Developmental Dysplasia of the Hip
abnormal configuration of, or relationship between, the femoral head
and the acetabulum. It is a continuum of disorders that ranges from
shallowness of the acetabulum, to instability and subluxation of the
femoral head, to frank dislocation. The term development dysplasia of the hip
has replaced the former term “congenital dislocation of the hip” (CDH)
to acknowledge that the disorder may not be present at birth, and can
change or progress with growth and development.
malformation of the components of the hip joint, and is usually
associated with a syndrome such as arthrogryposis or Larsen’s syndrome.
It is thought to be secondary to an underlying “germ plasm” defect.
|
TABLE 5-1 CLASSIFICATION OF DEVELOPMENTAL DYSPLASIA OF THE HIP
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
typical form of DDH. A strong hereditary component is also known;
first-degree relatives of a person with DDH have a much higher
incidence than the general population. The persistence of maternal
relaxin hormone in the infant’s bloodstream at the time of birth has
been implicated in DDH, but recent studies have not supported this
theory.
America and Europe is approximately 0.15% (i.e., 1.5 per 1,000). A
positive family history increases the incidence of DDH approximately 35
times. Girls are more frequently affected than boys by a ratio of
approximately 4 to 1. The left hip is more frequently involved. Breech
presentation increases the incidence of DDH to approximately 20%. Some
cultures, including certain Native Americans and Laplanders, have a
markedly high rate of DDH, but this increased incidence is probably due
to positioning in traditional infant swaddling, rather than to a
genetic predisposition.
-
Increased fat in the depths of the acetabulum
-
A tight iliopsoas muscle
-
Capsular constriction at the mouth of the acetabulum
-
Anteversion of the femoral neck
-
Decreased depth of the acetabulum
-
Hypertrophy of the transverse ligament
-
Hypertrophy of the ligamentum teres
-
The development of a neolimbus.
indicates increased risk for DDH. Also, a history of other family
members with DDH is significant.
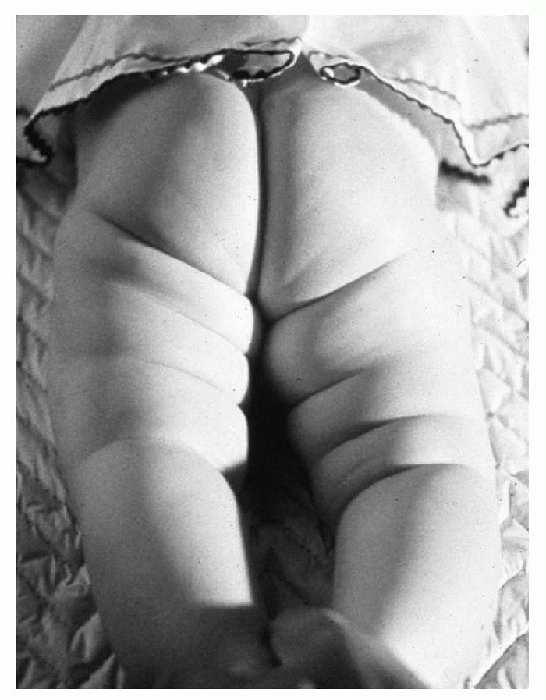
comfortable and relaxed (feeding can be helpful). Initially, inspection
of the child is carried out so that any asymmetry in the number of
thigh folds anteriorly and posteriorly (Fig. 5-1),
flexion deformities, or spinal deformities can be noted. The height of
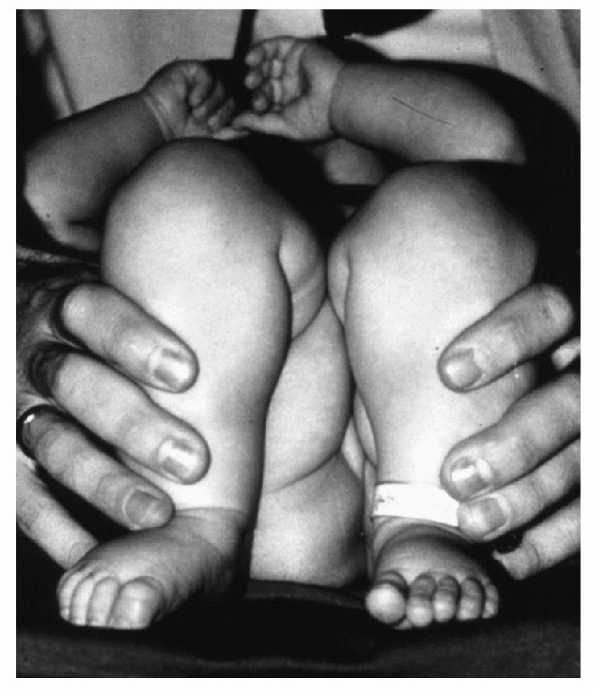
the knees with the knees and hips flexed at 90 degrees is observed
(Galeazzi sign; Fig. 5-2). In a child with a
posteriorly subluxed or dislocated hip, the femur is functionally
shortened, thus the knee on the affected side will appear lower. This
is also the reason for the increased thigh folds: the normal length
musculature of the thigh bunches up around the “short” femur.
-
Decreased abduction (less than 60 degrees)
-
Asymmetry of thigh folds (anteriorly and posteriorly)
-
Positive Galeazzi sign (Fig. 5-2)
-
Positive Ortolani signa
-
Positive Barlow signa
 |
|
Figure 5-1 Asymmetry of the thigh folds due to a dislocated left hip.
|
performed. These should be done with the baby fully undressed, on a
relatively firm surface to provide the necessary resistance.
 |
|
Figure 5-2 A positive Galeazzi sign indicating apparent shortening of the left femur due to a dislocated hip.
|
 |
|
Figure 5-3 Appropriate way of examining a newborn’s hip. One hand is holding the hip and pelvis stable (A) and the other hand is performing the maneuvers (B). (C) The middle finger is placed on the greater trochanter to detect a shift in position as seen in an Ortolani or Barlow sign.
|
-
The examiner holds the patient’s flexed
lower extremity so that the thumb is on the internal aspect of the
thigh, the patient’s knee is in the thenar web space, and the
examiner’s index or middle finger is placed over the greater trochanter
(Fig. 5-3). -
The hips are then gently abducted, one at a time, with anterior pressure on the greater trochanter.
-
A positive Ortolani sign is a palpable shift in position (clunk) of the hip with the initial abduction of the hip.
-
The hip is brought into adduction with gentle posterior pressure, and the Ortolani maneuver is repeated.
whereas a negative Ortolani test and a positive Barlow test indicate a
dislocatable hip.
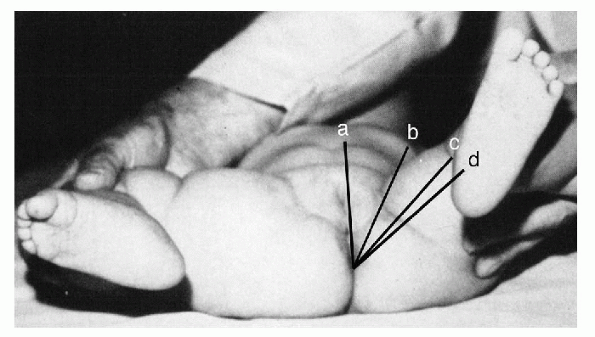
hip and the amount of adduction at which the hip re-dislocates (this
approximates the “safe zone”; Fig. 5-4). Some signs are more specific for DDH than others (i.e., suggestive signs) as indicated in Box 5-1.
and Barlow signs are likely to be negative, but the functional leg
length discrepancy in a unilateral dislocation will manifest as a limp
or toe-walking on the affected side. If both hips are dislocated, the
older child will tend to walk with a waddle, have decreased abduction
bilaterally, and have an increased lumbar lordosis. In the child over 6
months of age, decreased abduction bilaterally (less than 60 degrees)
might be the only sign of bilateral dislocations of the hips and should
be investigated with x-ray studies. Another indicator of bilateral
abnormality is the Klisic line. This is a line extrapolated through the
greater trochanter and anterior superior iliac spine. It should fall
through
or superior to the umbilicus and is independent of the contralateral
side. If the Klisic line falls inferior to the umbilicus, this
indicates a possible posterior subluxation/dislocation (Fig. 5-5).
 |
|
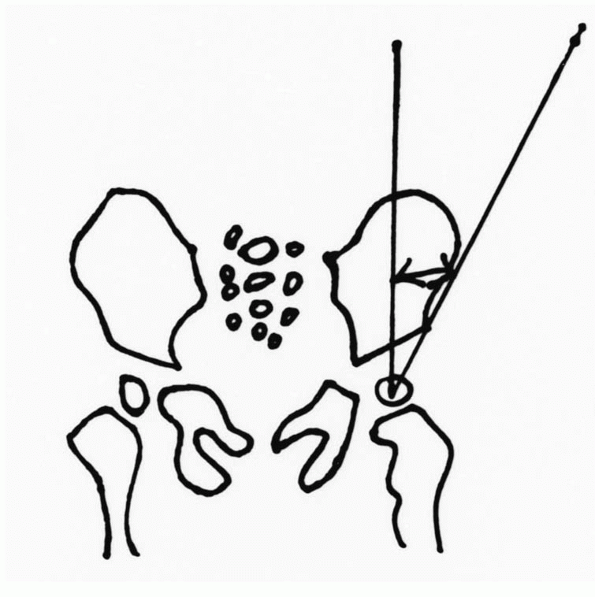
Figure 5-4
The angle a-d represents full abduction of the hip, angle a-c is 10 degrees less than full abduction, and angle a-b is the abduction at which the hip re-dislocates. The angle b-c is the “safe zone.” |
 |
|
Figure 5-5 Klisic line test.
|
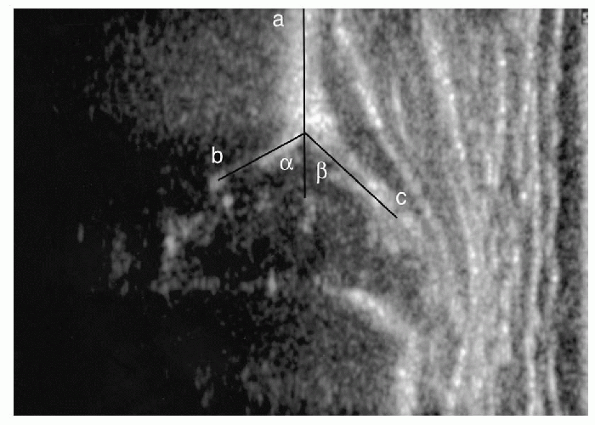
prior to the appearance of the ossific nucleus of the femoral head at
the age of 4 to 6 months. There are frequent false-positives in
newborns younger than 2 weeks of age, and because of this many
ultrasonographers prefer to obtain the initial study at 4 to 6 weeks of
age. Though routine ultrasound screening of all newborns is the norm in
some parts of Europe, it is not currently the standard in the United
States. In the United States ultrasonography (US) is generally used to
evaluate cases in which there is a highrisk history or abnormal or
equivocal physical exam. It can also be used to evaluate the results of
treatment with a Pavlic harness, and to help determine when it is safe
to terminate the Pavlic treatment.
 |
|
Figure 5-6 A normal static ultrasound picture is present with the α-angle (a-b) showing acetabular bony coverage more than 60 degrees and the β-angle (a-c) indicating the cartilaginous coverage of more than 55 degrees. Line a indicates the iliac ring.
|
important to know which one your ultrasonographer uses in order to
interpret the results. The Graf method is a static exam of the hip in
the coronal plane, and uses the relationship of the bony and
cartilaginous components of the hip joint to describe a variety of
angles, which can be followed over time (Fig. 5-6). The Harcke method is a dynamic exam which evaluates instability of the hip joint.
-
Shenton’s line: The curved line drawn
from the inferior femoral neck to the superior aspect of the obturator
foramen in the normal hip. This sign indicates no subluxation is
present if the arc is unbroken (Fig. 5-8). -
Quadrants: Four quadrants are formed by
the conjunction of the horizontal line of Hilgenreiner and the
perpendicular line of Perkins. The reduced femoral head resides in the
lower inner quadrant (see Fig. 5-8). -
Center-edge angle of Wiberg: In children
older than 6 years, the center of the femoral head is located on an AP
x-ray and a line is drawn vertically from this point. Another line is
drawn to the superior edge of the bony acetabulum and the angle formed
by these lines is recorded (Fig. 5-9).
-
Acetabular angle (acetabular index) less than 30 degrees
-
Break in Shenton’s line
-
Ossific nucleus not in lower inner quadrant
-
Decrease of center-edge angle of Wiberg (in children older than 6 years)
-
Distortion of the acetabular teardrop
-
Increased femoral metaphyseal-acetabular teardrop distance
-
Change in normal sourcil
 |
|
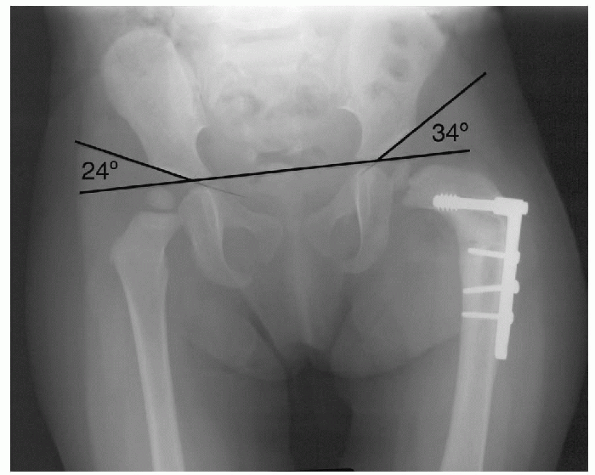
Figure 5-7
The hip is concentrically reduced after a femoral osteotomy and the acetabular angle is improved, but not below 30 degrees. The patient will probably require a pelvic osteotomy. |
 |
|
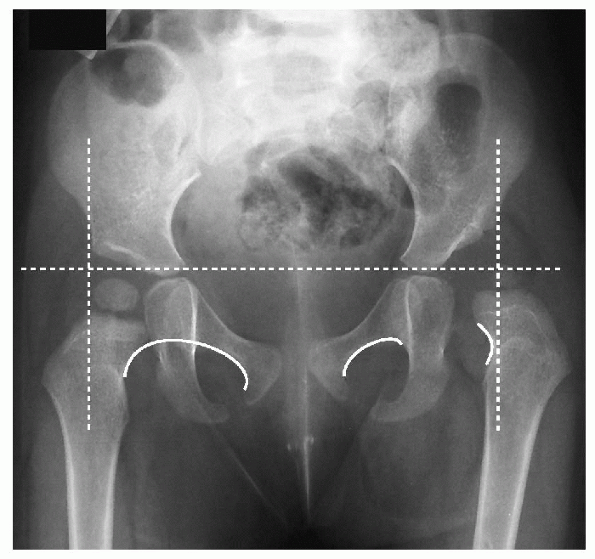
Figure 5-8
Dislocation of the left hip is present. The dashed lines reveal that the femoral head is outside and lower in the quadrant. The curved lines at right reveal a break in the Shenton’s line. |
 |
|
Figure 5-9 The center-edge angle of Wiberg.
|
in response to each other when in the reduced position, the principles
of treatment of DDH can be summarized as follows: The goal of the
treatment of DDH is to obtain and maintain, as early as possible, a
concentric reduction of the hip without force and by avoiding extremes
of position. The modes of treatment discussed in the subsequent
paragraphs are simply means to achieve this goal depending on the
patient’s age.
stable abducted position with the use of the Pavlic harness. There is a
90% to 95% success rate using this device. It must be applied properly
and the parents must be instructed in its care. The body strap is
positioned immediately below the nipple line, the anterior flexion
strap lies in front of the knee, and the posterior abduction strap is
loose to allow the baby some active motion while limiting adduction to
maintain the reduction while the soft tissues contract and stabilize
the hip. The hips are flexed to about 100 degrees (Fig. 5-10).
The Pavlic harness has been shown to stabilize reduction in 85% of hips
within 2 to 3 weeks. If, after 3 weeks of use, the hip is not reduced
on ultrasound, the use of the harness should be discontinued to prevent
complications and plans should be made for a closed reduction
arthrogram and spica casting under general anesthesia. Complications of
the use of the harness are enumerated in Box 5-3.
 |
|
Figure 5-10
The proper positioning of the straps of the Pavlic harness with the anterior straps against the medial aspect of the thigh producing sustained flexion of about 100 degrees, but no more. The posterior straps remain somewhat loose. |
-
Inferior subluxation caused by too much flexion
-
Femoral nerve palsy caused by too much flexion
-
Skin breakdown caused by lack of skin care
-
Cartilage damage or AVN caused by excessively tight straps or continued use after 3 weeks of nonreduction of the hip
 |
|
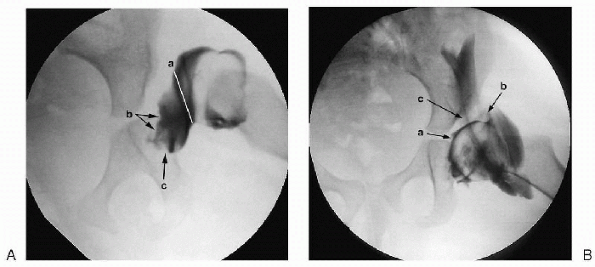
Figure 5-11 (A)
Arthrogram revealing narrowing of the capsule at the entrance of the acetabulum (a), medial soft tissue filling the acetabulum (b), and transverse acetabular ligament, which could possibly inhibit concentric reduction (c). (B) With abduction and internal rotation, there is a slight bit of medial dye-pooling (a), good coverage although the labrum is somewhat blunted (b). Dye is extravasated into the iliopsoas tendon sheath (c). |
harness is continued until the physical examination and ultrasound
examination of the hips are within normal limits. A very rough rule of
the thumb is that the harness needs to be used for the total time of
the sum of the patient’s age at the beginning of treatment plus 6 weeks
(i.e., if an infant is 3 weeks old at the onset of treatment, the
harness should be used for about 3 weeks plus 6 weeks, for a total of 9
weeks).
few degrees less than full abduction to the point of dislocation on
adduction. Immobilization in full abduction can cause avascular
necrosis and should be avoided, whereas dislocation results from too
little abduction. Thus, the safe zone is between these extremes (see Fig. 5-4). The smaller the safe zone in an individual patient, the more difficult the hip is to treat successfully nonoperatively.
Pavlic harness in this age group. Traditionally, skin traction has been
used to gradually and gently pull the femoral head distally so that it
descends past the superior edge of the acetabulum allowing a closed
reduction to be performed without excessive force, thus resulting in a
lower incidence of avascular necrosis (AVN). Traction can be performed
at home, if the facilities exist, but must be checked frequently since
skin complications and compartment syndromes are not unusual. A
percutaneous adductor tenotomy is usually employed to assist in this
treatment by improving the safe zone.
skin traction is not necessary to safely reduce the hip in this group,
and elect to perform a percutaneous adductor tenotomy, a hip arthrogram
(Fig. 5-11), and gentle closed reduction under
general anesthesia, followed by the maintenance of this reduction in a
double hip spica cast in the
“human
position” (abduction of about 45 degrees and flexion of about 100
degrees). A postoperative computed tomography scan is usually necessary
to confirm concentric reduction in the hip spica cast. Spica casting is
continued for 6 weeks to 6 months, with periodic changes, and a plastic
abduction brace is used at least until the child is walking, and
usually until the standing AP x-ray of the hips is within normal
limits. Treatment is discontinued if the criteria in Box 5-4 are met.
5-4 CRITERIA INDICATING FAVORABLE PROGNOSIS FOR FUTURE HIP DEVELOPMENT
AFTER CLOSED REDUCTION OF DEVELOPMENTAL DYSPLASIA OF THE HIPa
-
Shenton line essentially intact
-
Acetabular angle less than 30 degrees
-
Less than 2-mm difference between the teardrop distances
-
Femoral head in lower inner quadrant
arthrogram, and open reduction must be performed. Although European
studies have suggested that an open reduction has a lower incidence of
AVN after the appearance of the ossific nucleus (at about 6 months of
age) this observation has not been borne out in other literature, and
the timing of surgery remains somewhat controversial. If open reduction
is required in a child under the age of 12 months, a medial approach
(Ludloff, Staheli) or anterior-medial approach (Ponseti-Weinstein) can
be performed. I prefer the traditional anterior approach
(Smith-Petersen), since it affords visualization of the entire femoral
head and acetabulum and plication of the capsule can be done to ensure
stability of the hip. A “bikini” incision is used, since this incision
is cosmetically pleasing. In children over the age of 1 year, the
medial approach has a higher complication rate and is not recommended.
-
Varus derotation osteotomy of the femur, Pemberton
-
Salter osteotomy
-
Dega osteotomy
-
Pemberton osteotomy
-
Staheli shelf
-
± Femoral osteotomy with shortening
-
Triple osteotomy (Steele)
-
Double pelvic osteotomy (Southerland)
-
Staheli shelf
-
± Femoral shortening and osteotomy
-
Dial acetabular osteotomy (Eppright)
-
Wagner/Ganz
-
Chiari osteotomy
-
Femoral shortening osteotomy
in children between 12 and 18 months of age, a femoral osteotomy or
pelvic osteotomy can be performed. A variety of pelvic osteotomies may
be employed. Femoral and pelvic osteotomies can also be used together (Box 5-5).
In the child older than 2 to 3 years of age, a femoral shortening
should be performed in addition to the open reduction and femoral or
pelvic osteotomies, in order to minimize the risk of AVN. In the child
older than age 6 years, a unilateral dislocation will require an open
reduction, femoral shortening (with varus de-rotation as needed),
adductor release, iliopsoas release, and acetabular procedure such as a
Salter osteotomy (less than 8 years). In the child over 8 years, a
triple (Steele) or double (Southerland) pelvic osteotomy, or a shelf
procedure (e.g., Staheli) should be used. If the growth plates are
closed, a Chiari, Wagner, Dial (Eppright), triple, or double pelvic
osteotomy can be performed in addition to the soft tissue releases,
femoral shortening, and varus derotation osteotomy. The use of native
cartilage is theoretically preferable to cover the femoral head (e.g.,
Salter, triple osteotomy) rather than relying on the development of
fibrocartilage (e.g., Chiari).
10 years of age), the option of no treatment should be considered.
These patients frequently have a relatively pain-free existence up to
the age of about 50 years of age and the risks of surgical treatment
are considerable.
dislocation carries a complication rate of about 50% including
re-dislocation and AVN. Therefore, one should consider not treating
these hips, depending upon the patient’s overall health and functional
status. The signs and symptoms of untreated DDH are outlined in Box 5-6.
iatrogenic complication and produces poor results. AVN can be usually
prevented by avoiding extremes of position and excessive force during
casting. Signs of AVN are listed in Box 5-7.
the hip is stable in a walking position and a standing AP of the hips appears normal.
-
Apparent leg length discrepancy
-
Scoliosis
-
Ipsilateral knee pain
-
Ipsilateral valgus knee deformity with degenerative arthritis
-
Gait disturbance
-
Pain (with false acetabulum)
-
Lumbar spine degeneration and pain
-
Waddling gait (bilateral positive Trendelenburg gait)
-
Hyperlordosis
-
Back pain and early arthritis
-
Fatigue (early)
-
Pain (if false acetabulum present)
-
Positive Trendelenburg and antalgic gait
-
Early degenerative arthritis with severe pain (by 15-25 years of age); very early total hip replacement
hips without excessive force or extremes of position before the age of
4 usually results in hips that are very close to normal. Long-term
follow-up should consist of yearly office visits until the patient
attains skeletal maturity. It should be remembered that the
contralateral hip demonstrates abnormality in 50% of the cases of DDH
and should also be watched. Unrecognized subluxed hips or dislocated
hips can result in early degenerative changes, causing pain and
disability by the age of 15 to 25. This situation can necessitate early
total hip replacement, arthrodesis, or pelvic osteotomy.
-
Failure of appearance of ossific nucleus within 1 year after reduction
-
No increase in size of the existing ossific nucleus for 1 year after reduction
-
Widening of femoral neck within 1 year after reduction
-
Fragmentation or increased density of ossific nucleus
-
Deformation of ossified femoral head or neck
JK, Cavadias A. Open reduction of CDH before one year of age. 69 hips
followed for thirteen years. ACTA Orthop Scand 1993;64:188-192.
E, Choi IH, Gille JT, et al. Prognostic factors in congenital
dislocation of the hip treated with closed reduction. The importance of
arthrographic evaluation. J Bone Joint Surg (Am) 1992;74: 1140-1152.
HT. The role of ultrasound in the diagnosis and management of
congenital dislocation and dysplasia of the hip. J Bone Joint Surg (Am)
1991;73:622.
HO, Chen Kuo KN, Lubicky JP. Prognosticating factors in acetabular
development following reduction of development dysplasia of the hip. J
Pediatr Orthop 1994;14:3-8.
P, Jankovic L. Combined procedure of open reduction and shortening of
the femur in the treatment of congenital dislocation of the hips in
older children. Clin Orthop 1976;119:60.
The functional method of treatment using a harness with stirrups as a
primary method of conservative therapy for infants with congenital
dislocation of the hip. Clin Orthop 1992;281:4-10.
JT, Matan A, Coleman SS, et al. The predictive value of the development
of the acetabular teardrop figure and developmental dysplasia of the
hip. J Pediatr Orthop 1997;17:165-169.
