radiographic dysplasia following reduction of a
dislocated hip. In general, pelvic osteotomy should be done when severe
dysplasia is accompanied by significant radiographic changes (high
acetabular index, failure of lateral acetabular ossification) on the
acetabular side of the hip joint, as opposed to changes on the femoral
side (e.g., marked anteversion), which are best treated by femoral
osteotomy (5). Surgical treatment of definite
hip subluxation by either pelvic or femoral osteotomy before age 4
years will be accompanied by at least partial remodeling and resolution
of anatomic abnormalities on the opposite surface of the joint (12).
when expected remodeling has ceased (as assessed by serial radiographs)
and dysplasia or subluxation persists (5).
Often, after the hip is reduced, pelvic osteotomy can be postponed
until 4 years of age to allow adequate time for remodeling.
may be categorized as indicated either for primary treatment of
dysplasia (Salter innominate osteotomy, Pemberton osteotomy, triple
innominate osteotomy) or for salvage of a poor result in the later
stages of dysplasia when complete remodeling is not expected (Chiari
osteotomy). The primary osteotomies are generally reorientation
procedures for the acetabulum, although the Pemberton procedure allows
actual diminution of acetabular volume at the expense of some
acetabular congruity. The Salter and Pemberton osteotomies are the most
common osteotomies performed in North America.
osteotomy must be done only in the presence of a congruent reduction,
satisfactory range of motion, and reasonable femoral sphericity. These
prerequisites have been popularized primarily by Salter (18,19)
for his innominate osteotomy, and they are appropriate preoperative
goals for any primary osteotomy about the hip (acetabular or femoral).
concept, although both are designed to limit anterolateral subluxation
by improving coverage in this area. The Salter osteotomy, because it
goes completely through the pelvis, allows anterior and lateral
rotation of the acetabulum through an axis formed by the sciatic notch
and the pubic symphysis. There is a limit to the degree of correction
that can be obtained, and the procedure does not change acetabular
shape (17). Conversely, the Pemberton osteotomy
is an incomplete osteotomy that hinges the anterolateral acetabular
roof on the flexible triradiate cartilage for correction (16).
This actually changes the configuration of the acetabulum and
introduces joint incongruence that must be corrected by remodeling
during growth. For these reasons, the Pemberton procedure may be
indicated when there is an elongated, dysplastic acetabulum, but it is
most effectively done in children younger than 8 years, as there is
still flexibility in the triradiate cartilage and growth remains for
remodeling of the joint surfaces (29).
but a relatively congruent reduction, the Salter osteotomy does not
provide sufficient angular correction to improve stability. When the
triradiate cartilage is closed, the Ganz periacetabular osteotomy (see Chapter 104)
can achieve the extremes of reorientation required. When the triradiate
cartilage is open, the same freedom to reorient the acetabulum in space
can be achieved by cutting the ischium and pubis in addition to the
ilium (triple innominate osteotomy). Variations of this technique have
been described by Steel (24), Tönnis et al. (28), and Tachdjian (25). All are complex operations that should not be attempted by an inexperienced surgeon.
to remodel for the growth time remaining requires a different type of
procedure. The Chiari (3) osteotomy is probably
the most commonly used operation. It is a displacement osteotomy that
essentially provides a shelf or buttress to limit further proximal
subluxation of the femoral head. The superior hip capsule provides an
interpositional surface between the cancellous bone of the shelf and
the femoral head, and the capsular tissue may undergo metaplasia into
fibrocartilage. Thus, the functional size of the acetabulum can be
increased by the operation. If done properly, the Chiari osteotomy also
moves the hip joint center medially and improves the mechanical
advantage of the abductor muscles, both of which tend to decrease the
intra-articular resultant force across the hip joint. The Chiari
osteotomy does not require a concentric reduction; it may be done above
a subluxated hip. The chief indication for Chiari osteotomy is pain
associated with a subluxated, dysplastic hip in an older child. It
should not be performed if degenerative changes are present or the hip
is stiff. Do not do a capsulotomy at the same time as a Chiari
osteotomy.
hip dysplasia are controversial. The goal of surgery most often stated
is to treat chronic hip pain in an adolescent who has significant
dysplasia as seen on radiographs. For many surgeons, another
appropriate indication is radiographically demonstrated progressive
subluxation, often associated with increasing degenerative changes of
the hip. Although it may be unwise to consider surgery in an adolescent
who has no pain, regardless of the radiographic appearance of the hip,
there are surgeons who are exploring the use of late reconstructive
procedures (e.g., the Ganz osteotomy) in asymptomatic patients who have
severe radiographic dysplasia (see Chapter 104).
-
Prepare and drape the affected hip and
leg free. Use a transverse inguinal skin incision as described earlier
in this chapter (Salter describes a slightly more oblique incision),
and identify the lateral femoral cutaneous nerve where it exits at the
upper border of the sartorius; protect it with Silastic tape. Develop
the proximal interval between the sartorius and the tensor fasciae
latae muscles and between the straight head of the rectus femoris and
the tensor fasciae latae muscles. -
Split the iliac apophysis with a single longitudinal scalpel cut from the anterosuperior spine to the mid crest (Fig. 166.7A),
and carefully pull the cartilage away from the crest. Strip the inner
and outer walls of the ilium subperiosteally. Strip the anteroinferior
spine medially with its attached rectus femoris. Carry the
subperiosteal dissection to the sciatic notch. The notch is best
exposed by gently teasing the periosteum away from it both medially and
laterally with right-angle clamps; the tips of the two clamps should
touch when stripping is complete. Stay subperiosteal to avoid sciatic
nerve injury.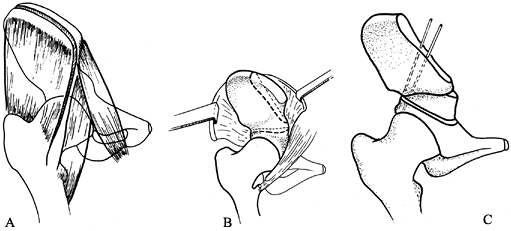 Figure 166.7. Surgical technique for Salter innominate osteotomy. A: Split of the iliac apophysis and fascial incision. B: Exposure of the ilium and sites of the osteotomy. C: Completed osteotomy.
Figure 166.7. Surgical technique for Salter innominate osteotomy. A: Split of the iliac apophysis and fascial incision. B: Exposure of the ilium and sites of the osteotomy. C: Completed osteotomy. -
In the inferior wound, identify the hip
capsule and the iliopsoas muscle anterior to it. Pull the tendinous
portion of the muscle into the wound with a right-angle clamp and sever
it. -
Pass a Gigli saw through the notch with
right-angle clamps. Saw a straight osteotomy from the notch to the
anteroinferior iliac spine (Fig. 166.7B),
keeping the hands as far apart as possible to avoid binding; protect
the skin with ribbon retractors. Incline the osteotomy slightly in the
frontal plane so that the lateral edge is superior to the medial edge. -
Open the osteotomy by externally
rotating, abducting, and extending the hip to place the extremity into
a figure-four position while holding the posterior osteotomy site
closed and slightly anteriorly with a tenaculum. Do not pull the
proximal ilium upward; this tends to displace the proximal ileum rather
than the distal fragment containing the acetabulum. Do not use a lamina
spreader because damage to the fragile ilium may result. -
With an oscillating saw (my preference)
or a large rib cutter, fashion a triangular graft with one angle of 30°
from the anterior portion of the proximal fragment. Place the graft
into the osteotomy site, keeping the posterior osteotomy closed, and
fix it with two threaded pins inserted from the proximal fragment,
through the graft, and into the distal ischium posterior to the hip
joint (Fig. 166.7C). Check the pin length
carefully, and move the hip joint to feel for any crepitus, which might
indicate pin protrusion into the joint. Temporarily leave the pin ends
long. -
Irrigate the wound and reapproximate the
apophysis over the pins with simple absorbable sutures passed directly
around the cartilaginous apophysis. Cut the pins so they will be
palpable beneath the skin, and close the subcutaneous tissue and skin
with fine, absorbable suture. -
Apply a well-molded one-and-one-half
spica cast with the hip in 25° of flexion, 25° of abduction, and slight
internal rotation. Remove the cast and pins 8 weeks after surgery, when
radiographic union has occurred, under a brief general anesthetic. The
patient can then begin weight bearing as tolerated. Physical therapy is
usually unnecessary.
-
Perform the operation on a radiolucent table with image-intensifier control.
-
Make a transverse skin incision in the
inguinal crease, but use subcutaneous dissection to mobilize the
proximal and distal flaps. Then use a standard Smith–Petersen exposure
of the hip (see Chapter 3). Protect the lateral femoral cutaneous nerve. -
Develop the interval between the
sartorius and tensor fasciae latae muscles, and incise the iliac
apophysis longitudinally with a sharp scalpel. -
Expose the anterior two thirds of the
inner and outer tables of the pelvis with a periosteal elevator. The
subperiosteal stripping does not need to go behind the sciatic notch
(as in the Salter osteotomy) but must proceed distally to the
triradiate cartilage. This can be felt as a line of resistance to
further stripping; facilitate a safe approach to the area by teasing
subperiosteally with a right-angle clamp. -
Beginning on the outer wall of the
pelvis, use a small, curved osteotome to make a cortical pericapsular
osteotomy, starting at the anteroinferior iliac spine and continuing
parallel to the joint. This osteotomy curves down to, but not into, the
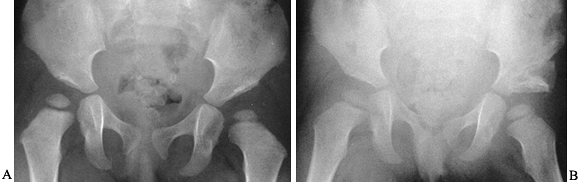
triradiate cartilage and must end anterior to the sciatic notch (Fig. 166.8A).![]() Figure 166.8. Pemberton osteotomy. A: Make a cortical pericapsular osteotomy cut. B,C: Make a similar cortical osteotomy in the inner wall of the pelvis. D: Cut a triangular graft from the proximal ilium, and carefully wedge the graft into the osteotomy site.
Figure 166.8. Pemberton osteotomy. A: Make a cortical pericapsular osteotomy cut. B,C: Make a similar cortical osteotomy in the inner wall of the pelvis. D: Cut a triangular graft from the proximal ilium, and carefully wedge the graft into the osteotomy site. -
Make a similar cortical osteotomy in the
inner wall of the pelvis, again ending at the triradiate cartilage but
avoiding both the sciatic notch and the joint itself (Fig. 166.8B). -
Join the two osteotomies, using a curved
or spherical osteotome and taking care to avoid penetration of the
sciatic notch or the joint. Use the image intensifier at this point to
confirm the safe position of the osteotome. -
Carefully pry the anterolateral
acetabular fragment distally with the osteotome and a smooth, broad
lamina spreader, without too much force. When this is properly done,
the triradiate cartilage should be visible in the depths of the
osteotomy. -
Cut a triangular graft from the proximal ilium; a saw helps to make this cut without crushing the bone (Fig. 166.8C).
Flatten a notch in the faces of the pelvic osteotomy, as needed, to
receive the graft and lock it in place. Carefully wedge the triangular
graft into the osteotomy site, and remove the lamina spreader; the
graft should be secure and require no fixation (Fig. 166.8D). -
Close the wound with absorbable sutures, and apply a spica cast as described in the technique of Salter osteotomy.
Allow weight bearing as tolerated. Physical therapy is unnecessary.
Older children may exhibit transient stiffness of the hip joint because
of changes in the acetabular surface configuration caused by the
Pemberton osteotomy.
 |
|
Figure 166.9. Radiographs of a Pemberton osteotomy of a dysplastic left hip. A: Preoperative radiograph. B: Radiograph taken 6 weeks postoperatively.
|
There is also significant potential risk of neural and vascular injury;
these are not operations for the inexperienced. Of the operative
approaches, I prefer Tachdjian’s (26), but each has its proponents. For fully detailed descriptions, readers are referred to the originators of each approach (24,26,28).
-
Drape the patient on a radiolucent table
with the leg free. The iliac portion of the osteotomy (usually
performed last) is performed exactly as in the Salter osteotomy.
 |
|
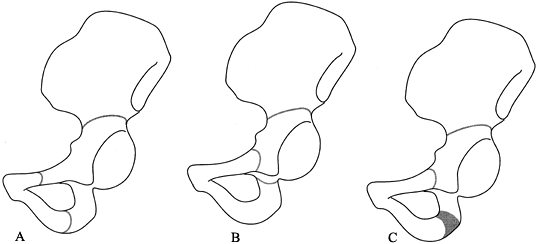
Figure 166.10. Site of iliac, pubic, and ischial osteotomies in the various triple innominate osteotomy procedures. A: Steel osteotomy. B: Tönnis osteotomy. C: Tachdjian triple osteotomy.
|
-
Flex the hip 90° to expose the buttock
and ischial tuber-osity. Make the ischial cut first through a
transverse incision positioned 1 cm proximal to the gluteal crease.
Retract the gluteus maximus laterally, and sharply dissect the origin
of the biceps femoris from the ischium. Identify the sciatic nerve,
using a nerve stimulator if necessary, and protect it throughout the
procedure. -
Separate the origins of the
semimembranosus and semitendinosus muscles, and pass a very curved
hemostat subperiosteally around the ischium, starting from the
obturator foramen and emerging posterior to the ischial ramus. Stay
carefully on the bone to avoid vascular injury. Cut the ramus, using
the clamp as protection, with an osteotome as wide as the ischial ramus
directed 45° posteriorly and laterally. Then close the wound. Steel
recommended changing gloves, gowns, and instruments at this stage
because of the risk of contamination in this area of the perineum. -
Expose the anterior pelvis as for a
Salter osteotomy (see above), continuing the dissection medially to
identify the pectineus muscle. Detach the pectineus from the pubic
ramus, clearing the pubis to about 1 cm medial to the pectineal
tubercle. Pass a significantly curved hemostat subperiosteally from
above the pubis and around the bone to emerge in the obturator foramen.
Again using the instrument for protection, cut the pubic ramus by
directing an osteotome posteriorly and medially. -
Then make the iliac cut as described for
the Salter osteotomy, and under image-intensifier control reposition
the entire acetabular unit to its desired position. A towel clip or
Steinmann pin (inserted as a “joystick”) can be helpful in controlling
the fragment. -
Close the wound, and immobilize the hip
in a one-and-one-half hip spica cast for 8 weeks. Follow-up care is
similar to that for Salter osteotomy.
He felt that redirection should emphasize more lateral and less
anterior coverage of the hip than advocated by Salter or Steel.
-
With the patient lying prone, expose the
ischial tuberosity through an oblique incision in the direction of the
fibers of the gluteus maximus, which are split bluntly and separated.
Cut the obturator internus and the inferior and superior gemellus
muscles to expose the ischial ramus. Protect the sciatic nerve and the
gluteal vessels with a blunt retractor in the sciatic notch, and place
special retractors around the ischial ramus, preserving the
sacrotuberous and sacrospinalis ligaments for stability. Make the
ischial cut as frontal as possible, from lateral to medial, connecting
the ischial and obturator foramina. The osteotomy must be complete,
without spikes remaining on the cut surfaces of the bone. -
Close the wound and reposition the
patient supine. Rather than using an extended inguinal incision (see
the Steel technique above), make a small incision over the pubis where
it is palpable just medial to the psoas. Insert two retractors above
the pubis and through the obturator foramen, and make the osteotomy cut
parallel with the hip joint. -
The remaining procedure is performed
similarly to the Steel osteotomy, except that in the frontal plane the
iliac osteotomy is oriented from superolateral to inferomedial, which
allows easier lateral rotation of the fragment.
-
With the extremity in the frog-leg
position, make a transverse adductor incision over and posterior to the
adductor longus. Although Tachdjian (26)
released the adductors, I have found that the ischium can usually be
exposed by bluntly developing the interval between adductor brevis and
magnus and then carefully dissecting toward the ischial tuberosity on a
line between the adductor magnus and obturator externus insertions.
Expose the ischium subperiosteally, and protect the soft tissues with
Chandler retractors. The ischial osteotomy
P.4256
is a laterally based about 1.5 cm wide wedge that allows moving the acetabulum medially. -
Expose the pubis through the same
incision by retracting the iliopsoas muscle (which may be fractionally
lengthened) laterally and elevating the pectineus to expose the
iliopectineal eminence. Protect the pubis subperiosteally with two
Chandler retractors. Make the pubic osteotomy parallel to the joint,
1.5 cm medial to the acetabulum as seen on image intensification, with
the osteotome directed 15° medially. -
Using a second incision (or an extension
of the medial one), perform the iliac osteotomy in a similar fashion to
that in the Steel osteotomy.
-
Drape the hip and leg free, with the affected side elevated on a small towel or sandbag.
-
Make an extended transverse inguinal
incision as previously, carrying it well lateral to the mid-lateral
line. Undermine the subcutaneous tissue to expose the proximal crest of
the ilium, and isolate and protect the lateral femoral cutaneous nerve. -
Detach and tag the straight head of the
rectus femoris. Split the iliac apophysis longitudinally, and expose
the inner and outer walls of the ilium by subperiosteal dissection down
to the sciatic notch. Carefully cut the reflected head of the rectus
femoris, and dissect it free to expose the edge of the capsule. Under
the reflected head of the rectus femoris, identify the edge of the
capsule where it attaches to the pelvis. Use an instrument and the
image intensifier to confirm the position of the capsular attachment on
the ilium. The correct spot will be several millimeters above the
superior edge of the acetabulum as seen on the fluoroscope because of
the thickness of the capsule.
was straight from the front to the back of the pelvis. Most surgeons
(including myself) prefer a curved cut, which limits anteroposterior
sliding of the osteotomy. However, if the cut is made as a conical
rather than cylindric curve three-dimensionally, the fragments will not
displace; therefore, accurate three-dimensional control is mandatory.
-
Make the osteotomy just at the superior
edge of the thickened hip capsule at a 15° upward angle as viewed in
the AP plane with the image intensifier. Use two alternate ¾ in (1.5–
2.0 cm) straight osteotomes and frequent radiographs to make a slightly
curved osteotomy from the front of the pelvis to near the notch. Both
osteotomes must be kept absolutely parallel to each other (at 15°
inclination); otherwise, the osteotomy will not slide properly.
Although logic suggests that the entire osteotomy should follow the arc
of the hip joint, there has never been any demonstrated advantage to
such a cut, and it is unrealistic to expect perfect congruence with the
hip capsule, except by the rapid remodeling that follows Chiari
osteotomy. -
Protect the inner wall of the pelvis with
malleable retractors. The cut must be smooth so there are no spikes of
bone to catch during displacement. -
Complete the posterior part of the
osteotomy with a Gigli saw passed behind the sciatic notch with
right-angle clamps, as described above for Salter osteotomy. -
Displace the osteotomy by abducting the
leg widely. The displacement should be one-half of the width of the
ilium at the site of the cut; too much displacement reduces the contact
area of the osteotomy surface and may lead to delayed union (Fig. 166.11).
Do not pull the proximal ilium laterally in an attempt to move the
fragments; if the cut will not displace, it is because the osteotomy is
not complete or is irregular or conical or because spikes of medial
cortex remain.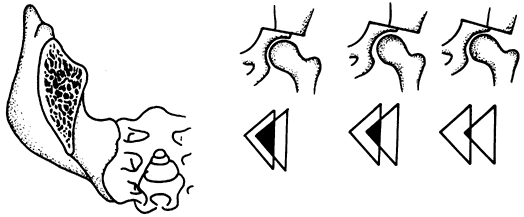 Figure 166.11.
Figure 166.11.
The Chiari osteotomy is made through a triangular section of the ilium.
Avoid excessive displacement of the distal fragment, which reduces the
contact area and may result in delayed union. -
If there is a large anterior defect over
the capsule after displacement, it may be filled with corticocancellous
graft from the proximal ilium. -
I prefer internal fixation with a long,
4.5 mm cancellous bone screw introduced from the lateral proximal ilium
into the distal fragment. Use the image intensifier to ensure that the
hip joint is not penetrated. Alternatively, threaded Steinmann pins may
be used. Internal fixation is not absolutely necessary, but if it is
not used, the leg must be immobilized in abduction (with a spica cast
or traction) to maintain displacement until the pelvis begins healing
in 2–3 weeks (Fig. 166.12).![]() Figure 166.12. An adolescent girl with a painful dysplastic hip was treated by Chiari osteotomy. A: Preoperative radiograph. B:
Figure 166.12. An adolescent girl with a painful dysplastic hip was treated by Chiari osteotomy. A: Preoperative radiograph. B:
Postoperative radiograph. Note the upward inclination of the osteotomy.
Postoperative hip function was excellent, with complete relief of pain. -
Close the wound over a suction drain. If internal fixation was used and is stable, allow early touch-down crutch walking.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
E, Huo MH, DeLuca PA. Early Innominate Osteotomy as a Treatment for
Avascular Necrosis Complicating Developmental Hip Dysplasia. J Pediatr Orthop B 1997;6:138.
DI, Broughton NS, Cole WG, Menelaus MB. Avascular Necrosis Following
Closed Reduction of Congenital Dislocation of the Hip: Review of
Influencing Factors and Long-term Follow-up. J Bone Joint Surg Br 1990;72:557.
Kleuver M, Kooijman MA, Pavlov PW, Veth RP. Triple Osteotomy of the
Pelvis for Acetabular Dysplasia: Results at 8 to 15 Years. J Bone Joint Surg Br 1997;79:225.
RD, Roach JW, Wenger DR, et al. One-stage Treatment of Congenital
Dislocation of the Hip in Older Children, Including Femoral Shortening.
J Bone Joint Surg Am 1989;71:734.
WK, Anderson MB, Alpert J, et al. The Value of Preliminary Traction in
the Treatment of Congenital Dislocation of the Hip. J Bone Joint Surg Am 1990;72:1043.
JR, Bowen JR, MacEwen GD. Varus Derotation Osteotomy in the Treatment
of Persistent Dysplasia in Congenital Dislocation of the Hip. J Bone Joint Surg Am 1985;67:195.
P, Jankovic L. Combined Procedure of Open Reduction and Shortening of
the Femur in Treatment of Congenital Dislocation of the Hips in Older
Children. Clin Orthop 1976;119:60.
T, Millis MB, Grifffin PP. The Early Identification and Classification
of Growth Disturbances of the Proximal End of the Femur. J Bone Joint Surg Am 1986;68:970.
RB. The First 15 Years’ Personal Experience with Innominate Osteotomy
in the Treatment of Congenital Dislocation and Subluxation of the Hip. Clin Orthop 1974;98:55.
PL, Strecker WB. Congenital Dislocation of the Hip in Children:
Comparison of the Effects of Femoral Shortening and of Skeletal
Traction in Treatment. J Bone Joint Surg Am 1984;66:21.
P, Capelli AM, Schoenecker PL. Pemberton Osteotomy for the Treatment of
Developmental Dysplasia of the Hip in Older Children. J Pediatr Orthop 1998;18:254.