CHRONIC AND ACUTE INJURIES OF THE ACROMIO-CLAVICULAR AND STERNO-CLAVICULAR JOINTS
IV – SPORTS MEDICINE > Shoulder > CHAPTER 78 – CHRONIC AND ACUTE
INJURIES OF THE ACROMIO-CLAVICULAR AND STERNO-CLAVICULAR JOINTS
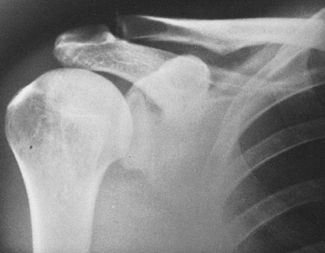
located between the lateral end of the clavicle and the medial margin
of the acromion process of the scapula (Fig. 78.1). DePalma (56)
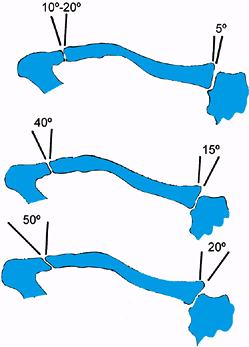
showed marked variability in the plane of the joint. Viewed from the
front, the inclination of the joint may be almost vertical, or it may
be inclined from downward medially, with the clavicle overriding the
acromion by an angle as large as 50° (Fig. 78.2) (23,181).
 |
|
Figure 78.1. Anteroposterior view of the normal shoulder. Note the AC joint, the coracoid process, and the CC interspace.
|
 |
|
Figure 78.2. Variations of the inclination of the AC and the SC joints. (Redrawn from DePalma AF. Surgery of the Shoulder. Philadelphia: JB Lippincott.)
|
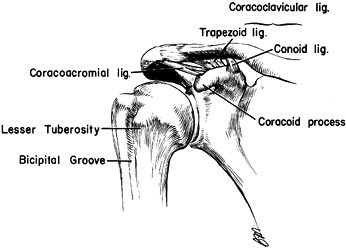
extracapsular [coracoclavicular (CC)] ligaments. The importance of the
muscles that cross the joint (deltoid and trapezius) in providing the
dynamic stability of the AC articulation cannot be overemphasized. A
portion of the anterior deltoid provides dynamic suspensory support of
the
arm
from the clavicle. The upper portion of the trapezius also contributes
support. It is important to repair the deltoid or trapezius fascia in
management of AC dislocation (110).
The fibers of the superior AC ligament (the strongest of the capsular
ligaments) blend with those of the deltoid and trapezius muscles, which
are attached to superior aspect of the clavicle and the acromion
process, adding to the stability of the joint.
 |
|
Figure 78.3. Normal anatomy of the AC joint.
|
from the outer, inferior surface of the clavicular to the base of the
coracoid process of the scapula (Fig. 78.3). It has two components: the conoid and the trapezoid ligaments.
upper extremity and helps to couple glenohumeral abduction and flexion
to scapular rotation on the thorax. Full overhead elevation cannot be
accomplished without combined and synchronous glenohumeral and
scapulothoracic motion (44,89,96) The clavicle rotates about its longitudinal axis through an arc of 40° to 50° during full abduction (89). Bearn (16)
stressed the importance of the sternoclavicular (SC) ligaments in
supporting the proximal end of the clavicle by preventing downward
displacement of the distal end of the clavicle. Urist (181) showed that complete dislocation of the AC joint can occur horizontally without rupture of the CC ligament.
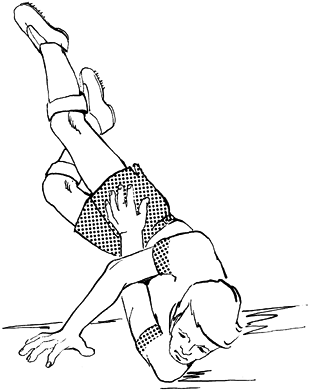
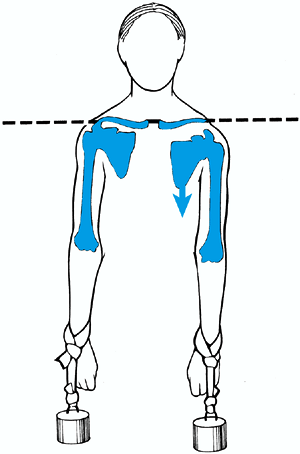
the point of the shoulder with the arm at the side in an adducted
position (Fig. 78.4) drives the acromion downward and medially and is the most common cause of AC injury (16).
If no fracture occurs, the force first sprains the AC ligaments, then
tears the AC ligaments and stresses the CC ligaments, and finally tears
the deltoid and trapezius muscle attachments from the clavicle and
ruptures the CC ligament, resulting in drooping of the shoulder (Fig. 78.5).
The mechanism for inferior dislocation of the clavicle under the
coracoid is thought to be a very severe direct force onto the superior
surface of the distal clavicle, along
with abduction of the arm and retraction of the scapula (122,142).
 |
|
Figure 78.4. The most common mechanism of injury is a direct force that occurs from a fall on the point of the shoulder.
|
 |
|
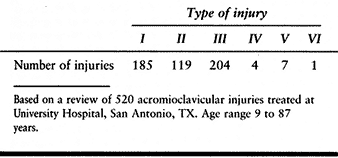
Figure 78.5.
Schematic drawing of a patient with a complete grade III AC dislocation. The major deformity seen in this injury is a downward displacement of the scapula and upper extremity—not an upward elevation of the clavicle. |
hand, which transmits a force up the arm, through the humeral head, and
into the acromion process, producing mild, moderate, or severe AC joint
injury. Forces can also be indirectly applied to the AC joint by a pull
through the upper extremity, which can forcibly draw the shoulder
downward and anteriorly (107).
 |
|
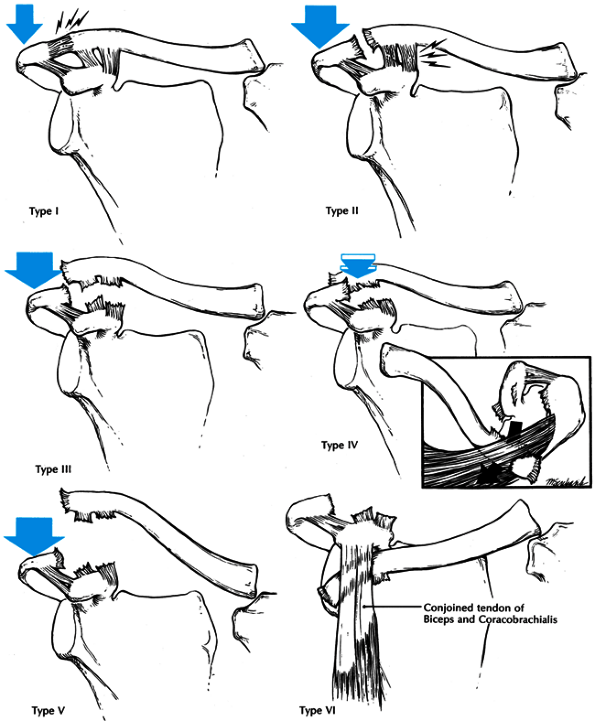
Figure 78.6. Schematic drawings of the classification of ligamentous injuries to the AC joint. Top left: In the type I injury a mild force applied to the point of the shoulder does not disrupt either the AC of the CC ligaments. Top right:
A moderate to heavy force applied to the point of the shoulder will disrupt the AC ligaments, but the CC ligaments remain intact. Center left: When a severe force is applied to the point of the shoulder both the AC and the CC ligaments are disrupted. Center right: In a type IV injury not only are the ligaments disrupted but the distal end of the clavicle is also displaced posteriorly into or through the trapezius muscle. Bottom left: A violent force applied to the point of the shoulder not only ruptures the AC and CC ligaments but also disrupts the muscle attachments and creates a major separation between the clavicle and the acromion. Bottom right: This is an inferior dislocation of the distal clavicle in which the clavicle is inferior to the coracoid process and posterior to the biceps and corabrachialis tendons. The AC and CC ligaments are also disrupted. |
 |
|
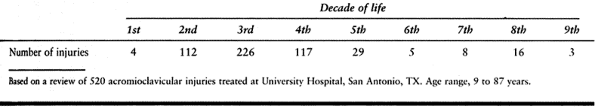
Table 78.1. Frequency of AC Injuries by Patient Age
|
 |
|
Table 78.2. Frequency of AC Injuries by Type
|
minor strain of the fibers of the AC ligaments. The ligaments remain
intact, and the AC joint remains stable.
enough to rupture the ligaments of the AC joint. The distal end of the
clavicle is unstable in the horizontal plane (i.e., anteroposterior),
but vertical (i.e., superoinferior) stability is preserved by virtue of
the intact CC ligament.
shoulder, “complete” AC dislocation occurs, and the AC and CC ligaments
are disrupted (see Fig. 78.6).
surfaces of the distal clavicle and acromion is accompanied by complete
disruption of the AC and CC ligaments. Children and adolescents
occasionally sustain Salter-Harris type I or II injuries in which the
epiphysis and intact AC joint remain in their anatomic locations while
the distal clavicular metaphysis is displaced superiorly through a
dorsal longitudinal rent in the periosteal sleeve (21,50,61,64,83,93).
The importance of recognizing this injury is that the intact CC
ligaments remain attached to the periosteal sleeve. Nonoperative
management most often results in healing of the clavicular fracture and
reestablishment of the integrity of the CC ligaments. A second uncommon
variation of the type III injury involves complete separation of the AC
joint combined with a fracture of the coracoid process (10,18,42,78,102,118,129,184,186).
the type III injury in which the distal clavicle is stripped of all its
soft-tissue attachments and lies subcutaneously near the base of the
neck.
sitting position, as the weight of the arm makes deformity more
apparent.
tenderness and swelling over the AC joint without palpable displacement
of the joint, only minimal pain with arm movements, and no tenderness
in the CC interspace.
moderate to severe pain is present, the outer end of the clavicle may
be noted to be slightly superior to the acromion, motion of the
shoulder produces pain in the AC joint, and the outer end of the
clavicle may appear to be unstable and free-floating.
joint, the arm is held adducted close to the body and supported in an
elevated position, the shoulder is depressed, the clavicle may be
prominent enough to tent the skin (Fig. 78.7),
and moderate pain is the rule. Any motion of the arm, particularly
abduction, increases the pain. Look for an associated clavicular shaft
fracture (103,190).
 |
|
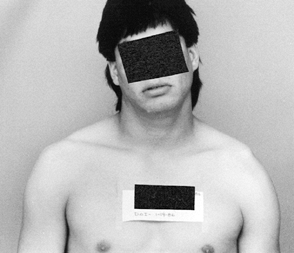
Figure 78.7.
This patient has a complete type III dislocation of the left AC joint. The left shoulder is drooping and there is prominence of the left distal clavicle. (From Rockwood CA, Young DC. Disorders of the AC Joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders.) |
III in which the distal end of the clavicle appears to be grossly
superiorly displaced toward the base of the neck. The patient has more
pain than with type III injury, secondary to extensive muscle and
soft-tissue disruption. The patient may have symptoms of traction on
the brachial plexus.
of the normal shoulder. With palpation, the acromion is prominent, and
there is a definite inferior stepdown to the superior surface of the
coracoid process. There may be associated fractures of the clavicle and
upper ribs or injury to the upper roots of the brachial plexus (67,122,142).
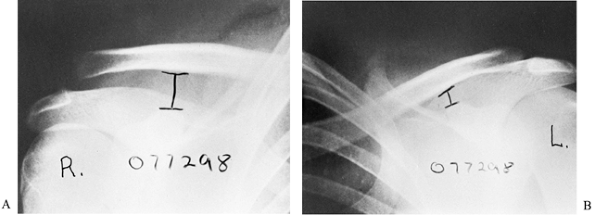
standing or sitting, with the back against the x-ray cassette and the
arms hanging unsupported at the side, imaging both shoulders
simultaneously on one large (14 × 17-in.) cassette.
shoulders, including the lateral third of the clavicle if possible.
This view will reveal any posterior displacement of the clavicle as
well as any small fractures that may have been missed on the
anteroposterior view.
anteroposterior radiograph with 10- to 15-lb weights suspended from
each arm with wrist straps. The weights should be hanging from the
wrists rather than held by the patient to encourage complete muscle
relaxation (Fig. 78.5).
apparent on routine radiographs because the patient has supported the
injured shoulder with the opposite arm and reduced the AC joint. In
addition, some type II injuries can be difficult to differentiate from
type III injuries.
normal, except for mild soft-tissue swelling, as compared with the
uninjured shoulder. There is no widening, no separation, and no
deformity. In a type II injury, the lateral end of the clavicle may be
slightly elevated, and the AC joint may appear to be widened. Stress
films reveal that the CC space is the same as that of the normal
shoulder.
with the lateral end of the clavicle displaced completely above the
superior border of the acromion. The CC interspace is significantly
greater than that in the normal shoulder (Fig. 78.8).
 |
|
Figure 78.8.
Radiograph appearance of a grade III injury to the right shoulder. Stress radiograph films were made to compare the right shoulder with the left. Not only is the right AC joint displaced compared with the left, but, more significantly, notice the great increase in CC interspace on the injured right shoulder compared with the normal left shoulder. |
fracture of the coracoid process rather than by disruption of the CC
ligaments. Although the fracture of the coracoid process is difficult
to visualize on routine radiographs, its presence should be suspected
because of the presence of complete AC separation and a normal CC
distance as compared with the uninjured shoulder.
posterior displacement of the distal clavicle, as seen on the axillary
lateral radiograph (Fig. 78.9).
 |
|
Figure 78.9. Axillary view of type IV posterior dislocation with the distal clavicle and acromion outlined.
|
is a marked increase (i.e., two to three times normal) in the CC
interspace. The clavicle appears to be grossly displaced superiorly
away from the acromion.
clavicle can be subacromial or subcoracoid. In the subacromial type,
radiographs reveal a decreased CC distance (i.e., less than the normal
side), and the distal clavicle is in a subacromial location. The
subcoracoid dislocation is characterized by a reversed CC distance,
with the clavicle displaced inferior to the coracoid process.
discomfort and protect the shoulder from further injury until there is
a painless full range of motion. Usually, the symptoms subside after 7
to 10 days of rest.
until the symptoms subside, followed by a gradual rehabilitation
program. Advise the patient to avoid heavy lifting or contact sports
for 8 to 12 weeks to allow complete ligament healing.
Pain can be caused by posttraumatic osteolysis of the clavicle, torn
capsular ligaments trapped within the joint, loose pieces of articular
cartilage, or a detached intra-articular meniscus that becomes
displaced in and out of the joint like a torn meniscus in the knee. An
AC joint arthroplasty may be required. If the articular surface of the
clavicle is degenerative, then perform an excision of the distal 2 cm
of the clavicle in addition to joint debridement and meniscectomy.
in a randomized, prospective study, showed there was no difference
between the operatively and nonoperatively treated patients except in
those with severe separations (2 cm or greater), where operative
fixation provided better results. No difference in strength and
endurance has been found in those treated nonoperatively, comparing the
injured with the noninjured side (69,116,162,188).
dissatisfaction with the results of surgical repairs, and reports of
good functional outcomes have led many authors to favor “skillful
neglect” over operative treatment (20,58,69,84,88,160,164).
Ninety percent to 100% satisfactory results with 5- to 7-year follow-up
in patients with type III AC dislocations can be expected. The types of
nonoperative treatment available are described in Chapter 10.
fixation, CC ligament repair, distal clavicle excision, and dynamic
muscle transfers.
-
Place the patient on a radiolucent table under general anesthesia. Prep and drape the shoulder with the upper extremity free.
-
If closed technique is to be used, insert a 1/8-in.
or larger smooth Steinmann pin antegrade from the lateral edge of the
acromion to the joint. Then reduce the joint closed and, under
fluoroscopic guidance, insert the pin across the joint into the
clavicle. -
Some authors prefer to open the joint for
debridement and reduction. Use a “saber cut” incision 5 cm or so in
length directly over the AC joint. Insert the pins retrograde from the
joint into the acromion and then into the clavicle after reduction of
the joint. Always bend the portion of the pin that protrudes through
the lateral acromion process to lessen the possibility of medial
migration (Fig. 78.10).![]() Figure 78.10.
Figure 78.10.
Open reduction of the AC joint and stabilization of the joint with two
pins effectively reduced the fractured coracoid. Note that the distal
ends of the pins have been bent to prevent medial migration. -
Repair the ligaments as close to anatomic
as possible and then do a layered closure of the wound with a
subcuticular skin closure.
excessive abduction of the shoulder to prevent breakage or migration of
the pins. Rowe (155) recommends that abduction
motion be limited to no more than 40°. Remove the pins after 6 to 8
weeks and begin range-of-motion and strengthening exercises.
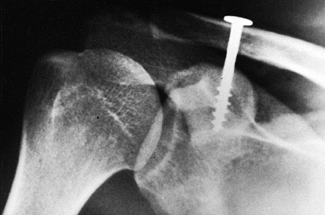
in 1941. The screw was placed percutaneously without repair of the CC
ligaments or exploration of the AC joint. Good results using various
modifications of Bosworth’s original technique have been reported (91,96,112; Fig. 78.11).
 |
|
Figure 78.11.
Postoperative anteroposterior radiograph of the shoulder with Bosworth screw in place. Note that the AC joint has been reduced and the coarse lag threads of the screw are well seated into the coracoid process. |
excision of the distal clavicle, which is usually done for an old,
symptomatic type II injury. In symptomatic type III injuries, in
addition to the excision of the distal clavicle, there must be a
reconstruction of the CC ligaments.
indicated in a symptomatic, chronic, incomplete AC dislocation—and
possibly in an acute injury with severe joint damage—we do not
recommend excision of a normal clavicle for an acute AC dislocation.
distal clavicle in a type IV injury and the gross superior displacement
in the type V, most authors recommend surgical repair (81,117,135,166).
In a type IV injury, the patient is quite symptomatic when the distal
end of the clavicle penetrates the trapezius muscle. In an inactive
patient in whom the clavicle can be manipulated out of the trapezius
muscle, a nonoperative approach is possible. If the clavicle cannot be
manipulated out of the trapezius muscle, however, one of the previously
described surgical procedures is indicated. In a type V injury, the
deformity is so gross that surgical repair is usually indicated.
reported using the extra-articular technique with the Rockwood CC lag
screw, with repair of the ligaments and imbrication of the
deltotrapezius fascia over the top of the clavicle.
 |
|
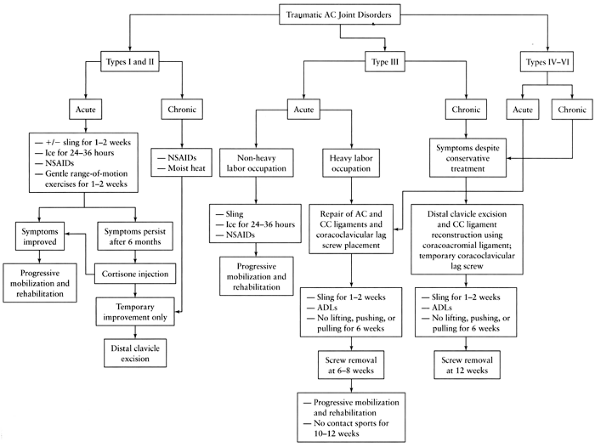
Figure 78.12. University of Texas at San Antonio treatment algorithm for traumatic disorders of the AC joint.
|
first 12 hours, followed by moist heat, and provide a sling to support
the arm. We encourage the patient to rest the shoulder but to maintain
a gentle, normal range of motion. The symptoms usually subside within 7
days. Advise patients to avoid heavy stresses, lifting, and contact
sports until there is a full range of motion and no pain to joint
palpation, which usually takes 2 to 3 weeks.
patient can use the arm for dressing, eating, and necessary everyday
living activities when symptoms permit, usually about the seventh day.
We advise patients to avoid heavy lifting, pushing, or contact sports
for at least 6 weeks.
labor (i.e., pushes a wheelbarrow, swings a sledge hammer, does a lot
of digging), then chronic pain can develop in the AC joint secondary to
traumatic arthritis. If conservative measures fail, then an
arthroplasty may be required.
procedure or put the arm into a sling for a few days and gradually
allow functional use of the shoulder. We do not use braces or
strappings, which tend to irritate or ulcerate the tender skin on top
of the shoulder.
25 years of age who have not yet established their future occupation or
sports, we proceed with surgical repair. An exception is a young
athlete who regularly subjects the shoulder to violent, unprotected
trauma (e.g., in soccer, rugby, and hockey). There is no sense in
repairing an injury only to have it recur when the patient falls on the
point of the shoulder. American football players with a grade III
injury treated nonoperatively can perform well with special shoulder
pads. Throwers can usually return to their sports with a grade III
injury after 4 to 8 weeks. In patients doing heavy labor, however,
operative repair yields a shoulder with more endurance that will stand
up to repetitive stresses and heavy loads.
closed reduction to dislodge the clavicle from the trapezius muscle or
from under the coracoid process. If it is successful, we then apply the
same indications as above for a type III problem. If the reduction
fails, then an operative reduction and repair are necessary. Type IV,
V, and VI injuries require operative repair.
-
Place a 10 × 12-in. x-ray cassette under the patient’s
P.2096P.2097
shoulder, and place the patient in the beach-chair position on the
operating table. A special head rest is used so the top of the
patient’s shoulder is completely free at the top of the corner of the
table. Deviate the head slightly toward the normal shoulder and secure
it to the head rest so there is complete access to the superior aspect
of the shoulder. Place the anesthesiologist and equipment at the
opposite shoulder so the surgeon can stand at the top of the table.
Preparation and draping must provide access from the top of the
shoulder to the base of the neck. -
Make a strap-like incision in Langer’s lines approximately 3 in. long (Fig. 78.13).
Begin 1 in. posterior to the clavicle, then cross the clavicle 1 in.
medial to the AC joint. Extend the incision downward to a point medial
to the tip of the coracoid process. Undermine the incision so the AC
joint, the distal 2 in. of the clavicle, and the anterior deltoid can
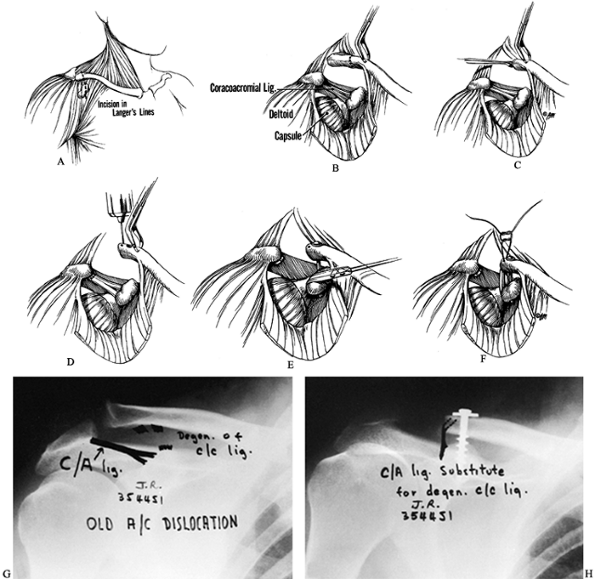
be visualized.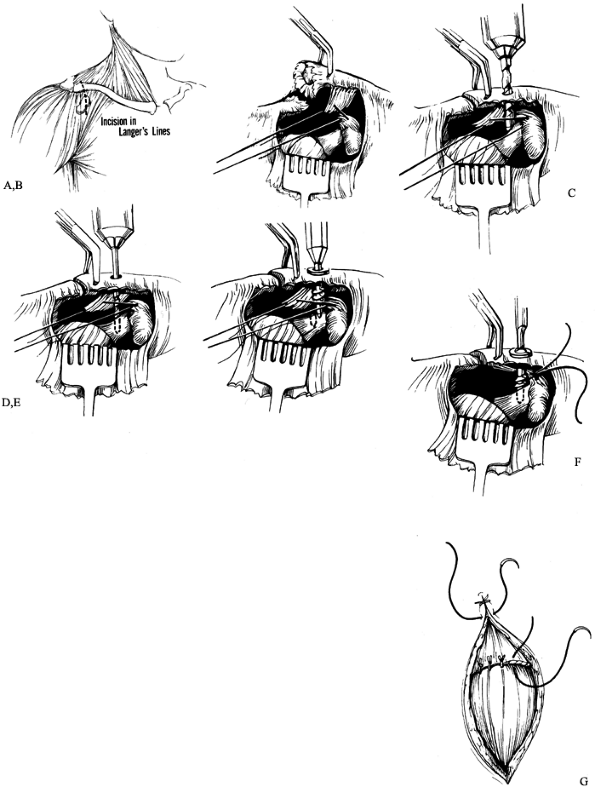 Figure 78.13. The authors’ repair for a complete AC dislocation. A:
Figure 78.13. The authors’ repair for a complete AC dislocation. A:
The skin incision is about 3 in. long and extends from the posterior
edge of the clavicle, 1 in. medial to the AC joint, then down in
Langer’s lines to a point just medial to the tip of the coracoid
process. B: The deltoid secondary to the
injury is usually subperiosteally stripped away from the distal
clavicle. It may have to be surgically detached to aid in
identification and reapproximation to the CC ligaments and the base of
the coracoid process. The distal end of the clavicle can be lifted up
with a towel clip or a bone hook to aid in the placement of the sutures
in the CC ligament. The AC joint is thoroughly debrided of the
meniscus. If the AC ligaments are amenable to repair, they are
preserved and later repaired. C: The distal end of the clavicle is held reduced adjacent to the acromion with a towel clip. A 3/16-in. drill bit is used to make a hole in the clavicle directly above the base of the coracoid. D: Through the 3/16-in. hole in the clavicle, a 9/64-in. drill bit is used to create a hole through both cortices of the base of the coracoid. E:
The specially designed lag screw of appropriate length is then placed
through the clavicle until the smooth shank of the screw is in the
clavicle. The nonthreaded nipple end of the screw is then passed into
the hole of the coracoid, and the screw is tightened home to depress
the clavicle down to the level of the acromion. F:
The stay sutures in the CC ligaments are then tied, and the screw is
tightened another half turn to take any tension off the reapproximated
ligaments. G: The muscle attachments of
the deltoid and trapezius are carefully repaired and, if possible, are
imbricated over the top of the clavicle and the AC joint. Note: In
measuring the length of the screw, it must be remembered to add 6 mm to
the measurement of the depth gauge so that the heavy threads will
purchase both cortices of the coracoid. -
In some instances, the deltoid and
trapezius muscle fascia may have been torn from the distal 2 to 3 in.
of the clavicle. If not, open this interval so the clavicle can be
grasped with a clamp and lifted upward while the deltoid muscle is
retracted distally to visualize the torn ends of the CC ligament and
the base of the coracoid process. If the deltoid has been stripped off
the clavicle with an intact periosteal tube, then split the deltoid
distally 2 in. in line with its fibers, and detach the distal 2 in.
from its insertion into the clavicle. This technique will allow
exposure of the CC ligaments and the base of the coracoid process (Fig. 78.13). -
Grasp the distal end of the clavicle and
lift it upward and debride the joint of the torn intraarticular disc
and any loose tags of the AC ligament. Identify the torn ends of the CC
ligament and tag them with two or three #1 cottony dacron sutures. Do
not tie the sutures at this time. -
Reduce the AC joint anatomically. With
the superior surface of the clavicle exposed and the base of the
coracoid clearly visualized, place a screw vertically through the
clavicle and both cortices of the base of the coracoid. Place a 3/16-in.
drill hole in the clavicle 1 to 1½ in. medial to the distal end of the
clavicle, directly over the base of the coracoid. Next, drill a 9/64-in. hole through the base of the coracoid (Fig. 78.13).
Measure with a depth gauge for the screw length. Then insert Rockwood’s
modification of the Bosworth screw (DePuy Orthopaedics, Warsaw, IN)
through the clavicle into the coracoid (Fig. 78.14).
Be certain that the tip of the screw enters the hole in the center of
the coracoid and doesn’t skid off either side. As the screw is
tightened, the clavicle is gradually reduced down to the level of the
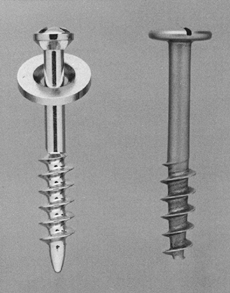
upper border of the acromion.![]() Figure 78.14.
Figure 78.14.
Comparison of the modified CC lag screw (left) with the original
Bosworth screw (right). The large head of the original screw made it
possible to use the self-retaining screwdriver. Furthermore, the
threads extended all the way down to the tip of the screw, making it
difficult for the surgeon to place the screw into the hole in the base
of the coracoid. The modified screw, which has a washer in place of the
large head, can be used with a self-retaining screwdriver. The distal ¼
inch of the screw, which has no threads and is smooth tipped, is used
to seek out the hole in the base of the coracoid. (Courtesy of DePuy
Orthopaedics Co., Warsaw, IN.) -
Next, take a radiograph using the preoperatively positioned cassette under the shoulder to check the position of the screw (Fig. 78.15).
 Figure 78.15.
Figure 78.15.
Postoperative radiograph showing the acromioclavicular joint reduced
and held temporarily in place with a special modified CC lag screw. -
At this point, tie the stay sutures in
the CC ligament and then take another half-turn on the screw, which
takes any tension off the sutures. The primary purpose of the screw is
to hold the clavicle reduced vertically and horizontally to the scapula
and to take tension off the CC ligament repair until the CC ligaments
have healed. -
Repair the deltotrapezius muscle fascia
back to the clavicle. Try double-breasting or imbricating the fascia
over the top of the clavicle.
weeks but allow the patient to use the arm for gentle daily living
activities. After 1 to 2 weeks, discontinue use of the sling and allow
the patient to use the arm for most everyday living activities,
avoiding any lifting, pushing, and pulling for 4 to 6 weeks.
Ordinarily, by 3 weeks, most patients have a functional range of
motion. Remove the screw by 6 to 8 weeks after surgery under local
anesthesia. After screw removal, instruct the patient not to perform
any heavy lifting, pushing, pulling, or contact sports for 10 to 12
weeks from the initial operative repair. Athletes are not permitted to
return to contact sports until 12 weeks postoperatively, and only after
they have recovered full strength of the shoulder with a full range of
motion.
excellent. Most patients recover full range of motion and have no pain
within 2 weeks.
leaving only a small percentage who require debridement or excision of
the outer end of the clavicle because of arthritis in the joint (6,17,48,183).
III, IV, V, and VI injuries with both operative and nonoperative
treatment. Nonoperative treatment usually suffices in a sedentary
office worker; people who do heavy labor do better with surgical
repair. In general, given the proper treatment for a specific patient,
the end results tend to be completely acceptable in more than 90% of
patients.
other injuries about the shoulder, neck, and chest, particularly in
high-velocity injuries. Scapulothoracic dissociation is characterized
by lateral displacement of the scapula, a severe neurovascular injury,
and an injury to bone (either an AC separation, a displaced clavicle
fracture, or an SC disruption). Scapulothoracic dissociations are,
however, usually clinically obvious (see Chapter 15). Injuries associated with AC separations may, however, be less obvious and may include injuries to the chest wall and organs (9), fractures of the clavicle, the acromion process, and the coracoid process, and dislocation of the SC joint (190).
Complications unique to repair of the AC joint can occur (i.e., a
fracture through a drill hole, loss of purchase of the internal
fixation, metal failure, and migration of the fixation device to other
parts of the body).
migrate or break because of motion in the joint. They have been
reported to have migrated to the lung (119), spinal cord (137), neck (108), subclavian artery (163), aorta (73), and liver (150).
bending a hook on the portion of the pin that protrudes from the
acromion process. However, the pins can break, and then the proximal
part of the pin is free to migrate. For that reason, most surgeons
avoid the use of pins across the AC joint.
additional support of internal fixation may lead to failure. This is
particularly true in chronic complete injury to the AC joint when there
is a major separation between the clavicle and the coracoid. Even the
transfer of the acromial attachment of the CA ligament onto or into the
medullary canal of the distal clavicle may fail.
both nonoperative treatment and surgical fixation of the AC joint. If
there are significant findings of degenerative changes or traumatic
injury to the AC joint at the time of initial repair, then excise the
distal clavicle. Use of the CA ligament to reconstruct the CC ligaments
is rarely indicated in the surgical management of acute AC trauma.
injuries, and the patient does not respond to nonoperative treatment,
then excision of the distal clavicle is indicated. Distal clavicle
excision may be performed as an open (76,132) or arthroscopic procedure (19,66,124,165,178).
separates the two articular surfaces of the AC joint begins in the
second decade of life (55) and can progress as
part of the natural aging process, associated with progressive AC joint
space narrowing. Radiographic findings of AC degeneration are seen in
nearly 60% of elderly patients, with tenderness of one or both AC
joints in 42% to 70% of patients (87).
fashion similar to that of other joints, with discomfort localized to
this area in 63% of rheumatoid patients with painful shoulders (144).
tissue, capsular swelling, and subchondral erosion, which is more
marked inferiorly in the region of the coracoid process (148).
Radiographic findings include joint space narrowing, osteopenia of the
acromial process, inferior surface erosions of the distal clavicle, and
osteolysis of the acromial end of the clavicle with tapering (2,3,129,144). These findings are progressive and are found in about 80% of rheumatoid patients with painful shoulders.
follow an acute injury, or it may occur in patients who have repeated
stress on the shoulder. Most cases involve weight lifters who complain
of a dull ache, weakness, and pain with flexion and abduction. A 10°
cephalic tilt radiograph of the AC joint may show osteoporosis,
osteolysis, tapering, or osteophyte formation of the distal clavicle.
Usually, bony changes are unilateral and do not occur in the acromion (Fig. 78.16). Technetium bone scans have also been found to be quite helpful (40).
 |
|
Figure 78.16.
Traumatic osteolysis of the right distal clavicle in a patient who had an injury to the right shoulder and gradually developed increasing pain. Radiograph made 3 months after the injury shows an absorption of the distal clavicle and new bone formation on the dorsal aspect of the clavicle. (From Rockwood CA, Green DP, eds. Fractures, 3rd ed. Philadelphia: JB Lippincott, 1991:1236.) |
joint with an old type II injury is appropriate. We recommend excision
of a minimum of 2 cm of the distal clavicle. If the excision of the
distal clavicle is too small, it eventually may develop a spur that
will impinge against the acromion, producing symptoms and pain just as
before the operation.
(i.e., a chronic type III, IV, V, or VI injury), the CC ligament must
be reconstructed, and distal clavisectomy must be performed.
-
Position, prep, and drape the patients,
using the same surgical approach described for an acute repair of a
type III injury. Excise the distal 2 cm of the clavicle. Remove enough
clavicle so the stump of the clavicle is located just at the lateral
edge of the base of the coracoid (Fig. 78.17).
Then drill the medullary canal of the distal clavicle and widen it with
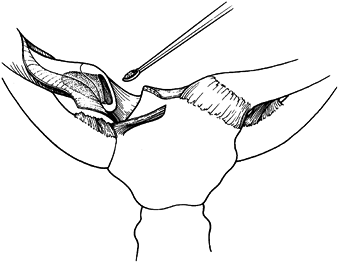
a curet to be able to receive the transferred CA ligament.![]() Figure 78.17. The authors’ method to reconstruct a chronic type III, IV, V, or VI AC dislocation. A: The incision is made in Langer’s lines. B: The distal end of the clavicle is excised. C: The medullary canal is drilled out and curetted to receive the transferred CA ligament. D:
Figure 78.17. The authors’ method to reconstruct a chronic type III, IV, V, or VI AC dislocation. A: The incision is made in Langer’s lines. B: The distal end of the clavicle is excised. C: The medullary canal is drilled out and curetted to receive the transferred CA ligament. D:
Two small drill holes are made through the superior cortex of the
distal clavicle. The CA ligament is carefully detached from the
acromion process. E–H: With the CA
ligament detached from the acromion, a heavy nonabsorbable suture is
woven through the ligament. The ends of the suture are passed out
through the two small drill holes in the distal end of the clavicle.
The CC lag screw is inserted; and when the clavicle is reduced down to
its normal position, the sutures used to pull the ligament snugly up
into the canal are tied. -
Use a knife blade to remove the acromial attachment of the CA ligament from the acromion (Fig. 78.17).
With the clavicle held reduced to just above the base of the coracoid,
determine if the CA ligament is long enough to reach into the
intramedullary canal of the clavicle. This ligament can be further
lengthened by detaching the anterior fasciculus of the CA ligament from
the waist of the coracoid process. Then weave a heavy 1-0,
nonabsorbable suture back and forth through the ligament so that both
ends of the suture exit through the acromial end of the CA ligament. -
Drill two small holes in the superior cortex of the distal stump of the clavicle and into the medullary canal (Fig. 78.17). Now prepare the clavicle and coracoid process for insertion of a CC screw as described above for an acute repair.
-
Before inserting the lag screw, pass the
two ends of the suture in the CA ligament into the medullary canal and
out the two small drill holes in the superior cortex of the clavicle.
Then insert the lag screw through the clavicle and into the coracoid
and tighten it to vertically reduce the clavicle down to just above the
coracoid process. As previously described in treating an acute injury
to the AC joint with the lag screw, be sure that the lag screw is long
enough so that the threads have purchase in both cortices of the
coracoid process. -
Then use the sutures to pull the CA
ligament into the medullary canal. Tie the suture, securing the
ligament into the distal clavicle (Fig. 78.17).
Occasionally we will supplement the fixation with two pieces of
nonabsorbable heavy suture that pass under the coracoid and through
drill holes in the distal clavicle. -
Postoperatively, allow the patient to use
the arm for everyday activities but avoid any heavy lifting, pushing,
or pulling. After 12 weeks, remove the screw under local anesthesia.
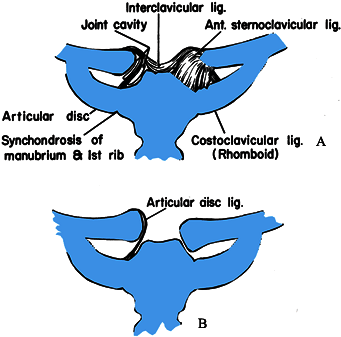
and is the only true articulation between the clavicle and the axial
skeleton (Fig. 78.18). The enlarged bulbous
medial end of the clavicle is concave front to back and convex
vertically; it therefore creates a saddle-type joint with the
clavicular notch of the sternum (72,74).
 |
|
Figure 78.18. A:
Normal anatomy around the SC joint. Note that the articular disc ligament divides the SC joint cavity into two separate spaces and inserts onto the superior and posterior aspects of the medial clavicle. B: The articular disc ligament acts as a checkrein for medial displacement of the proximal clavicle. (Reprinted with permission form Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders.) |
intra-articular disc ligament, the extra-articular costoclavicular
ligament (rhomboid ligament), the capsular ligament, and the
interclavicular ligament. The intra-articular disc ligament is a very
dense, fibrous structure that arises from the synchondral junction of
the first rib to the sternum and passes through the SC joint, which
divides the joint into two separate joint spaces (Fig. 78.18) (72,74).
The upper attachment is on the superior and posterior aspects of the
medial clavicle. The disc acts as a checkrein against medial
displacement of the inner clavicle.
ligament, is short and strong and consists of an anterior and a
posterior fasciculus (16,43,74).
The costoclavicular ligament attaches below to the upper surface of the
first rib and at the adjacent part of the synchondral junction with the
sternum and above the margins of the impression on the inferior surface
of the medial end of the clavicle, sometimes known as the rhomboid
fossa (72,74).
aspects of each clavicle with the capsular ligaments and the upper
sternum (Fig. 78.18). According to Grant (72), this band may be comparable to the wishbone of birds. This ligament helps the capsular ligaments hold up the shoulder.
posterior aspects of the joint and represents thickenings of the joint
capsule (Fig. 78.18). The anterior portion of
the capsular ligament is heavier and stronger than the posterior
portion. It may be the strongest ligament of the SC joint, and it is
the first line of defense against the upward displacement of the inner
clavicle caused by a downward force on the distal end of the shoulder (16).
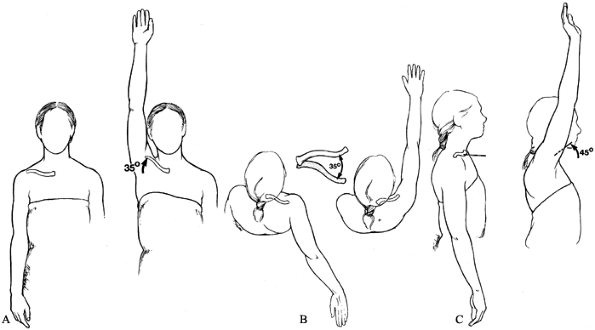
ball-and-socket joint in that the joint has motion in all planes,
including rotation (23,114).
The clavicle, and therefore the SC joint, in normal shoulder motion is
capable of 30° to 35° of upward elevation, 35° of combined forward and
backward movement, and 45° to 50° of rotation around its long axis (Fig. 78.19).
It is most likely the most frequently moved joint of the long bones in
the body because almost any motion of the upper extremity is
transferred proximally to the SC joint.
 |
|
Figure 78.19. Motions of the clavicle and the SC joint. A: With full overhead elevation, the clavicle elevates 35°. B: With adduction and extension, the clavicle displaces anteriorly and posteriorly 35°. C: The clavicle rotates 45° on its long axis as the arm is elevated to the full overhead position.
|
to ossify (fifth intrauterine week), the epiphysis at the medial end of
the clavicle is the last of the long bones in the body to appear and
the last epiphysis to close, ossifying between the 18th and 20th year
and fusing around the 23rd to 25th year (72,74,146). This knowledge of the epiphysis is important, because many SC dislocations are actually fractures through the physeal plate.
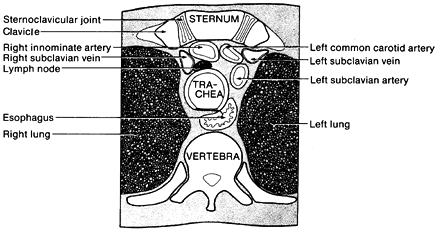
sternohyoid, sternothyroid, and scaleni posterior to the SC joint and
the inner third of the clavicle. This curtain blocks the view of vital
structures, including the innominate artery, innominate vein, vagus
nerve, phrenic nerve, internal jugular vein, trachea, and esophagus (Fig. 78.20). Surgery on the SC joint takes place immediately adjacent to these vital structures.
 |
|
Figure 78.20.
Applied anatomy of the vital structures posterior to the SC joint. Sagittal views in a cross section demonstrate the structures posterior to the SC joint. |
to the anterior margin of the sternum. Posterior SC dislocation is
uncommon. The medial end of the clavicle is displaced posteriorly or
posterosuperiorly with respect to the posterior margin of the sternum.
moderate, or severe. In a mild sprain, all the ligaments are intact,
and the joint is stable. In a moderate sprain, there is subluxation of
the SC joint. The capsular, intra-articular disc, and costoclavicular
ligaments may be partially disrupted. The subluxation may be anterior
or posterior. In a severe sprain, there is complete disruption of the
SC ligaments, and the dislocation may be anterior or posterior.
heal, mild to moderate forces may produce recurrent dislocations; this
is a rare occurrence.
irreducible, or the physician may decide not to reduce certain
dislocations.
or dislocate anteriorly during overhead motion. The problem usually is
not painful (Fig. 78-21).
 |
|
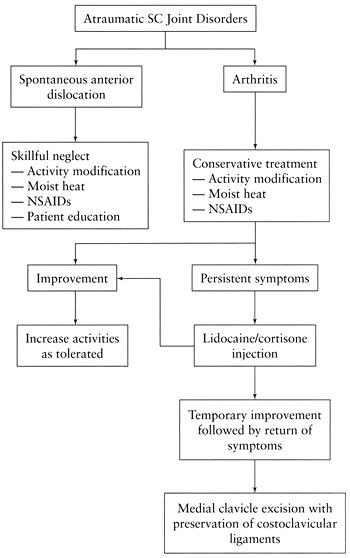
Figure 78.21. University of Texas at San Antonio treatment algorithm for atraumatic SC joint disorders.
|
Routine degenerative arthritis in postmenopausal women has been singled
out as “postmenopausal arthritis,” but it is not a unique disorder (22,29,156).
occurs in women over the age of 40 and may be secondary to chronic
stress on the joint. The joint is swollen and tender, and radionuclide
studies reveal an increased uptake. Routine laboratory results are
within normal limits. X-ray films show sclerosis and slight expansion
of the medial third of the clavicle. The inferior portion of the
sternum end of the clavicle shows sclerotic changes. Some osteophytes
may be present, but the joint space is preserved. The changes of the
medial clavicle are best detected with a CT scan. Most patients do well
with conservative treatment (i.e., anti-inflammatory medications).
Kruger and associates (101) recommend incisional or excisional biopsy in refractory cases.
both sexes between 30 and 50 years of age. The process begins at the
junction of the medial clavicle, the first rib, and the sternum as an
ossification in the ligaments and later involves the bones. In some
cases, the hyperostosis is extensive and forms a solid block of bone of
the sternum, ribs, and clavicle. Patients may have peripheral
arthritis. Subperiosteal bone changes have been noted in other bones (68). The condition has been graded into three stages by Sonozaki (177,178 and 179).
Stage I is mild ossification in the costoclavicular ligaments; stage II
is characterized by an ossific mass between the clavicle and the first
rib;
in
stage III, a bone mass exists between the clavicle, sternum, and first
rib. As might be expected with the fusion of the SC joint, shoulder
motion is severely restricted.
surfaces of skin may be seen. There is no specific laboratory test,
except for an occasional elevation of the serum alkaline phosphatase (68).
subluxation may be associated with acute, subacute, or chronic
bacterial arthritis. Predisposing conditions include intravenous drug
addiction and the presence of the human immunodeficiency virus (HIV) (47,187).
Common predisposing causes to infection in nonaddicts are bacteremia,
infectious invasion from surrounding bone, rheumatoid arthritis,
alcoholism, and chronic debilitating diseases. The CT scan is very
helpful in making an early diagnosis of a septic SC joint (109,130,187).
nine patients with infection of the SC joint secondary to tuberculosis.
The average time from onset of the disease until diagnosis was 1.4
years.
motion of the upper extremity, and because the joint is so small and
poorly matched, one would think it would be the most commonly
dislocated joint in the body. However, the ligamentous supporting
structure is so strong and so designed that it is, in fact, one of the
least commonly dislocated joints in the body. A traumatic dislocation
of the SC joint usually requires tremendous forces, either direct or
indirect.
aspect of the clavicle, the clavicle is pushed posteriorly behind the
sternum and into the mediastinum. A force applied indirectly to the SC
joint from the anterolateral or posterolateral aspects of the shoulder
is the most common mechanism of injury to the SC joint (85,123).
If the shoulder is compressed and rolled forward, an ipsilateral
posterior dislocation results; if the shoulder is compressed and rolled
backward, an ipsilateral anterior dislocation results (Fig. 78.22).
 |
|
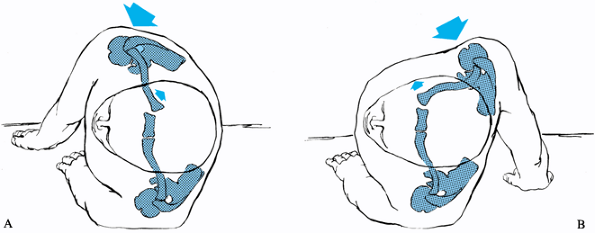
Figure 78.22. Mechanisms that produce anterior or posterior dislocations of the SC joint. A:
If the patient is lying on the ground, and a compression force is applied to the posterolateral aspect of the shoulder, the medial end of the clavicle will be displaced posteriorly. B: When the lateral compression force is directed from the anterior position, the medial ends of the clavicle are dislocated anteriorly. |
The patient complains of a mild to moderate amount of pain,
particularly with movement of the upper extremity. The joint may be
slightly swollen and tender to palpation, but instability is not noted.
joint. The ligaments are either partially disrupted or severely
stretched. Swelling is noted, and pain is marked, particularly with any
movement of the arm. Anterior or posterior subluxation may be obvious
to the examiner when the injured joint is compared with the normal SC
joint.
dislocation may be anterior or posterior. The capsular ligaments and
the intra-articular disc ligament are ruptured. The patient with a SC
dislocation has severe pain that is increased with any movement of the
arm, particularly when the shoulders are pressed together. The patient
usually
supports
the injured arm across the trunk with the normal arm. The affected
shoulder appears to be shortened and thrust forward when compared with
the normal shoulder. The head may be tilted toward the side of the
dislocated joint. Discomfort increases when the patient is placed in
the supine position, at which time it will be noted that the involved
shoulder will not lie back flat on the table.
 |
|
Figure 78.23. A:
With the patient supine, view the clavicles from around the level of the patient’s knees. It is apparent that the right clavicle is dislocated anteriorly. B: Clinically, an anterior dislocation of the right SC joint is evident (arrow). |
than a patient with an anterior dislocation. The anterosuperior
fullness of the chest produced by the clavicle is less prominent. The
medial end of the clavicle is displaced posteriorly. The corner of the
sternum is easily palpated, as compared with the normal SC joint.
Venous congestion may be present in the neck or in the upper extremity (172).
Breathing difficulties, shortness of breath, or a choking sensation may
be noted. Circulation to the ipsilateral arm may be decreased. The
patient may complain of difficulty in swallowing or a tight feeling in
the throat or may be in a state of complete shock or possibly have
pneumothorax.
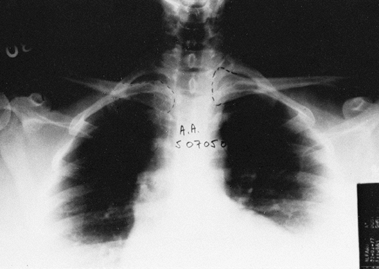
radiographs of the chest or SC joint may suggest that something is
wrong with one of the clavicles, because it appears to be displaced as
compared with the normal side (Fig. 78.24). It
would be ideal to take a view at right angles to the anteroposterior
plane, but because of human anatomy, it is impossible to take a true
90° cephalic-to-caudal lateral view.
 |
|
Figure 78.24.
Anteroposterior radiograph of the SC joints with anterosuperior displacement of the left medial clavicle. The displacement is quite noticeable when the clavicles are outlined. |
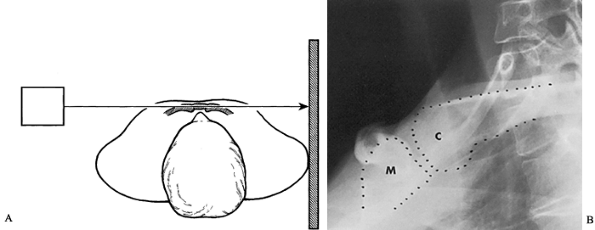
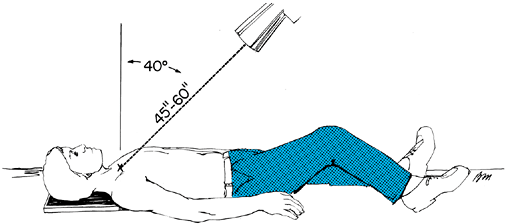
approximately 30 in. from the involved SC joint and direct the central
ray tangential to the joint and parallel to the opposite clavicle (85). Place the cassette against the opposite shoulder and centered on the manubrium (Fig. 78.25).
 |
|
Figure 78.25. A: Positioning of the patient for radiograph evaluation of the SC joint, as described by Heinig. B: Heinig view demonstrating a normal relationship between the medial end of the clavicle (C) and the manubrium (M).
|
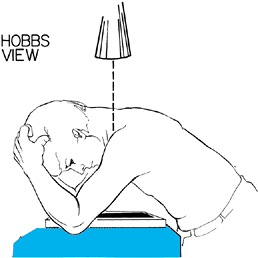
the patient at the x-ray table, high enough to lean forward over the
table. Place the cassette on the table, and position the lower anterior
rib cage against the cassette (Fig. 78.26).
Have the patient lean forward so that the nape of the flexed neck is
almost parallel to the table. The flexed elbows straddle the cassette
and support the head and neck. Place the x-ray source above the nape of
the neck, and direct the central beam through the cervical spine to
project the SC joints onto the cassette.
 |
|
Figure 78.26.
Positioning of the patient for radiograph evaluation of the SC joint, as recommended by Hobbs. (Redrawn from Hobbs DW. The SC Joint: A New Axial Radiographic View. Radiology 1968;90:801.) |
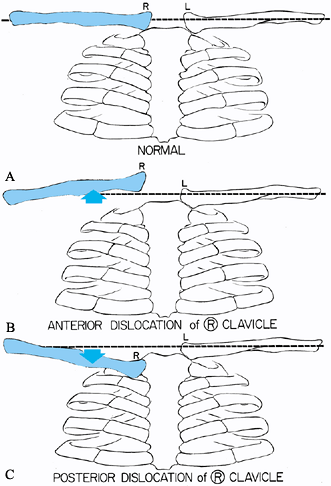
On this view the medial end of the clavicle will be displaced more
anteriorly for an anterior dislocation and posteriorly for a posterior
dislocation compared with the normal side (Fig. 78.28).
 |
|
Figure 78.27.
Positioning of the patient to take the “serendipity” view of the SC joints. The x-ray tube is tilted 40° from the vertical position and aimed directly at the manubrium. The nongrid cassette should be large enough to receive the projected images of the medial halves of both clavicles. In children, the tube distance from the patient should be about 45 in.; in thicker-chested adults, the distance should be 60 in. |
 |
|
Figure 78.28. Interpretation of the cephalic tilt x-ray films of the SC joints. A: In the normal person, both clavicles appear on the same imaginary line drawn horizontally across the film. B:
In a patient with anterior dislocation of the right SC joint, the medial half of the right clavicle is projected above the imaginary line drawn through the level of the normal left clavicle. C: If the patient has a posterior dislocation of the right SC joint, the medial half of the right clavicle is displaced below the imaginary line drawn through the normal left clavicle. |
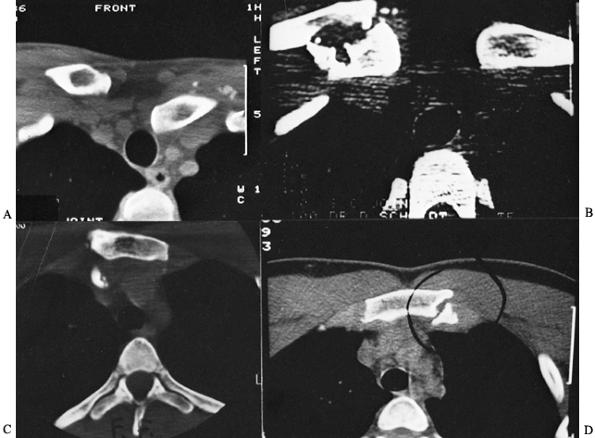
It clearly distinguishes injuries of the joint from fractures of the
medial clavicle and defines minor subluxations of the joint.
 |
|
Figure 78.29. Computed tomography scans of the SC joint demonstrating various types of injuries. A: Posterior dislocation of the left clavicle compressing the great vessels and producing swelling of the left arm. B: Fracture of the medial clavicle that does not involve the articular surface. C: Fragment of bone displaced posteriorly into the great vessel. D: Fracture of the medial clavicle into the SC joint. (Reprinted with permission from Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders.)
|
first 12 to 24 hours, followed by heat. Place the upper extremity in a
sling for 3 to 4 days, then allow the patient gradually to use the arm
in everyday activities.
in the first 48 hours as above. Whether the joint is subluxated
anteriorly or posteriorly, reduce it by drawing the shoulders backward
as if reducing and holding a fracture of the clavicle. Use a
figure-of-eight clavicle strap to hold the reduction. Also apply a
sling and swath to hold up the shoulder and to prevent motion of the
arm. Protect the shoulder for 4 to 6 weeks.
joint may be accomplished with local or general anesthesia or, in stoic
patients, with conscious sedation or without anesthesia. Position the
patient supine on a table, lying on a 3- to 4-in.-thick pad between the
shoulders. In this position, the clavicle may reduce with direct gentle
pressure over the anteriorly displaced clavicle. Sometimes, both
shoulders must be pushed back to the table while an assistant applies
pressure to the anteriorly displaced clavicle. When the pressure is
released, the clavicle usually dislocates again, but occasionally the
clavicle will remain reduced.
reduced, stabilize the shoulders with a soft figure-of-eight dressing,
a commercial clavicle strap harness, or a plaster figure-of-eight cast
(see Chapter 10) combined with a sling.
Continue immobilization for 6 weeks and then have the patient avoid
strenuous activities for another 2 weeks. If the SC joint again
dislocates when the reduction pressure is released, as it usually does,
use a figure-of-eight dressing or a sling for symptomatic treatment.
Although
some authors have recommended operative repair of anterior dislocations
of the SC joint, we believe that the operative complications are too
great, and the end results are too unsatisfactory, to consider an open
reduction.
posterior dislocation of the SC joint; prompt diagnosis and treatment
are important.
CT scan is indicated occasionally, combined with an aortogram, if
vascular injury is suspected. Consultation with a thoracic or vascular
surgeon may be indicated before reduction. Posterior dislocation of the
clavicle into the right pulmonary artery has been reported (189).
a posterior dislocation of the SC joint, although reduction with
conscious sedation is possible. The treatment of choice for posterior
SC dislocation is closed reduction (38,45,46,65,75,85,120,121,127,143,158,173).
-
For the abduction traction technique (57,65,127,152,158),
position the patient supine with the dislocated shoulder near the edge
of the table. Place a 3- to 4-in.-thick sandbag between the shoulders (Fig. 78.30).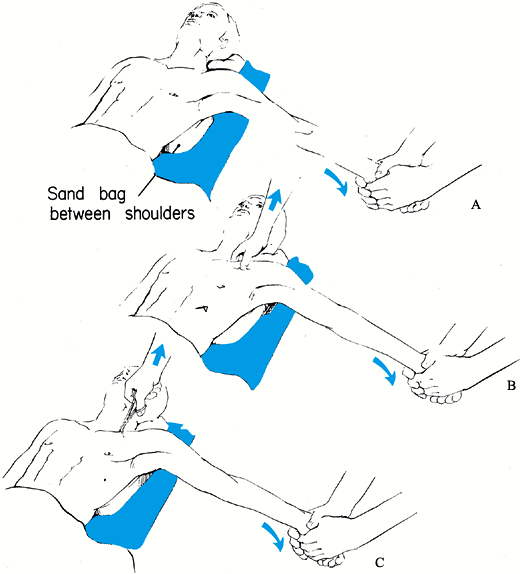 Figure 78.30. Technique for closed reduction of the SC joint. A:
Figure 78.30. Technique for closed reduction of the SC joint. A:
The patient is positioned supine with a sandbag placed between the
shoulders. Traction is then applied to the arm against countertraction
in an abducted and slightly extended position. In anterior
dislocations, direct pressure over the medial end of the clavicle may
reduce the joint. B: In posterior
dislocations, in addition to the traction, it may be necessary to
manipulate the medial end of the clavicle with the fingers to dislodge
the clavicle from behind the manubrium. C:
In stubborn posterior dislocations, it may be necessary to sterilely
prepare the medial end of the clavicle and use a towel clip to grasp
around the medial clavicle to lift it back into position. -
Apply lateral traction to the abducted
arm and gradually extend the shoulder. This procedure may be all that
is necessary to accomplish the reduction. The clavicle usually reduces
with an audible snap or pop, and it is almost always stable. Too much
extension can bind the anterior surface of the dislocated medial
clavicle on the back of the manubrium. Occasionally, it may be
necessary to grasp the medial clavicle with your fingers to dislodge it
from behind the sternum. If this maneuver fails, prep the skin, and use
a sterile towel clip to grasp the medial clavicle to apply lateral and
anterior traction to reduce it. -
In the adduction traction technique,
position the patient supine with a 3- to 4-in. bolster between the
shoulders. Apply traction to the arm in adduction while downward
pressure is exerted on the shoulders. The pressure levers the clavicle
over the first rib into its normal position. This technique may succeed
when the abduction traction technique has failed (34). -
Alternative techniques include placing
the patient supine on the table with three or four folded towels
between the shoulders and applying forward pressure on both shoulders,
or placing a knee between the shoulders of the seated patient and
pulling back on both shoulders (62,85).
Closed reduction usually becomes more difficult after 48 hours, but it
has been successful as late as 4 and 5 days after the injury (34,104).
ligaments, if possible. If anterior ligaments remain intact, then, with
the shoulders held back in a figure-of-eight dressing, the reduction
may be stable. If all the ligaments are disrupted, then stabilization
of the SC joint or resection of the medial 1 to 1.5 in. of the medial
clavicle and stabilization of the remaining clavicle to the first rib
may be necessary.
-
Local ligament repair and pin or wire stabilization (30,32,54,56,62).
-
Circlage wires across the joint (7,60,77,80,95,138,145,173,174).
-
Figure-of-eight carbon fiber (36).
-
Reconstruction of the SC ligaments with tendons or fascia of the sternocleidomastoid, subclavian, or pectoralis major muscles (11,37,72,74,82,115).
-
Loops of fascia lata between the clavicle and sternum or first rib (7,98,113,125,171).
-
Arthodesis (150) is to be avoided.
the clavicle into the mediastinum and late complications involving
underlying vascular structures, so an operative procedure to correct
the situation is nearly always required. These include open reduction
and one of the reconstructions mentioned above or resection of the
medial end of the clavicle (described under Authors’ Preferred Method
of Treatment; 13,14,28,121,125,147).
Because children usually have an epiphyseal slip, remodeling will often
correct the deformity, and surgery is rarely required (154).
will be unstable, we try to reduce the anterior displacement, using the
technique previously described.
patients up to 25 years of age are not dislocations of the SC joint but
type I or II physeal injuries, which heal and remodel without operative
treatment. Patients older than 23 to 25 years with anterior
dislocations of the SC joint do have persistent prominence of the
anterior clavicle. It does not, however, seem to interfere with usual
activities and, in some cases, has not even interfered with heavy
manual labor.
open reduction of the joint and would never recommend transfixing pins across the SC joint.
dislocations. Furthermore, once the joint has been reduced closed, it
is usually stable. For closed reduction, we use the traction–abduction
method previously described.
successful, grasp or push down on the clavicle to dislodge it from
behind the sternum. If unsuccessful, use the sterile towel clip method
described previously. With the towel clip, grasp completely around the
shaft of the clavicle, as the dense cortical bone prevents the purchase
of the towel clip tines into the clavicle. Following the reduction, the
SC joint is normally stable, but we always hold the shoulders back in a
well-padded figure-of-eight clavicle strap for 3 to 4 weeks to allow
for soft-tissue healing.
the residual stability of the medial clavicle. If the costoclavicular
ligaments are intact, the clavicle medial to the ligaments can be
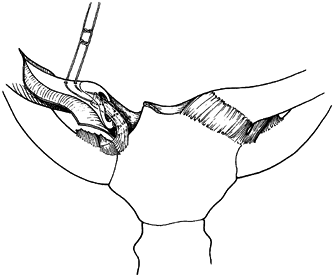
resected and beveled smooth (Fig. 78.31). If
the ligaments are gone, the clavicle must be stabilized to the first
rib. If too much clavicle is resected, or if the clavicle is not
stabilized to the first rib, an increase in symptoms can occur.
 |
|
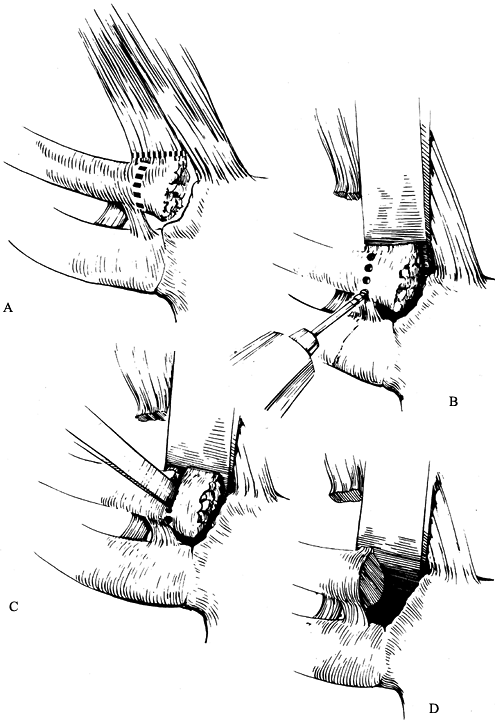
Figure 78.31. Technique for resecting the medial clavicle for degenerative arthritis. A:
Care must be taken to remove only that part of the clavicle medial to the costoclavicular (rhomboid) ligaments. There must be adequate protection for the vital structures that lie posterior to the medial end of the clavicle. B,C: An air drill with a side-cutting bur can be used to perform the osteotomy. D: When the fragment of bone has been removed, the dorsal and anterior borders of the clavicle should be smoothed to give a better cosmetic appearance. |
-
Place the patient supine, with three to
four towels or sandbags between the scapulae. Drape the upper extremity
free so that lateral traction can be applied during the surgery. In
addition, place a folded sheet around the patient’s thorax to be used
for countertraction if traction on the involved extremity is required. -
Make an anterior incision that parallels
the superior border of the medial 3 to 4 in. of the clavicle and then
extends downward over the sternum just medial to the SC joint (Fig. 78.32).
(Having a thoracic surgeon available may be advisable.) Remove
sufficient soft tissues to expose the joint but leave the anterior
capsular ligament intact.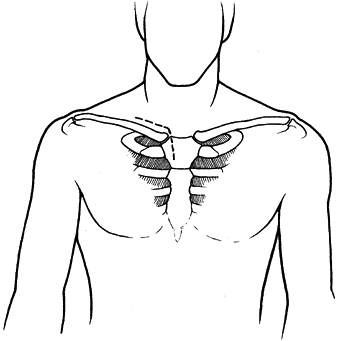 Figure 78.32. Proposed skin incision for open reduction of a posterior SC dislocation.
Figure 78.32. Proposed skin incision for open reduction of a posterior SC dislocation. -
Reduce the clavicle with traction and
countertraction while lifting up anteriorly with a clamp around the
medial clavicle. Along with the traction and countertraction, it may be
necessary to use an elevator to pry the clavicle back into its
articulation with the sternum. When the reduction has been obtained,
and with the shoulders held back, the reduction will be stable because
the anterior capsule has been left intact. -
If the anterior capsule is damaged or is
insufficient to prevent anterior displacement of the medial end of the
clavicle, we recommend excision of the medial 1 to 1.5 in. of the
clavicle and securing the residual clavicle to the first rib with 1-mm
Dacron tape. -
Expose the medial clavicle by careful
subperiosteal dissection. Identify and preserve any remnant of the
capsular or intra-articular disc ligaments, as these structures can be
used to stabilize the medial clavicle. Ordinarily, the intra-articular
disc ligament is a very dense, fibrous structure that arises from the
synchondral junction of the first rib to the sternum and passes through
the SC joint, dividing the joint into two separate spaces. The capsular
ligament covers the anterosuperior and posterior aspects of the joint
and represents thickenings of the joint capsule. This ligament is
primarily attached to the epiphysis of the medial clavicle and is
usually avulsed from this structure with posterior SC dislocations.
Similarly, the intra-articular disc ligament is usually intact where it
arises from the synchondral junction of the first rib and sternum and
avulsed from its attachment site on the medial clavicle. -
If the sternal attachment site of these
structures is intact, weave a nonabsorbable #1 cottony Dacron suture
back and forth through the ligaments so that the ends of the suture
exit through the avulsed free end of the tissue. -
Resect the medial end of the clavicle,
being careful to protect the underlying structures. Do not damage the
costoclavicular (rhomboid) ligament or the vascular structures that are
located posterior to the medial clavicle and SC joint. Protect these
vital structures by passing a curved crego or ribbon retractor around
the posterior aspect of the medial clavicle. Drill holes through both
cortices of the clavicle at the intended site of clavicular osteotomy,
and then use an air drill with a side-cutting burr or an osteotome to
complete the osteotomy. Bevel the anterior and superior corners of the
clavicle with an air burr. -
Next, enlarge the medullary canal of the
medial clavicle with drills and curets to receive the transferred
intra-articular disc ligament (Fig. 78.33). Drill two small holes in the superior cortex of the medial clavicle, approximately 1 cm lateral to the site of resection (Fig. 78.34). Pass the free ends of the suture into the medullary
P.2113
canal of the medial clavicle and out two small drill holes in the superior cortex of the clavicle (Fig. 78.35).
While the clavicle is held in a reduced position, pull the ligament
tightly into the medullary canal of the clavicle and tie the sutures,
thus securing the transferred ligament into the clavicle (Fig. 78.36).
Complete the stabilization procedure by passing several 1-mm cottony
Dacron sutures around the medial end of the remaining clavicle and
securing the periosteal sleeve of the clavicle to the costoclavicular
ligament.![]() Figure 78.33. The medullary canal of the medial clavicle is curretted in preparation for receiving the transferred intra-articular ligament.
Figure 78.33. The medullary canal of the medial clavicle is curretted in preparation for receiving the transferred intra-articular ligament.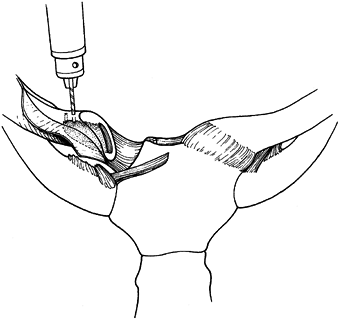 Figure 78.34. Drill holes are placed in the superior cortex of the clavicle, approximately 1 cm lateral to the osteotomy site.
Figure 78.34. Drill holes are placed in the superior cortex of the clavicle, approximately 1 cm lateral to the osteotomy site.![]() Figure 78.35. The free ends of the suture are passed into the medullary canal and out the two holes in the superior cortex.
Figure 78.35. The free ends of the suture are passed into the medullary canal and out the two holes in the superior cortex.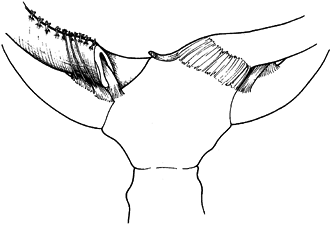 Figure 78.36.
Figure 78.36.
Closure of the periosteal sleeve around the medial clavicle and secure
fixation of these structures to the costoclavicular ligament. -
Postoperatively, keep the patient in a figure-of-eight dressing for 4 to 6 weeks to allow for healing.
and permanent anterior dislocation of the SC joint are not very
symptomatic, have almost a complete range of motion, and can work and
even perform manual labor without many problems. In patients who have
had a previous failed SC surgery, we perform a repeat arthroplasty with
a resection of the medial clavicle, as described above.
arthritis for 6 to 12 months following a dislocation, and if the
symptoms can be completely relieved by injection of local anesthetic
into the SC joint region, we perform an arthroplasty similar to that
described earlier in this chapter.
be associated with the clavicle remaining displaced posteriorly into
the mediastinum, an open reduction is usually indicated. This requires
excision of the medial 1 in. of the clavicle and stabilization to the
first rib as described above.
dislocation of the SC joint. About the only symptoms they have is that
the medial end of the clavicle subluxates or dislocates anteriorly when
they raise their arms overhead (153). This
occurs spontaneously and without any significant trauma. Many of these
patients have generalized ligamentous laxity. This problem might be
considered voluntary or involuntary because it occurs whenever the
patient raises the arms to the overhead position. We explain to
patients that surgery is of little benefit, that they should
discontinue the voluntary aspect of the dislocation, and that in time
either the symptoms will disappear or they will completely forget that
the dislocation is a problem.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
SH, Streitz WL. Acute Acromioclavicular Injuries: A Report of Nineteen
Cases Treated Non-operatively Employing Dynamic Splint Immobilization. Clin Orthop 1974;103:143.
GC, Wallace WA, Stableforth PG, Hutson MA. The Management of Acute
Acromioclavicular Dislocation: A Randomized Prospective Controlled
Trial. J Bone Joint Surg 1989;71B:848.
JH, Driessen AP. Fracture of the Coracoid Process of the Scapula with
Acromioclavicular Separation: Case Report and Review of the Literature.
Acta Orthop Belg 1989;55:499.
TN Jr, Brunet ME, Haddad RJ. Fractured Coracoid Process in
Acromioclavicular Dislocations: Report of 4 Cases and Review of the
Literature. Clin Orthop 1983;175:226.
C, Neugebauer R. Carbon Fiber Replacement of the Ligaments of the
Shoulder Girdle and the Treatment of Lateral Instability of the Ankle
Joint. Clin Orthop 1985;196:112.
R, Riddervold HO. Posterior Dislocation of the Sternoclavicular Joint:
Report on Two Cases, with Emphasis on Radiological Management and Early
Diagnosis. Skel Radiol 1988;17:247.
M, Lapadula G, Pipitone N, et al. Isolated Sternoclavicular Joint
Arthritis in Heroin Addicts and/or HIV Positive Patients: A Report of
Three Cases. Clin Rheumatol 1993;12:422.
RH, Gehweileer JA Jr. Case Report 236: Diagnosis: Neuropathic
Arthropathy of the Sternoclavicular Joint, Secondary to Syringomyelia. Skel Radiol 1983;10:113.
KK. Steingold RA, Richardson RA, et al. The Conservative Treatment of
Acromioclavicular Dislocation: Review after Five Years. J Bone Joint Surg 1987;69B:719.
JM, Milburn LJ, Haggerty JF, Nishimoto D. Dislocated Acromioclavicular
Joint: Follow-up Study of 35 Unreduced Acromioclavicular Dislocations. Am J Sports Med 1977;5:264.
DJ, Johnson EE. Avulsion Fracture of the Coracoid Associated with
Acromioclavicular Dislocation: Case Report and Review of the
Literature. J Orthop Trauma 1993;7:381.
R, Wain S, Apple J, Martinez S. Osteoarthritis of the Sternoclavicular
Joint: Radiographic Features and Pathologic Correlation. Invest Radiol 1986;21:226.
RW, Gutowski WT. The Migration of a Broken Pin Following Fixation of
the Acromioclavicular Joint: A Case Report and Review of the
Literature. Orthopedics 1986;9:413.
RW, Leach JA. Sternoclavicular Osteomyelitis and Pyoarthrosis as a
Complication of Subclavian Vein Catheterization: A Case Report and
Review of the Literature. Orthopedics 1984;7:1017.
A, Marco L, Cebrian R. Acute Dislocation of the Acromioclavicular
Joint. Traumatic Anatomy and the Importance of Deltoid and Trapezius. J Bone Joint Surg 1994;76BN:602.
PB, Alexander MJ, Frejuk J, Johnson G. Comprehensive Functional
Analysis of Shoulders Following Complete Acromioclavicular Separation. Am J Sports Med 1988;16:475.
T, Rodriguez-Merchan C, Munuera-Martinez L. Fracture of the Coracoid
Process: Presentation of Seven Cases and Review of the Literature. J Trauma 1993;30:1597.
JF. Arthroscopic Debridement of the Acromioclavicular Joint and Distal
Clavicle Resection. In: McGinty JB, Caspari RB, Jackson RW, et al, eds.
Operative Arthroscopy. New York: Raven Press, 1991;557.
T, Stuyek J, Fabry G. Conservative Treatment of Acromioclavicular
Dislocation: Evaluation of Functional and Radiological Results after
Six Years Follow-up. Acta Orthop Belg 1993;59:255.
H. Llewellyn RC. Migration of a Threaded Steinmann Pin from an
Acromioclavicular Joint into the Spinal Canal: A Case Report. J Bone Joint Surg 1965;46A:1024.
CA Jr, Odor JM. Spontaneous Atraumatic Anterior Subluxations of the
Sternoclavicular Joint in Young Adults: Report of 37 Cases (Abstract). Orthop Trans 1988;12:557.
SV, Haarsma SM, Speeckaert MTC. Conservative Treatment of
Acromioclavicular Dislocation: Jones Strap vs. Mitella (Abstract). Acta Orthop Scand 1984;55:483.
H, Azuma A, Okai K, et al. Inter-sterno-costo-clavicular Ossification
with a Special Reference to Cases of Unilateral Type. Kanto J Orthop Traumatol 1978;9:196.
H, Furusawa S, Seki H, et al. Four Cases with Symmetrical Ossifications
between the Clavicles and the First Ribs of Both Sides. Kanto J Orthop Traumatol 1974;5:244.
T, Ishikwaw S, Tanaka S, et al. Development of Significant
Sternoclavicular Joint Hypertrophy Following Radical Neck Dissection. Otorhinolaryngology 1989;51:317.
JG, Eftekhari F, Haskin ME. Erosion of the Sternal Ends of the
Clavicles: A New Sign of Primary and Secondary Hyperparathyroidism. Radiology 1974;113:323.
J, Jaskiewicz A. [Idiopathic Displacement of Kirschner Wire to the
Thoracic Cavity after the Osteosynthesis of Acromioclavicular Joint.] Chir Narzadow Ruchu Ortop Pol 1984;49:399.
MR. Complete Dislocation of the Acromioclavicular Joint: The Nature of
the Traumatic Lesion and Effective Methods of Treatment with an
Analysis of 41 Cases. J Bone Joint Surg 1946;28:813.
WM, Peterson DA, Shelton G, Newmann RD. Shoulder Strength Following
Acromioclavicular Dislocation and Coracoclavicular Ligament Rupture: A
Case Report and Review of the Literature. Clin Orthop 1994;300:120.
K, Hsu K, Shih C. Coracoid Process Fracture Combined with
Acromioclavicular Dislocation and Coracoclavicular Ligament Rupture: A
Case Report and Review of the Literature. Clin Orthop 1994;300:120.
KM, Colwill JC. Combined Acromioclavicular Dislocation with
Coracoclavicular Ligament Disruption and Coracoid Process Fracture. Am J Sports Med 1989;17:697.