LIMB-LENGTH DISCREPANCY IN CHILDREN
Staff Surgeon, Shriners’ Hospital for Children, Portland Department of
Orthopaedics, Oregon Health Sciences University, Portland, Oregon,
97201.
growth complicates the longitudinal evaluation of each patient.
Therefore, the orthopaedic surgeon must have an understanding of growth
and the methods by which to analyze and predict future changes; this is
particularly important before considering any surgery to correct
limb-length discrepancy.
torso, and head. The limbs constitute approximately half of this total
height, and they are the most kinetic component of the body during
gait. Length abnormalities of the limbs have the potential to affect
both height and efficiency of gait.
common. Reports have suggested some level of discrepancy in up to 70%
of adult males (72). In a review of more than
100 Swedish laborers, 30% had a limb-length discrepancy of 1.0 to 1.5
cm, 4% had 2.0 to 2.5 cm, and 0.7% had more than a 2.5 cm discrepancy (35).
Estimates are especially difficult in the changing pediatric
population, but for individual congenital conditions, the incidence
could be predicted more reliably.
pediatric orthopaedic conditions, is the natural history of the
condition. Parents are commonly concerned about the long-term effects
of a limb-length discrepancy on the spine, but cause-and-effect
relationships are unknown. Low back pain in the child is rare, even for
a child with a limb-length discrepancy. Given the high rate of back
pain in the normal adult population, we may assume that this rate of
back pain must also exist for the same reasons in the population with
limb-length discrepancies. Changes in adult spine radiographs, such as
vertebral wedging and traction spurs, have been associated with
limb-length differences of more than 9 mm, but these findings have not
been correlated with symptoms (22,26,27,79). Reviews of adults with minor discrepancies have suggested a relatively low association with low back pain (62,77,92).
Other studies confirm that adult patients presenting with low back pain
associated with limb-length discrepancy appear to have symptomatic
relief after equalization surgery (71,84).
However, the causative effects of one deformity on the other are
unknown. Lumbar facet orientation does not correlate well with
asymmetric changes in limb length (24). The direction of the curve is not always in the direction expected based on the limb-length difference (33). This makes it more difficult to postulate that the limb-length difference is the causative factor.
Theoretically, this problem should result in force concentration on the
lateral edge of the acetabulum, with resultant early arthritis. Gait
lab studies, however, suggest the possibility that high-side hip forces
may actually decrease during stance phase (13). Little long-term clinical information exists on the subject.
seem to be common in children. A report has been made of increased
incidence of knee pain in athletes (47). The
most common associated problem in the foot is equinus on the short
side. When the problem is not followed closely, a contracture may
result from years of compensation in this position.
compensate for differences in limb length. Their increased joint
flexibility and higher strength-to-weight ratio may result in
adjustments that produce a smooth, even gait. With greater
discrepancies between the two legs, compensation becomes more
difficult. Coronal plane pelvic tilt may increase the energy
consumption of gait.
discrepancies have suggested a quite variable pattern of compensation
among individuals (44,51,76).
Those with less than 3% discrepancy do not require compensatory
strategies. Compensation for greater discrepancies results in greater
work and greater vertical displacement of the center of body mass. Each
child applies compensatory mechanisms differently; the most common are
walking with the short-side ankle in equinus or the long-side knee in
flexion. Energy consumption studies have yet to be completed to confirm
the meaning of these changes to gait efficiency.
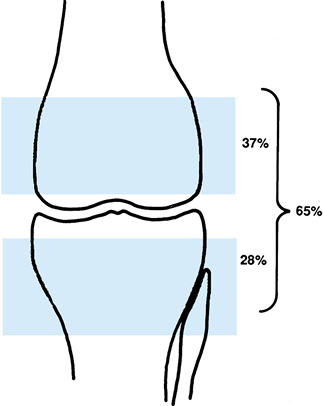
physeal new bone production and actual epiphyseal size increase.
Epiphyseal size increase usually accounts for only about 5% of the
total growth of the limb, but for calculation purposes, this increase
is usually ignored (Fig. 170.1).
The growth plates at the knee contribute the most to total limb length,
whereas the distal tibial and proximal femoral physes add lesser
amounts.
 |
|
Figure 170.1.
The distal femoral and proximal tibial physes contribute constant proportions to the growth of the leg. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:855, with permission.) |
understanding patterns of growth in the short term. One study suggests
that children have week-to-week variability in limb growth, with
pulsatile patterns of miniature growth spurts every 30 to 55 days,
alternating with periods of slower growth (32). In the longer term, however, the growth pattern evens out.
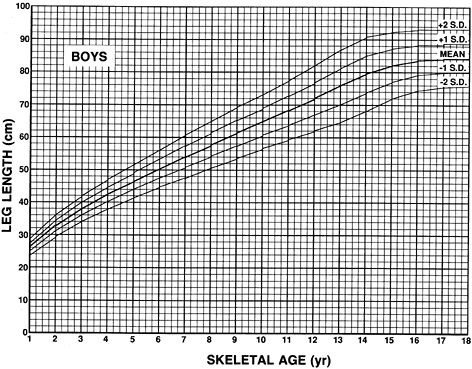
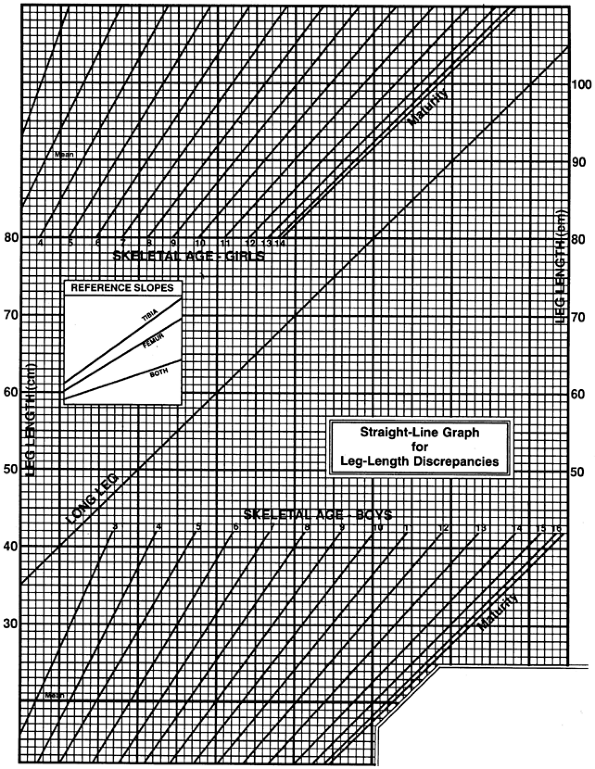
In one, data were collected instantaneously on children between 5 years
of age and maturity. In the other, a group was followed longitudinally
until maturity. Their data were reported in tabular and graphic forms
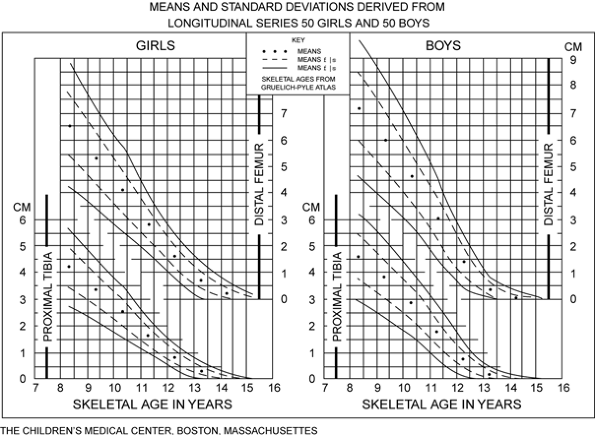
as total limb length as a function of skeletal age (Fig. 170.2). These were converted into the growth-remaining charts for the distal femur and proximal tibia (Fig. 170.3).
 |
|
Figure 170.2.
Graph of total limb length (femur plus tibia only) for boys. An individual boy may be plotted instantaneously and projected into the future based on his current situation. (From Anderson M, Messner MB, Green WT. Distribution of Lengths of the Normal Femur and Tibia in Children from One to Eighteen Years of Age. J Bone Joint Surg 1964;46A:1197, with permission.) |
 |
|
Figure 170.3.
Green-Anderson growth-remaining graph for girls and boys. This plots the amount of remaining growth from each of the distal femoral and proximal tibial epiphyses as functions of the skeletal age. The mean is in the center, whereas one and two standard deviations in each direction are represented by the other lines. This enables the calculation of results if an epiphysiodesis is done. (From Anderson M, Green WT, Messner MB. Growth and Predictions of Growth in the Lower Extremities. J Bone Joint Surg 45A:1963, with permission.) |
the interaction of patient age, maturity, and limb length. Growth rate
is maximal at the time of birth, both in percentage gain and in
absolute terms. The absolute rate of growth relative to chronologic
years drops slightly between 3 years of age and the adolescent growth
spurt. During the adolescent growth spurt, the absolute rate of growth
increases. Cessation of growth occurs in boys at 16 to 17 years of age,
and in girls at 14 to 15 years of age. When we compare different
people, it becomes quickly evident that their times of maturation, as
measured in chronologic years, vary considerably. One child who may
appear to be tall may just be going through the process of maturation
at an earlier time. In fact, this “temporarily” tall child may then end
up shorter than a second child who, although shorter initially, matures
at a later time as measured by chronologic age.
appears to be radiographs of the bones. The standard radiograph has
become the anteroposterior view of the left wrist, although other x-ray
techniques are available (81). The skeletal age
of a patient is defined as the age at which the general population, on
average, reaches the same level of bony development as that patient.
This skeletal age correlates more closely than chronological age with
other signs of maturation, including menarche, secondary sexual
characteristics, height, and limb length. Measurement of skeletal age
with the anteroposterior view of the wrist, however, remains the weak
point in predicting limb-length discrepancy, both because of
reliability of readings and because of more variability in children
with limb-length discrepancy (15,18).
chronologic age, the average skeletal age should equal chronologic age.
However, time of maturation varies greatly between people; thus, for
any given child, the skeletal age does not necessarily equal the
chronologic age. A child who matures earlier than his peers appears to
go
through
a maturation spurt in which the skeletal age years are changing more
quickly than the chronologic years. The other milestones of maturity
(secondary sexual characteristics, menarche, and limb growth) are
moving forward at a similar, early rate.
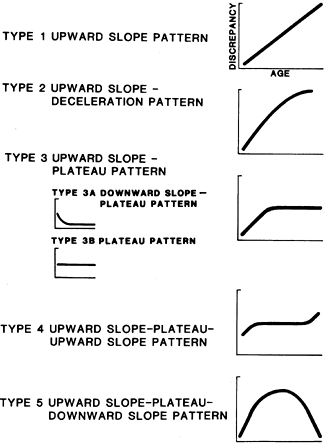
Three phases are used to describe the change over time: In the initial
phase, the discrepancy develops; in the middle phase, a pattern of
difference is established during further growth; and the final phase is
the period of time before growth cessation. Patient age is plotted
against the limb-length discrepancy on a graph. By definition, the
initial phase results in an increase in discrepancy. During the middle
phase, the discrepancies are variable; some continue to increase (e.g.,
a traumatic physeal closure), whereas others plateau (e.g., a patient
being treated for juvenile rheumatoid arthritis). The final phase is
also variable in that a discrepancy may increase, plateau, or decrease.
Again, conditions that cause permanent physeal damage tend to cause a
steady increase in discrepancy, whereas other conditions are associated
with a plateau in differences (e.g., improvement in functional level in
a paralytic limb, as with a brace). The most common scenario for an
actual decrease in limb-length discrepancy is
that of a treated juvenile rheumatoid arthritis patient (75,86).
 |
|
Figure 170.4.
Various patterns of changes in limb-length discrepancy over time. The patterns shown are based on absolute magnitude of discrepancy, and thus the graphs do not take into account the natural slowing of growth near maturity. (Shapiro F. Developmental Patterns in Lower Extremity Length Discrepancies. J Bone Joint Surg 1982;64-A:639.) |
discrepancy by Shapiro’s technique are useful for large groups of
patients, but it may be less useful for the individual patient. This is
because patterns are plotted to age 13 rather than maturity, and the
differences are related to chronologic age rather than the skeletal
age. This technique also does not compare the pattern of the
limb-length difference curve with the normal growth curve or take into
account lengthening of either leg with growth, whether it is normal or
not.
limbs that make up the leg’s effective length. Variable heights of the
two sides of the pelvis and pelvic obliquity to the floor result in a
functional difference in limb lengths. Scoliosis and hip abduction and
adduction contractures are common situations in which resultant changes
in the orientation of the pelvis to the ground create apparent changes
in the limb length. The other commonly overlooked source of difference
between limb lengths is the foot. Some loss of height may be expected
from either varus or valgus collapse of the foot, and the operated
hindfoot may lose a portion of its vertical height.
change length directly or from an alteration in growth. Fractures,
dislocations, and surgery are the only mechanisms by which length is
changed acutely.
congenitally short limb is genetically programmed to be shorter via
slower physeal growth. A growth plate injury may result in slowing or
complete cessation of growth. External influences such as disuse, as
may occur in polio or hemiplegia, may also cause slowing of growth.
Experimental denervation of sciatic nerves in animal models suggest a
slowed rate of maturation in denervated bone (20).
hemihypertrophic or hemiatrophic, although distinguishing between the
two may be difficult (7). Typically, the
shortening involves all parts of the involved limb. It is probably best
to consider each limb as being genetically programmed at a different
rate of growth. Plotting sequential growth on the straight-line graph
should confirm this.
anomalies of other bones or independently. The congenital short femur
is considered to be a variant of proximal focal femoral deficiency (43).
The spectrum of the presentation includes anterior cruciate ligament
deficiency, absence of the fibula, progressive ankle valgus deformity,
absence of the lateral ray or rays of the foot, and tarsal coalitions.
Congenitally short tibiae are commonly associated with both posterior
and anterior bowing deformities.
the zone of hypertrophy. Fortunately, this weak area of the physis is
not responsible for the continued generation of growth cells, which
occurs closer to the epiphysis. Thus in the Salter-Harris
classification of epiphyseal fracture type I and II injuries (see Chapter 164)
tend not to result in long-term growth disturbances, with a few
exceptions. The type V crush injury, however, may permanently damage
cells at all levels of the physis. Type III and IV fractures do cross
the growth zone of the physis; thus, they are most prone to formation
of a bridge of bone or physeal closure. Anatomic reduction of type III
and IV fractures helps prevent physeal abnormalities. When physeal bars
form or partial closure occurs, angular malalignment occurs because of
asymmetric involvement of the growth plate. Physeal closure has also
been recognized as a complication of diaphyseal fractures of the
ipsilateral limb (8).
severe results because of the young age at which this occurs. Direct
invasion of the physeal cells occurs in hematogenous osteomyelitis,
sometimes in conjunction with a septic joint. The bridges that result
tend to be broader and more central than those that result from
fractures, and thus, they are more difficult to resect successfully. A
so-called sick physis may develop when an infection has a global effect
on a physis. The cellular effects of the infection on the physis then
either slow the rate of growth or create a delayed complete or partial
arrest. Meningococcemia is one of the more common infectious processes
that create this delayed growth arrest.
completely clear. Theories have included decreased blood flow, poor
venous return, decreased neurogenic input to the physis, and disuse
atrophy. Polio commonly results in
significant
differences in limb lengths. Hemiplegic cerebral palsy patients may
have small differences in length, which seldom require surgical
correction. Hemiplegic patients often appear to have more of a
discrepancy because of asymmetric muscle tone and other joint
contractures that result in pelvic obliquity.
destructive effect similar to infection. Abnormal cartilage emanating
from the physeal cells may also disturb normal growth patterns. In
enchondromatosis and Ollier’s disease, abnormal physeal cells produce
tumor cartilage rather than cartilage for longitudinal growth.
Osteochondromata may have more of a mechanical effect on growth plates
that may disturb growth, such as at the distal tibia. This is more
commonly angular than longitudinal.
clinical problems arising secondary to avascular necrosis. Fortunately,
the proximal femur is responsible for only about 15% of limb length.
Clinical presentations include the treated developmental hip
dislocation, traumatic hip dislocations and fractures, slipped capital
femoral epiphysis, and Legg-Calvé-Perthes disease. A common situation
with avascular necrosis of the proximal femur is a severe adduction
contracture secondary to femoral head collapse. This results in a large
apparent length discrepancy, which is actually due to a marked coronal
plane pelvic obliquity.
arteriovenous malformation, inflammation, fracture, and tumor. From a
clinical standpoint, surgical creation of a situation that mimics these
conditions has failed to provide reproducible increases in growth.
growth stimulation, presumably via increased blood flow. Other
nonvascular growths such as neurofibromatosis, fibrous dysplasia, and
Wilms’ tumor may result in overgrowth, usually of focal areas of bones.
If the fibula is not also fractured, a relative increase in tibial
length results in progressive valgus deformity at the knee.
cases, chronic osteomyelitis may actually result in physeal
stimulation. Another common example is pauciarticular juvenile
rheumatoid arthritis, in which overgrowth of the involved limb is
common, particularly before 3 years of age (75,86).
assessment in limb-length differences. Physicians may tend to focus on
radiographic findings; however, radiographic methods can have inherent
artifacts from patient movement or from poor conversion of an angular
deformity to two-plane measurement. In addition, many other clinical
factors not measured by radiographs are important in making treatment
decisions. Once the complete historical and physical evidence has been
obtained, radiographs may be used to fine-tune data and to follow the
condition precisely.
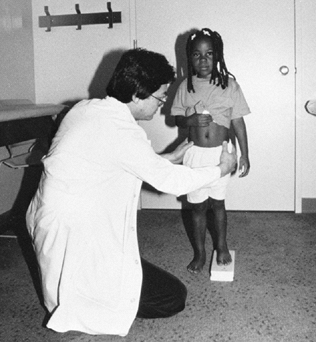
the foot of the short side of the patient in the standing position. The
height can be adjusted until the pelvis is level, as judged by the
anterior superior iliac spines from the front or the posterior iliac
crests from the back (Fig. 170.5) This
technique is generally the most reliable and provides the most
comprehensive information, because it allows the clinician to take into
account pelvic obliquity, contractures, angular deformities, and
differences in foot height. To use the technique even more effectively,
shoe lifts of variable heights may be used; this allows evaluation of
gait and dynamic events, with partial to complete correction of
differences (Fig. 170.17).
 |
|
Figure 170.5.
The standing technique of limb-length measurement is done with the patient standing on blocks on the short side until the anterior superior iliac spines are at the same level. It may also be visualized from behind the patient, using the top of the iliac crests as the measure of level. |
 |
|
Figure 170.17.
Variable sizes of lifts are attached to the bottom of the shoe with hook-and-pile strips. These allow trials of differing amounts, which are particularly helpful in deciding how much to shorten a limb. |
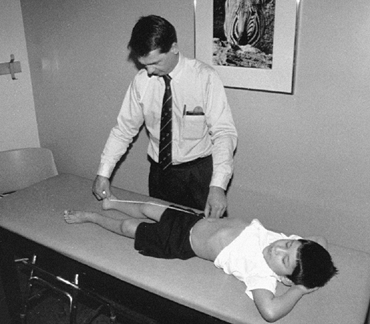
been to measure from the anterior superior iliac spine to the medial
malleolus, in the supine or standing position, using a tape measure. (Fig. 170.6).
This method has some value, but reproducibility may be poor because of
poorly palpable landmarks, tenting of the tape, angular deformity at
the knee, and differences in the height of the pelvis (49). In addition, this measurement does not take into account angular deformity (i.e., obliquity) about the pelvis.
 |
|
Figure 170.6.
The supine technique of limb-length measurement is done with the tape measure from the anterior superior iliac spine to the medial malleolus with the knee straight. Because of difficulties in reproducing accurate measurements, the standing technique is generally preferred. |
they may be more valuable over the long term for evaluating growth
trends. All of the radiographic techniques used have variability
between readings because of differences in technician techniques,
changes in patient position, and differences in techniques and
landmarks of people reading the films. The orthopaedic surgeon must
review all of the data derived from radiographs before considering
surgery, check for consistency, and correlate the data with clinical
findings.
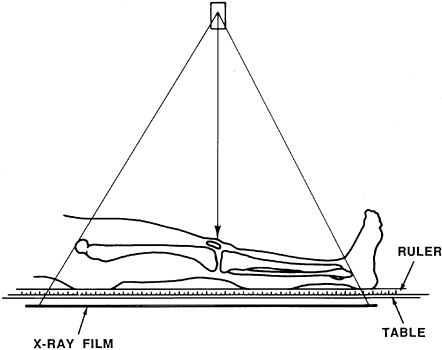
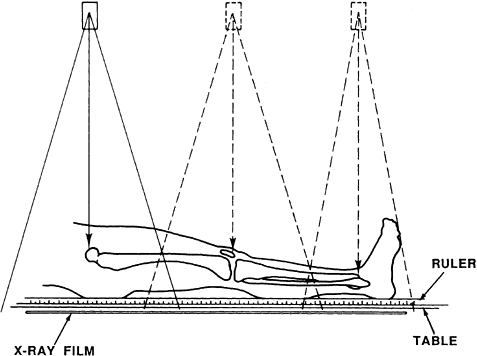
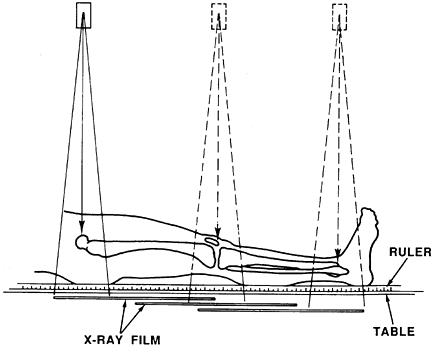
radiographic measurement techniques. The original scanogram was done
with a collimated x-ray beam directed through a transverse slit that
exposed a film beneath the patient as the x-ray tube was moved from one
end of the limb to the other. The teleoradiograph is a single-exposure
x-ray shot from a 2 m (6 ft) distance with a radiopaque ruler placed on
the film cassette. It can reveal an angular deformity but has the
disadvantage of increasing distortion through parallax of the x-ray
beam (Fig. 170.7) The orthoradiograph avoids
the parallax problem by taking three separate exposures on the same
ruled cassette. Like the teleoradiograph, the large film size can be
cumbersome (Fig. 170.8). The current scanogram
technique uses three exposures, but the cassette is moved beneath the
patient between each image. The ruler must be fixed to the x-ray table,
which is not a necessity with the single exposure techniques (Fig. 170.9).
The patient must be able to remain still between exposures with the
teleoradiograph and the scanogram. For children younger than 5 or 6
years of age, the teleoradiograph is more appropriate.
 |
|
Figure 170.7.
The supine teleoradiogram method. Parallax effect is greater with a single exposure. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:865, with permission.) |
 |
|
Figure 170.8.
The orthoradiograph. When three separate exposures are used, parallax is minimized, but the patient must be able to hold still for three images to avoid inaccuracies. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:865, with permission.) |
 |
|
Figure 170.9.
The scanogram: The three exposures are taken after positioning a portion of the 14-by-17-inch cassette behind each of the hip, knee, and ankle joints. (From Moseley CF. Leg-Length Discrepancy. In Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:866.) |
on one film of relatively convenient size. As long as the patient does
not move between exposures and no joint contractures are present, this
provides an accurate and relatively reproducible methodology (3,29).
When knee contractures are present, the bones may be measured
individually by placing the patient prone for a ruled radiograph of the
femur, and in the lateral position for the film of the tibia.
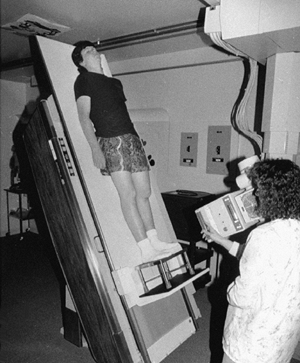
semierect, with the short side blocked up beneath the foot to level the
pelvis. Separate images are then taken of the hips, knees, and ankles,
including the plantar portion of the foot (Fig. 170.10).
The semierect position has the advantage of mimicking the upright
weight-bearing position, leveling the pelvis for more accurate
measurement, limiting patient motion between exposures, and allowing
evaluation of the contribution of the foot to the discrepancy. The only
disadvantage is that a tilting x-ray table is required.
 |
|
Figure 170.10.
The semierect scanogram method. The tilt table allows for placement of lifts for leveling the pelvis, and will give more accurate information about joint and length changes with weight bearing. The three images of the hips, knees, and ankles are taken in the same way as with the supine technique shown in Figure 170.7. |
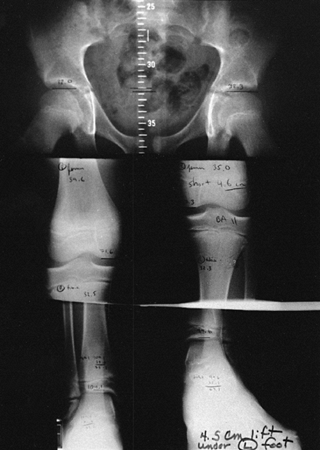
are the tops of the femoral head and the middle of the “saddle” formed
by the subchondral bone of the distal tibial plafond. If separation
into femoral and tibial components is required, use the medial femoral
condyle. Then draw a horizontal line from the chosen points to the
ruled area on the film. Each of these lines should be parallel to the
edge of the film. (This assumes that the edge of the cassette is close
to being perpendicular to the orientation of the leg.) By subtracting
these numbers, the lengths
of both legs and the femoral and tibial components may be calculated (Fig. 170.11.)
 |
|
Figure 170.11.
Sample orthoroentgenogram. Results may be analyzed on one film of convenient size, but this film does not allow accurate calculation of mechanical or anatomical axis. |
the orthoroentgenogram. It offers the advantage of being more accurate
and delivering less radiation, but for many centers, the technique is
more cumbersome and it is expensive to obtain (1,36).
A decision should be made on the basis of cost and availability because
the accuracy of the two techniques appears to be comparable.
an effective screening tool, although slightly less accurate than
radiography, for limb-length determination (42,82).
radiographic landmarks of maturity with standards. The Greulich-Pyle
atlas is the most commonly used standard today (30).
The left hand and wrist are imaged in the anteroposterior plane;
separate standards are used for boys and girls. The standard radiograph
in the atlas represents the median level of bony maturity for the
chronologic age. Given a random sampling of children at the same
chronologic age, half of the left hand and wrist radiographs would
appear more mature and half would appear less mature than the standard.
For any given child, then, the skeletal age is that which corresponds
with the best radiographic match from the atlas (Fig. 170.12).
 |
|
Figure 170.12. Left hand and wrist anteroposterior radiograph taken for bone age estimation.
|
weakest link in the process of limb-length calculations. Differences
between children in the order of bone maturation around the wrist,
extrapolation between ages in the atlas, and congenital anomalies of
wrist bones may result in different interpretations of the radiograph
for skeletal age (15,18).
Other methods have been used to determine skeletal age and are probably
more exacting, but they are also more cumbersome. In addition, all of
the predictive growth data derived by Green and Anderson are based on
the Greulich-Pyle atlas. Other methods of skeletal age
determination
do not necessarily correlate with the Greulich-Pyle skeletal age and,
thus, should not be used with Green and Anderson’s data for surgical
calculations.
change without surgical intervention. The growing child, on the other
hand, is continuously changing. The goal of the orthopaedic surgeon
must be to predict the situation at maturity. In most cases, this means
analyzing the data from a young age to predict the limb-length
difference at maturity. Treatment should be based on this prediction,
so careful analysis of the data is crucial (10).
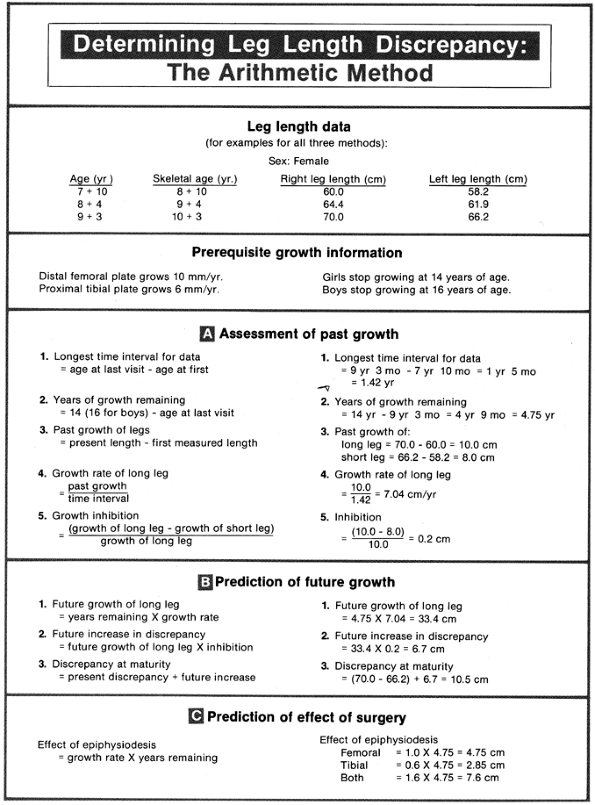
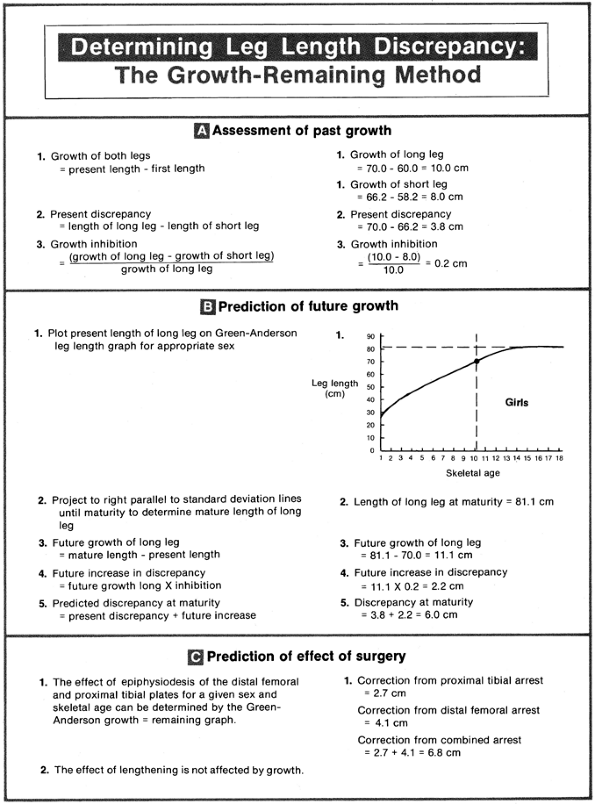
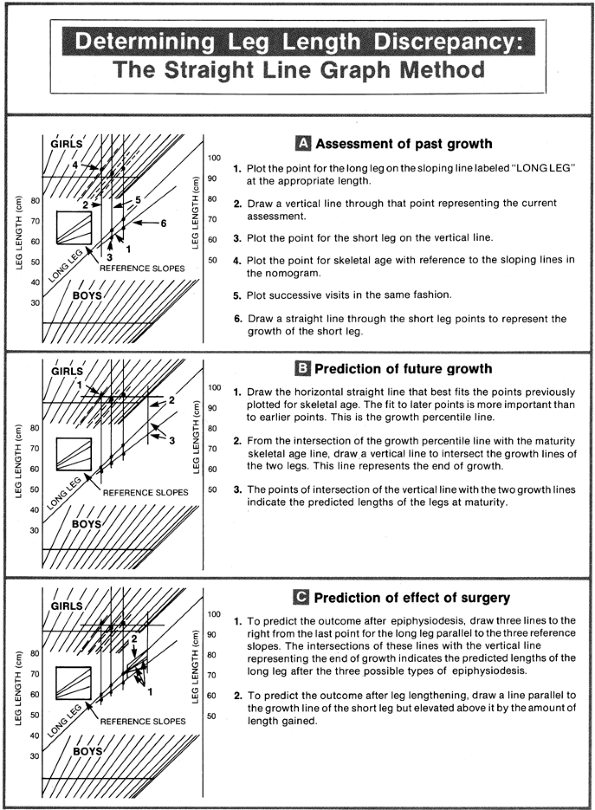
At present, three general methods are used widely for data analysis—the
arithmetic method, the growth-remaining method, and the straight-line
graph method. They all use roughly the same steps of analysis but with
different techniques. The first step is evaluation of past growth, the
second step is prediction of future growth, and the third step is
evaluation of what the results of surgical correction would be.
 |
|
Figure 170.13.
Arithmetic method of limb-length discrepancy determination. In the left column, a theoretical explanation, and on the right, a sample calculation. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:869.) |
-
Girls stop growing at chronologic age 14.
-
Boys stop growing at chronologic age 16.
-
The distal femur grows at a rate of 3/8 inch (10 mm) per year.
-
The proximal tibia grows at a rate of ¼ inch (6 mm) per year.
inaccuracies. The estimations of growth are most accurate during the
last few years of growth, but are relatively inaccurate in younger
children. In addition, the chronologic age is the basis for the
measurements and determinations. As discussed earlier, the patient’s
chronologic age and bone age may vary considerably, but the bone age is
a more reliable indicator of skeletal maturity for individual patients.
well before surgery is being considered. As the time for surgery nears,
other, more precise methods should be used to minimize errors and make
correction as exacting as possible.
The percentage of growth inhibition of the short leg is first
calculated. Using these data, the lengths of long and short legs at
maturity can be predicted. The graphs of the growth remaining from the
distal femoral and proximal tibial physes are used to determine
appropriate times for epiphysiodesis (Fig. 170.14).
 |
|
Figure 170.14.
Growth-remaining method of leg-length discrepancy determination. In the left column, a theoretical explanation, and on the right, a sample calculation. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:870.) |
uses growth percentile of the child to predict future growth. The
technique does have some disadvantages: It requires two sets of graphs
in making the calculations, and it relies heavily on the most recent
skeletal age for predictions.
and is used as a method of recording, analyzing, and predicting both
growth and the results of treatment. The method is based on two
principles: First, the growth of each leg can be graphically
represented as a straight line, and second, a nomogram can be used to
determine the growth percentile, based on skeletal age and limb length (Fig. 170.15).
 |
|
Figure 170.15.
Straight-line graph, composed of three sections. The central line for plotting the length of the long leg in centimeters is predefined by the graph. The sloping lines are areas for plotting bone ages, with girls above and boys below. The reference slopes allow plotting of growth lines to predict changes after epiphysiodesis. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:871.) |
each end, representing the high rate of growth during infancy and the
slowing rate before skeletal maturity. By manipulation of the scale of
the x-axis at each end of the growth curve, the length of the limb can
be graphically represented as a straight line. The long limb is thus
assigned the graphic slope of 1.00, representing 100% of normal growth.
If no variable disease process or treatment is changing the short limb,
it will also follow a straight line on the graph over time. The
discrepancy between the two limbs is thus represented by the vertical
distance between the two growth lines, and the inhibition by the
difference in the lines’ slopes.
graph to allow the long limb length to be compared with that of the
Green-Anderson population. If a child grew such that the bone age and
limb lengths progressed together exactly as the Green and Anderson data
would suggest, the points on the nomogram would describe a perfect
horizontal line. This rarely happens, both because of the inherent
differences in the reading of bone ages and differences in growth of
individual children. As an increasing number of estimates of bone age
are obtained, these differences tend to diminish such that a more
accurate best horizontal line estimate through the points can be
obtained. Generally, heavier weighting is given to the most recent bone
age readings when making a best horizontal line estimate.
graph as well. Changes in the growth rate of either leg result in a
change in slope of the line representing
that
leg. Lengthening a limb results in simple upward vertical displacement
of the line; shortening results in downward vertical displacement. When
an epiphysiodesis is performed on a long limb, the slope of the line
representing that leg decreases by an exact amount. This is because
each epiphysis contributes a known amount to the length of the leg.
Reference slopes placed on the graph include slopes of lines
representing a normal (long) limb after proximal tibial epiphysiodesis,
after distal femoral epiphysiodesis, and after both epiphysiodeses done
simultaneously. Figure 170.16 shows a sample calculation using the straight-line graph.
 |
|
Figure 170.16.
Straight-line graph method of leg-length discrepancy determination. The step-by-step instructions for a sample patient are shown, using the same example as in Figure 170.13. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:873.) |
represents the time of birth, and the long limb begins at 35 cm, not
zero. If calculations depend on inhibition from the time of conception
(such as congenitally short limbs), the long-limb and the short-limb
lines will converge off the graph to the left, where the limb length is
zero. If the growth inhibition began at a later date after birth (such
as early physeal closure from infection), then convergence of lines
will occur at a later date on the graph.
takes into account growth percentile in prediction of future growth and
results of surgery, decreases the inherent
error
of single skeletal age measurements, eliminates the need for cumbersome
arithmetic, and spots values that appear to be out of line with others
in longitudinal assessment. It also allows all data to be accumulated
sequentially at a single place in the medical record.
described for limb-length inequality evaluation. One is based on data
from Dutch children between 1979 and 1994. It suggests that children
today have longer bones than the children in the study of Green and
Anderson from the 1940s and 1950s (9). The
technique uses principles similar to those of the straight-line graph.
In the second technique, a graphic display is made based on plotting
limb-length discrepancy versus chronologic age. This is a graphic
variation of the arithmetic technique (21).
limb-length discrepancy, studies vary with respect to interpretation of
success. Theoretically, the Green and Anderson method and the
straight-line graph methods should give the same prediction because
they are derived from the same growth data. General success has been
reported with both of these methods (19,48,61,69,78). Another recent review reported disappointing results with all three commonly used methods (50). Continued study and refinement are needed.
discrepancy is based on a thorough assessment of the patient’s
problems, both clinically and radiographically. Each patient may have
differing goals, reflecting a unique combination of associated
problems. In general, it is best to consider correcting coexisting
conditions before addressing the limb-length difference. Correcting a
spinal deformity affects pelvic obliquity. Correcting angular deformity
in the lower limb, whether it is at the level of a malunion or a
contracture at a joint, usually has the effect of lengthening that limb.
same length, but this may not always be the best goal. In the patient
with polio residuals, it is usually desirable to leave a weak extremity
slightly short, which allows it to function better in the swing phase
of gait. In the neuromuscularly normal child, it is best to plan for a
limb-length difference of between 5 mm and 1 cm at maturity when
considering epiphysiodesis. This allows for slight changes in growth
patterns after the epiphysiodesis and inaccuracies in the preoperative
assessment while not compromising adult height any more than necessary.
level in the limb at which to correct a discrepancy. The ideal
situation would be to lengthen the short bone or shorten the long bone
to a normal length. A general goal is to keep the legs symmetric so
that knee height is equal. However, in some cases, a well-timed
epiphysiodesis at one level (for instance, the distal femur) will
eliminate the need for a later procedure involving two growth plates
(distal femur and proximal tibia), even though it may leave the knee
heights at slightly different levels. During lengthening procedures,
this may be of even more concern, because differences made up are often
greater than with epiphysiodeses. If lengthening is proceeding well, it
may be more desirable to continue lengthening the segment past the
predicted length at maturity of that segment on the opposite side so as
to avoid the necessity of another segment lengthening as well.
Asymmetry of knee height is generally of little functional significance
but is of some cosmetic concern.
assessment of limb-length discrepancy has focused on the magnitude of
discrepancy at maturity. This is because the predicted amount of
difference at maturity helps determine the exact amount to correct and
the treatment group likely to be best for equalization. These treatment
groups with their suggested approaches, given a normal height range,
are as follows:
-
Difference of 0 to 2 cm: no treatment
-
Difference of 2 to 6 cm: shoe lift, epiphysiodesis, shortening
-
Difference of 4 to 15 cm: lengthening procedure
-
Difference of more than 15 cm: prosthetic fitting
do not have functional significance for the majority of adults of
normal stature, and therefore do not need treatment (31,72). For those patients who feel unbalanced, a shoe lift can be tried.
generally the first choice for treatment. For greater levels of
discrepancy, shortening procedures are usually not considered because
of disproportionate appearance in the shortened segment and loss of
stature. Also, if the limb is shortened acutely, the normal-sized
muscle-tendon units also have difficulty adapting to the shortened
bone, and consequently they become weaker. Correction of a difference
of greater than 6 cm with epiphysiodesis may be considered when the
long limb is clearly the abnormal side, because loss of stature and
disproportionate appearance are not a concern.
preference may be taken into consideration as the complications and
long-term goals of lengthening versus shortening are weighed. For
discrepancies greater than 6 cm, lengthening becomes the preferred
treatment option. The total length possible from a lengthening
procedure is variable. Generally the maximum length attainable at a
single lengthening is 20% of the bone’s length. Thus, if both the femur
and tibia are lengthened (usually done in a staged manner), this may
total more than 15 cm length gained. A complete assessment of patient
needs and psychosocial situation are crucial before beginning any
lengthening procedure, but the entire lengthening team must pay
particularly close attention to these factors for the longer
lengthenings. Consideration can be given to staged lengthenings of the
same bones, spaced apart by several years for joint and soft-tissue
recovery. An epiphysiodesis may also be used in combination with an
opposite-side lengthening procedure as a method of limiting the amount
of length required.
length, prosthetic fitting is the usual choice of treatment. Often,
this is combined with an amputation, fusion of a joint, or
rotationplasty for more functional prosthetic wear. Common clinical
situations include the severe end of the spectrum of fibular hemimelia
and proximal focal femoral deficiency. In many cases, discussion with
the family centers on how quickly the child can return to normal
function. The prosthetic option often allows a relatively fast return
to a high functional level. If a lengthening device is used, much more
time is required to attain the same functional level as that using a
prosthetic device.
acceptable method of treatment, particularly when the patient will not
consider or is not an appropriate candidate for surgery. A lift becomes
more unwieldy and thus a less viable alternative as more height is
added. The weight of the lift and ankle instability are the chief
problems with larger lifts. In addition, patients find them
cosmetically unappealing. Lifts can be used as a trial in the
preoperative period to determine the most comfortable or functional
amount of lengthening or shortening (Fig. 170.17).
long limb to allow the short side to catch up. It is simple, effective,
and predictable; is done in one stage; and has a low complication rate (25,28,55,78). It is the usual procedure of choice when predicted discrepancy at maturity is 2 to 6 cm (80).
When the procedure is completed, the growth at that physis is assumed
to be completely stopped. Loss of percentage contribution to limb
length will be 38% for the distal femur, 27% for the proximal tibia,
and 65% for the two combined. The distal tibia contributes 18% of leg
length and occasionally is also considered for closure. The exact
amount of shortening desired can be achieved only by completing the
epiphysiodesis at exactly the correct time. Usually, this choice of
timing comes down to three different options that correspond to the
surgical site: femur only, tibia only, or both femur and tibia. Because
proper timing is so important, close preoperative follow-up of patients
is necessary for prediction of growth. In one review of 67
epiphysiodeses, more than half were deemed failures due solely to
improper interpretation of growth data (10).
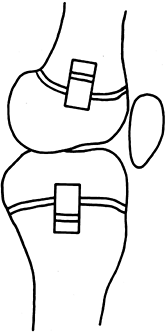
goal of all of them is production of symmetric physeal closure to
prevent future growth. The traditional Phemister technique uses removal
of a rectangular block of bone medially and laterally at the level of
the physis that is then replaced in a 18° rotated position (68) (Fig. 170.18). The rectangular window is also used to remove remaining bits of physis with a curet. White and Stubbins (90)
described removal of a square block at the level of the lateral physis,
which is then rotated 90° and replaced. Epiphysiodesis by stapling was
originally thought to be a good technique to stop physeal growth
temporarily, but problems developed
with asymmetric and complete physeal closure; thus it should be considered a permanent form of growth arrest (12).
Stapling has fallen out of favor but may be appropriate in less
developed areas of the world without routine access to fluoroscopy (73). Screw epiphysiodesis at the knee has also been described (56).
 |
|
Figure 170.18.
The Phemister technique of epiphysiodesis. An open exposure is done both medially and laterally. The rectangular blocks of bone are replaced in a reversed position to create a physeal bar and thus stop growth. (From Moseley CF. Leg-Length Discrepancy. In: Morrissy RT, Weinstein SL. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia: J.B. Lippincott, 1996:878.) |
-
Make longitudinal incisions medially and
laterally. Use separate incisions for both the femur and tibia as
necessary. If the tibia has been chosen, make an incision
posterolaterally as well for the fibula. Incisions can be limited to
approximately 1 cm in length or may be made longer if a rotated block
is to be used. -
Under image control use a 2 mm wide curet
to locate the medial and lateral borders of the physis. Then bore the
curet into the physis both medially and laterally, using a turning
motion with the curet. Sweeping from anteriorly to posteriorly with the
curet scrambles the physeal cartilage. -
The lateral side of the femur and tibia
can be completed through lateral incisions, and the medial side can be
completed through the medial incisions. The curet tip can be crossed to
the opposite side of the bone to allow more surface area to be reached.
Close 50% to 75% of the area of the growth plate using this method. The
remaining amount ensures that strength remains for ambulation without
immobilization. -
Complete the approach to the fibula in
the same manner, but with a wide enough exposure to allow direct
visualization of the edge of the physis. This extra exposure allows the
common peroneal nerve to be protected. -
The technique can be modified slightly in
the femur and tibia by using a power drill to complete the physeal
closure. A drill bit or straight Steinmann pin with a slightly bent tip
damages the growth plate enough to cause closure.
until the wound is healed. Allow the patient to have full range of
motion about the knee postoperatively and to bear weight as tolerated
with the aid of crutches initially. A knee immobilizer may be added for
2 to 3 weeks for pain relief. Full activities can usually be resumed in
6 to 8 weeks. Bony fusion across the physis occurs within 8 weeks.
limb-length discrepancies. However, it is compensatory in that a normal
leg is made abnormal and usually involves decreasing the patient’s
stature. For these reasons, other procedures are also considered.
with the same amounts of discrepancy as those for epiphysiodesis but
who are too old for full correction with physeal closure. In the
patient who has matured, it has a distinct advantage in that the exact
amount of discrepancy is known and no future growth predictions are
necessary.
shortening. The amount of shortening tolerable in the femur is
approximately 5 cm. Greater shortening results in ineffective recovery
of muscle-tendon units. The tibia may also be shortened but to a lesser
degree (14). Maximum shortening in the tibia
should be 3 cm because of shorter muscle-tendon unit lengths. Also,
tibial shortening by intramedullary technique is less feasible because
the bone is subcutaneous. Thus, the femur is strongly preferred.
osteotomies with interfragmentary screws for fixation, but better
implants have made these procedures obsolete. Current techniques
include open shortening with plate fixation or proximal femoral
shortening with blade plate fixation. The plating technique offers the
advantage of ease of fixation but requires hardware removal and may
result in scarring and stiffness of the quadriceps mechanism. Blade
plate fixation offers the advantage of being proximal to most of the
quadriceps origins but has the disadvantage of a more involved
operation.
for more details. The intramedullary saw is used to make two transverse
cuts in the femur. The segment of bone is then split vertically and
displaced to the sides, and the femur is then shortened over an
intramedullary femoral nail and locked proximally and distally. The
technique is demanding technically and requires experience with closed
intramedullary nailing techniques. Malrotation can be a problem; assess
this before awakening the patient. In children, the nail is removed
after complete healing has occurred. The procedure is cosmetic and
allows secure intramedullary fixation with its inherent healing
capabilities. Implant removal is less involved than plating techniques.
However, this procedure causes temporary quadriceps weakness similar to
that of femoral plating. Complications in the young patient have been
reported, including intraoperative or postoperative fat embolus
syndrome; one center reported that 4 out of 100 patients had this
complication (53).
extremity have been tried, including electrical stimulation,
sympathectomy, surgical construction of arteriovenous fistulae,
placement of foreign bodies next to the physis, and packing bone
beneath the periosteum near the physis. None of these techniques have
produced reproducible or clinically significant results. At present,
growth stimulation through the physis is not a realistic option.
most desirable approach because it allows correction of the abnormal
extremity to a normal length while not changing the normal limb.
However, lengthening is generally reserved for those patients with the
most severe deformities. This is because lengthening techniques are
associated with multiple complications and a prolonged treatment time.
has a projected discrepancy of between 4 and 20 cm. Relatively stable
joints above and below the level to be lengthened are a prerequisite.
Rotational or angular malalignment usually decreases the total length
attainable through lengthening procedures. The patient should be
emotionally mature. The youngest child we generally consider for a
lengthening is 8 to 9 years of age so that the patient can cooperate
with physical therapy. Occasionally, a younger child is considered for
lengthening when two different stages of lengthening are required. A
decision is made preoperatively for a target goal of length.
described by Ilizarov, has focused interest on the biology of
lengthening. Lengthening success has been clearly related to the
emphasis on the exact rate of small incremental lengthening of bone.
Others have modified the technique of using only thin wires by adding
thicker half pins for stability (16). In
addition, lengthening with the uniplane frame over an intramedullary
nail, which allows significantly reduced external fixator time, is
gaining popularity (65). The uniplane frame
alone also has a place in pure length correction when angular
correction at the same time is not needed. In all of these techniques,
the rate of lengthening should be the same whichever external frame is
used because the recent successes have been based on a biology that is
highly dependent on technique.
the intramedullary area as multipotential cells differentiate into
osteoblasts. Their bone formation resembles intramembranous growth
because no cartilage matrix is laid down. Cells appear to lay down in a
longitudinal direction of the retreating bone end (40).
Patients are allowed to bear weight fully immediately postoperatively
and participate vigorously in exercise to prevent joint contractures.
lengthened is when to remove the fixator. The actual length of time
that the fixator is left on will vary because the amount of length
gained and the bone quality laid down differs among patients.
lengthening techniques. Most series have reported more than one major
complication per patient. Pin-track infection or inflammation is almost
universally expected. Joint contractures are a persistent problem as
well, particularly flexion or extension contracture of the knee and
equinus position of the ankle. Joint subluxation or dislocation at the
hip or knee are relatively common complications (41,60). In addition, nonunion, malunion, and device failures have been reported.
One review suggested normal or even accelerated growth after moderate
external fixator frame lengthening, whereas longer amounts of time and
length may actually diminish later growth (70).
of treatment, but it may be the best choice when a large discrepancy or
severe deformity exists. When predicted discrepancy at maturity exceeds
15 to 20 cm, or 20% of the long side, this approach should be
considered. A single operation can be performed during one
hospitalization,
so that multiple procedures and complications can be avoided.
without associated femoral shortening, has a large predicted
discrepancy at maturity as well as progressive valgus in the foot. A
Syme amputation followed by prosthetic fitting results in a functional
below-knee amputation that results in a near-normal gait and activity
level. This procedure is best performed when the child is younger than
1 year old. Waiting until a later age often results in a great
emotional attachment of the family and the patient to saving the foot.
deficiency, Syme amputation with or without a knee fusion may be the
best option. This is followed with fitting for an above-knee
prosthesis. Another option is the Van Nes rotationplasty, which
reverses the ankle joint to power a modified below-knee prosthesis (23,46,85).
The Van Nes procedure can be performed on children at any age, but
results are optimal when the procedure is completed at 3 or 4 years of
age. It is particularly helpful to have parents of these patients see
and talk with parents of older patients who have undergone these
procedures.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
A, Weinstein D, Thickman D, Eilert R. Comparison of
Orthoroentgenography and Computed Tomography in the Measurement of
Limb-Length Discrepancy. J Bone Joint Surg 1992;74-A:897.
M, Green W. Lengths of the Femur and Tibia: Norms Derived from
Orthoroentgenograms of Children from 5 Years of Age Until Epiphyseal
Closure. Am J Dis Child 1948;75:279.
M, Messner M, Green W. Distribution of Lengths of the Normal Femur and
Tibia in Children from One to Eighteen years of age. J Bone Joint Surg 1964;46A:1197.
A, Lampe HI, Swierstra BA, et al. The Straight Line Graph in Limb
Length Inequality. A New Design Based on 182 Dutch Childern. Acta Orthop Scand 1997;68:366.
J, Fabry G. The Timing of Epiphysiodesis. A Comparative Study Between
the Use of the Method of Anderson and Green and the Moseley Chart. Acta Orthop Belg 1992;58:43.
W, Anderson M. Experiences with Epiphyseal Arrest in Correcting
Discrepancies in Length of the Lower Extremities in Infantile
Paralysis. J Bone Joint Surg 1947;29:659.
W, Pyle S. Radiographic Atlas of the Skeletal Development of the Hand
and Wrist. Stanford, CA: Stanford University Press, 1959.
L. The Munkfors Investigation. A Study of the Frequency and Causes of
the Stiff Neck-Brachialgia and Lumbago-Sciatica Syndromes, as well as
Observations on Certain Signs and Symptoms from the Dorsal Spine and
the Joints of the Extremities in Industrial and Forest Workers. Acta Orthop Scand 1954:16(Suppl).
G, Palienko L, Shreiner A. Bone Marrow Hematopoietic Function and Its
Relationship to Osteogenesis Activity during Reparative Regeneration in
Leg Lengthening in the Dog. Ontogenez 1984;15:146.
JP, Gillespie R, Hall JE, Hubbard S. Van Nes Rotational Osteotomy for
Treatment of Proximal Femoral Focal Deficiency and Congenital Short
Femur. J Bone Joint Surg 1975;57-A:1039.
U, Friberg O, Aalto T, et al. Lower Limb Asymmetry and Patellofemoral
Joint Incongruence in the Etiology of Knee Exertion Injuries in
Athletes. Int J Sports Med 1987;8:214.
HI, Swierstra BA, Diepstraten AF. Timing of Physiodesis in Limb Length
Inequality. The Straight Line Graph Applied in 30 Patients. Acta Orthop Scand 1992;63:672.
HI, Swierstra BA, Diepstraten AF. Measurement of Limb Length
Inequality. Comparison of Clinical Methods with Orthoradiography in 190
Children. Acta Orthop Scand 1996;67:242.
M, Hall J. Transiliac Lengthening of the Lower Extremity. A Modified
Innominate Osteotomy for the Treatment of Postural Imbalance. J Bone Joint Surg 1979;61-A:1182.
SF, Wu KD, Galski T, Feinberg JH. Low Back Pain in College Athletes. A
Prospective Study Correlating Lower Extremity Overuse or Acquired
Ligamentous Laxity with Low Back Pain. Spine 1998;23:828.
D, Herzenberg JE, Paremain G, Bhave A. Femoral Lengthening Over an
Intramedullary Nail. A Matched-Case Comparison with Ilizarov Femoral
Lengthening. J Bone Joint Surg 1997;79-A:1464.
S, Whiffen J, Shapiro F. Leg-Length Discrepancies in Monoarticular and
Pauciarticular Juvenile Rheumatoid Arthritis. J Bone Joint Surg
1981;63-A:209.
A, Alaranta H, Tallroth K, Heliovaara M. Leg-Length Inequality in
People of Working Age. The Association Between Mild Inequality and
Low-Back Pain is Questionable. Spine 1991;16:429.
MM, Hsu LCS, Leong JCY. Leg Length Discrepancy after Femoral Shaft
Fractures in Children: Review after Skeletal Maturity. J Bone Joint Surg 1989;71-B:615.
RW, Bowen JR, Guille JT, Choi IH. Prospective Evaluation of Fifty-three
Consecutive Percutaneous Epiphysiodeses of the Distal Femur and
Proximal Tibia and Fibula. J Pediatr Orthop 1997;11:350.
I, Correll J, Niethard F. Closed Distraction Epiphyseolysis for Leg
Lengthening and Axis Correction of the Leg in Children. Z Orthop 1986;124:743.
T, Hoikka V, Poussa M, Osterman K. Leg-Length Inequality and Low-Back
Pain after Perthes’ Disease: A 28–47-year Follow-up of 96 Patients. J Spinal Disord 1992;5:443.
