Growth-Plate Injury
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Growth-Plate Injury
Growth-Plate Injury
Paul D. Sponseller MD
Description
-
Injury to the growing portion of children’s bones, the physis, or physeal plate
-
Some growth-plate injuries do not produce
growth disturbances; only those causing substantial crushing or
malalignment of the growth plate cause such sequelae. -
The most commonly affected bones are the long bones of the growing child.
-
The 4 most commonly injured growth plates are the distal radius, distal tibia, phalanges, and proximal humerus (1).
-
When injured, the distal femur and the distal tibia are the sites that most commonly show a growth disturbance.
-
-
Synonyms: Physeal injuries; Salter-Harris fractures (named after the system for describing growth plate injuries) (2)
General Prevention
-
If growth-plate damage is detected early, adverse effects may be prevented in some cases.
-
The “bar” of bone that forms in the area
of damage may be resected if it is <50% to allow normal growth;
otherwise, corrective osteotomy for angulation or lengthening the
damaged limb (if it is >4 cm short) can be done (1). -
A simple option is to stop the growth in the contralateral growth plate to maintain symmetry.
Epidemiology
-
Younger patients have a higher risk of serious sequela of a growth plate fracture because they have more growth remaining (3).
-
Boys are affected twice as frequently as girls (1).
Incidence
-
These injuries account for 15–20% of all pediatric fractures (1).
-
Growth-plate injuries may occur at any age, but adolescents have a higher incidence of physeal fractures.
Prevalence
These injuries occur most frequently in girls 11–12
years old and in boys 12–14 years old, when growth is most rapid and
trauma is most serious (3).
years old and in boys 12–14 years old, when growth is most rapid and
trauma is most serious (3).
Risk Factors
Adolescent boys
Etiology
-
Trauma is the most common cause of growth plate injury.
-
Other causes that damage the physis:
-
Infection
-
Tumors
-
Drugs (e.g., steroids, estrogen, testosterone)
-
Excessive heat or cold
-
Classification
-
The Salter-Harris classification (2):
-
Universally used
-
5 patterns of growth plate fractures (types III, IV, and V are at high risk for growth plate damage) (Fig. 1):
-
Type I: Split along and parallel to the physis without involvement of the metaphysis or epiphysis
-
Type II (most common): Split along the physis that exits through the metaphysis
-
Type III: Intra-articular fracture of the epiphysis that exits transversely out of the physeal plate
-
Type IV: Fracture of the epiphysis that exits through the metaphysis
-
Type V: Crush injury to the physis
-
-
Associated Conditions
-
Ligamentous injury
-
Chest, abdominal, and head trauma
-
Neurovascular injury
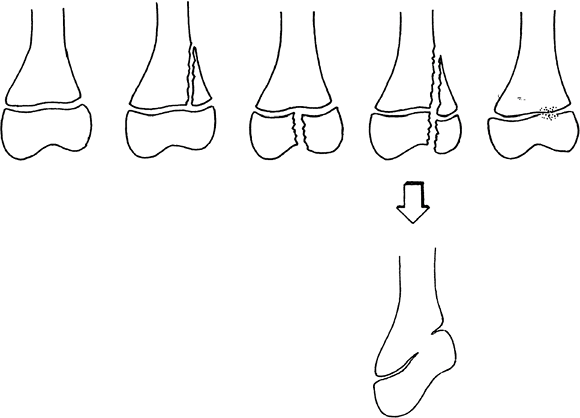 Fig. 1. The Salter-Harris classification divides growth plate injuries into types I to V (left to right). These injuries may result in deformities (lower).
Fig. 1. The Salter-Harris classification divides growth plate injuries into types I to V (left to right). These injuries may result in deformities (lower).
Signs and Symptoms
-
Pain and swelling are the most frequent findings, often accompanied by deformity.
-
Sometimes crepitus can be felt.
Physical Exam
The limb should be evaluated carefully for open wounds and distal neurovascular status.
Tests
Pathological Findings
-
The growth plate consists of the zone of growth, cartilage transformation, ossification, and the metaphysis (1).
-
Physeal fractures usually cleave at the zone of cartilage transformation.
-
Permanent injury occurs when a fracture
causes malalignment of the edges of the growth plate, or when fracture
or infection causes the death of cells of the growth plate.
Imaging
-
AP and lateral radiographs of the involved area are required.
-
Occasionally, tomograms or CT scans may be needed to evaluate more complicated fracture patterns.
-
MRI is the best method with which to diagnose an established injury to the growth plate.
-
It shows the cartilage line of the growth plate as distinct from bone.
-
Order a gradient echo sequence of the
growth plate. (This should be discussed with the radiologist in advance
to select the best settings.)
-
Differential Diagnosis
-
In the chronic setting, other causes of growth plate injury must be considered.
-
Infection may be especially insidious.
P.161
General Measures
-
Immediate care for any fracture includes immobilization and ice.
-
The neurovascular status of the extremity should be evaluated and treated if necessary.
-
Pain medication can be used if compartment syndrome is not a concern.
-
Nondisplaced fractures should be splinted immediately.
-
Displaced fractures should be reduced
using conscious sedation, hematoma block, or general anesthesia; the
fracture then is splinted, and reduction is checked with repeat
radiographs. -
If a fracture involves the growth plate:
-
Patients should be seen within 3–5 days.
-
Splints usually are maintained for 1–2 weeks and then replaced by a circumferential cast once edema has mostly resolved.
-
-
The patient is referred to the orthopaedic surgeon for definitive management.
-
Nonweightbearing is indicated for lower extremity fractures, and upper extremity fractures often are protected with a sling.
Medication
Pain control is indicated.
Surgery
-
Anatomic reduction is the best way to minimize growth disturbance in most growth-plate fractures.
-
If closed reduction is not possible, some fractures must be reduced openly in the operating room.
-
These fractures and any other fracture
that is not stable after reduction must be pinned percutaneously or
internally stabilized.
-
-
Almost all open fractures require operative irrigation and débridement.
Prognosis
-
Most physeal fractures heal without difficulty.
-
The higher the Salter-Harris classification, the more common is the incidence of growth abnormality (1).
-
The closer the patient is to skeletal maturity, the less a growth abnormality will affect growth (3).
-
Anatomic regions:
-
Certain regions (e.g., distal tibia and distal femur) are more prone to growth disturbance.
-
Other regions (e.g., distal radius and proximal humerus) are relatively protected from growth disturbance.
-
Complications
-
Growth arrest (physis stops growing)
-
Malunion
-
Growth disturbance (physis grows abnormally with resultant angulation), a more serious complication than growth acceleration.
-
Growth acceleration from increased blood
flow for healing, which may occur in any child <10 years old with a
fracture, and which usually amounts to only 5–10 mm
Patient Monitoring
-
Patients with growth-plate injuries and
at increased risk of growth disturbance (Salter-Harris types III to V
and all distal femur and distal tibial physeal injuries) should be
followed for at least 6–12 months to ensure normal growth. -
At that time, the physician should:
-
Look for equality of limb length and angulation.
-
Look for the presence of a clean “open” growth-plate line on a radiograph.
-
Look for the “growth-arrest line” of bone
that was formed at the time of injury to be separated from the growth
plate by an even layer of normal newly formed bone.
-
References
1. Rang M, Wenger DR. The physis and skeletal injury. In: Rang M, Pring ME, Wenger DR, eds. Rang’s Children’s Fractures, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2005:11–25.
2. Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg 1963;45A: 587–622.
3. Dimeglio A. Growth in pediatric orthopaedics. In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006:35–65.
Codes
ICD9-CM
-
813.42 Fracture of distal radial epiphysis
-
821.22 Fracture of distal femoral epiphysis
-
824.4 Fracture of distal tibial epiphysis
Patient Teaching
-
The family must understand:
-
Proper cast care and the possibility of future growth abnormality with physeal injury
-
The need to bring the child for
6–12-month follow-up of Salter-Harris classification III or IV fracture
or any fracture of distal femur or proximal tibia
-
FAQ
Q: After a growth-plate injury, what is the possibility of a clinically significant deformity developing?
A:
It depends on the fracture pattern, age, and region of the bone
injured. On the whole, normal growth is more likely than substantial
growth disturbance.
It depends on the fracture pattern, age, and region of the bone
injured. On the whole, normal growth is more likely than substantial
growth disturbance.
Q: Do growth-plate injuries take longer to heal than other fractures?
A: They heal at the same rate.
